Prescription weight loss pills while breastfeeding
Diet and medication while breastfeeding
Diet and medication while breastfeeding | Pregnancy Birth and Baby beginning of content6-minute read
Listen
Breastfeeding mothers often worry that what they eat and drink (consume) can affect their baby. You don't need to follow a special diet when breastfeeding. But you do need to be careful with some things.
Your diet and breastfeeding
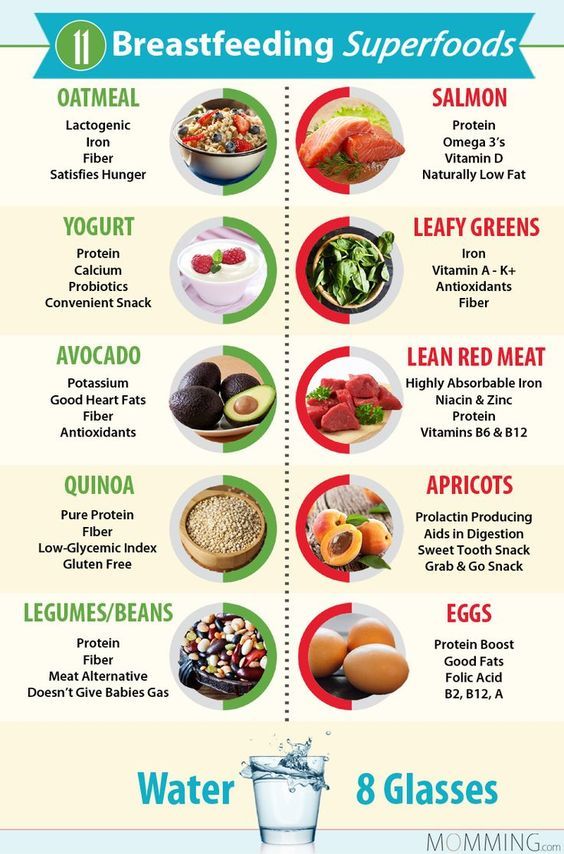
No matter what foods you eat, your body will make healthy breast milk. Eating a nutritious diet and drinking enough fluids will help you produce enough milk.
Breastfeeding uses a lot of calories so you may need to eat a little more than normal.
Make sure to include plenty of protein, calcium and iron in your diet. You may also need an iodine supplement.
You might worry that some foods like spices, garlic, beans or cabbage might make your baby gassy and irritable. Food is rarely the cause, and you should rule out some other possibilities before changing your diet.
There is no need to avoid allergenic foods such as peanuts, egg or milk while you are breastfeeding. The research suggests that this will not stop your baby becoming allergic to these foods.
There is little evidence to support eating foods that claim to boost your milk supply. If you are worried about your milk supply you should talk to your doctor.
Caffeine and breastfeeding
Most breastfeeding mothers can consume a few cups of tea or coffee each day.
But caffeinated energy drinks are not recommended for pregnant or breastfeeding women.
The amount of caffeine in your breast milk usually peaks about 1 hour after you consume it.
You should not have more than 200mg of caffeine per day while breastfeeding. The following is a handy guide:
- espresso coffee has 60–120 mg per 250 mL cup
- instant coffee (one teaspoon/ cup) has 60–80 mg per 250 mL cup
- tea has 10–50 mg per 250 mL cup
Newborn babies are particularly sensitive to caffeine. This is because it can take them between 2 and 4 days to process caffeine.
This is because it can take them between 2 and 4 days to process caffeine.
Alcohol and breastfeeding
It’s best to limit alcohol while you’re breastfeeding. The amount of alcohol in your breast milk is the same as in your blood.
Alcohol enters your breast milk 30 minutes to 1 hour after you start drinking. This depends on how much alcohol you drink, whether you have eaten, how much you weigh and how quickly you are drinking.
It takes about 2 hours for your body to get rid of the alcohol from one standard drink.
If you do have an occasional drink, feed your baby and express milk before you start drinking. Your baby can drink the expressed milk while there is still alcohol in your body.
The safest option is to avoid drinking alcohol when you are breastfeeding.
If you do plan on drinking alcohol use the Feed Safe apps.
Medications and breastfeeding
Ask your doctor or pharmacist for advice on medicines that are safe to take while breast feeding.
