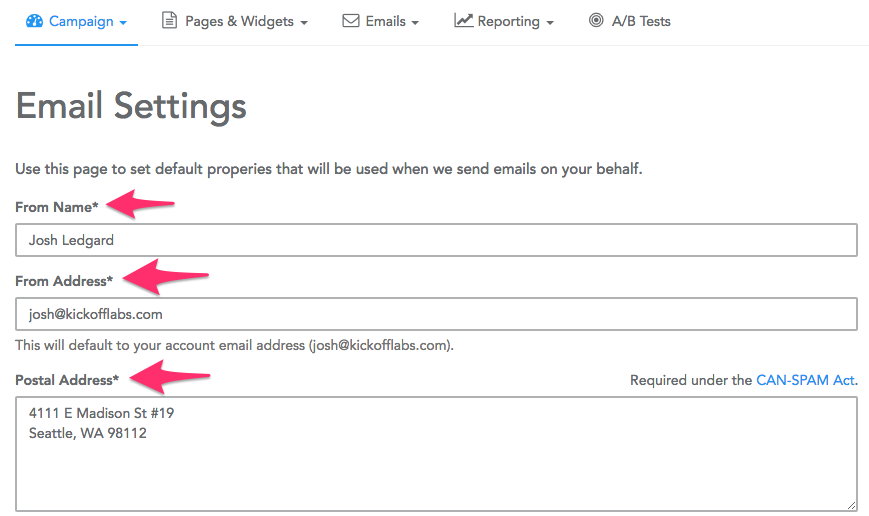
Non stop vomiting pregnancy
Severe vomiting in pregnancy - NHS
Sickness in pregnancy (sometimes called morning sickness) is common. Around 8 out of every 10 pregnant women feel sick (nausea), are sick (vomiting) or both during pregnancy. This does not just happen in the morning.
For most women, this improves or stops completely by around weeks 16 to 20, although for some women it can last longer.
Some pregnant women experience very bad nausea and vomiting. They might be sick many times a day and be unable to keep food or drink down, which can impact on their daily life.
This excessive nausea and vomiting is known as hyperemesis gravidarum (HG), and often needs hospital treatment.
Exactly how many pregnant women get HG is not known as some cases may go unreported, but it's thought to be around 1 to 3 in every 100.
If you are being sick frequently and cannot keep food down, tell your midwife or doctor, or contact the hospital as soon as possible. There is a risk you may become dehydrated, and your midwife or doctor can make sure you get the right treatment.
Symptoms of hyperemesis gravidarum
HG is much worse than the normal nausea and vomiting of pregnancy.
Signs and symptoms of HG include:
- prolonged and severe nausea and vomiting
- being dehydrated. Symptoms of dehydration include, feeling thirsty, tired, dizzy or lightheaded, not peeing very much, and having dark yellow and strong-smelling pee
- weight loss
- low blood pressure (hypotension) when standing
Unlike regular pregnancy sickness, HG may not get better by 16 to 20 weeks. It may not clear up completely until the baby is born, although some symptoms may improve at around 20 weeks.
See your GP or midwife if you have severe nausea and vomiting. Getting help early can help you avoid dehydration and weight loss.
Getting help early can help you avoid dehydration and weight loss.
There are other conditions that can cause nausea and vomiting, and your doctor will need to rule these out first.
See the healthtalk.org website for videos and written interviews of women talking about their experiences of hyperemesis gravidarum and how they coped.
What causes hyperemesis gravidarum?
It's not known what causes HG, or why some women get it and others do not. Some experts believe it is linked to the changing hormones in your body that occur during pregnancy.
There is some evidence that it runs in families, so if you have a mother or sister who has had HG in a pregnancy, you may be more likely to get it yourself.
If you have had HG in a previous pregnancy, you are more likely to get it in your next pregnancy than women who have never had it before, so it's worth planning in advance.
Treating hyperemesis gravidarum
There are medicines that can be used in pregnancy, including the first 12 weeks, to help improve the symptoms of HG. These include anti-sickness (anti-emetic) drugs, vitamins (B6 and B12) and steroids, or combinations of these.
You may need to try different types of medicine until you find what works best for you.
You can visit the Bumps website to find out which medicines are safe to use in pregnancy.
If your nausea and vomiting cannot be controlled, you may need to be admitted to hospital. This is so doctors can assess your condition and give you the right treatment to protect the health of you and your baby.
Treatment can include intravenous fluids, which are given directly into a vein through a drip. If you have severe vomiting, the anti-sickness drugs may also need to be given via a vein or a muscle.
The charity Pregnancy Sickness Support has information and tips on coping with nausea and vomiting, including HG.
