Oral thrush in 1 year old
Oral Thrush (for Parents) - Nemours KidsHealth
Reviewed by: Michelle P. Tellado, MD
en español Muguet (candidiasis oral)
What Is Oral Thrush?
Oral thrush is a very common yeast infection in babies. It causes irritation in and around a baby's mouth.
What Are the Signs and Symptoms of Oral Thrush?
Oral thrush (also called oral candidiasis) can affect anyone, but is most common in babies younger than 6 months old and in older adults.
A baby with oral thrush might have cracked skin in the corners of the mouth or white patches on the lips, tongue, or inside the cheeks that look a little like cottage cheese but can't be wiped away.
Some babies may not feed well or are uncomfortable when sucking because their mouth feels sore, but many babies don't feel any pain or discomfort.
What Causes Oral Thrush?
Oral thrush is caused by the overgrowth of a yeast (a type of fungus) called Candida albicans.
Most people (including infants) naturally have Candida in their mouths and digestive tracts, which is considered normal growth. Usually, a healthy immune system and some "good" bacteria control the amount of this fungus in the body.
But if the immune system is weakened (from an illness or medicines like chemotherapy) or not fully developed (as in babies), Candida in the digestive tract can overgrow and lead to an infection. Candida overgrowth also causes diaper rash and vaginal yeast infections. Babies can have oral thrush and a diaper rash at the same time.
Candida overgrowth also can happen after a baby has been given antibiotics for a bacterial infection because antibiotics can kill off the "good" bacteria that keep the Candida from growing. Oral thrush also can happen after the use of steroid medicines.
How Is Oral Thrush Treated?
See your doctor if you think your baby may have thrush. Some cases go away without medical treatment within a week or two, but the doctor may prescribe an antifungal solution for your baby's mouth. This medicine is usually applied several times a day by "painting" it on the inside of the mouth and tongue with a sponge applicator.
This medicine is usually applied several times a day by "painting" it on the inside of the mouth and tongue with a sponge applicator.
Depending on your baby's age, the doctor also might suggest adding yogurt with lactobacilli to your baby's diet. The lactobacilli are "good" bacteria that can help get rid of the yeast in your child's mouth.
If your baby keeps getting oral thrush, especially if he or she is older than 9 months old, talk with your doctor because this might be a sign of another health issue.
Can Oral Thrush Be Prevented?
Oral thrush is a common infection in babies, but you can help prevent it:
- If you formula-feed your baby or use a pacifier, thoroughly clean the nipples and pacifiers in hot water or a dishwasher after each use. That way, if there's yeast on the bottle nipple or pacifier, your baby won't be reinfected. Store milk and prepared bottles in the refrigerator to prevent yeast from growing.
- If you breastfeed and your nipples are red and sore, you might have a yeast infection on your nipples, which you and your baby can pass back and forth.
 Talk to your doctor, who might recommend using an antifungal ointment on your nipples while your baby is treated with the antifungal solution.
Talk to your doctor, who might recommend using an antifungal ointment on your nipples while your baby is treated with the antifungal solution.
To prevent diaper rash, change diapers often.
Reviewed by: Michelle P. Tellado, MD
Date reviewed: September 2019
Oral thrush in babies | Pregnancy Birth and Baby
Oral thrush in babies | Pregnancy Birth and Baby beginning of content3-minute read
Listen
Oral thrush is a type of fungus infection, very common among babies. It appears as moist, milky-white patches in and around a child's mouth. Usually oral thrush is not serious and can sometimes even go unnoticed.
What causes oral thrush?
Oral thrush is a yeast infection caused by a fungus called Candida albicans. While around 1 in every 2 people live healthily with the fungus, at times it grows too quickly, causing a visible infection. If your child is on antibiotic treatment or taking inhaled corticosteroids (such as those in many commonly-used asthma puffers), they are more likely to have oral thrush. An immunocompromised child (a child with a weak immune system — either as a result of illness or a medical treatment), is also more likely to be infected.
While around 1 in every 2 people live healthily with the fungus, at times it grows too quickly, causing a visible infection. If your child is on antibiotic treatment or taking inhaled corticosteroids (such as those in many commonly-used asthma puffers), they are more likely to have oral thrush. An immunocompromised child (a child with a weak immune system — either as a result of illness or a medical treatment), is also more likely to be infected.
