Blood during miscarriage
What Does a Miscarriage Look Like? Bleeding, Duration, and More
A miscarriage is a spontaneous pregnancy loss before 20 weeks of gestation. Some 8 to 20 percent known pregnancies end in miscarriage, with the majority happening before the 12th week.
The signs and symptoms of miscarriage vary from person to person. Symptoms may also vary depending on how far along you are. For example, a fetus at 14 weeks will be much larger than a fetus at 5 weeks of gestation, so there may be more bleeding and tissue loss with a later miscarriage.
Miscarriage symptoms may include:
- spotting or bleeding from the vagina
- abdominal cramping or pain in the lower back
- passage of tissue, fluid, or other products from the vagina
Read on to learn more about identifying a miscarriage and what to do if you suspect you’re experiencing one.
Bleeding may start as light spotting, or it could be heavier and appear as a gush of blood. As the cervix dilates to empty, the bleeding becomes heavier.
The heaviest bleeding is generally over within three to five hours from the time heavy bleeding begins. Lighter bleeding may stop and start over one to two weeks before it completely ends.
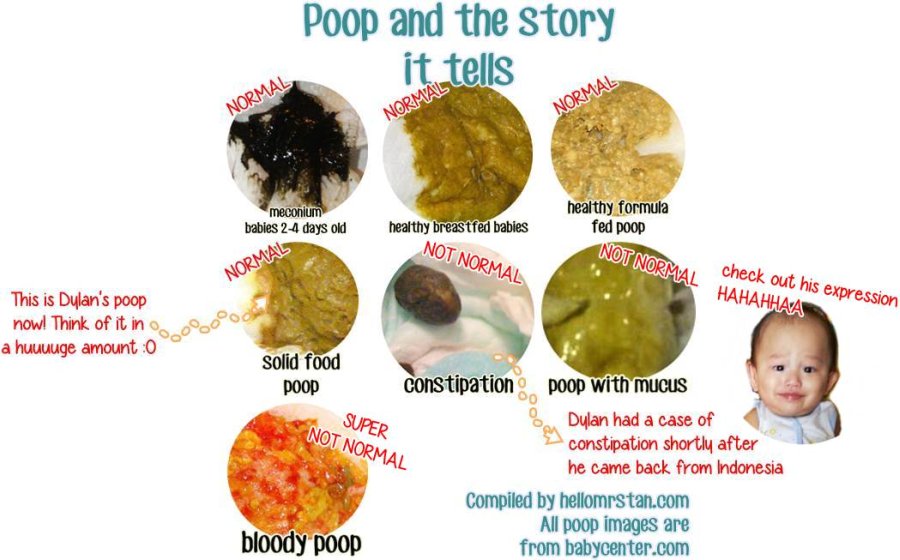
The color of the blood can range from pink to red to brown. Red blood is fresh blood that leaves the body quickly. Brown blood, on the other hand, is blood that’s been in the uterus a while. You may see discharge the color of coffee grounds, or near black, during a miscarriage.
Exactly how much bleeding you’ll experience depends on a variety of circumstances, including how far along you are and whether or not your miscarriage is progressing naturally.
While you may see a lot of blood, let your doctor know if you fill more than two sanitary pads an hour for two or more hours in a row.
What does a missed miscarriage look like?
You may not experience bleeding or other symptoms with a miscarriage, at least at first.
A missed miscarriage, also referred to as a missed abortion, happens when the fetus has died but the products of conception remain in the uterus.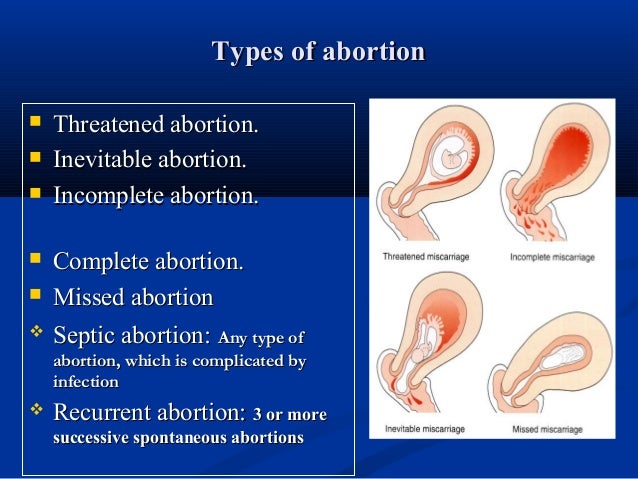 This type of miscarriage is usually diagnosed via ultrasound.
This type of miscarriage is usually diagnosed via ultrasound.
Just as with the amount of blood you’ll see, the duration of a miscarriage will vary from person to person and even from pregnancy to pregnancy.
In many cases, a miscarriage will take around two weeks to pass naturally. Your doctor may prescribe the medication misoprostol (Cytotec) to help a miscarriage pass more quickly. Bleeding may start within two days of beginning the medication. For others, it may take up to two weeks.
Once the miscarriage has started, the tissue and heaviest bleeding should be passed in about three to five hours. After the fetus has passed, you may still experience spotting and mild tissue loss for one to two weeks.
It may be difficult to tell a very early miscarriage from a late period. In fact, many miscarriages happen before a person even knows they’re pregnant.
In general, a miscarriage will cause more intense symptoms than a menstrual period. For example:
- Your menstrual flow may be relatively similar from month to month with heavy days and light days.
 A miscarriage can also have heavy and light days, but bleeding may be especially heavy at times and last longer than you’re used to.
A miscarriage can also have heavy and light days, but bleeding may be especially heavy at times and last longer than you’re used to. - Bleeding from a miscarriage may also contain large clots and tissue you don’t normally see during your period.
- Cramps can be a part of your normal monthly cycle, but with a miscarriage, they may be particularly painful as the cervix dilates.
- The color of blood during your period can range from pink to red to brown. If you see a color you’re not used to seeing, it may be a sign of miscarriage.
Always contact your doctor if you’re pregnant and experience bleeding. While a miscarriage can’t be stopped once it starts, you doctor can run tests to help determine if you’re experiencing the loss of your pregnancy or something else.
