Placenta and fetus
About the placenta – role and complications
About the placenta – role and complications | Pregnancy Birth and Baby beginning of content7-minute read
Listen
What is the placenta?
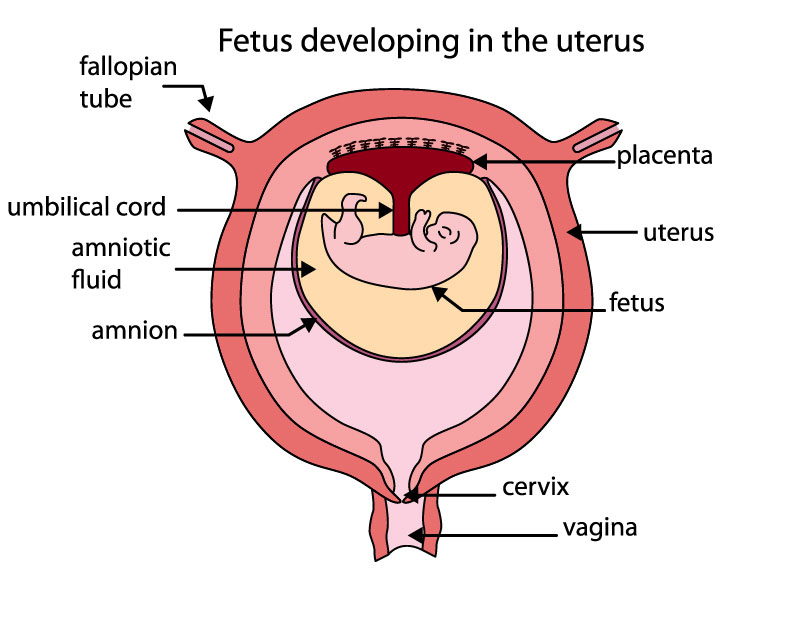
The placenta is a temporary organ that develops during pregnancy. It attaches to the lining of your uterus and delivers oxygen and nutrients to your growing baby through the umbilical cord.
If something goes wrong with the placenta, it can be serious and even life-threatening to both mum and baby.
What is the role of the placenta during pregnancy?
The placenta passes oxygen, nutrients and antibodies from your blood to your baby. It also carries waste products from your baby back to your blood, so your body can get rid of them.
The placenta also produces some hormones like oestrogen and progesterone that are needed during pregnancy.
What is the normal position of the placenta during pregnancy?
The placenta should attach to the wall of the uterus, usually at the top, side, front or back. The exact location will vary from person to person and in each pregnancy.
The placenta can sometimes develop low in the uterus but will generally move higher as your uterus stretches. The position of the placenta will be checked at your 18-week ultrasound.
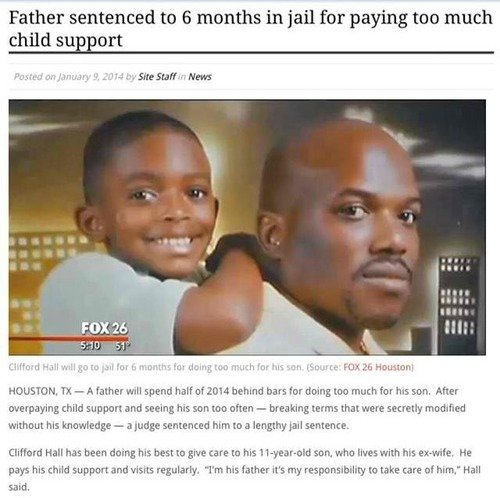
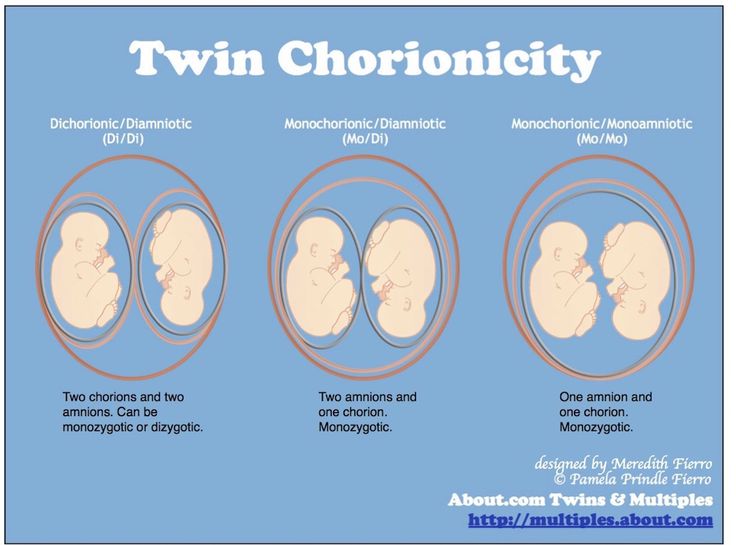
This image shows a normal placental location, with the placenta attached at the top of the uterus.How does the placenta work in twin pregnancies?
Fraternal twins come from separate eggs and each have their own placenta. Identical twins come from the same egg that separates, and they may share a placenta or have their own.
Can medicines cross the placenta?
Alcohol, nicotine, medicines and other drugs can cross the placenta and affect your baby’s health.
What should I do to keep my placenta healthy during pregnancy?
It’s important to visit your healthcare provider regularly during pregnancy.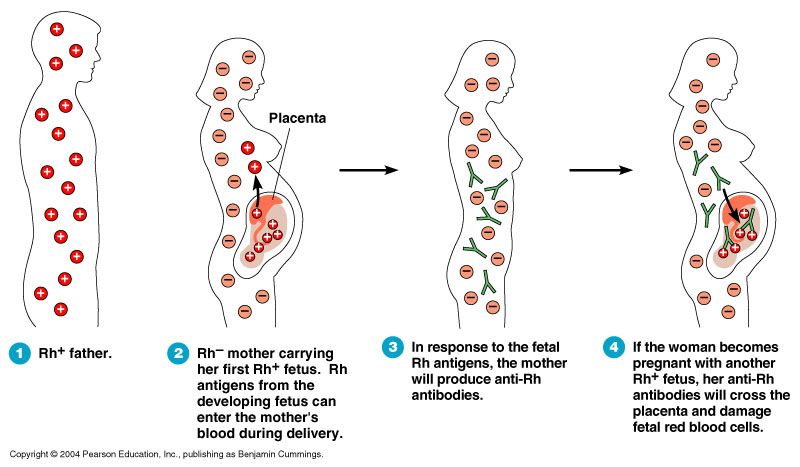 If there are complications, they can be identified during these appointments.
If there are complications, they can be identified during these appointments.
Tell your doctor if you have had problems with the placenta in a previous pregnancy, or if you have had any surgery to your uterus.
If you smoke, drink alcohol or take certain drugs during pregnancy, this increases the likelihood of problems with the placenta.
Always consult your doctor before you take any medicines, including over-the-counter medicines, natural therapies and supplements, while you are pregnant.
Speak with your doctor or midwife if you have any concerns, or if you experience:
- severe abdominal (stomach) pain or back pain
- vaginal bleeding
- contractions
- any trauma to your abdomen, for example from a fall or car accident
What happens to the placenta after my baby is born?
After your baby is born, you will need to birth your placenta. This is called the third stage of labour.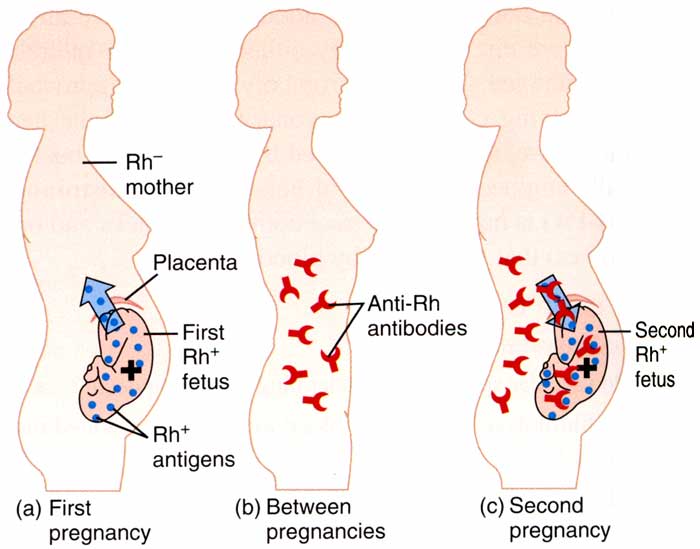 This stage of labour can be managed in different ways.
This stage of labour can be managed in different ways.
If you had a vaginal birth, you will usually have some mild contractions and need to give a few pushes to help your placenta to come out.
If you have a caesarean section, your doctor will remove the placenta at the same time your baby is born.
Once you birth your placenta your doctor or midwife will check that it looks complete. If there is any concern that your placenta isn’t complete, they may suggest further investigations. If any bits of placenta are retained (stay inside you), they may have to be surgically removed to prevent infection.
Can I take my placenta home with me?
It is your choice what you do with your placenta. You may choose to discard it; in which case your hospital or birthing centre will take care of this.
If you wish to take your placenta home, you can speak to your doctor or midwife to arrange this.
In some cultures, people bury the placenta in a special place.
‘Placentophagy’ is a practice where people cook and eat their placenta. There is no research to support health benefits from this. However, you may choose to do this for cultural, spiritual, or personal reasons.
There is no research to support health benefits from this. However, you may choose to do this for cultural, spiritual, or personal reasons.
Some commercial service providers offer to turn your placenta into capsules for you to swallow. It should be noted that there may be a risk of infection from poor preparation. These practices should be treated with caution.
Can anything go wrong with my placenta?
Problems with your placenta can happen during pregnancy, birth and after birth. These are potentially dangerous for both you and your baby.
If your bleeding is severe and you have significant pain, call triple zero (000) for an ambulance or go to your nearest hospital emergency department.
If you have any vaginal bleeding during pregnancy, it’s important to see your doctor as soon as possible.
Placental abruption is when some or all the placenta comes away from the wall of the uterus before your baby is born.
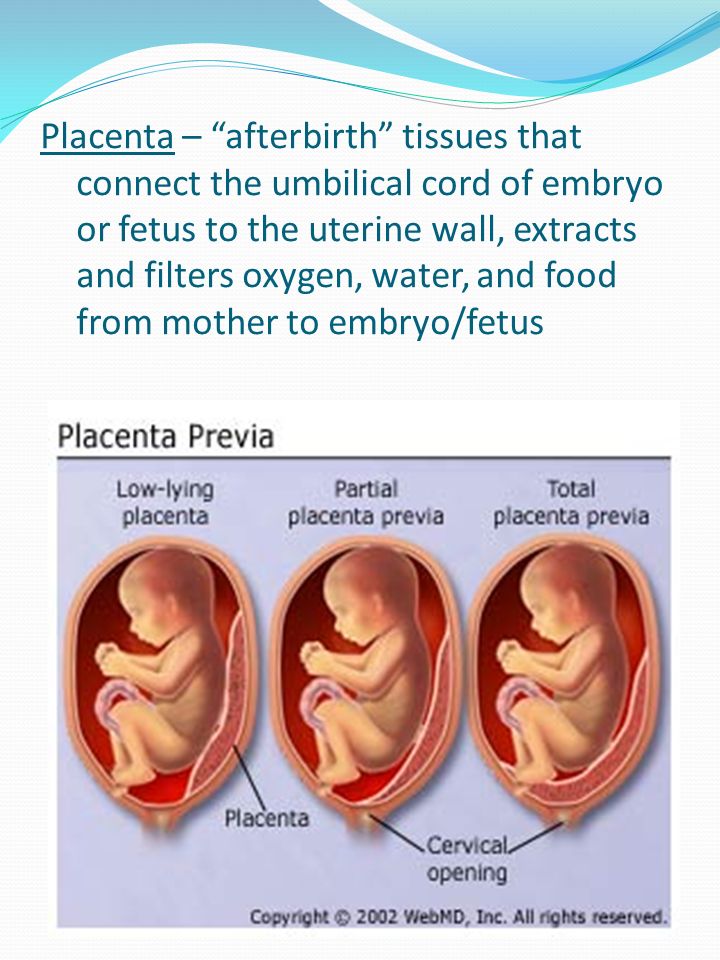
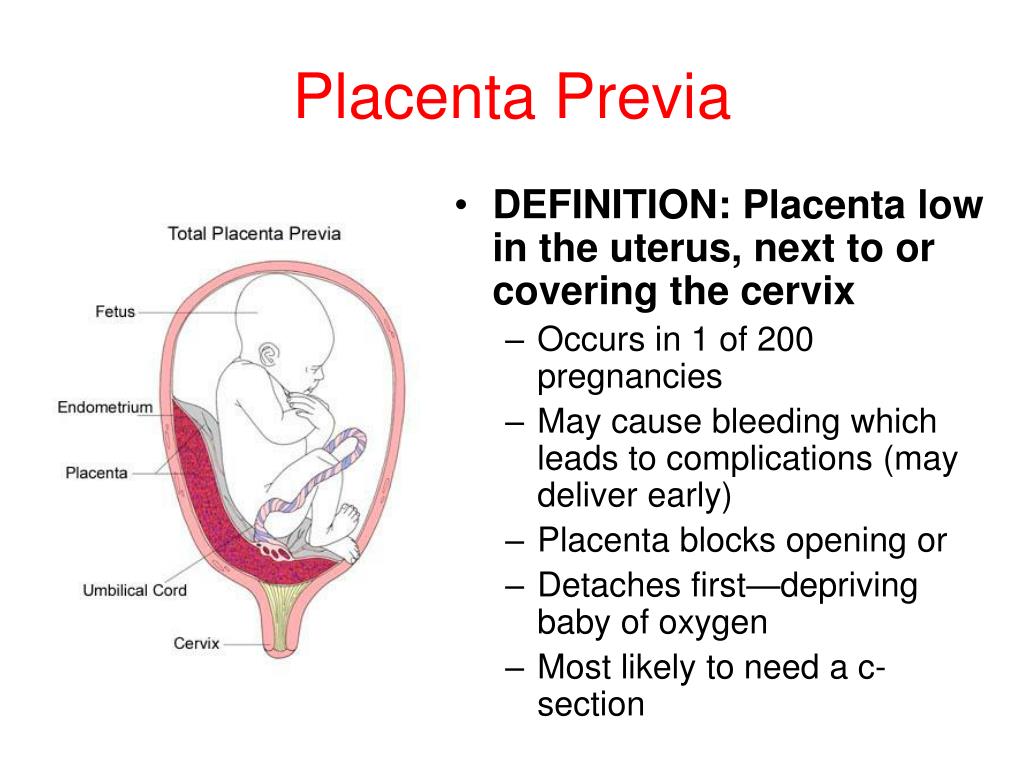
Placenta praevia is when the placenta partially or totally covers the cervix (the narrow opening in the uterus).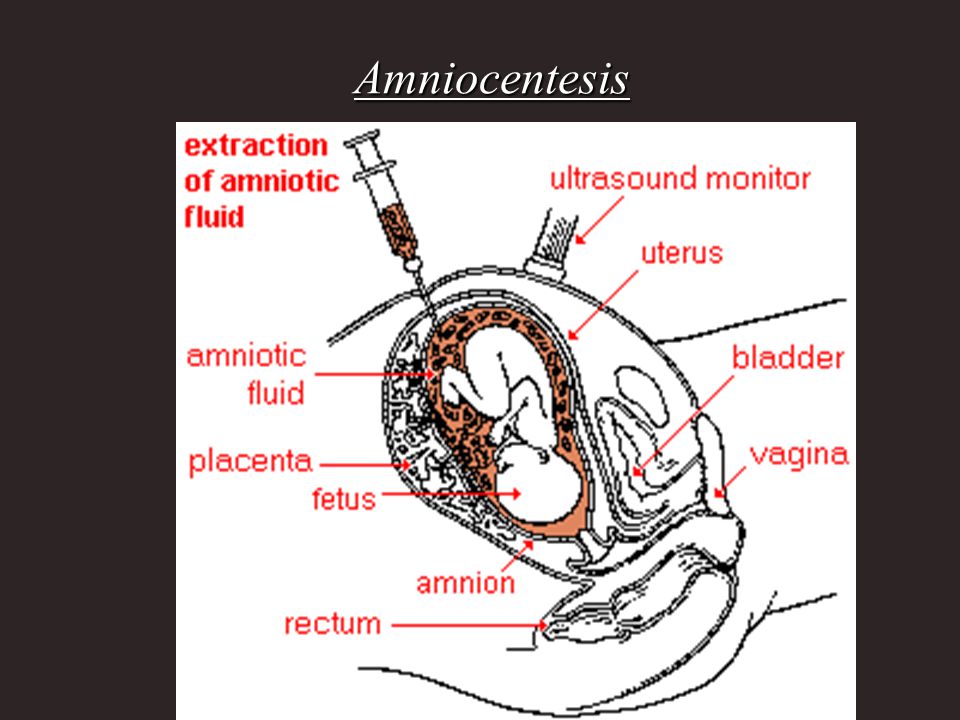
Placental insufficiency is when the placenta doesn’t work properly during pregnancy. It deprives the baby of oxygen and nutrients they need to grow and develop.