What are the symptoms?
Oral thrush appears as milky, white patches on the insides of a child's cheeks, tongue or lips and cannot be wiped away easily, as the infection is under the skin. The patches might also appear red or inflamed. Usually, the infection doesn't cause irritation, however if the mouth area is very red and raw, it might be hard for your child to eat. Another sign that your child may have an oral thrush infection is drooling.
Thrush can also appear in the nappy area (nappy rash).
Is oral thrush contagious?
While the fungus is contagious, it doesn't transfer easily. The most common points of transfer include:
The most common points of transfer include:
- teething toys
- dummies
- teats
- bottles
The yeast might transfer from one person to another, for example, when a child chews on an infected child's toy. Another common infection point for a baby is their mother's vagina (vaginal oral thrush) during birth, as the yeast often lives in small amounts in the vagina.
Treating oral thrush
Your doctor can prescribe your child antifungal drops or gel to help manage the infection. If you are a breastfeeding mother with an infected child, your doctor might also prescribe an antifungal gel for your nipples. This is because you might be spreading the infection to your child when feeding. You can continue to breastfeed as usual if your baby has oral thrush.
Preventing oral thrush
Maintaining a high level of oral (mouth) and personal hygiene is a good way to prevent the spread of the infection. If your child has teeth, this includes brushing twice a day and taking them to the dentist for check-ups and treatments. It is important to sterilise items that come into contact with your child's mouth, including teething toys, dummies, and bottles. Clean teats well in between feeds to ensure that your child doesn't become reinfected.
It is important to sterilise items that come into contact with your child's mouth, including teething toys, dummies, and bottles. Clean teats well in between feeds to ensure that your child doesn't become reinfected.
Does my child need to see a doctor?
If you think your child may have oral thrush, it's a good idea to take your child to see a doctor to get a diagnosis. Most cases are very mild, and will quickly clear up with prescription gel or drops.
Be sure to take your child to the doctor if:
- white patches appear in their mouth
- the rash keeps on coming back after treatment
- they have a fever or are feeling generally unwell
- you are concerned about your child’s health
Sources:
Raising Children Network (Oral thrush in babies and children), DermNet NZ (Oral candidiasis), Better Health Channel (Oral conditions - young children)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2020
Back To Top
Related pages
- Regular health checks for babies
Need more information?
Oral thrush in babies and children | Raising Children Network
Oral thrush is a fungal infection in and around babies’ mouths. It’s common and isn’t usually anything to worry about. Read about oral thrush treatment.
Read more on raisingchildren.net.au website
Dental health - Diabetes Australia
The mouth is often overlooked as an area of the body with complications associated with diabetes.
Read more on Diabetes Australia website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.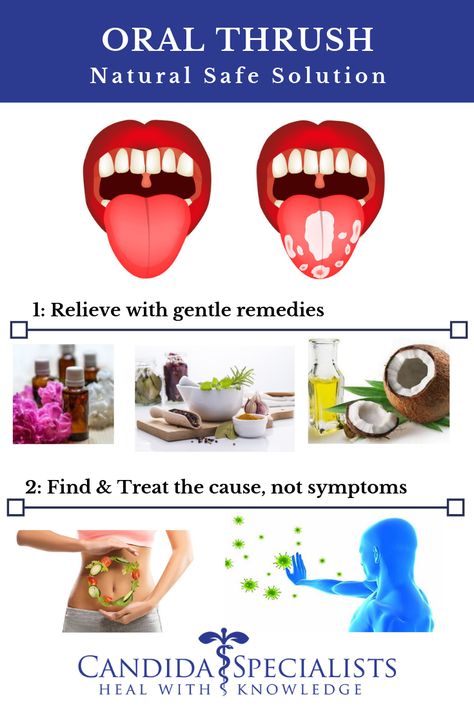
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.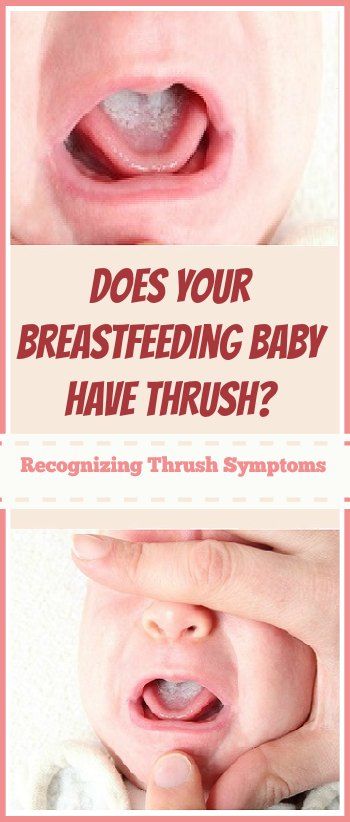
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Children's stomatitis - causes, symptoms, types of stomatitis, methods of diagnosis and treatment of children's stomatitis in the "SM-Clinic" for children and adolescents
Signs of stomatitis in a child depend on the form of pathology and the cause that caused the disease.