Most medicines are safe to take at the recommended dose while breastfeeding. Even if the medicine does pass into your breast milk, it’s usually in such a small amount that it won’t harm your baby.
Take special care if your baby was premature, is sick or on medication.
For more information on medicines that are safe to take while breastfeeding, call the Medicines Line on 1300 MEDICINE (1300 633 424) Monday to Friday, 9am to 5pm AEST.
Contraception and breastfeeding
If you are breastfeeding, you can get still pregnant, even if your periods haven't started again.
Except for combined hormonal contraception (products that contain both oestrogen and progestogen), contraception can be safely used immediately after birth. Talk to your doctor about protection while breastfeeding.
Complementary and alternative medicines and breastfeeding
Complementary and alternative medicines (CAMs) include vitamins, dietary supplements, aromatherapy and homeopathic products.
We often think of CAMs as safer than pharmaceutical medicines. But there is little research to support the safety of CAMs.
Many CAMs are not recommended for use when breastfeeding. Talk to your doctor, pharmacist or call the Medicines Line before you take any CAMs while breastfeeding.
If you’re unsure about consuming something while you’re breastfeeding, ask your doctor or lactation consultant about it.
Smoking and breastfeeding
It is best not to smoke if you are breastfeeding.
If you can’t quit smoking, it is still better for your baby to be breastfed.
The amount of nicotine in your breast milk halves about 1.5 hours after each cigarette. So, if you smoke, do so right after a breastfeed. The longer the time you leave between a cigarette and the next feed, the better.
It is very important to protect your baby from cigarette smoke, which puts your baby at risk of chest infections, asthma and sudden infant death syndrome. Don’t smoke around your baby, in the house. Smoking in your car with a child aged under 16 years is illegal.
Smoking in your car with a child aged under 16 years is illegal.
Where to get more advice:
- Pregnancy, Birth and Baby - 1800 882 436
- Poisons Information Centre - 13 11 26
- Australian Breastfeeding Association - 1800 686 268
Sources:
Cochrane Library (Oral galactagogues (natural therapies or drugs) for increasing breast milk production in mothers of non‐hospitalised term infants), Food Standards Australia and New Zealand (Pure and highly concentrated caffeine products), RACGP (Breastfeeding Evidence based guidelines for the use of medicines), RANCOG (FSRH Guideline Contraception After Pregnancy), Australian Breastfeeding Association (Breastfeeding and food sensitivities), Australian Breastfeeding (Breastfeeding and maternal), Australian Breastfeeding Association (Alcohol and breastfeeding), Australian Breastfeeding Association (Breastfeeding and smoking), NSW Health (Smoking with kids in the car is illegal), NHMRC Dept of Health and Ageing (Eat for Health: Infant Feeding Guidelines Information for Health Workers)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2022
Back To Top
Related pages
- Breastfeeding your baby
Need more information?
Breastfeeding diet, exercise & lifestyle | Raising Children Network
A healthy breastfeeding diet has a wide variety of foods from the five main food groups. Physical activity is also important for your health and wellbeing.
Read more on raisingchildren.net.au website
Breastfeeding and your diet - Better Health Channel
Breastfeeding women need to eat regularly and include a wide variety of healthy foods in their diet.
