Constant sickness during pregnancy
Severe vomiting in pregnancy - NHS
Sickness in pregnancy (sometimes called morning sickness) is common. Around 8 out of every 10 pregnant women feel sick (nausea), are sick (vomiting) or both during pregnancy. This does not just happen in the morning.
For most women, this improves or stops completely by around weeks 12 to 20, although for some women it can last longer.
Some pregnant women experience very bad nausea and vomiting. They might be sick many times a day and be unable to keep food or drink down, which can impact on their daily life.
This excessive nausea and vomiting is known as hyperemesis gravidarum (HG), and often needs hospital treatment.
Exactly how many pregnant women get HG is not known as some cases may go unreported, but it's thought to be around 1 to 3 in every 100.
If you are being sick frequently and cannot keep food down, tell your midwife or doctor, or contact the hospital as soon as possible. There is a risk you may become dehydrated, and your midwife or doctor can make sure you get the right treatment.
Symptoms of hyperemesis gravidarum
HG is much worse than the normal nausea and vomiting of pregnancy.
Signs and symptoms of HG include:
- prolonged and severe nausea and vomiting
- dehydration – symptoms include feeling thirsty, tired, dizzy or lightheaded, not peeing very much, and having dark yellow and strong-smelling pee
- weight loss
Unlike regular pregnancy sickness, HG may not get better by 16 to 20 weeks. It may not clear up completely until the baby is born, although some symptoms may improve at around 20 weeks.
See your GP or midwife if you have severe nausea and vomiting. Getting help early can help you avoid dehydration and weight loss.
There are other conditions that can cause nausea and vomiting, and your doctor will need to rule these out first.
See videos and written interviews of women talking about their experiences of hyperemesis gravidarum on the healthtalk website.
What causes hyperemesis gravidarum?
It's not known exactly what causes HG, or why some women get it and others do not. There is evidence that it is linked to the changing hormones in your body that occur during pregnancy.
There is some evidence that it runs in families, so if you have a mother or sister who has had HG in a pregnancy, you may be more likely to get it yourself.
If you have had HG in a previous pregnancy, you are more likely to get it in your next pregnancy than women who have never had it before, so it's worth planning in advance.
Treating hyperemesis gravidarum
There are medicines that can be used in pregnancy, including the first 12 weeks, to help improve the symptoms of HG. These include anti-sickness (anti-emetic) drugs, steroids, or a combination of these.
These include anti-sickness (anti-emetic) drugs, steroids, or a combination of these.
You may need to try different types of medicine until you find what works best for you.
You can visit the Bumps website to find out which medicines are safe to use in pregnancy.
If your nausea and vomiting cannot be controlled, you may need to be admitted to hospital. This is so doctors can assess your condition and give you the right treatment to protect the health of you and your baby.
Treatment can include intravenous fluids, which are given directly into a vein through a drip. If you have severe vomiting, the anti-sickness drugs may also need to be given into a vein or a muscle.
The charity Pregnancy Sickness Support has information and tips on coping with nausea and vomiting, including HG.
Will hyperemesis gravidarum harm my baby?
HG can make you feel very unwell, but it's unlikely to harm your baby if treated effectively.
However, if it causes you to lose weight during pregnancy, there is an increased risk that your baby may be born smaller than expected (have a low birthweight).
How you might feel
The nausea and vomiting of HG can impact your life at a time when you were expecting to be enjoying pregnancy and looking forward to the birth of your baby.
It can affect you both emotionally and physically. The symptoms can be hard to cope with. Without treatment HG may also lead to further health complications, such as depression or tears in your oesophagus.
Severe sickness can be exhausting and stop you doing everyday tasks, such as going to work or even getting out of bed.
In addition to feeling very unwell and tired, you might also feel:
- anxious about going out or being too far from home in case you need to vomit
- isolated because you do not know anyone who understands what it's like to have HG
- confused as to why this is happening to you
- unsure about how to cope with the rest of the pregnancy if you continue to feel very ill
If you feel any of these, do not keep it to yourself. Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to a partner, family members and friends if you want to.
Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to a partner, family members and friends if you want to.
If you want to talk to someone who has been through HG, you can contact Pregnancy Sickness Support's help section. They have a support network across the UK and can put you in touch with someone who has had HG.
Bear in mind that HG is much worse than regular pregnancy sickness. It is not the result of anything you have or have not done, and you do need treatment and support.
Another pregnancy
If you have had HG before, it's likely you will get it again in another pregnancy.
If you decide on another pregnancy, it can help to plan ahead, such as arranging child care so you can get plenty of rest.
