Pill to dry up breast milk
Stopping breastfeeding after the loss of your baby or child
Stopping breastfeeding after the loss of your baby or child
Breast milk may still be produced by your body after the loss of your baby or child. Producing milk is distressing for some women and comforting for others. Some women feel their milk is the last link they have to their baby or child.
Producing milk is distressing for some women and comforting for others. Some women feel their milk is the last link they have to their baby or child.
Your breast milk can be stopped naturally or with medication.
Using medication to stop your breast milk
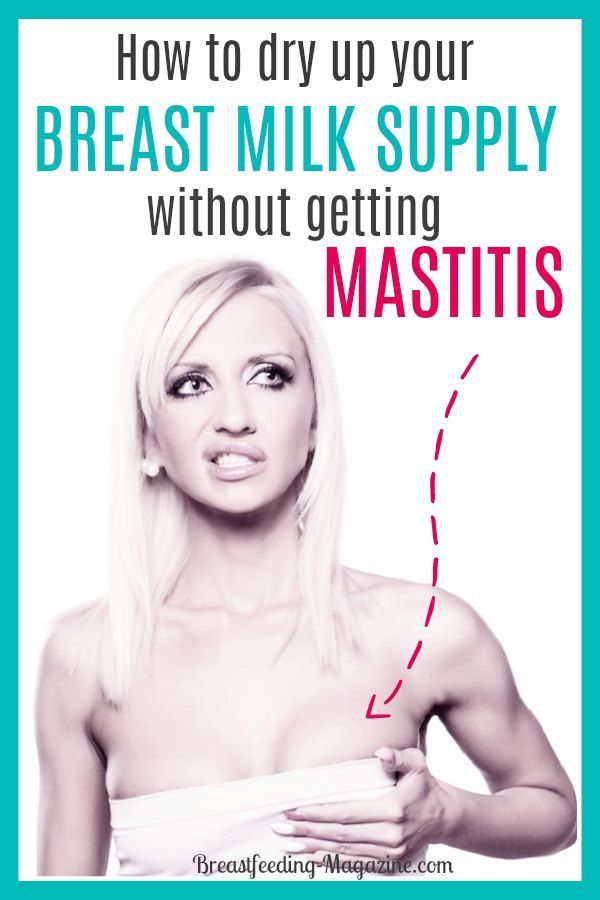
Taking drugs such as Cabergoline or Dostinex® to stop breast milk works best for mothers who have not been breastfeeding for long.
Talk to your doctor, midwife or nurse if you would like more information about these drugs.
Stopping your breast milk naturally
- Express only enough breast milk for comfort.
The more you express, the more breast milk you will produce.
- For the first 1 to 2 days express each breast every 4 hours, but only for 5 minutes. The aim is not to empty your breasts completely, but enough to be comfortable.
- For the next few days express every 5 hours, but only for 3 to 4 minutes.
- Then just express a few times a day to keep your breasts from feeling full.
- It may take from several days to weeks for breast milk to stop being produced.
- Wear a firm supportive bra.
- Drink if you are thirsty. Drinking less will not stop your breast milk from being produced.
Pain management advice
- If you get very full or heavy breasts, have a warm shower or use a heat pack for a few minutes before expressing.
- If you get lumps, red or sore spots, massage the lumps while expressing.
- Use cold packs on your breasts after expressing if they are sore or swollen.

- Use pain medicine if needed (for example paracetamol or ibuprofen).
- Refer to your midwife or doctor for any advice
You may develop mastitis
Mastitis is pain and swelling of the breast. There is usually a painful red area on the breast. You may feel like you have the flu.
If this does not get better in 12 to 24 hours or you feel very ill, see your doctor, as you might need antibiotics.
If you have mastitis you may have to empty the breast fully until this clears, then return to the plan above.
Can my milk be used for another baby?
The Perron Rotary Express Milk (PREM) Bank (external site) collects breast milk from healthy screened donors, processes it to ensure safety, and provides it to sick and premature babies.
Contact the PREM Bank on phone 9340 1563 to discuss donating your breast milk.
Who can I call for advice?
Australian Breastfeeding Association
- Phone: 1800 686 268.

- Visit the Australian Breastfeeding Association website (external site).
You can also contact:
- your local child health nurse
- your local GP.
Acknowledgements
Paediatric Palliative Care, Child and Adolescent Health Service – Community Health
This publication is provided for education and information purposes only. It is not a substitute for professional medical care. Information about a therapy, service, product or treatment does not imply endorsement and is not intended to replace advice from your healthcare professional. Readers should note that over time currency and completeness of the information may change. All users should seek advice from a qualified healthcare professional for a diagnosis and answers to their medical questions.
7 Methods to Try and 3 to Avoid
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
If you buy through links on this page, we may earn a small commission Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Certain medications and herbs may help dry up your breast milk production. But stopping breastfeeding abruptly may cause side effects.
There are many reasons why you may want to quickly dry up your breast milk supply. This process of drying up breast milk is called lactation suppression.
Whatever the case, weaning slowly and without stress is best for both you and your baby. The ideal time to wean is when both the lactating parent and the infant are ready.
Sometimes, you have to discontinue breastfeeding more quickly than you wish. Several factors will affect how long it takes for your milk to dry up, including your baby’s age and how much milk your body’s making.
Some people may stop producing over just a few days. For others, it may take several weeks for their milk to dry up completely. It’s also possible to experience let-down sensations or leaking for months after suppressing lactation.
Weaning gradually is recommended, but it may not always be feasible. That said, abrupt weaning may be uncomfortable and lead to infection or other medical issues. Speak with your doctor, midwife, or lactation consultant about your options before trying any of these methods.
Your milk can slow on its own if you don’t breastfeed or stimulate your breasts. Depending on how long you’ve been breastfeeding, it may take time.
Keep these tips in mind when trying this method:
- Wear a supportive bra that holds your breasts in place.
- Use ice packs and over-the-counter pain (OTC) medications to help with pain and inflammation.
- Hand express milk to ease engorgement. Do this sparingly so you don’t continue to stimulate production.
Try it: Shop for ice packs and anti-inflammatory medications.
Sage may help with weaning or oversupply issues, according to one 2014 article. However, there are no studies that examine sage’s specific effect on excess milk production.
Not much is known about the safety of using sage if your infant consumes your breastmilk after you’ve consumed sage.
You should start with a small amount of sage and see how your body reacts. Herbal teas containing sage are available. These could easily be diluted until you find an amount that works best for you.
