Pregnancy and radiation exposure at work
Ionizing Radiation - Pregnant Workers
Pregnant Workers
Note: These are NOT OSHA regulations. However, they do provide guidance from their originating organizations related to worker protection.
National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC)
The National Institute for Occupational Safety and Health (NIOSH) maintains a webpage on reproductive health and the workplace, which includes information about reproductive hazards from occupational exposure to ionizing radiation and occupational settings that may be associated with such hazards.
NIOSH also provides information for aircrew (pilots and flight attendants) exposed to cosmic ionizing radiation at levels that may be of concern during pregnancy.
Nuclear Regulatory Commission (NRC)
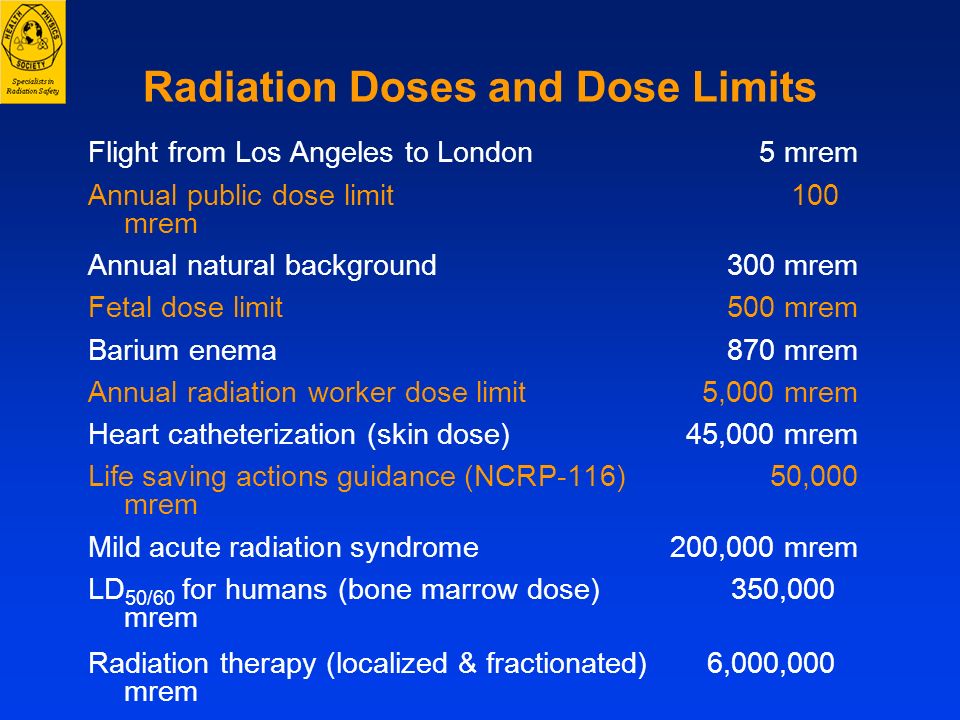
The Nuclear Regulatory Commission (NRC) Standards for Protection Against Radiation (10 CFR 20) require licensees to limit exposure to the embryo/fetus of an occupationally exposed individual to 500 mrem (5 mSv) or less during pregnancy for a declared pregnant worker who is exposed to radiation from licensed radioactive materials (10 CFR 20. 1208) including radionuclides. Under NRC's definitions (10 CFR 20.1003), a declared pregnant worker is a worker who has voluntarily informed the employer, in writing, of the pregnancy and the estimated date of conception. The declaration remains in effect until the declared pregnant worker withdraws the declaration in writing or is no longer pregnant.
The NRC's Instruction Concerning Prenatal Radiation Exposure, Regulatory Guide 8.13, provides information to pregnant women, and other personnel, to help them make decisions regarding radiation exposure during pregnancy.
International Commission on Radiological Protection (ICRP)
The International Commission on Radiological Protection (ICRP) 2007 recommendations include a limit of radiation exposure to a member of the general public of 100 mrem/year (1 mSv/year) and a limit for the fetus of an occupationally exposed individual of 100 mrem (1 mSv) for a declared pregnant worker during the pregnancy. See Publication 103: The 2007 Recommendations of the International Commission on Radiological Protection.
Publication 90: Biological Effects after Prenatal Irradiation (Embryo and Fetus) discusses pregnancy, radiation during pregnancy, health effects, and radiation protection.
Publication 88: Doses to the Embryo and Fetus from Intakes of Radionuclides by the Mother provides specific recommendations on the control of radiation exposures to pregnant workers after intakes of radionuclides before or during pregnancy.
National Council on Radiation Protection (NCRP)
National Council on Radiation Protection (NCRP) Report No. 128: Radionuclide Exposure of the Embryo/Fetus contains information on the effects of radiation exposure during pregnancy. It also provides radiation dose estimates for 83 radionuclides.
NCRP Report No. 116: Limitation of Exposure to Ionizing Radiation recommends an effective dose limit for radiation exposure to a member of the general public of 100 mrem/year (1 mSv/year) and an equivalent dose limit for the fetus of an occupationally exposed individual of 50 mrem (0.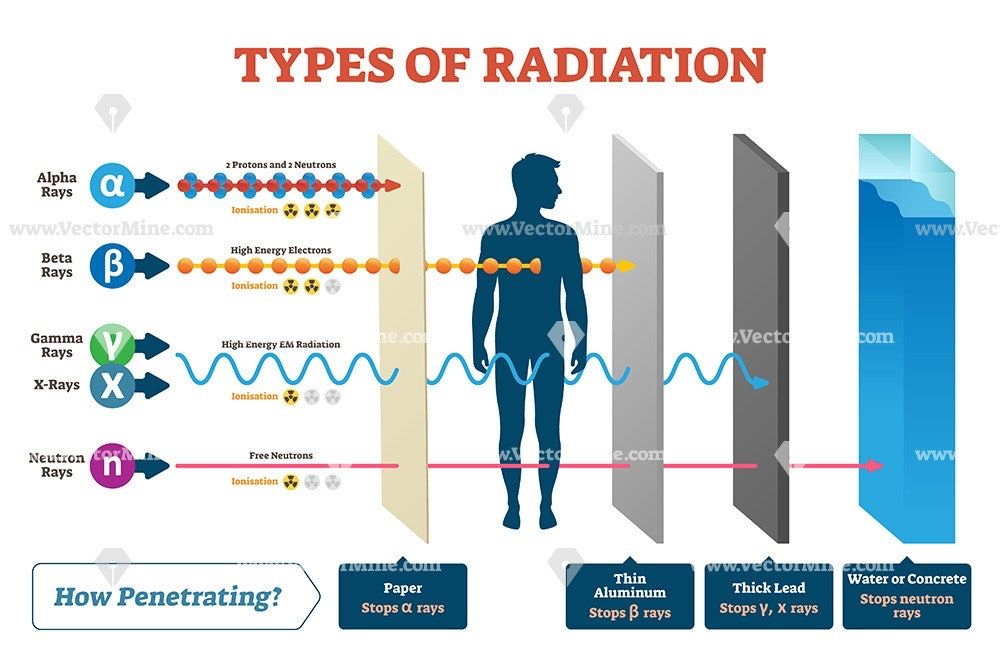 5 mSv) per month during the pregnancy.
5 mSv) per month during the pregnancy.
Conference of Radiation Control Program Directors (CRCPD)
The Conference of Radiation Control Program Directors (CRCPD) Suggested State Regulations for Control of Radiation currently recommend in Subpart D: Standards for Protection Against Radiation that the dose equivalent to the fetus due to occupational exposure of a declared pregnant worker be kept below 500 mrem (5 mSv) during the pregnancy.
Society for Cardiovascular Angiography and Interventions (SCAI)
The Society for Cardiovascular Angiography and Interventions (SCAI) published a consensus document concerning radiation exposure to pregnant individuals working in heart (cardiac) catheterization facilities, including interventional cardiologists, technicians, and nurses. SCAI Consensus Document on Occupational Radiation Exposure to the Pregnant Cardiologist and Technical Personnel reviewed current scientific data about risk to the fetus from occupational radiation exposure and recommended measures that pregnant physicians, technicians, and nurses should take to reduce radiation exposure.
Society of Interventional Radiology (SIR)
The Society of Interventional Radiology (SIR) jointly published Occupational Radiation Protection of Pregnant or Potentially Pregnant Workers in Interventional Radiology: A Joint Guideline of the Society of Interventional Radiology and the Cardiovascular and Interventional Radiology Society of Europe with guidance for radiation protection for pregnant workers for fluoroscopically-guided interventional procedures.
Radiation and Pregnancy: Information for Clinicians
This overview provides physicians with information about prenatal radiation exposure as an aid in counseling pregnant women.
How to use this document
This information is for clinicians. If you are a patient, we strongly advise that you consult with your physician to interpret the information provided, as it may not apply to you. Information on radiation exposure during pregnancy for members of the public can be found on the Health Information for Specific Groups webpage.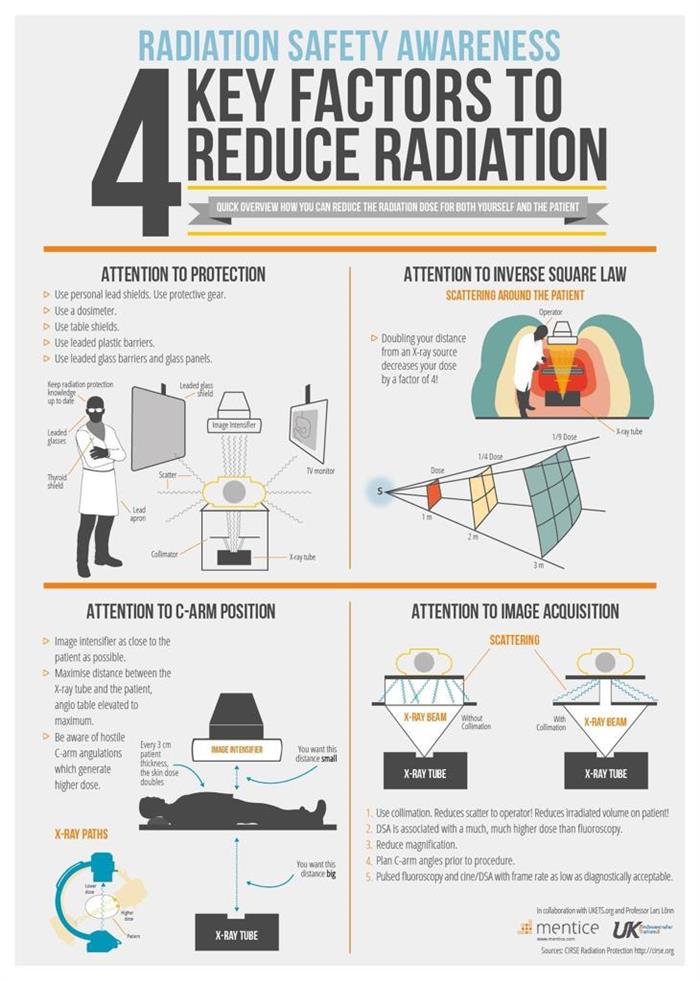
CDC recognizes that providing information and advice about radiation to expectant mothers falls into the broader context of preventive healthcare counseling during prenatal care. In this setting, the purpose of the communication is always to promote health and long-term quality of life for the mother and child.