You could try doing things that helped last time.
Talk to your doctor about starting medicine early.
Blood clots and hyperemesis gravidarum
Because HG can cause dehydration, there's also an increased risk of having a blood clot (deep vein thrombosis), although this is rare.
If you are dehydrated and immobile, there is treatment that you can be given to prevent blood clots.
Read more about how to prevent deep vein thrombosis.
Severe Morning Sickness (Hyperemesis Gravidarum) (for Parents)
What's Morning Sickness?
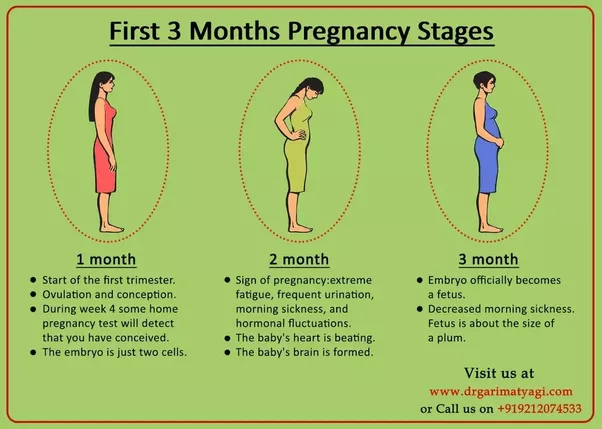
During the first trimester of pregnancy, many women have the bouts of nausea and vomiting known as morning sickness.
Despite its name, morning sickness can happen day or night. It usually starts around the 6th week of pregnancy, is at its worst around week 9, and stops by weeks 16 to 18. Although unpleasant, morning sickness is considered a normal part of a healthy pregnancy.
What’s Severe Morning Sickness?
Severe morning sickness is when nausea and vomiting get so serious that a pregnant woman vomits several times a day, loses weight, and gets dehydrated or is at risk for dehydration.
If this rare pregnancy-related condition isn’t treated, it can affect a woman's health and her baby's ability to thrive.
The medical term for severe morning sickness is "hyperemesis gravidarum" (hi-per-EM-eh-sis grav-ih-DARE-um), which means "excessive vomiting during pregnancy." It usually follows a similar timeline to normal morning sickness. But it can go longer, sometimes lasting for the whole pregnancy. Often, the symptoms get less severe as the pregnancy continues.
Most cases of hyperemesis gravidarum affect a woman's first pregnancy. But women who have it in one pregnancy are more likely to have it in future pregnancies.
What Causes Severe Morning Sickness?
The cause of severe morning sickness isn’t known. But it might be related to the hormone changes of pregnancy. A hormone called human chorionic gonadotropin, or HCG, might be to blame because severe morning sickness most often happens when HCG levels are at their highest in a pregnant woman's body.
A hormone called human chorionic gonadotropin, or HCG, might be to blame because severe morning sickness most often happens when HCG levels are at their highest in a pregnant woman's body.
Severe morning sickness also might run in families. It’s more common in women whose close family members (such as mothers and sisters) have had it.
Other things that can increase a woman's chances of having severe morning sickness include:
- carrying multiples (twins, triplets, etc.)
- history of motion sickness
- migraine headaches with nausea or vomiting
What Problems Can Happen?
The nausea and vomiting that happen in severe morning sickness are so extreme that they can harm the mother and the baby. Not being able to keep down food makes it hard for the mom to meet her nutritional needs. So she might lose weight. And a loss of fluids, combined with the loss of stomach acid from vomiting, can cause dehydration and electrolyte imbalances.
If severe morning sickness isn’t treated, it can cause many problems, including organ failure and the early birth of her baby.
When Should I Call the Doctor?
Call the doctor right away if you’re pregnant and have any of these symptoms:
- nausea that lasts throughout the day, making it impossible to eat or drink
- vomiting three to four times per day or not being to keep anything in the stomach
- brownish vomit or vomit with blood or streaks of blood in it
- weight loss
- fainting or dizziness
- peeing less than usual
- a fast heart rate
- a lot of headaches
- unpleasant, fruity mouth or body odor
- extreme tiredness
- confusion
How Is Severe Morning Sickness Treated?
Treatments used for morning sickness, such as eating dry crackers in the morning or a bland diet, may be recommended for women with extreme morning sickness. But these might not help with severe symptoms.