These could easily be diluted until you find an amount that works best for you.
According to the 2014 article, other herbs that have the potential to dry up breast milk include:
- peppermint
- chasteberry
- parsley
- jasmine
Little is known about the effect of these herbs on infants, but some can be dangerous to a baby. Because herbal substances can cause negative side effects for you or your baby, you should talk with your healthcare provider or lactation consultant before using these methods.
Try it: Shop for sage tea (including ones intended for use during weaning), chasteberry tea, and parsley.
Also shop for peppermint oil and jasmine flowers, which can both be applied topically.
Cabbage leaves may suppress lactation when used for long periods of time, though more studies are needed.
To use cabbage:
- Take apart and wash the leaves of a green cabbage.
- Put the leaves in a container and put the container in the refrigerator to chill.

- Place one leaf over each breast before putting on a bra.
- Change leaves once they’ve wilted, or about every two hours.
The leaves may help to reduce swelling as your milk supply diminishes. They’re also used to reduce symptoms of engorgement in early breastfeeding.
Try it: Shop for cabbage.
Progestin-only birth control doesn’t necessarily impact supply. Contraceptive pills that contain the hormone estrogen, on the other hand, may work well for suppressing lactation.
These effects are even notable after milk supply is well-established.
Not everyone will experience these suppressive effects, but many will. Talk with your medical provider about the recommended timing for starting a pill containing estrogen when you’re postpartum.
Birth control isn’t approved for this use by the U.S. Food and Drug Administration (FDA), but it may be prescribed in certain situations. This is known as off-label drug use.
Off-label drug useOff-label drug use means a drug that’s approved by the FDA for one purpose is used for a different purpose that hasn’t yet been approved.
However, a doctor can still use the drug for that purpose. This is because the FDA regulates the testing and approval of drugs, but not how doctors use drugs to treat their patients. So, your doctor can prescribe a drug however they think is best for your care.
In a small study in 2003 of 8 lactating women, a single 60-milligram (mg) dose of the cold medicine pseudoephedrine (Sudafed) was shown to significantly reduce milk production.
In addition, taking the daily maximum dose of this medication didn’t adversely affect babies who continued breastfeeding as lactation was being suppressed. The maximum dose is 60 mg, four times each day (maximum 240mg in any 24-hour period).
Talk to your healthcare professional before you take any OTC medication while breastfeeding. Sudafed is used off-label to dry up breast milk and may cause irritability in breastfed infants.
Try it: Shop for Sudafed.
If you haven’t breastfed your infant yet, high doses of vitamins B-1 (thiamine), B-6 (pyridoxine), and B-12 (cobalamin) may work to suppress lactation.
A study from the 1970s showed that high doses B-6, B-1, and B-12 suppressed lactation for 96 percent of the participants, with no unpleasant side effects.
More recent studies, including ones from a 2017 literature review, have presented conflicting information regarding the effectiveness of this option.
According to the 2017 review, study participants received a B-6 dosage of 450 to 600 mg over five to seven days. Two of the studies included found that vitamin B-6 was effective in suppressing lactation, but the other five studies did not.
There’s not much known about the negative effects of taking too much vitamin B-1 or B-12, or how long it’s safe to take elevated doses.
However, at doses of more than 200mg per day, vitamin B-6 can cause a loss of feeling in the arms and legs. In some cases, with prolonged use, this effect can become permanent.
You should talk with your healthcare provider or lactation consultant before starting a new vitamin supplement.
Try it: Shop for vitamin B-1, vitamin B-6, and vitamin B-12 supplements.
Cabergoline can be used for milk suppression. It works by stopping the body’s production of prolactin.
This drug isn’t approved for this use by the FDA, but may be prescribed off-label. Your doctor can explain the benefits and risks.
Some people see their milk dry up after just one dose of medication. Others may need additional doses.
Not much is known about the safety of cabergoline for breastfed infants whose lactating parents took cabergoline. You should talk with your healthcare provider or lactation consultant before taking it.
Some milk-suppressing medications you may have heard of — such as bromocriptine — are no longer recommended for this use because of long-term side effects.
Women also used to get a shot of high-dose estrogen to stop milk production. This practice has stopped due to blood clotting risks.
The following are some methods you may have heard about anecdotally, but which are unproven or potentially dangerous.
1. Binding
Binding means to tightly wrap the breasts. Breast binding has been used throughout history to help women stop producing breast milk.
In a 2003 study on non-breastfeeding, postpartum women, the effects of binding were compared to those of wearing a support bra.
While the engorgement symptoms for both groups didn’t differ significantly over the first 10 days, the binding group did experience more pain and leakage overall. As a result, researchers don’t recommend binding.
A supportive bra or a gentle binding helps better support the tender breasts when moving and can reduce the discomfort.
2. Restricting fluids
Breastfeeding parents are often told to stay hydrated to maintain their milk supplies. You may wonder if restricting fluid intake may have the opposite effect. This method isn’t well studied.
Researchers have discovered that increasing fluids may not actually increase supply. Without clear evidence that drinking more increases (or decreases) supply, it’s best to stay hydrated regardless.
3. Pregnancy
If you become pregnant while breastfeeding, your milk supply or the taste of your milk may change. Breastfeeding advocacy group La Leche League explains that it’s common to see a drop in supply between the fourth and fifth months of pregnancy.
Since the changes vary by individual, pregnancy isn’t a reliable “method” for drying up breast milk. Many people breastfeed successfully throughout their pregnancy.
Gradual weaning is generally the safest plan, when possible.
How long it takes for milk to dry up depends on the method you try and how long you’ve been breastfeeding. It may take just a few days, or up to several weeks or months, depending on your method of lactation suppression and your current supply.
Even after most of your milk is gone, you may still produce some milk for months after you wean. If your breast milk comes back in without any reason, talk to your medical team.
Abruptly stopping breastfeeding does come with the risk of engorgement and the potential for blocked milk ducts or infection.
You may need to express some milk to relieve the feeling of engorgement. However, the more milk you express, the longer it’ll take to dry up.
Lactation suppression can be uncomfortable at times, but if you experience pain and other worrisome symptoms, call your doctor, midwife, or lactation consultant.
Sometimes, a plugged duct will lead to breast tenderness. Gently massage the area while expressing or breastfeeding.
Contact a medical professional if you can’t unblock a milk duct within 12 hours or if you have a fever. A fever is a symptom of a breast infection such as mastitis.
