How to lose a baby in your stomach
Miscarriages (for Parents) - Nemours KidsHealth
What Is a Miscarriage?
A miscarriage is the loss of a pregnancy (the loss of an embryo or fetus before it's developed enough to survive). This sometimes happens even before a woman knows she is pregnant. Unfortunately, miscarriages are fairly common.
A miscarriage usually happens in the first 3 months of pregnancy, before 12 weeks' gestation. A very small number of pregnancy losses are called stillbirths, and happen after 20 weeks’ gestation.
What Happens During a Miscarriage?
Often, a woman can have an extra heavy menstrual flow and not realize it’s a miscarriage because she hadn’t known she was pregnant.
Some women who miscarry have cramping, spotting, heavier bleeding, abdominal pain, pelvic pain, weakness, or back pain. Spotting does not always mean a miscarriage. Many pregnant women have spotting early in the pregnancy and go on to have a healthy baby. But just to be safe, if you have spotting or any of these other symptoms anytime during your pregnancy, talk with your doctor.
What Is Stillbirth?
Many experts define a stillbirth as the death of a baby after the 20th week of pregnancy. It can happen before delivery or during labor or delivery. A stillbirth also is sometimes referred to as intrauterine fetal death or antenatal death.
There are some known risk factors for stillbirth, such as smoking, obesity, problems with the placenta, a pregnancy lasting longer than 42 weeks, and some infections. But the cause of many stillbirths isn’t found.
The most common sign of a stillbirth is decreased movement in the baby. If you notice your baby moving less than usual, call your doctor right away. Your doctor can use an ultrasound to look for the heartbeat or, later in pregnancy, give you a fetal non-stress test. This involves lying on your back with electronic monitors on your abdomen. The monitors record the baby's heart rate and movements, and contractions of the uterus.
Why Do Miscarriages Happen?
The most common cause of pregnancy loss is a problem with the chromosomes that would make it impossible for the fetus to develop normally.
Other things that could play a role include:
- low or high hormone levels in the mother, such as thyroid hormone
- uncontrolled diabetes in the mother
- exposure to environmental and workplace hazards, such as radiation or toxic agents
- some infections
- uterine abnormalities
- incompetent cervix, which is when the cervix begins to open (dilate) and thin (efface) before the pregnancy has reached term
- the mother taking some medicines, such as the acne drug Accutane
A miscarriage also can be more likely in pregnant women who:
- smoke, because nicotine and other chemicals in the mother’s bloodstream cause the fetus to get less oxygen
- drink alcohol and or use illegal drugs
What Happens After a Miscarriage?
If a woman miscarries, her doctor will do a pelvic exam and an ultrasound to confirm the miscarriage. If the uterus is clear of any fetal tissue, or it is very early in the pregnancy, many won’t need further treatment.
Sometimes, the uterus still contains the fetus or other tissues from the pregnancy. A doctor will need to remove this. The doctor may give medicine to help pass the tissue or may dilate the cervix to do:
- a dilation and curettage (D&C), a scraping of the uterine lining
- a dilation and extraction (D&E), a suction of the uterus to remove fetal or placental tissue
A woman may have bleeding or cramping after these procedures.
If a baby dies later in a woman’s pregnancy, the doctor might induce labor and delivery. After the delivery, the doctor will have the baby and the placenta examined to help find the cause of death if it's still unknown.
Women who have had several miscarriages may want to get checked to see if any anatomic, genetic, or hormonal problems are making miscarriages more likely.
Can Miscarriages Be Prevented?
In most cases, a miscarriage cannot be prevented because it’s caused by a chromosomal abnormality or problem with the development of the fetus. Still, some things — such as smoking and drinking — put a woman at a higher risk for losing a pregnancy.
Still, some things — such as smoking and drinking — put a woman at a higher risk for losing a pregnancy.