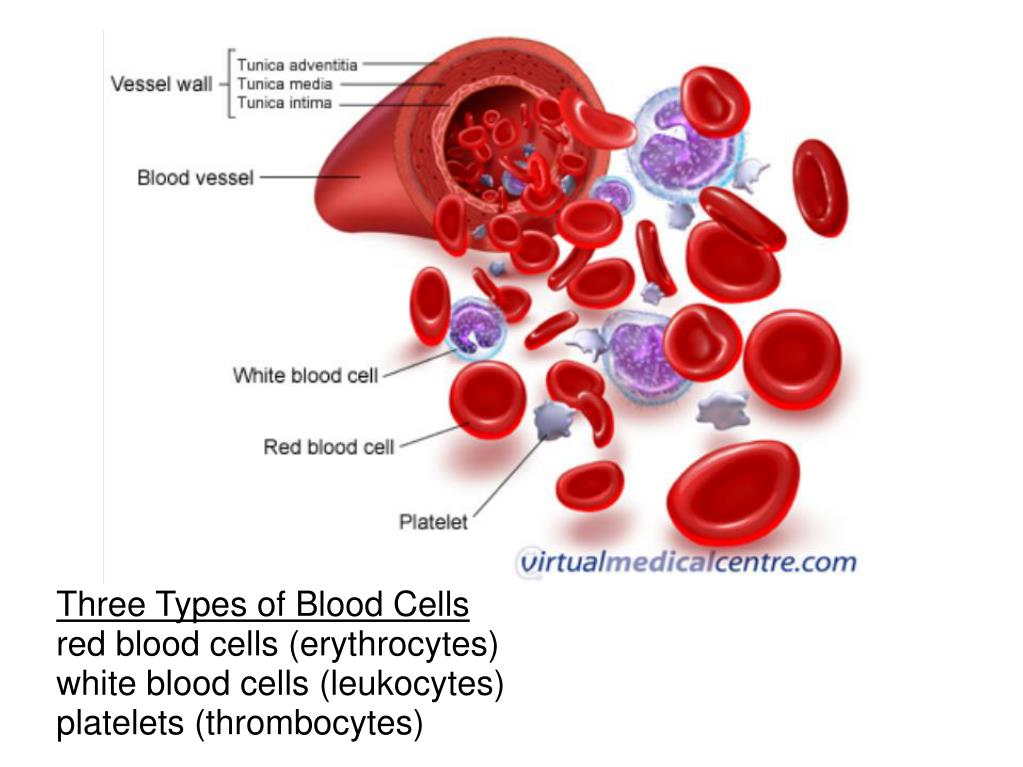
To diagnose a miscarriage, your doctor will likely perform an ultrasound to look for the baby’s heartbeat, if you’re far enough along to see a heartbeat. Your doctor may also order a blood test to check human chorionic gonadotropin (hcG) levels to see if they’re rising or falling.
If a miscarriage is confirmed, your doctor may suggest “expectant management” or waiting for the miscarriage to pass naturally. This generally happens within two weeks.
Incomplete miscarriage
The miscarriage may be incomplete if:
- your bleeding is particularly heavy
- you have a fever
- an ultrasound reveals there’s still tissue in your uterus
If this is the case, your doctor may suggest a dilation and curettage (D and C), which is a surgical procedure done to remove remaining tissue. The procedure is done under general or regional anesthesia, and is considered safe. D and C doesn’t usually lead to long-term complications.
Threatened miscarriage
It’s important to report any bleeding or pain you experience in your pregnancy to your doctor. In some cases, you may have what’s called a threatened miscarriage, and there may be certain treatments that can help. These include:
- hormone supplements if the bleeding is caused by low progesterone
- a cerclage (stitch in the cervix) if the issue is with the cervix opening prematurely
Speak with your healthcare provider if you’re looking to get pregnant again after a miscarriage. While it may be safe to start trying after your first normal period, you may want to schedule a checkup depending on the cause or the number of miscarriages you’ve had.
While it may be safe to start trying after your first normal period, you may want to schedule a checkup depending on the cause or the number of miscarriages you’ve had.
The reason for loss isn’t always known, but around half of miscarriages are caused by issues with the baby’s chromosomes.
Other possible causes include:
- uterine issues
- hormonal imbalances
- other health conditions, such as diabetes, autoimmune disorders, or polycystic ovary syndrome
After a miscarriage, you may have hcG in your blood for one to two months, which could lead to a false positive pregnancy test. In most cases, your period will return within four to six weeks, though you may start ovulating almost immediately following a miscarriage.
Speak with your doctor about birth control options if you don’t wish to become pregnant after a miscarriage.
Will I miscarry again?
Having one miscarriage doesn’t necessarily increases your chances of having another. The risk remains around 20 percent.
The risk remains around 20 percent.
Two or more miscarriages is referred to as recurrent pregnancy loss (RPL). The risk of miscarriage after two losses is 28 percent. After three consecutive losses, it increases to 43 percent.
Only 1 percent of people experience three or more miscarriages. About 65 percent of those with unexplained RPL go on to have successful pregnancies.
Activities like exercise, work, morning sickness, and sex don’t cause miscarriages. Even things like smoking or drinking alcohol or caffeine, which can lead to other complications, are also unlikely to lead to early pregnancy loss.
A miscarriage can be physically painful, and it may also cause a variety of emotions. While your body may recover in a few weeks, be sure to take time to process your feelings, grieve, and reach out for help when you need it.
Signs of Early Miscarriage | Obstetrics & Gynecology
Skip to main content
Department of Obstetrics and Gynecology
News | Careers | Giving | UC Davis Health
- UC Davis Health
- Obstetrics and Gynecology
- Miscarriage Management
- Signs of Early Miscarriage
Early miscarriage refers to loss of a pregnancy in the first trimester. The majority of early miscarriages occur before the pregnancy is 10 weeks gestation. Some miscarriages happen very early, even before a woman is sure she is pregnant. Still, miscarriage can be a hard and sad experience, no matter when it occurs.
The majority of early miscarriages occur before the pregnancy is 10 weeks gestation. Some miscarriages happen very early, even before a woman is sure she is pregnant. Still, miscarriage can be a hard and sad experience, no matter when it occurs.
Miscarriage is more common than many people realize. About 10 to 20% of women who learn they are pregnant will have an early miscarriage. The rates of early miscarriage are even higher when women are checking home pregnancy tests very close to the time of their period and are finding a positive test VERY early. By chance alone, 1% to 4% of women will have two miscarriages in a row. However, it is very rare to have 3 or more miscarriages in a row, which is recurrent miscarriage.
In medical terms, early miscarriage is called an early pregnancy failure. This means that the pregnancy failed to develop. Almost all early miscarriages are due to circumstances beyond anyone’s control, and were destined to happen before the woman even knows she is pregnant.
What are the symptoms of early miscarriage?
- Bleeding – light bleeding early in pregnancy is fairly common, and does not mean you will have a miscarriage.
- Brown discharge: This may look like coffee grounds. This “discharge” is actually old blood that has been in the uterus for a while and is just coming out slowly.