Medical treatment can include:
- a short period of not eating to rest the gastrointestinal system
- intravenous (IV) fluids
- vitamin and nutritional supplements
Some women might get medicine to stop the vomiting, either by mouth or through an IV.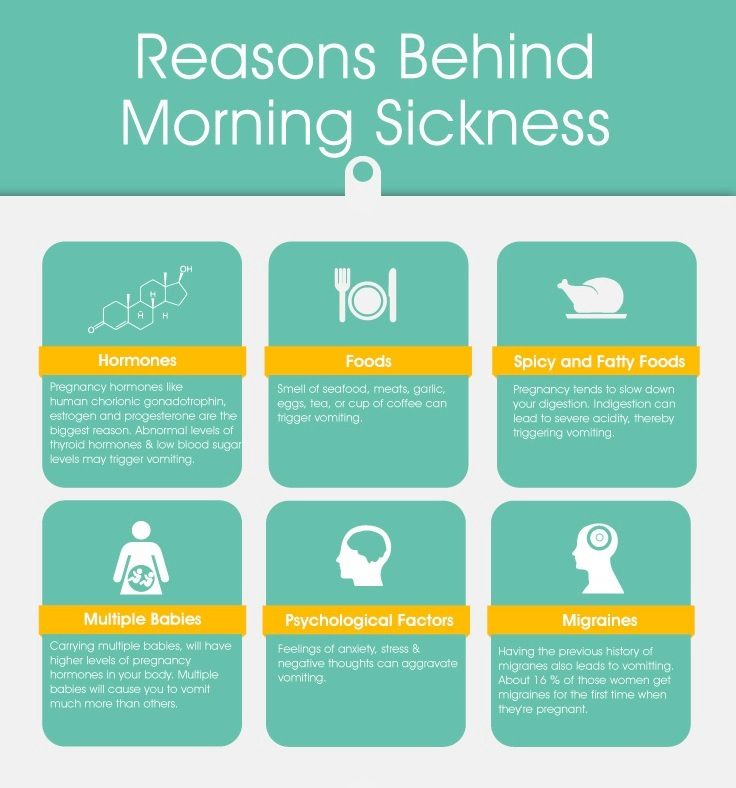 The doctor might recommend eating foods with ginger or taking vitamin B6 supplements to help ease nausea. It can also help to:
The doctor might recommend eating foods with ginger or taking vitamin B6 supplements to help ease nausea. It can also help to:
- Eat a bland diet.
- Eat frequent small meals.
- Drink plenty of liquids when not feeling nauseated.
- Avoid spicy and fatty foods.
- Eat high-protein snacks.
- Avoid sensory stimuli that can act as triggers (like specific smells or noises).
If a woman feels anxious or depressed about her condition, talking to a therapist or counselor might help her cope with her feelings.
What Else Should I Know?
With treatment, women with severe morning sickness can feel better and get the nourishment they need so they and their babies thrive. And lifestyle changes can help ease nausea and vomiting and make the pregnancy more enjoyable.
With time, symptoms usually do improve. And, of course, they stop by the time a woman's next journey starts: parenthood.
1st trimester of pregnancy: what happens to the fetus
1st trimester of pregnancy: what happens to the fetus - Private maternity hospital Ekaterininskaya Clinics1st trimester: 1st-12th weeks
The gestational age is calculated from the first day of the last menstruation, since it is difficult to determine the exact day of conception. Since conception usually occurs in the middle of the menstrual cycle, you are not actually pregnant during the first two weeks, but this period is counted as the beginning of pregnancy.
Since conception usually occurs in the middle of the menstrual cycle, you are not actually pregnant during the first two weeks, but this period is counted as the beginning of pregnancy.
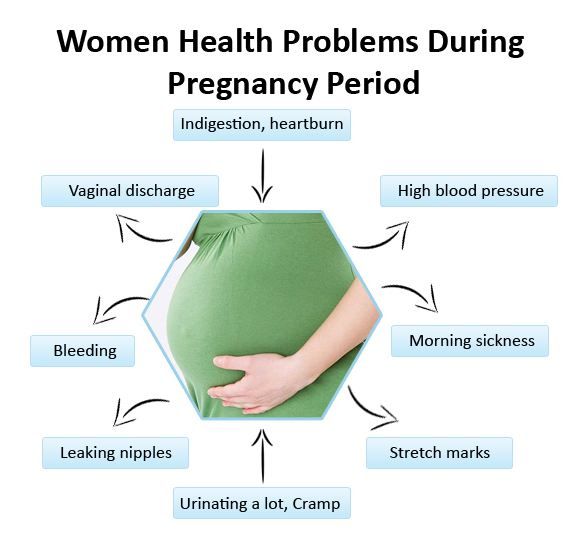
As soon as the fertilization of the egg takes place around the 3rd week, the hormones begin to produce changes in your body little by little. As a result, you may experience some of the following symptoms:
- Morning sickness. As a result of rising levels of hormones characteristic of pregnancy, up to 80% of women in the 1st trimester experience morning sickness with symptoms such as nausea and vomiting. The idea that such malaise is observed only in the morning is a common misconception. In fact, symptoms can appear at any time of the day or night. Up to 1 in 5 women experience morning sickness in the 2nd trimester of pregnancy and can sometimes persist throughout pregnancy.
