When can babies regulate their temperature
How to Choose the Right Room Temperature for Your Baby
Written by WebMD Editorial Contributors
In this Article
- The Best Room Temperature for Babies
- Why the Right Temperature Is Important
- Is Baby Too Hot or Cold?
- How to Regulate Your Baby’s Temperature
When the bedroom is too hot or too cold, it's hard to get a good night’s sleep. This is as true for babies as it is for adults. Finding the right room temperature for your baby is important to keeping them safe and healthy.
The Best Room Temperature for Babies
Your baby can’t put into words how they feel, so it’s up to you as a parent to find the right room temperature for them. You don’t want your baby’s room to be either too hot or too cold. It's recommended that the best temperature for babies is between 68 to 72 degrees Fahrenheit or 20 to 22 degrees Celsius.
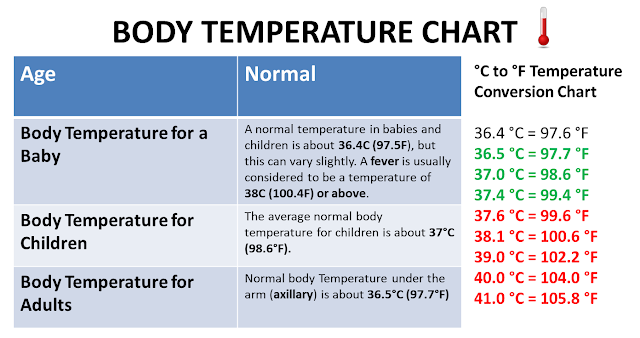
Babies are more sensitive to changes in room temperature because they're so small and their bodies are still growing. By around 11 weeks, though, babies’ bodies start to regulate their temperature at night just like older humans do. Within four hours of bedtime, babies reach a minimum core body temperature of 97.5 degrees Fahrenheit.
You can monitor the temperature in your baby’s room with an indoor thermometer if the room doesn’t have a thermostat. However, it’s not necessary to constantly monitor the temperature or to keep the heating or cooling running throughout the night if your baby is properly dressed for the weather.
Both babies and toddlers feel comfortable at the same room temperature as adults do. Sometimes your baby will need an extra layer, but you should dress your baby the same way that you dress yourself: not too hot and not too cold.
Why the Right Temperature Is Important
Lots of parents think that they need to keep their baby bundled and extra warm, but this isn’t really true. It’s crucial that your baby has a stable temperature that isn’t too hot or cold. In fact, the risk of sudden infant death syndrome (SIDS) goes up if your baby becomes too hot. Children are at risk of SIDS throughout their toddler years, but the highest risk is within the first six months of life.
Children are at risk of SIDS throughout their toddler years, but the highest risk is within the first six months of life.
Overheating is linked to SIDS, so it’s important that you don’t bundle your baby too tightly in the winter. Try to keep their room cool in the months when the temperature outside is higher than 70 degrees Fahrenheit. There's some evidence that suggests that high environmental temperatures are also linked to SIDS.
Is Baby Too Hot or Cold?
In the beginning, it might be hard to tell if your baby is too hot or cold. Follow these steps to help you figure out the ideal temperature for your little bundle of joy:
Is Baby Too Hot?
To check if your baby is too warm, touch the nape of their neck to see if it's sweaty. Babies usually don’t sweat the same way that adults do, but sweat on the neck can indicate that they're too hot.
You can also try putting your hand on your baby’s chest or ears to test the temperature of their skin. Avoid checking their hands and feet, as they will always feel cooler than the rest of your baby’s body. Your baby’s skin might be flushed, or they might be irritable if they're too hot.
Avoid checking their hands and feet, as they will always feel cooler than the rest of your baby’s body. Your baby’s skin might be flushed, or they might be irritable if they're too hot.
Is Baby Too Cold?
It’s a bit easier to know when your baby is too cold. Their hands and feet may turn slightly blue, which is normal for infants. Their fingers and toes will feel quite cold to the touch, and your baby may even shiver. To warm themselves up, babies have to burn extra calories that they can’t spare.
How to Regulate Your Baby’s Temperature
Many parents swaddle or wrap up their baby to sleep, but it’s not necessary. Too many blankets and wrapping your baby too tightly increases their risk of SIDS. Instead, opt for minimal bedding in their crib, and consider using a lightweight sleep sack to keep them comfortable. Never use hot water bottles or electric blankets in your baby’s crib.
In Warmer Months
When the outside temperature is warm, your baby doesn’t need to wear as much clothing. Consider using a fan in their room to circulate the air, but don’t point it directly at the baby. Studies also show that using a fan in your baby’s room can reduce the risk of SIDS.
Consider using a fan in their room to circulate the air, but don’t point it directly at the baby. Studies also show that using a fan in your baby’s room can reduce the risk of SIDS.
If it's safe to do so, you can keep the window or door of your baby’s room open to let in some fresh air and keep them cool.
In Cooler Months
When the weather cools down, use light, breathable blankets that only come up to your baby’s chest, or a light sleep sack. Make sure that their head is uncovered to reduce the risk of SIDS.
Baby Temperature Regulation - Snuza Baby Breathing Monitors
Did you know that babies cannot regulate their own body temperature until they are about 1.5 or 2 years old? In a recent poll of new parents, one subject that came up repeatedly was baby body temperature and figuring out whether they were too hot or too cold. So today, we’re going to tackle baby temperature regulation. Let’s get into it!