Herpetic or viral stomatitis
It is caused by the introduction of the herpes simplex virus type 1, and can have two forms in children: acute primary and secondary recurrent. In newborns and breastfed infants, it is rare due to the presence in the body of a large number of antibodies received from the mother, or it occurs in a mild form almost imperceptibly. At an older age, the pathology manifests itself acutely, with severe symptoms of intoxication. The most common ways of infection: household items, toys, close contact with carriers, airborne.
In newborns and breastfed infants, it is rare due to the presence in the body of a large number of antibodies received from the mother, or it occurs in a mild form almost imperceptibly. At an older age, the pathology manifests itself acutely, with severe symptoms of intoxication. The most common ways of infection: household items, toys, close contact with carriers, airborne.
Symptoms of herpetic stomatitis in babies are:
- ulceration on the mucosa simultaneously in several places of approximately the same type and size;
- an increase in temperature, often to high values \u200b\u200band even before the first rashes appear;
- undulating reappearance of painful sores, which each time is accompanied by a rise in temperature;
- swelling of the gums, their redness;
- the appearance of an unpleasant, putrid odor from the mouth.
Candidiasis stomatitis
In the people, this disease is commonly called children's thrush. Most often this form affects children under 3 years of age. It is fungal in nature, caused by the yeast-like fungus Candida. This type of stomatitis is preceded by a burning sensation in the mouth, excessive dryness of the affected mucosa, an unpleasant taste and smell. The child behaves restlessly, refuses to eat; observed sleep and eating disorders. Soon, the inner side of the cheeks, tongue, gums and even lips are covered with small whitish dots, which, merging and forming a dense white coating of curdled consistency, multiply rapidly. In advanced cases, plaque acquires a dirty gray color. It is almost impossible to remove it, under it a swollen, inflamed surface is found, which, at the slightest physical impact, begins to bleed.
Angular stomatitis
Sometimes it is considered as a kind of candida, because it can be caused by the same Candida fungi or streptococci. In this case, the corners of the lips are affected, which makes it difficult for the child to open his mouth, eat, and even talk. It is more common in children of school age. When affected by streptococci, a purulent crust forms on the surface of the ulcers, which, when removed, immediately grows again. The disease is recurrent in nature and is often popularly referred to as "zayed".
Aphthous stomatitis
Aphthous stomatitis is accompanied by the following symptoms:
- temperature increase;
- loss of appetite;
- burning and itching in the mouth.
- the appearance on the inner surface of the cheeks, gums, tongue and palate of painful white sores with a red border and a cloudy film on top - aphthae, which have clear and even edges characteristic of this type of disease.
Often this form of pathology occurs against the background of severe weakness, drowsiness of the baby. In some children, aphthous stomatitis is rare, in others it is observed up to 2 or more times a year.
Bacterial stomatitis
One of the diseases of "dirty hands". The cause of development is a bacterial infection that has entered the mouth. The introduction occurs especially quickly when the integrity of the mucosa is violated: with a wound in the mouth, a bitten inner surface of the cheeks or lips, a newly erupted tooth, etc. The same form of the disease includes infections obtained during passage through the birth canal, especially in the case of a mother with venereal diseases, scarlet fever, etc.