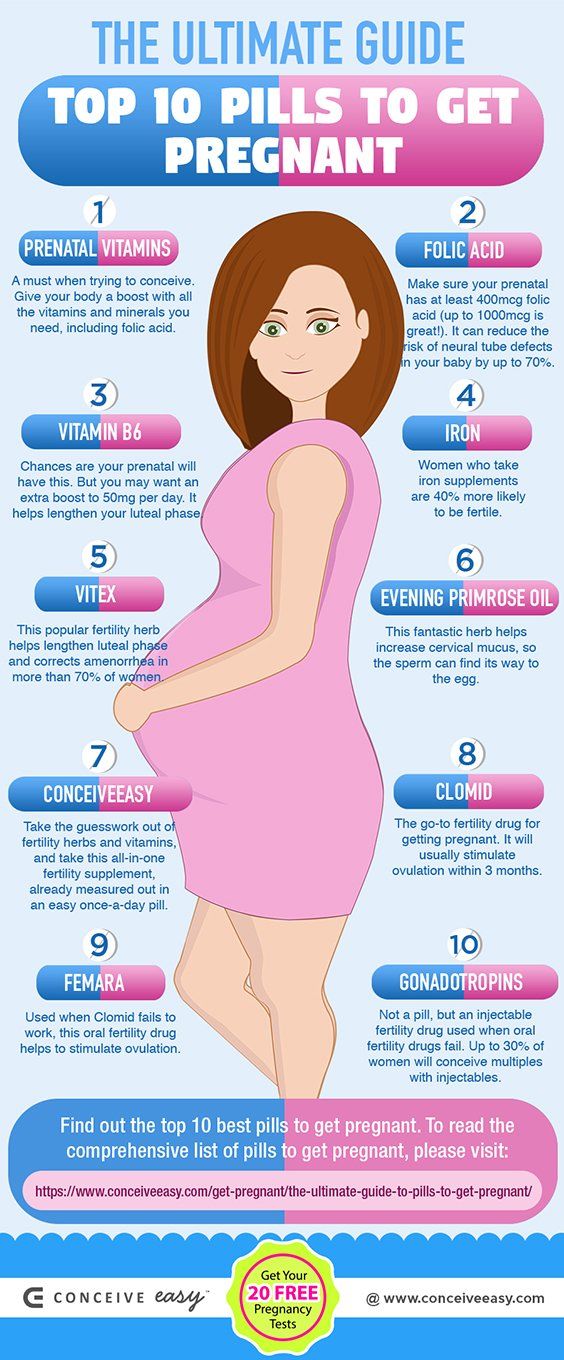
Good prenatal care can help moms and their babies stay healthy throughout the pregnancy. If you’re pregnant:
- Eat a healthy diet with plenty of folic acid and calcium.
- Take prenatal vitamins daily.
- Exercise regularly after you've gotten your doctor's OK.
- Keep a healthy weight. Pregnant women who are overweight or too thin may be more likely to have miscarriages.
- Avoid drugs and alcohol.
- Avoid deli meats and unpasteurized soft cheeses such as feta and other foods that could carry listeriosis.
- Limit caffeine intake.
- If you smoke, quit.
- Talk to your doctor about all medicines you take. Unless your doctor tells you otherwise, many prescription and over-the-counter medicines should be avoided during pregnancy.
- Avoid activities that could cause you to get hit in the belly.
- Make sure you’re up to date on all recommended vaccines.
- Know your family medical and genetic history.
- Go to all of your scheduled prenatal visits and discuss any concerns with your doctor.
- Call your doctor right away if you have fever; feel ill; notice the baby moving less; or have bleeding, spotting, or cramping.
Trying Again After a Miscarriage
If you've had a miscarriage, take time to grieve. The loss of a baby during pregnancy is like the loss of any loved one. Give yourself time to heal emotionally and physically. Some health care providers recommend that women wait one menstrual cycle or more before trying to get pregnant again.
Some other things that can help you get through this difficult time:
- Find a support group. Ask your doctor about local support groups for women who are trying again after a loss.
- Find success stories. Other women who have had a successful pregnancy after having a miscarriage can be a great source of encouragement.
 Your doctor might know someone to talk with.
Your doctor might know someone to talk with.
During future pregnancies, it can help to:
- Be proactive. The more you know about the medical aspects of your pregnancy, the better you'll be able to discuss treatment options and outcomes with your doctor.
- Monitor the baby's movements. If you're far enough along to feel kicks and jabs — usually between 18 and 22 weeks — keep a log of the baby's activities each morning and night and report any changes or lack of movement to your doctor. If your baby isn't moving, eat or drink something sugary and lie down on your side. You should feel at least 10 movements in a 2-hour period. If you don't, call your doctor right away.
- Try not to compare. No two pregnancies are exactly alike, so try not to dwell on any similarities between this pregnancy and the one that ended in a loss.
- Stay positive. Envision a good end to help you stay positive.

Reviewed by: Larissa Hirsch, MD
Date reviewed: October 2020
Your post-baby belly: why it's changed and how to tone it
In this article
- Why do I still look pregnant?
- How long will it take for my belly to shrink back to normal?
- How can I safely lose weight to help my belly look better?
- What else can I do to help regain my pre-pregnancy belly?