Read more on Better Health Channel website
Healthy eating when you’re pregnant or breastfeeding | Eat For Health
Eating well during pregnancy and while breastfeeding has health benefits for you and your baby.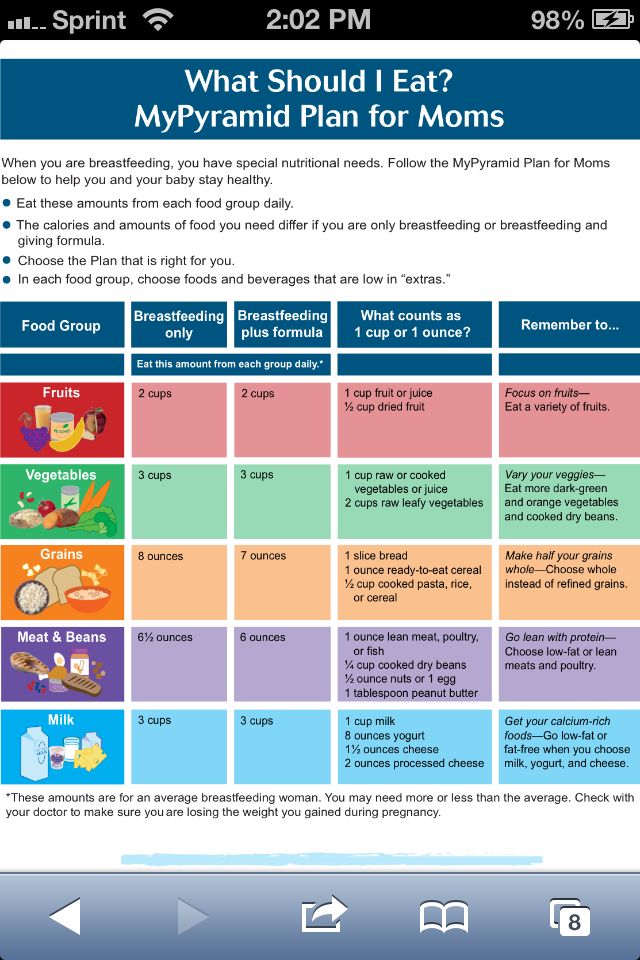
Read more on NHMRC – National Health and Medical Research Council website
Breastfeeding
Breastfeeding is learnt over the first weeks and months of your child’s life. It is a unique and special experience for families as no two mothers or babies are the same.
Read more on Karitane website
Healthy diet during pregnancy
A healthy diet is an important part of a healthy lifestyle at any time, but especially vital if you're pregnant or planning a pregnancy.
Read more on Pregnancy, Birth & Baby website
Breastfeeding Helpline | Australian Breastfeeding Association
Free 24/7 information and support from qualified breastfeeding counsellors
Read more on Australian Breastfeeding Association website
Losing weight after birth safely
Tips for losing weight after birth, including how to enjoy a healthy lifestyle, setting realistic goals, breastfeeding and weight loss and when to seek help.
Read more on Pregnancy, Birth & Baby website
Vegetarian and vegan eating - Better Health Channel
A well-planned vegetarian or vegan diet can meet nutritional needs during all stages of life.
Read more on Better Health Channel website
Vasospasm and breastfeeding
Vasospasm affects the flow of milk from the nipple and can be a painful condition for women breastfeeding. Learn about vasospasm and how to relieve the pain.
Read more on Pregnancy, Birth & Baby website
My breastfeeding plan | Australian Breastfeeding Association
Made a birth plan? What about making a breastfeeding plan?
Read more on Australian Breastfeeding Association website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.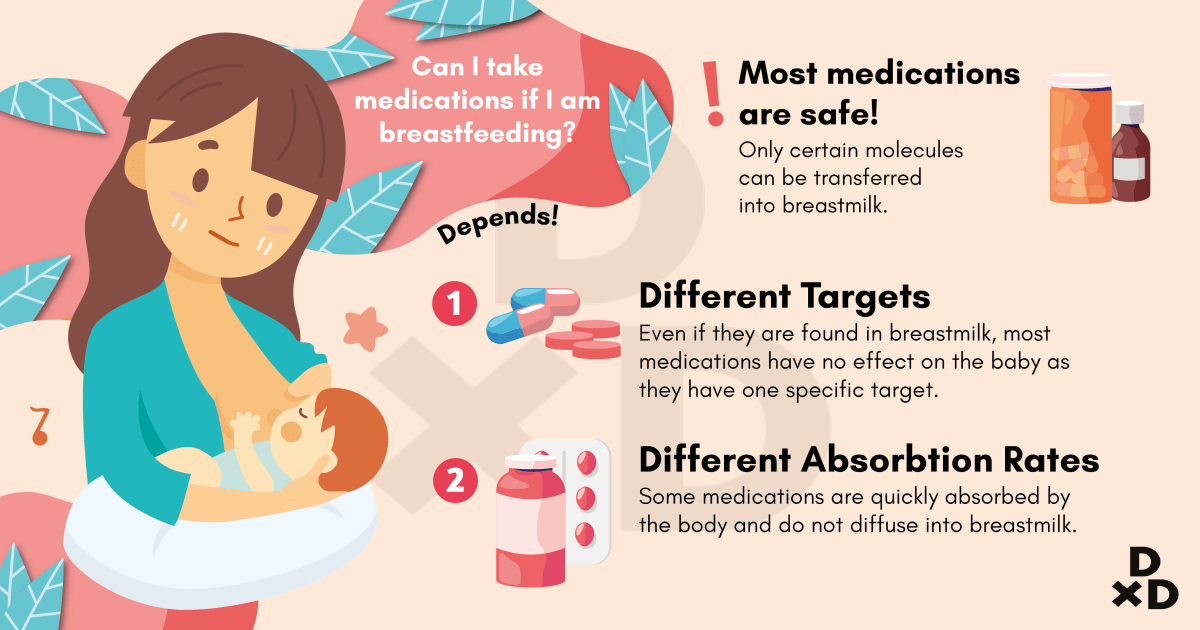
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Should You Try Weight Loss Supplements While Breastfeeding? – milkdust
Weight loss supplements can be safe and helpful while breastfeeding. Sometimes breastfeeding causes a road block for weight loss. Herbal, safe supplements can help new mommies let go of the extra weight gained during pregnancy.
