Can identical twins have their own placenta
Fraternal twins & identical twins
About twins
We usually describe twins according to:
- how many eggs they develop from – 1 or 2
- whether they share a placenta in their mother’s womb.
The main types of twins are fraternal twins and identical twins.
Most twins are born healthy, but a twin pregnancy can mean a higher chance of health complications for you and your babies. If you're pregnant with twins, you and your babies will need extra check-ups.
Fraternal twins
All pregnancies start when a sperm fertilises an egg. This fertilised egg is called a zygote.
Sometimes a woman’s ovaries release 2 eggs, and a separate sperm fertilises each egg. This forms twins. These twins are called fraternal twins, dizygotic twins (meaning two zygotes) or non-identical twins.
During pregnancy, the developing babies get oxygen and food from their mother through the placentas and umbilical cords. Fraternal twins have separate placentas and umbilical cords. The technical name for this is dichorionic.
Fraternal twins can be the same or opposite sex and their genes are as different as any other brother and sister. Often, same-sex fraternal twins look different. For example, they might have different hair or eye colour. Occasionally they look quite similar.
Fraternal twins happen in about 70% of twin births in Australia.
Very rarely, fraternal twins share a placenta. These types of twins are called chimaeric twins.
Identical twins
Sometimes a fertilised egg splits within a few days of conception to produce genetically identical twins. Because these twins come from one zygote, they’re also known as monozygotic. Identical twins are the same sex.
There are 3 types of identical twins.
About one-third of identical twins split soon after fertilisation and form completely separate twins. Like fraternal twins, these twins have separate placentas.
The other two-thirds split after they attach to the wall of the womb. As a result, they share a placenta. The technical name for this is monochorionic.
In a very small number of identical twins, splitting might happen even later. In this case, both twins share an inner sac, called the amnion, in addition to sharing a placenta. The technical name for this is monoamniotic twins. They’re often called MoMo twins.
Identical twins happen in around 1 in 250 pregnancies in Australia.
Although identical twins have the same genes, they don’t always look the same. This is because children’s health and development are shaped not only by genes but also by experiences in the womb and after birth. For example, a twin who gets less blood from a shared placenta might weigh less at birth.
Sharing a placenta or inner sac: why it’s important to know