If you experience morning sickness, avoid foods that make you sick, eat little and often, avoid fatty and spicy foods, drink more water.
 If you experience severe symptoms or symptoms that bother you, see your doctor.
If you experience severe symptoms or symptoms that bother you, see your doctor. - Breast changes. The mammary glands will begin to increase in size, soreness may appear. The nipples will increase in size, become darker and more protruding.
- Fatigue. High levels of the hormone progesterone can make you feel tired and sleepy. Rest as often as possible in a horizontal position with your legs up and eat as well as possible, which is not easy if you are experiencing morning sickness!
- Increased emotionality. A higher level of emotionality, manifested as a result of an increase in hormone levels, is normal. Understanding and patience on the part of your partner and loved ones is very important here.
- Food likes and dislikes. You may find yourself intolerant of one food and addicted to another. This is usually not a problem, unless you feel like eating weird foods like chalk.
 If you are concerned about the situation, contact your doctor.
If you are concerned about the situation, contact your doctor. - Frequent urination. As your fluid levels increase and your uterus puts pressure on your bladder, you will become more likely to visit the toilet. Go to the toilet as soon as you feel the need - this minimizes the pressure on the bladder.
- Feeling of dizziness. Sometimes you may feel a little dizzy (this is due to hormonal changes). Try not to stay on your feet for a long time and slowly rise from a sitting or lying position. If you experience severe dizziness, contact your doctor immediately.
- Heartburn and constipation. Your digestive system will slow down to give you more time to digest your food. This can lead to heartburn and constipation. To help manage heartburn, try to eat small meals at regular intervals and avoid fried or spicy foods and carbonated drinks. Constipation is helped by eating a diet rich in fiber, maintaining physical activity and drinking plenty of water.

1st trimester milestones
- Approximately 7 days after fertilization, the embryo implants in the uterine wall. The placenta, umbilical cord and amniotic sac will begin to form to provide nourishment and protection to the embryo.
- By the end of the first 12 weeks of pregnancy, the uterus is palpable through the wall of the abdomen, the abdomen will begin to grow.
Child development in the 1st trimester of pregnancy
By the end of the 1st trimester:
- All the main organs of the baby are formed, the circulatory system works.
- The development of the sexual organs has begun.
- Fingers are formed on the hands and feet, nails have appeared.
- Facial features have formed.
- The length of the baby's body is about 6 cm from the head to the lower part of the body, he is already recognizable. The baby moves in the amniotic sac, but you don't feel it move yet.

Clinic mobile app
You can make an appointment with a doctor, get tests
and much more...
Fill out the form to make an appointment or order a call back
I agree with personal data processing policy and user agreement I also give my consent to the processing of personal data.
Sign up for a consultation
I agree with personal data processing policy and user agreement I also give my consent to the processing of personal data.
By continuing to use rd.clinic23.ru, you agree to the use of cookies. How to ban the use of certain cookies can be found in Politics
Toxemia, Intestinal Problems & Heartburn
Find out how pregnancy affects the digestive tract, which trimesters are more likely to show symptoms of indigestion and nausea, and what to do to manage them.

During pregnancy, the burden on the mother's body increases. The body needs more nutrients, the body produces additional hormones. And the growing fetus puts pressure on neighboring organs, including the stomach and intestines. We tell you what symptoms are observed in each trimester, how to cope with toxicosis and get rid of heartburn.
Contents:
- 2. Toxicosis and pregnancy
- 3. Causes, risks and treatment of diarrhea during pregnancy
- 4. Heartburn and stomach pain during pregnancy
- 5. Bloating, constipation and microbiota during pregnancy
- 6. Note
Changes in the work of the gastrointestinal tract by trimesters of pregnancy
The average duration of pregnancy is 40 weeks, which are usually divided into trimesters in accordance with the stages of intrauterine development of the child.