Milk Dust is a helper for weight loss because it naturally curbs sugar cravings using vitamins and minerals rather than stimulants. This is the key to safe weight loss supplements. They need to be comprised of specific nutrients, vitamins and minerals that are helpful to both mama and baby.
This is the key to safe weight loss supplements. They need to be comprised of specific nutrients, vitamins and minerals that are helpful to both mama and baby.
What makes a weight loss supplement safe for breastfeeding?
There are some very specific requirements for a weight loss supplement to be safe for breastfeeding.
- Comprised of nutrients
- Free of stimulants
- No caffeine
- No synthetic replications of vitamins
- Hormonal support
- Nourishment support
- Cognitive support
A safe weight loss supplement looks at the root of the cause, rather than covering up appetite or hunger. Stimulants like caffeine can cover up hunger, but it doesn't look at the root cause behind the lack of energy, slow weight loss or nutrient needs. Milk Dust specifically looks at common nutrient needs to help satisfy hunger and balance blood sugar. Cravings often come from your body's need for a nutrient, cognitive support or even extra carbs to support a tired brain. Many mamas crave sugar while breastfeeding, but what their brain needs are more healthy carbs to function on little sleep.
Many mamas crave sugar while breastfeeding, but what their brain needs are more healthy carbs to function on little sleep.
Nutrient Deficiencies That Slow or Halt Weight Loss While Breastfeeding:
Breastfeeding mamas specifically need more nutrients than non-lactating women, and many nutrients needs don't change that much after pregnancy. Some of these nutrients include:
- Folate
- Vitamin B12
- Chromium, Magnesium, Potassium and Sodium
- Protein
- Fiber (not a nutrient, but essential carbohydrate)
Folate and vitamin B12 can really create some lethargy and lack of motivation to eat healthy. Both of these B vitamins relate to cognitive function, energy, and they are necessary for baby. If these are lacking, your body can't function they way it should. The same with protein and fiber. Without protein, there can be a lot of ups and down with blood sugar, which causes excessive hunger. Fiber creates a feeling of fullness that makes you want to stop eating. If there isn't enough fiber, there is a constant hunger or feeling of never getting enough food. This leads to that ravenous, always hunger feeling many breastfeeding mamas experience.
If there isn't enough fiber, there is a constant hunger or feeling of never getting enough food. This leads to that ravenous, always hunger feeling many breastfeeding mamas experience.
Not all weight loss supplements have this sort of blend in vitamins and nutrients, but Milk Dust has all of this and more. With protein, fiber and essential vitamins and minerals, in addition to galactagogue herbs like Fenugreek, fennel seed, milk thistle and brewer's yeast, a mother can support her lactation and weight loss at the same time.