Placenta accreta is when the placenta grows too deeply into the wall of the uterus. This can lead to severe bleeding during or after delivery and can be life-threatening.
Retained placenta is when your placenta does not completely come out after the birth. This might be because it is stopped by your cervix or is still attached to your uterus.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
UNSW Embryology (KA02 Fetus or newborn affected by complications of placenta), Royal Women's Hospital (Placenta problems), RANZCOG (Intrauterine Growth Restriction: Screening, Diagnosis, and Management - Placenta accreta), The Royal Women’s Hospital Victoria Australia (Taking Your Placenta Home For Burial Or Consumption), International Journal of Women’s Health (Retained placenta after vaginal delivery: risk factors and management), NHS UK (What complications can affect the placenta?)Learn more here about the development and quality assurance of healthdirect content.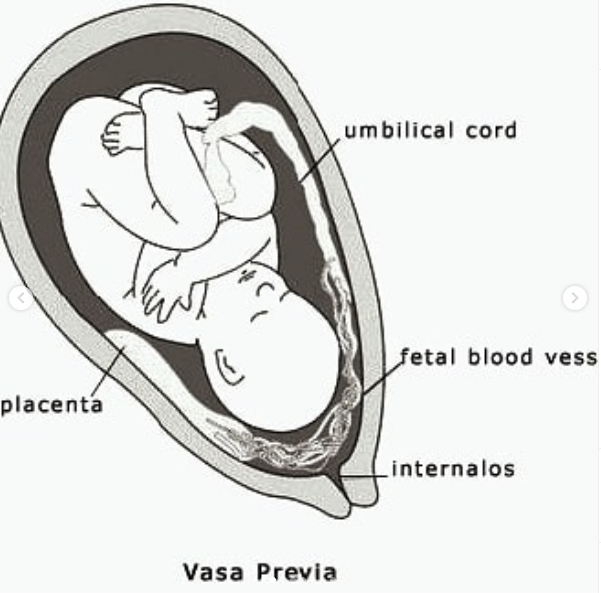
Last reviewed: July 2022
Back To Top
Related pages
- Giving birth - stages of labour
- Mum's first 24 hours after birth
Need more information?
Placenta previa - Better Health Channel
Placenta previa means the placenta has implanted at the bottom of the uterus, over the cervix or close by.
Read more on Better Health Channel website
Retained placenta
A retained placenta is when part or all of the placenta is not delivered after your baby is born. It can lead to serious infection or blood loss.
Read more on Pregnancy, Birth & Baby website
Placenta praevia
Placenta praevia is a condition where the placenta lies low and may cover the cervix, blocking the baby's exit during birth.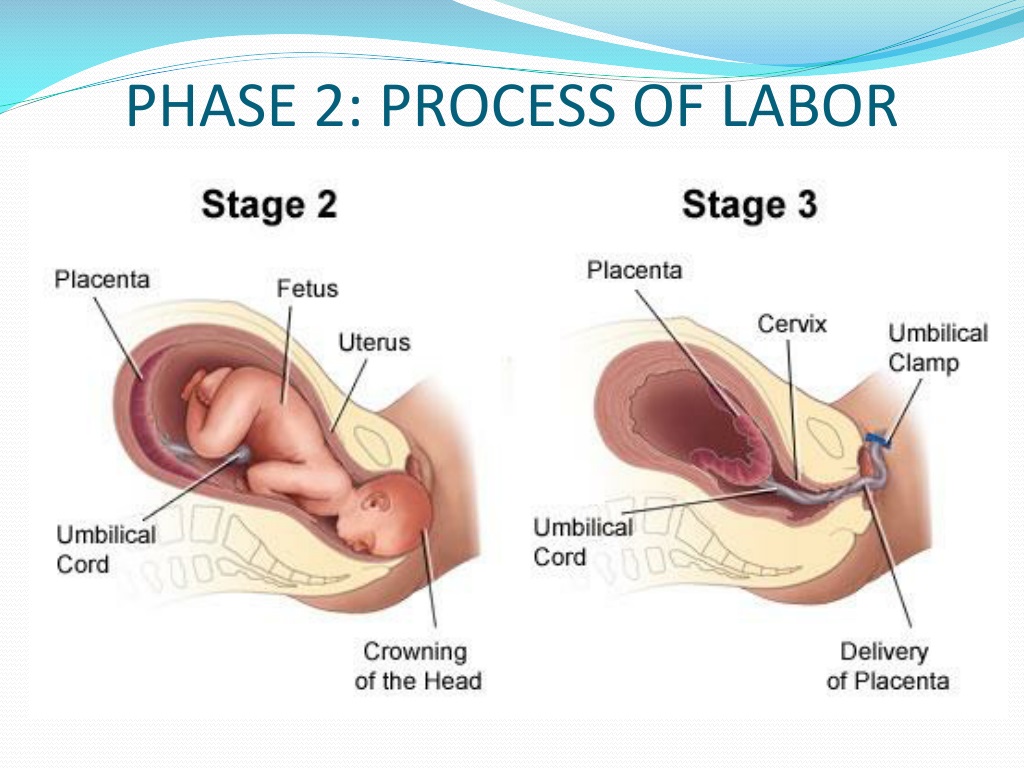
Read more on Pregnancy, Birth & Baby website
Placenta accreta
Placenta accreta is a serious but rare pregnancy complication that causes heavy bleeding. If you have it, you will need special care at the birth.
Read more on Pregnancy, Birth & Baby website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
It is not just a woman’s issue - Alcohol and Drug Foundation
If a woman drinks during pregnancy the alcohol crosses the placenta to the baby.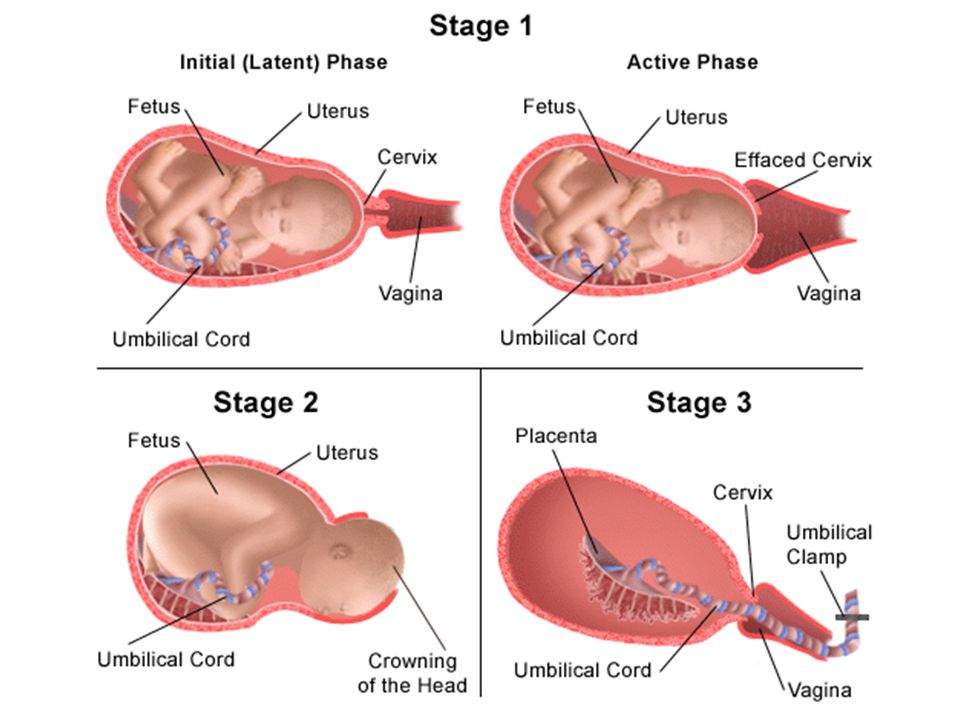 But what about the effect of alcohol on men?
But what about the effect of alcohol on men?
Read more on Alcohol and Drug Foundation website
Placental insufficiency
Find out about placental insufficiency - when the placenta does not work properly, and your baby doesn't get the oxygen and nutrients they need.
Read more on Pregnancy, Birth & Baby website
Placental abruption
Placental abruption is when some or all of the placenta peels away from the uterus wall before birth. It can deprive the baby of oxygen and nutrients.
Read more on Pregnancy, Birth & Baby website
Pregnancy test - Pathology Tests Explained
Starting approximately two weeks after conception, a hormone called human chorionic gonadatropin (hCG) hormone is produced by the developing placenta and can be detected in urine and in blood
Read more on Pathology Tests Explained website
4 weeks pregnant: Key points
When you are 4 weeks pregnant your body and your new baby are undergoing rapid changes.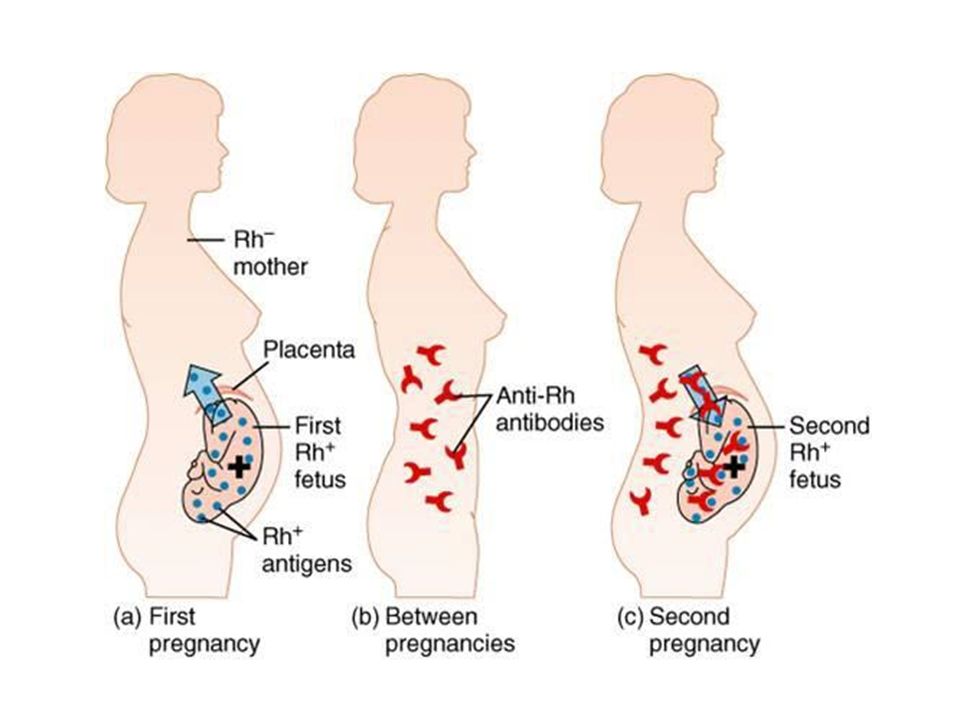 The placenta forms and begins producing a hormone called human chorionic gonadotrophin (hCG), which is the substance a pregnancy test detects to confirm you are pregnant. The cells which are growing into your new baby establish membranes which connect them to the placenta and prepare themselves for differentiation into different types of cells, which will occur next week when you are 5 weeks pregnant. These developments may cause you to experience unusual emotions and also cause changes in your body such as darkening of the areolas of your nipples.
The placenta forms and begins producing a hormone called human chorionic gonadotrophin (hCG), which is the substance a pregnancy test detects to confirm you are pregnant. The cells which are growing into your new baby establish membranes which connect them to the placenta and prepare themselves for differentiation into different types of cells, which will occur next week when you are 5 weeks pregnant. These developments may cause you to experience unusual emotions and also cause changes in your body such as darkening of the areolas of your nipples.