Baby bodies
They’re so tiny when they are born, and then lose more weight in the first few days! Babies average at about 3.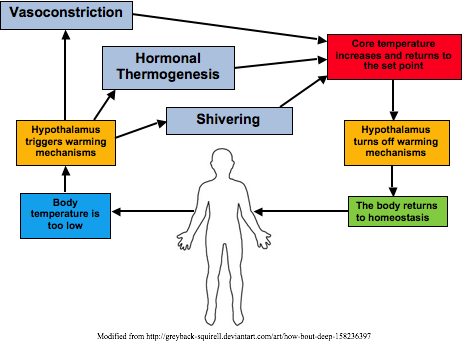 5 kilograms, with preterm and premature babies weighing even less. Their bodies don’t have much fatty tissue yet, so they lose body heat up to four times faster than we do. Babies also can’t shiver to increase their body temperature. In addition, being too hot or too cold can affect your baby’s breathing and oxygen use, using up their precious energy that much faster.
5 kilograms, with preterm and premature babies weighing even less. Their bodies don’t have much fatty tissue yet, so they lose body heat up to four times faster than we do. Babies also can’t shiver to increase their body temperature. In addition, being too hot or too cold can affect your baby’s breathing and oxygen use, using up their precious energy that much faster.
The ideal body temperature for babies is 36.5°C (97.7° F). The ideal ambient temperature for babies is 20°C to 22.2°C (68° F to 72°F 9).
How to prevent overheating
In hot weather, dress your baby lightly and try not to cover their heads, especially while sleeping. The head acts like a little radiator, giving off excess heat so covering it, even in a sun hat, can make your baby overheat. Rather keep your baby in a shady place, than use a hat and stay out in the sun.
On hot nights, don’t be afraid to let your baby sleep in just a nappy and a light, muslin swaddle (if they like to be swaddled). Don’t direct a fan directly at your baby’s bed, but a fan in the room can help to reduce the overall heat level if it is very hot.
Don’t direct a fan directly at your baby’s bed, but a fan in the room can help to reduce the overall heat level if it is very hot.
Signs your baby is overheating are:
- They feel warm to the touch, and their skin is red
- They have a rapid heartbeat or are breathing more quickly
- They have a fever but aren’t sweating
- Your baby is lethargic or unresponsive
- Your baby is vomiting or seems dizzy and confused
How to cool an overheated baby
If your baby seems to be overheating, immediately remove them to a cooler place. If outside in the sun, go indoors to a cool room. Remove any excess clothing, and wipe your baby down with a cool, damp cloth. If your baby is able to drink, offer them fluids, either breastfeeding or a bottle, or if old enough, some cool water.
If symptoms don’t improve, take your baby to the emergency room or consult a doctor.
How to prevent a chill
Getting too cold is also problematic. Experts advise against over-bundling and overdressing babies, as they are unable to remove clothing themselves if they get too hot. Dress your baby in layers — the rule of thumb says to add one more layer than you are wearing to feel comfortable.
To check if your baby is too hot or cold, feel their tummy, back and neck. As these are closer to your baby’s core, they are a truer measure of their actual body temperature. Your baby’s skin should feel warm, not hot, to the touch, and not cold or sweaty. If their hands and feet are feeling cool, they could be getting too cold, so you should keep an eye on them and consider adding another layer.
Also, as we advise not to put a hat onto a baby when it’s hot, feel free to dress your baby in a hat when it’s cold! Just make sure that they don’t sleep with one on, especially during the night, as it can slip over their face and smother them.
How to warm a chilled baby
If your baby has gotten too cold — their torso is cold, and they are uninterested in feeding, as they are too busy trying to get warm — there are things that you can do.
- Place baby skin-to-skin on your chest and cover both of you with a blanket.
- Use your body heat to touch and gently rub your baby’s hands, feet, legs, arms, and back while they lay on your body.
- Keep your baby on your skin and keep warming them until their skin is warm and dry, then redress them adding extra layers as needed.
If your baby has gotten too cold and is floppy and unresponsive, they need medical attention immediately and will need to be warmed up carefully and gently at the hospital.
Balance the room and the baby warming
Studies have shown that when babies are either too hot or too cold, they sleep poorly. That can be restlessness or sleeping too deeply, which increases the risk of SIDS. The same studies show that the optimal room temperature for an infant to sleep in is around 20°C to 22.2°C (68° F to 72°F 9). At this temperature, babies sleep peacefully but do tend to wake up to auditory signals, rather than sleep through it which can cause SIDS.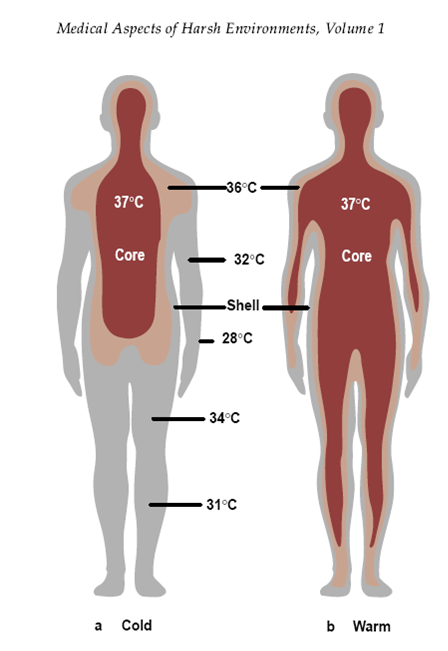
If, however, you have the room at the right temperature but your baby still feels cold, you might be tempted to use blankets. Other than a fitted swaddle — on babies under 2 months old — experts don’t recommend blankets or duvets. However, you can use a baby sleep sack which buttons on at the shoulders and allows their arms to remain free. This helps to keep their body heat in and warm them, without posing the smothering risk that loose blankets do.