Other symptoms of a breast infection include:
- warmth or redness
- general malaise
- breast swelling
Sometimes, oral antibiotics are recommended to help treat this condition before it becomes more serious.
You can also contact a certified lactation consultant. These professionals are trained in all things breastfeeding and can suggest different methods or help troubleshoot any issues you’re having.
Drying up your milk supply is a highly individual decision and is sometimes necessary for a variety of reasons.
If you’re weaning due to a medical condition (or other reasons), but still want to provide breast milk for a baby, there are milk banks across the United States and Canada. You can find one through the Human Milk Banking Association of North America (HMBANA).
The breast milk is tested and pasteurized so it’s safe for consumption. These organizations also take donations from parents who’ve either lost a child or otherwise wish to donate their milk.
Instructions for use, home delivery
Characteristics
| Pack quantity | 50 pcs |
| Maximum allowable storage temperature, °С | 25 °C |
| Expiration date | 36 months |
| Storage conditions | In a dry place In a place protected from the sun Keep out of the reach of children |
| Form | Coated tablets |
| Country of origin | Russia |
| Release procedure | Prescription |
| Pharmacological group | N05AN01 Lithium |
| Registered as | Medicine |
Description
round biconvex white film-coated tablets.![]() In cross section, the nucleus is white or almost white.
In cross section, the nucleus is white or almost white.
Active substances
Carbonate Carbonate
Form of release
tablets
Composition
Substances: 300 mg
Excipients: Nucleus: Nucleus: Magic starch - 14.62 MHI, CROSKAREMEN (primellose) - 20.00 mg, povidone (polyvinylpyrrolidone, povidone K-25) - 55.38 mg, talc - 6.00 mg, calcium stearate - 4.00 mg
shell: hypromellose (hydroxypropyl methylcellulose) 15 cps - 5.87 mg, povidone (polyvinylpyrrolidone, povidone K-25) - 1.837 mg, polysorbate 80 (tween-80) - 0.543 mg, titanium dioxide - 2.10 mg, talc - 1.65 mg.
Pharmacological effect
Normothymic agent (normalizes the mental state without causing general lethargy), also has antidepressant, sedative and antimanic effects. The effect is due to lithium ions (Li +), which, being antagonists of sodium ions (Na +), displace them from cells and, thereby, reduce the bioelectric activity of brain neurons. Accelerates the breakdown of biogenic amines (the content of norepinephrine and serotonin in the brain tissues decreases). Increases the sensitivity of hippocampal neurons and other areas of the brain to the action of dopamine. Interacts with lipids formed during the metabolism of inositol.
Accelerates the breakdown of biogenic amines (the content of norepinephrine and serotonin in the brain tissues decreases). Increases the sensitivity of hippocampal neurons and other areas of the brain to the action of dopamine. Interacts with lipids formed during the metabolism of inositol.
At therapeutic concentrations, it blocks the activity of inosyl-1-phosphatase and reduces the concentration of neuronal inositol, which plays a role in the regulation of neuronal sensitivity.
The beneficial effect of lithium preparations in migraine may be associated with a change in serotonin concentrations in depression with an increase in serotonergic activity and a decrease in the regulation of beta-adrenergic receptor function.
Pharmacokinetics
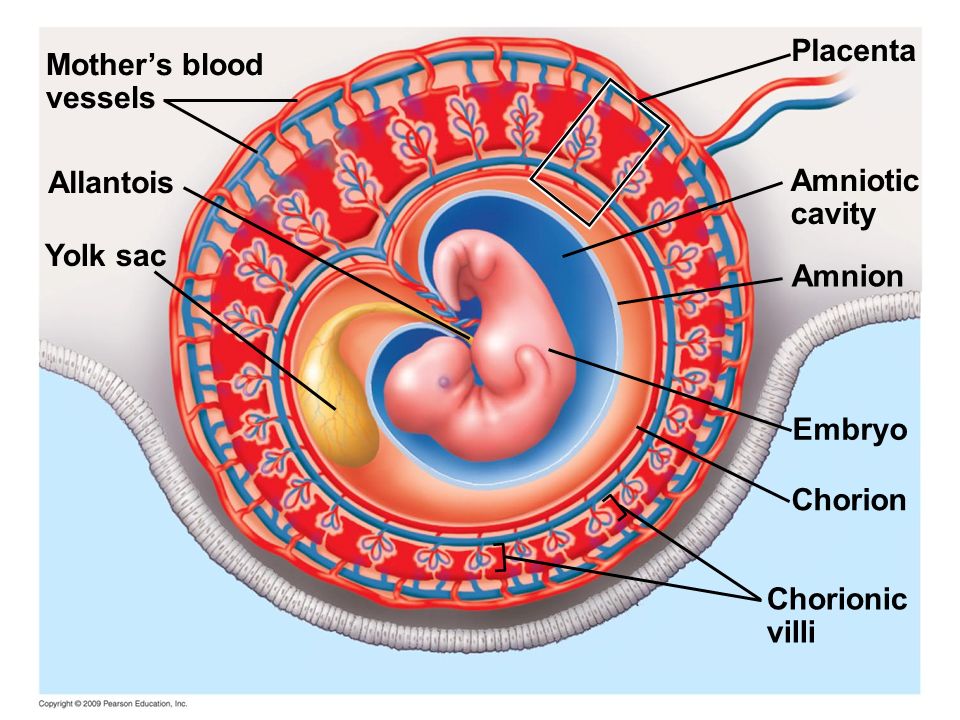
Absorption is rapid and complete within 6-8 hours. Does not bind to blood proteins. Therapeutic range of concentrations in the blood ranging from 0.6 to 1.2 mmol / l. The time to reach the maximum concentration in the blood (Cmax) is 1-3 hours. Stable serum concentration is reached after 4 days. The drug penetrates the blood-brain barrier (BBB) (concentrations in the cerebrospinal fluid are half the level in plasma), the placental barrier, penetrates into breast milk. Biotransformation is not subjected. The half-life (T1 / 2) in adults is 24 hours, in adolescents - 18 hours, in the elderly up to 36 hours. The values of T1 / 2 depend on the amount of Na + ions in the plasma. Excreted by the kidneys - 95%, with faeces - less than 1%, with sweat - 4 5%. Excretion by the kidneys depends on the ratio of the concentrations of Li +, Na + and K + ions in the blood.