Read more on Parenthub website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.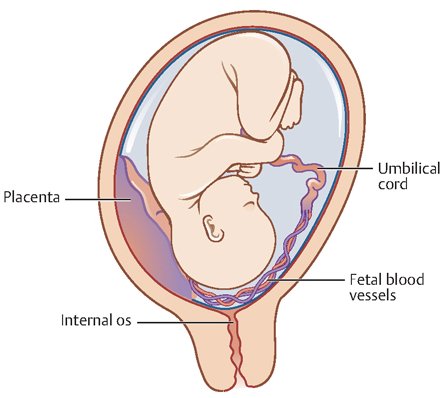
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Embryology, Placenta - StatPearls - NCBI Bookshelf
Introduction
The placenta is a vital organ with multiple functions, such as endocrine, immune, and physiological.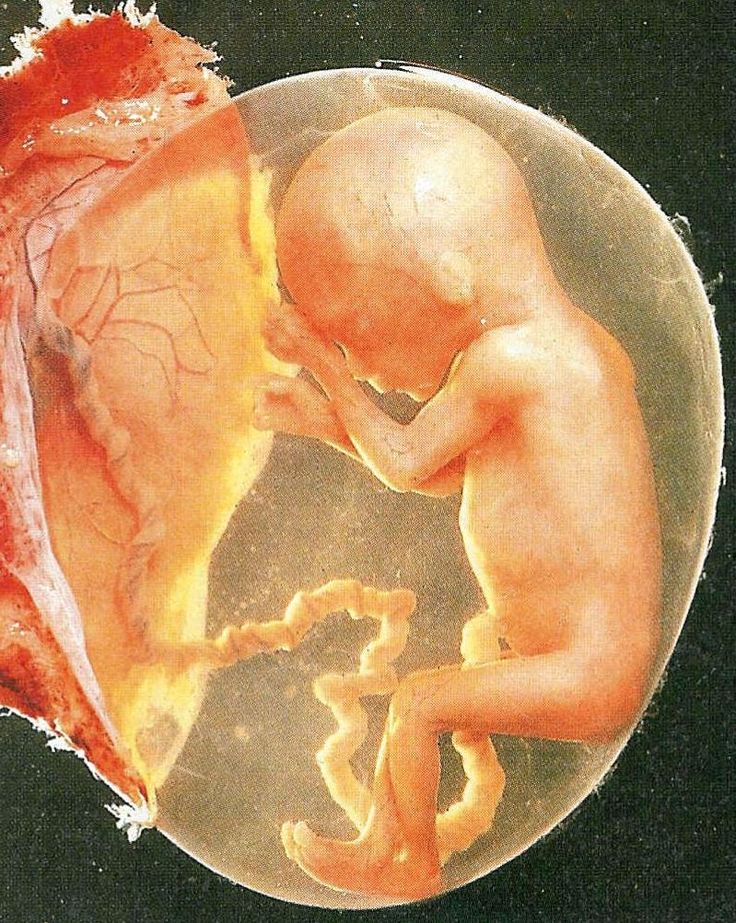 The placenta is formed gradually during the first three months of pregnancy, while, after the fourth month, it grows parallel to the development of the uterus. Once completed, it resembles a spongy disc 20 cm in diameter and 3 cm thick. It is a temporary organ, whose genetic characteristics are identical to those of the developing child. The placenta interacts with the environment in which it is present and vice versa. Proper development of the placenta is essential for a successful pregnancy. There are several layers of tissue that make up this delicate organ that need to develop normally for proper function during gestation. Without proper function, there can be devastating consequences to the pregnancy.
The placenta is formed gradually during the first three months of pregnancy, while, after the fourth month, it grows parallel to the development of the uterus. Once completed, it resembles a spongy disc 20 cm in diameter and 3 cm thick. It is a temporary organ, whose genetic characteristics are identical to those of the developing child. The placenta interacts with the environment in which it is present and vice versa. Proper development of the placenta is essential for a successful pregnancy. There are several layers of tissue that make up this delicate organ that need to develop normally for proper function during gestation. Without proper function, there can be devastating consequences to the pregnancy.
Development
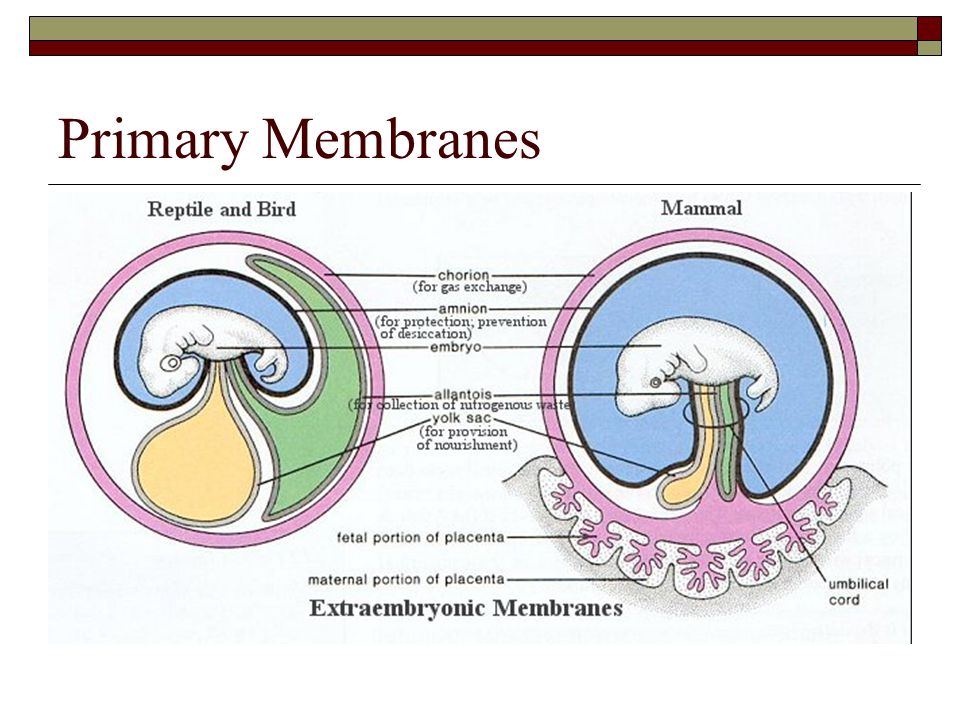
The placenta is a fetal organ made up of its parenchyma, chorion, amnion, and umbilical cord. The fetal structures form from the zygote and therefore separate the fetus from the endometrium. The fetal tissues form from the chorionic sac - which includes the amnion, chorion, yolk sac, and allantois.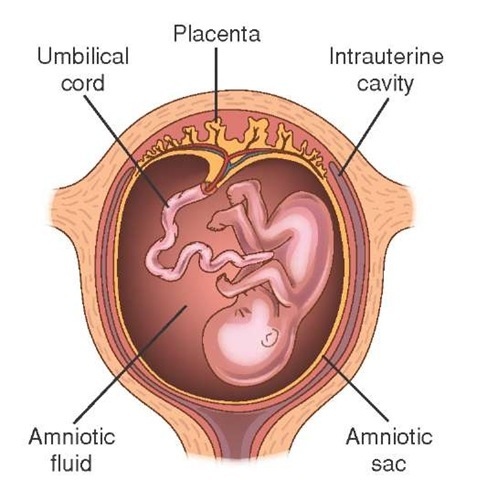 These tissues get delivered after birth. The maternal part comes from the endometrium and is called the decidua. There are three parts to the decidua - the decidua basalis (deep at the implantation site), the decidua capsularis (covers the implantation site), and the decidua parietalis (everything else).[1]
These tissues get delivered after birth. The maternal part comes from the endometrium and is called the decidua. There are three parts to the decidua - the decidua basalis (deep at the implantation site), the decidua capsularis (covers the implantation site), and the decidua parietalis (everything else).[1]
After fertilization, the fertilized ovum evolves into a morula, which will develop into the embryo and fetal placenta. The inner cell mass develops into the embryoblast, and the outer cell mass is the trophoblast. The morula then takes in fluid and forms a blastocyst with the trophoblast surrounding the inner cell mass and fluid. The blastocyst implants into the uterus approximately six days after fertilization. The contact of the trophoblast with the endometrium causes the development of the syncytiotrophoblast, which secretes human chorionic gonadotrophic hormone (hCG) and the cytotrophoblast which secretes enzymes that break down the bond between endometrial cells so the syncytiotrophoblast can invade the endometrial wall.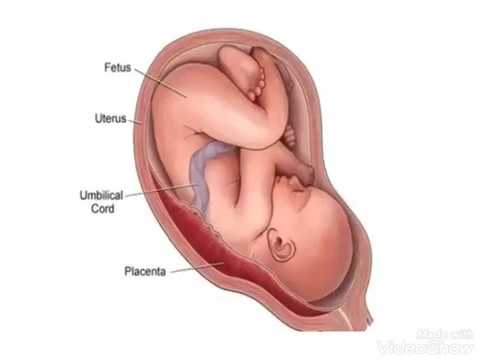 Both the cytotrophoblast and the syncytiotrophoblast are part of the chorion, which develops into the placenta along with the extraembryonic mesoderm.[2][3][4]
Both the cytotrophoblast and the syncytiotrophoblast are part of the chorion, which develops into the placenta along with the extraembryonic mesoderm.[2][3][4]
The chorion forms the placenta and consists of the syncytiotrophoblast, cytotrophoblast, and extraembryonic mesoderm. The cytotrophoblast grows into the syncytiotrophoblast as finger-like projections, which are called the primary chorionic villi. The extraembryonic mesoderm splits into somatic and splanchnic mesoderm, and the somatic mesoderm grows into the primary villi creating the secondary villi. The mesenchyme gives rise to blood cells and vessels, which designates tertiary villi when formed. Capillary beds grow from the villi, which connect to the embryo heart. Maternal blood flowing through the embryonic capillaries provide oxygen and nutrients to the fetus. The villi continue to grow and branch into the villus chorion, which is the fetal placenta.[5]
As development continues, cells from the cytotrophoblast continue to extend through the syncytiotrophoblast to eventually form a cytotrophoblastic shell.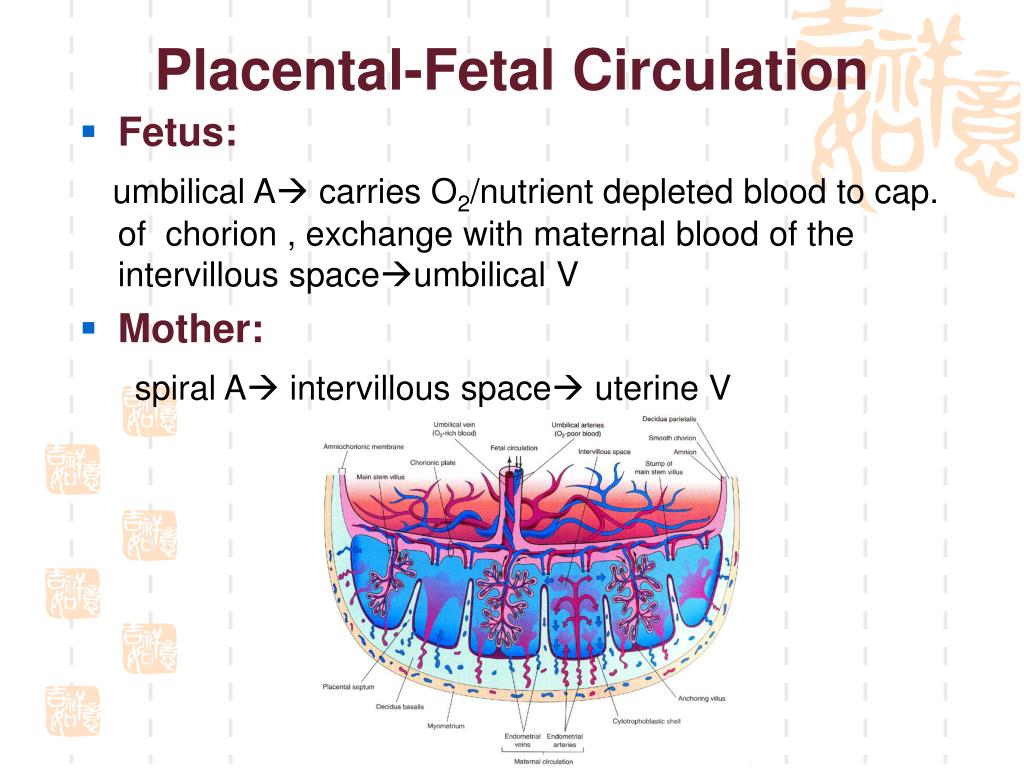 As progesterone increases, the decidua connective tissue develops into “decidua cells,” which help protect the uterus from an invasion of the syncytiotrophoblast. As the sac continues to grow, the decidua capsularis villi degenerate and eventually disappear as they fuse with the decidua parietalis.
As progesterone increases, the decidua connective tissue develops into “decidua cells,” which help protect the uterus from an invasion of the syncytiotrophoblast. As the sac continues to grow, the decidua capsularis villi degenerate and eventually disappear as they fuse with the decidua parietalis.
The amniotic sac enlarges faster than the chorionic sac, which causes them eventually to come into contact and fuse into the amniochorionic membrane. The amniochorionic membrane then fuses to the decidua capsularis and, ultimately, the decidua parietalis for stability. The amniochorionic membrane ruptures during labor. The amniochorionic membrane with the fetal vessels makes up the chorionic plate. Parts of the decidua basalis grow into the chorionic plate dividing it into separated septa called cotyledons, in which each contains stem villi.[6]
The fetomaternal junction provides stability for the chorion. The chorionic villi that attach to the decidua basalis are an anchor for the fetal chorionic sac to the endometrium. Endometrial vessels, called spiral arteries, make their way through openings in the cytotrophoblastic shell and reside inside the villi where they release maternal blood to bath the chorionic villi in each cotyledon; this allows for maternal blood to provide oxygen and nutrients to the fetus across the placental membrane. Endometrial veins then drain the blood. Although the fetal vessels are bathed in maternal blood, there is normally no mixing between maternal and fetal red blood cells.[7]
Endometrial vessels, called spiral arteries, make their way through openings in the cytotrophoblastic shell and reside inside the villi where they release maternal blood to bath the chorionic villi in each cotyledon; this allows for maternal blood to provide oxygen and nutrients to the fetus across the placental membrane. Endometrial veins then drain the blood. Although the fetal vessels are bathed in maternal blood, there is normally no mixing between maternal and fetal red blood cells.[7]
The placental membrane is where the mother and fetus exchange gases, nutrients, etc. The membrane forms by the syncytiotrophoblast, cytotrophoblast, embryonic connective tissue (Wharton’s jelly), and the endothelium of fetal blood vessels.
The umbilical cord serves to attach the fetus to the placenta and consists of two umbilical arteries and one umbilical vein.
Cellular
The placenta has several cellular structures to protect the health of the fetus. We can find substances that are part of the superfamily of ATP binding cassettes (ABC), such as multidrug resistance protein type 1, breast cancer resistance protein, multidrug-resistance like protein type 2 and 5.
The placenta can be considered an immune and endocrine organ. It produces many hormones and growth factors in autocrine and paracrine modalities, such as progesterone, corticotropin-releasing hormone, the human chorionic gonadotropin, the human placental lactogen, fibroblast growth factor, and many others.
Biochemical
The placenta has several metabolic functions that are vital for the healthy growth of a fetus. The placenta can make its own glycogen and cholesterol from mom’s glucose and fatty acids, respectively. The glycogen gets stored as energy for the fetus, and the cholesterol is used to make hormones such as progesterone, estrogen, and glucocorticoids. It also synthesizes peptide hormones such as human chorionic gonadotropin (hCG) and human placental lactogen (hPL), growth hormone (GH), vascular endothelial growth factor (VEGF), corticotropin-releasing hormone (CRH), insulin-like growth factor (IGF), placental growth factor (PIGF), and cytokines.[8][9]
Molecular
Several molecules interact with the placenta.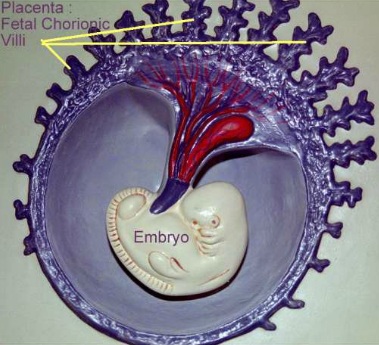 For example, leptin ensures the health of the placenta, thanks to its actions as a homeostatic agent, proliferation, and protein synthesis, as an anti-apoptotic molecule. In turn, leptin is under the control of other substances, such as insulin, many growth factors, human chorionic gonadotropin, steroids, and hypoxia.