Summary
In general, aim to keep your baby at Goldilock’s temperature: not too warm, not too cold, just right. This can be a matter of learning your own baby’s tendency to run warm or cold and adding and removing layers frequently, especially during season changes. To check your baby’s temperature, check the skin on their body and neck, but also ensure that their hands and feet are not too cool, as that can be a sign of heading towards being too chilled.
Sources:
- Keeping Your Baby Warm: https://www.
 stanfordchildrens.org/en/topic/default?id=warmth-and-temperature-regulation-90-P02425
stanfordchildrens.org/en/topic/default?id=warmth-and-temperature-regulation-90-P02425 - Is Your Baby Overheating? Signs Your Baby Is Too Hot: https://www.happiestbaby.com/blogs/baby/baby-overheating
- Is my baby too cold at night?: https://infantcpr.com/blog/posts/is-my-baby-too-cold-at-night/
The role of the incubator in the thermal protection of the newborn
The incubator keeps the baby warm by reducing heat transfer to the environment. That is, the child does not need to spend his metabolic resources to deal with heat. stress, which causes growth retardation and interferes with the normal functioning of the body.
The energy resources of a newborn should be directed primarily to the functioning of internal organs, thermoregulation and growth.
Thermoregulation occurs at the expense of a significant part of the return of energy to newborns (especially in premature and low birth weight children). The exchange of heat with the environment in children is much higher than in adults due to the large ratio of body surface to weight, poorly developed subcutaneous tissue, and high skin permeability. All this explains the increased risk of hypo- and hyperthermia in newborns.
All this explains the increased risk of hypo- and hyperthermia in newborns.
Although the newborn maintains a constant body temperature, he cannot use his thermoregulatory mechanisms for a long time. It has been estimated that a 3 kg newborn, left at 25°C, can maintain its temperature for 2.8 days.
The incubator provides the newborn with the necessary comfortable temperature environment. The temperature in the incubator should be thermoneutral, at which the newborn can maintain his constant body temperature by passive thermoregulation with minimal energy and metabolic costs.
IMPORTANT! A decrease in room temperature by 1.2°C lowers the body temperature of a 1 kg newborn by 0.86°C in 30 minutes!
Optimal Thermoneutral Temperature
The optimal thermoneutral temperature depends on many factors: gestational and postnatal age, body weight, clothing, physical status, nutrition and environment. But there is one objective criterion: maintaining the stability of the temperature core of the newborn between 36. 5°C and 37.5°C.
5°C and 37.5°C.
- Heat products
- Heat dissipation
- Thermal neutrality
Maintaining a stable core temperature of the newborn between 36.5°C and 37.5°C can only be achieved by controlling heat loss, ie no change in heat production and no change in heat loss due to evaporation. This occurs mainly due to vasomotor reactions. In a newborn, the thermoneutral zone is very limited and barely exceeds 1°C in premature babies.
It is important to take into account not only the factors on which thermal neutrality depends, but also the mechanisms of heat transfer:
- Conductivity
- Convection
- Emission
- Evaporation
The easiest way to check if a child is in the thermoneutral zone is to measure their body temperature, which should fall between 36.5°C and 37.5°C.
How can the child's heat exchange with the environment be controlled?
If the ambient temperature is lower than the baby's skin temperature, heat will radiate from the skin to the environment (due to conduction, convection, radiation and evaporation).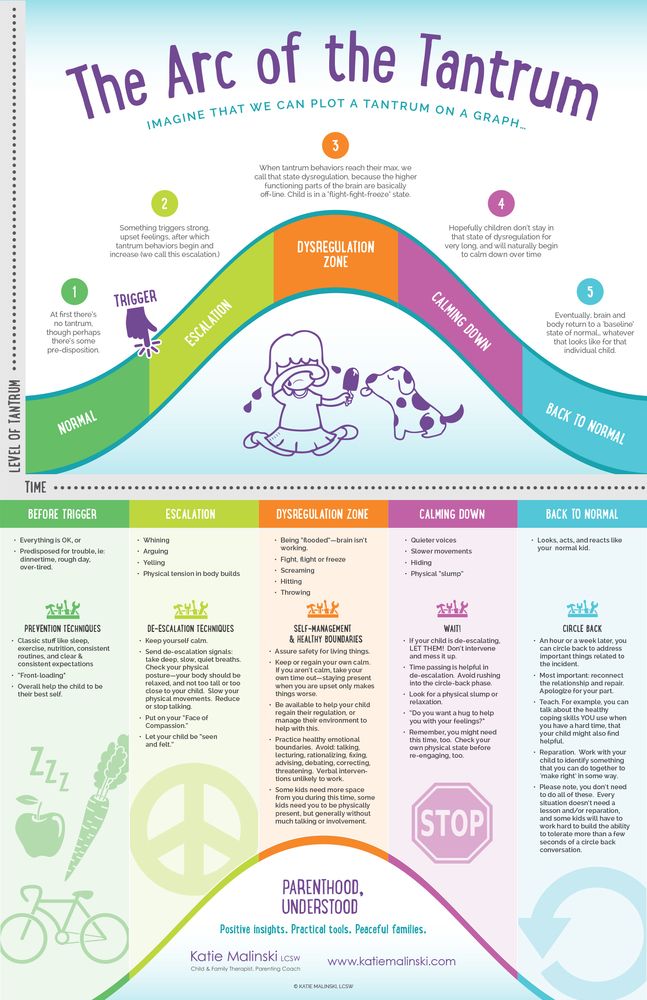 If the ambient temperature is higher than the baby's skin temperature, then the body will accumulate heat (through convection, conduction and radiation). In the latter case, only evaporation provides heat transfer.