Each trimester is accompanied by a number of changes in the body, including in the gastrointestinal tract:
Causes of gastrointestinal problems during pregnancy
Every pregnancy is accompanied by inevitable changes in the functioning of the digestive system.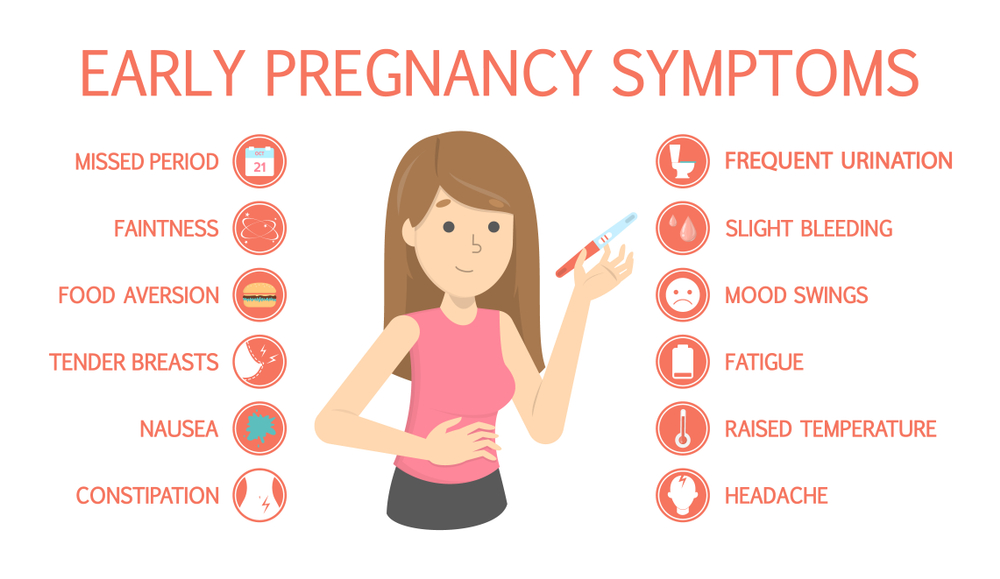 They are most often caused by hormonal changes and increased stress on the organs, but they can also be associated with lifestyle and health conditions, for example:
They are most often caused by hormonal changes and increased stress on the organs, but they can also be associated with lifestyle and health conditions, for example:
- Sedentary lifestyle and unbalanced diet;
- Certain drugs, including calcium or aluminum antacids;
- Viral and bacterial infections;
- Intolerance to certain nutrients and allergic reactions;
- Stress;
- Diseases of the thyroid gland.
If you have chronic diseases of the gastrointestinal tract and you are planning a pregnancy, try to consult your doctor in advance. Symptoms of conditions such as irritable bowel syndrome (IBS) or acid reflux are more likely to get worse during pregnancy. Your doctor will help prepare your body and create a prevention plan to help relieve symptoms during this time.
Irritable bowel syndrome, or IBS, is a functional bowel disease that causes frequent abdominal pain, impaired peristalsis, bloating, constipation, or diarrhea.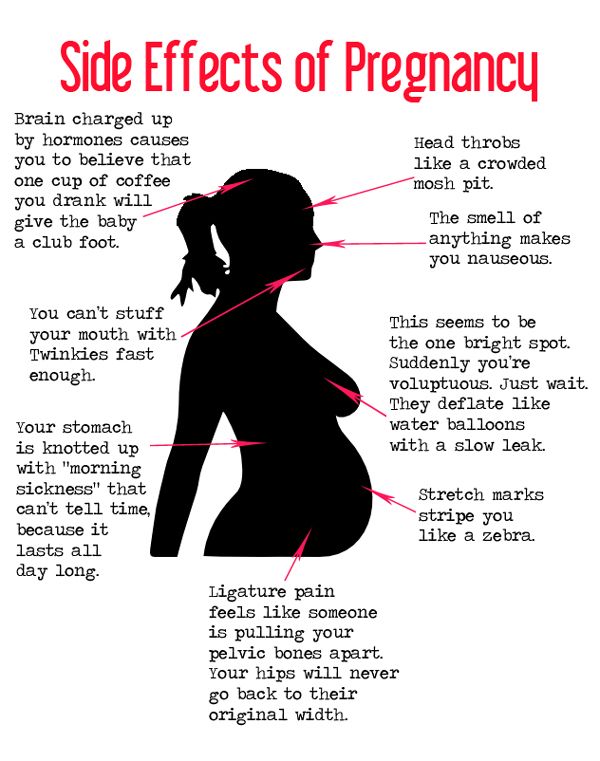
Morning sickness, vomiting and general malaise during pregnancy
Morning sickness and morning sickness during early pregnancy are common, because the body undergoes important changes necessary for the development of the child.