- My tummy muscles feel slack. Is this normal?
Why do I still look pregnant?
It takes time for your body, and especially your tummy, to fully recover from pregnancy. You've had your baby, but you may look as if you're still six months pregnant, with a tummy that's squishier and rounder than you expected.
Imagine your tummy as a balloon, slowly inflating as your baby grows. Giving birth doesn't pop the balloon, it just starts a slow leak. The decrease in your tummy size may be slow, but it will be steady.
From the moment your baby is born, hormonal changes cause your tummy to decrease in size. However, it takes another six to eight weeks for your womb (uterus) to contract to its pre-pregnancy size (Berens 2019).
The extra fluid that built up in your body during pregnancy will gradually decrease, reducing swelling and bloating (Berens 2019). And any extra fat you put on to nourish your baby will start to burn off, especially if you're breastfeeding and exercising (Berens 2019). But it takes at least a few weeks to see noticeable results.
After giving birth you may still have a dark line down your tummy called a linea nigra, as well as a web of stretch marks.
The linea nigra is caused by pigmentation in the skin where your tummy muscles have stretched and slightly separated, to accommodate your baby as she grew (APA nd). This line of pigmentation usually fades within a few months of giving birth (APA nd).
Stretch marks are caused by your skin stretching over your fast-growing body during pregnancy (NHS 2019c). You may have them on your tummy, thighs and breasts (NHS 2019c).
You may have them on your tummy, thighs and breasts (NHS 2019c).
You can't get rid of stretch marks completely, but they will fade over time. Eventually, the lines will look like fine streaks that are closer to your skin colour (NHS 2019c). Try to be patient. You may not like your stretch marks now, but they will look a lot better in six months' time.
How long will it take for my belly to shrink back to normal?
We've all heard stories of new mums who regain their pre-pregnancy bodies within weeks of giving birth. Although this is possible, it doesn't happen that way for most mums. Bear in mind that your body may change shape after pregnancy. You may find it difficult to return to your exact pre-pregnancy weight or shape.
Patience is the key. It took nine months for your tummy muscles to stretch to accommodate a full-term baby. So it makes sense that it can take weeks or months to tighten up again (Berens 2019).
The speed and degree of this tightening up depends on a few factors, including:
- What shape and size you were before you conceived your baby.

- How much weight you gained during pregnancy (NICE 2010).
- How active you are (NICE 2010).
- Something you can't do anything about: your genes.
You may find it easier to shed the weight if:
- You gained less weight than average during pregnancy.
- You breastfeed.
- This is your first baby.
(Berens 2019)
Most women don’t get back to their pre-pregnancy weight until about six months after their baby's birth (IQWiG2018, Adegboye et al 2013).
How can I safely lose weight to help my belly look better?
Breastfeeding may help, especially in the early months after giving birth. If you breastfeed, you'll burn extra calories to make milk – about 300 calories a day (NHS nd), though the exact amount is different for everyone. You may lose your pregnancy weight more quickly than mums who formula-feed their babies but it’s not guaranteed (Jarlenski et al 2014).
Breastfeeding also triggers contractions that help to shrink your womb, which may help you to get in shape faster. However, if you eat more than you burn off, you will put on weight, even if you breastfeed (Adegboye et al 2013).
It's fine to lose weight while you are breastfeeding. Your body is very efficient at making milk, and losing up to 1kg (about 2lb) a week shouldn't affect the amount of milk you make (Adegboye et al 2013, NICE 2010).
However, if you have a newborn to look after, you'll need plenty of energy. Trying to lose weight too soon after giving birth may delay your recovery and make you feel even more tired (IQWiG 2018). It’s especially important not to attempt a very low-calorie diet (NHS 2019a). So try to wait until you've had your postnatal check before trying to lose weight (NICE 2010).
Eating healthily, combined with gentle exercise, will help you to get in shape (Adegboye et al 2013). The following general guidelines will help you to achieve and maintain a healthy weight:
- Make time for breakfast.

- Eat at least five portions of fruit and vegetables a day.
- Include plenty of fibre-rich foods, such as oats, beans, lentils, grains and seeds, in your diet.
- Include a starchy food such as bread, rice, pasta (preferably wholegrain varieties for added fibre) or potatoes in each meal.
- Go easy on high-fat and high-sugar foods, such as biscuits, cakes, fast food and takeaways.
- Watch your portions at mealtimes and the number and type of snacks you eat between meals (NICE 2010).