Will hyperemesis gravidarum harm my baby?
HG can make you feel very unwell, but it's unlikely to harm your baby if treated effectively.
However, if it causes you to lose weight during pregnancy, there is an increased risk that your baby may be born smaller than expected (have a low birthweight).
Other symptoms you may experience
Pregnancy Sickness Support is in touch with many women who have had HG, and who report having some or all of the following symptoms in addition to the main symptoms listed above:
- extremely heightened sense of smell
- excessive saliva production
- headaches and constipation from dehydration
If you experience these symptoms, you are not alone. Many women have them and they will go away when the HG stops or the baby is born.
Many women have them and they will go away when the HG stops or the baby is born.
How you might feel
The nausea and vomiting of HG can impact your life at a time when you were expecting to be enjoying pregnancy and looking forward to the birth of your baby.
It can affect you both emotionally and physically. The symptoms can be hard to cope with. Without treatment HG may also lead to further health complications, such as depression or tears in your oesophagus.
Severe sickness can be exhausting and stop you doing everyday tasks, such as going to work or even getting out of bed.
In addition to feeling very unwell and tired, you might also feel:
- anxious about going out or being too far from home in case you need to vomit
- isolated because you do not know anyone who understands what it's like to have HG
- confused as to why this is happening to you
- unsure about how to cope with the rest of the pregnancy if you continue to feel very ill
If you feel any of these, do not keep it to yourself. Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to your partner, family and friends if you want to.
Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to your partner, family and friends if you want to.
If you want to talk to someone who has been through HG, you can contact Pregnancy Sickness Support's help section. They have a support network across the UK and can put you in touch with someone who has had HG.
Bear in mind that HG is much worse than regular pregnancy sickness. It is not the result of anything you have or have not done, and you do need treatment and support.
Another pregnancy
If you have had HG before, it's likely you will get it again in another pregnancy.
If you decide on another pregnancy, it can help to plan ahead, such as arranging child care so you can get plenty of rest.
You could try doing things that helped last time.
Talk to your doctor about starting medicine early.
Blood clots and hyperemesis gravidarum
Because HG can cause dehydration, there's also an increased risk of having a blood clot (deep vein thrombosis), although this is rare.
If you are dehydrated and immobile, there is treatment that you can be given to prevent blood clots.
Read more about how to prevent deep vein thrombosis.
Severe Morning Sickness (Hyperemesis Gravidarum) (for Parents)
What's Morning Sickness?
During the first trimester of pregnancy, many women have the bouts of nausea and vomiting known as morning sickness.
Despite its name, morning sickness can happen day or night. It usually starts around the 6th week of pregnancy, is at its worst around week 9, and stops by weeks 16 to 18. Although unpleasant, morning sickness is considered a normal part of a healthy pregnancy.
What’s Severe Morning Sickness?
Severe morning sickness is when nausea and vomiting get so serious that a pregnant woman vomits several times a day, loses weight, and gets dehydrated or is at risk for dehydration.
If this rare pregnancy-related condition isn’t treated, it can affect a woman's health and her baby's ability to thrive.
The medical term for severe morning sickness is "hyperemesis gravidarum" (hi-per-EM-eh-sis grav-ih-DARE-um), which means "excessive vomiting during pregnancy." It usually follows a similar timeline to normal morning sickness. But it can go longer, sometimes lasting for the whole pregnancy. Often, the symptoms get less severe as the pregnancy continues.
Most cases of hyperemesis gravidarum affect a woman's first pregnancy. But women who have it in one pregnancy are more likely to have it in future pregnancies.
What Causes Severe Morning Sickness?
The cause of severe morning sickness isn’t known. But it might be related to the hormone changes of pregnancy. A hormone called human chorionic gonadotropin, or HCG, might be to blame because severe morning sickness most often happens when HCG levels are at their highest in a pregnant woman's body.
A hormone called human chorionic gonadotropin, or HCG, might be to blame because severe morning sickness most often happens when HCG levels are at their highest in a pregnant woman's body.
Severe morning sickness also might run in families. It’s more common in women whose close family members (such as mothers and sisters) have had it.
Other things that can increase a woman's chances of having severe morning sickness include:
- carrying multiples (twins, triplets, etc.)
- history of motion sickness
- migraine headaches with nausea or vomiting
What Problems Can Happen?
The nausea and vomiting that happen in severe morning sickness are so extreme that they can harm the mother and the baby. Not being able to keep down food makes it hard for the mom to meet her nutritional needs. So she might lose weight. And a loss of fluids, combined with the loss of stomach acid from vomiting, can cause dehydration and electrolyte imbalances.