Sharing a placenta means that twins share a blood supply during pregnancy. Sometimes the blood supply is shared unequally, which can cause health problems for both twins.
Sometimes the blood supply is shared unequally, which can cause health problems for both twins.
Women who are pregnant with twins sharing a placenta need to be checked more often than women who are pregnant with twins with separate placentas. Frequent checks help to pick up any complications early.
Twins sharing an inner sac (monoamniotic) are also at a higher risk of complications during pregnancy because of the chance that their umbilical cords might tangle and cut off their blood supply. These twins are checked even more closely. Medical professionals often recommend that these twins are born at 32-34 weeks. This is earlier than other types of twins, who are generally born at 37-38 weeks.
Medical professionals use ultrasound to work out how many placentas twins have. The earlier the ultrasound, the more accurately it can say how many placentas there are. It gets harder to work out later in pregnancy. After the birth, medical staff will look at the placentas to check what type of twins they are.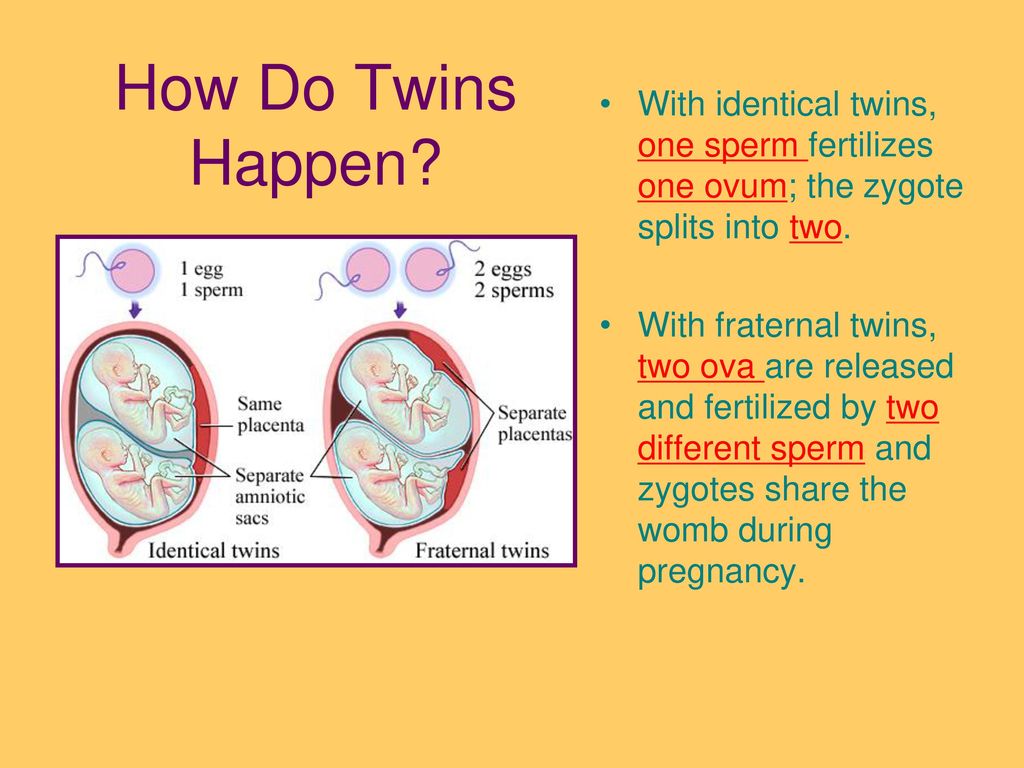
Fraternal or identical: why it’s important to know
Same-sex twins with separate placentas can be fraternal or identical. For health reasons, it’s good to know whether your twins are fraternal or identical.
To find out whether twins are identical or fraternal, you can ask for a genetic test after your babies are born. This is called a zygosity test. The test doesn’t hurt and involves collecting a sample of cheek cells by rubbing the inside of your babies’ cheeks with a soft applicator (like a cotton bud). The cost of this test starts at $199 (for both twins) in Australia.
Identical twins are more likely than fraternal twins to get the same illness. If one of a pair of identical twins is diagnosed with a particular disease or health condition, like high blood pressure, the other twin should be checked often for early symptoms.
Because of their genetic make-up, identical twins will always be compatible for organ transplantation, if they ever need it.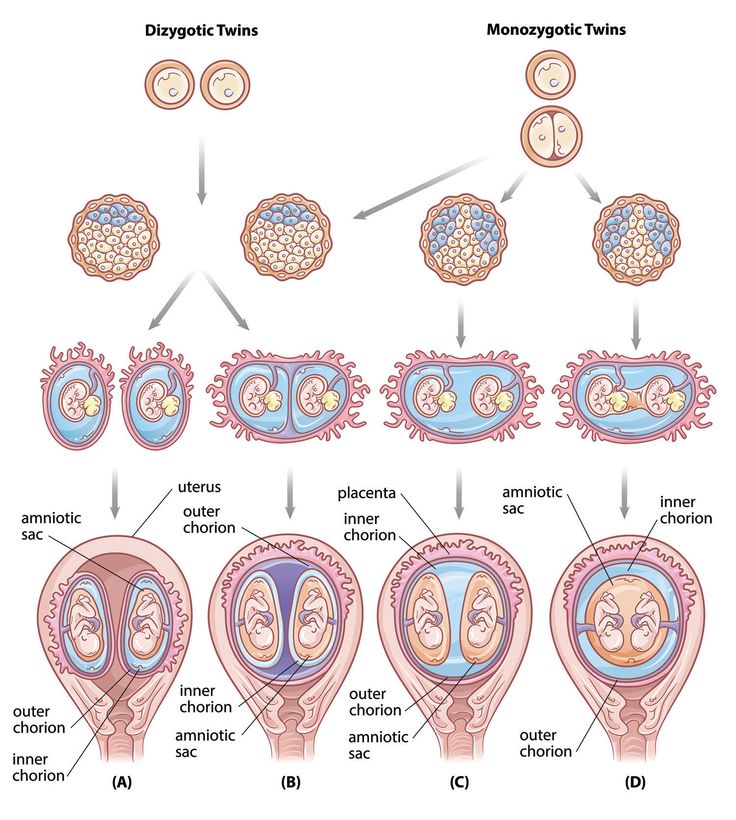 Fraternal twins are compatible only sometimes.
Fraternal twins are compatible only sometimes.
Other reasons why twins and parents of twins might want to know whether they’re fraternal or identical include:
- trying to work out the chance of having more twins in future pregnancies (only fraternal twins run in families)
- making sure they have the right information about their genetic make-up
- being able to answer questions from family, friends and others
- being involved in twin research
- just being curious!