There's no right answer about how many calories a day you should have. The amount you need to eat depends on your weight and how active you are (Amorim Adegboye et al 2013). For more tips on healthy weight loss after birth, see our diet for a healthy breastfeeding mum and parents' tips for managing your weight after having a baby.
What else can I do to help regain my pre-pregnancy belly?
Exercise can help to tone stomach muscles and burn calories (Evenson et al 2014, Amorim Adegboye et al 2013). You can do light exercise like walking and stretching even in the early weeks after having your baby (POGP 2017).
You can do light exercise like walking and stretching even in the early weeks after having your baby (POGP 2017).
If you stopped exercising during your pregnancy or are a newcomer to fitness, start slowly and gradually build up your exercise levels (POGP 2015).
Fitness aside, all new mums can begin pelvic floor exercises and work on gently toning up lower tummy muscles as soon as they feel ready (Evenson et al 2014, POGP 2017). This may help you to get back to your pre-pregnancy shape and help to flatten your tummy (POGP 2017).
When you feel up to it, take your baby out for walks in his buggy (Evenson et al 2014). Getting out and about will help to lift your mood and exercise your body gently (Evenson et al 2014, NHS 2019b). You may find there are buggy workouts with other new mums in your local park.
Read about toning up after a caesarean.
Postnatal exercises: abdominals
If your stomach muscles have separated, or you just want to tone your post-baby belly, try these easy exercises. More postnatal exercise videos
More postnatal exercise videos
My tummy muscles feel slack. Is this normal?
If your tummy muscles feel very slack, it could be because pregnancy has over-stretched them (St George's Healthcare 2018, Berens 2019). If this is the case, you may also notice a bulge developing on the front of your tummy, above and below your belly button (St George's Healthcare 2018).
The medical term for this over-stretching is diastasis recti (DR) (St George's Healthcare 2018). Diastasis simply means separation.
There are four layers of muscle across your tummy. The top layer is a pair of long, flat muscles that run vertically down each side of your abdomen (rectus abdominis), commonly known as the six-pack (Guy's and St Thomas' 2014). DR happens when the two halves pull away from each other, stretching and thinning the connective tissue between them (St George's Healthcare 2018).
At least half of women experience DR after having a baby (St George's Healthcare 2018). It's more likely to happen if you:
It's more likely to happen if you:
- have given birth more than once (Nahabedian and Brooks 2019)
- had twins or more (Donnelly 2019, Nahabedian and Brooks 2019)
- have had more than one caesarean birth (Nahabedian and Brooks 2019)
- regularly strained your abdominal muscles during pregnancy through frequent heavy lifting (Sperstad et al 2016), straining on the toilet, or chronic coughing or vomiting (Donnelly 2019)
There's not enough research to tell us whether being obese before pregnancy, or gaining a lot of weight during pregnancy, also makes DR more likely (Nahabedian and Brooks 2019).
It's likely that DR may run in families (Donnelly 2019), so if your mother or sister has DR, you're more likely to develop it too.
If you’re unsure whether you have DR, here's how to check:
- Lie on your back, with your knees bent and your feet flat on the floor or bed.
- Place your palm down on your tummy, just below or above your belly button.

- Lift your shoulders off the floor slightly and look down at your stomach. With the tips of your fingers, feel between the edges of the muscles, both above and below your belly button.
- See how many fingers you can fit into the gap between the muscles. The number of finger widths is the size of your diastasis. Do the test regularly - as your muscles get stronger, the gap should reduce.
(NHS 2019d)
If the gap you feel is bigger than two finger-widths, you may have DR (Nahabedian and Brooks. 2019).
The separation gap often returns to normal within the first eight weeks after giving birth (NHS 2019d, St George’s Healthcare 2018). If the size of the gap hasn’t decreased, or you’re worried about it, see your GP or health visitor. She may be able to refer you to a women's health physiotherapist who can give you specific exercises to help you (NHS 2019d). In some areas of the UK, you may be able to refer yourself directly for physio.
Leaving DR untreated isn't harmful, but it may weaken your abdominal core. This can increase your chances of getting a bad back and will make exercise and other activities more difficult (Hills et al 2018, Nahabedian and Brooks 2019).
More information:
- Find out more about diastasis recti.
- Check out these real-life post-baby belly pics.
- See Sarah Cawood's brutally honest diastasis recti journey.
- Learn more about exercising after having a baby.