If the ambient temperature is higher than the baby's skin temperature, then the body will accumulate heat (through convection, conduction and radiation). In the latter case, only evaporation provides heat transfer.
To protect the newborn from hypo- and hyperthermia, it is important to consider the following heat transfer mechanisms:
- Conductivity, i.e. heat exchange through skin-to-object contact. Conductivity depends on the conductivity coefficient of the object that is in contact with the skin, the contact surface and the temperature difference between the skin and the object. Heat exchange between the baby's skin and the mattress in the incubator is minimal (1-3% of the total heat transfer), but it can become dominant when using a warming mattress or skin-to-skin contact. The more we touch the surface, the more heat transfer will be. Conductivity can be limited by controlling the temperature of objects in contact with newborns.
- Convection, i.e. heat exchange between the surface of the body and the air circulating around the child.
 Heat exchange by convection provides 40% of the total heat transfer. The intensity of convection depends on the skin surface involved in the process, temperature difference and air flow rate. You can regulate convection by assigning the necessary body temperature depending on the situation. Opening the incubator doors, drafts, changes in air flow can affect convection. Do not place things, soft toys near the ventilation ducts of the incubator.
Heat exchange by convection provides 40% of the total heat transfer. The intensity of convection depends on the skin surface involved in the process, temperature difference and air flow rate. You can regulate convection by assigning the necessary body temperature depending on the situation. Opening the incubator doors, drafts, changes in air flow can affect convection. Do not place things, soft toys near the ventilation ducts of the incubator. - Radiation, i.e. heat exchange between the newborn and surrounding objects and surfaces due to infrared radiation. Heat exchange by radiation provides 50% of the total heat exchange. Radiation depends on the surface of the skin and the difference in temperature between the child's skin and the object or surface. The walls of the incubator are impervious to infrared radiation, so there is no heat exchange between the newborn and the room. However, the newborn exchanges heat with the walls of the incubator, which in turn exchange heat with the environment.
 Therefore, incubators should be placed in temperature controlled rooms. The incubator must not be placed under air conditioning or in direct sunlight.
Therefore, incubators should be placed in temperature controlled rooms. The incubator must not be placed under air conditioning or in direct sunlight. - Evaporation provides 7-9% of the total heat transfer. Evaporation through the skin and loss of moisture through respiration decrease as the child grows. Evaporation can be reduced by clothing or by achieving optimum humidity in the incubator.
Relationship between skin temperature and temperature core
The skin temperature measured in the right lateral region of the abdomen (at the point of intersection of perpendicular lines - the anterior axillary line and the line drawn from the navel) reflects the temperature core, which is usually at 0, 5°C below skin temperature.
Temperature core is the most reliable indicator of the somatic health of a newborn. Measurement of rectal temperature is not recommended due to the risk of intestinal perforation. The temperature will depend on the location of the temperature sensor.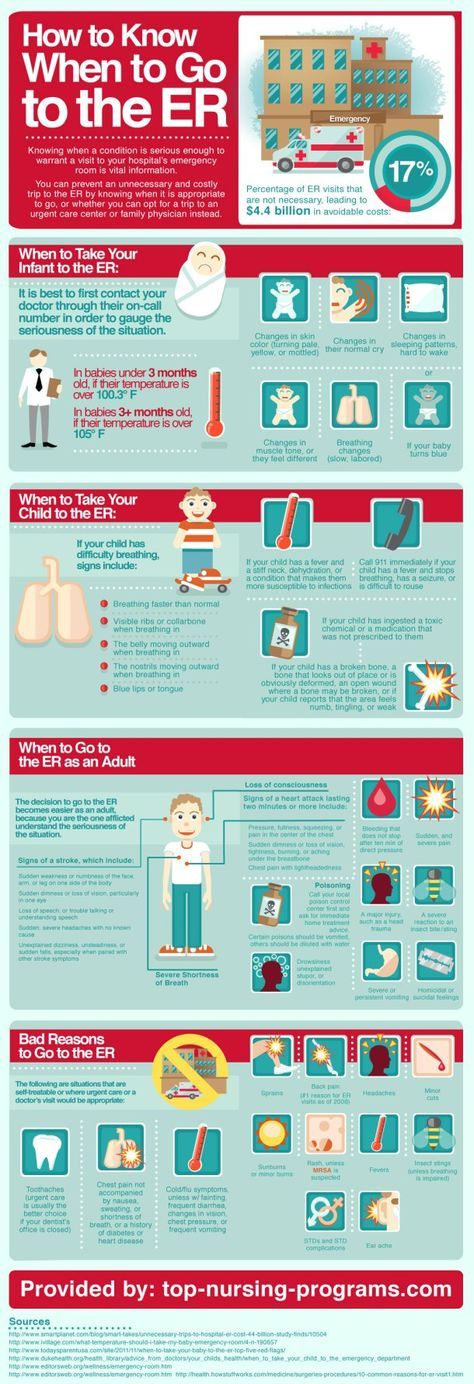 The use of a sensor does not mean that there is no need to regularly measure the body temperature of a newborn.