For example, leptin ensures the health of the placenta, thanks to its actions as a homeostatic agent, proliferation, and protein synthesis, as an anti-apoptotic molecule. In turn, leptin is under the control of other substances, such as insulin, many growth factors, human chorionic gonadotropin, steroids, and hypoxia.
Function
The placenta is the means of communication between mom and fetus. The placental membrane is where the exchange of substances happens between mother and fetus. This exchange is essential for the transfer of gases, electrolytes, hormones, maternal antibodies, fetal waste, and nutrition such as water, amino acids, glucose, vitamins, and free fatty acids. Fetal waste includes urea, uric acid, and bilirubin. Alpha-fetoprotein and other proteins also get exchanged. These transfers are beneficial to the fetus, but many harmful substances can pass through the placental membrane such as certain drugs, live vaccines, carbon monoxide, anti-Rh antibodies, and several infectious agents (“ToRCHes” infections).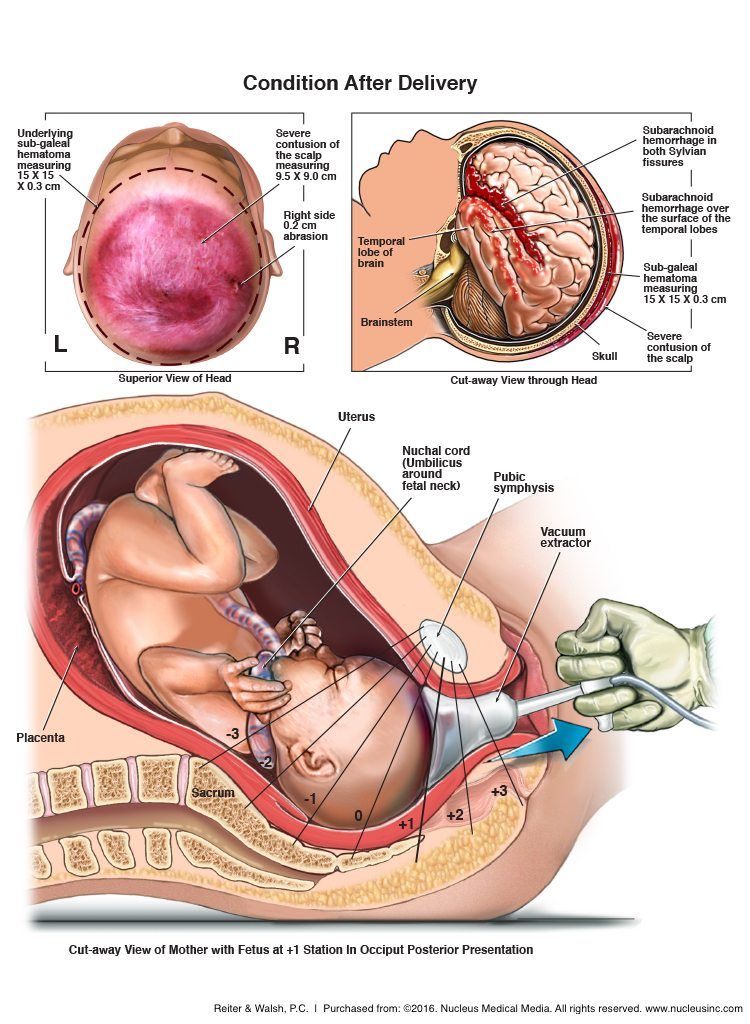 [10][11] Solvent drag is the bulk flow of water, which brings in nutrients across the placental membrane into each cotyledon to be absorbed. The higher the pressure, the more nutrients that will be absorbed.[12] Solutes and gases are absorbed by simple diffusion depending on their molecular makeup and properties. Oxygen and carbon dioxide are highly permeable across the placental tissues due to their lipophilicity. Their exchange is perfusion limited, which can cause fetal growth restriction if there is tissue hypoxia.[13] The placenta also uses channels for ion transport down their electrochemical gradient, facilitated diffusion for glucose using carrier proteins, and active transport for several solutes.[14]
[10][11] Solvent drag is the bulk flow of water, which brings in nutrients across the placental membrane into each cotyledon to be absorbed. The higher the pressure, the more nutrients that will be absorbed.[12] Solutes and gases are absorbed by simple diffusion depending on their molecular makeup and properties. Oxygen and carbon dioxide are highly permeable across the placental tissues due to their lipophilicity. Their exchange is perfusion limited, which can cause fetal growth restriction if there is tissue hypoxia.[13] The placenta also uses channels for ion transport down their electrochemical gradient, facilitated diffusion for glucose using carrier proteins, and active transport for several solutes.[14]
Due to its multiple nutritional properties, many mammals besides humans, have the habit of eating the expelled placenta after giving birth.
Mechanism
Fetal circulation flows from the fetus to the two umbilical arteries (deoxygenated), then to chorionic arteries in the cotyledons, through the capillary beds to exchange gases with maternal blood, then back to the fetus via a single umbilical vein (oxygenated).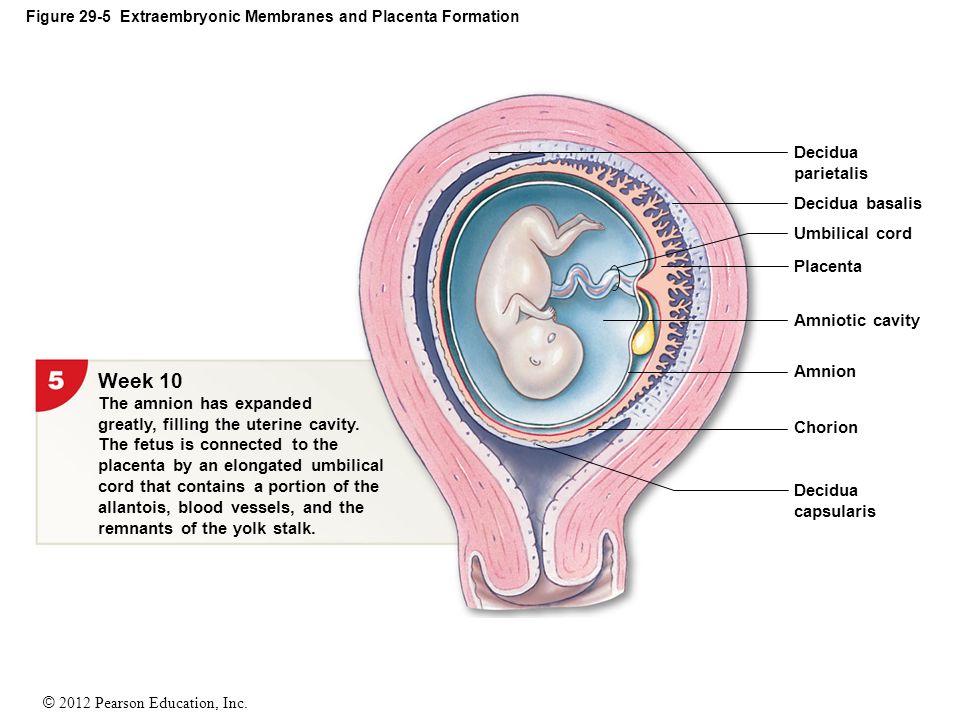
Testing
Chorionic villus sampling (CVS) is either a transabdominal or transcervical procedure where clinicians take samples of the placenta at 10 to 13 weeks of gestation for genetic testing. This test is beneficial because it can be done much earlier than amniocentesis and therefore receive screening results earlier. If the results lead to termination of the pregnancy, there are fewer risks than later termination. Earlier gestation also causes less accurate results. The procedure complications can include infection, bleeding, fetal injury, and fetal death.[15][16]
Amniocentesis is a similar transabdominal procedure where amniotic fluid gets sampled for genetic testing. This procedure can take place at any time after 15 weeks. Amniotic fluid contains cells and substances that are created by the fetus, which can be measured to assess for disorders such as Down syndrome, infection, neural tube defects, fetal blood type determination, and lung development. The risks are similar to CVS, including infection, injury to the fetus or fetal death, and leakage of amniotic fluid.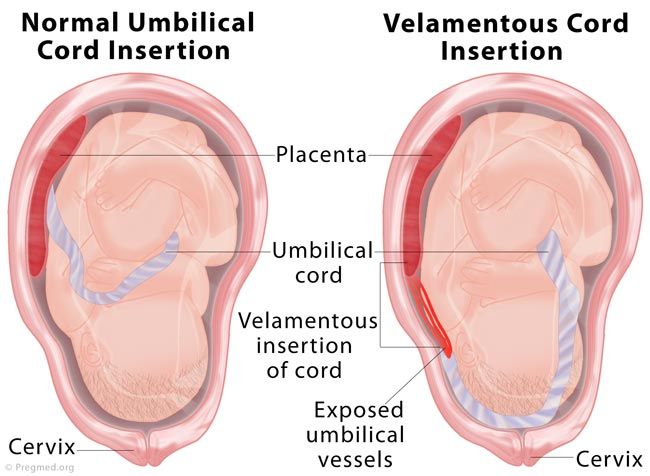 [17]
[17]
Pathophysiology
Normally, there is no mixing of fetal and maternal blood. Although, this is possible with specific infectious agents or small breaks in the placental membrane that can happen during parturition. If there are breaks in the membrane, maternal red blood cells are able to cross into the fetal circulation and vice versa. Treponema pallidum (syphilis infection) can cross the barrier without breaks in the membrane. Toxoplasma gondii (toxoplasma infection) can create its own breaks in the membrane to get across into fetal circulation and infect the fetus.
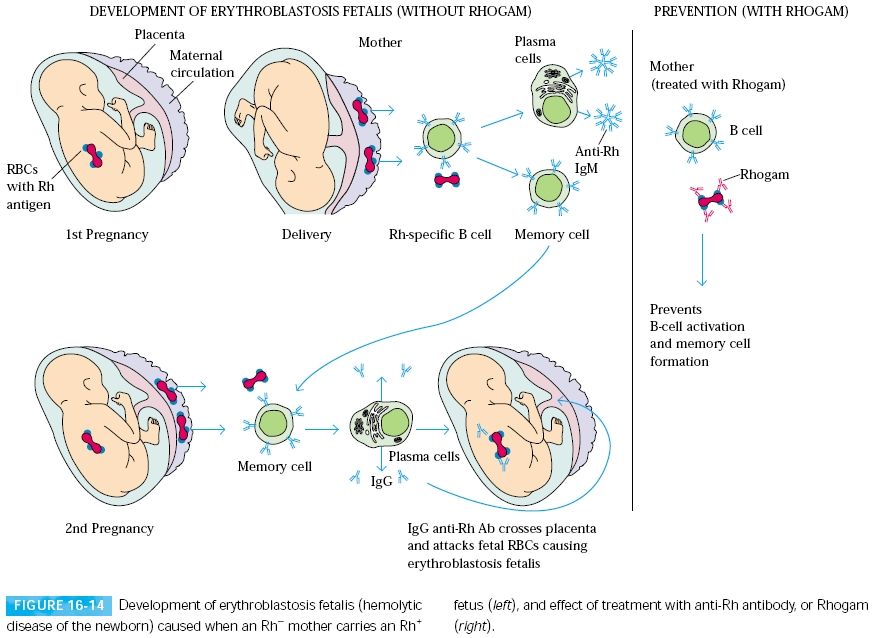
Erythroblastosis fetalis, also referred to as hemolytic disease of the newborn, happens when the mother makes antibodies to the fetus’s Rh factor after an Rh-negative mother becomes exposed to the fetus’s Rh-positive blood. The mom makes IgG anti-Rh antibodies, which can cross the placenta. The first pregnancy is not an issue because it takes time for mom to elicit this response, but can cause problems in future pregnancies with an Rh-positive fetus.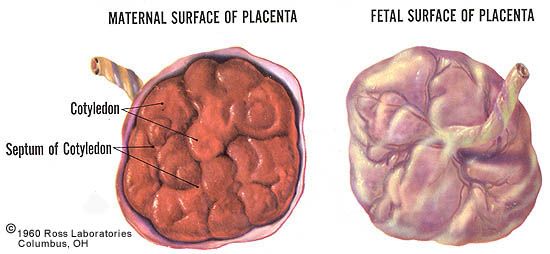 The antibodies can cross the placenta and attack the fetal red blood cells, causing fetal hydrops (anemia and edema).[18]
The antibodies can cross the placenta and attack the fetal red blood cells, causing fetal hydrops (anemia and edema).[18]
Placenta accreta is when the placenta grows too far into the myometrium due to a lack of decidua, which allows the villi to anchor to the myometrium. In placenta increta, the villi bury even deeper into the myometrium. Placenta percreta is when the placenta grows through the full thickness of the myometrium and reaches the serosa of the uterus. This invasion of myometrium can cause bleeding during pregnancy and bleeding complications postpartum.[19][20]
A healthy umbilical cord should contain two umbilical arteries and one umbilical vein. If there is only one artery, there may be other defects present in the fetus, such as growth restriction or genetic abnormalities.[21] There can also be multiple arteries, which may also be associated with genetic abnormalities or congenital defects.[22] There can also be cysts in the umbilical cord filled with fluid. They are visible on ultrasound throughout the pregnancy.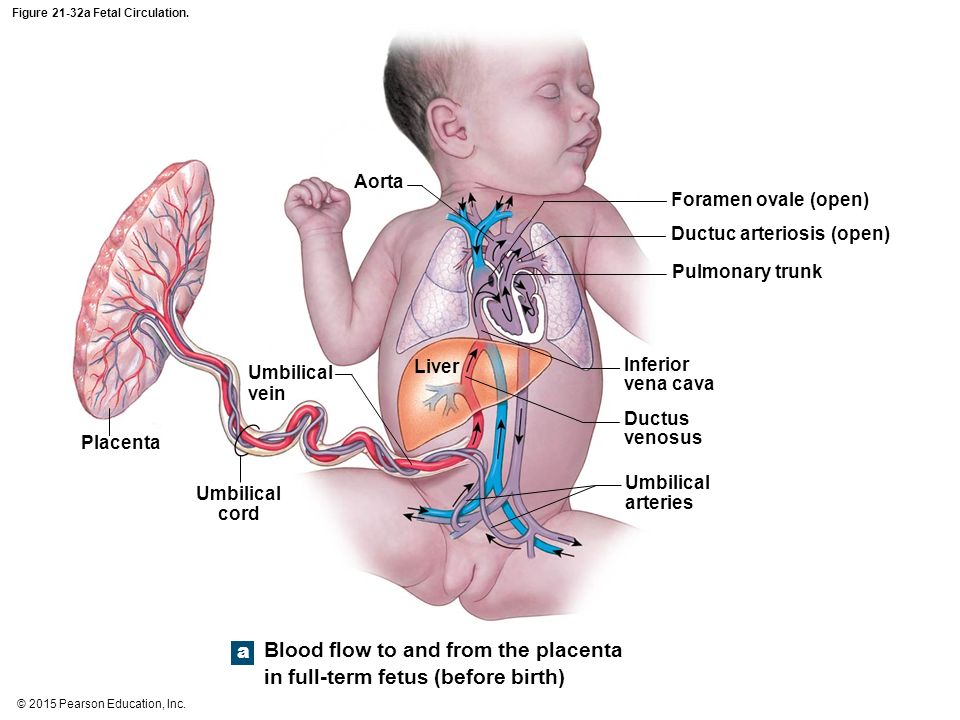 [23] Cysts may resolve on their own, or if there are multiple cysts, there may also be chromosomal abnormalities.[24] A rare complication from a cyst could be torsion or hematoma that could potentially cause fetal death.[25] True and false knots are also an abnormality of the umbilical cord. A false knot is when the vessels inside the cord become tortuous, but there is no knot in the cord itself. There is no adverse outcome associated with this type of knot. A true knot, however, can be dangerous to the fetus. A true knot is where the cord actually twists into a knot, which could potentially cause fetal demise if it is too tight.[26][27]
[23] Cysts may resolve on their own, or if there are multiple cysts, there may also be chromosomal abnormalities.[24] A rare complication from a cyst could be torsion or hematoma that could potentially cause fetal death.[25] True and false knots are also an abnormality of the umbilical cord. A false knot is when the vessels inside the cord become tortuous, but there is no knot in the cord itself. There is no adverse outcome associated with this type of knot. A true knot, however, can be dangerous to the fetus. A true knot is where the cord actually twists into a knot, which could potentially cause fetal demise if it is too tight.[26][27]