If severe morning sickness isn’t treated, it can cause many problems, including organ failure and the early birth of her baby.
When Should I Call the Doctor?
Call the doctor right away if you’re pregnant and have any of these symptoms:
- nausea that lasts throughout the day, making it impossible to eat or drink
- vomiting three to four times per day or not being to keep anything in the stomach
- brownish vomit or vomit with blood or streaks of blood in it
- weight loss
- fainting or dizziness
- peeing less than usual
- a fast heart rate
- a lot of headaches
- unpleasant, fruity mouth or body odor
- extreme tiredness
- confusion
How Is Severe Morning Sickness Treated?
Treatments used for morning sickness, such as eating dry crackers in the morning or a bland diet, may be recommended for women with extreme morning sickness. But these might not help with severe symptoms.
Medical treatment can include:
- a short period of not eating to rest the gastrointestinal system
- intravenous (IV) fluids
- vitamin and nutritional supplements
Some women might get medicine to stop the vomiting, either by mouth or through an IV. The doctor might recommend eating foods with ginger or taking vitamin B6 supplements to help ease nausea. It can also help to:
The doctor might recommend eating foods with ginger or taking vitamin B6 supplements to help ease nausea. It can also help to:
- Eat a bland diet.
- Eat frequent small meals.
- Drink plenty of liquids when not feeling nauseated.
- Avoid spicy and fatty foods.
- Eat high-protein snacks.
- Avoid sensory stimuli that can act as triggers (like specific smells or noises).
If a woman feels anxious or depressed about her condition, talking to a therapist or counselor might help her cope with her feelings.
What Else Should I Know?
With treatment, women with severe morning sickness can feel better and get the nourishment they need so they and their babies thrive. And lifestyle changes can help ease nausea and vomiting and make the pregnancy more enjoyable.
With time, symptoms usually do improve. And, of course, they stop by the time a woman's next journey starts: parenthood.
Toxicosis during pregnancy | Nutriclub
The first trimester is considered one of the most important in the process of bearing a child, but often this time is overshadowed by an unpleasant complication of pregnancy: toxicosis. The expectant mother may feel sick in the morning, she sometimes feels dizzy or salivation suddenly increases - and in general there may be unexpectedly many unpleasant symptoms. The good news is that this condition passes. You just need to know when it will happen and how you can help yourself.
The expectant mother may feel sick in the morning, she sometimes feels dizzy or salivation suddenly increases - and in general there may be unexpectedly many unpleasant symptoms. The good news is that this condition passes. You just need to know when it will happen and how you can help yourself.
What is toxicosis?
From a medical point of view, toxicosis (toxicosis) is a condition of a pregnant woman, which includes, in addition to nausea and vomiting, other unpleasant symptoms: muscle cramps, dermatitis, asthma during pregnancy, etc. But most often women experience nausea, therefore, in everyday life toxicosis is called morning sickness and vomiting. The causes of this condition are currently not fully understood, but there are a number of versions, among which the following are recognized as the main ones:
Neuro-reflex theory
The meaning of the theory is that during pregnancy, the growing fetus irritates the receptors of the uterine tissues, and this leads to irritation of the subcortical structures of the brain, including the vomiting center (as well as the olfactory center, areas that regulate the activity digestion, circulation, respiration, secretion, etc. ). In response to this irritation, the whole complex of symptoms of toxicosis can occur: nausea, vomiting, palpitations, salivation, pallor of the skin, etc. By the end of the first trimester, these symptoms disappear because the body of a pregnant woman is adapting to such irritations.
). In response to this irritation, the whole complex of symptoms of toxicosis can occur: nausea, vomiting, palpitations, salivation, pallor of the skin, etc. By the end of the first trimester, these symptoms disappear because the body of a pregnant woman is adapting to such irritations.
Hormonal theory
Explains the occurrence of toxicosis of pregnant women by increased production of a specific pregnancy hormone - human chorionic gonadotropin (hCG), which is responsible for the normal growth and development of the placenta. According to this theory, after three months of pregnancy, the intensity of hCG production decreases, and the symptoms of toxicosis disappear.
Immunological theory
There is a version that the cause of toxicosis can be immunological reactions: the growing fetus is a foreign organism for the mother, and her immune system reacts to the fetus by producing antibodies, which lead to symptoms of toxicosis.
Psychogenic theory
Explains the occurrence of symptoms of toxicosis in especially impressionable women by the experiences associated with pregnancy.:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg)
How does toxicosis manifest itself?