Some identical twins are mirror twins – for example, their hair parts on opposite sides, they are oppositely handed, or they have birthmarks on opposite sides of their body. In some rare cases, their internal organs can be mirror images of each other. It’s not known why some twins are like this.
In very rare cases, twins can be born physically joined together in different ways. These twins, called conjoined twins (previously called Siamese twins), can happen if the fertilised egg splits quite late after fertilisation.
Triplets (1 in 5000 births) and quadruplets (less than 1 in 100 000 births) can develop as a result of combinations of fraternal and identical twinning. There are no reliable figures for quintuplets (5 babies) and sextuplets (6 babies).
More about twins
In Australia, twins happen in 1 in every 80 births. This means that 1 in 40 Australians is a twin.
The birth rate of identical twins is the same around the world and doesn’t vary with the mother’s age.
In contrast, the birth rate of fraternal twins varies widely across countries and can be influenced by the mother’s age. Women aged over 35 years are the most likely to have fraternal twins, because their ovaries are more likely to release more than one egg at a time.
More twins were born from the 1990s to the mid-2000s. This is because it was common to transfer more than one embryo during in-vitro fertilisation (IVF) treatments. The rate of twins from IVF is now lower, because it’s now usual practice to transfer only a single embryo.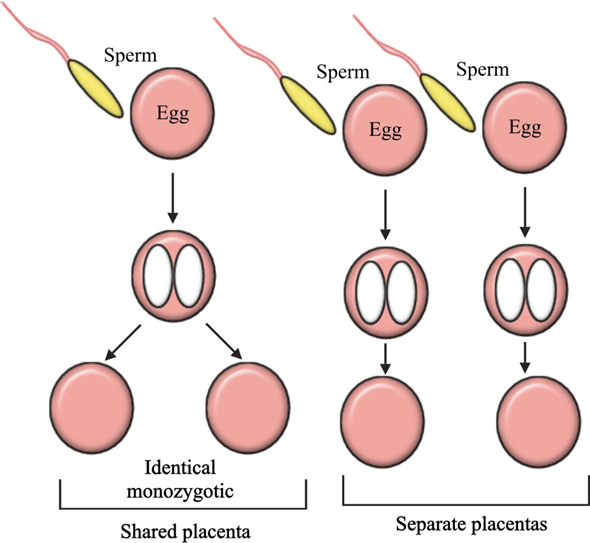
Monochorionic Twins
What are monochorionic twins?
A single placenta normally supports a single fetus. When the situation arises in which two fetuses have to share a single placenta, complications may sometimes develop. Identical twins that share a single placenta are called monochorionic twins (MC). “Chorion” is the Latin root that refers to the placenta, while the word “amnion” refers to the sac, or “membranes” that surround each fetus. While fraternal twins (2 eggs and 2 sperm) are always surrounded in their own sacs and have their own individual placentas, 70% of identical twins may end up sharing a single placenta. Only 1% of identical twins share both a single placenta and a single sac, and this poses significant risk.
When two fetuses share one placenta, their umbilical cords may implant anywhere – there is no set or predictable pattern – and depending on where they implant, one fetus may get less of a ‘share’ of the placenta than it’s co-twin, resulting in less blood flow and nutrition to one fetus, with more to the other (unequal placental sharing). As a result, although identical twins usually share the same genetic material, they may actually grow differently. Like the roots of a tree, the blood vessels that run from each implanted cord may connect with each other beneath the surface, as there is nothing separating them within a single placenta. Depending on which types of vessels connect to which, one fetus may transfuse blood to the other. We will discuss each of these complications, their risks, and potential treatments, below.
As a result, although identical twins usually share the same genetic material, they may actually grow differently. Like the roots of a tree, the blood vessels that run from each implanted cord may connect with each other beneath the surface, as there is nothing separating them within a single placenta. Depending on which types of vessels connect to which, one fetus may transfuse blood to the other. We will discuss each of these complications, their risks, and potential treatments, below.
- Watch Video (in Mandarin)
- Watch Video (in Spanish)
The following recommendations are meant for both patients and their providers as guidance during a pregnancy with monochorionic twins. For questions and referrals please call us at 1-800-RX-FETUS.
You can also download and print this information with our Monochorionic Twins Recommendations PDF brochure.