Stable serum concentration is reached after 4 days. The drug penetrates the blood-brain barrier (BBB) (concentrations in the cerebrospinal fluid are half the level in plasma), the placental barrier, penetrates into breast milk. Biotransformation is not subjected. The half-life (T1 / 2) in adults is 24 hours, in adolescents - 18 hours, in the elderly up to 36 hours. The values of T1 / 2 depend on the amount of Na + ions in the plasma. Excreted by the kidneys - 95%, with faeces - less than 1%, with sweat - 4 5%. Excretion by the kidneys depends on the ratio of the concentrations of Li +, Na + and K + ions in the blood.
Indications
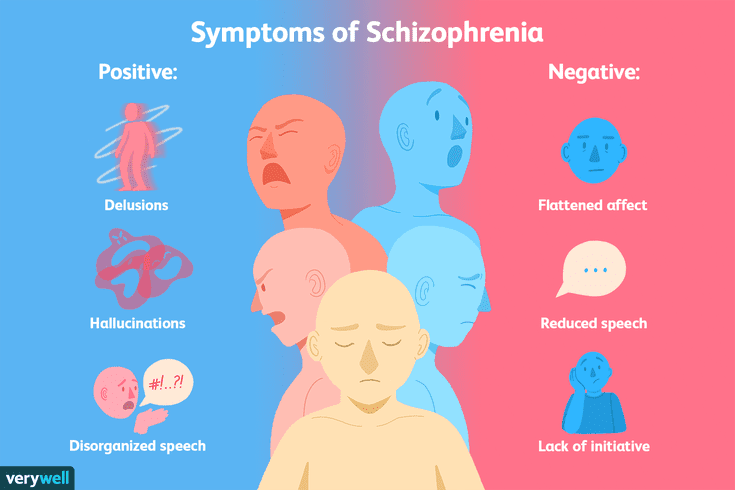
Manic and hypomanic states of various origins, affective psychoses (manic-depressive, schizoaffective), alcoholism (affective disorders), migraine, Meniere's syndrome, sexual disorders, drug dependence (some forms).
Contraindications
Hypersensitivity to lithium and other components of the drug severe surgical interventions leukemia pregnancy, breastfeeding period children under 12 years of age (efficacy and safety of use have not been established) diseases of the cardiovascular system associated with heart rhythm disturbances presence of Brugada syndrome / family history of Brugada syndrome severe renal failure untreated or uncompensated hypothyroidism low sodium levels in the body, for example, in patients with dehydration, patients on a low-salt diet, or patients with Addison's disease.
Precautions
Precautions: diseases of the cardiovascular system (including atrioventricular and intraventricular blockade), diseases of the central nervous system (epilepsy, parkinsonism), diabetes mellitus, thyrotoxicosis, hyperparathyroidism, infections, psoriasis, renal insufficiency, urinary retention.
Use in pregnancy and lactation
Sedalit® is contraindicated during pregnancy, especially during the first trimester, unless lithium therapy is strictly necessary.
Lithium carbonate crosses the placental barrier. The use of lithium carbonate during pregnancy, especially in the first trimester, increases the risk of congenital malformations, mainly of the cardiovascular system: especially Ebstein's anomalies (right ventricular hypoplasia and tricuspid valve insufficiency).
If pregnancy occurs while using the drug, the patient should be warned about the possible risks to the fetus. As a prenatal diagnosis, such patients need an ultrasound examination, as well as an electrocardiogram of the newborn in the postnatal period.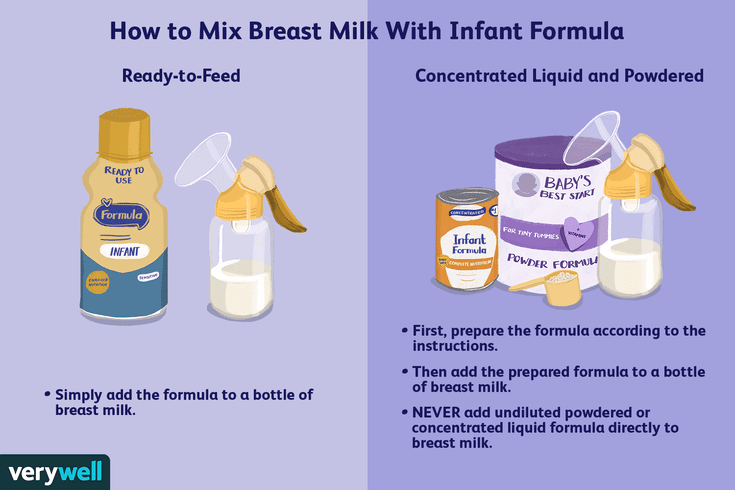
In certain cases where the withdrawal of lithium is associated with a serious risk to the patient, treatment during pregnancy may be continued.
If continued lithium therapy during pregnancy is necessary, serum lithium levels should be closely monitored by frequent measurements. This is due to a gradual change in kidney function during pregnancy, and a sharp change during childbirth. The dose must be adjusted. Lithium intake is recommended to stop shortly before childbirth and resume - a few days after them.
Newborns with signs of lithium intoxication require fluid therapy. Newborns with low blood lithium concentrations may have a lethargic appearance that does not require special treatment.
Women of childbearing potential
Women receiving lithium carbonate should use adequate methods of contraception. When planning pregnancy, lithium therapy should be discontinued.
Breastfeeding period
Lithium carbonate is known to pass into breast milk, so if it is necessary to use the drug during lactation, the issue of abolishing breastfeeding should be considered.
Method of administration and doses
Inside (for 3-4 doses, the last time before bedtime), after meals, the initial dose is 0.6-0.9 g / day, followed by an increase to 1.2 g / day day, then the dose is increased daily by 0.3 to reach a daily dose of 1.5-2.1 mg, the maximum daily dose is 2.4 g. During the selection of therapy, the concentration of Li + ions in plasma should not be lower than 0.6 and not higher 1.2 -1.6 mmol / l. In doses exceeding 2 g / day, the duration of treatment is 1 - 2 weeks.
After the disappearance of manic symptoms, the daily dose is gradually reduced to a prophylactic dose (0.6 - 1.2 g). If, after a dose reduction, signs of mania reappear, the dose is increased.
In acute manic state, the therapeutic concentration of Li+ ions in the blood should be 0.8 - 1.2 mmol/l, with maintenance treatment - 0.4 - 0.8 mmol/l if the concentration of Li+ ions exceeds 1.2 mmol/l the daily dose should be reduced.
A positive result of prophylactic monotherapy is manifested by maintaining a stable blood concentration in the range of 0. 4 - 0.8 mmol / l for at least 6 months, for children - at a dose that allows maintaining therapeutic concentrations in the range of 0.5 - 1 mmol / l.