- Spotting, bright red bleeding or clots
- Passage of tissue through the vagina
- A gush of clear or pink vaginal fluid
- Abdominal pain or cramping
- Pregnancy symptoms, such as breast tenderness and nausea, begin to go away
- Dizziness, lightheadedness, or feeling faint
If you have any symptoms of a miscarriage, you should contact a doctor right away to have an evaluation. It will be important to have an ultrasound exam to look into the uterus to see if the pregnancy is normal or you are having a miscarriage. Even if you think you passed the entire pregnancy and are feeling better, you should see a doctor.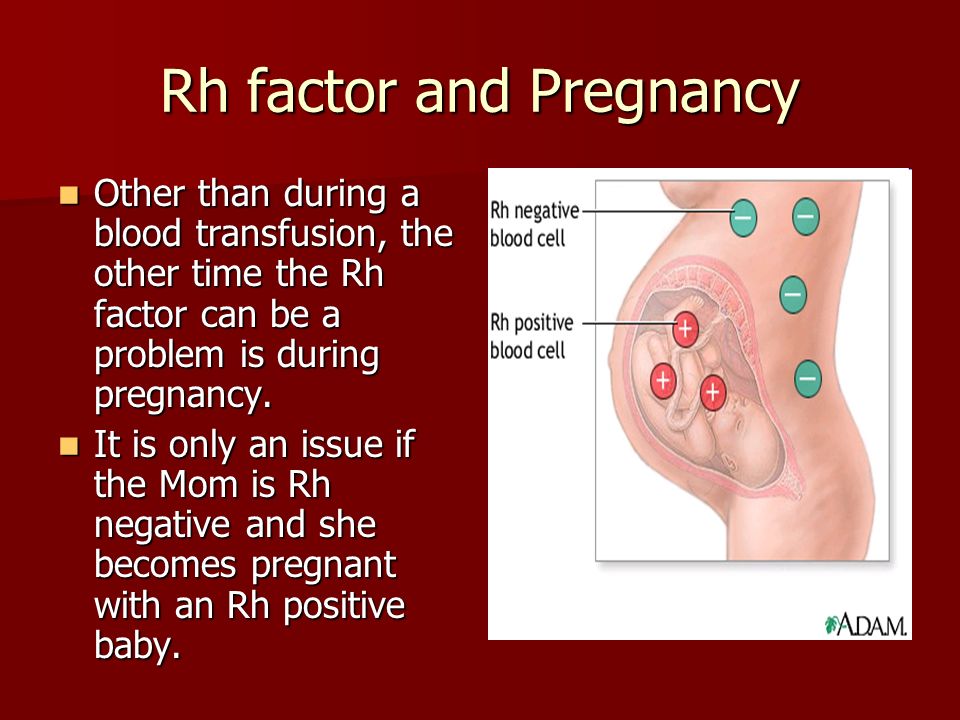 Sometimes, passing tissue occurs with an ectopic pregnancy (pregnancy outside of the uterus) which can be life-threatening if not diagnosed early.
Sometimes, passing tissue occurs with an ectopic pregnancy (pregnancy outside of the uterus) which can be life-threatening if not diagnosed early.
Types of early miscarriage
Early miscarriage is a non-medical term for lots of different types of events that might or might not actually result in pregnancy loss. The types of miscarriage include the following:
Spotting or bleeding in the first trimester in which the patient and the doctor are not yet sure if the pregnancy will miscarry or not. About 1/3 of all women will bleed in the first trimester, but only about half of those women will have a miscarriage.
The entire pregnancy is passed from the uterus, most commonly with bleeding and cramping, and no additional treatment or observation is needed.
The pregnancy is definitely miscarrying, but only some of the pregnancy tissue has passed. The tissue that is still in the uterus will eventually pass on its own. Some women may need emergency treatment if there is also heavy vaginal bleeding.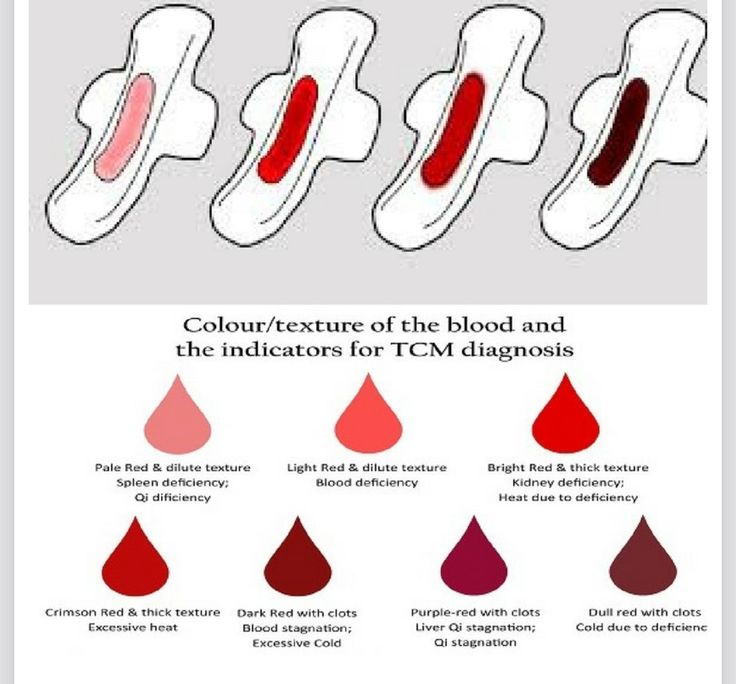 Otherwise, women can use medicines to cause the rest of the tissue to pass or simply wait for the rest of the tissue to pass from the uterus.
Otherwise, women can use medicines to cause the rest of the tissue to pass or simply wait for the rest of the tissue to pass from the uterus.
With this type of miscarriage, the pregnancy implanted but the embryonic tissue (the part of the pregnancy that will develop into a fetus) never developed, or started to develop and then stopped.
With this type of miscarriage, the early embryo (or fetus once 10 weeks pregnant) stops developing and growing.
This is an uncommon type of miscarriage today. With a missed abortion, the pregnancy stops developing but the pregnancy tissue does not pass out of the uterus for at least 4 weeks. Sometimes, dark brown spotting or bleeding occurs, but there is no heavy bleeding.
Some miscarriages occur with an infection in the uterus. This is a serious condition that requires urgent treatment to prevent shock and death. With septic miscarriage, the patient usually develops fever and abdominal pain and may have bleeding and discharge with a foul odor.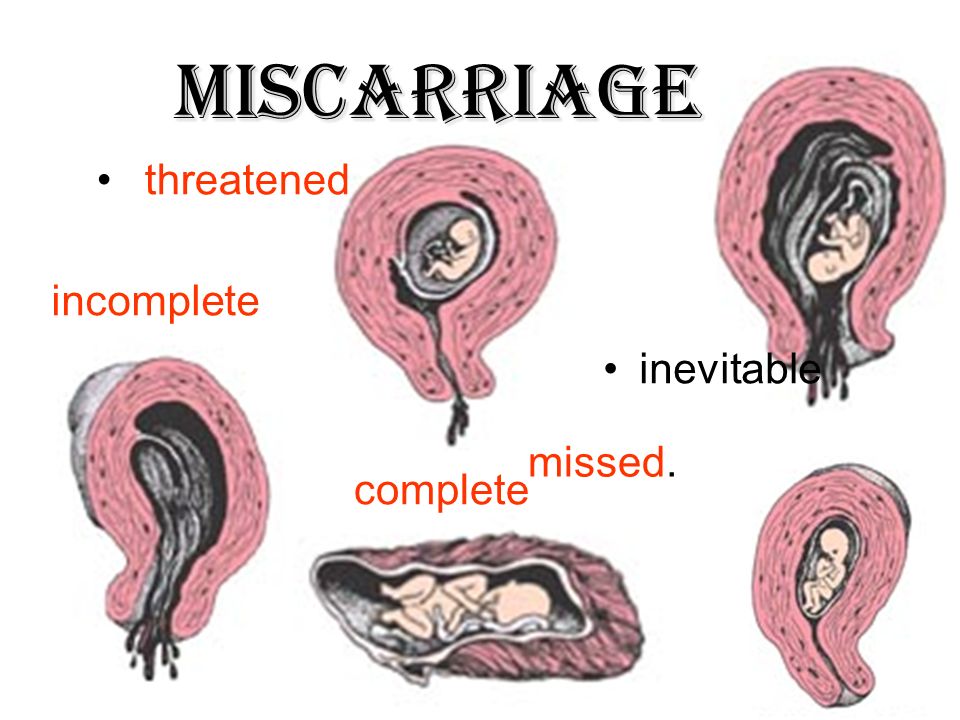 Antibiotics and suction evacuation of the uterus are important to start as quickly as possible.