Complications Unique to Monochorionic Twins
- Unequal placental sharing
- Selective intrauterine growth restriction (S-IUGR) in one fetus
- TTTS - clinically defined as a deepest vertical pocket of > 8 cm in one twin and > 2 cm in in the other twin, simultaneously; TTTS can be seen overlapping with growth discordance, but these are separate diagnoses with different pathophysiologies
- Twin anemia polycythemia sequence (TAPS)
- Non-TTTS amniotic fluid discordance
- Discordant anomalies
- TRAP Sequence
Components of UCSF Evaluation
- Level II anatomic survey for (discordant) fetal anomalies
- Special attention paid to cord insertion locations and vascular mapping
- Fetal echocardiography for structural and functional integrity
- Fetal brain MRI > 22 weeks when indicated and appropriate
Potential Surgical Procedures
- Selective fetoscopic laser ablation
- Radiofrequency ablation (RFA) for cord occlusion
Timeframe for Referrals to UCSF
We welcome your call at any time to discuss your findings and obtain guidance about timing for referral and level of urgency 1-800-RX-FETUS.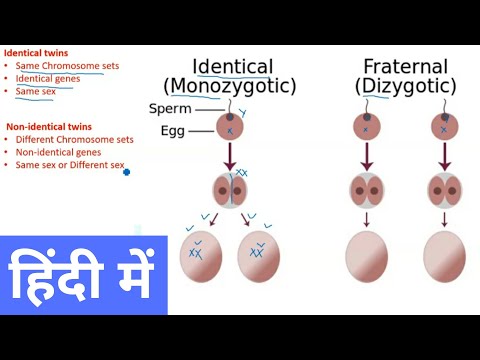
Consider Referral
- Significant amniotic fluid discordance
- Significant growth discordance (>20 percent)
- Isolated abnormal Doppler results
- Suspected discordant anomaly
Unless there is a lethal anomaly, if possible refer prior to 24 weeks to retain the option of RFA.
We encourage you to call our center to discuss your findings if you have concerns at 1-800-RX-FETUS
Call for Timely Referral (need to see patient within 1 week)
- Concurrent DVPs >8 cm and >2 cm, with normally sized bladder visualized and normal umbilical arterial (UA) Doppler results.
Call for Urgent Referral (need to see patient within a couple days)
- Concurrent DVPs >8 cm and >2 cm and either no visible donor twin bladder, abnormal UA Doppler results, suspected recipient cardiomyopathy or hydrops.
What is Needed For Referral
Patients referred to UCSF for an evaluation should have the following faxed to 415-502-0660:
-
Demographic information
-
A copy of the front/back of their health insurance card
-
All obstetric/maternal-fetal medicine (OB/MFM) medical records
-
If insurance authorization is required, for proper codes please download the Monochorionic Evaluation Codes.

-
Afterwards, call 1-800-RX-FETUS or 1-800-793-3887 to discuss your patient and complete the referral process.
The presence of an identical twin is manifested in the features of DNA methylation
The birth of identical twins in humans is a rare event (3-4 per 1000). It is not completely clear what exactly must happen in the initial stages of embryo development in order for pregnancy to develop according to this scenario. Meanwhile, multiple pregnancies are high-risk pregnancies in which one of the fetuses is likely to be lost: this happens in half of triplets and about 30% of twin pregnancies. Therefore, it is important for scientists to understand what leads to pregnancy according to the "twin" scenario. In an attempt to do this, Dutch researchers analyzed the DNA of several hundred identical twins. They did not achieve their original goal, but instead discovered an interesting fact. It turned out that in identical twins, not only DNA is identical, but also specific sites of DNA methylation. By analyzing such areas, it is possible to determine whether a person is one of identical twins or not.
By analyzing such areas, it is possible to determine whether a person is one of identical twins or not.