This page is also available as a PDF pdf icon[365 KB]
Radiation exposure to a fetus
Most of the ways a pregnant woman may be exposed to radiation, such as from a diagnostic medical exam or an occupational exposure within regulatory limits, are not likely to cause health effects for a fetus. However, accidental or intentional exposure above regulatory limits may be cause for concern.
Although radiation doses to a fetus tend to be lower than the dose to the mother, due to protection from the uterus and surrounding tissues, the human embryo and fetus are sensitive to ionizing radiation at doses greater than 0.1 gray (Gy). Depending on the stage of fetal development, the health consequences of exposure at doses greater than 0.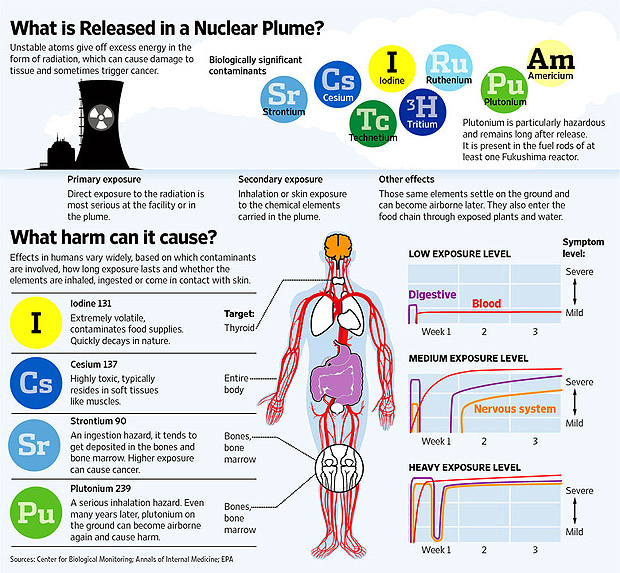 5 Gy can be severe, even if such a dose is too low to cause an immediate effect for the mother. The health consequences can include growth restriction, malformations, impaired brain function, and cancer.
5 Gy can be severe, even if such a dose is too low to cause an immediate effect for the mother. The health consequences can include growth restriction, malformations, impaired brain function, and cancer.
Estimating the Radiation Dose to the Embryo or Fetus
Health effects to a fetus from radiation exposure depend largely on the radiation dose. Estimating the radiation dose to the fetus requires consideration of all sources external and internal to the mother’s body, including the following:
- Dose from an external source of radiation to the mother’s abdomen.
- Dose from inhaling or ingesting a radioactive substance that enters the bloodstream and that may through the placenta.
- Dose from radioactive substances that may concentrate in maternal tissues surrounding the uterus, such as the bladder, and that could irradiate the fetus.
Most radioactive substances that reach the mother’s blood can be detected in the fetus’ blood. The concentration of the substance depends on its specific properties and the stage of fetal development. A few substances needed for fetal growth and development (such as iodine) can concentrate more in the fetus than in corresponding maternal tissue.
A few substances needed for fetal growth and development (such as iodine) can concentrate more in the fetus than in corresponding maternal tissue.
Consideration of the dose to specific fetal organs is important for substances that can localize in specific organs and tissues in the fetus, such as iodine-131 or iodine-123 in the thyroid, iron-59 in the liver, gallium-67 in the spleen, and strontium-90 and yttrium-90 in the skeleton.
Radiation experts can assist in estimating the radiation dose to the embryo or fetus
Hospital medical physicists and health physicists are good resources for expertise in estimating the radiation dose to the fetus. In addition to the hospital or clinic’s specialized staff, physicians may access resources from or contact the following organizations for assistance in estimating fetal radiation dose.
- The National Council on Radiation Protection and Measurementsexternal icon’ Report No. 174, “Preconception and Prenatal Radiation Exposure: Health Effects and Protective Guidance” [NCRP2013] provides detailed information for assessing fetal doses from internal uptakes.

- The International Commission on Radiological Protection’s “Publication 84: Pregnancy and Medical Radiation”external icon [ICRP2000] provides fetal dose estimations from medical exposures to pregnant women.
- The Conference of Radiation Control Program Directorsexternal icon maintains a list of state Radiation Control/Radiation Protection program contact information.
- The Health Physics Societyexternal icon maintains a list of active certified Health Physicists.
- The American Association of Physicists in Medicineexternal icon provides information resources.
Once the fetal radiation dose is estimated, potential health effects can be assessed.
Potential Health Effects of Prenatal Radiation Exposure (Other Than Cancer)
Table 1 summarizes the potential non-cancer health risks of concern. This table is intended to help physicians advise pregnant women who may have been exposed to radiation, not as a definitive recommendation. The indicated doses and times post-conception are approximations.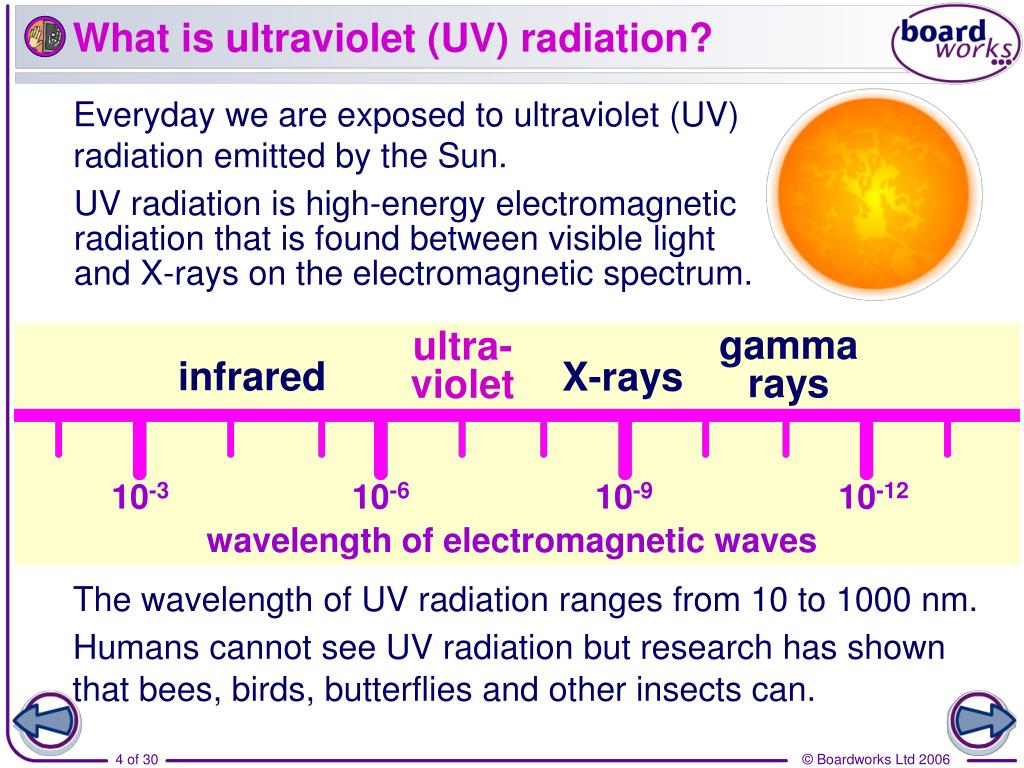
| Acute Radiation Dose* to the Embryo/Fetus | Time Post Conception (up to 2 weeks) | Time Post Conception (3rd to 5th weeks) | Time Post Conception (6th to 13th weeks) | Time Post Conception (14th to 23rd weeks) | Time Post Conception (24th week to term) |
|---|---|---|---|---|---|
| <0.10 Gy (10 rads) | Noncancer health effects NOT detectable | ||||
0.10–0. 50 Gy (10–50 rads) 50 Gy (10–50 rads) | Failure to implant may increase slightly, but surviving embryos will probably have no significant (non-cancer) health effects. | Growth restriction possible | Growth restriction possible | Noncancer health effects unlikely | |
| > 0.50 Gy (50 rads) The expectant mother may be experiencing acute radiation syndrome in this range, depending on her whole-body dose. | Failure to implant will likely be high, depending on dose, but surviving embryos will probably have no significant (non- cancer) health effects. | Probability of miscarriage may increase, depending on dose. Probability of major malformations, such as neurological and motor deficiencies, increases. Growth restriction is likely | Probability of miscarriage may increase, depending on dose. Growth restriction is likely. | Probability of miscarriage may increase, depending on dose.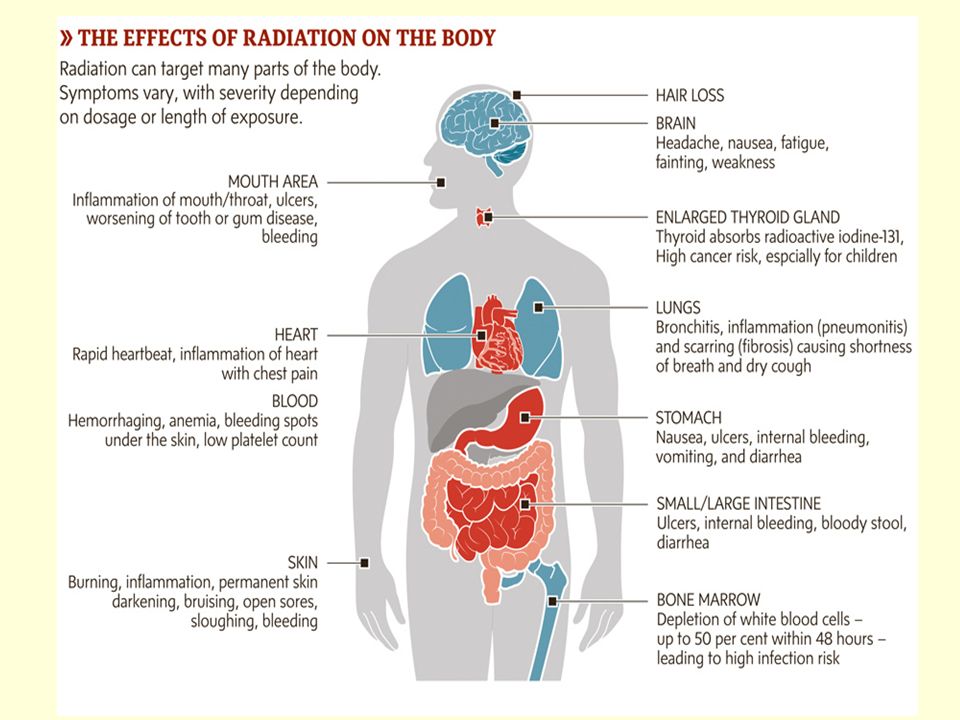 Growth restriction is possible, depending on dose. (Less likely than during the 6th to 13th weeks post conception) Probability of major malformations may increase | Miscarriage and neonatal death may occur, depending on dose. § |
| 8th to 25th Weeks Post Conception: The most vulnerable period for intellectual disability is 8th to 15th weeks post conception Severe intellectual disability is possible during this period at doses > 0.5 Gy Prevalence of intellectual disability (IQ<70) is 40% after an exposure of 1 Gy from 8th to 15th week Prevalence of intellectual disability (IQ<70) is 15% after an exposure of 1 Gy from 16th to 25th week Table adapted from Table 1.1. of the National Council on Radiation Protection and Measurements’ Report No. 174, “Preconception and Prenatal Radiation Exposure: Health Effects and Protective Guidance” [NCRP2013]. | |||||
Gestational age and radiation dose are important determinants of potential non-cancer health effects.