Antibiotics and suction evacuation of the uterus are important to start as quickly as possible.
What causes early miscarriage?
Almost nothing you can do will cause an early miscarriage. Avoiding sex or heavy work will not impact an early pregnancy. There are a lot of changes that need to occur with the cells and genes in a developing pregnancy, and sometimes those changes do not happen perfectly. There are some health conditions or habits that can increase the chance that an early miscarriage will occur, including:
- Heavy smoking
- Use of illicit drugs, especially cocaine
- Poorly controlled diabetes
- Hyperthyroidism or hypothyroidism
- Physical problems with the uterus, including fibroids or abnormalities of development of the uterus
Why see our specialists at UC Davis Health?
Our specialists can evaluate you quickly in an office setting. Any laboratory testing or ultrasound examinations that need to be done can be performed easily and conveniently.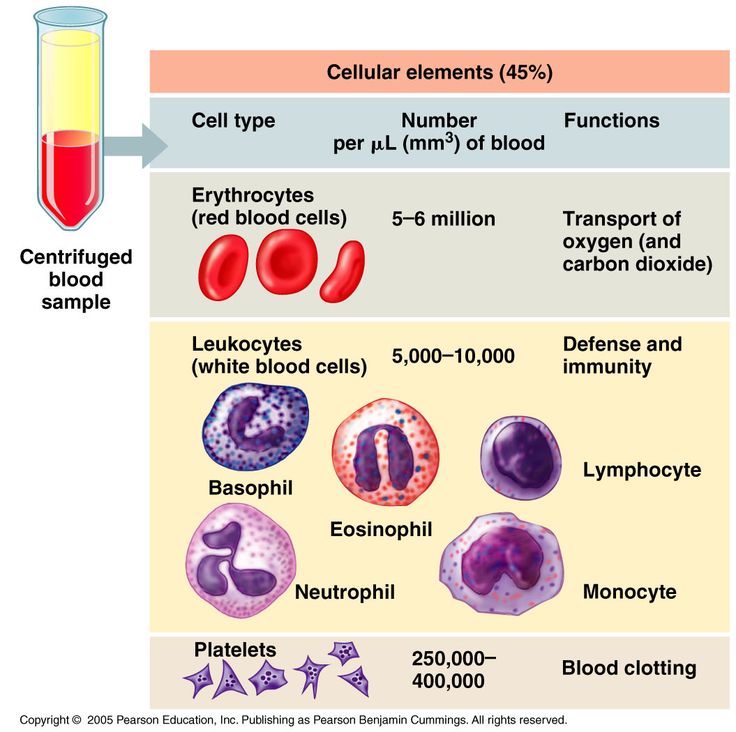 We perform our own ultrasound examination in the office and can share the results with you immediately.
We perform our own ultrasound examination in the office and can share the results with you immediately.
If we do confirm you have a miscarriage, we can discuss expectant management or treatment options with you immediately. Should you need blood testing to evaluate the pregnancy, the laboratory is in the same building as our office.
If you are having very heavy vaginal bleeding or are feeling very sick, you should go to the Emergency Room to see our physicians.
Treatment of early miscarriage
Not all miscarriages “need” treatment. The choice of whether to wait for the pregnancy to completely pass without any treatment is up to you. Our doctors are committed to providing options for all patients, including the pros and cons of all available options when miscarriage is diagnosed. All patients with Rh-negative blood, regardless of which option they choose, need treatment with Rh-immune globulin, an injection that prevents a woman from forming substances in her blood that may attack the baby during a future pregnancy.
When a diagnosis of miscarriage is made, options include:
This means that you will not receive any treatment; just continued follow-up. In an early miscarriage, with time, most women will pass the pregnancy completely. The main issue is time – there is no way to predict exactly when this will occur. You will typically have heavy bleeding and severe abdominal cramping when the pregnancy does pass. Should you want this option, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications can be used once the pregnancy begins to pass from the uterus.
This treatment uses medicines to cause the pregnancy tissue to pass from the uterus. The medicines cause cramping and bleeding, just like what will occur with natural passing of the pregnancy tissue. Using the medicines is like expectant management, except that you know when the pregnancy is going to pass. Most women will pass the pregnancy within 24 hours of taking the medication. Similar to expectant management, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications to use during treatment. If the pregnancy does not pass, you can repeat the medical treatment, have a suction aspiration, or continue to wait.
Similar to expectant management, our doctors can review exactly what to expect, how much bleeding is too much bleeding, and what pain medications to use during treatment. If the pregnancy does not pass, you can repeat the medical treatment, have a suction aspiration, or continue to wait.
- This brief procedure can be done in the office or the operating room. The following steps occur regardless of the location:
- The woman is in the same position as during a regular pelvic exam, like when a Pap test is done.