Weakness, drowsiness, irritability, fatigue, loss of appetite, strong salivation and nausea in the morning are sure signs of toxicosis. Of course, it is not at all necessary that a pregnant woman is guaranteed to experience all of the listed symptoms. For example, some women at the beginning of pregnancy constantly want to sleep, and at the same time they do not feel sick at all. For others, the taste may change, and familiar foods may suddenly start to cause nausea or vomiting. Symptoms of toxicosis also include mild dizziness, weight loss, spasms of the calf muscles.
Depending on the intensity of symptoms, toxicosis can be:
- Mild
A pregnant woman vomits no more than 5 times a day. Urine and blood tests are normal, and weight loss does not exceed 2 kg per week.
- Moderate
A woman vomits up to 10 times a day, she loses 3-5 kilograms per week. In this case, there may also be a slight increase in temperature and pulse rate, sleep disturbance and constant nausea during the day.
- Severe toxicosis or intractable vomiting (Hyperemesis Gravidarum)
The state when it is time to sound the alarm. In this case, nausea and vomiting (or the urge to vomit, since food and liquid are practically not retained in the stomach) are constant throughout the day. Indomitable vomiting is dangerous because it threatens a pregnant woman with dehydration.
When does toxicosis start and when does it go away?
Most often, early toxicosis begins at 4-5 weeks of pregnancy and lasts up to 12-16 weeks, although the timing of manifestation is always very individual. Doctors orient expectant mothers to the fact that at 12-14 weeks (the beginning of the second trimester) there is a chance to say goodbye to unpleasant sensations and return to the usual rhythm of life. In rare cases, symptoms persist into the 2nd trimester and continue into the third. However, late toxicosis of pregnant women, which develops in the second half of pregnancy, is considered a more dangerous condition, called preeclampsia, and is treated in a hospital.
What can help you cope with the symptoms of toxicosis?
At the onset of early toxicosis, it is necessary to consult a doctor: like any problematic condition during pregnancy, toxicosis requires medical supervision. In most cases, with a mild degree of toxicosis, there is no need to prescribe drug therapy. The fact is that many medications can affect the intrauterine development of the child. In order to somehow alleviate her condition during toxicosis, the expectant mother can:
- Walk more - if possible, spend half the day outside. When returning home or going to work, it is better to leisurely walk a few stops on foot than to take public transport. If a woman travels by car more often, it is better for her to leave herself time for evening or morning walks. Fresh air is important for the health of a pregnant woman and often helps to relieve nausea.
- In the morning, drink small sips of water left by the bed in the evening. It's best to do this before you get up.
 Also, in this case, you can put a slice of lemon, a cracker, cookies, bread next to it - in a word, look for something that will help you get up and not feel instant nausea. The choice must be individual.
Also, in this case, you can put a slice of lemon, a cracker, cookies, bread next to it - in a word, look for something that will help you get up and not feel instant nausea. The choice must be individual. - Fruit or vegetable smoothies to taste - a good solution if breakfast in pieces causes nausea.
- Eat small meals 6-8 times a day, not three large meals a day. Low-fat yogurt, apples, and other healthy foods often save the day and keep nausea at bay.
- Ginger or mint tea also helps with nausea.
- Playing sports can also help to cope with bouts of nausea (the level of endorphins rises, and the expectant mother begins to feel better). However, all physical activity must be agreed with the doctor leading the pregnancy.
When is toxicosis dangerous and what to do in emergency cases?
In most cases, toxicosis is not dangerous and goes away on its own by the beginning of the second trimester. You can sympathize with a woman in the first trimester: she is not yet entitled to maternity leave, and she needs to go to work in this state. However, there are cases when a woman needs not psychological, but medical help.
However, there are cases when a woman needs not psychological, but medical help.
- Indomitable vomiting (Hyperemesis Gravidarum)
This is a reason to see a doctor. With a severe course of toxicosis, constant indomitable vomiting and severe weight loss, a woman needs to be hospitalized. The hospital will help her manage her fluid loss with saline and glucose drips, as well as protein, vitamins, antiemetics, and drugs to help protect and improve liver function.
- Late toxicosis (preeclampsia) of pregnant women
May start after 20 weeks, is very dangerous and requires medical supervision and assistance. It is manifested by severe edema, increased pressure and the appearance of protein in the urine. Preeclampsia can be accompanied by serious complications and threatens both the life of the mother and the life of the child. This condition requires careful medical supervision.
In an emergency, do not waste time and call your doctor. The conviction that pregnancy is not a disease should not become an obstacle to contacting doctors. In normal times - yes, indeed, pregnancy is not dangerous and the expectant mother can work, travel and do her favorite things with virtually no restrictions. But in cases of severe toxicosis, it is better to be vigilant.