External symptoms directly depend on the type of bacteria, and its manifestation depends on the state of the child's immune system. Often manifested by inflammation of the gums or the appearance of a dirty gray film on them. The child experiences pain while eating, especially sharp when eating spicy and pickled foods, citrus fruits, etc. The mucous membrane of the mouth is edematous and acquires a darker shade, burns and itches. Then bubbles appear on it, which quickly ulcerate or crack, begin to bleed. The process is very painful and is accompanied by a putrid specific smell from the mouth. Against this background, the temperature often rises to high values, the head and joints hurt, symptoms of intoxication of the body may be present. The child becomes weak, lethargic and capricious.
Common symptoms for any form of stomatitis are fever, ulceration of the oral mucosa and swollen lymph nodes.
Stomatitis in children - treatment, causes and symptoms of the disease
Stomatitis is an inflammatory process of the oral mucosa, often of an infectious or allergic origin. Stomatitis is one of the most common diseases of the oral cavity in children of all ages, from infants to schoolchildren, although it can sometimes occur in adults. The special predisposition of children to this disease is explained by the fact that at a young age the oral mucosa is softer and thinner than in adults.
Types of stomatitis and causes in children
The causes of stomatitis in children can be different, and they are directly related to the type of disease. In this section, we consider the main types of stomatitis and their causes in babies.
Herpetic viral stomatitis
This type of stomatitis is the most common and frequently encountered. Sometimes this type of disease is simply called herpetic stomatitis or viral . It usually occurs in children aged 1 to 4 years.
Infection often occurs by airborne droplets. Infection with herpetic viral stomatitis is also possible through children's toys, dishes and other items. Against the background of weak immunity, the virus enters the body and settles in the most damaged areas of the mucosa. Such places can be, for example, small wounds that appear after biting the lips of a child.
Aphthous (allergic) stomatitis
This type of stomatitis is often also called medical stomatitis, since the main cause of this type of disease is allergic reactions to various drugs. It is impossible to say exactly which drugs can cause stomatitis, this is an individual predisposition, and can only be accurately established when visiting a pediatric dentist after all the necessary diagnostics have been carried out. This type of disease occurs infrequently and, most often, in preschool children.
Traumatic stomatitis
As the name implies, this kind of disease occurs after mechanical injuries of the child's oral cavity and the ingress of dirt and bacteria into these places.
Injuries can be of a completely different nature. It could be purely a dental problem. For example, due to an incorrect bite, a child may bite his tongue or lips all the time. Other types of mechanical damage to the mucosa include burns, for example, from too hot food, too hard a nipple, various bad habits (pulling toys into your mouth, gnawing a pencil, etc.).
Candidal (fungal) stomatitis
The main cause of candidal stomatitis is Candida species. Basically, this type of disease is typical for children under 1 year of age who are breastfed. The particles of mother's milk that remain in the baby's mouth after feeding serve as an excellent environment for the development of this type of fungus. For this reason, sometimes this kind of stomatitis is called thrush .
Infectious (microbial) stomatitis
The main cause of infectious stomatitis in children is a decrease in immunity against the background of such diseases as tonsillitis, sinusitis, pneumonia and other diseases of the nasopharynx. This type of disease occurs in children of both school and preschool age. Especially often, infectious stomatitis develops in the autumn-winter period, when there is a weakening of the child's immunity.
Symptoms of stomatitis in children
As well as the causes of stomatitis in children, its symptoms are wide and also depend on the type of disease. In this section, we will group the characteristic symptoms for each form of stomatitis in children.
Symptoms of viral stomatitis in children
The main symptom of viral (herpetic) stomatitis is the appearance of vesicles on the oral mucosa, which, after opening, form small erosions covered with plaque. Such erosions can be multiple in nature and located both at a distance from each other, and merge together, forming large affected areas of the oral mucosa. They can be located on the lips, larynx, cheeks, tongue, or palate and are usually very painful and highly responsive to touch, hot or cold food, and other stimuli.
Symptoms of candidal stomatitis in children
Usually, before the onset of candidal stomatitis, the child experiences dryness of the oral mucosa, burning, a feeling of unpleasant aftertaste and smell from the mouth. By the behavior of the baby, you can suspect the onset of the disease. As a rule, during this period, children are capricious during meals, behave restlessly, and sleep poorly. Further, with the development of the disease, many small white dots appear, which form the site of the lesion, covered with a white curdled coating. With advanced forms of the disease, plaque may become gray. This indicates the transition of the disease to a severe form. In a severe form of candidal stomatitis, it is difficult to clear the mucosa from plaque and, at the slightest touch to the damaged area, it manifests itself as severe pain and bleeding.