- A speculum is placed in the vagina
- A cleansing antibacterial solution is applied to the cervix and vagina
- Numbing medicine is applied to the cervix to decrease cramping
- The cervix is dilated (opened) with thin rods; with early miscarriage, the cervix does not need to be opened much to complete the procedure
- A thin straw-like tube is placed through the open cervixThe pregnancy is removed using a mechanical suction pump attached to the tube
- Everything is removed from the vagina when the procedure is done
You may choose to have the procedure in the office or operating room based on your preferences – different women have different needs.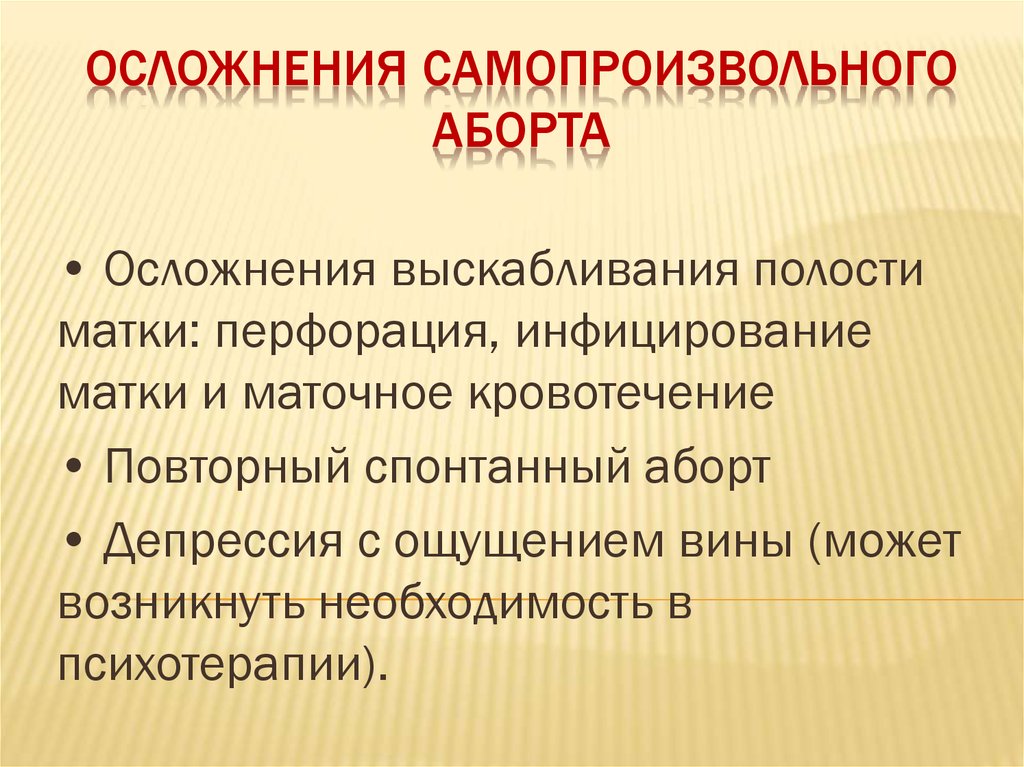
Office procedure:
- A spouse, partner, friend or relative can be in the room with you
- If desired, oral medications can be taken before the procedure to help you feel more relaxed
- You can eat or drink anything you want before the procedure
- The suction used in the office is most commonly a syringe that creates the suction so no noisy machine is used
- You will usually goes home 15-30 minutes after the procedure and can resume relatively normal activities
- Operating room procedure
- The procedure is done in an outpatient operating suite or in the main hospital
- You will be asleep during the procedure
- You cannot eat or drink anything after midnight on the night before the procedure because you will be receiving anesthesia
- You will feel sleepy for the whole day after the procedure and will need someone to be able to drive you home and be with you for the whole day after the procedure
- The operating room is more appropriate for women with certain medical conditions
After treatment for a miscarriage
Bleeding may continue for several weeks after a miscarriage but tends to be much lighter with a suction aspiration.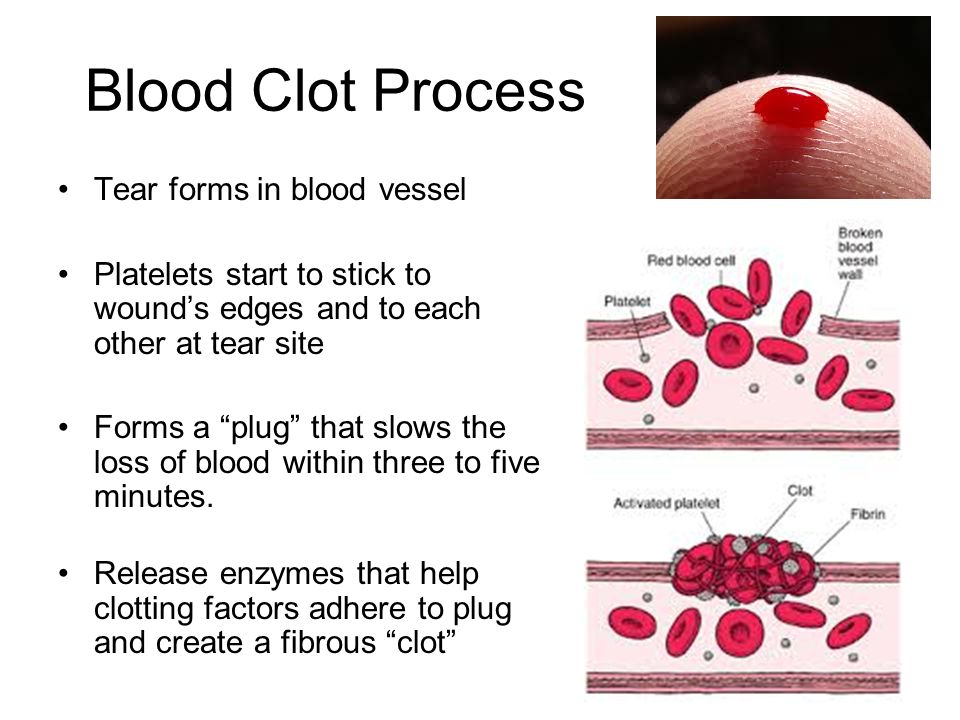 Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier after the miscarriage instead of lighter, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant after the miscarriage, it will be very important to start an effective method of contraception.
Any bleeding may change in color from bright red to pink or brown. Lower abdominal cramping in the few days after treatment is also common. You should contact a doctor right away if the bleeding gets heavier after the miscarriage instead of lighter, if a fever develops, or if vaginal discharge or a strange or unpleasant vaginal odor occurs. Avoid intercourse, douching, or using tampons for one week. Regular activities can be resumed right away, based on how you feel. Importantly, if you want to delay getting pregnant after the miscarriage, it will be very important to start an effective method of contraception.
Frequently asked questions about miscarriage
Having one miscarriage does not increase your chances of having another. If you have had only one prior miscarriage, the rate of miscarriage in the next pregnancy is similar to the overall rate in the general population.
No. Working, exercise and sexual activity do not increase the risk of miscarriage.
Patients were told years ago to wait one or two menstrual cycles to wait to get pregnant.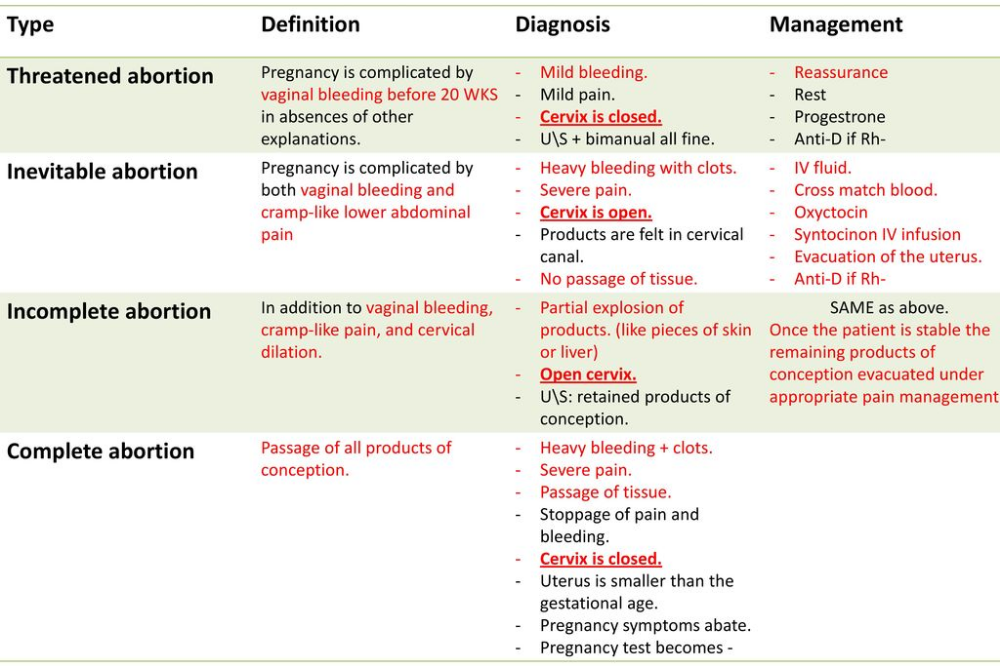 We know that it is highly unlikely that any problems occur with a next pregnancy if you get pregnant right away. How soon you decide to try again will depend on whether you want to be pregnant right away and if you feel you need time to recover emotionally from the miscarriage. Ovulation can resume as early as two weeks after a miscarriage, so if you do not want to get pregnant right away, you need effective contraception immediately.