4 - 0.8 mmol / l for at least 6 months, for children - at a dose that allows maintaining therapeutic concentrations in the range of 0.5 - 1 mmol / l.
Side effects
Side effects are presented depending on the effect on organs and organ systems.
Side effects are usually dependent on the serum lithium concentration and are less common in patients with lithium levels below 1.0 mmol/L.
Initiation of therapy may be accompanied by fine hand tremors, polyuria and thirst.
From the circulatory and lymphatic systems: leukocytosis.
From the side of the immune system: an increase in the titer of antinuclear antibodies.
From the endocrine system: disorders of the thyroid gland, including (euthyroid) goiter, hypothyroidism and hyperthyroidism, hyperparathyroidism, parathyroid adenoma.
From the side of metabolism and nutrition: hypercalcemia hypermagnesemia hyperglycemia anorexia weight gain.
From the nervous system: coma idiopathic intracranial hypertension irreversible lithium neurotoxicity syndrome (SILENT) encephalopathy stupor, convulsions neuroleptic malignant syndrome myasthenia gravis serotonin syndrome parkinsonism, symptoms of extrapyramidal disorders ataxia dizziness memory disorders, mild cognitive impairment in case of long-term use nystagmus slurred speech vertigo revival deep tendon reflexes lethargy fine hand tremor.
On the part of the organs of vision: scotoma and blurred vision.
From the side of the heart: cardiac arrest ventricular fibrillation ventricular tachycardia ventricular arrhythmia torsades de pointes tachycardia prolongation of the QT interval cardiomyopathy arrhythmia bradycardia sinus node dysfunction ECG changes.
From the vascular side: peripheral circulatory failure, hypotension.
From the gastrointestinal tract: gastritis nausea diarrhea vomiting dry mouth excessive salivation. Lithium salts can cause taste perversion.
From the side of the skin and subcutaneous tissue: allergic rash exacerbation of psoriasis acne alopecia acne papular rashes folliculitis itching rash.
From the musculoskeletal system and connective tissue: muscle weakness.
From the side of the kidneys and urinary tract: symptoms of nephrogenic diabetes insipidus renal failure irreversible changes in the kidneys nephrotic syndrome histological changes in the kidneys with interstitial fibrosis after long-term use of polyuria polydipsia.
From the reproductive system and breast: sexual dysfunction.
General disorders and reactions at the injection site: sudden death edema asthenia lethargy thirst fatigue and malaise may be due to lithium intoxication.
Some side effects are noted with an increase in the level of lithium in the blood - see the symptoms in the "Overdose" section.
Overdose
Lithium carbonate has a narrow "therapeutic window". Symptoms of lithium overdose (lithium intoxication) may be due to concomitant diseases, iatrogenic and poisoning.
Any overdose in a patient on long-term lithium therapy should be considered a potentially serious condition.
Acute overdose
Acute overdose usually carries little risk in patients experiencing only mild symptoms, regardless of serum lithium concentration. However, later, with a decrease in the rate of excretion of lithium due to the presence of kidney failure, more severe symptoms may appear. The lethal dose in a single dose is likely to be greater than 5 g.
Acute overdose in patients on long-term lithium therapy
Acute overdose in a patient on long-term lithium therapy can result in severe toxic effects, even with moderate overdose, because the extravascular tissues are already saturated with lithium.
Patients with elevated blood lithium concentrations are at higher risk of toxic exposure in the presence of the following pathological conditions: arterial hypertension, diabetes mellitus, congestive heart failure, chronic renal failure, schizophrenia, Addison's disease.
Symptoms
The onset of symptoms may be delayed; their maximum severity may not reach earlier than 24 hours, especially in patients who do not receive long-term lithium therapy.
Mild symptoms: nausea diarrhea blurred vision polyuria dizziness fine rest tremor muscle weakness and drowsiness.
Moderate symptoms: progressive confusion loss of consciousness fasciculations revitalization of deep tendon reflexes myoclonic muscle contractions and twitches choreoathetoid movements urinary or fecal incontinence progressive agitation followed by stupor hypernatremia.
Severe symptoms: coma convulsions cerebellar symptoms cardiac arrhythmias including sinoatrial block sinus and nodal bradycardia first degree heart block hypotension or rarely hypertension vascular insufficiency renal insufficiency.
Tactics
There is no known antidote for lithium poisoning.
In case of accumulation of lithium, it is necessary to stop taking it and evaluate its concentration in the blood every six hours. Particular attention should be paid to maintaining fluid and electrolyte balance, as well as kidney function. Forced diuresis and diuretics should not be used under any circumstances. Required supportive care may include measures to control hypotension and seizures.
All patients must be observed for a minimum of 24 hours. If symptoms are present, ECG monitoring is necessary. Measures should be taken to correct hypotension.
When taking the drug in a dose of more than 4 g, an adult or a significant amount of a child needs gastric lavage - no later than an hour later. With chronic accumulation, intestinal decontamination is not effective.
With chronic accumulation, intestinal decontamination is not effective.
Note: activated carbon does not absorb lithium.
In severe poisoning, hemodialysis is the treatment of choice. It should be prescribed to all patients with severe neurological symptoms. This method is most effective for rapidly lowering lithium levels. However, after the cessation of dialysis, its reverse increase may be noted. This may require prolonged or repeated treatment.
Hemodialysis may also be indicated for acute overdose, acute overdose on long-term therapy, overdose on long-term therapy in symptomatic patients, regardless of serum lithium concentration.
Note: Improvement usually takes longer than reduction in serum lithium, regardless of the method used.
Interactions with other medicinal products
Interactions may occur as a result of an increase or decrease in the concentration of lithium, or through other mechanisms, the most important of which is neurotoxicity, which can occur at therapeutic concentrations of lithium when co-administered with other drugs, centrally affecting the CNS.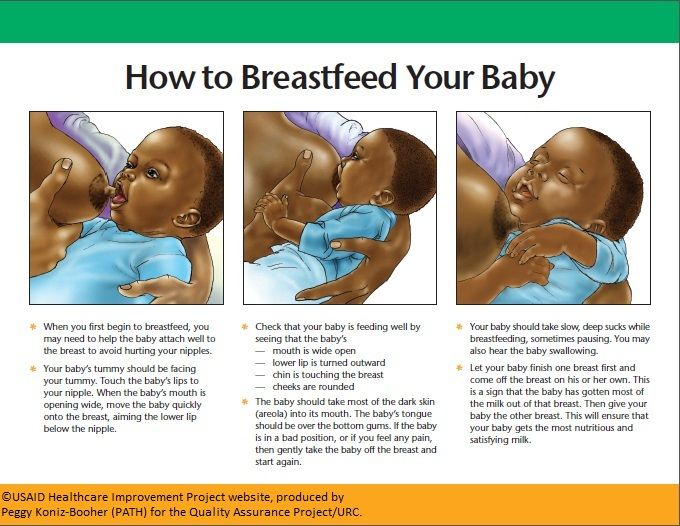
Interactions leading to increased serum lithium concentrations
Co-administration of the following medicinal products may lead to increased lithium concentrations and a risk of toxic effects:
thus toxic effects. If the use of the drug is strictly necessary, careful monitoring of the level of lithium in the blood and dose adjustment, if necessary, is required.