The use of a sensor does not mean that there is no need to regularly measure the body temperature of a newborn.
What are the consequences of a child not being in the thermoneutral zone?
Out of thermoneutral zone by 1-2°С. has a dangerous effect on the newborn (interrupted sleep, low weight gain, apnea, etc.).
Both hypothermia and hyperthermia are dangerous for the newborn.
Studies have shown that when the temperature rises or falls by 1-2°C from the thermoneutral zone, it leads to an increase in morbidity and mortality in newborns. Changing the temperature in the incubator by 2.5°C increases the risk of apnea by 50%. A difference of 2°C is sufficient to cause interrupted sleep in a low-birth-weight baby.
Where should the temperature sensor be placed?
Most often, the temperature sensor is placed in the right side of the abdomen (at the intersection of perpendicular lines - the anterior axillary line and the line drawn from the navel).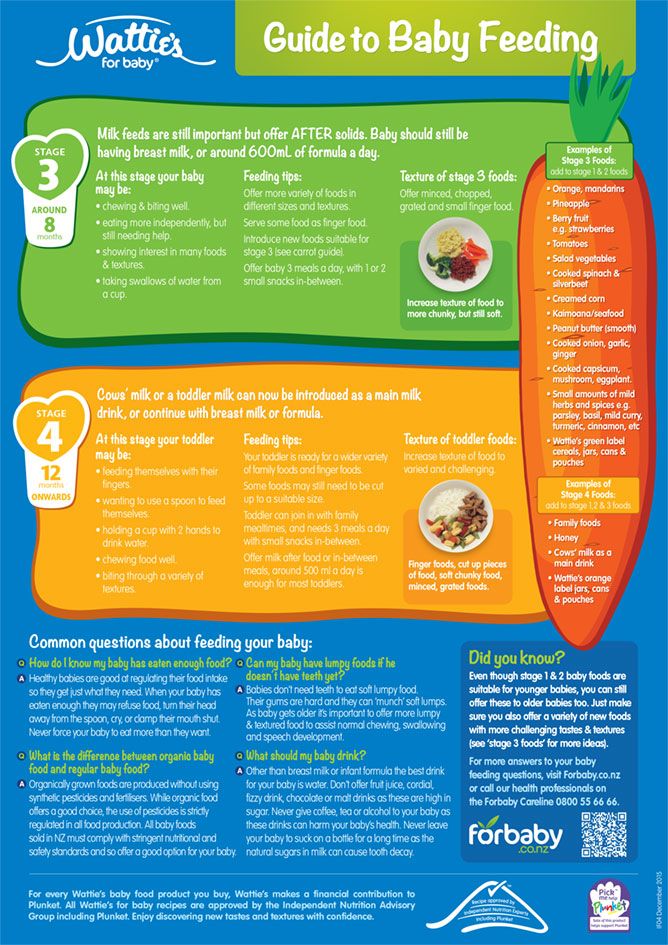
The transducer must not be placed in the area of bones, nor should it be attached too tightly to the skin surface (this may change vasomotor responses). It is the responsibility of the personnel to ensure that the sensor is properly positioned on the skin. If the sensor is dislodged or peeled off, the temperature shown by it will not be reliable. This is especially dangerous in the "skin temperature" mode, as the incubator will operate depending on the temperature of the baby's skin.
“Air mode”
In order to set the required temperature in “air mode”, several factors must be taken into account: the gestational and postnatal age of the child, the presence of clothing and the humidity in the incubator.
Some researchers have found that in the first week of life, thermoneutral temperature depends on gestational and postnatal age. After the first week of life, the thermoneutral temperature depends on the weight of the child and postnatal age. These studies were carried out in a room with a temperature equal to the temperature of the incubator and at a humidity of 50%.
Which mode to choose?
Unfortunately, there is no single protocol. The choice depends on the status of the baby: term, preterm, thermoneutral, hypothermal, or hyperthermal. The skin mode is the most commonly used, but it has its drawbacks, especially for low birth weight babies.
There are two ways to regulate the air temperature in the incubator:
- Using the "air mode", that is, by setting the desired air temperature.
- Using the "skin mode", that is, use the incubator system, which will itself set the required temperature depending on the temperature of the baby's skin.
Incubator Humidification
Low birth weight babies suffer from hypothermia even when the incubator is running at full capacity. This is due to increased heat transfer, especially in the first 5 days after birth. Humidification will help reduce heat transfer, namely evaporation, but in any case, it is very important to control the air temperature.
IMPORTANT! Relative humidity reduces the evaporation of heat through the skin, but increases the risk of infection and skin maceration.
Recommendations:
- After changing the relative humidity in the incubator, remember to reset the thermoneutral temperature.
- To prevent water condensation on the walls of the incubator, turn on the humidifier only when the temperature in the incubator has stabilized.
- Opening the doors of the incubator will cause a change in humidity and, consequently, condensation of water on the walls of the incubator. It is recommended to turn off the humidifier during the procedures.
- Demineralized sterile water must be used.
- In premature babies, water loss through the skin is 204g/kg of body weight per day! This parameter is normalized by 2 weeks after birth.