Identical twins are the result of fertilization of one egg by one sperm. In the early stages of development, the embryo can divide into two (very rarely more) parts. If the separation occurred before the formation of a 16-cell embryo (morula), then both twins have separate placentas and an amniotic sac (Fig. 1). Like all identical twins, they have virtually identical DNA. If the separation happened later - at the blastocyst stage, when the inner cell mass and the trophoblast separate, which give rise to the embryonic body and placenta - then each twin will have its own amniotic sac, but one placenta. This is the most common situation. A rarer variant is separation at later stages, resulting in a common amniotic sac and one placenta for both twins. The rarest case is the formation of Siamese twins. Identical twins are rare (3-4 per 1000 births), and, apparently, the frequency of their occurrence does not depend either on the age of the mother or on any genetic characteristics of the parents.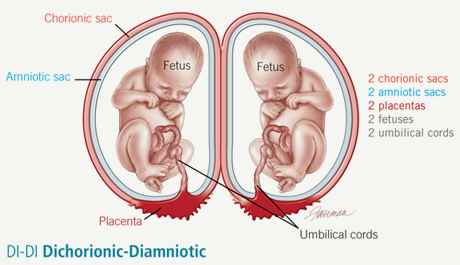
In addition to the fact that the birth of identical twins is a rare event, the bearing of such pregnancies is often accompanied by complications for both the mother and the fetus. Fetal development takes a long time and requires a lot of resources. Therefore, children who are born in multiple pregnancies (including in pairs of fraternal twins that occur if a woman ovulates several eggs fertilized by different spermatozoa at once, see Fig. 1) are often born prematurely and with low birth weight. For the mother, such a pregnancy also increases the risk of preeclampsia and gestational diabetes.
There are also rare, specific complications. In feto-fetal transfusion syndrome, the blood pathways of twins with the same placenta begin to connect. This leads to the fact that one twin receives too much blood, and this increases the load on his cardiovascular system and kidneys, while the second, on the contrary, receives too little blood, oxygen and nutrients. In severe cases, with a probability of 60–100%, this leads to a fatal outcome for the fetus.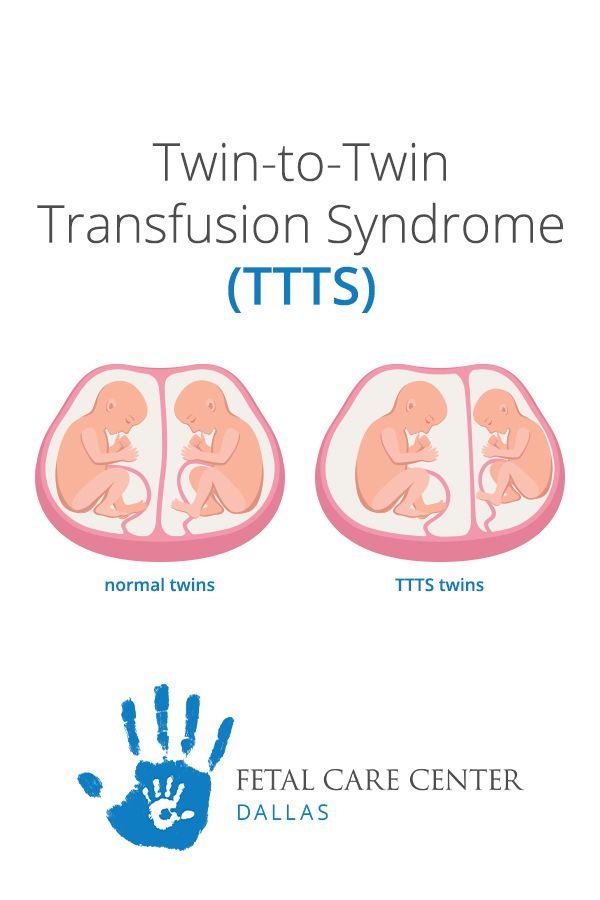
Another complication is the so-called "vanishing twin phenomenon" (see Vanishing twin), in which one of the fetuses does not survive in the early stages of development. This can also happen in cases of pregnancy with fraternal twins. The most common scenario is that the fetus is reabsorbed. This is a common occurrence in the animal world: in hares, the level of embryonic and fetal reabsorption is 42%, in dogs and mice - about 10% (Drews et al., 2020. Spontaneous embryo resorption in the mouse is triggered by embryonic apoptosis followed by rapid removal via maternal sterile purulent inflammation). In this case, the fetus and placenta are destroyed and absorbed by the walls of the uterus. In more rare cases, only the embryo is resorbed, or the fetus is mummified and flattened, squeezed out by a healthy developing fetus. It is believed that 20-30% of multiple pregnancies are accompanied by the "phenomenon of the disappeared twin", but there is no information about how many of them are fraternal and how many are identical.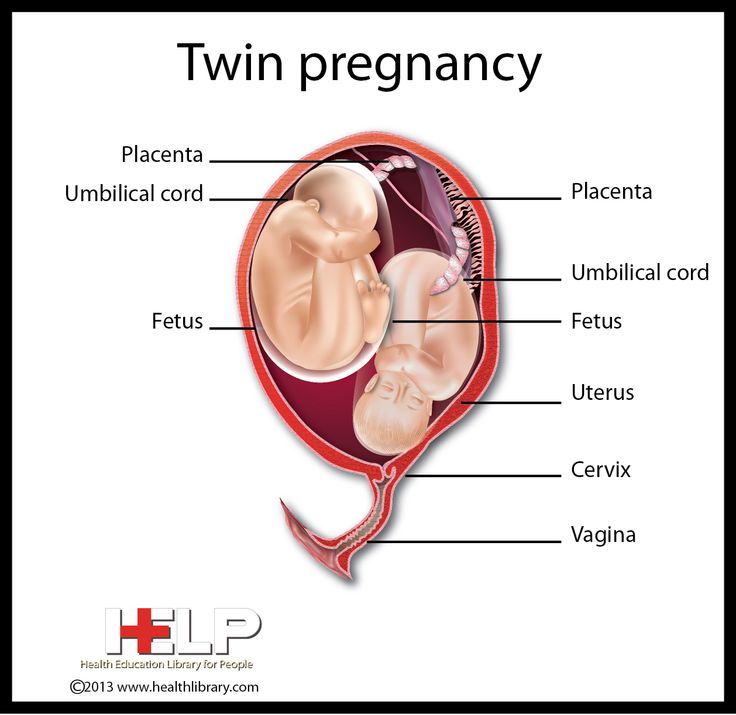