up to 90%
women experience nausea during pregnancy
Doctors find it difficult to say with certainty why pregnant women feel sick in the morning. The main theory is hormonal changes. But there are some patterns associated with an increased risk of morning sickness:
- Multiple pregnancy;
- Toxicosis during a previous pregnancy;
- History of morning sickness during pregnancy in close relatives;
- Tendency to motion sickness in transport;
- Use of oral contraceptives containing estrogen before pregnancy;
- Frequent migraines;
- BMI 30 and above;
- Elevated levels of stress hormones
Risks of severe morning sickness and how to reduce nausea
Nausea and vomiting are usually not associated with a risk for mother and child and disappear by 16-20 weeks of pregnancy, but it is not necessary to wait so long - there are ways that can help reduce nausea and enjoy the process of waiting for a new person:
- Get plenty of rest - fatigue increases toxicosis;
- Avoid smells and foods that cause nausea;
- Eat something right after waking up.
 A toast or a slice of bread will help reduce nausea;
A toast or a slice of bread will help reduce nausea; - Avoid hunger - empty stomach increases nausea. Eat small meals often, prefer low-fat, high-carbohydrate foods;
- Try ginger - studies show it helps with nausea;
- Sip as often as possible and prefer still water.
In rare cases, pregnant women may develop hyperemesis gestationis or excessive vomiting. This is a serious condition that can lead to dehydration, kidney damage, seizures, abnormal heart rhythms, and even death.
Signs of dehydration include dry mouth, dizziness, dark urine, infrequent urination and/or dizziness.
Symptoms of excessive pregnancy vomiting:
- frequent nausea for a long time and regular vomiting after meals;
- dry skin and lips;
- sudden weight loss;
- low blood pressure (below 90/60).
If symptoms of excessive pregnancy vomiting occur, do not wait until the condition resolves on its own. It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
It is necessary to seek medical help as soon as possible - the doctor will prescribe treatment, help adjust the diet and lifestyle of the expectant mother.
0.5–2%
pregnant women experience excessive vomiting
Diarrhea in pregnancy
The word "diarrhea" comes from the Greek language and literally means "to flow through". This is a condition during which bowel movements or bowel movements occur three times a day or more often. This phenomenon is especially typical for the third trimester of pregnancy, but it can also occur earlier.
Symptoms of diarrhea:
- Three or more bowel movements per day
- Urgent urge to have a bowel movement
- Abdominal pain and cramps
- Bloating
Causes of diarrhea during pregnancy poisoning, dysbiosis, bacterial and viral infections:
| Gastroenteritis | Lactose and gluten use in case of intolerance to these nutrients |
| Bacterial infections: listeriosis or salmonella | Chronic gastrointestinal diseases: Crohn's disease, IBS, ulcerative colitis |
| Some antibiotics and antacids to reduce acidity | Laxatives |
| Sugar substitutes such as sorbitol | Overconsumption of certain foods |
Tip: If you have recently returned from a vacation in an exotic country with nausea and diarrhea and find out you are pregnant, see your doctor as soon as possible.
Gastroenteritis
One common cause of diarrhea during pregnancy is gastroenteritis or stomach flu. It is caused by bacterial or viral infections: norovirus, rotavirus, E. coli, salmonella, which enter the body through contact with contaminated surfaces, dishes, food and water.
Gastroenteritis usually lasts about three days. However, severe illness is a health hazard, especially during pregnancy, as it can cause dehydration, electrolyte imbalance, and lead to preterm labor.
The main symptoms of gastroenteritis are diarrhea without blood, nausea and vomiting, stomach cramps and pain, slight fever, headache and muscle pain.
Take extra precautions to reduce your risk of getting sick: frequent handwashing and surface disinfection. If the expectant mother has small children, they are not recommended to use the same cutlery.
Risks of diarrhea during pregnancy
Usually diarrhea during pregnancy is not a cause for concern. However, you should consult a doctor if the following symptoms occur during this period:
However, you should consult a doctor if the following symptoms occur during this period:
- Diarrhea for more than two days;
- Blood or mucus stools;
- Sudden weight loss;
- Abdominal pain;
- Dehydration.
How to treat diarrhea during pregnancy
If you have diarrhea during pregnancy, drink plenty of fluids, avoid foods high in fat and sugar, avoid dairy products, and caffeinated drinks.