Skin Mode
Skin temperature must be between 36.8°C and 36.9°C
Example:
- Axillary temperature 36.
 8°C
8°C - Temperature in the right side of the abdomen 36.5°C
- Difference: 0.3°C
- The temperature of the incubator must be 36.7°C (temperature core 37°C minus 0.3°C equals 36.7°C).
There are some recommendations for "air mode":
- Raise the thermoneutral air temperature by 1°C as soon as the temperature difference between the room and the incubator reaches 7°C.
- Lower the thermoneutral air temperature by 0.5°C as soon as the humidity in the incubator rises from 25% to 75%.
- Lower the thermoneutral temperature if the child is clothed.
- Raise the temperature if the child is being manipulated in any way.
- Lower the temperature if the baby is lying quietly in the incubator.
What should be done if the child is too cold?
You need:
- Increase the air temperature in the incubator
- Increase the humidity in the incubator
- Dress a child
In hypothermia, heat loss exceeds heat production. Hypothermia increases the risk of developing hypoglycemia, respiratory distress syndrome, intraventricular hemorrhage in preterm infants. Hypothermia must be corrected immediately.
Hypothermia increases the risk of developing hypoglycemia, respiratory distress syndrome, intraventricular hemorrhage in preterm infants. Hypothermia must be corrected immediately.
To combat hypothermia:
- Put a cap on the child's head or cover the body with a plastic bag.
- Do not open the incubator doors.
- Increase the temperature in the incubator (gradually increasing by 0.5°C).
- Increase the relative humidity in the incubator.
- Place a plastic tunnel in the incubator to reduce heat transfer by radiation.
What should I do if my baby is too hot?
You need:
- Reduce the temperature in the incubator.
- Reduce the humidity in the incubator.
- Undress the child.
During hyperthermia, heat production exceeds heat transfer. Studies have shown that sometimes it is enough just to remove the cap from the child's head to prevent hyperthermia. If necessary, you can turn off the incubator and air humidifier until the temperature returns to normal.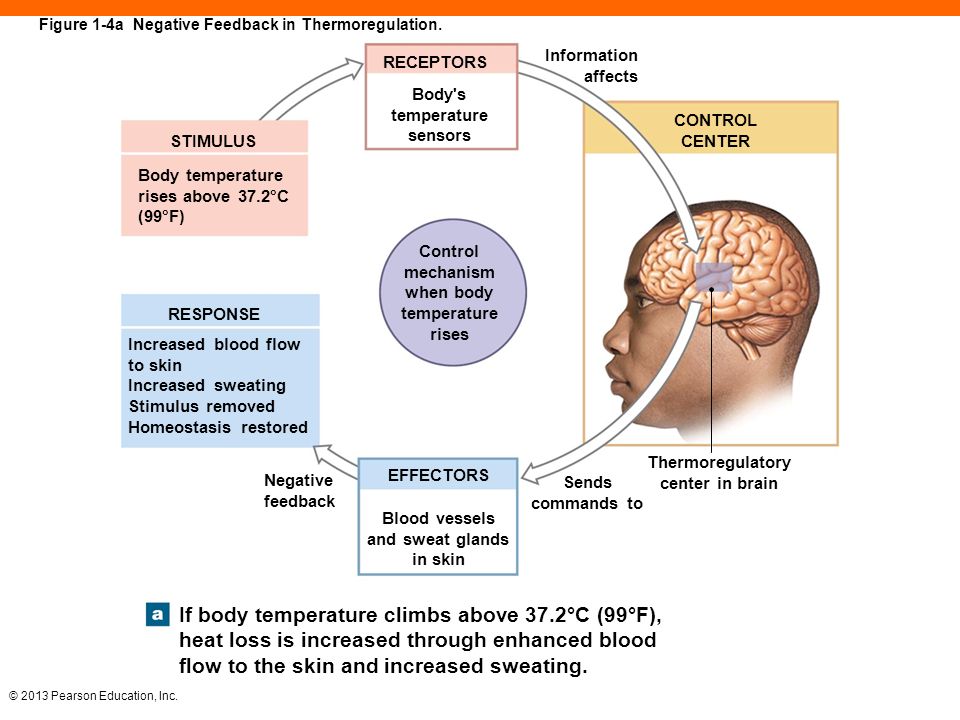
Sofya Anpilova
Development Manager
Child's temperature - measuring correctly | Mamovediya
Many parents are very much afraid of any change in the temperature of the child's body. And this is understandable, since any increase in the baby's body temperature can be a signal of negative changes in the body.
Parents need to know that, unlike adults, children have their own body temperature. In order to understand what the child's body temperature depends on and how to measure it correctly, it is necessary to have an idea of the mechanisms of formation and maintenance of body temperature.
