Constipation for pregnant women
Constipation in Pregnancy: 5 Fool-Proof Remedies
Infrequent bowel movements. Abdominal pain. The passage of hard stools.
If you’re pregnant, you’ve probably experienced these three familiar signs of constipation. Hormonal changes, pressure on the womb, and the iron in prenatal vitamins are to blame.
Why Am I Constipated?
An increase in the progesterone hormone during pregnancy causes the relaxation of your body’s muscles. That includes your intestines. And slower moving intestines means slower digestion. This can lead to constipation.
Constipation is common during pregnancy. Almost three out of four pregnant women will experience constipation and other bowel issues at some point, according to a study published in Acta Obstetricia et Gynecologica Scandinavica.
From over-the-counter pills to natural cures, there are a whole host of remedies available for relieving constipation.
But when pregnancy’s involved, the number of solutions shrinks.
These five remedies are pregnancy-safe.
Share on Pinterest
A diet high in fiber helps prevention constipation. It also supplies pregnant women with vitamins and antioxidants.
Pregnant women should try to consume 25 to 30 grams of dietary fiber each day to stay regular and healthy.
Good choices include fresh fruits, vegetables, beans, peas, lentils, bran cereals, prunes, and whole-grain bread.
Try cutting up some raspberries, apples, bananas, figs, and strawberries for a refreshing fruit salad. Or roast some sweet corn, Brussels sprouts, and carrots for a delightful side dish.
Share on Pinterest
It’s important to stay hydrated during pregnancy. That might mean doubling your water intake.
Pregnant women should drink at least eight 12-ounce glasses of water a day. This will help keep your bowels soft and moving smoothly through your digestive tract.
Share on Pinterest
Try breaking up your daily food intake into five or six smaller meals to help with constipation relief. This will allow the stomach to digest food without having to work overtime, and allow it to transfer food to the intestine and colon smoothly.
This will allow the stomach to digest food without having to work overtime, and allow it to transfer food to the intestine and colon smoothly.
Eating large meals can overload your stomach and make it harder for your digestive system to process what you’ve consumed.
Share on Pinterest
Regular physical activity can help reduce constipation. Exercise stimulates your bowels. Pregnant women should try to exercise three times a week for 20 to 30 minutes each.
The options for exercise are endless. Try walking down your favorite hiking path, swimming at your local gym, or practicing prenatal yoga on a relaxing afternoon.
Check with your doctor about what exercises are safe for you and your baby.
Share on Pinterest
If other natural options have failed, doctors will sometimes prescribe stool softeners like Colace on a short-term basis to help pregnant women with constipation. Colace stool softeners are available online. However, long-term use can lead to dehydration or change your electrolyte balance.
Stool softeners help moisten your bowels so they are easier to pass. They are especially useful for pregnant women taking constipation-causing iron supplements. Doctors will often prescribe softeners along with iron pills. You can find a variety of iron supplements here.
Stool softeners are medications, so it’s best to check with your doctor if they are safe for you.
Takeaway
Constipation relief during pregnancy is common, and it can be remedied.
Just follow the steps above to help ease the discomfort of backed up bowels while you wait for your little one to arrive.
Tips for a Healthy and Happy PregnancyConstipation in Pregnancy: 5 Fool-Proof Remedies
Infrequent bowel movements. Abdominal pain. The passage of hard stools.
If you’re pregnant, you’ve probably experienced these three familiar signs of constipation. Hormonal changes, pressure on the womb, and the iron in prenatal vitamins are to blame.
Why Am I Constipated?
An increase in the progesterone hormone during pregnancy causes the relaxation of your body’s muscles. That includes your intestines. And slower moving intestines means slower digestion. This can lead to constipation.
That includes your intestines. And slower moving intestines means slower digestion. This can lead to constipation.
Constipation is common during pregnancy. Almost three out of four pregnant women will experience constipation and other bowel issues at some point, according to a study published in Acta Obstetricia et Gynecologica Scandinavica.
From over-the-counter pills to natural cures, there are a whole host of remedies available for relieving constipation.
But when pregnancy’s involved, the number of solutions shrinks.
These five remedies are pregnancy-safe.
Share on Pinterest
A diet high in fiber helps prevention constipation. It also supplies pregnant women with vitamins and antioxidants.
Pregnant women should try to consume 25 to 30 grams of dietary fiber each day to stay regular and healthy.
Good choices include fresh fruits, vegetables, beans, peas, lentils, bran cereals, prunes, and whole-grain bread.
Try cutting up some raspberries, apples, bananas, figs, and strawberries for a refreshing fruit salad. Or roast some sweet corn, Brussels sprouts, and carrots for a delightful side dish.
Or roast some sweet corn, Brussels sprouts, and carrots for a delightful side dish.
Share on Pinterest
It’s important to stay hydrated during pregnancy. That might mean doubling your water intake.
Pregnant women should drink at least eight 12-ounce glasses of water a day. This will help keep your bowels soft and moving smoothly through your digestive tract.
Share on Pinterest
Try breaking up your daily food intake into five or six smaller meals to help with constipation relief. This will allow the stomach to digest food without having to work overtime, and allow it to transfer food to the intestine and colon smoothly.