Antibiotics (metronidazole, tetracycline, co-trimoxazole, trimethoprim). N.B. Symptoms of toxic effects may occur at low or normal lithium concentrations when co-administered with co-trimoxazole or trimethoprim. Toxic effects of lithium have been reported in isolated cases in patients taking spectinomycin.
Non-steroidal anti-inflammatory drugs (including selective COX-2 inhibitors) in case of initiation or discontinuation of therapy with non-steroidal anti-inflammatory drugs, more frequent monitoring of serum lithium concentrations is necessary.
Drugs affecting the renin-angiotensin system (ACE inhibitors, angiotensin II receptor antagonists).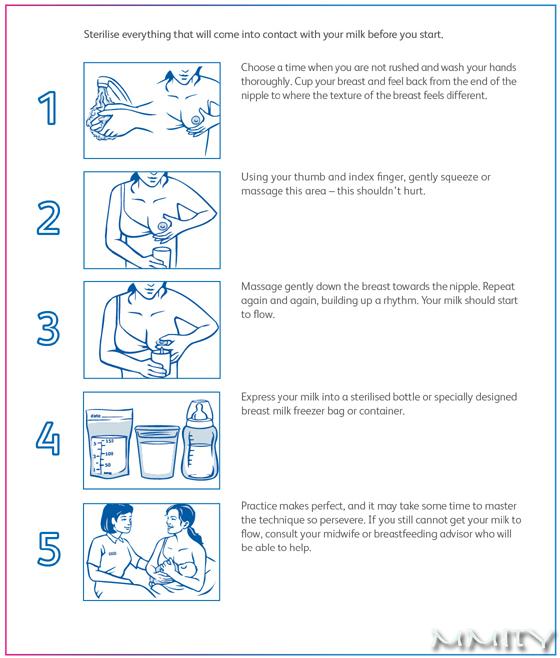
Diuretics (including herbal preparations). In addition to the effects noted above, thiazide diuretics exhibit a paradoxical antidiuretic effect, resulting in possible water retention and lithium toxicity. Loop diuretics (furosemide and bumetanide, ethacrynic acid) are less likely to cause lithium retention, however, care must be taken.
Other drugs that affect electrolyte balance, such as steroids, may change the rate of lithium excretion, and therefore their combined use should be avoided.
Interactions leading to decreased serum lithium concentrations:
Co-administration of the following drugs may result in decreased lithium concentrations and risk of reduced efficacy:
xanthine derivatives (eg, theophylline, caffeine)
Preparations containing large amounts of sodium, such as sodium bicarbonate
Carbonic anhydrase inhibitors
Urea.
Interactions that may not be associated with an increase or decrease in the concentration of lithium:
The co-administration of the following drugs may precipitate the onset of symptoms of toxic effects when the concentration of lithium is within the normal range:
Antipsychotics, including atypical antipsychotics: high doses olanzapine, clozapine and haloperidol
Karbamazepin
Phenytoin
methyldop
Clonazepam
Tricyclic and tetracyclic antidepressants
Calcium Calcium Calcians. These drugs can cause neurotoxic reactions in
These drugs can cause neurotoxic reactions in
Neuromuscular blockers can cause neurotoxic reactions.
Selective serotonin reuptake inhibitors: co-administration with lithium may exacerbate serotonin syndrome.
Non-steroidal anti-inflammatory drugs, including selective COX-2 inhibitors: Serum lithium levels should be monitored more frequently when starting or stopping treatment with non-steroidal anti-inflammatory drugs.
Triptans: toxic effects of lithium resembling serotonin syndrome have been noted.
Neuromuscular blockers: Lithium may prolong the effect of neuromuscular blockers.
Drugs that lower seizure threshold
Caution is advised when lithium is coadministered with drugs that lower the seizure threshold, such as antidepressants, antipsychotics, anesthetics, and theophylline.
Drugs that prolong the QT interval
Lithium may prolong the QT interval, especially when its concentration in the blood is high. Therefore, co-administration of drugs with a potential risk of QT interval prolongation should be avoided, and other potential risk factors should be taken into account, such as: older age, female sex, congenital long QT syndrome, heart and thyroid diseases, and such disorders.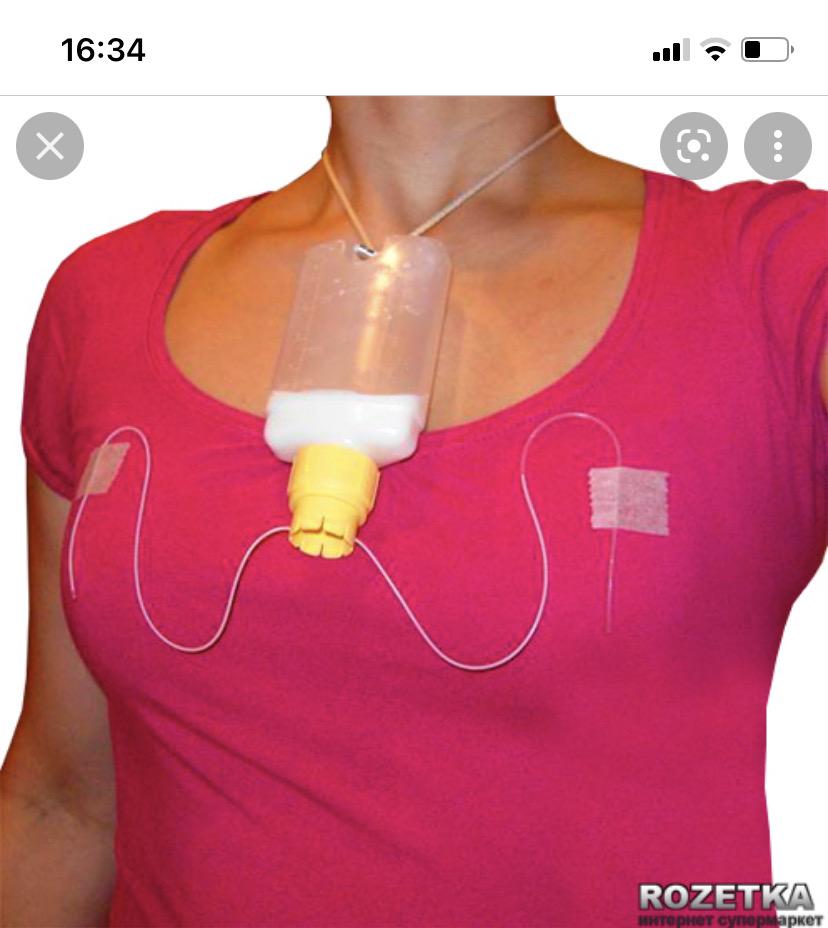 metabolism such as hypokalemia, hypocalcemia and hypomagnesemia.