References
Amorim Adegboye AR and Linne YM. 2013. Diet or exercise, or both, for weight reduction in women carrying excess weight after childbirth. Cochrane Database Of Systematic Reviews. www.cochrane.org [Accessed December 2019]
APA. nd. Pregnancy line – linea nigra. American Pregnancy Association. americanpregnancy.org [Accessed January 2020]
Berens P. 2019. Overview of the postpartum period: physiology, complications and maternal care. UpToDate www.uptodate.com [Accessed January 2020]
UpToDate www.uptodate.com [Accessed January 2020]
Donnelly G. 2019. Rectus diastasis awareness. ROAR #pelvicroar. www.pelvicroar.org [Accessed June 2019]
Evenson KR, Mottola MF, Owe KM et al. 2014. Summary of international guidelines for physical activity after pregnancy. Obstet Gynaecol Surv. Jul; 69 (7): 407-14 [Accessed December 2019]
Guy's and St Thomas'. 2014. Divarication of rectus abdominis muscles (DRAM) postpartum. Physiotherapy department patient information. Leaflet number: 3913/VER1. www.guysandstthomas.nhs.uk
Hills NF, Graham RB, McLean L. 2018. Comparison of trunk muscle function between women with and without diastasis recti abdominis at 1 year postpartum. Phys Ther 98(10):891-901.
Jarlenski M, Bennett W, Bleich S et al. 2014. Effects of breastfeeding on postpartum weight loss among US women. Prev Med, Dec 2014, pages 146-50 [accessed December 2019]
Nahabedian M, Brooks DC. 2019. Rectus abdominus diastasis. UpToDate. www.uptodate.com [Accessed June 2019]
UpToDate. www.uptodate.com [Accessed June 2019]
NHS. nd. Your questions answered. NHS Start4Life, Breastfeeding. www.nhs.uk [Accessed January 2020]
NHS. 2017. Benefits of breastfeeding NHS,. Health you’re your pregnancy and baby guide. www.nhs.uk [Accessed December 2019]
NHS. 2019a. Very low calorie diets. NHS. Live Well. www.nhs.uk [Accessed December 2019]
NHS. 2019b. Keeping fit and healthy with a baby. NHS, Health A to Z, Your pregnancy and baby guide. www.nhs.uk [Accessed December 2019]
NHS. 2019c. Stretch marks in pregnancy. NHS,. Health A to Z. www.nhs.uk [Accessed December 2019]
NHS. 2019d. Your post-pregnancy body. NHS, Health A-Z, Your pregnancy and baby guide. www.nhs.uk [Accessed December 2019]
NICE. 2010. Weight management before, during and after pregnancy. National Institute for Health and Care Excellence. NICE public health guidance 27. www.nice.org.uk [.pdf file, accessed December 2019]
POGP. 2015. Fit and safe to exercise in the childbearing year. Pelvic Obstetric and Gynaecological Physiotherapy. www.pogp.csp.org.uk [accessed December 2019]
2015. Fit and safe to exercise in the childbearing year. Pelvic Obstetric and Gynaecological Physiotherapy. www.pogp.csp.org.uk [accessed December 2019]
POGP. 2017. Fit for the future – essential advice and exercises following childbirth. Pelvic Obstetric & Gynaecological Physiotherapy. www.pogp.csp.org.uk [accessed December 2019]
IQWiG. 2018. <Weight gain in pregnancy. Institute for Quality and Efficiency in Health Care, Informed Health, Pregnancy and birth. www.informed health.org [Accessed January 2020]
Sperstad JB, Teefjord MK, Hilde G, et al. 2016. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med 50(17):1092-6. bjsm.bmj.com [Accessed June 2019]
St George’s Healthcare. 2018. Rectus abdominus diastasis. St George’s Healthcare NHS Trust. www.stgeorges.nhs.uk [Accessed January 2020]
Show references Hide references
Why is it so important for us to talk about the loss of a child
Why is it so important for us to talk about the loss of a child?- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find country »
- A
- B
- B
- g
- D
- E
- ё
- F
- °
- and
- l
- H 9000
- R
- C
- T
- in
- x
- C 9000
- WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Spotlight/
- Why is it so important for us to talk about the loss of a child
Why is it important for us to talk about the loss of a child
WHO/M. Purdie
Purdie
© A photo
The loss of a child during pregnancy due to miscarriage or stillbirth is still a taboo subject around the world, with condemnation or shame associated with it. Many women who lose a child during pregnancy or childbirth continue to receive neither the proper care nor the respect they deserve. In this material we want to share stories told by women from different countries.