 The following points are of particular note.
The following points are of particular note.- During the first 2 weeks post-conception, the health effect of concern from an exposure of ≥ 0.1 Gy is the possibility of death of the embryo. Because the embryo is made up of only a few cells, damage to one cell, the progenitor of many other cells, may cause the death of the embryo, and the blastocyst may fail to implant in the uterus. Embryos that survive, however, are unlikely to exhibit congenital abnormalities or other non-cancer health effects, no matter what dose of radiation they received.
- In all stages post-conception, radiation-induced non-cancer health effects are not detectable for fetal doses below about 0.10 Gy.
Carcinogenic Effects of Prenatal Radiation Exposure
Radiation exposure to an embryo/fetus may increase the risk of cancer in the offspring, especially at radiation doses > 0.1 Gy, which are well above typical doses received in diagnostic radiology. However, attempting to quantify cancer risks from prenatal radiation exposure presents many challenges. These challenges include the following:
These challenges include the following:
- The primary data for the risk of developing cancer from prenatal exposure to radiation come from the lifespan study of the Japanese atomic bomb (A-bomb) survivors. [Preston et al. 2008]. The analysis of that cohort includes cancer incidence data only up to the age of 50 years. This precludes making lifespan risk estimates as a result of prenatal radiation exposure.
- From the Japanese lifespan study [Preston et al. 2008], it can be concluded that for those exposed
in early childhood (birth to age 5 years), the theoretical risk of an adult-onset cancer by age 50 is approximately ten-fold greater than the risk for those who received prenatal exposure. Therefore, the risk following prenatal exposure may be considerably lower than for radiation exposure in early childhood
[NCRP2013]. - No reliable epidemiological data are available from studies to determine which stage of pregnancy is the most sensitive for radiation-induced cancer in the offspring [NCRP2013].
The lifespan study of the Japanese A-bomb survivors is continuing as the cohort ages. Future analyses of the accumulating data should provide a better understanding of the lifetime risk of cancer from prenatal and early childhood radiation exposure.
References
ICRP2000] International Commission on Radiological Protection. 2000. Valentin, J. (2000). Pregnancy and medical radiation. Oxford: Published for the International Commission on Radiological Protection.
[NCRP2013] National Council on Radiation Protection and Measurements. 2013. Preconception and Prenatal Radiation Exposure Health Effects and Protective Guidance. (2013). Bethesda: National Council on Radiation Protection & Measurements.
Preston DL, Cullings H, Suyama A, Funamoto S, Nishi N, Soda M, Mabuchi K, Kodama K, Kasagi F, Shore RE. 2008. Solid cancer incidence in atomic bomb survivors exposed in utero or as young children. J Natl Cancer Inst 100(6):428-436.
[UNSCEAR2013] United Nations Scientific Committee on the Effects of Atomic Radiation.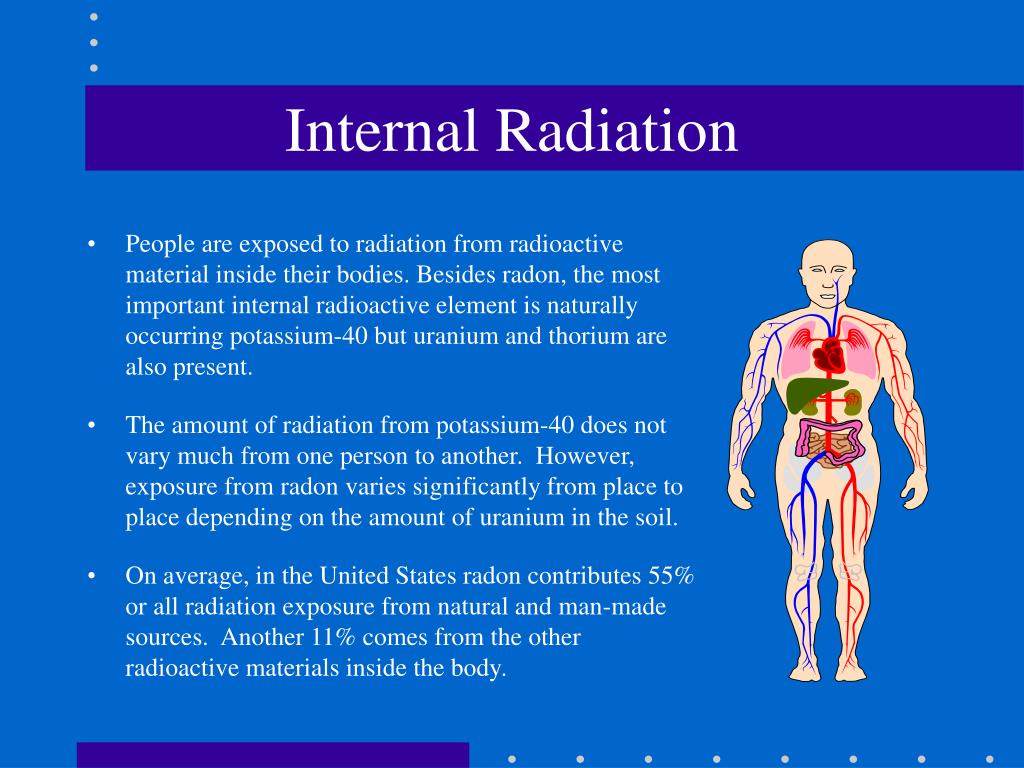 2013. Sources, effects and risks of ionizing radiation. Vol. II, Scientific Annex B: Effects of radiation exposure of children.
2013. Sources, effects and risks of ionizing radiation. Vol. II, Scientific Annex B: Effects of radiation exposure of children.
For more information on medical management and other topics on radiation emergencies:
Radiation Emergency Assistance Center/Training Siteexternal icon (REAC/TS) is a program uniquely qualified to teach medical personnel, health physicists, first responders and occupational health professionals about radiation emergency medical response.
Radiation Emergency Medical Management (REMM)external icon provides guidance to health care providers (primarily physicians) about clinical diagnosis and treatment of radiation injury during radiological and nuclear emergencies.
Conference of Radiation Control Program Directorsexternal icon
Health Physics Societyexternal icon
International Commission on Radiological Protectionexternal icon
National Council on Radiation Protection and Measurementsexternal icon
American Association of Physicists in Medicineexternal icon
Ionizing radiation, health effects and protective measures
Ionizing radiation, health effects and protective measures- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 O
- P
- R
- C
- T
- in
- Ф
- x
- C hours
- Sh
- K
- U
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find the country »
- A
- B
- B
- G
- D
- E
- and
- L
- N
- O
- P
- With
- T
- U
- F
- x
- Sh
- e
- i
- i
004 b
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Events
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Ionizing radiation, health effects and protective measures
\n
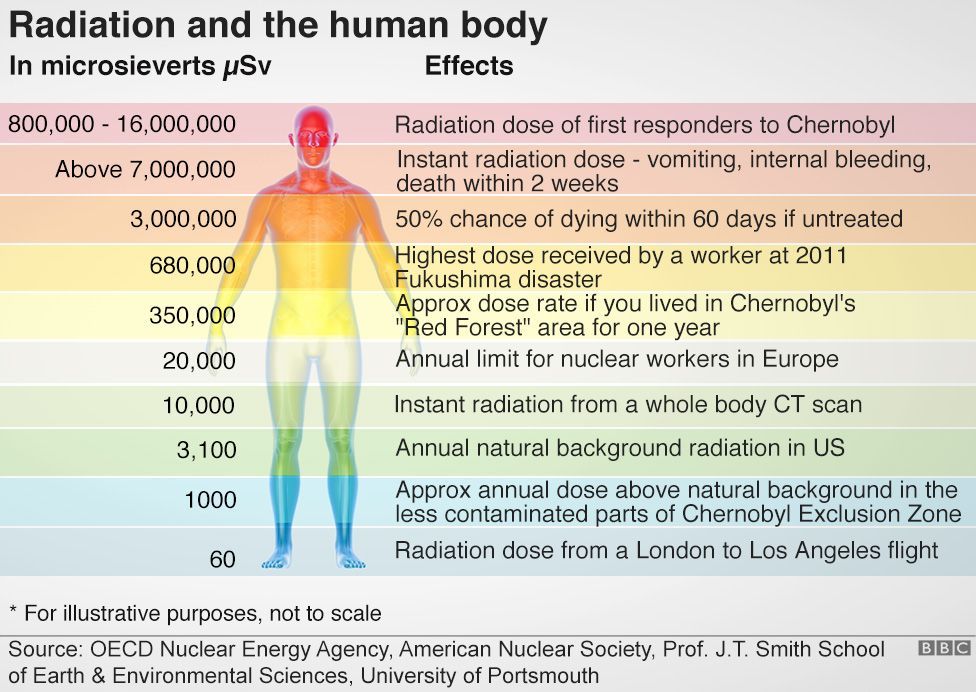
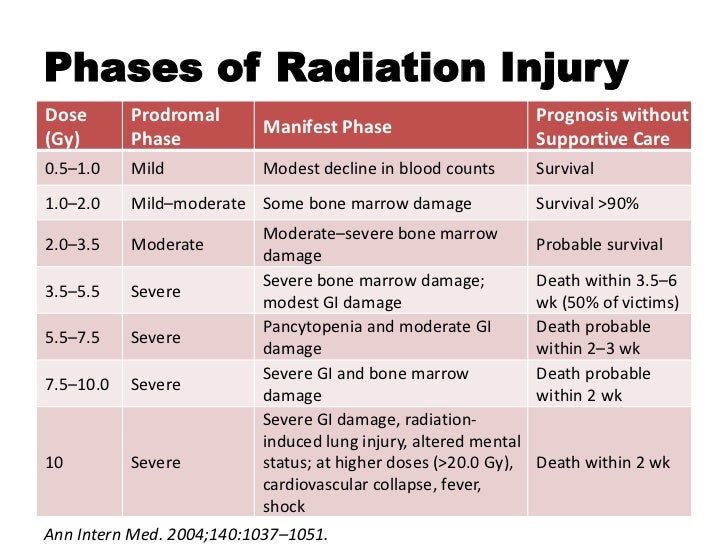
\nAbove certain thresholds, exposure to radiation may impair tissue and/or organ function and may cause acute reactions such as reddening of the skin, hair loss, radiation burns, or acute radiation syndrome. These reactions are stronger at higher doses and higher dose rates. For example, the threshold dose for acute radiation syndrome is approximately 1 Sv (1000 mSv).