We know that it is highly unlikely that any problems occur with a next pregnancy if you get pregnant right away. How soon you decide to try again will depend on whether you want to be pregnant right away and if you feel you need time to recover emotionally from the miscarriage. Ovulation can resume as early as two weeks after a miscarriage, so if you do not want to get pregnant right away, you need effective contraception immediately.
Since most early miscarriages are caused by problems specific to that fertilized egg, and miscarriage overall is relatively common, most experts do not recommend special testing until you have had three early miscarriages (or two miscarriages in women 40 years and older). At that point it is termed "recurrent" miscarriage and further testing may be needed. Studies have shown that even after a woman has experienced three consecutive miscarriages, her chance of the next pregnancy being normal is still about 70%. All women who have a pregnancy loss later in pregnancy should have further testing.
Tips to help support parents after pregnancy loss
UC Davis Health social worker Brenna Rizan, who works within the Department of Obstetrics/Gynecology provides supportive tips and advice for grieving parents, family and friends after pregnancy loss.
Related stories
Miscarriages are more common than people think - KCRA (Interview with Brenna Rizan)
Facebook Live: Discussing miscarriages with Dr. Mitch Creinin
UC Davis Early Pregnancy and Miscarriage Center
Miscarriage, symptoms - Health Clinic 365 Yekaterinburg
Causes of miscarriage
Questions to the doctor about miscarriage
Diagnosis of miscarriage
Treatment and prevention of miscarriage
According to statistics, 10 to 20% of all pregnancies end in miscarriage. However, the real numbers could be much higher, as a large number of miscarriages happen very early, and women are not even aware of their pregnancy.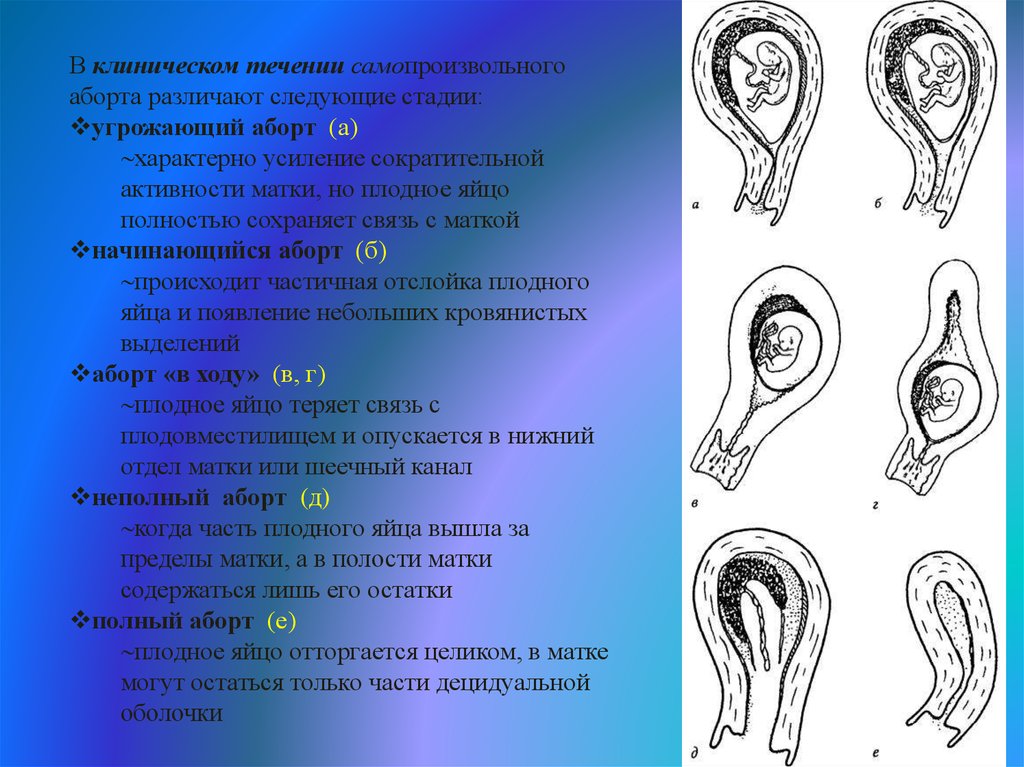 Most miscarriages happen due to abnormal development of the fetus.
Most miscarriages happen due to abnormal development of the fetus.
Miscarriage is quite common, but this fact does not make things any easier. It is always difficult to cope with the realization that there was a pregnancy, but no child. Try to deal with the situation psychologically and understand what could be causing the miscarriage, what increases the risk of it, and what type of treatment might be needed.
Miscarriage symptoms .
Most miscarriages occur before 12 weeks. Signs and symptoms of a miscarriage include:
- Vaginal bleeding or spotting (although quite common in early pregnancy)
- Pain or cramps in the abdomen or lower back
- Fluid vaginal discharge or tissue fragments
It is important to consider the fact that in early pregnancy, spotting or vaginal bleeding is quite common. In most cases, women who experience light bleeding during the first three months have an uneventful pregnancy thereafter.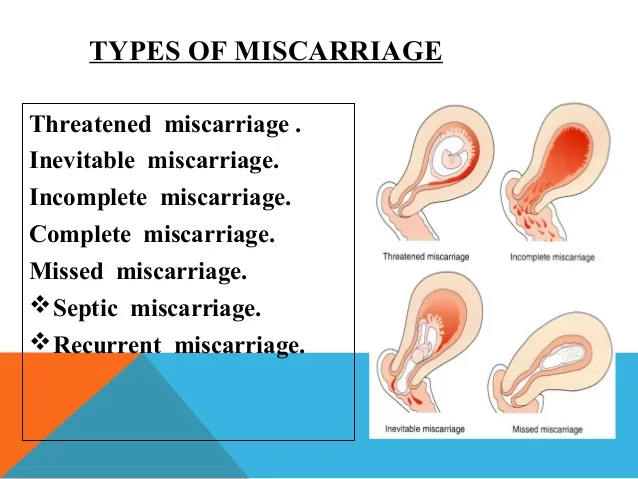 In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
In some cases, even with heavy bleeding, the pregnancy does not end in a miscarriage.