The separation of identical twins occurs at one of the critical moments in human development. The union of the mother's egg and the father's sperm has just occurred and the formation of a new diploid genome. It will remain practically unchanged, but its activity will gradually change: genes will be switched on and off, which will ensure the development of the organism. This happens due to epigenetic regulation of genes and other DNA-related processes, in which the nucleotide sequence is not affected. DNA methylation is one of the ways in which a methyl group is attached to cytosine, most often located next to guanine (CpG, where C is cytosine, p is a phosphodiester bond, G is guanine). However, methylation of cytosines before other nucleotides is also possible. DNA methylation most often "turns off" genes if CpGs are methylated on DNA regions associated with the "start" of genes (promoters). At the same time, transcription factors cannot bind to these sites, and chromatin packaging also changes, which also reduces the transcriptional activity of the promoter.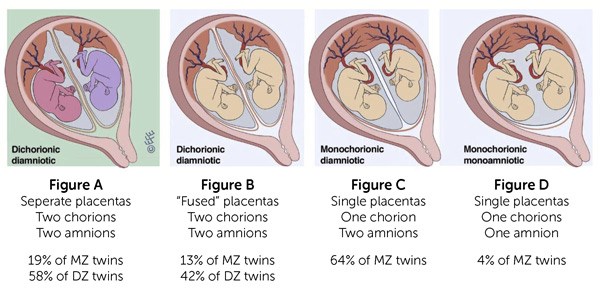
Egg and sperm DNA are methylated, but after the formation of the zygote they "reset": most of the methyl groups are removed either due to "dilution" during DNA duplication (new strands remain unmethylated), or special enzymes. This global demethylation continues until the formation of the blastocyst, and at the next stage, the formation of the gastrula, new methyl marks are established. After that, the methylation pattern changes, reflecting different stages in organogenesis and growth of the embryo, and then the fetus (Fig. 2). Each new cell type will have its own label distribution pattern.
The distribution of methyl marks depends not only on which genes should be active in a particular type of cell, but also on environmental factors, in particular exposure to toxins, diet and lifestyle. Therefore, despite the fact that identical twins have almost identical DNA, the distribution of epigenetic markers can differ even in newly born babies, and even more so this difference increases with age (L. Gordon et al., 2012. Neonatal DNA methylation profile in human twins is specified by a complex interplay between intrauterine environmental and genetic factors, subject to tissue-specific influence). There are a number of studies comparing methylation in identical twins, one of which has a disease, such as autism spectrum disorder (S. Liang et al., 2019. Genome-Wide DNA Methylation Analysis Reveals Epigenetic Pattern of Sh3B1 in Chinese Monozygotic Twins Discordant for Autism Spectrum Disorder) or schizophrenia (C. Castellani et al., 2015. DNA methylation differences in monozygotic twin pairs discordant for schizophrenia identifies psychosis related genes and networks). It uses the genome-wide epigenetic association study (EWAS, Epigenome-wide association study) method, which allows you to compare the methylation status of various DNA regions in the studied population (identical twins and the control group) and associate them with some traits or diseases.