Miscarriage is the most common cause of pregnancy loss. Estimates of the prevalence of this phenomenon vary somewhat, although according to the March of Dimes Foundation, an organization dedicated to maternal and child health, the prevalence of miscarriage in women who knew they were pregnant is 10-15%. Different countries around the world use different definitions of pregnancy loss, but as a rule, the death of a child before 28 weeks of gestation is considered a miscarriage, and death at or after 28 completed gestational weeks is considered a stillbirth. There are 2.6 million stillborn babies born each year, and many of these deaths could have been prevented. However, even in developed countries, miscarriages and stillbirths are not systematically recorded, so the actual figures may be even higher.
There are 2.6 million stillborn babies born each year, and many of these deaths could have been prevented. However, even in developed countries, miscarriages and stillbirths are not systematically recorded, so the actual figures may be even higher.
Worldwide, women's access to health care varies by country of residence, with hospitals and outpatient facilities very often under-resourced and understaffed in many countries. As varied as the experience of bereaved women, stigma, guilt and shame are common themes around the world. Women who have lost their children have shared personal experiences that they felt they had to keep their grief quiet, either because miscarriages or stillbirths remain common or because people perceive them as inevitable.
Jessica Zucker, Clinical Psychologist and Writer, USA
“I am a clinical psychologist specializing in mental health issues related to reproduction and motherhood. I have been doing this for over ten years. But when I myself had a miscarriage at 16 weeks, only then could I truly feel that heartache, that re-experienced feeling of grief and loss that my patients have been telling me about for so many years.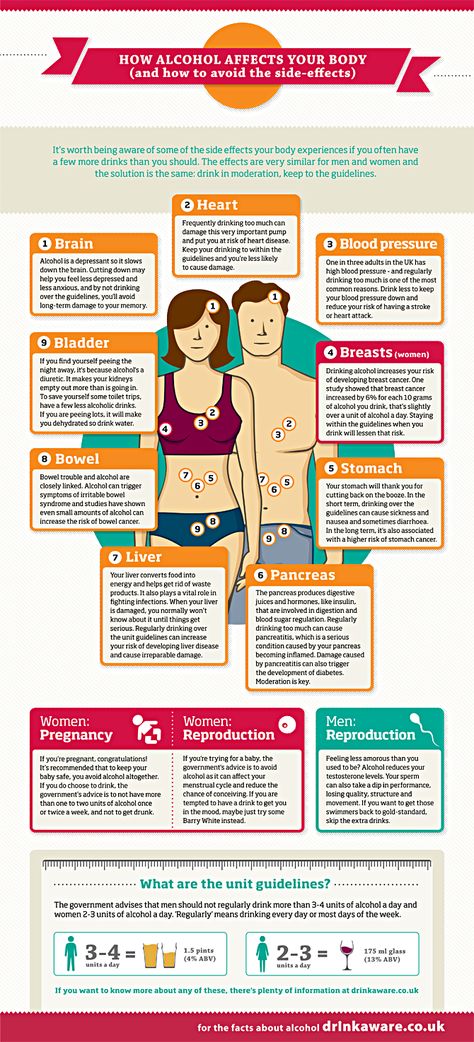
Jessica's story
All this has an extremely hard effect on women. Many women who lose a child during pregnancy may develop mental health problems that last for months or years, even if they later have healthy children.
Cultural and social views on the loss of a child in different parts of the world can be very different from each other. Thus, in sub-Saharan Africa, the prevailing opinion is that a baby can be born dead because of witchcraft or the machinations of evil spirits.
Larai, 44, pharmacist, Nigeria
“I took everything that happened after my miscarriage very hard. This was greatly facilitated by the medical workers themselves, despite the fact that I am also a doctor. Another issue is cultural representations. Here, the loss of a child brings shame to the woman, because there is a perception that if a woman has lost a child several times, something is wrong with her, and that she may have had extramarital affairs, and the loss of a child in that case, God's punishment.