How To Know If You Need A Weight Loss Supplement While Nursing:
Not all mamas need a weight loss supplement while nursing. Some just need to count calories and determine their energy needs. Weight loss is all about energy in verses energy out. Of course, not all calories are created equal. This means that 100 calories of cookies verses 100 calories of broccoli are going to be used, processed and metabolized very, very differently. One can leave you feeling super full (broccoli from fiber), and the other starving in 30 minutes.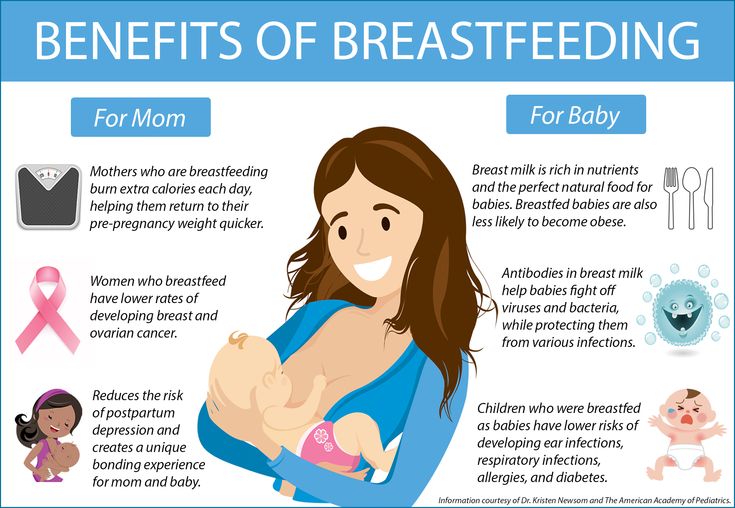
If you are struggling to eat healthy and manage your breastfeeding hunger, weight loss supplements might be just the answer to give you a jump start.
Here are some signs a weight loss supplement can help your weigh loss after pregnancy:
- Constant hunger
- Intense sugar cravings
- Carbohydrate addiction
- Hunger soon after large meals
- Exhaustion after eating
- Lack of physical energy
- Weight gain while breastfeeding
If you are experiencing any of these issues, safe weight loss supplements are awesome tools to move your body into healthier eating habits. Milk Dust is a breastfeeding weight loss supplement that fully supports nourishment and lactation in new mommies.
Milk Dust Works As A Weight Loss Supplement While Breastfeeding:
Milk Dust helps with weight loss by providing satiation through protein and fiber. We recommend blending Milk Dust with whole fruits and veggies either frozen or fresh. By adding the additional nutrients to our powder, the powerful combination creates a small meal or snack that covers your bases. Here's the run down of how Milk Dust acts as a weight loss and lactation supplement for breastfeeding mamas:
By adding the additional nutrients to our powder, the powerful combination creates a small meal or snack that covers your bases. Here's the run down of how Milk Dust acts as a weight loss and lactation supplement for breastfeeding mamas:
- Satiating protein
- Sweet taste to relieve those sugar cravings
- Essential vitamins and minerals
- Energy boosting super foods like Chlorella and Spirulina
- Galactagogue herbs for lactation support
- Super fruits and veggies like spinach and blue berries
- Turmeric and Cinnamon bark for additional blood sugar control, antioxidant support and adrenal support
- Vegan, non-dairy, no soy, no corn, no gluten for easier digestion
- Plant-based protein
- Chia seeds, flax seeds and pumpkin seeds for Omega-3s and Zinc
Nutritional support is one of the safest ways to encourage healthy weight loss. Avoiding stimulants and using nutrients while breastfeeding helps for safe weight loss.
Finding a safe weight loss supplement while breastfeeding is helpful for mamas looking to lose weight naturally.
Back to blogRelated blogs
View all-
IBS and Pregnancy: How To Safely Manage IBS For Pregnant Women
The fact that more than 67% of the population have Irritable Bowel Syndrome (IBS) is enough to give you a gist of what we're about to discuss today. Pregnancy, as...
-
How To Count Macros While Breastfeeding
Many new moms are looking for ways to get back in shape without sacrificing milk production. Losing weight while breastfeeding can be super tricky because lactation requires extra calories, yet...
1 / of 2
View all
Breastfeeding and drug use
And now the birth is behind, the labor pain has been forgotten, lactation has been established, and at any moment a new problem may arise in front of the young mother: how the medicine will affect the newborn baby when breastfeeding. Unfortunately, not every mother can boast of excellent health and there is a need to take medication.
Unfortunately, not every mother can boast of excellent health and there is a need to take medication.
The degree of adverse effect of the drug on the body of the newborn is determined by the following factors:
- drug toxicity;
- the true amount of the drug that entered the child's body;
- a feature of the effect of the drug on the immature organs of the child;
- the duration of the drug excretion from the child's body;
- the duration of taking the medicine by a nursing mother;
- individual sensitivity of the child to this drug;
- the risk of developing allergic reactions.
Of the most commonly used drugs, most are not very toxic drugs that cause significant toxic effects on organs and tissues. Therefore, it is believed that in many cases, with medical treatment, breastfeeding can be continued.