Gordon et al., 2012. Neonatal DNA methylation profile in human twins is specified by a complex interplay between intrauterine environmental and genetic factors, subject to tissue-specific influence). There are a number of studies comparing methylation in identical twins, one of which has a disease, such as autism spectrum disorder (S. Liang et al., 2019. Genome-Wide DNA Methylation Analysis Reveals Epigenetic Pattern of Sh3B1 in Chinese Monozygotic Twins Discordant for Autism Spectrum Disorder) or schizophrenia (C. Castellani et al., 2015. DNA methylation differences in monozygotic twin pairs discordant for schizophrenia identifies psychosis related genes and networks). It uses the genome-wide epigenetic association study (EWAS, Epigenome-wide association study) method, which allows you to compare the methylation status of various DNA regions in the studied population (identical twins and the control group) and associate them with some traits or diseases.
In a recent study, Dutch researchers used EWAS to compare methylation in leukocytes and buccal (i.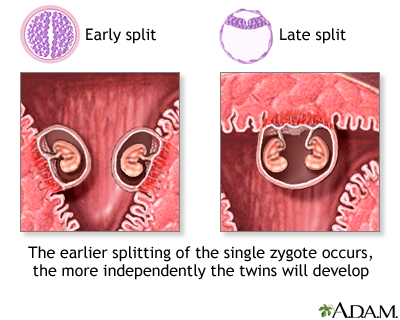 e., taken from the inside of the cheek) scrapings of adults, each of whom had an identical twin (of which 924 people were studied). The study also included fraternal twins (1033 people). They acted as an ideal control, since they were also present in the mother's uterus together, therefore they were exposed to all the same factors that could affect DNA methylation as identical twins.
e., taken from the inside of the cheek) scrapings of adults, each of whom had an identical twin (of which 924 people were studied). The study also included fraternal twins (1033 people). They acted as an ideal control, since they were also present in the mother's uterus together, therefore they were exposed to all the same factors that could affect DNA methylation as identical twins.
Participants' DNA samples were obtained from the Netherlands Twin Registry. Since the early 1980s, it has included data on 120,000 twins and about the same number of their close relatives. When analyzing methylation, we looked for DNA regions whose methylation status (whether the region is more or less methylated) is similar in identical twins, but not in fraternal twins. 234 such DNA regions were found. The scientists also decided to see if such special marks would be observed in other twin registries. The authors also found them in other databases: the UK Adult Twin Registry, the Finnish Twin cohort, the E-Risk (Environmental Risk (E-Risk) Longitudinal Twin Study) and BSGS ( Brisbane Systems Genetics Study). Interestingly, such marks were present not only in adults, who made up the bulk of the participants, but also in a cohort of children from the Netherlands registry. This observation is very important, as it shows that marks are preserved not only with age, but also in tissues of different origins (leukocytes originate from the mesoderm, while cheek epithelial cells from the ectoderm).
Interestingly, such marks were present not only in adults, who made up the bulk of the participants, but also in a cohort of children from the Netherlands registry. This observation is very important, as it shows that marks are preserved not only with age, but also in tissues of different origins (leukocytes originate from the mesoderm, while cheek epithelial cells from the ectoderm).
Data from all studies pooled (total 5723 participants). It turned out that 834 sites have a special methylation status in identical twins. 60% of them were less methylated than fraternal twins, and the rest had more methyl marks. The marks differed between pairs of twins, but within one pair, the differences were estimated at 0.8–7.8%, depending on the DNA regions. All such DNA segments are distributed unevenly throughout the genome. The less methylated regions were mainly located at the ends of the chromosomes, near the telomeres, and the more methylated regions were located near the centromeres (Fig.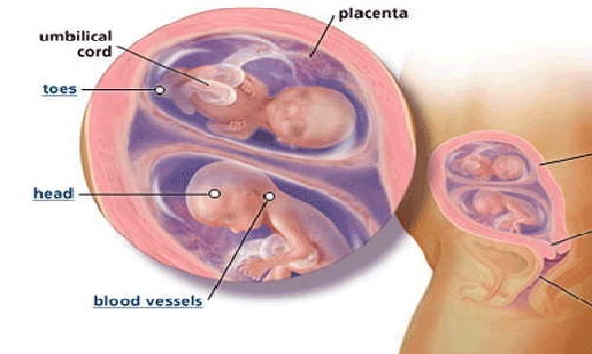 3a).
3a).