These reactions are stronger at higher doses and higher dose rates. For example, the threshold dose for acute radiation syndrome is approximately 1 Sv (1000 mSv).
\n
\nIf the dose is low and/or for a long period of time (low dose rate), the risk associated with this is significantly reduced, since in this case the probability of repair of damaged tissues increases. However, there is a risk of long-term consequences, such as cancer that may take years or even decades to appear. Effects of this type do not always appear, but their probability is proportional to the radiation dose. This risk is higher in the case of children and adolescents, as they are much more sensitive to the effects of radiation than adults.
\n
\nEpidemiological studies in exposed populations, such as atomic bomb survivors or radiotherapy patients, have shown a significant increase in the likelihood of cancer at doses above 100 mSv. In some cases, more recent epidemiological studies in humans exposed as children for medical purposes (Childhood CT) suggest that the likelihood of cancer may be increased even at lower doses (in the range of 50-100 mSv) .
In some cases, more recent epidemiological studies in humans exposed as children for medical purposes (Childhood CT) suggest that the likelihood of cancer may be increased even at lower doses (in the range of 50-100 mSv) .
\n
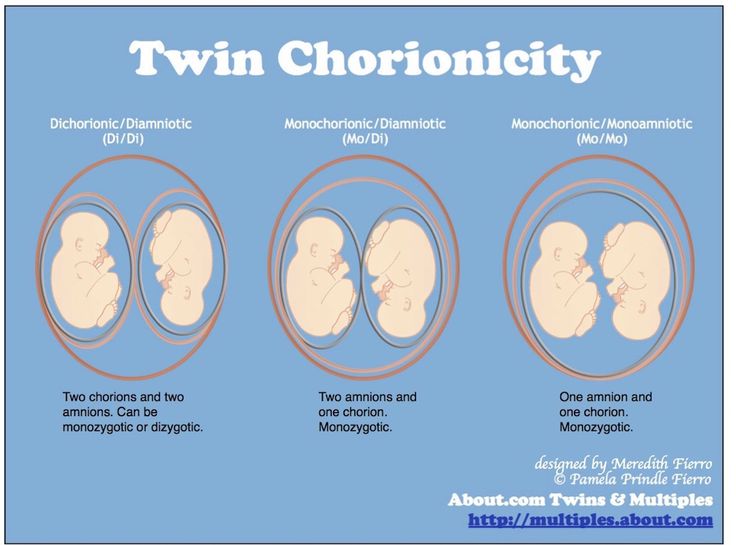
\nPrenatal exposure to ionizing radiation can cause fetal brain damage at high doses in excess of 100 mSv between 8 and 15 weeks of gestation and 200 mSv between 16 and 25 weeks of gestation. Human studies have shown that there is no radiation-related risk to fetal brain development before 8 weeks or after 25 weeks of gestation. Epidemiological studies suggest that the risk of developing fetal cancer after exposure to radiation is similar to the risk after exposure to radiation in early childhood.
\n
WHO activities
\n
\nWHO has developed a radiation program to protect patients, workers and the public from the health risks of radiation exposure in planned, existing and emergency exposures. This program, which focuses on public health aspects, covers activities related to exposure risk assessment, management and communication.
This program, which focuses on public health aspects, covers activities related to exposure risk assessment, management and communication.
\n
\nIn line with its core function of \"setting, promoting and monitoring norms and standards\", WHO collaborates with 7 other international organizations to revise and update international standards for basic safety related to radiation (SBB). WHO adopted new international PRSs in 2012 and is currently working to support the implementation of PRSs in its Member States.
\n
","datePublished":"2016-04-29T09:30:00.0000000+00:00","image":"https://cdn.who.int/media/images/default -source/imported/radiation/radiation-africa630x420-jpg.jpg?sfvrsn=e8581c1b_10","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo": {"@type":"ImageObject","url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo. jpg","width":250,"height":60}},"dateModified ":"2016-04-29T09:30:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/ionizing-radiation-health -effects-and-protective-measures","@context":"http://schema.org","@type":"Article"};
jpg","width":250,"height":60}},"dateModified ":"2016-04-29T09:30:00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/ionizing-radiation-health -effects-and-protective-measures","@context":"http://schema.org","@type":"Article"};
Key Facts
- Ionizing radiation is a form of energy released by atoms in the form of electromagnetic waves or particles.
- People are exposed to natural sources of ionizing radiation such as soil, water, plants, and man-made sources such as X-rays and medical devices.
- Ionizing radiation has numerous useful applications, including medicine, industry, agriculture, and scientific research.
- As the use of ionizing radiation increases, so does the potential for health hazards if it is used or restricted inappropriately.
- Acute health effects such as skin burn or acute radiation syndrome may occur when the radiation dose exceeds certain levels.
- Low doses of ionizing radiation may increase the risk of longer term effects such as cancer.
What is ionizing radiation?
Ionizing radiation is a form of energy released by atoms in the form of electromagnetic waves (gamma or x-rays) or particles (neutrons, beta or alpha). The spontaneous decay of atoms is called radioactivity, and the excess energy that results from this is a form of ionizing radiation. Unstable elements formed during decay and emitting ionizing radiation are called radionuclides.
All radionuclides are uniquely identified by the type of radiation they emit, the energy of the radiation, and their half-life.
Activity, used as a measure of the amount of radionuclide present, is expressed in units called becquerels (Bq): one becquerel is one decay per second. The half-life is the time required for the activity of a radionuclide to decay to half its original value. The half-life of a radioactive element is the time it takes for half of its atoms to decay. It can range from fractions of a second to millions of years (for example, the half-life of iodine-131 is 8 days, and the half-life of carbon-14 is 5730 years).
Radiation sources
People are exposed to natural and artificial radiation every day. Natural radiation comes from numerous sources, including over 60 naturally occurring radioactive substances in soil, water and air. Radon, a naturally occurring gas, is formed from rocks and soil and is the main source of natural radiation. Every day people inhale and absorb radionuclides from air, food and water.
Humans are also exposed to natural radiation from cosmic rays, especially at high altitudes. On average, 80% of the annual dose that a person receives from background radiation is from naturally occurring terrestrial and space sources of radiation. The levels of such radiation vary in different rheographic zones, and in some areas the level can be 200 times higher than the global average.
Humans are also exposed to radiation from man-made sources, from nuclear power generation to the medical use of radiation diagnosis or treatment. Today, the most common artificial sources of ionizing radiation are medical devices, such as x-ray machines, and other medical devices.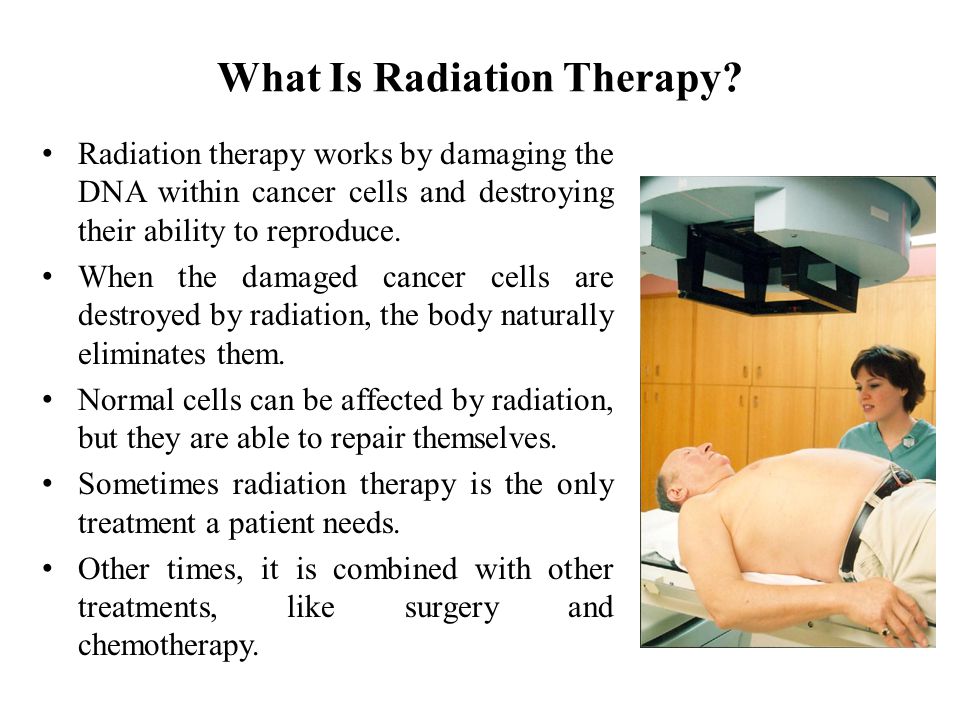
Exposure to ionizing radiation
Exposure to radiation can be internal or external and can occur in a variety of ways.