metabolism such as hypokalemia, hypocalcemia and hypomagnesemia.
The following drugs can cause QT interval prolongation and torsades de pointes:
Class Ia antiarrhythmics (aimalin, cybenzoline, disopyramide, hydroquinidine, procainamide, quinidine)
, ibutilide, sotalol)
Antipsychotics (amisulpride, haloperidol, droperidol, mesoridazine, pimozide, sertindole, thioridazine and clozaril)
Antibiotics (erythromycin, sparfloxacin with intravenous administration)
Antagonists of serotonin receptors (ketanserin, dolasetron of mesilate)
Antihistamines (astemizole, terphenin)
Cesides, miflohin, gallophanthrines)
000ol and ranolazine.
ECG monitoring should be performed after initiation of treatment if the patient develops symptoms or changes in the course of the disease or therapy associated with an increased risk of interaction or arrhythmia.
Non-drug interactions:
Low sodium diet. A rapid decrease in sodium intake can cause an increase in lithium levels.
Co-morbidity may cause lithium toxicity.
Special instructions
Lithium carbonate has a narrow "therapeutic window". The required dose of the drug should be carefully selected and regularly adjusted, based on data on the concentration of lithium in the blood plasma. If it is not possible to regularly measure the concentration of lithium in the blood plasma, therapy should not be started.
Elderly patients often require lower doses of lithium to achieve therapeutic levels of the drug. They are most susceptible to the toxic effects of lithium, and lithium excretion can also be reduced. Symptoms of toxicity in elderly patients may develop at blood lithium concentrations that are satisfactorily tolerated by younger patients.
Since there is no information on the safety and efficacy of lithium carbonate in children under 12 years of age, its use in this category of patients is contraindicated.
Before prescribing long-term therapy with lithium preparations, in order to avoid the development of toxic effects, it is necessary to conduct a thorough medical examination before and during treatment. Before prescribing the drug, it is necessary to evaluate the function of the kidneys, the thyroid gland (before the start of lithium therapy, the patient must be in a euthyroid state) and the cardiovascular system, especially in patients with diseases of the cardiovascular system. Against the background of treatment, periodic evaluation of the function of the kidneys, thyroid gland and cardiovascular system is required.
Before prescribing the drug, it is necessary to evaluate the function of the kidneys, the thyroid gland (before the start of lithium therapy, the patient must be in a euthyroid state) and the cardiovascular system, especially in patients with diseases of the cardiovascular system. Against the background of treatment, periodic evaluation of the function of the kidneys, thyroid gland and cardiovascular system is required.
Lithium carbonate is known to reduce sodium reabsorption in the renal tubules, which can lead to a decrease in sodium concentration. Thus, it is essential for patients to follow a diet including adequate fluid intake (2500-3000 ml) and salt, at least during the period of stabilization. Decreased tolerance to lithium has been noted following profuse sweating or diarrhoea. In such cases, an additional intake of fluids and table salt under medical supervision is necessary, as well as a dose reduction or temporary discontinuation of the drug until the condition resolves.
During the first month of therapy, the concentration of Li + ions in the blood plasma is determined weekly, then, when a stable concentration is reached, the control is carried out monthly, then at 2-3 months. A return to weekly monitoring is required if the dosage of lithium carbonate is changed, if there is an intercurrent infectious or other serious illness, if there are significant changes in the amount of sodium and / or fluid received, if you take drugs that change the renal clearance of lithium, if you take drugs that affect the electrolyte balance.
Blood samples are always taken in the morning, ie. 12 hours after taking the last dose at night or 24 hours after taking a single dose in the morning.
When prescribing long-term lithium therapy, the physician should give patients clear instructions regarding the symptoms of developing toxicity, and also recommend prompt medical attention should such symptoms occur.
Toxic effects are expected at a serum lithium concentration of about 1. 5 mmol/l, however, they may occur at lower concentrations. If toxic effects occur, treatment must be stopped immediately and is always taken very seriously.
5 mmol/l, however, they may occur at lower concentrations. If toxic effects occur, treatment must be stopped immediately and is always taken very seriously.
May cause depression or mania at the start of treatment.
During therapy with the drug, changes in the results of laboratory tests are possible (including leukocytosis, a decrease in the concentration of thyroxine and triiodothyronine, a decrease in creatinine clearance, albuminuria, etc.).
Lithium carbonate should be discontinued 24 hours before major surgery. In case of minor surgery, treatment can be continued with proper control of fluid and electrolyte levels.