The researchers also determined the location of these special regions depending on the relationship with transcriptional activity. It turned out that less methylated regions are most often found with genes that are active during development, but become silent after its completion, while more methylated regions are found in heterochromatic regions of the genome. In addition, the authors compared the already found sections with the so-called metastable epialleles, that is, DNA sections that are “marked” with methyl marks during early embryonic development (including due to environmental factors) and remain so in all cells of the body. Such areas differ in different people, but remain similar in monozygotic twins (T. van Baak et al., 2018. Epigenetic supersimilarity of monozygotic twin pairs). Special methylation sites are often present in metastable epialleles.
By analyzing methylated DNA sequences, it is possible to determine whether they contain binding sites for various transcription factors required for the activity of certain genes. It turned out that regions with a reduced level of methylation are in the binding motifs of 31 transcription factors involved in the early development of the embryo. The authors do not offer an explanation for this phenomenon. However, sites with increased methylation in identical twins were found in the binding motifs of 13 transcription factors, which are also associated with cell adhesion. 79DNA sections are present in the cluster of protocadherin genes (clustered protocadherins) - proteins involved in cell adhesion. This discovery is extremely interesting, since it is protocadherins and cadherins that are likely to be involved in the process of embryo division and the formation of identical twins. How increased methylation might affect this is unknown and requires further study.
In addition to actually determining the location of areas with a special methylation status, the authors also investigated their relationship with the development and life of identical twins. They compared how the DNA of the studied regions in cells from buccal scrapings from different types of twins was methylated. The most similarity in methylation was in twins with a common placenta and an amniotic sac, which, let me remind you, are the last to separate. Least of all - in twins with separate placentas and amniotic sacs (Fig. 3, b-d). The greatest differences were observed in the protocadherin gene clusters.
The results of the study also have practical applications. The authors developed a special algorithm based on data on specific twin methylation sites, which is able to distinguish between a person from a pair of identical twins and a person who did not have a twin. This is not only an interesting analysis that allows you to get to know yourself better, but also an important diagnostic method. The fact is that methylation patterns can help determine why certain diseases occur in people. There are a number of defects and syndromes that often occur in identical twins, but can also occur in children from singleton pregnancies. One of the common hypotheses for their appearance is the connection with the division of the embryo into two. It is assumed that in this case, too, the fetus had a twin who disappeared. It is methylation that can help determine the correctness of this hypothesis.
Whether the methylation features of identical twins are a cause, a consequence, or just an event accompanying their appearance remains a mystery.
Source: Jenny van Dongen et al. Identical twins carry a persistent epigenetic signature of early genome programming // Nature Communications . 2021. DOI: 10.1038/s41467-021-25583-7.
Ekaterina Gracheva
reasons - CSM Zdravitsa - CSM Zdravica
July 22, 2022
- What is a multiple pregnancy?
This is pregnancy, when not one fetus develops in the mother's body, but several at once. A multiple pregnancy is identical or dizygotic twins (triplets and more children).
- Monochorionic monoamniotic twins - when there is a common placenta and there is no septum between the twins, it is always identical twins.
- Monochorionic diamniotic twins - when the common placenta and septum, i.e. each fetus has its own amniotic sac.
- Dichorionic diamniotic twins - when each fetus has its own placenta and its own amniotic bladder.
Identical twins are always the same sex, have the same blood type, and are very similar in appearance. Accordingly, the opposite is true for fraternal twins. They have phenotypic differences (eye color, facial features), there may be a different blood type. Fraternal twins may be of different sexes.
Fraternal twins are formed when different eggs are fertilized by different spermatozoa. Most often, this occurs under the influence of hormonal ovarian stimulation (ovulation stimulation, assisted reproductive technologies), when several follicles with eggs are formed at once or one follicle with several eggs at the same time. Accordingly, each egg will be fertilized by a separate sperm.
The development of identical twins occurs when one egg is fertilized by one sperm, but in the process of division of the fetal egg into two, three or four parts at different stages of its development. In this case, each part develops as a separate organism. It is assumed that such separation can occur when the implantation (attachment) of the fetal egg is delayed due to oxygen deficiency. Also, the occurrence of identical twins is also associated with the fertilization of an egg that had two or more nuclei.
Most often, identical twins do not have a septum between them and the fetuses have one common placenta. But depending on the stage of development, separation has occurred; identical twins can be separated by a septum from each other and may have different placentas or one common placenta, but each is in its own amniotic bladder.
Theoretically, it is possible to fertilize two eggs of different ovulation periods.