Internal exposure to ionizing radiation occurs when radionuclides are inhaled, ingested, or otherwise enter the circulation (eg, injection, injury). Internal exposure stops when the radionuclide is excreted from the body, either spontaneously (with feces) or as a result of treatment.
External contamination can occur when radioactive material in the air (dust, liquid, aerosols) is deposited on skin or clothing. Such radioactive material can often be removed from the body by simple washing.
Exposure to ionizing radiation may also occur as a result of external radiation from a suitable external source (eg, such as exposure to radiation emitted by medical x-ray equipment). External exposure stops when the radiation source is closed, or when a person goes outside the radiation field.
People can be exposed to ionizing radiation in a variety of settings: at home or in public places (public exposure), in their workplace (occupational exposure), or in health care settings (patients, caregivers and volunteers).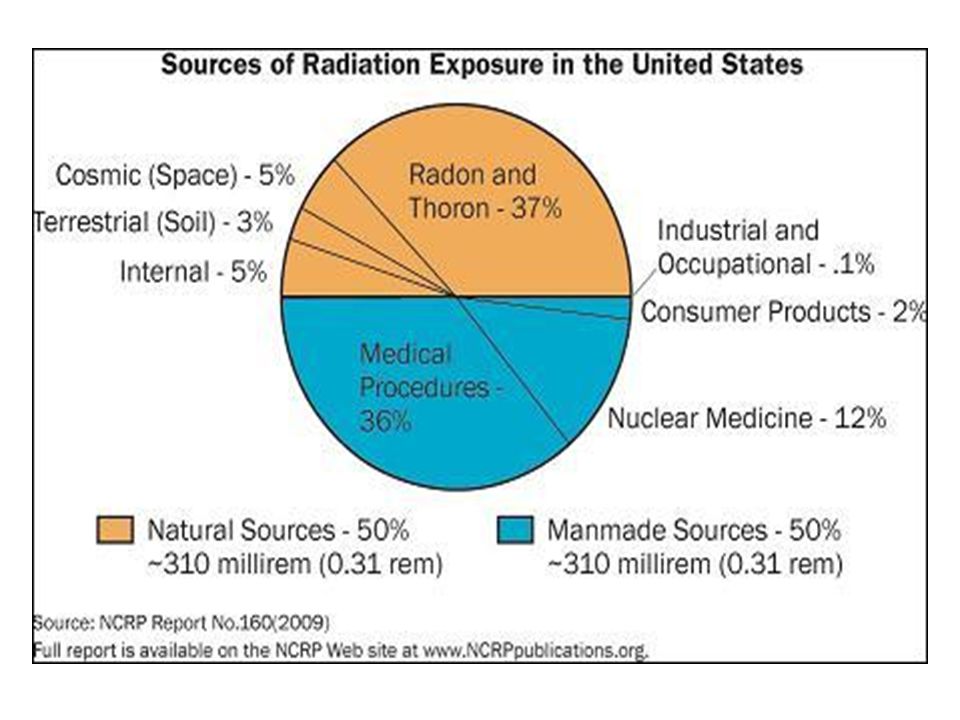
Exposure to ionizing radiation can be classified into three types of exposure.
The first case is planned exposure, which is due to the intentional use and operation of radiation sources for specific purposes, for example, in the case of the medical use of radiation for the diagnosis or treatment of patients, or the use of radiation in industry or for scientific research purposes.
The second case is existing sources of exposure where radiation exposure already exists and for which appropriate control measures need to be taken, such as exposure to radon in homes or workplaces, or exposure to natural background radiation in environmental conditions.
The last case is exposure to emergencies caused by unexpected events requiring prompt action, such as nuclear incidents or malicious acts.
Medical uses of radiation account for 98% of total radiation dose from all artificial sources; it accounts for 20% of the total impact on the population. There are 3,600 million diagnostic radiological examinations, 37 million nuclear procedures and 7.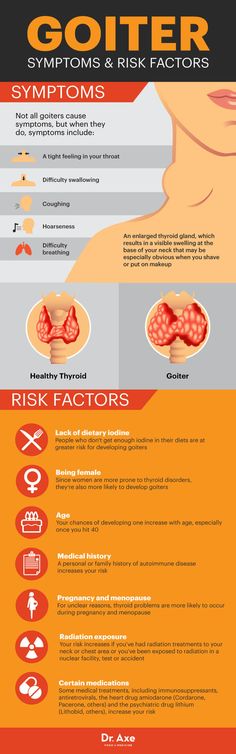 5 million therapeutic radiotherapy procedures worldwide each year.
5 million therapeutic radiotherapy procedures worldwide each year.
Health effects of ionizing radiation
Radiation damage to tissues and/or organs depends on the received radiation dose or absorbed dose, which is expressed in grays (Gy).
Effective dose is used to measure ionizing radiation in terms of its potential to cause harm. Sievert (Sv) is a unit of effective dose, which takes into account the type of radiation and the sensitivity of tissues and organs. It makes it possible to measure ionizing radiation in terms of the potential for harm. Sv takes into account the type of radiation and the sensitivity of organs and tissues.
Sv is a very large unit, so it is more practical to use smaller units such as millisievert (mSv) or microsievert (µSv). One mSv contains 1000 µSv, and 1000 mSv equals 1 Sv. In addition to the amount of radiation (dose), it is often useful to show the release rate of that dose, such as µSv/hour or mSv/year.
Above certain thresholds, exposure may impair tissue and/or organ function and may cause acute reactions such as reddening of the skin, hair loss, radiation burns, or acute radiation syndrome. These reactions are stronger at higher doses and higher dose rates. For example, the threshold dose for acute radiation syndrome is approximately 1 Sv (1000 mSv).
These reactions are stronger at higher doses and higher dose rates. For example, the threshold dose for acute radiation syndrome is approximately 1 Sv (1000 mSv).
If the dose is low and/or a long period of time is applied (low dose rate), the resulting risk is significantly reduced, since in this case the likelihood of repair of damaged tissues increases. However, there is a risk of long-term consequences, such as cancer that may take years or even decades to appear. Effects of this type do not always appear, but their probability is proportional to the radiation dose. This risk is higher in the case of children and adolescents, as they are much more sensitive to the effects of radiation than adults.
Epidemiological studies in exposed populations, such as atomic bomb survivors or radiotherapy patients, have shown a significant increase in the likelihood of cancer at doses above 100 mSv. In some cases, more recent epidemiological studies in humans exposed as children for medical purposes (Childhood CT) suggest that the likelihood of cancer may be increased even at lower doses (in the range of 50-100 mSv) .
Prenatal exposure to ionizing radiation can cause fetal brain damage at high doses in excess of 100 mSv between 8 and 15 weeks of gestation and 200 mSv between 16 and 25 weeks of gestation. Human studies have shown that there is no radiation-related risk to fetal brain development before 8 weeks or after 25 weeks of gestation. Epidemiological studies suggest that the risk of developing fetal cancer after exposure to radiation is similar to the risk after exposure to radiation in early childhood.
WHO activities
WHO has developed a radiation program to protect patients, workers, and the public from the health hazards of radiation in planned, existing, and emergency exposures. This program, which focuses on public health aspects, covers activities related to exposure risk assessment, management and communication.
Under its core function of "setting, promoting and monitoring norms and standards", WHO is collaborating with 7 other international organizations to revise and update international standards for basic radiation safety (BRS).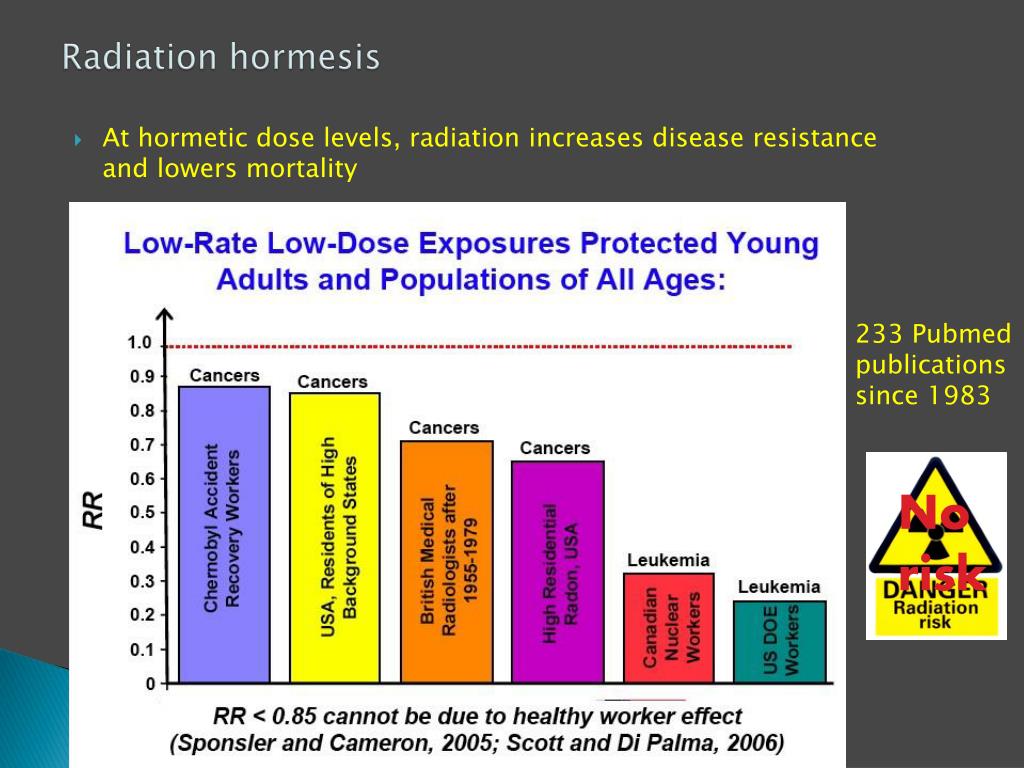 WHO adopted new international PRSs in 2012 and is currently working to support the implementation of PRSs in its Member States.
WHO adopted new international PRSs in 2012 and is currently working to support the implementation of PRSs in its Member States.