Larai's story
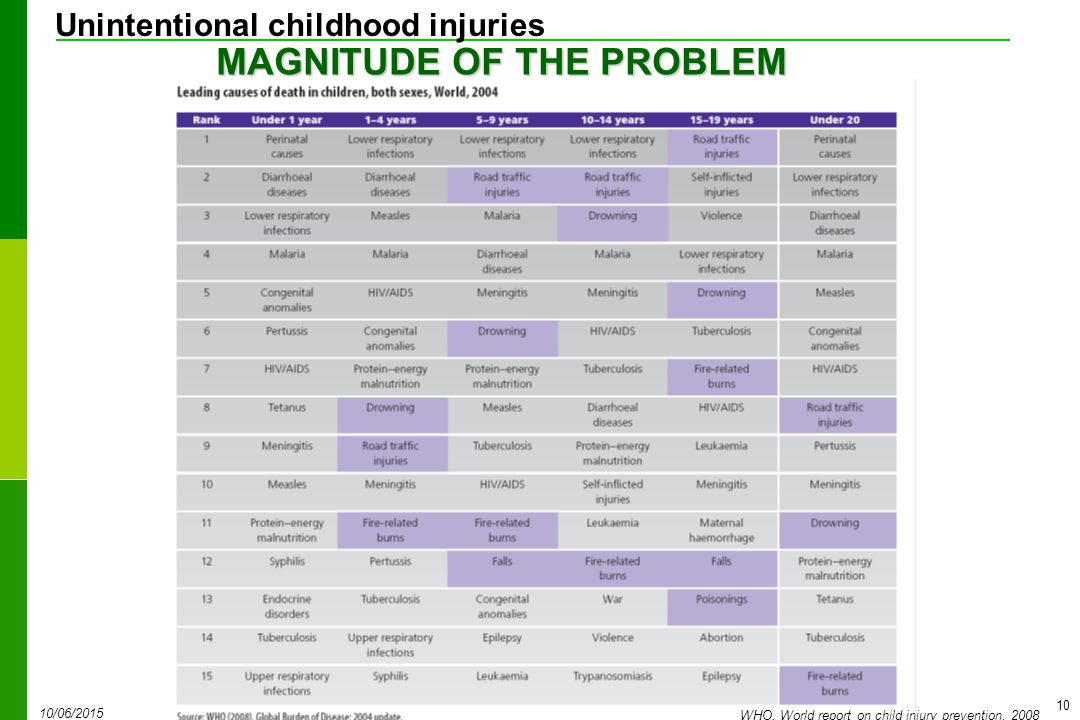
There are many possible causes for miscarriages or stillbirths, including fetal abnormalities, maternal age, and infections, many of which (such as malaria and syphilis) are preventable, although identifying the exact cause is often difficult.
General recommendations for preventing miscarriage include a healthy diet, physical activity, avoiding smoking, drug and alcohol use, limiting caffeine intake, managing stress, and maintaining a normal body weight. This approach focuses on lifestyle factors, and in the absence of specific explanations for what happened, this can lead to women feeling guilty that it was their behavior that caused the miscarriage.
Lisa, 40, Marketing Manager, UK
“I've had four miscarriages. Every time this happens, a part of you dies. The first time was the hardest. It was my very first pregnancy. We were so happy that we will soon have a baby. But when we went to our local hospital in the southeast of England at week 12 for a routine ultrasound, I was told that I had a miscarriage, or miscarriage, which meant that my baby had died long ago, although I did not feel no signs. "
"
Lisa's story
As with some other medical topics, such as mental health, which remain a huge taboo, many women report that, regardless of their cultural background, education and upbringing, their friends and families don't want to talk about their loss. Apparently, this is due to the general tradition to surround any grief with a veil of silence.
Susan, 34, writer, USA
“I've been dealing with infertility for almost five years now. After I decided to try IVF, I actually managed to get pregnant, but after a few weeks the baby stopped growing. It took doctors two and a half weeks to confirm this. It took another two weeks before I had a miscarriage that lasted 19days. I could not imagine that it could be so painful, for so long and with such heavy bleeding.
Susan's story
Stillbirths occur later in pregnancy, namely after 28 gestational weeks, as defined by WHO. About 98% of stillbirths occur in low- and middle-income countries. Lack of proper care and supervision during labor results in one in two stillbirths occurring during delivery, many of which could have been prevented with quality care and proper supervision of the woman in labour.
Lack of proper care and supervision during labor results in one in two stillbirths occurring during delivery, many of which could have been prevented with quality care and proper supervision of the woman in labour.
Better care during pregnancy and childbirth could prevent more than half a million stillbirths globally. Even in high-income countries, non-compliance with standards of care is an important cause of stillbirths.
There are clear ways to reduce the number of children who die during pregnancy, namely: improving access to antenatal care (in some parts of the world, women do not see a health worker until they are several months pregnant), introducing continuous care models, provided by midwives, as well as community care where possible. Integrating infection management during pregnancy, fetal heart rate monitoring and birth monitoring into a comprehensive care package could save 1.3 million lives of otherwise stillborn babies.
Emilia, 36, shopkeeper, Colombia
“When my baby was stillborn at 32 weeks, we already gave him a name. The doctor referred me for an ultrasound examination, during which he told me that the child was not showing signs of life. I knew right away that my baby was dead. I know this could have been avoided. If from the very beginning I had been told everything about my condition in more detail, if the doctors had treated me more attentively during the critical periods of my pregnancy, my child could have been saved.