Some women who have a miscarriage develop an infection in the uterus. This infection, also called septic miscarriage, can cause:
- Fever (feeling hot, chills)
- Body pains
- Thick, foul-smelling vaginal discharge
When to see a doctor.
Call your doctor if:
- Bleeding, even if only light spotting occurs
- Profuse, liquid vaginal discharge without pain or bleeding
- Isolation of tissue fragments from the vagina
You can put a piece of tissue to be isolated in a clean container and take it to your doctor for examination. It is unlikely that the study will give any accurate results, but if it is determined that the fragments of the excreted tissue are from the placenta, the doctor will be able to conclude that the symptoms that appear are not associated with the presence of a tubal (ectopic) pregnancy.
You can get more detailed information about miscarriage from the gynecologists of the Health 365 clinic in Yekaterinburg.
Prices
Gynecologist, initial appointment
2300 i
Early miscarriage help
- home /
- Blog /
- How to avoid an early miscarriage
In a miscarriage, the fetus is shed from the endometrium, the inner lining of the uterus. According to experts, two out of 10 clinically established pregnancies end in spontaneous abortion. It is necessary to understand in more detail the causes, symptoms and methods of dealing with miscarriage.
How an early miscarriage occurs
There are three steps in this process. First, the fetus dies, after which it detaches from the endometrial layer. This is manifested by the fact that bleeding begins.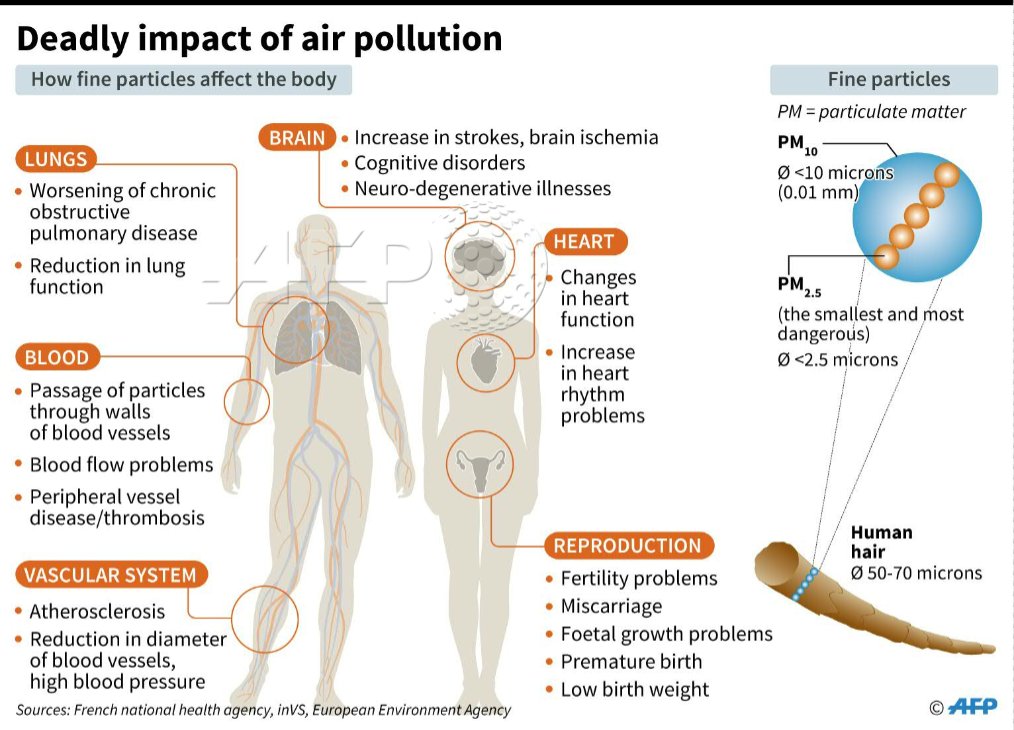
At the third stage, everything that has exfoliated is removed from the uterine cavity. The process may be complete or incomplete. In the early stages - five to six weeks - the process resembles ordinary menstruation. They are characterized by painful and much more unpleasant sensations. You can find out that it was just an early miscarriage by taking tests for the ratio of hCG in the blood.
Symptoms of a miscarriage
Signs of miscarriage are abdominal cramps, cramps or spotting. However, they do not always appear. It is necessary to note the most typical manifestations of the presented state and their main characteristics.
Temperature
For a short period of time, hyperthermia may well not be observed. Fever is not the most common symptom. In some cases, the thermometer readings really rise to 38 degrees or more.
At the same time, when hyperthermia is accompanied by a number of additional symptoms, a septic miscarriage is likely. These are its symptoms:
These are its symptoms:
- severe pain in the abdomen and in the depths of the vagina;
- increase in the tone of the uterus, which is felt by shocks inside;
- pungent, pungent and unpleasant odour.
All this indicates that the infection has joined. In such a case, emergency hospitalization is strongly recommended to stop the development of the process. It is better not to engage in self-medication or the use of folk recipes.
Discharge
Early miscarriage can indeed be accompanied by discharge. They may be habitual, as during menstruation. Also, the discharge may be smearing, insignificant.
Brown, scanty secretion, much less likely to end in spontaneous abortion. Most often, this is indicated by abundant and bright red discharge. It is blood that normally appears when the fetus is rejected from the inner layer of the uterus.
Pain
The severity of unpleasant and specific sensations may differ from each other depending on the duration of pregnancy.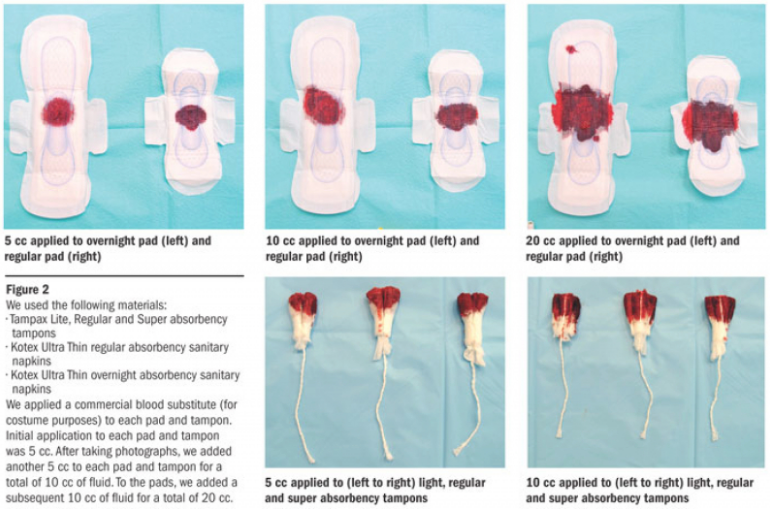 Probably the accession of pain, similar to menstruation. Most often, a similar symptom indicates an early miscarriage - no more than six weeks.
Probably the accession of pain, similar to menstruation. Most often, a similar symptom indicates an early miscarriage - no more than six weeks.
Probably cramping pains in the abdomen, which pull in the back. Their strength can vary from subtle to much more pronounced. In the rarest cases, when the clinical picture is complicated by a long course, this leads to a state of shock.