- Consequences of the Chernobyl accident for health
X-ray computed tomography during pregnancy (yes vs. no)
[read] (or download)
article in PDF format
Computed tomography (hereinafter referred to as CT) is a study of human internal organs using x-rays (the full name of CT is X-ray computed tomography [RCT]). The patient's body is exposed at different angles with small doses of X-rays using a CT-tomograph beam tube, the result of which is recorded by special ultra-sensitive detectors, obtaining many layer-by-layer images of the body area under study (as a result of complex computer processing of the difference in X-ray attenuation by tissues of different density).
Historical and technical information .
 Computed tomography (CT) has been used in clinical practice since 1974. It is customary to distinguish two main technologies for CT examination: step-by-step and spiral. Step-by-step technology involves stopping the x-ray tube after each rotation, during which the table with the patient moves to the next position (i.e. "step by step, one turn per layer") through the gantry window [ring] (gantry - English, bed) , which houses the X-ray tube and detectors. This technology is the main and the only one on devices manufactured before the middle of 90s of XX century. The first tomographs of that time had only one X-ray tube, which was directed at one detector (the first generation of tomographs). One rotation made it possible to obtain an image of one layer. The processing time of the image of one layer took ~ 4 - 5 minutes, and the processing of the obtained data and the reconstruction of the image on a special computer took 2.5 hours.
Computed tomography (CT) has been used in clinical practice since 1974. It is customary to distinguish two main technologies for CT examination: step-by-step and spiral. Step-by-step technology involves stopping the x-ray tube after each rotation, during which the table with the patient moves to the next position (i.e. "step by step, one turn per layer") through the gantry window [ring] (gantry - English, bed) , which houses the X-ray tube and detectors. This technology is the main and the only one on devices manufactured before the middle of 90s of XX century. The first tomographs of that time had only one X-ray tube, which was directed at one detector (the first generation of tomographs). One rotation made it possible to obtain an image of one layer. The processing time of the image of one layer took ~ 4 - 5 minutes, and the processing of the obtained data and the reconstruction of the image on a special computer took 2.5 hours.
However, in the second generation of tomographs of that time, several detectors were installed in front of the X-ray tube, working simultaneously, and the tube emitted not a sharply directed beam, but a fan beam (fan type of construction).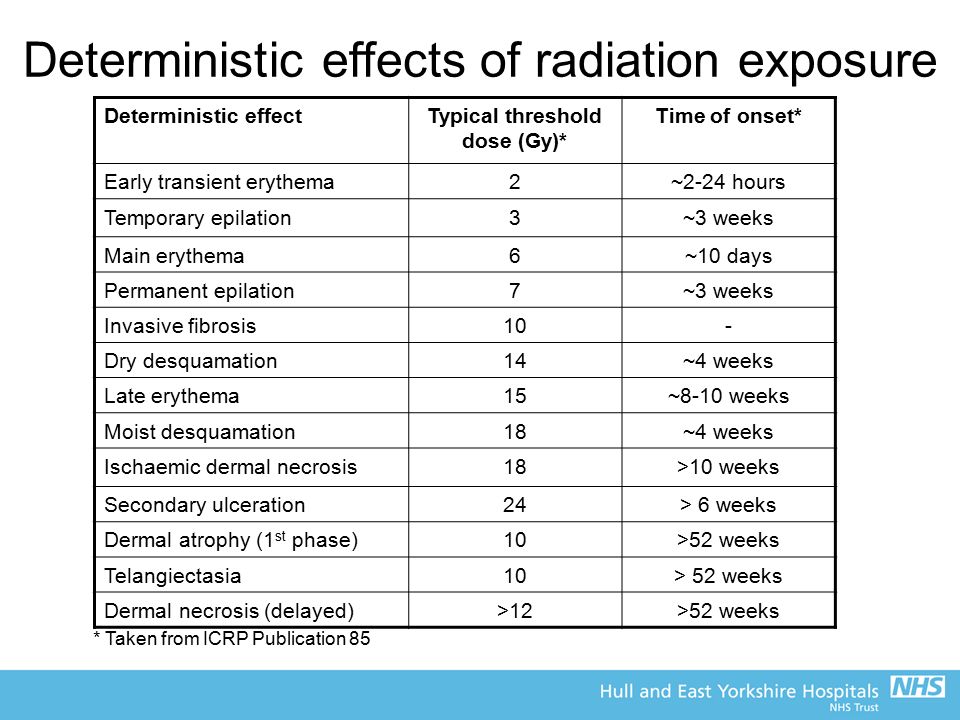 The total measurement time required to obtain one image was significantly reduced and amounted to ~ 20 seconds.
The total measurement time required to obtain one image was significantly reduced and amounted to ~ 20 seconds.
The third generation of scanners introduced the term helical computed tomography (SCT). The principle of operation of the device is based on the simultaneous rotation of the X-ray tube, which generates radiation (directed to a plurality of detectors - about 700 - located in an arc), and the continuous movement of the table on which the patient lies around the longitudinal scanning axis (the tube and detectors in one step of the table synchronously performed full clockwise rotation). With this combination, the trajectory of the movement of the tube relative to the direction of movement of the table takes the form of a spiral. This technology made it possible to reduce the examination time (up to ~ 10 seconds, and in modern tomographs up to 0.75 - 3.0 seconds) and reduce the radiation load on the patient's body.
The fourth generation scanners have a solid fixed ring (not an arc!) of detectors (1088 luminescent sensors) and an X-ray tube emitting a fan beam of rays, rotating around the patient inside the ring. The scan time for each projection has been reduced to ~0.7 seconds and the image quality has improved.
The scan time for each projection has been reduced to ~0.7 seconds and the image quality has improved.
The essence of the fifth generation of [spiral] tomographs (= electron beam tomographs) is the use of several rows of detectors instead of one - multilayer ("multispiral", "multi-slice" [or "volumetric"]) computed tomography (MSCT). That is, the fundamental difference between MSCT and SCT of previous generations is that along the gantry circumference there are not one, but two or more (see below) parallel rows of detectors (giving a similar number of slices). In order for X-ray radiation to be simultaneously received by detectors located on different rows, a new one was developed - a three-dimensional geometric shape of the beam, through the use of a compact linear accelerator (which performs the function of an X-ray tube). In it (the accelerator) the electrons are accelerated, and the electron beam is formed and spatially oriented. The speed of rotation of the electron beam and hence the x-ray beam around the patient is thousandths of a second.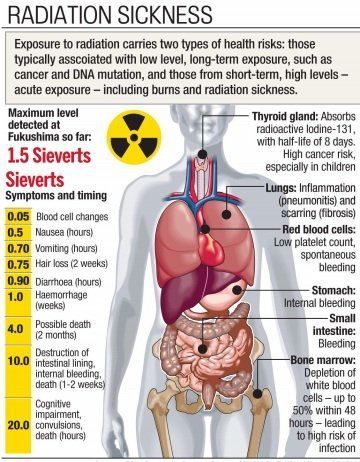 This allows you to get up to 10 - 20 images per second and observe the CT picture in real time. With the successive appearance of 4, 16, 64, 128, 320, 512- and 640-slice tomography, previously unattainable diagnostic horizons opened up, fundamentally changing diagnostic approaches to many diseases. MSCT allows not only to obtain images, but also makes it possible to observe the physiological processes occurring in the brain and heart in almost “real” time; MSCT angiography, perfusion MSCT, virtual colonoscopy, 3D reconstruction (3D models of all organs and body systems) also appeared. The modern generation of tomographs actually marked the transition from multispiral to volumetric (volumetric) tomography.
This allows you to get up to 10 - 20 images per second and observe the CT picture in real time. With the successive appearance of 4, 16, 64, 128, 320, 512- and 640-slice tomography, previously unattainable diagnostic horizons opened up, fundamentally changing diagnostic approaches to many diseases. MSCT allows not only to obtain images, but also makes it possible to observe the physiological processes occurring in the brain and heart in almost “real” time; MSCT angiography, perfusion MSCT, virtual colonoscopy, 3D reconstruction (3D models of all organs and body systems) also appeared. The modern generation of tomographs actually marked the transition from multispiral to volumetric (volumetric) tomography.
Information [ reference ], which you will need when reading (assimilating) the information in this post: is the amount of radiation absorbed by a substance). 1 Rad is equal to the absorbed radiation dose at which 100 erg of ionizing radiation energy is transferred to an irradiated substance weighing 1 gram: 1 Rad = 100 erg/g = 0.
 01 J/kg = 0.01 Gy (see below).
01 J/kg = 0.01 Gy (see below). The SI system for measuring absorbed dose is Gray (Gy, Gy). 1 Gray is the amount of energy of radioactive radiation in 1 J, which is absorbed by a substance weighing 1 kg, regardless of the type of radioactive radiation and its energy. 1 Gray (Gy) = 1J/kg = 100 rad radioactive radiation). In the SI system for measuring the equivalent dose, the Sievert (Sv, Sv) is used. At K=1 (for x-ray, gamma, beta radiation, electrons and positrons) 1 Sv corresponds to an absorbed dose of 1 Gy: 1 Sv = 1 Gy = 100 rad (i.e. for x-ray, gamma, beta radiation, electrons and positrons, the values rad, Gy, and Sv turn out to be equivalent in assessing human exposure).
From the European Society of Cardiology guidelines for the management of cardiovascular disease during pregnancy (2011), p. 7:
“Radiation exposure. The effect of radiation on the fetus depends on the dose of radiation and the gestational age at which the exposure occurs. If possible, procedures should be delayed until at least the completion of the period of primary organogenesis (>12 weeks post-menses). There is no evidence of an increased risk of congenital malformations, mental retardation, fetal growth restriction or termination of pregnancy at a dose to a pregnant woman <50 mGy. There may be a slight increase in risk (1:2000 vs 1:3000) of cancer in children. The threshold for increased risk of congenital malformations has not been definitively elucidated. Some evidence suggests that the risk of malformations is increased at doses >100 mGy, while the risk is clearly less between 50 and 100 mGy. During the first 14 days after conception, fetal survival or death is most likely the result of >50 mGy exposure. After the first 14 days, radiation exposure >50 mGy may be associated with an increased risk of congenital malformations, growth restriction, and mental retardation. Most medical procedures do not expose the fetus to such high levels of radiation (Table 3). For most diagnostic medical procedures involving fetal exposure up to ~1 mGy, the risk of childhood cancer is very low. As a rule of thumb, in accordance with the As Low As Possible (ALARA) principle, all radiation exposure doses from medical procedures should be as low as possible [read source].