If a woman combines breastfeeding and treatment, then it may be useful to select the optimal scheme for alternating the drug and feeding. It is necessary to take the medicine in such a way that the time of feeding does not fall on the period of its maximum concentration in the blood.
It is necessary to take the medicine in such a way that the time of feeding does not fall on the period of its maximum concentration in the blood.
When using the medicine, a woman during breastfeeding should be aware that the side effects caused by this drug may also occur in a child.
If the risk of adverse effects of the drug on the child's body is high, then for the duration of treatment you need to stop breastfeeding, but continue pumping milk to maintain lactation. After the end of the course of treatment, it is necessary to resume breastfeeding. It is believed that after a course of antibiotics incompatible with breastfeeding, you can feed 24 hours after the last dose of the drug. And when using a number of radioactive agents, the radioactivity of milk can persist from 3 days to 2 weeks.
Features of the use of various groups of drugs during breastfeeding
Medicines contraindicated while breastfeeding:
Cytostatics and radioactive preparations (drugs used to treat tumors and autoimmune diseases, rheumatoid arthritis). These drugs significantly suppress immunity and cell division. If necessary, these drugs stop breastfeeding.
These drugs significantly suppress immunity and cell division. If necessary, these drugs stop breastfeeding.
Antibiotics is used to treat various infectious and inflammatory diseases. Penicillins, cephalosporins, macrolides, aminoglycosides are usually not contraindicated in breastfeeding. These antibiotics pass into milk in small amounts, so their toxicity to the child is low.
Macrolides (erythromycin, sumamed, vilprofen, etc.) penetrate milk well, but their use during breastfeeding is possible. There is a potential risk of developing complications associated with the occurrence of allergic reactions, disruption of the normal intestinal flora (diarrhea), reproduction of fungi (candidiasis - thrush). For the prevention of dysbacteriosis, it is recommended that the child be given probiotics (Bifidum Bacterin, Linex). If an allergic reaction occurs in a child, you should stop taking this antibiotic or temporarily stop breastfeeding.
Tetracyclines, sulfonamides (Bactrim, Biseptol, etc. ), Metronidazole, Clindamycin, Lincomycin, Ciprofloxacin penetrate into milk, and the likelihood of negative reactions is high. Therefore, the use of these drugs during breastfeeding is contraindicated.
), Metronidazole, Clindamycin, Lincomycin, Ciprofloxacin penetrate into milk, and the likelihood of negative reactions is high. Therefore, the use of these drugs during breastfeeding is contraindicated.
Side effects of tetracyclines - growth retardation of the child, a violation of the development of bone tissue and tooth enamel of the child. Side effect of Clindamycin - risk of gastrointestinal bleeding; and Levomycetin - toxic damage to the bone marrow, the effect on the cardiovascular system.
Antihypertensive agents are used in hypertension.
When breastfeeding, the following drugs can be used with caution: Dibazol, Dopegit, Verapamil.
Contraindicated in breastfeeding: Cordaflex, ACE inhibitors (Enap, Kapoten), Diazoxide, Reserpine.
The use of antihistamines for allergies during breastfeeding is possible. It is advisable to use Cetirizine, Loratadine. It is not desirable to use 1st generation drugs (Suprastin, Tavegil), which can cause drowsiness in a child. Erius is contraindicated in breastfeeding.
Erius is contraindicated in breastfeeding.
Antithyroid drugs for breastfeeding
Antithyroid drugs are used in diseases of the thyroid gland, occurring with an increase in its function. These drugs are used when breastfeeding with caution, controlling the condition of the child. They suppress the function of the child's thyroid gland.
Salbutamol, terbutaline, fenoterol are approved for use during breastfeeding. It is necessary to monitor the condition of the child, since their side effect is excitement, increased heart rate.
Hormones (prednisolone, dexamethasone, hydrocortisone) are used for autoimmune diseases (rheumatoid arthritis, systemic connective tissue diseases, autoimmune hepatitis, etc., with adrenal insufficiency) are usually not contraindicated in breastfeeding.
However, if it is necessary to treat them for more than 10 days, the issue of continuing breastfeeding is decided individually. If a woman needs long-term hormonal treatment at a high dose, breastfeeding should be stopped.