The umbilical cord normally attaches to the center of the placenta. The umbilical cord can implant abnormally both in the fetus and the placenta. In the placenta, there can be a velamentous insertion or a marginal insertion. A velamentous insertion is when the vessels separate as they develop between the amnion and chorion as they grow toward the placenta.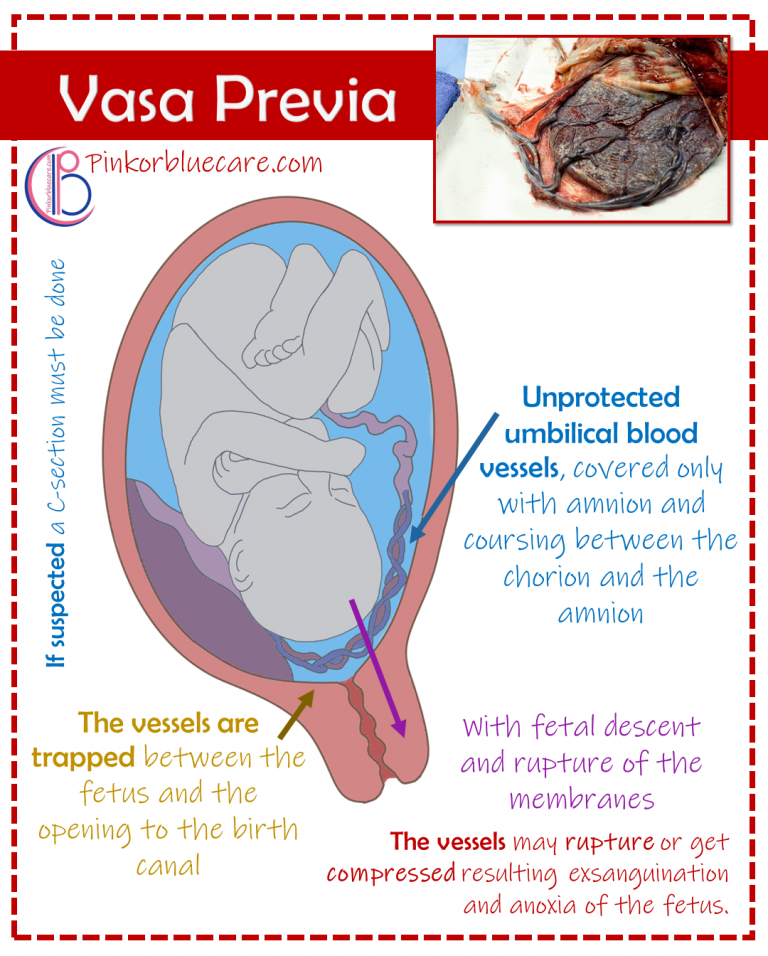 As they get closer to the placenta, they are exposed and not protected by Wharton’s jelly; this can be dangerous, especially in vasa previa where the vessels are especially prone to rupture.[28] Marginal insertion is where the cord inserts on the edge of the placenta. There is still an increased risk of placenta previa and abruption but not quite as high as a velamentous insertion.[29][30]
As they get closer to the placenta, they are exposed and not protected by Wharton’s jelly; this can be dangerous, especially in vasa previa where the vessels are especially prone to rupture.[28] Marginal insertion is where the cord inserts on the edge of the placenta. There is still an increased risk of placenta previa and abruption but not quite as high as a velamentous insertion.[29][30]
Many pathologies of the placenta are visible on histological examination, but some pathologies are visible grossly.[31] Gross pathologies include meconium myonecrosis green discoloration, vasculitis yellow-green discoloration, abscesses, placental infarction orange discoloration, masses, cysts, thrombi, and incomplete tissue collection indicating retained placenta. The placenta may be stored fresh in a refrigerator or placed in fixative if needed for further examination after parturition.[11][32]
The detachment of the placenta is a very dangerous circumstance: if it happens, in fact, the placenta detaches from the uterus causing a strong haemorrhage, putting not only the life of the fetus at risk, which does not receive more oxygen and nutrients needed to survive but also of the expectant mother.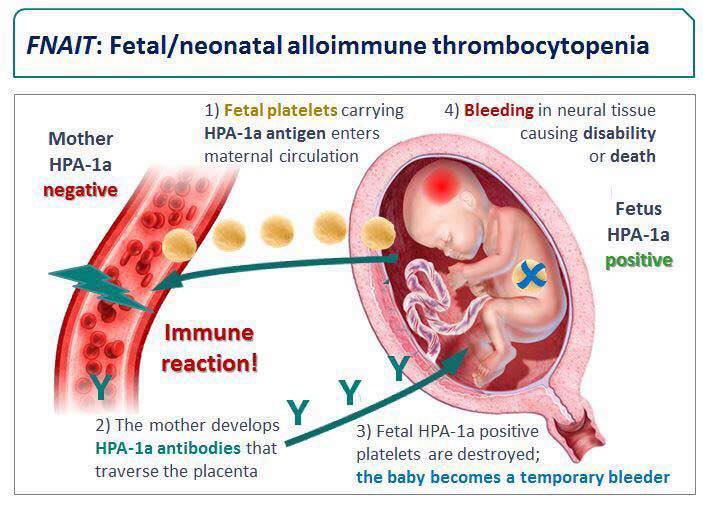 Placental detachment may be due to: hypertension, overdistention of uterine walls due to excess of amniotic fluid (polyhydramnios), multi-twin pregnancy, diabetes, drug use.
Placental detachment may be due to: hypertension, overdistention of uterine walls due to excess of amniotic fluid (polyhydramnios), multi-twin pregnancy, diabetes, drug use.
Clinical Significance
The placenta is a vital fetal organ necessary for a healthy pregnancy for both mother and fetus. Incomplete or disordered development of the placenta may cause fetal abnormalities or adverse events in the mother as well. An early gestational sampling of the placenta can be done to test for fetal anomalies, but these procedures do not come without risk to the wellbeing of the fetus. In the case of an abnormal delivery or fetal defects, the placenta can undergo examination for gross and histological analysis.
Most placental diseases can have treatment by preserving the pregnant woman and the fetus from serious consequences. Placenta previa: often, a low placenta returns to its normal position after a few weeks, thanks to the push of the uterus. Where the condition of the low placenta remains throughout the pregnancy, a cesarean section is a strong recommendation.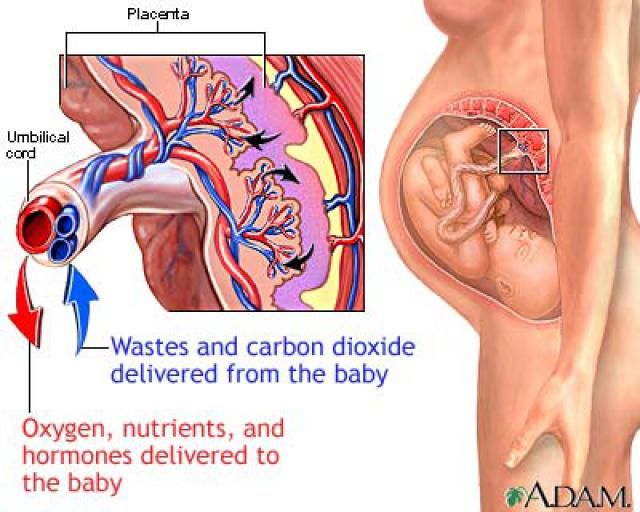 Placenta accreta: to prevent the risk of hemorrhage, an early cesarean section of a few weeks is recommended. In these cases, a hysterectomy, or removal of the uterus without precluding future pregnancies, cannot be excluded. Aged placenta: a diet based on vitamins and calcium and good habits (for example, not smoking) prevents the calcification of the placenta. Placental insufficiency: there is no specific treatment for this type of problem. It is good to undergo periodic checks close to each other to monitor the evolution of the fetus, as well as where it is possible, treat the behavior or pathology of the pregnant woman. Placental detachment: depending on the type of detachment, the hypothesis of monitoring the patient by asking for absolute rest or, as in most cases, proceeding with cesarean section, depending on the time of pregnancy, will be evaluated.
Placenta accreta: to prevent the risk of hemorrhage, an early cesarean section of a few weeks is recommended. In these cases, a hysterectomy, or removal of the uterus without precluding future pregnancies, cannot be excluded. Aged placenta: a diet based on vitamins and calcium and good habits (for example, not smoking) prevents the calcification of the placenta. Placental insufficiency: there is no specific treatment for this type of problem. It is good to undergo periodic checks close to each other to monitor the evolution of the fetus, as well as where it is possible, treat the behavior or pathology of the pregnant woman. Placental detachment: depending on the type of detachment, the hypothesis of monitoring the patient by asking for absolute rest or, as in most cases, proceeding with cesarean section, depending on the time of pregnancy, will be evaluated.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
Figure
Development of the Fetal membrane and the Placenta, Diagram showing the expansion of amnion and delimitation of the umbilicus, Heart, Fore-gut, Embryo, Amniotic cavity, Placental villi. Contributed by Gray's Anatomy Plates
Figure
Development of the Fetal membrane and the Placenta, Diagram of a transverse section, showing the mode of formation of the amnion in the chick. The amniotic folds have nearly united in the middle line, Ectoderm is blue is the mesoderm; red is the entoderm (more...)
Figure
Development of the Fetal Membranes and Placenta, Model of human embryo 1.3 mm long, Neurenteric Canal, Neural Groove, Amnion, Body-stalk, Vitelline veins, Entoderm, Splanchnic mesoderm, Yolk sac, Somatic Mesoderm. Contributed by Gray's Anatomy Plates (more...)
Figure
Development of the Fetal Membranes and Placenta, Scheme of Placental circulation, Marginal sinus, Chorion, Amnion, Trophoblast, Umbilical Arteries and Veins in the Cord.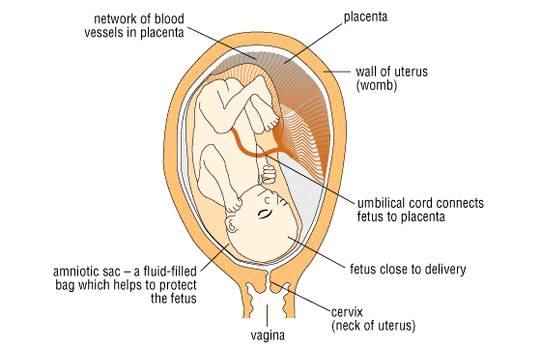 Contributed by Gray's Anatomy Plates
Contributed by Gray's Anatomy Plates
Figure
The figure shows a human placenta. Contributed by Bruno Bordoni, PhD.
References
- 1.
Burton GJ, Jauniaux E. What is the placenta? Am J Obstet Gynecol. 2015 Oct;213(4 Suppl):S6.e1, S6-8. [PubMed: 26428504]
- 2.
Guttmacher AE, Maddox YT, Spong CY. The Human Placenta Project: placental structure, development, and function in real time. Placenta. 2014 May;35(5):303-4. [PMC free article: PMC3999347] [PubMed: 24661567]
- 3.
Wamaitha SE, Niakan KK. Human Pre-gastrulation Development. Curr Top Dev Biol. 2018;128:295-338. [PubMed: 29477167]
- 4.
Maître JL. Mechanics of blastocyst morphogenesis. Biol Cell. 2017 Sep;109(9):323-338. [PubMed: 28681376]
- 5.
Solnica-Krezel L, Sepich DS. Gastrulation: making and shaping germ layers. Annu Rev Cell Dev Biol. 2012;28:687-717. [PubMed: 22804578]
- 6.
Favaron PO, Carvalho RC, Borghesi J, Anunciação AR, Miglino MA.
 The Amniotic Membrane: Development and Potential Applications - A Review. Reprod Domest Anim. 2015 Dec;50(6):881-92. [PubMed: 26510939]
The Amniotic Membrane: Development and Potential Applications - A Review. Reprod Domest Anim. 2015 Dec;50(6):881-92. [PubMed: 26510939]- 7.
Labarrere CA, DiCarlo HL, Bammerlin E, Hardin JW, Kim YM, Chaemsaithong P, Haas DM, Kassab GS, Romero R. Failure of physiologic transformation of spiral arteries, endothelial and trophoblast cell activation, and acute atherosis in the basal plate of the placenta. Am J Obstet Gynecol. 2017 Mar;216(3):287.e1-287.e16. [PMC free article: PMC5881902] [PubMed: 28034657]
- 8.
Hahn D, Blaschitz A, Korgun ET, Lang I, Desoye G, Skofitsch G, Dohr G. From maternal glucose to fetal glycogen: expression of key regulators in the human placenta. Mol Hum Reprod. 2001 Dec;7(12):1173-8. [PubMed: 11719595]
- 9.
Herrera E, Amusquivar E, López-Soldado I, Ortega H. Maternal lipid metabolism and placental lipid transfer. Horm Res. 2006;65 Suppl 3:59-64. [PubMed: 16612115]
- 10.
Neu N, Duchon J, Zachariah P.
 TORCH infections. Clin Perinatol. 2015 Mar;42(1):77-103, viii. [PubMed: 25677998]
TORCH infections. Clin Perinatol. 2015 Mar;42(1):77-103, viii. [PubMed: 25677998]- 11.
Kaplan C. Gross Examination of the Placenta. Surg Pathol Clin. 2013 Mar;6(1):1-26. [PubMed: 26838700]
- 12.