Eating large meals can overload your stomach and make it harder for your digestive system to process what you’ve consumed.
Share on Pinterest
Regular physical activity can help reduce constipation. Exercise stimulates your bowels. Pregnant women should try to exercise three times a week for 20 to 30 minutes each.
The options for exercise are endless. Try walking down your favorite hiking path, swimming at your local gym, or practicing prenatal yoga on a relaxing afternoon.
Try walking down your favorite hiking path, swimming at your local gym, or practicing prenatal yoga on a relaxing afternoon.
Check with your doctor about what exercises are safe for you and your baby.
Share on Pinterest
If other natural options have failed, doctors will sometimes prescribe stool softeners like Colace on a short-term basis to help pregnant women with constipation. Colace stool softeners are available online. However, long-term use can lead to dehydration or change your electrolyte balance.
Stool softeners help moisten your bowels so they are easier to pass. They are especially useful for pregnant women taking constipation-causing iron supplements. Doctors will often prescribe softeners along with iron pills. You can find a variety of iron supplements here.
Stool softeners are medications, so it’s best to check with your doctor if they are safe for you.
Takeaway
Constipation relief during pregnancy is common, and it can be remedied.
Just follow the steps above to help ease the discomfort of backed up bowels while you wait for your little one to arrive.
Tips for a Healthy and Happy PregnancyConstipation during pregnancy: causes, recommendations
In addition, constipation in pregnant women may be caused by changes in the nature of food, the use of smooth muscle-relaxing drugs (lowering uterine activity, progesterone) 3 or mineral supplements containing iron and calcium4. Sometimes a woman has to lie down all the time, and at least minimal physical activity is necessary to maintain a normal bowel movement 3 . Another reason for the formation of constipation in pregnant women can be a decrease in fluid intake, starting from the earliest dates 4 .
In addition, constipation in pregnant women may be caused by changes in the nature of food, the use of smooth muscle-relaxing drugs (lowering uterine activity, progesterone) 3 or mineral supplements containing iron and calcium4. Sometimes a woman has to lie down all the time, and at least minimal physical activity is necessary to maintain a normal bowel movement 3 . Another reason for the formation of constipation in pregnant women can be a decrease in fluid intake, starting from the earliest dates 4 .
Sometimes a woman has to lie down all the time, and at least minimal physical activity is necessary to maintain a normal bowel movement 3 . Another reason for the formation of constipation in pregnant women can be a decrease in fluid intake, starting from the earliest dates 4 .
Thus, low bowel tone during pregnancy is generally initially protective, but may result in constipation 1 .
Possible complications of constipation in pregnancy
Gestational constipation can not only drastically reduce the quality of life, but also pose a certain threat to the well-being of the pregnant woman and the fetus.
Prolonged stagnation of feces can lead to a series of disorders, among other things, to the activation of opportunistic microorganisms. The penetration of microbes and their metabolic products through the intestinal wall can be at least a predisposing factor, and sometimes a direct cause of complicated pregnancy, problems in childbirth and the postpartum period 1 .
Disruption of the normal balance of the colonic microbiota during constipation may later cause a change in the composition of the microflora of the cervical canal.
This condition can cause intrauterine ascending infection and the occurrence of various complications of the gestation period. The course of pregnancy against the background of stagnation in the large intestine can lead to the threat of interruption, untimely discharge of amniotic fluid, inflammation of the uterine mucosa 1 .
The pathological increase in intestinal permeability caused by constipation impairs its barrier function, and even after childbirth it may not fully recover. That is why constipation is a situation that cannot be ignored and must be treated 1 .
Disruption of the normal balance of the colonic microbiota during constipation may later cause a change in the composition of the microflora of the cervical canal.

This condition can cause intrauterine ascending infection and the occurrence of various complications of the gestation period. The course of pregnancy against the background of stagnation in the large intestine can lead to the threat of termination, untimely discharge of amniotic fluid, inflammation of the uterine mucosa 1 .
The pathological increase in intestinal permeability caused by constipation impairs its barrier function, and even after childbirth it may not fully recover. That's why constipation is a situation that cannot be ignored and must be treated 1 .
Treatment of gestational constipation
The main rules for the prevention and treatment of constipation in pregnant women are primarily diet and recommendations for increasing physical activity 4 . Treatment of constipation, especially in pregnant women, begins with dietary measures 4 .
Treatment of constipation, especially in pregnant women, begins with dietary measures 4 .
For a laxative purpose, foods rich in indigestible plant fibers (fiber) are introduced into the menu. There are many such substances in raw fruits and vegetables, wholemeal bread 4 .
In terms of nutritional properties, wheat bran is considered the most acceptable for human consumption, which can be added 2-3 teaspoons to prepared meals 3 .
Prunes, kefir, dried apricots are considered products that help relieve constipation. The menu is recommended to include beets, zucchini, cabbage, lettuce, cucumbers and tomatoes. It is recommended to limit the consumption of strong tea and coffee, sweets and cocoa, flour dishes in the diet 3 .