Paracetamol is not contraindicated during breastfeeding if used in the usual dose (1 tablet up to 3-4 times a day, no more than 2-3 days). Exceeding the dose and long-term use of paracetamol should be avoided, since the side effect of the drug is a toxic effect on the liver and blood.
Contraceptives for breastfeeding
When breastfeeding, drugs containing progesterone are allowed. Other medicines are contraindicated during breastfeeding.
Expectorants during breastfeeding
- Ambroxol, Bromhexine, ACC can be used during breastfeeding.
- Pre- and probiotics (Linex, Hilak forte, etc.) are compatible with breastfeeding.
It should be noted that in our Center for Mother and Child, all medications used are safe for the health of the baby and mother. We try to minimize the prescription of drugs, only in the most extreme cases are prescribed drugs that are contraindicated during breastfeeding. And the most important recommendation is not to prescribe medications on your own, especially to nursing mothers! Health to you and your Babies!
Obstetrician-gynecologist Nugmanova M. K .
K .
Checked the head. genus. house number 2 Markashova M. Yu.
How to lose weight while breastfeeding
How to lose weight while breastfeeding 8 812 380 02 38St. Petersburg
Make an appointment
Feeding a nursing mother is a very important issue. The health of the child, as well as the health and appearance of the mother, depend on a correct and balanced diet. In magazines and the Internet you can find a huge number of recommendations, but, unfortunately, many of them are far from the truth. For example, it is recommended to increase the daily caloric intake of a nursing woman to 3000 - 3500 kcal. For comparison: the daily calorie content of the diet of people engaged in heavy, manual, non-mechanized labor (manually drag bricks to the tenth floor all day) is 4000 kcal. Knowledge workers (an engineer who travels to and from work by public transport and walks at lunchtime), i. e. people with minimal physical activity should receive about 2000 kcal per day. No matter how much they write about how hard it is to be a mother, how much you need to do (wash, wash, iron), modern life is greatly facilitated by household appliances. If not every apartment still has a dishwasher, then everyone has a washing machine, and no one uses heavy cast-iron irons either. So whatever one may say, a nursing mother is a woman with minimal physical activity. And an extra thousand calories will go not to increase the calorie content, fat content and nutritional value of milk, but to the mother’s hips and stomach.
e. people with minimal physical activity should receive about 2000 kcal per day. No matter how much they write about how hard it is to be a mother, how much you need to do (wash, wash, iron), modern life is greatly facilitated by household appliances. If not every apartment still has a dishwasher, then everyone has a washing machine, and no one uses heavy cast-iron irons either. So whatever one may say, a nursing mother is a woman with minimal physical activity. And an extra thousand calories will go not to increase the calorie content, fat content and nutritional value of milk, but to the mother’s hips and stomach.
A large number of studies have been conducted, according to which it has been established that women living in a wide variety of conditions (favorable and not very favorable) can fully lactate. Women in primitive cultures, on a very modest diet, produce milk in sufficient quantity and proper quality to feed their child. Lack of nutrition does not affect the quality of milk. An increase in the calorie content of the daily diet also does not lead to changes in the composition of breast milk.
An increase in the calorie content of the daily diet also does not lead to changes in the composition of breast milk.
Most women are concerned about maintaining their figure after having a baby.
During pregnancy, a woman's body stores fat. Therefore, the weight after the birth of a child is somewhat greater than before. These fat reserves are necessary for the body to maintain strength in case of real hunger. After all, nature must make sure that all the cubs survive. And it is during the period of breastfeeding that these fat reserves begin to be consumed. Therefore, if a woman after the birth of a child eats properly and in a balanced way, then by the end of the breastfeeding period (in 1.5 - 2 years), her weight will return to its previous indicators.
Once again, there is no need to follow any special diets either for weight loss or to increase the fat content of breast milk (yogurt 9% fat and 35% sour cream will not affect the fat content of milk, but will affect your thighs).
The main task of a mother in the struggle for the harmony of her figure is to try not to increase her weight after the birth of a child. And in this she will be helped by the well-known principles of a healthy and rational diet.
The calorie content of the daily diet should correspond to the woman's physical activity. If she works in the field for agricultural work - the calorie content is higher, if she sits at home and walks at a slow pace with a stroller in the park - the calorie content is much lower.
- So, what are the basic principles of a healthy diet? Daily calorie content is about 2000 kcal, depending on physical activity. No more needed, tk. excess calories will be stored as excess weight. Less is also not necessary, tk. this will lead to a slowdown in metabolism and poor health for both mother and child.