Brownbill P, Mahendran D, Owen D, Swanson P, Thornburg KL, Nelson DM, Sibley CP. Denudations as paracellular routes for alphafetoprotein and creatinine across the human syncytiotrophoblast. Am J Physiol Regul Integr Comp Physiol. 2000 Mar;278(3):R677-83. [PubMed: 10712288]
- 13.
Carter AM. Factors affecting gas transfer across the placenta and the oxygen supply to the fetus. J Dev Physiol. 1989 Dec;12(6):305-22. [PubMed: 2701106]
- 14.
Sibley CP, Brownbill P, Glazier JD, Greenwood SL. Knowledge needed about the exchange physiology of the placenta. Placenta. 2018 Apr;64 Suppl 1:S9-S15. [PubMed: 29370939]
- 15.
Wapner RJ. Chorionic villus sampling. Obstet Gynecol Clin North Am. 1997 Mar;24(1):83-110.
 [PubMed: 9086520]
[PubMed: 9086520]- 16.
Sileo FG, Curado J, Bhide A. A survey of current clinical practice of chorionic villus sampling. Prenat Diagn. 2019 Mar;39(4):299-302. [PubMed: 30682214]
- 17.
Baird PA, Yee IM, Sadovnick AD. Population-based study of long-term outcomes after amniocentesis. Lancet. 1994 Oct 22;344(8930):1134-6. [PubMed: 7934498]
- 18.
ALLEN FH, DIAMOND LK. Erythroblastosis fetalis. N Engl J Med. 1957 Oct 10;257(15):705-12 contd. [PubMed: 13477375]
- 19.
Khong TY. The pathology of placenta accreta, a worldwide epidemic. J Clin Pathol. 2008 Dec;61(12):1243-6. [PubMed: 18641410]
- 20.
Piñas Carrillo A, Chandraharan E. Placenta accreta spectrum: Risk factors, diagnosis and management with special reference to the Triple P procedure. Womens Health (Lond). 2019 Jan-Dec;15:1745506519878081. [PMC free article: PMC6777059] [PubMed: 31578123]
- 21.
Ghezzi F, Raio L, Di Naro E, Franchi M, Cromi A, Dürig P.
 Single and multiple umbilical cord cysts in early gestation: two different entities. Ultrasound Obstet Gynecol. 2003 Mar;21(3):215-9. [PubMed: 12666213]
Single and multiple umbilical cord cysts in early gestation: two different entities. Ultrasound Obstet Gynecol. 2003 Mar;21(3):215-9. [PubMed: 12666213]- 22.
Beck R, Naulty CM. A human umbilical cord with four arteries. Clin Pediatr (Phila). 1985 Feb;24(2):118-9. [PubMed: 3967448]
- 23.
Aoki S, Hata T, Ariyuki Y, Makihara K, Hata K, Kitao M. Antenatal diagnosis of aberrant umbilical vessels. Gynecol Obstet Invest. 1997;43(4):232-5. [PubMed: 9194620]
- 24.
Sepulveda W, Reyes M, Gonçalves LF. Two uncommon umbilical vessel anomalies in a fetus with trisomy 18. Prenat Diagn. 1998 Oct;18(10):1098-9. [PubMed: 9826906]
- 25.
Sepulveda W, Wong AE, Gonzalez R, Vasquez P, Gutierrez J. Fetal death due to umbilical cord hematoma: a rare complication of umbilical cord cyst. J Matern Fetal Neonatal Med. 2005 Dec;18(6):387-90. [PubMed: 16390804]
- 26.
Gembruch U, Baschat AA. True knot of the umbilical cord: transient constrictive effect to umbilical venous blood flow demonstrated by Doppler sonography.
 Ultrasound Obstet Gynecol. 1996 Jul;8(1):53-6. [PubMed: 8843621]
Ultrasound Obstet Gynecol. 1996 Jul;8(1):53-6. [PubMed: 8843621]- 27.
Hertzberg BS, Bowie JD, Bradford WD, Bolick D. False knot of the umbilical cord: sonographic appearance and differential diagnosis. J Clin Ultrasound. 1988 Oct;16(8):599-602. [PubMed: 3152409]
- 28.
Rocha J, Carvalho J, Costa F, Meireles I, do Carmo O. Velamentous cord insertion in a singleton pregnancy: an obscure cause of emergency cesarean-a case report. Case Rep Obstet Gynecol. 2012;2012:308206. [PMC free article: PMC3517836] [PubMed: 23243528]
- 29.
Nkwabong E, Njikam F, Kalla G. Outcome of pregnancies with marginal umbilical cord insertion. J Matern Fetal Neonatal Med. 2021 Apr;34(7):1133-1137. [PubMed: 31164018]
- 30.
Ebbing C, Kiserud T, Johnsen SL, Albrechtsen S, Rasmussen S. Prevalence, risk factors and outcomes of velamentous and marginal cord insertions: a population-based study of 634,741 pregnancies. PLoS One. 2013;8(7):e70380.
 [PMC free article: PMC3728211] [PubMed: 23936197]
[PMC free article: PMC3728211] [PubMed: 23936197]- 31.
Kaplan CG. Gross pathology of the placenta: weight, shape, size, colour. J Clin Pathol. 2008 Dec;61(12):1285-95. [PubMed: 18708423]
- 32.
Roberts DJ. Placental pathology, a survival guide. Arch Pathol Lab Med. 2008 Apr;132(4):641-51. [PubMed: 18384216]
Makarov I.O. • Placenta and its role in the development of pregnancy
Ultrasound scanner HS60
Professional diagnostic tools. Tissue elasticity assessment, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiac examinations.
From the very beginning of pregnancy and up to its end, the mother-placenta-fetus system is formed and functions . The most important component of this system is placenta , which is a complex organ, in the formation of which derivatives of the trophoblast and embryoblast , as well as decidual tissue take part. The function of the placenta, first of all, is aimed at providing sufficient conditions for the physiological course of pregnancy and the normal development of the fetus. These functions include: respiratory, nutritional, excretory, protective, endocrine. All metabolic, hormonal, immune processes during pregnancy are provided through maternal and fetal vascular system . Despite the fact that the blood of the mother and fetus does not mix, since their is separated by the placental barrier , the fetus receives all the necessary nutrients and oxygen from the mother's blood. The main structural component of the placenta is villous tree .
The function of the placenta, first of all, is aimed at providing sufficient conditions for the physiological course of pregnancy and the normal development of the fetus. These functions include: respiratory, nutritional, excretory, protective, endocrine. All metabolic, hormonal, immune processes during pregnancy are provided through maternal and fetal vascular system . Despite the fact that the blood of the mother and fetus does not mix, since their is separated by the placental barrier , the fetus receives all the necessary nutrients and oxygen from the mother's blood. The main structural component of the placenta is villous tree .
In the normal development of pregnancy, there is a relationship between the growth of the fetus, its body weight and the size, thickness, weight of the placenta. Up to 16 weeks of pregnancy, the development of the placenta outstrips the growth rate of the fetus. In case of death embryo (fetus) inhibition of growth and development of chorionic villi and progression of involution-dystrophic processes in the placenta.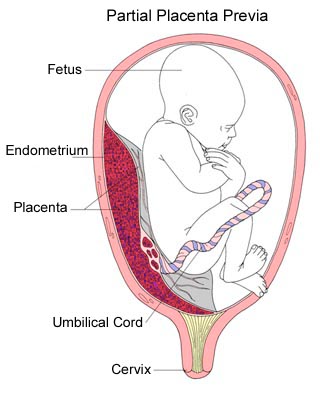 Having reached the required maturity at 38-40 weeks of pregnancy, the processes of formation of new vessels and villi in the placenta stop.
Having reached the required maturity at 38-40 weeks of pregnancy, the processes of formation of new vessels and villi in the placenta stop.
Diagram of the structure of the placenta and uteroplacental circulation
1 - umbilical cord arteries
2 - stem villi
3 - decidual septum
4 - decidua
5 - myometrium
6 - veins
7 - spiral arteries
8 - chorion
9 - amnion
10 - intervillous space
11 - vein of the umbilical cord
12 - cotyledon
The mature placenta is a disc-shaped structure 15-20 cm in diameter and 2. 5-3.5 cm thick. Its mass reaches 500-600 g. The maternal surface of the placenta , which faces the uterine wall, has a rough surface formed by the structures of the basal part of the decidua. Fruit surface of placenta , which faces the fetus, is covered by amniotic membrane . Under it are visible vessels that go from the place of attachment of the umbilical cord to the edge of the placenta. The structure of the fruiting part of the placenta is represented by numerous chorionic villi , which are combined into structural formations - cotyledons. Each cotyledon is formed by a stem villus with branches containing fetal vessels. The central part of the cotyledon forms a cavity, which is surrounded by many villi. In a mature placenta, there are 30 to 50 cotyledons. Cotyledon of the placenta is conditionally comparable to a tree, in which the supporting villi of the 1st order are its trunk, the villi of the 2nd and 3rd orders are large and small branches, the intermediate villi are small branches, and the terminal villi are leaves.
5-3.5 cm thick. Its mass reaches 500-600 g. The maternal surface of the placenta , which faces the uterine wall, has a rough surface formed by the structures of the basal part of the decidua. Fruit surface of placenta , which faces the fetus, is covered by amniotic membrane . Under it are visible vessels that go from the place of attachment of the umbilical cord to the edge of the placenta. The structure of the fruiting part of the placenta is represented by numerous chorionic villi , which are combined into structural formations - cotyledons. Each cotyledon is formed by a stem villus with branches containing fetal vessels. The central part of the cotyledon forms a cavity, which is surrounded by many villi. In a mature placenta, there are 30 to 50 cotyledons. Cotyledon of the placenta is conditionally comparable to a tree, in which the supporting villi of the 1st order are its trunk, the villi of the 2nd and 3rd orders are large and small branches, the intermediate villi are small branches, and the terminal villi are leaves. Cotyledons are separated from each other by partitions (septa) emanating from the basal plate.
Cotyledons are separated from each other by partitions (septa) emanating from the basal plate.
Intervillous space on the fetal side is formed by the chorionic plate and villi attached to it, and on the maternal side it is limited by the basal plate, decidua and septa extending from it. Most of the placental villi are freely immersed in the intervillous space and are bathed in maternal blood . There are also anchor villi, which are fixed to the basal decidua and provide attachment of the placenta to the wall of the uterus.
Diagram of blood circulation in the fetus
1 - superior vena cava
2 - oval hole
3 - inferior vena cava
4 - venous duct
5 - portal sinus
6 - portal vein
7 - vein of the umbilical cord
8 - umbilical cord arteries
9 - placenta
10 - epigastric arteries
11 - ductus arteriosus
Spiral arteries , which are the terminal branches of the uterine and ovarian arteries, feeding the pregnant uterus , open into the intervillous space with 120-150 orifices, providing a constant flow of maternal oxygen-rich blood into the intervillous space.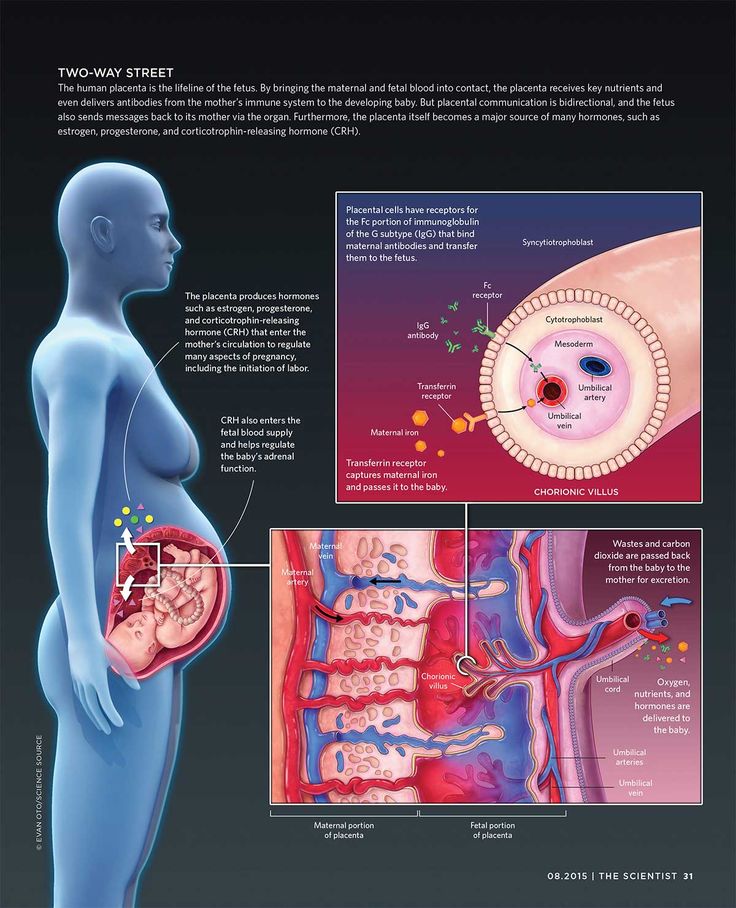 Due to pressure difference , which is higher in the maternal arterial bed compared to the intervillous space, blood saturated with oxygen from the mouths of the spiral arteries is sent through the center of the cotyledon to the villi, washes them, reaches the chorionic plate and returns to the dividing septa maternal blood flow through venous orifices. In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix among themselves.
Due to pressure difference , which is higher in the maternal arterial bed compared to the intervillous space, blood saturated with oxygen from the mouths of the spiral arteries is sent through the center of the cotyledon to the villi, washes them, reaches the chorionic plate and returns to the dividing septa maternal blood flow through venous orifices. In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix among themselves.