Symptoms of bacterial (infectious) stomatitis in children
- The mucous membrane turns dark red;
- There is a formation of yellow crusts, which, as it were, stick together the lips;
- The child has increased salivation;
- There is bad breath.
Also, depending on the infection that caused the appearance of stomatitis, the following symptoms may be observed: the formation of fibrinous films, bleeding of damaged areas, severe plaque on the tongue.
Symptoms of aphthous stomatitis in children
With aphthous stomatitis, ulcers and aphthae form on the oral mucosa. Aphtha is a painful area of the mucous membrane of a rounded shape, covered with a fibrinous coating. With aphthous stomatitis, children become lethargic, irritable, moody and complain of pain in the oral cavity. As a rule, aphthous stomatitis is chronic and can worsen 1-2 times a year.
Treatment of stomatitis in children
There is no single correct treatment for stomatitis in children. Treatment is selected individually for each child after visiting a pediatric dentist and is highly dependent on the form of stomatitis. Depending on the type of disease, treatment may include both local and general therapy methods.
Despite the impossibility of choosing a treatment for all types of stomatitis, there are a number of recommendations that should be followed in any form of the disease. During the course of the disease, it is recommended to adhere to a strict diet that excludes the intake of hot or too cold food, as well as the rejection of other foods that irritate the oral cavity. Particular attention should be paid to oral hygiene. It is recommended to rinse your mouth after every meal. For rinsing, you can use special herbs or antiseptics.
In the treatment of the viral form of stomatitis in children, various anesthetics and antiviral drugs, anti-inflammatory ointments and gels, and immunomodulating drugs are used topically.
To treat candidal stomatitis, it is necessary to create a certain alkaline environment in the oral cavity. This is achieved by lubricating the baby's oral cavity with a solution of soda or boric acid. Also in pharmacies there are special antifungal solutions, such as Candide. It is recommended to lubricate after each meal.
In the treatment of bacterial stomatitis, as in the treatment of other infections, antibiotics are used. Self-administration of antibiotics is strictly prohibited. Antibiotics should be correctly selected and prescribed only by a pediatric dentist, based on the sensitivity of microorganisms to certain drugs.
In the treatment of aphthous stomatitis, anesthesia of the oral cavity with the help of anesthetic gels is used, the mucous membrane is treated with antiseptic preparations. Light therapy with ultraviolet rays is also used. At the same time, it is recommended to carry out general immunostimulating therapy, with the help of special preparations and vitamins.
Cost of services. Children's dentistry.
| Pediatric dentistry | |||
|---|---|---|---|
| A11.07.012 | Remineralizing therapy (deep fluoride of enamel one tooth) | ₽ | |
| A11.022 | Treatment of the mucous membrane 1,200.001 | Treatment of pulpit of temporary tooth by vital amputation with the subsequent restoration of the crown part of the tooth with photo composite material (second visit) | 3 500 ₽ |
| A16.07.002 | Treatment of temporal ampli -to -prison method in one | ||
| А16.07.025.001 | Selective grinding of one tooth | 250 RUB | |
| А16. | Minimum manipulation in children's dentistry | 1 000 ₽ | |
| A16.07.030 006 | Treatment of pulpitis (periodontitis) of a permanent tooth with unformed roots 2-channel tooth | 6 400 ₽ | |
| 0166 | 7 800 ₽ | ||
| A16.07.03.03.007 | Treatment of pulpit (periodontitis) of a permanent tooth 4-channel tooth | 8 800 ₽ | |
| A165 A165 A165 A165 A165 A165 A165 A165 A165 A165 A165 A165 A165 A165A teeth using special cleaning pastes and brushes) temporary bite | 2 400 ₽ | ||
| A16.07.051 | Professional oral hygiene (teeth cleaning using special cleaning pastes and brushes, PROPHY Flex system) temporary/replacement bite | 2 800 ₽ | |
| A16.07.051 | Professional oral hygiene (teeth cleaning using special cleaning pastes and brushes, Prophy Flex system) constant bite | 3 800 ₽ | AND RUBS | Mechanical cleaning of teeth using cleaning pastes (one tooth) | 220 ₽ |
| A16. |