There is no evidence of an increased risk of congenital malformations, mental retardation, fetal growth restriction or termination of pregnancy at a dose to a pregnant woman <50 mGy. There may be a slight increase in risk (1:2000 vs 1:3000) of cancer in children. The threshold for increased risk of congenital malformations has not been definitively elucidated. Some evidence suggests that the risk of malformations is increased at doses >100 mGy, while the risk is clearly less between 50 and 100 mGy. During the first 14 days after conception, fetal survival or death is most likely the result of >50 mGy exposure. After the first 14 days, radiation exposure >50 mGy may be associated with an increased risk of congenital malformations, growth restriction, and mental retardation. Most medical procedures do not expose the fetus to such high levels of radiation (Table 3). For most diagnostic medical procedures involving fetal exposure up to ~1 mGy, the risk of childhood cancer is very low. As a rule of thumb, in accordance with the As Low As Possible (ALARA) principle, all radiation exposure doses from medical procedures should be as low as possible [read source].
From article : "Obstetric aspects of acute cerebrovascular disorders during pregnancy, childbirth and the postpartum period (literature review)" R.R. Harutamyan, E.M. Shifman, E.S. Lyashko, E.E. Tyulkina, O.V. Konysheva, N.O. Tarbaya, S.E. Flock; Department of Reproductive Medicine and Surgery, FPDO, Moscow State University of Medicine and Dentistry. A.I. Evdokimova; City Clinical Hospital №15 named after O.M. Filatov; Department of Anesthesiology and Resuscitation, FPC MR, Peoples' Friendship University of Russia, Moscow (Reproduction Problems magazine No. 2, 2013), pp. 83 - 84):
“Examinations such as computed tomography of the head involve the use of ionizing radiation and raise some safety concerns for the fetus. Ionizing radiation can cause fetal death, birth defects, growth retardation, mental retardation and malignant tumors. The risk is determined on the basis of the absorbed dose, it is measured in rads or grays, Gy (100 rads = 1 Gy).
The risk is estimated and calculated from observations of high-dose victims of the Hiroshima and Nagasaki bombings using linear extrapolation to lower doses. The maximum fetal absorbed dose is 0.5 mrad (0.005 mGy/mSv) for head CT, SCT (spiral CT), 10 mrad (0.1 mGy/mSv) for cerebral angiography, and 1.0 mrad (0.01 mGy/mSv). mSv) on chest x-ray. It should be noted that the absorbed dose of natural radiation is about 300 mrad per year. The additional chance of cancer by age 15 is 1 in 17,000 for every 100 mrad (1 mGy/mSv) of dose absorbed by the fetus. The estimated risk of an increase in the likelihood of cancer in a CT scan of the mother's head in a child is 0.07%. Since about 1 in 4 people develop some form of cancer during their lifetime, these risks are considered extremely low. Until about 10 weeks of gestation, the threshold for detecting an additional risk of congenital fetal anomalies is 5000 mrad (0.05 Gy or 0.00005 mGy). It should be noted that there is no evidence that performing diagnostic tests on a pregnant woman can cause malignant tumors or congenital anomalies in the fetus.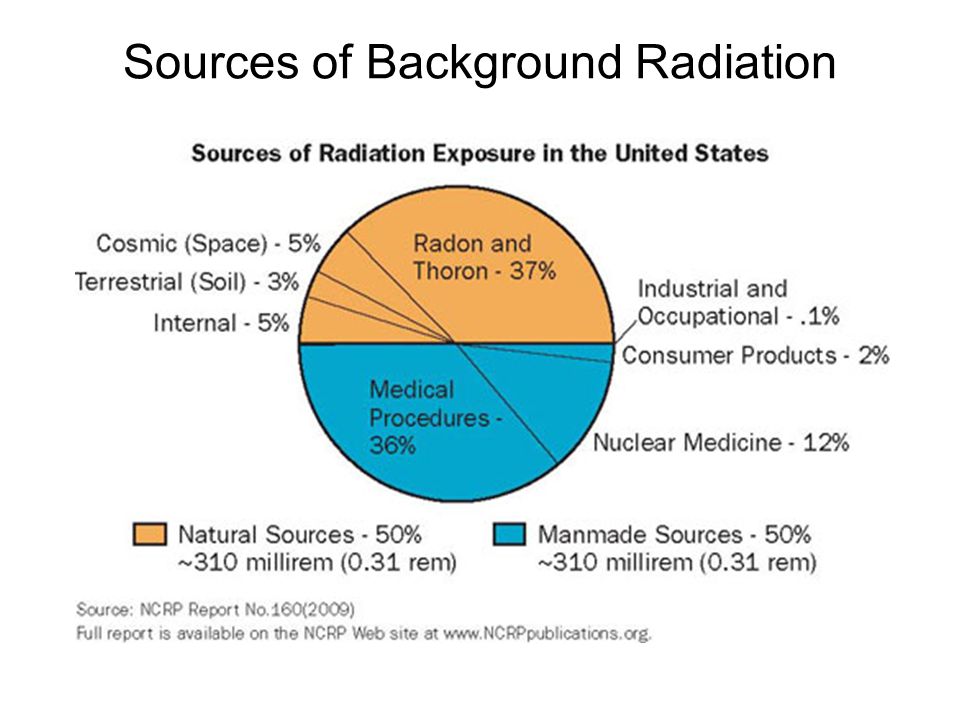 An analysis of the available data suggests that if the radiation dose is less than 5000 mrad, then there are no additional risks to the fetus compared to those women who receive a natural dose of radiation” [read source].
An analysis of the available data suggests that if the radiation dose is less than 5000 mrad, then there are no additional risks to the fetus compared to those women who receive a natural dose of radiation” [read source].
From the ESC guidelines for the diagnosis and management of patients with acute pulmonary embolism (working group on the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology [ESC], 2014) [Russian Journal of Cardiology No. 8 (124), 2015, pp. 105 - 106]:
"The radiation dose received by the fetus during various diagnostic tests is shown in Table 14. The hazard threshold for the fetus is considered to be 50 mGy/mSv (50,000 µGy/µSv)), and all radiological methods must fit into this value. However, scintigraphy, when available, may be preferred over CT as it does not expose the breasts as in CT angiography, which slightly but significantly reduces the lifetime risk of breast cancer. Generally, a ventilation scan is not needed because the chest x-ray is normal to reduce radiation exposure.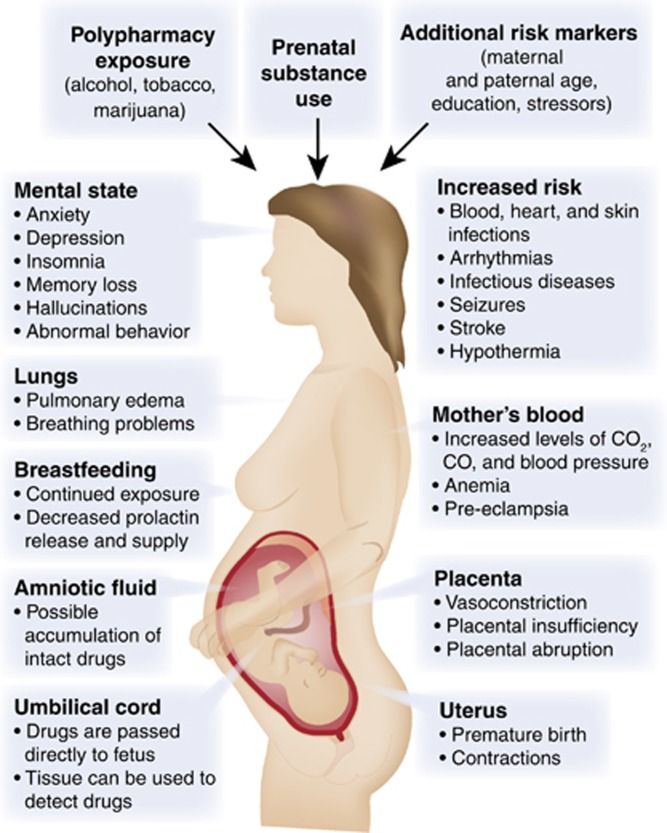 The diagnostic value of scintigraphy is approximately 80%, with 70% of tests showing normal results and 5 - 10% with data giving a high probability. This is at least as high as for CT in relation to this special situation, due to the generally higher proportion of questionable CT findings during pregnancy. Normal perfusion scanning and negative CT are equally safe for ruling out pulmonary embolism during pregnancy, as shown in a number of retrospective studies. Classical pulmonary angiography gives a significantly higher fetal exposure (2.2-3.7 mGy/mSv) and should not be used in pregnancy” [read].
The diagnostic value of scintigraphy is approximately 80%, with 70% of tests showing normal results and 5 - 10% with data giving a high probability. This is at least as high as for CT in relation to this special situation, due to the generally higher proportion of questionable CT findings during pregnancy. Normal perfusion scanning and negative CT are equally safe for ruling out pulmonary embolism during pregnancy, as shown in a number of retrospective studies. Classical pulmonary angiography gives a significantly higher fetal exposure (2.2-3.7 mGy/mSv) and should not be used in pregnancy” [read].
From the book "Computed tomography in emergency medicine" electronic edition edited by S. Mirsadre, K. Mankad, E. Chalmers; Translation from the English edition of Cand. honey. Sciences O. V. Uskova, Ph.D. honey. Sciences, Associate Professor O. A. Ettinger; Moscow, BINOM, Knowledge Lab, 2012; See section on CT in Pregnant Patients (p. 23):
“It is recommended to avoid exposure to ionizing radiation in a pregnant patient as much as possible, especially during the first trimester of pregnancy. However, studies regarding the assessment of safe fetal radiation doses tend to conclude that the risk of adverse fetal exposure to radiation is minimal, and the potential benefit of the diagnostic information obtained from the study should not limit the use of a diagnostic technique for examining a pregnant patient. The need to minimize the received dose of radiation during CT examination in pregnant women remains essential in the choice of protocol.
However, studies regarding the assessment of safe fetal radiation doses tend to conclude that the risk of adverse fetal exposure to radiation is minimal, and the potential benefit of the diagnostic information obtained from the study should not limit the use of a diagnostic technique for examining a pregnant patient. The need to minimize the received dose of radiation during CT examination in pregnant women remains essential in the choice of protocol.
IV contrast should be avoided whenever possible during pregnancy unless it is a condition for diagnosis. If necessary, it is safe to use non-ionized contrast, in respect of which no harmful effects on the fetal thyroid gland have been described ”[read source].