The transfer of blood gases, nutrients , metabolic products and other substances from maternal blood to fetal and back is carried out at the moment of contact of the villi with the mother's blood through the placental barrier . It is formed by the outer epithelial layer of the villus, the stroma of the villus, and the wall of the blood capillary located inside each villus. Fetal blood flows through this capillary.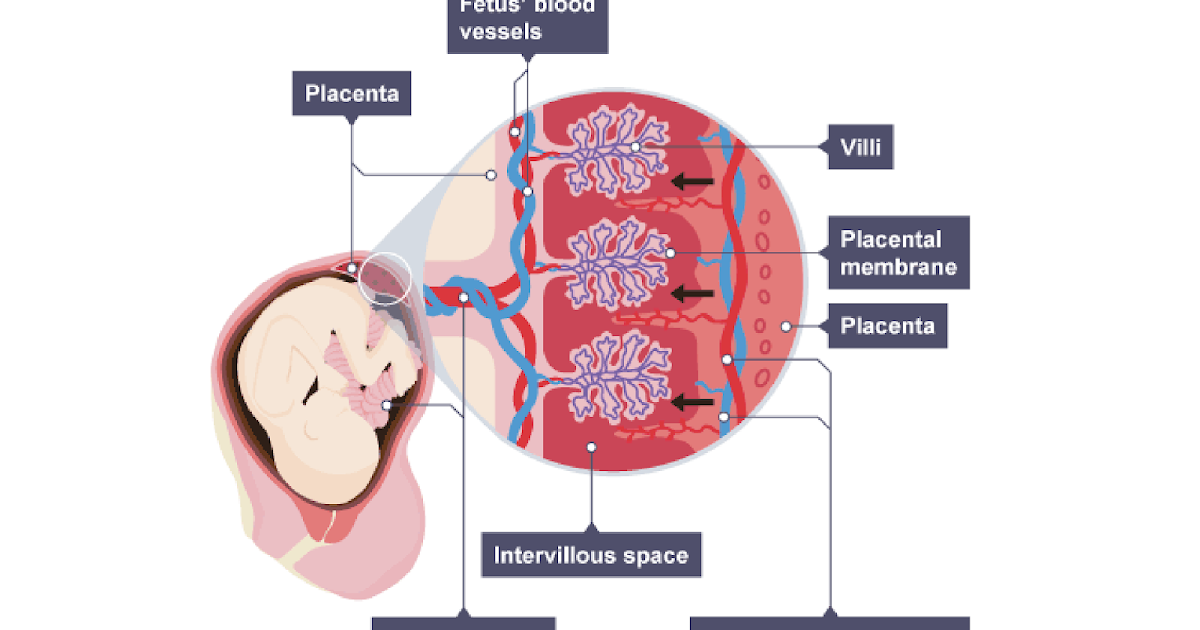 Saturated in this way with oxygen, the blood of the fetus from the capillaries of the villi is collected into larger vessels, which eventually combine into vein of the umbilical cord , through which oxygenated blood flows to the fetus . Having given up oxygen and nutrients in the body of the fetus, blood, depleted in oxygen and rich in carbon dioxide, flows from the fetus through two umbilical arteries to the placenta , where these vessels divide radially in accordance with the number of cotyledons. As a result of further branching of the vessels inside the cotyledons, the fetal blood again enters the capillaries of the villi and is again saturated with oxygen, and the cycle repeats. Due to the passage through the placental barrier of blood gases and nutrients, the respiratory, nutritional and excretory functions of the placenta are realized. At the same time, oxygen enters the bloodstream of the fetus and carbon dioxide and other metabolic products of the fetus are excreted .
Saturated in this way with oxygen, the blood of the fetus from the capillaries of the villi is collected into larger vessels, which eventually combine into vein of the umbilical cord , through which oxygenated blood flows to the fetus . Having given up oxygen and nutrients in the body of the fetus, blood, depleted in oxygen and rich in carbon dioxide, flows from the fetus through two umbilical arteries to the placenta , where these vessels divide radially in accordance with the number of cotyledons. As a result of further branching of the vessels inside the cotyledons, the fetal blood again enters the capillaries of the villi and is again saturated with oxygen, and the cycle repeats. Due to the passage through the placental barrier of blood gases and nutrients, the respiratory, nutritional and excretory functions of the placenta are realized. At the same time, oxygen enters the bloodstream of the fetus and carbon dioxide and other metabolic products of the fetus are excreted .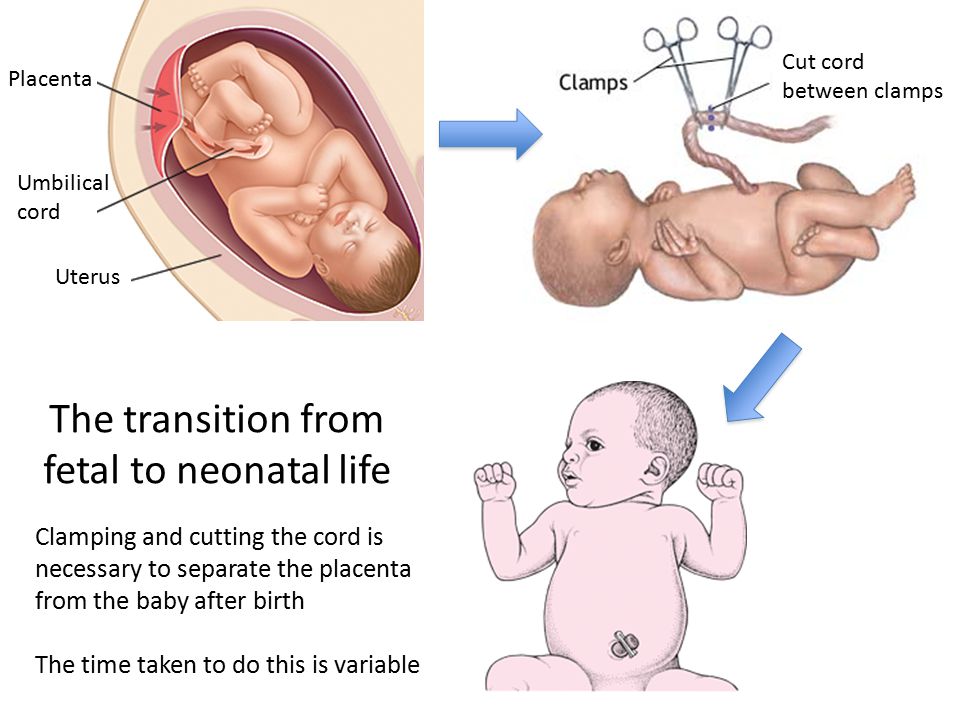 At the same time, proteins, lipids, carbohydrates, microelements, vitamins, enzymes and much more are transported towards the fetus.
At the same time, proteins, lipids, carbohydrates, microelements, vitamins, enzymes and much more are transported towards the fetus.
Scheme of the placental barrier
1 - capillary endothelium of terminal villi
2 - villus capillary
3 - villus stroma
4 - epithelial cover of villi
The placenta performs an important protective (barrier function) through the placental barrier, which is selectively permeable in both directions. In the normal course of pregnancy, the permeability of the placental barrier increases up to 32-34 weeks of pregnancy, after which it decreases in a certain way. However, unfortunately, a fairly large number of drugs, nicotine, alcohol, narcotic substances, pesticides, other toxic chemicals, as well as a number of pathogens of infectious diseases penetrate the placental barrier relatively easily into the fetal circulation, which has an adverse effect on the fetus.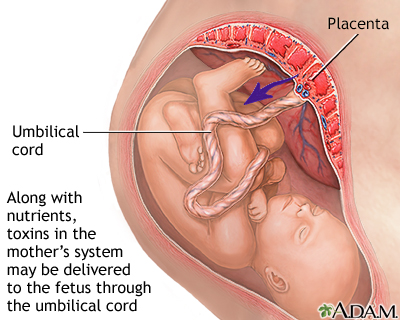 In addition, under the influence of pathogenic factors, the barrier function of the placenta is even more disturbed.
In addition, under the influence of pathogenic factors, the barrier function of the placenta is even more disturbed.
The placenta is anatomically and functionally related to the amnion (aqueous membrane) that surrounds the fetus. The amnion is a thin membrane that lines the surface of the placenta facing the fetus, passes to the umbilical cord and merges with the skin of the fetus at the umbilical ring. Amnion is actively involved in the exchange of amniotic fluid , in a number of metabolic processes, and also performs a protective function.
Connects placenta and fetus umbilical cord , which is a cord-like formation. The umbilical cord contains two arteries and one vein . Two arteries in the umbilical cord carry oxygen-depleted blood from the fetus to the placenta. The vein of the umbilical cord carries oxygenated blood to the fetus. The vessels of the umbilical cord are surrounded by a gelatinous substance, which was called "wharton jelly" .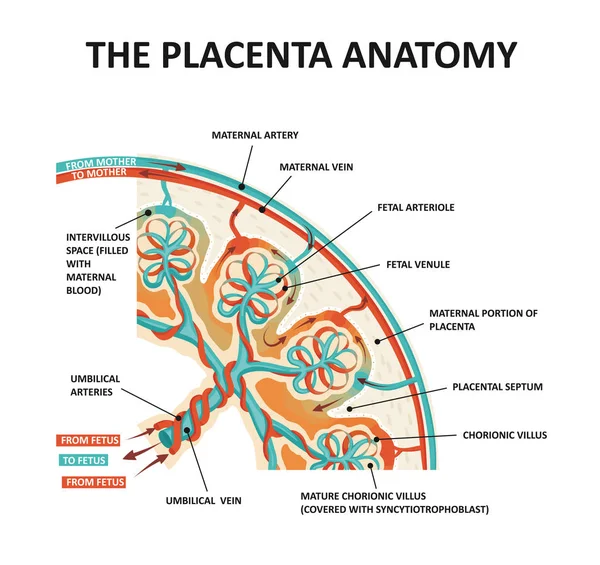 This substance provides the elasticity of the umbilical cord, protects the vessels and provides nutrition to the vascular wall. The umbilical cord may attach (most often) to the center of the placenta and less commonly to the side of the umbilical cord or to the membranes. The length of the umbilical cord in a full-term pregnancy is on average about 50 cm.
This substance provides the elasticity of the umbilical cord, protects the vessels and provides nutrition to the vascular wall. The umbilical cord may attach (most often) to the center of the placenta and less commonly to the side of the umbilical cord or to the membranes. The length of the umbilical cord in a full-term pregnancy is on average about 50 cm.
Placenta, membranes and umbilical cord together form placenta , which is expelled from the uterus after the birth of the child.
Ultrasound scanner HS60
Professional diagnostic tools. Tissue elasticity assessment, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiac examinations.
Maternity hospital №7, Novosibirsk - What is the placenta?
Anna Valentinovna Yakimova, obstetrician-gynecologist, doctor of medical sciences talks about the placenta and placental insufficiency.
Picture from the site http://s7ya7.zdorovo-zivi.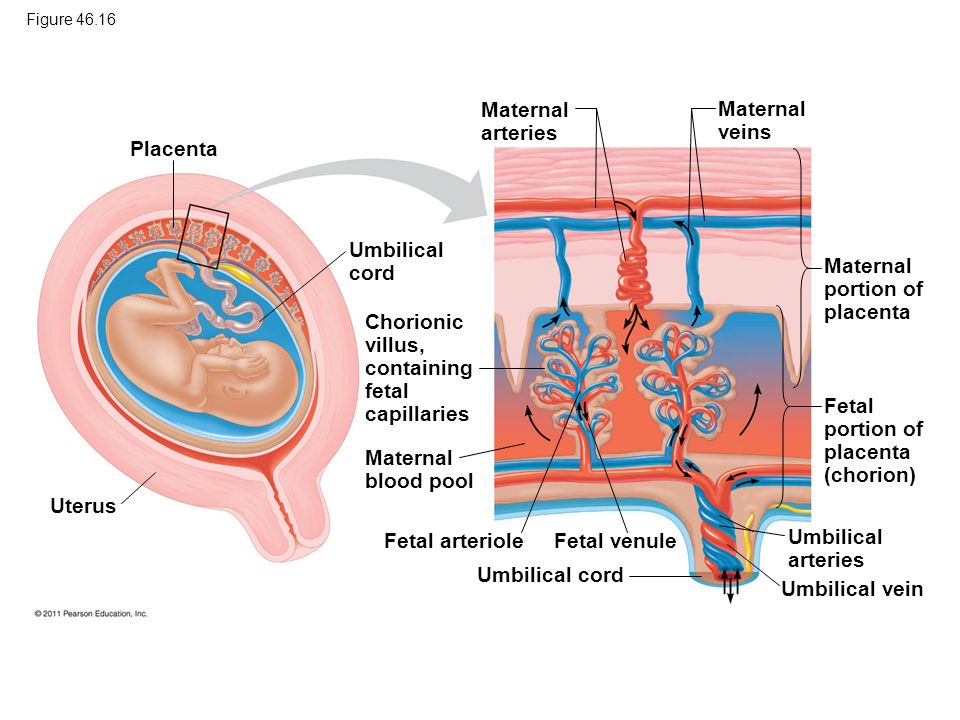 ru
ru
Placenta. The name of the organ comes from lat. placenta - cake, cake, pancake. This is an extra-embryonic organ, consisting of villi, thanks to which the fetus is nourished, respired, and waste products are removed from its blood. There are free and fixing (anchor) villi. The placenta is formed in the place where the embryo was implanted, arises as a result of the connection of the chorion - extraembryonic tissue with a thickened uterine mucosa (decidual tissue). Despite the fact that the blood of the mother and fetus does not mix, as they are separated by the placental barrier, the fetus receives all the necessary nutrients and oxygen from the mother's blood. In addition, the placenta produces hormones that ensure the preservation of pregnancy. The placenta has two surfaces. The surface that faces the fetus is called the fetal. It is covered with a smooth shell - the amnion, through which large vessels shine through. The one that is attached to the wall of the uterus is called maternal.
The main structural unit of the placenta is cotelidone. Cotyledon of the placenta is conditionally comparable to a tree. Each cotyledon is formed by a stem villus, from which, like branches of a tree, villi of the second and third order extend, containing vessels. The central part of the cotyledon forms a cavity, which is surrounded by many villi. Between the cotyledons there is a space - mejvirus, which on the maternal side is limited by partitions (septa) extending from the mucous membrane of the uterus. Most of the placental villi are freely immersed in the intervillous space (free villi) and are bathed in maternal blood. The spiral arteries, which are small branches of the arteries that supply the uterus, open into the intervillous space and supply oxygen-rich blood to the intervillous space. Due to the pressure difference, which is higher in the mother's arterial bed compared to the intervillous space, oxygenated blood from the mouths of the spiral arteries is directed through the center of the cotyledon to the villi, washes them, reaches the chorionic plate and returns to the maternal circulation through the venous orifices through the separating septa.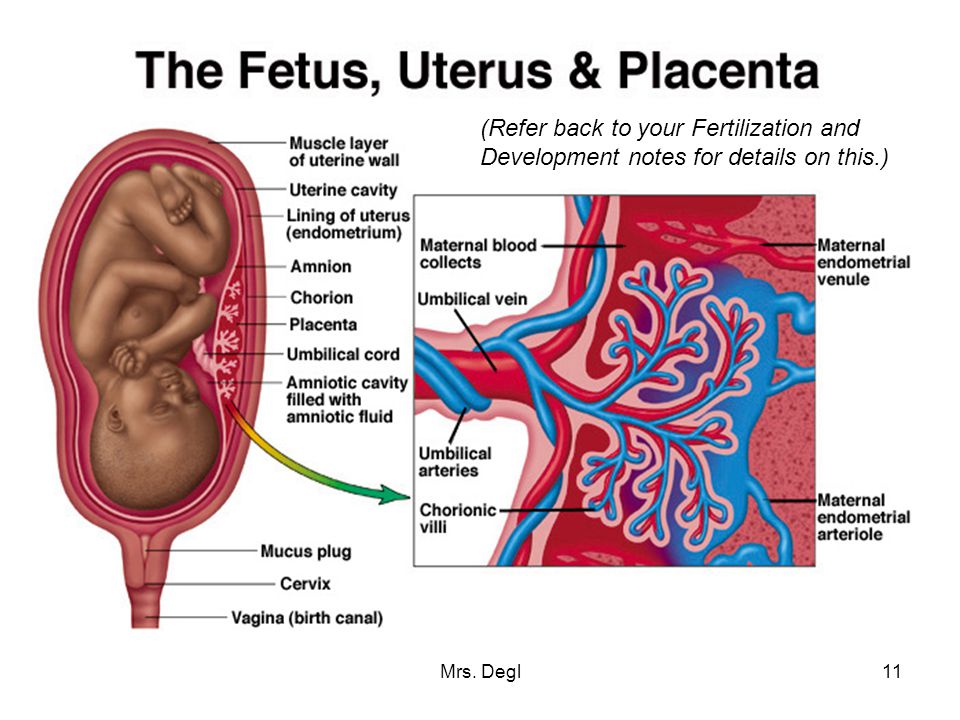 . In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix. Thus, the concept of the placental barrier appears: the blood of the mother of the fetus does not mix, because they are separated by the wall of the villus, loose connective tissue inside the villus and the wall of the vessel that is inside the villus, and in which the blood of the fetus circulates.