The conviction that pregnancy is not a disease should not become an obstacle to contacting doctors. In normal times - yes, indeed, pregnancy is not dangerous and the expectant mother can work, travel and do her favorite things with virtually no restrictions. But in cases of severe toxicosis, it is better to be vigilant.
When using any materials from the site nutriclub.ru, a link to the site is required.
© Nutriclub, 2020
Termination nausea
Photo author, PA
Caption before pregnancy; in the worst cases, women must remain in bedAn estimated 10,000 pregnant women each year suffer from acute nausea and vomiting - a condition known as hyperemesis gravidarum - much more severe than the usual morning sickness that occurs every third expectant mother.
In particular, the Duchess of Cambridge suffers from hyperemesis and is due to give birth to her second child soon.
Her problems with pregnancy brought attention to this serious condition, which sometimes causes women to spend days in bed and throw up thirty times a day. But for 10% of patients, the symptoms of hypermesis are simply unbearable.
They feel they have no choice but to terminate the pregnancy.
British charity Pregnancy Sickness Support has published a report on various cases of pregnancy hyperemesis called "I Can't Survive Another Day". The data presented in the document indicate that a large number of pregnant women do not receive the necessary care and treatment.
The report is based on the stories of 70 British women who, over the past 10 years, have decided to terminate a pregnancy due to extreme nausea.
"Really Bad"
The experience of these women is that general practitioners and antenatal clinics are sometimes unwilling to prescribe medication for nausea or acknowledge the severity of the condition.
Lily (not her real name) knows what severe hyperemesis is.
My first pregnancy was "really bad, but I endured it," she says.
For the first few months she lay in bed, could only take a few sips of water and vomited up to 30 times a day. She suffered from dehydration and hunger, losing a total of 19 kg in weight during this period.
"I was very weak and could not stand on my feet, I was dizzy. I could not stand any smell of food - what's there, even the smell of my husband made me sick."
"I remember once I tried to swallow some beans - but they came back in a matter of seconds."
Sometimes a therapist came to Lily and prescribed medicines for her nausea, but they did not help.
Finally, after 22 weeks of pregnancy, the disease gradually subsided, and vomiting occurred only once a day.
In 2011, Lily's daughter was born.
"I begged the doctors for steroids"
But a few months later she became pregnant again, and this time she could not even drink water - she was so sick.
She was very ill, and since there was a child at home, she simply could not take care of herself.
"I begged the doctors for steroids (they are sometimes prescribed for women who are not helped by other anti-nausea drugs), but we had just moved, I did not have an up-to-date urinalysis, and I was not admitted to the hospital for rehydration therapy."
Image copyright, Getty
Caption to photo,The Duchess of Cambridge is one of those women who suffers from hyperemesis
0002 Headline story as our journalists explain
Episodes
End podcast
According to the report, women are sometimes told that steroids can harm the fetus or are too expensive.
Fewer than one in ten women were offered steroid treatment; 47% of the women interviewed said that they were either denied such treatment in response to their request, or simply did not remember about it.
According to Caitlin Dean, director of Pregnancy Sickness Support, many women are wrongly convinced that there are no safe drugs for pregnant women. Sometimes this belief is reinforced by their doctors.
"But there are actually quite a few medicines that are both safe and effective. Some of them have been known for over 50 years."
"There is plenty of evidence that they do not cause any problems."
Dr. Dagny Rajasingham, Consultant Obstetrician at St Thomas' Hospital in London and Fellow of the Royal College of Obstetricians and Gynecologists, states that hyperemesis gestationis is a well-known condition that should be taken seriously.
"First, women should be given anti-nausea pills, then hospitalized for intravenous rehydration and nutrition if necessary, and in very severe cases, steroids."
Awareness of hyperemesis will help doctors and midwives be more empathetic towards patients with acute nausea, she adds.
"We must give every pregnant woman a guarantee that she will have someone to discuss these problems with."
No choice
Lily gave up her efforts to get better medical care during her second pregnancy, as all her strength was spent on daily survival.
In the end, it seemed to her that there was no choice.
"With all our maternal instincts, it would take desperation to end a child's life."
Image copyright, ivanmikhailov
Photo caption,Even plain water can cause severe nausea in women with severe hypermesis
"I really felt like I was about to stretch my legs."
A woman says she doesn't want to have any more children and is afraid of getting pregnant.
"I don't trust doctors. They don't take this problem seriously enough, so it ends up with just another abortion."
As for Caitlin Dean, she had three pregnancies with hyperemesis, but thanks to a competent doctor and good medical care before and after conception, the third pregnancy was much easier.