From clinical guidelines (treatment protocol) “Hypertensive disorders during pregnancy, childbirth and the postpartum period. Preeclampsia. Eclampsia” Ministry of Health of the Russian Federation, letter dated June 7, 2016 N 15-4/10/2-3483:
“Indications for computed tomography or magnetic resonance imaging of the brain:
[ 1 ] a seizure occurring earlier than the 20th week of pregnancy or in the first two days after childbirth;
[ 2 ] eclampsia resistant to magnesium sulfate therapy in the presence of severe focal neurological symptoms;
[ 3 ] hemiparesis;
[ 4 ] coma persisting after cessation of sedation for 24 hours” [read source].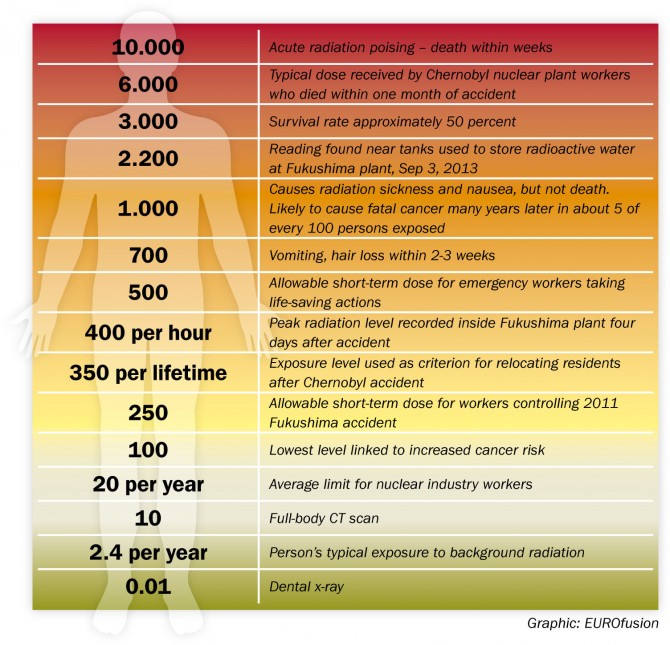
From the article "Diagnostics of acute cerebrovascular accidents in pregnant women, puerperas and women in childbirth" Yu.D. Vasiliev, L.V. Sidelnikova, R.R. Arustamyan; City Clinical Hospital №15 named after O.M. Filatov, Moscow; 2 SBEE HPE "Moscow State University of Medicine and Dentistry named after A.I. A.I. Evdokimov” of the Ministry of Health of Russia, Moscow (Reproduction Problems magazine No. 4, 2016):
“Computed tomography, angiography (CT and CT-AG) are performed [for pregnant women] if there are contraindications for the use of MRI. When performing multislice computed tomography (MSCT), a narrowly collimated x-ray beam, a few millimeters wide, is used, which minimizes the impact on adjacent body tissues, unlike conventional x-ray tubes. The received dose does not exceed 2.0 mSv. Indications for MSCT of pregnant women: [ 1 ] traumatic brain injury; [ 2 ] ONMK. In case of intra- and extracranial vascular pathology (aneurysms, arteriovenous malformations, stenoses), MSCT is a screening study (study time is 2-3 minutes)” [read source].
From SanPiN (a) 2.6.1.1192-03 “Hygienic requirements for the design and operation of X-ray rooms, apparatus and X-ray examinations” (p. 20 - 21):
“7.16. The appointment of pregnant women for X-ray examination is carried out only according to clinical indications. Studies should, if possible, be carried out in the second half of pregnancy, except in cases where the issue of termination of pregnancy or the need for emergency or emergency care must be decided. If pregnancy is suspected, the question of the admissibility and necessity of an x-ray examination is decided on the basis of the assumption that there is a pregnancy.
7.17. Pregnant women are not allowed to participate in x-ray studies (support for a child or a seriously ill relative).
7.18. X-ray examinations of pregnant women are carried out using all possible means and methods of protection so that the dose received by the fetus does not exceed 1 mGy / mSv for two months of undiagnosed pregnancy.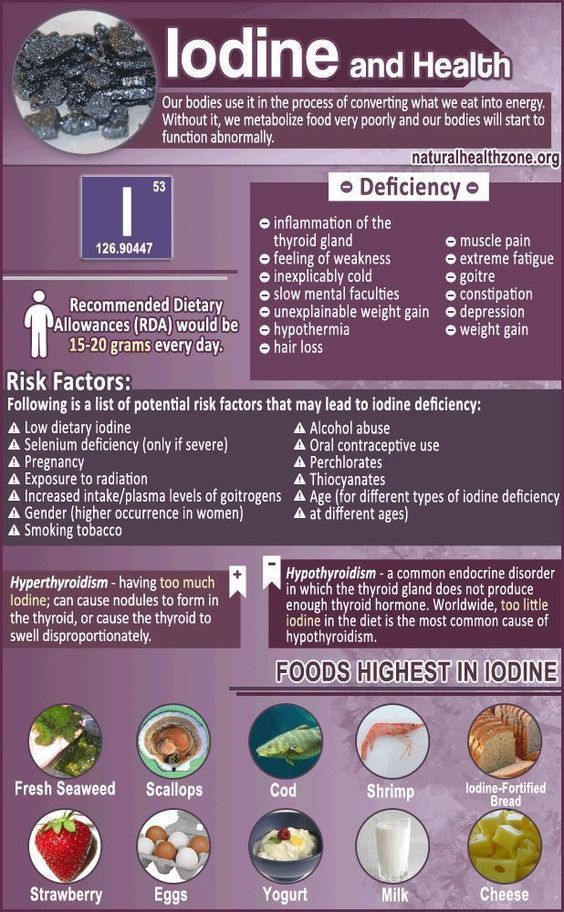 If the fetus receives a dose exceeding 100 mGy/mSv, the doctor must warn the patient about the possible consequences and recommend terminating the pregnancy” [read source].
If the fetus receives a dose exceeding 100 mGy/mSv, the doctor must warn the patient about the possible consequences and recommend terminating the pregnancy” [read source].
From verified source (kakras.ru website): “According to UN estimates, the average annual doses received by people around the world from natural background radiation are 2.4 mSv / year, and the typical range of these doses is 1 - 10 mSv/year. Thus, the accumulated doses from natural radiation, during a lifetime, can be about 100 - 700 mSv (on different continents and in different regions of the planet - their values). Human exposure doses can be considered low if they are comparable to levels of natural background radiation, typically a few mSv per year.
According to the norms of the Federal Law "On radiation safety of the population" Article 9. p.2, the effective dose for a person, in total, for the period of his life (taken in calculations equal to 70 years) - should not exceed 70 mSv, which will not affect on health and is considered a safe level of absorbed radiation” [read the source on the website kakras.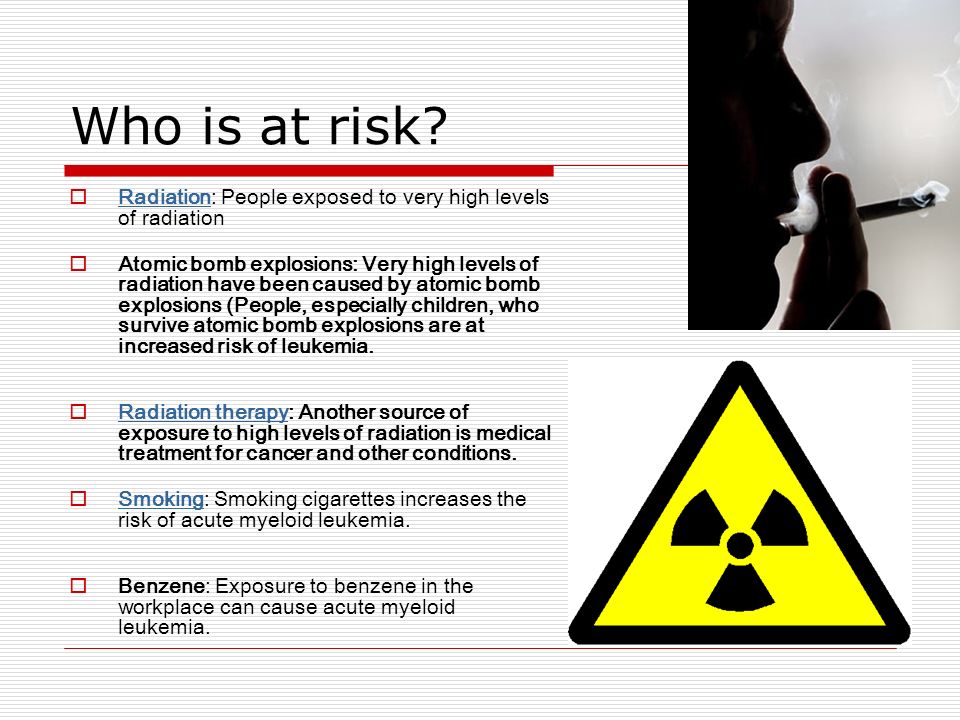 ru].
ru].
From article "Modern approaches to the diagnosis of pulmonary embolism" I.V. Bagrova, G.A. Kukharchik, V.I. Serebryakova, I.V. Konstantinova, M.Yu. Kaputin; SBEE HPE "North-Western State Medical University named after I.I. Mechnikov” of the Ministry of Health and Social Development of the Russian Federation; GBU "St. Petersburg Research Institute of Emergency Medicine named after A.I. I.I. Dzhanelidze", St. Petersburg (magazine "Phlebology" No. 4, 2012):
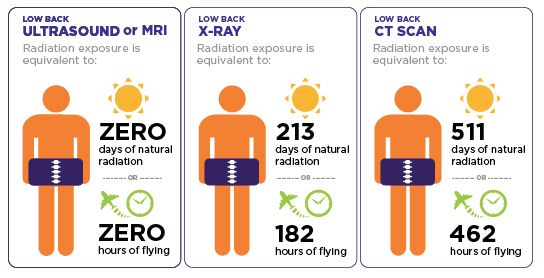
“The radiation exposure during CT scan of the chest is 2-6 mSv. For comparison, according to M. Hofer (2008), the annual total radiation dose received by a resident of Germany is 4.2 mSv, while the average annual level of exposure from natural sources is about 2.4 mSv, and associated with human activity - 1, 8 mSv. When discussing the potential dangers of CTs associated with exposure to ionizing radiation, the example of air travel is often used - during a transatlantic flight, an aircraft passenger receives an additional dose of radiation due to cosmic radiation.