. In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix. Thus, the concept of the placental barrier appears: the blood of the mother of the fetus does not mix, because they are separated by the wall of the villus, loose connective tissue inside the villus and the wall of the vessel that is inside the villus, and in which the blood of the fetus circulates.
At the end of pregnancy, the placenta is a soft disk 15-18 cm in diameter, 2-4 cm thick in the central part, weighing about 500-600 g. their capillaries - 12 m2. The placenta, membranes, and umbilical cord together form the afterbirth, which is expelled from the uterus after the baby is born.
Normally, the placenta is attached to the uterine cavity on its anterior or posterior surface, sometimes in the fundus. If the placenta is attached in the lower part of the uterine cavity, close to the internal opening of the cervix - the internal pharynx, then its blood supply is often insufficient and the fetus may suffer from lack of oxygen and nutrients - a phenomenon called placental insufficiency occurs.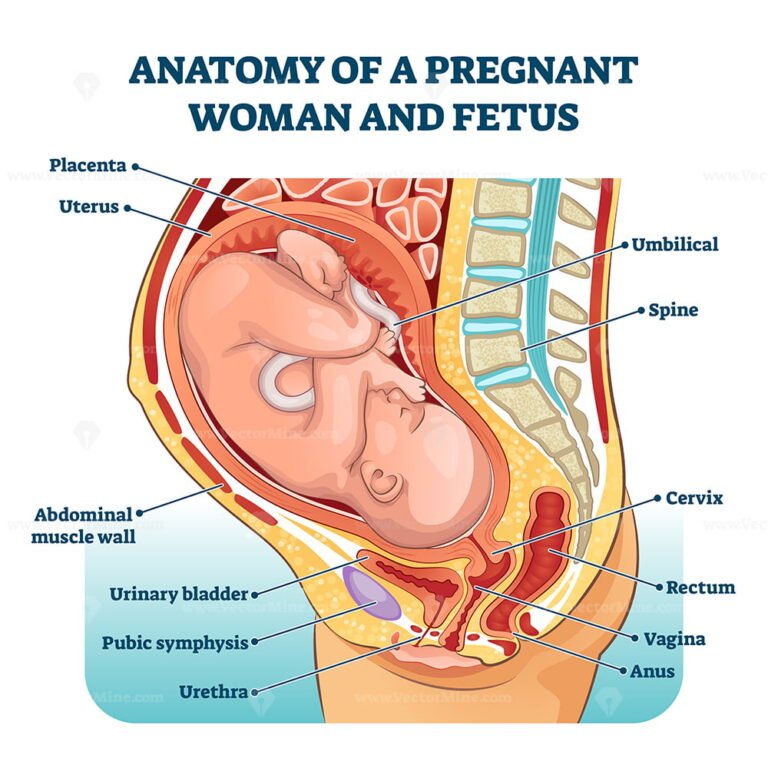
Placental insufficiency is a violation of all or some of the functions of the placenta, ultimately leading to oxygen starvation (hypoxia), fetal growth retardation or death and / or early termination of pregnancy.
Placental insufficiency may occur early in pregnancy due to abnormal formation of the placenta, for example, if the spiral arteries that supply the villi do not lose their ability to narrow their lumen in response to exposure to vasoconstrictor substances. It is possible that there is a violation of the development of blood vessels inside the villi, the vessels can form in the central part of the villus, and not close to its wall, then the transfer of nutrients from the mother's blood to the fetal blood and the flow of metabolic products back will be difficult. The process of development of the placenta (in particular, vascular formation) occurs to a greater extent in the first and second trimesters of pregnancy, ending at about 30-32 weeks. After this period, involutive processes predominate ("aging", immuring the villi with fibrinoid).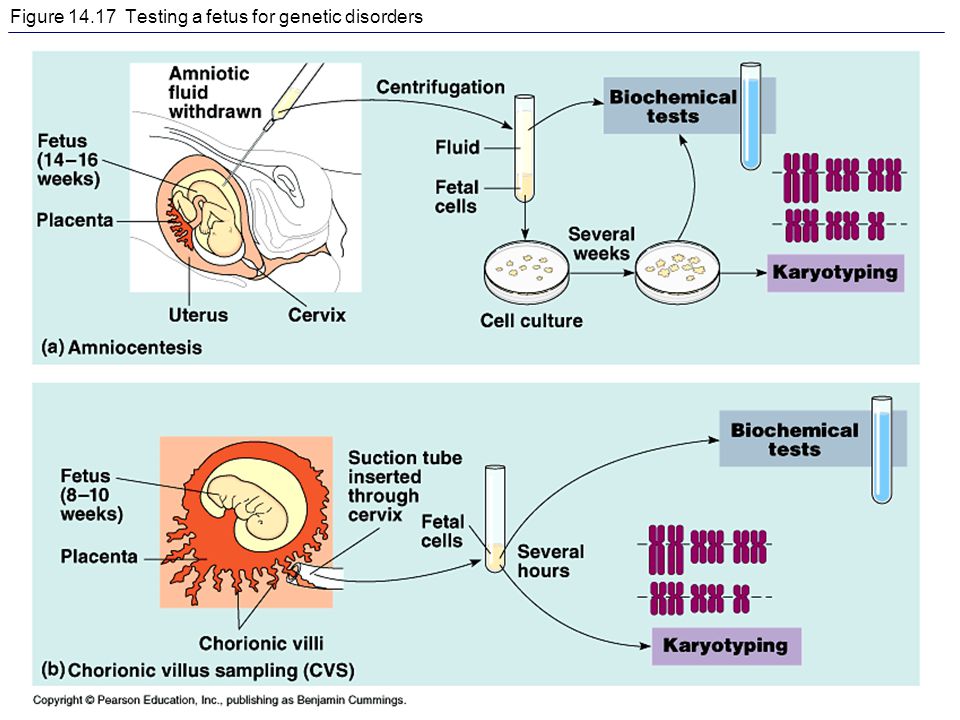 Along with the processes of involution in the placenta during pregnancy, young villi develop, more often avascular, which, however, only partially compensate for the function of mature villi containing vessels that have “fallen out” of the circulation.
Along with the processes of involution in the placenta during pregnancy, young villi develop, more often avascular, which, however, only partially compensate for the function of mature villi containing vessels that have “fallen out” of the circulation.
In another scenario, placental insufficiency occurs at a later date, as a result of damage to the placenta in inflammatory processes, diabetes in a pregnant woman, or high blood pressure, when blood flow to the uterus is disturbed, which can also occur with increased maternal blood clotting . It is believed that it is the violation of the uteroplacental circulation that plays the main role in the formation of the intrauterine growth retardation syndrome. Before the advent of Doppler ultrasound research methods in obstetric practice, there were no non-invasive methods for studying blood flow in the mother-placenta-fetus system. To date, Doppler is the most preferred instrumental method that provides useful information in relation to the detection of blood flow disorders and the determination of pregnancy management tactics for placental insufficiency.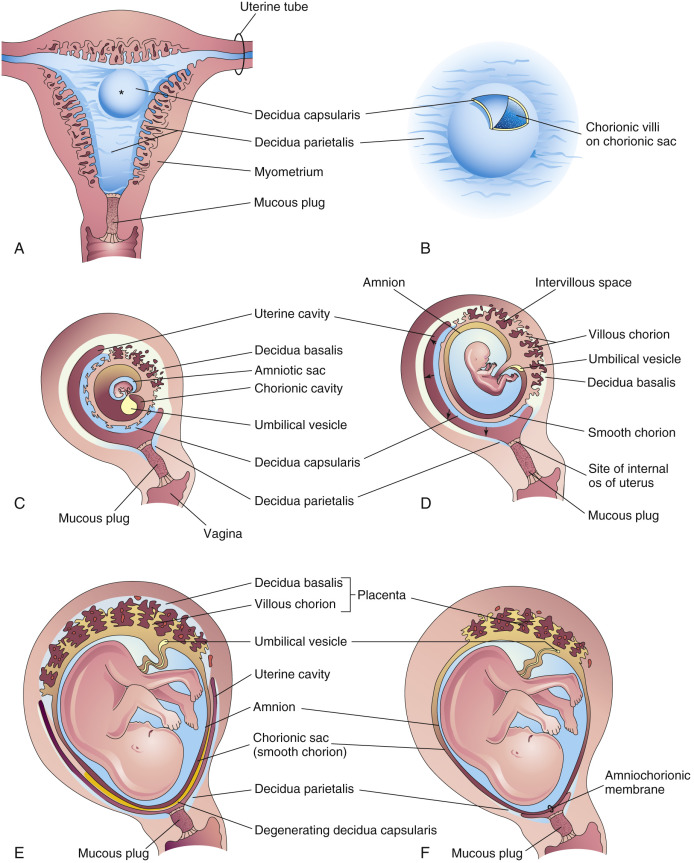 If there are symptoms of placental insufficiency - a mismatch in the height of the uterine fundus, signs of a threat of early termination of pregnancy, rapid or slow fetal heart rate (normal: 120-160 beats per minute), an altered amount of amniotic fluid - it is necessary to conduct an ultrasound examination, Doppler blood flow in the vessels of the uterus, umbilical cord and fetus, and in the third trimester - cardiotocography. The earliest sign of placental dysfunction is a decrease in its production of hormones and proteins, therefore, in pregnant women with a known risk of placental dysfunction (for example, if she has a chronic inflammatory process or often / constantly increased blood pressure, etc.), you can examine the level placental lactogen, progesterone, unconjugated estriol in the blood. And on the basis of the data obtained, predict the further development of pregnancy and take preventive measures.
If there are symptoms of placental insufficiency - a mismatch in the height of the uterine fundus, signs of a threat of early termination of pregnancy, rapid or slow fetal heart rate (normal: 120-160 beats per minute), an altered amount of amniotic fluid - it is necessary to conduct an ultrasound examination, Doppler blood flow in the vessels of the uterus, umbilical cord and fetus, and in the third trimester - cardiotocography. The earliest sign of placental dysfunction is a decrease in its production of hormones and proteins, therefore, in pregnant women with a known risk of placental dysfunction (for example, if she has a chronic inflammatory process or often / constantly increased blood pressure, etc.), you can examine the level placental lactogen, progesterone, unconjugated estriol in the blood. And on the basis of the data obtained, predict the further development of pregnancy and take preventive measures.
Can placental insufficiency be treated? The answer to this question is ambiguous.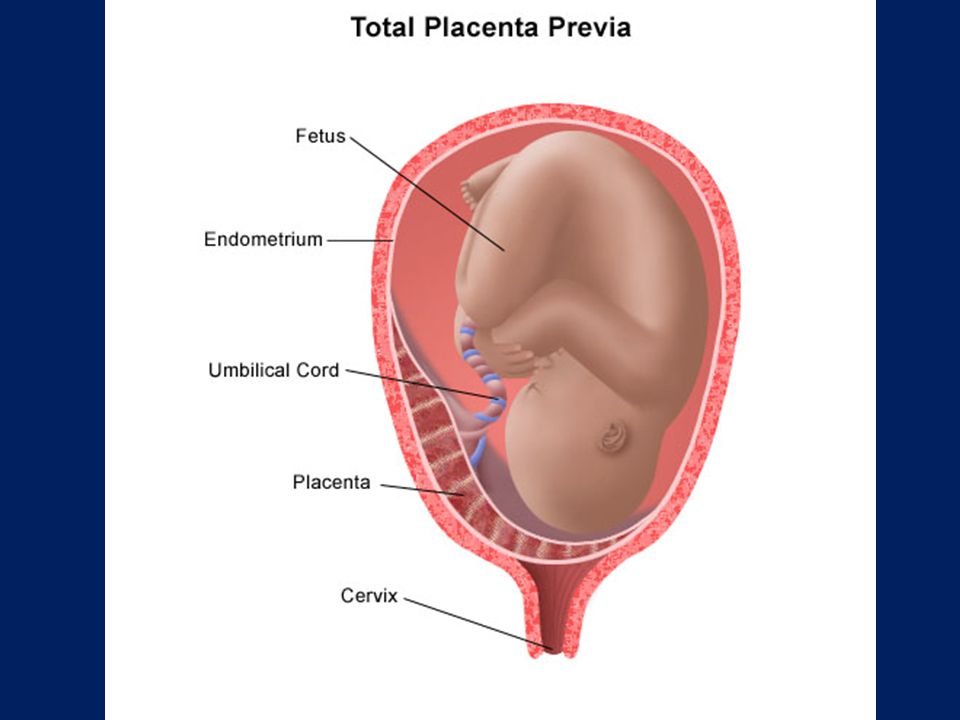 It is possible to influence the development of the placenta when it is incomplete, improving the conditions for development - by eliminating, for example, the inflammatory process, normalizing blood pressure, lowering the tone of the uterus, and normalizing blood clotting. You can influence the metabolism in the cells of the placenta - by doing this, for example, by introducing drugs into the body of a pregnant woman that help improve the utilization of glucose by cells. It is possible to influence the tone of the vessels, reduce the permeability of the wall and, in this way, the swelling of the tissues decreases and the penetration of oxygen into them improves. But we must understand that we do not cure placental insufficiency, we are only trying to influence the compensatory mechanisms that exist in the placenta, if this succeeds, the manifestations of placental insufficiency disappear. But more often, treatment is aimed at prolonging the pregnancy to the term of a viable fetus.
It is possible to influence the development of the placenta when it is incomplete, improving the conditions for development - by eliminating, for example, the inflammatory process, normalizing blood pressure, lowering the tone of the uterus, and normalizing blood clotting. You can influence the metabolism in the cells of the placenta - by doing this, for example, by introducing drugs into the body of a pregnant woman that help improve the utilization of glucose by cells. It is possible to influence the tone of the vessels, reduce the permeability of the wall and, in this way, the swelling of the tissues decreases and the penetration of oxygen into them improves. But we must understand that we do not cure placental insufficiency, we are only trying to influence the compensatory mechanisms that exist in the placenta, if this succeeds, the manifestations of placental insufficiency disappear. But more often, treatment is aimed at prolonging the pregnancy to the term of a viable fetus.
But if the signs of placental insufficiency increase, and the gestation period is more than 32 weeks, when even in a normal placenta it undergoes involution, the placenta initially developed incorrectly, and now it performs its functions worse, the fetus suffers, then it is useless to treat placental insufficiency, it is better to carry out early delivery and to nurse the newborn without the risk of intrauterine death, which is possible if the placenta depletes its reserves.