In renal insufficiency, lithium excretion is reduced, which increases the risk of developing toxic reactions. Lithium is contraindicated in severe renal failure. With mild to moderate renal failure, careful monitoring of the concentration of lithium in the blood plasma is required. Monitoring of renal function is also required in patients with polyuria and polydipsia.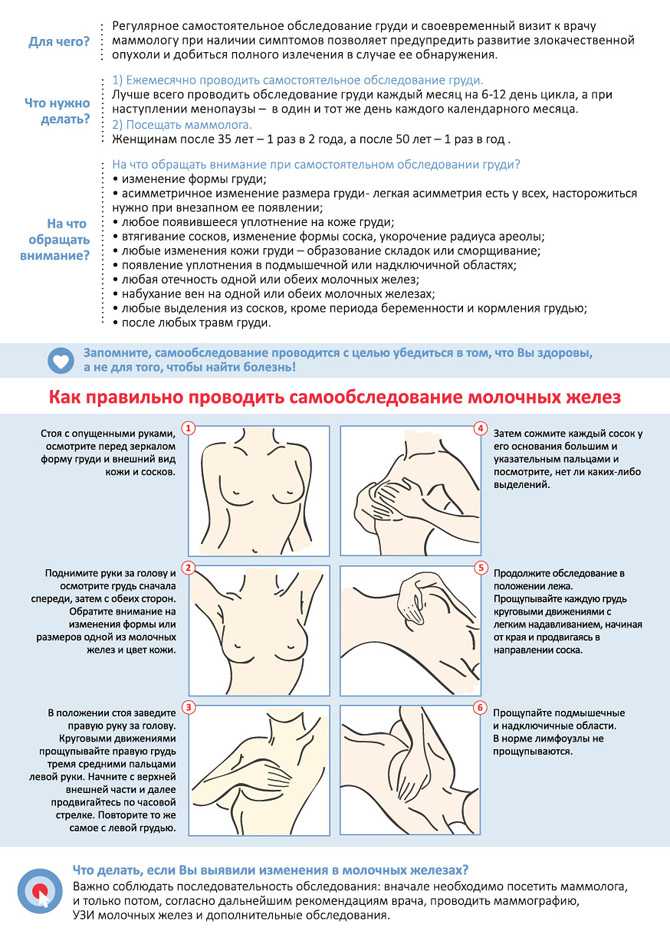
In patients on long-term lithium therapy, morphological changes in the kidneys in the form of glomerular interstitial fibrosis and nephron atrophy were noted. Morphological changes have also been noted in patients with manic-depressive states who have never been prescribed lithium. The relationship between renal function, morphological changes and lithium therapy has not been proven. In patients taking drugs that lower the epileptic threshold and in patients with epilepsy, lithium carbonate increases the risk of developing seizures.
It is not recommended to prescribe lithium carbonate together with antipsychotics. Some patients who took lithium together with antipsychotics developed an encephalopathic syndrome (characterized by weakness, apathy, fever, tremors, confusion, extrapyramidal symptoms, leukocytosis, etc.). In some cases, this syndrome was accompanied by irreversible brain damage. In connection with the existence of a possible causal relationship between the development of encephalopathic syndrome and the combined use of lithium and antipsychotics, it is necessary to carefully monitor patients on combined treatment in order to early detect neurological toxicity requiring immediate discontinuation of treatment. The encephalopathic syndrome may proceed similarly or analogously to neuroleptic malignant syndrome.
The encephalopathic syndrome may proceed similarly or analogously to neuroleptic malignant syndrome.
Do not co-administer with antipsychotics.
Lithium carbonate should be avoided in patients with congenital prolongation of the QT interval, as well as in patients taking drugs that can prolong the QT interval. Caution must be exercised in patients with risk factors for QT interval prolongation, which primarily include heart disease, bradycardia, thyroid disease, hypokalemia, hypomagnesemia, hypocalcemia, female gender, and older age.
Lithium therapy may cause or exacerbate Brugada syndrome, a hereditary sodium channel disorder with characteristic ECG changes (right bundle branch block and right precordial ST elevation), which can lead to cardiac arrest or sudden death . Lithium carbonate should not be used in patients with Brugada syndrome or a family history of Brugada syndrome. Use with caution in patients with a family history of cardiac arrest or sudden death.
Long-term therapy with the drug may be associated with a decrease in the concentration ability of the kidneys, which contributes to the development of nephrogenic diabetes insipidus, with polyuria and polydipsia. Such patients need to carefully monitor renal function, as well as the absence of dehydration due to lithium retention and its toxicity. As a rule, these changes are reversible and regress after discontinuation of drug therapy.
There is evidence of the occurrence of hyperparathyroidism and hypothyroidism, which persist after discontinuation of the drug.
There are reports of increased intracranial pressure and swelling of the optic nerve head (false brain tumor syndrome). With the development of this syndrome, drug therapy should be discontinued. Patients should be warned about the need to report cases of recurrent headache and / or visual disturbances to the doctor.
Patients on long-term lithium carbonate therapy should be instructed about symptoms of toxicity and instructed to seek immediate medical attention at the first sign of such symptoms.
During therapy with the drug, the following pathological changes on the electroencephalogram can be recorded: diffuse deceleration, expansion of the frequency spectrum, potentiation and disorganization of the background rhythm.
Storage conditions
Store below 25°C. Keep out of the reach of children.
Prescription
Yes
Arpimed
To be used only in the diagnosis of irritable bowel syndrome. Take into account the following.
Check with your doctor before using loperamide in the following cases:
If any of the above apply to you, check with your doctor before taking Loperamide.
How to take Loperamide
Loperamide should be taken exactly as directed on the package insert or as directed by your doctor. If you have any doubts, you should consult your doctor or pharmacist.
Follow the dosage below
- Take the required number of capsules without opening them with water.
 The drug is intended for oral administration only.
The drug is intended for oral administration only. - Do not take more than what is listed in the package insert.
- The drug is not intended for the long-term treatment of diarrhea.
Acute short-term diarrhea
Adults and adolescents over 12 years of age
The initial dose is 2 capsules (4 mg), followed by 1 capsule (2 mg) after each liquid bowel movement.
The duration of treatment should not exceed 48 hours. The maximum daily dose should not exceed 6 capsules.
You can replace fluid lost during diarrhea by drinking more fluid than usual.
Loperamide should not be used in children under 12 years of age.
Duration of treatment for short-term diarrhea
The duration of treatment should not exceed 48 hours. If there is no clinical improvement within 48 hours from the start of treatment for acute diarrhea, stop taking the drug and contact your doctor.
Diarrhea due to irritable bowel
Adults and adolescents over 18 years of age
Initial dose is 2 capsules (4 mg), followed by 1 capsule (2 mg) after each diarrheal bowel movement (or as prescribed by a doctor) .
- You can use the drug to treat recurring attacks for up to 2 weeks. But it should not be used in cases of diarrhea lasting more than 48 hours.
- The maximum daily dose should not exceed 6 capsules (12 mg).
- You can replace fluid lost during diarrhea by drinking more fluid than usual.
- Do not use in children and adolescents under 18 years of age.
Stop taking the drug and consult a doctor:
- If you have been using this medicine continuously for more than 48 hours.
- If you develop new symptoms of irritable bowel.
- If symptoms worsen in irritable bowel syndrome.
- If symptoms of irritable bowel do not improve within 2 weeks.