Dehydration is a serious risk, especially during pregnancy, so electrolyte balance should be restored first with fluids and simple foods:
| Moderate fruit juices | Drinks without alcohol and caffeine |
| Bananas | Potato |
| Rice | Toast |
| Rusks | Light soups and broths |
| Pasta | Applesauce |
Use the Atlas Microbiota Test to find out your body's ability to break down lactose and gluten.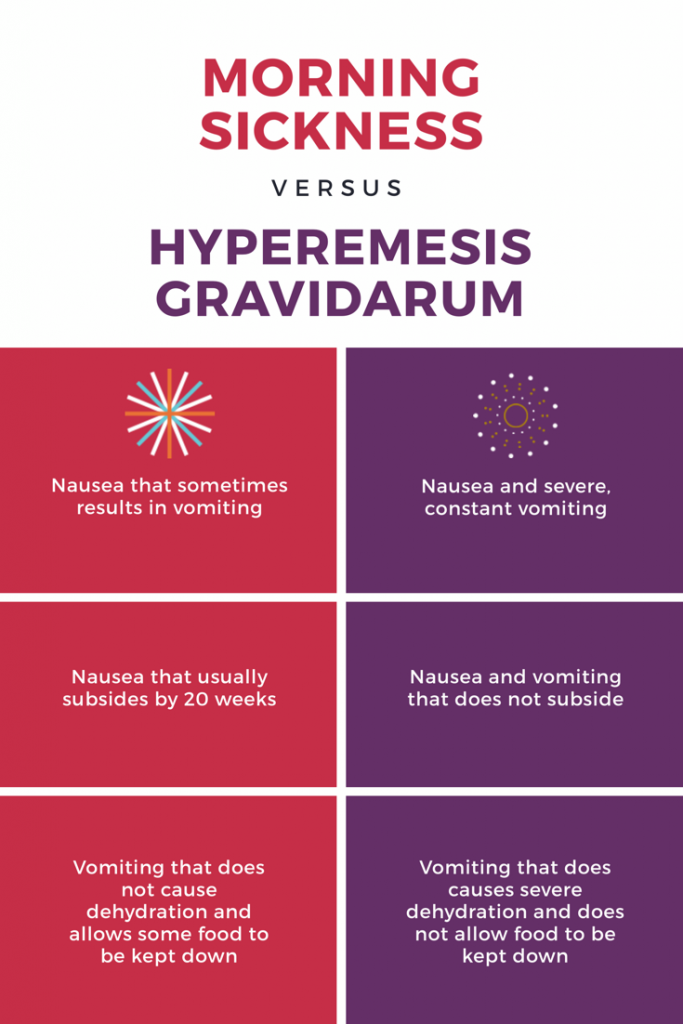
Stomach pain and heartburn during pregnancy
Many women experience stomach pain during pregnancy, especially the upper part of the stomach, as well as heartburn - a burning sensation in the chest and esophagus.
This is more common in the third trimester, after about 27 weeks. This is an unpleasant but natural phenomenon during pregnancy: the baby grows inside the uterus and presses on other organs, including the stomach. And hormones cause the muscles to relax, which causes acid from the stomach to enter the esophagus and irritate it. In addition, pain can be caused by problems with certain organs such as the gallbladder, or inflammation of the pancreas.
Symptoms of heartburn during pregnancy:
- Burning in chest and esophagus;
- Feeling of overeating, heaviness or bloating;
- Belching, including with acid and/or food particles;
- Nausea.
It is unlikely that you will be able to avoid cramps and heartburn during pregnancy. However, some tips can help reduce their frequency:
However, some tips can help reduce their frequency:
Nutrition : try to avoid overeating - eat easily digestible food in small portions; do not eat three hours before bedtime; watch your posture while eating - so the pressure on your stomach will be less.
Smoking and alcohol: In addition to known harms to mothers and babies, tobacco smoke also relaxes the muscles in the lower esophagus, allowing acid to enter the esophagus. And alcohol provokes heartburn and acid reflux.
Although stomach pain and heartburn often accompany pregnancy, abdominal pain, especially in the third trimester, should be taken seriously. It can be a sign of preterm labor or placental abruption, and puts mother and baby at risk.