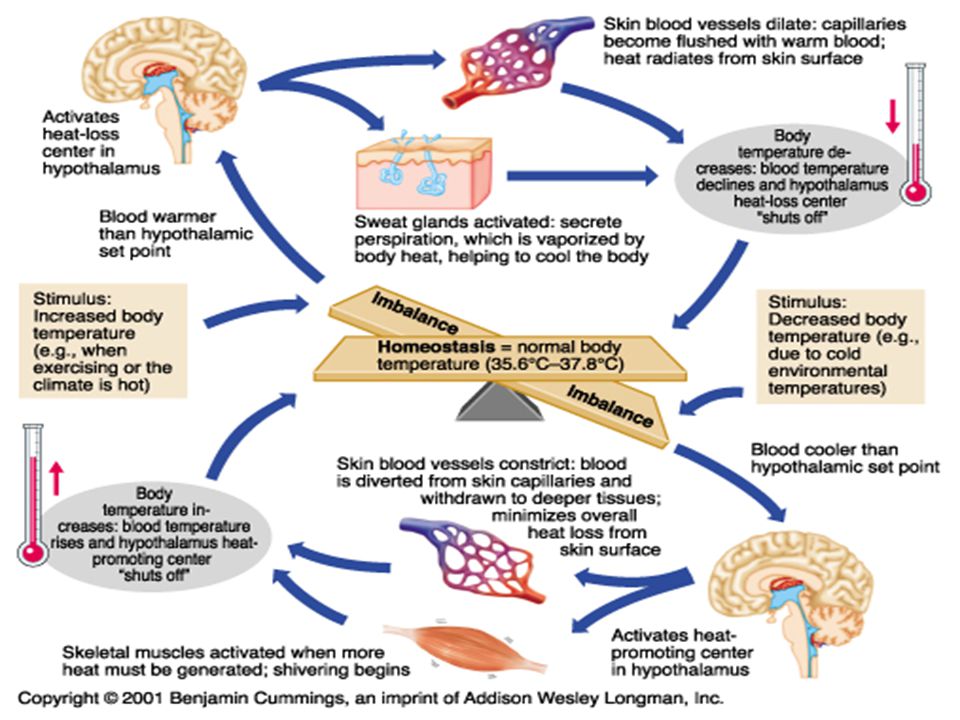
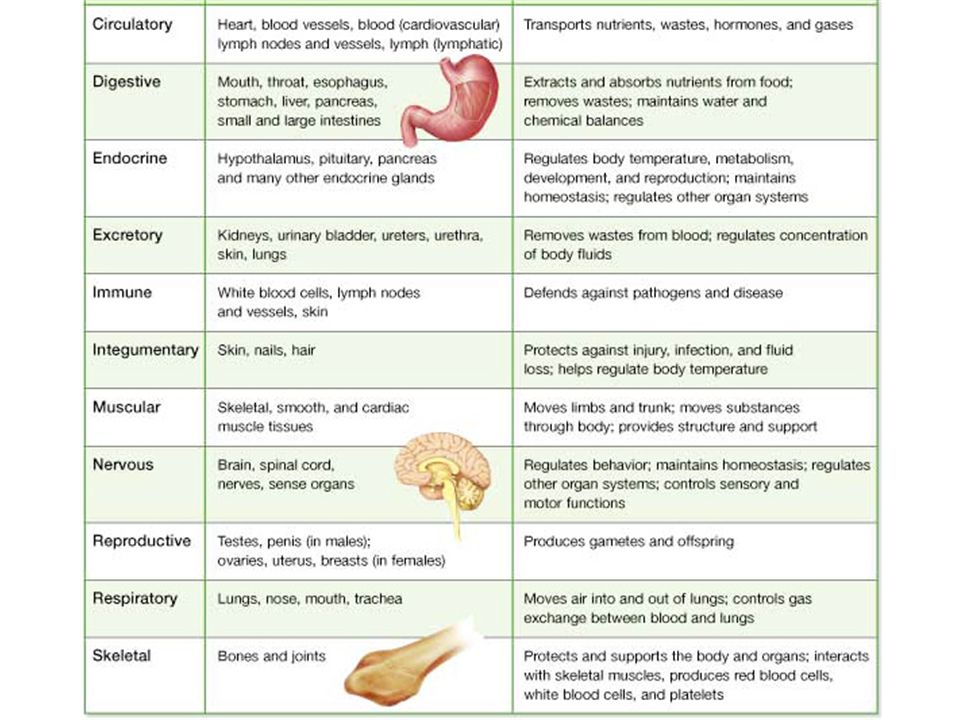
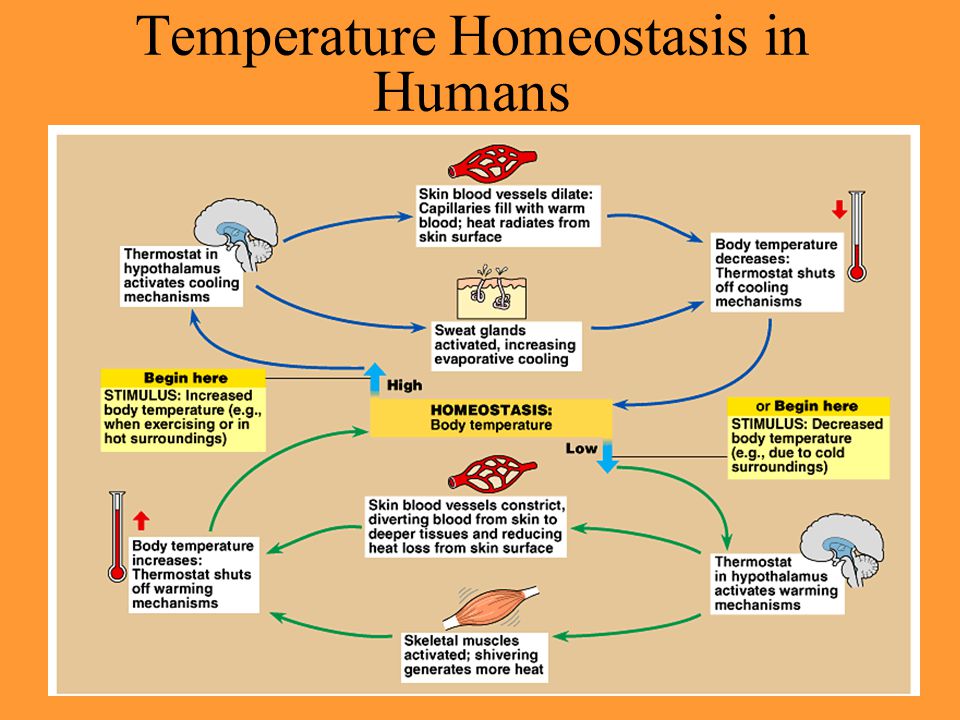
The process of maintaining body temperature in a child occurs due to the processes of heat production and heat transfer. In order for there to be a balance between heat production and heat transfer, a thermoregulation system works in the body, the center of which is located in the brain. An increase in body temperature in a child is caused by substances such as pyrogens that are in the blood.