It may also be necessary to correct the mode of motor activity, the amount of which is discussed with the doctor 3 . Gymnastics, walking or swimming in the pool may be recommended for a pregnant woman, if this is not contraindicated for health reasons 4 .
In some cases, despite following all recommendations, it may be necessary to use laxatives 4 . The choice of a possible drug cannot be made independently, because self-medication with laxatives during pregnancy is especially undesirable 1 .
The use of any medicine during pregnancy carries certain risks that only a doctor can weigh.
Therefore, only with medical permission, laxatives may be recommended. One of the laxatives that can be prescribed by a doctor to pregnant women starting from the 2nd trimester is Guttalax®: in the 1st trimester of pregnancy, the drug is contraindicated, in the 2nd and 3rd trimesters of pregnancy it is used with caution. Guttalax® is available in drops and tablets5,6. In view of the lack of studies, the use of Guttalax® tablets during pregnancy is recommended only in cases where the potential benefit to the mother outweighs the possible risk to the fetus. During pregnancy, the drug can be used only after consultation with a specialist.
During pregnancy, the drug can be used only after consultation with a specialist.
More about the drug
To increase the efficiency of preparation for the study, the individual functional state of the large intestine is also taken into account. If you have chronic constipation, you need to pay special attention to diet. In preparation for research, Guttalax® Express can be used in suppositories 8 .
The active substance - bisacodyl - becomes active and acts only in the lumen of the large intestine, therefore it does not affect the digestion and absorption of nutrients in the small intestine 8 . The drug Guttalax® Express enhances peristalsis, stimulates the natural process of bowel movement, and softens the stool. The development time of the laxative effect of the drug is 20 minutes (from 10 minutes to 30 minutes, in some cases - 45 minutes) 8 .
THERE ARE CONTRAINDICATIONS. IT IS NECESSARY TO CONSULT WITH A SPECIALIST.
Treatments for constipation during pregnancy
What's the problem?
The term "constipation" is defined as difficulty in passing stools and decreased frequency of stools (defecations - bowel movements to empty it). Constipation is characterized by discomfort, excessive straining, hard or lumpy stools, a feeling of incomplete emptying, and infrequent bowel movements. Constipation is a common symptom during pregnancy. This may be the result of a combination of factors including hormonal changes (shifts) during pregnancy affecting the digestive system, physical inactivity, and dietary changes during pregnancy. Also, as the fetus (baby) grows, it can compress the mother's intestines and thereby cause bowel delays/obstructions.
Why is this important?
Constipation during pregnancy is associated with impaired quality of life and distress for pregnant women, as well as physical problems, including the development of hemorrhoids. A number of treatment options have been suggested, including the use of medications, nutritional supplements, or dietary changes.
A number of treatment options have been suggested, including the use of medications, nutritional supplements, or dietary changes.
Non-pharmacological interventions (changes in diet, water intake and exercise) are generally recommended initially, and if these are ineffective or insufficient, medical (pharmacological) interventions are recommended. Medical interventions include a wide range of drugs: lubricants (lubricants), bulking agents, osmotic and stimulant laxatives, stool softeners (emollient laxatives), enemas and suppositories (laxatives in suppositories and enemas).
This review looked at the benefits of drug and non-drug interventions for constipation in pregnancy and whether they are safe for women and children.
What evidence did we find?
We identified four studies, but only two studies (a total of 180 women) provided data for analysis. These studies compared stimulant laxatives with bulk laxatives and dietary supplements (dietary fiber) with no intervention.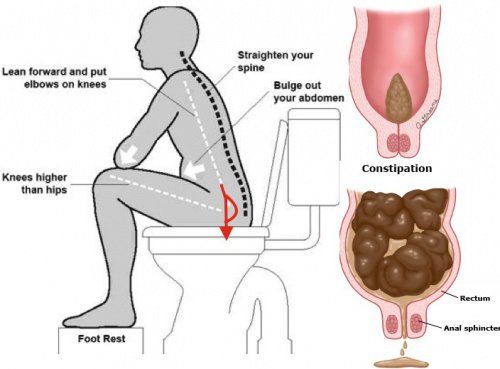 The included studies were considered to be of moderate (moderate) quality.
The included studies were considered to be of moderate (moderate) quality.
We have considered two main comparisons. In the first comparison, we found that stimulant laxatives may be more effective in treating constipation than bulk laxatives ( moderate-quality evidence ). However, it can also lead to more abdominal discomfort ( low-quality evidence ) and diarrhea ( moderate-quality evidence ). We found no difference in women's satisfaction ( moderate quality of evidence ). A second comparison between fiber supplementation and no intervention found that fiber supplementation may be effective in increasing stool frequency ( moderate-quality evidence ). The use of dietary supplements (fibers) was associated with improved stool consistency as defined by the testers (hard stool frequency decreased by 11% to 14%, normal stool frequency increased by 5% to 10%, and loose stool frequency increased by 0% to 6 %).
There were no studies looking at other interventions such as osmotic laxatives, stool softeners (stool softener laxatives), lubricants (lubricating laxatives), enemas, and suppositories (suppositories).