- Eat often about 5-6 times a day, avoiding the appearance of a strong feeling of hunger. It has been proven that a strong feeling of hunger leads to overeating, and therefore to the appearance of excess weight.
- Food should be satisfying. For example, meat with vegetables. Vegetables are a source of carbohydrates, which contribute to a quick feeling of satiety, because. fill the stomach. Meat is protein. It is absorbed longer than carbohydrates, which contributes to the long-term preservation of the feeling of satiety.
- Do not be distracted by anything while eating: do not watch TV, do not read a magazine, even if the baby is crying, try not to be distracted. For 30 minutes that you eat nothing will happen, savor every bite. The process of eating should be treated very carefully. Eating on the run does not contribute to proper digestion or weight management.
When choosing food for yourself, it is important to remember that the main task of food is to maintain energy and saturate the body with all the necessary nutrients: vitamins, minerals, microelements.
The basis of the diet, oddly enough, is carbohydrates. You get them from grain products and vegetables. They are the best sources of fiber, B vitamins, trace elements. The most useful grain products are wild and brown rice, pearl barley, oatmeal, buckwheat and millet, wholemeal pasta, cereal bread. It is advisable to eat 10 servings of grain products per day. One serving is ½ cup of porridge or pasta or 1 slice of whole grain bread.
They are the best sources of fiber, B vitamins, trace elements. The most useful grain products are wild and brown rice, pearl barley, oatmeal, buckwheat and millet, wholemeal pasta, cereal bread. It is advisable to eat 10 servings of grain products per day. One serving is ½ cup of porridge or pasta or 1 slice of whole grain bread.
Vegetables and fruits - any. 10-13 servings per day. One serving: 1 cup fresh herbs, ½ cup vegetables, 1 banana or apple or orange, ½ cup canned fruit.
Proteins are fish, meat, poultry, eggs, dairy products (kefir, cottage cheese). Fish is a source of heart-healthy fatty acids, as well as calcium and phosphorus, necessary for strong bones. The need for fish is 2-3 servings per week. One serving is a piece the size of a palm without fingers. Meat is a source of trace elements. These are low-fat varieties of beef, pork, rabbit. The need is 4-5 servings per week. The portion size is the same. Dairy products are a source of calcium, the norm is 2 servings per day. One serving is one glass. (And another essential serving of calcium per day is 1 cup of spinach or broccoli.)
One serving is one glass. (And another essential serving of calcium per day is 1 cup of spinach or broccoli.)
Fats are found in butter (animal fat) and vegetable (vegetable fat) oils. And the share of animal fats should account for only 10%. This means that food should be cooked mainly using vegetable oil.
In addition to the composition of the products, great importance is attached to the method of cooking.
For example, raw vegetables and fruits retain more vitamins and minerals.
Meat, fish, poultry, it is better to boil or bake in the oven, which allows you to reduce the calorie content of the finished dish, because. no oil is added.
Keep in mind that beverages such as juices contain a lot of extra calories and very little fiber and vitamins. Therefore, to compensate for the deficiency of vitamins and fiber, it is better to eat an apple. And to quench your thirst, use drinking water. The amount of liquid in the diet of a nursing mother is about 2 - 2. 5 liters per day. It is considered that soups and fruits are 100% liquid.
5 liters per day. It is considered that soups and fruits are 100% liquid.
As for “empty” products that contain neither fiber, nor vitamins, nor microelements, but only extra calories, these are a wide variety of rich products: cookies, crackers, dryers, cakes, cakes, ice cream. Since, after the birth of a child, a mother constantly wants to eat, and there is not enough time to prepare a full meal, she begins to absorb cookies in unlimited quantities. And the weight, of course, increases. I'm not talking about the fact that the cause of colic and flatulence in a small child is very often the excessive consumption of "empty" carbohydrates by the mother.
And a little more about calories. Everyone talks about them, but no one knows what they look like. So, 100 kcal are contained in 1 banana, or 8 tablespoons of cooked beans, or 1.3 cookies, or 2 medium apples, or 340 ml of light beer, or 1/5 of a big mac, or 1/12 of a medium pizza with meat, or 4 slices of french fries, or 1/5 pita bread, or 2 gin tonics, or 17 peanuts, or 300 ml of milk, or 9 chips.