Another typical manifestation of pain is discomfort in the back or abdomen. Only then are the discharges identified. A similar situation is most typical for spontaneous abortion at the seventh or eighth week of pregnancy.
Causes of miscarriage
The first factor is genetic abnormalities in the development of the fetus. It is they who most often lead to miscarriage in the early stages. Violations can be expressed in qualitative or quantitative failures in chromosomes. In this regard, the female body recognizes the defect, and therefore does not allow such a fetus to develop further.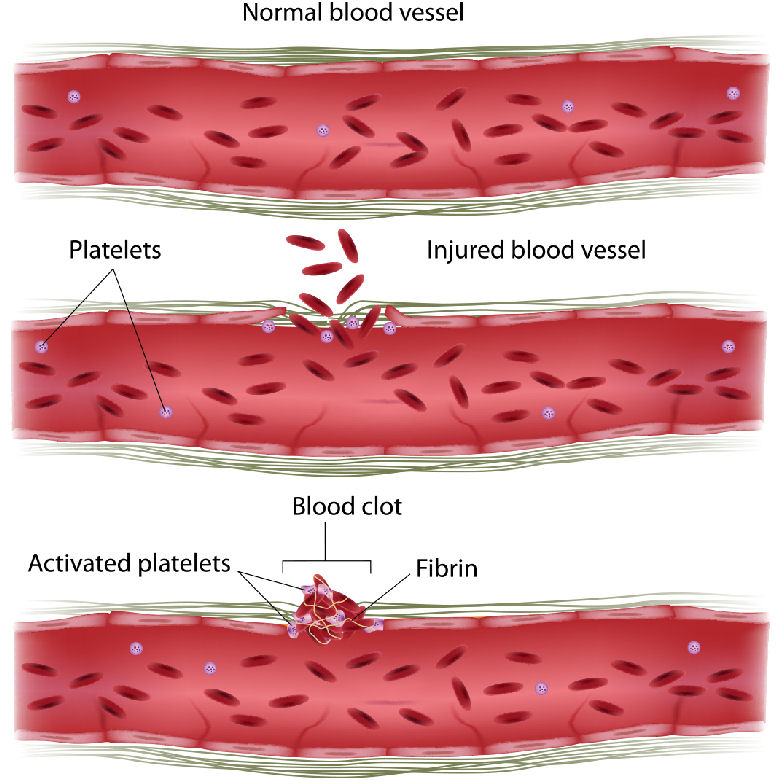 Most often, such rejection is noted in the third week of pregnancy.
Most often, such rejection is noted in the third week of pregnancy.
The next reason that an early miscarriage has developed may be disturbances in the work of the endocrine gland. Hormones determine not only the success and regularity of the cycle, but also how well the fetus is attached to the mucous surface of the uterus. If, due to a malfunction of the thyroid gland, the endometrium is not able to provide the fetus with all the necessary components, the pregnancy will not go well. Most often, a miscarriage occurs at the beginning or at the end of the fourth week.
Other reasons why pregnancy is terminated:
- Rhesus conflict. If the parents have different Rh factors, then the risk that a miscarriage will occur after the first weeks of pregnancy increases significantly. This happens if a woman has a negative Rh, and the child has a positive, inherited from the father. In such a situation, the female body recognizes the fetus as a foreign object. Therefore, it is excreted from the uterus.
 Timely diagnosis allows you to save the child through full-fledged drug therapy.
Timely diagnosis allows you to save the child through full-fledged drug therapy. - Sexually transmitted diseases, other infections. Similar problematic conditions also lead to spontaneous abortion. In this case, the embryo is infected at a very early stage. That is why the body will perceive it as a foreign object. In this regard, a miscarriage will occur already in the fifth week.
- Previous abortions. Another common reason why a miscarriage occurred. Abortion is a huge stress for the reproductive system, which leads to thinning of the lining of the uterus. That is why the risk of miscarriage may be greater.
Abdominal injuries should not be excluded from the injury list. Sharp pressure on the peritoneum, including when lifting weights, can provoke an abortion. Also on the list are severe stress, anxiety and depression. Anything that violates the normal state of a woman can lead to serious consequences.
How to avoid miscarriage
The main goal of treatment is to relieve tension in the uterus. It will be equally important to stop the bleeding and prolong the pregnancy, but only on the condition that the fetus is viable. The sooner medical assistance is provided, the higher the likelihood of preserving the fetus, without the need to determine the expected timing of miscarriages.
It will be equally important to stop the bleeding and prolong the pregnancy, but only on the condition that the fetus is viable. The sooner medical assistance is provided, the higher the likelihood of preserving the fetus, without the need to determine the expected timing of miscarriages.
Our specialists will help you with this. Only we have the most qualified and experienced doctors who know exactly how to treat even the most difficult cases. They will conduct a full diagnosis and prescribe the most effective, effective medicines.
Drug treatment
Hormonal drugs are used. They at an early stage determine the normal course of pregnancy. Medicines based on the hormone progesterone are effective.
- The use of hemostatic drugs. In the case of pregnant women, droppers are used with drugs such as Dicinon or Tranexam. They are needed to stop bleeding.
- Antispasmodics. Experts recommend injections of Drotaverin, followed by a switch to painkillers such as No-shpa.
 Papaverine suppositories, droppers with the addition of magnesia are also used. All of them are necessary in order to remove a number of signs of a pathological condition, namely, an increased tone of the uterus and pronounced pain.
Papaverine suppositories, droppers with the addition of magnesia are also used. All of them are necessary in order to remove a number of signs of a pathological condition, namely, an increased tone of the uterus and pronounced pain. - Use of Tocopherol. Vitamin E is an indispensable component for women, including pregnant women. It ensures the normal and full functioning of the ovaries. Tocopherol also strengthens the vascular walls, eliminates the formation of blood clots.
- Sedative preparations. Use motherwort or valerian tincture. The presented measure is recommended for increased irritability or nervousness of a pregnant woman.
To prevent early miscarriage, the specialists of our clinic recommend glucocorticosteroids. Apply Dexamethasone or Metipred. They are prescribed to patients with diagnosed immune disorders that can lead to early termination of pregnancy.
Optionally, a special relief ring can be installed. The presented procedure is carried out in the second trimester, or rather after the 20th week of gestation.
Remove such device not earlier than 38 weeks. It is necessary for a woman to maintain the correct position of the uterus. Also, the unloading ring helps to prevent premature birth.
Additional measures
To avoid early miscarriage, it is recommended to stop physical activity. Especially when it comes to jumping, lifting weights. Rest, lack of sudden physical activity and adherence to bed rest will help to keep the pregnancy.
Another preventive measure will be the exclusion of sudden movements. At any stage of pregnancy, they can provoke detachment of the embryo or lead to serious complications in its development.
An early miscarriage will be excluded by:
- emotional calm and absence of stress;
- refusal to take a hot bath or visit a bath, sauna - this is due to the fact that high temperatures provoke increased bleeding, as well as detachment of the fetus;
- restriction of sexual intercourse - if there is a threat that an early miscarriage will occur, they refuse to have sex;
- exclusion of alcohol, nicotine addiction.