If you experience severe abdominal pain during pregnancy that is accompanied by the following symptoms, seek medical attention as soon as possible:
| Abdominal pain and fever | Bleeding |
| Regular seizures | Unusual vaginal discharge/ spotting |
| Vomiting | Low back pain |
| Pain or burning when urinating | Severe pain that lasts 30-60 minutes |
Bloating, constipation and microbiota during pregnancy
Excessive gas and constipation during pregnancy can be caused by hormonal changes, such as increased production of progesterone.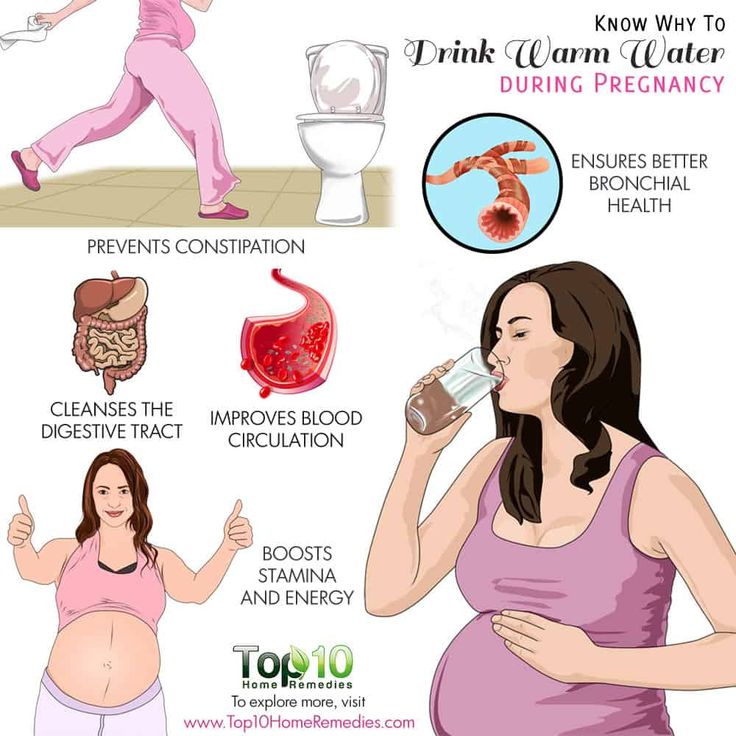 This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
This hormone, essential for nourishing the uterus and fetus, relaxes the muscles of the body, including the muscles in the intestines, which slows down digestion and increases flatulence. A similar reaction of the body can be observed before each menstruation, when the production of progesterone increases.
Flatulence - bloating of the abdomen due to the accumulation of gases.
Here are a few simple rules that will help improve intestinal motility and avoid constipation and bloating:
- If you do not usually eat a lot of fiber and indigestible foods like legumes, try to gradually introduce them into the diet;
- Avoid carbonated drinks and fatty foods;
- Move more;
- Drink plenty of fluids.
If bloating and constipation are accompanied by severe pain that lasts more than 30 minutes, or if you have been constipated for two or more weeks, see your doctor.
Gut microbiota and bacteria during pregnancy
A woman's body goes through many changes during pregnancy, and this can affect the microbiota, the bacterial ecosystem that lives in the gut. Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
Trillions of microorganisms do important work for the whole body: they synthesize vitamins and essential acids, keep your intestines working and protect it from disease and inflammation.
The additional influx of female hormones that accompanies pregnancy alters gut function and affects the microbiota. This is good, because the bacterial community is constantly adjusting to external and internal conditions in order to keep up with the needs of the body.
To keep your gut bacteria running smoothly, they need your help. Provide them with healthy foods and plant fibers. Fruits, vegetables, whole grains, nuts, and seeds contain prebiotics, special substances that beneficial bacteria feed on. When properly balanced, the bacteria even increase your body's defenses against harmful microorganisms that can cause gastroenteritis during pregnancy.
The Atlas Microbiota Test will help you understand how to prepare your intestines for a future pregnancy and reduce the risk of digestive problems.
☝️ Take note
Now you have all the necessary knowledge and tools to help you deal with digestive problems during pregnancy. They are quite varied and quite natural, but in some cases it is necessary to immediately seek medical help:
- Vomiting blood;
- Blood in stool;
- Diarrhea for more than two days;
- Constipation for more than two weeks;
- Sudden weight loss;
- Severe pain interfering with daily activities;
- Difficulty breathing;
- Pain when swallowing or difficulty swallowing;
- Excessive fatigue.
More articles on the causes of digestive problems on the blog:
- 7 foods that cause gas and bloating
- Leaky intestine
- When the intestine is upset
- Mayo Clinic, Morning20 Morning20
- Lindsey J Wegrzyniak, Treatment of Hyperemesis Gravidarum, 2012
- Edwards A. et al., The Maternal Gut Microbiome During Pregnancy, 2018
- National Health and Safety (NHS), Vomiting and morning sickness in pregnancy
- Kudzai Kanhutu, Travel and pregnancy: an infectious diseases perspective, 2011
- CDC, Pregnant travelers
- U.