A newborn baby has an immature nervous system, which explains the immaturity of the thermoregulatory system as well. Until the age of three months, it is quite difficult for a baby to regulate and maintain body temperature, and it fluctuates depending on indoor and outdoor conditions.
Most newborns may experience an increase in body temperature up to 38-39 degrees during the first days. This phenomenon is considered normal, because, thus, the child is adapting the body to exist in the external environment.
By the age of three months, the baby's thermoregulation system is gradually getting better. In a child, the maximum body temperature is observed in the afternoon, its peak reaches 16-18 hours, and the minimum usually occurs at night and in the morning.
How to measure the temperature of a child?
Firstly, the child's body temperature must be measured in a calm state, so the ideal state is when the child is sleeping.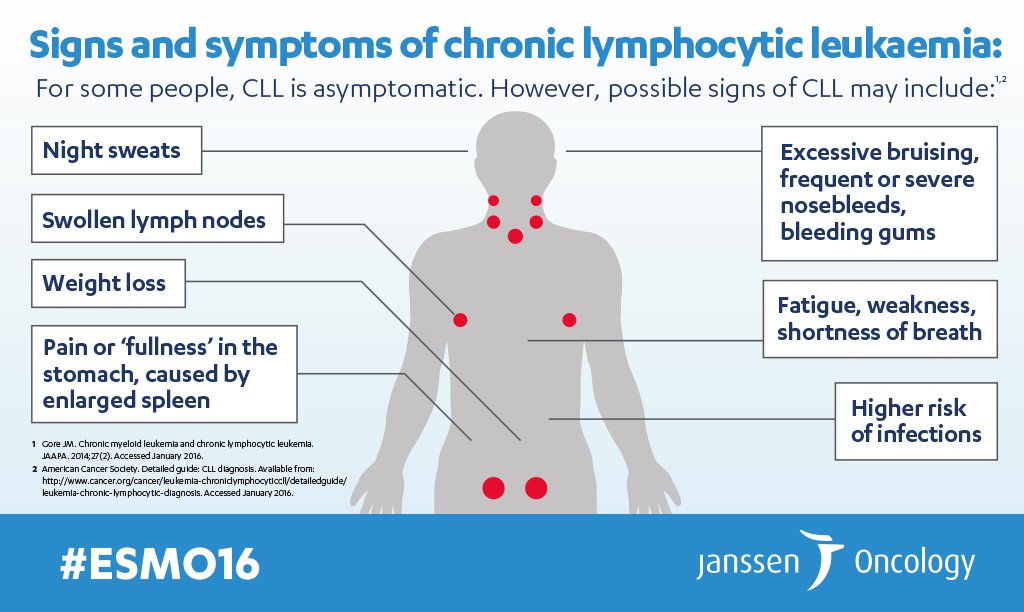 The baby should be picked up, or if the child is sleeping, then turn on its side.
The baby should be picked up, or if the child is sleeping, then turn on its side.
Next, it is very important to correctly install the thermometer. To do this, it must be placed between the arm and the body of the child on the side opposite from the mother.
Adequate temperature assessment is also very important. In order to correctly assess the condition of the child, it is necessary to have an idea of what indicators of the baby's body temperature can be considered normal.
Parents should remember that up to the age of seven, body temperature in the armpits is considered normal - 36.4-37.2 ° C, rectal - 36.9-37.5 ° C and oral - 36.6-37.2 °C.
In addition, the temperature in different parts of the child's body may differ, so the temperature in the axillary, inguinal or elbow folds will always be lower than oral and rectal. The difference in temperature in the armpit can be 0.2-0.3 degrees from the oral, and 0. 3-0.6 degrees from the rectal.
3-0.6 degrees from the rectal.
But, it is also worth considering the fact that the normal body temperature of each child will be individual. Therefore, try to take the temperature of a healthy child twice a day at about the same time during the week. By calculating the average readings of the thermometer, you can determine what temperature is normal for your baby.
There is a wide variety of thermometers available for children today, including mercury, digital, infrared, and thermometers. Each of them has its own advantages and disadvantages, and every mother has the right to choose the type of thermometer that will be more optimal and convenient for her.
However, to date, the most accurate and affordable is still a conventional mercury thermometer. Of course, it is dangerous in terms of use, but, nevertheless, it has many advantages. You can measure the temperature with a mercury thermometer only in the armpit.
Since an increase in the body temperature of a child, in most cases, can be a signal of illness, it is necessary to determine it accurately.