The doctor referred me for an ultrasound examination, during which he told me that the child was not showing signs of life. I knew right away that my baby was dead. I know this could have been avoided. If from the very beginning I had been told everything about my condition in more detail, if the doctors had treated me more attentively during the critical periods of my pregnancy, my child could have been saved.
Emilia's story
Attitude towards women during pregnancy is related to the extent to which their sexual and reproductive rights are generally realized; many women around the world do not have the ability to make autonomous decisions in this area.
In many parts of the world, the pressure of public opinion is forcing women to become pregnant when they are not yet physically or psychologically ready for it. Even in 2019, 200 million women who want to avoid pregnancy do not have access to modern methods of contraception. And when pregnancy does occur, 30 million women are forced to give birth outside of health facilities, and 45 million women do not receive adequate antenatal care or no antenatal care at all, greatly increasing the risk of complications and death for both the mother and the mother. child.
child.
Cultural practices, such as ritual female genital mutilation and child marriage, cause great harm to girls' sexual and reproductive health and the health of their children. Having children at a young age can be dangerous for both mother and child. Adolescent girls (aged 10–19 years) are significantly more likely to have eclampsia or intrauterine infections than women aged 20–24 years, increasing the risk of stillbirth in this age group. In addition, babies born to women younger than 20 are more likely to have low birth weight, prematurity, or severe health problems in the first month of life, which also increases the risk of stillbirth.
Female genital mutilation increases a woman's risk of protracted or difficult labour, bleeding, severe tears and increases the frequency of instrumental use in childbirth. At the same time, children of such mothers are much more likely to need resuscitation during childbirth and increase the risk of death during childbirth or after birth.
Putting women at the center of care is critical to creating a positive pregnancy experience—the biomedical and physiological aspects of health services need to be complemented by social, cultural, emotional and psychological support.
However, many women, even in developed countries with access to the best health care systems, do not receive adequate care after the loss of a child. Even the language used by medical professionals in relation to miscarriage and stillbirth can be traumatic in itself: the use of terms such as "cervical failure" or "dead gestational sac" can be painful.
Andrea, 28, stylist and singer, Colombia
“When I was 12 weeks pregnant, I had a scheduled appointment with the doctor, where I had an ultrasound. The doctor told me that I was not doing well, but did not specify what exactly was wrong. The next day, when I woke up, I noticed blood stains on the sheets. I didn't get any information about why I had a miscarriage. My doctor was very kind to me, but he didn't explain anything to me. But the nurses were completely indifferent and unfriendly and behaved as if I had undergone an ordinary medical procedure, and nothing more. No one gave me any support."
My doctor was very kind to me, but he didn't explain anything to me. But the nurses were completely indifferent and unfriendly and behaved as if I had undergone an ordinary medical procedure, and nothing more. No one gave me any support."
Depending on the rules of the particular medical facility, stillborn bodies may be treated as clinical waste and may be incinerated. It happens that when a woman learns that her child has died, she is forced to continue to carry the dead baby for several weeks before she can give birth. Even if this delay may be clinically justified, this situation is excruciating for both the woman and her partner. Even in developed countries, women may be forced to give birth to their dead babies in maternity wards, surrounded by women who have healthy children, which is very difficult from a psychological point of view and reminds the woman of her loss.
Not all inpatient or outpatient facilities can adopt a new care strategy or provide more services. This is the reality that reflects the overload of health systems. And yet, there is no extra cost to be more sensitive in dealing with bereaved couples and to remove the taboo and stigma around talking about the loss of a child. This is evidenced by some of the stories told here.
This is the reality that reflects the overload of health systems. And yet, there is no extra cost to be more sensitive in dealing with bereaved couples and to remove the taboo and stigma around talking about the loss of a child. This is evidenced by some of the stories told here.
Medical staff are fully capable of being sensitive and compassionate, acknowledging the depth of the parents' feelings, providing clear information about the situation, and understanding that parents may need special support, both in relation to the loss of a child and in relation to the possible desire for more children. . To provide competent maternal and newborn health care and to meet the requirements for clinical competence in general, it is necessary that this care be provided from a human rights perspective, on the basis of respect, protecting the dignity of patients and taking into account their socio-cultural characteristics.
Learn more about the work of WHO
Learn more about the work of WHO in collaboration with partner organizations
Miscarriage, how to avoid - Planning and management of pregnancy in the gynecology of the Literary Fund polyclinic after a miscarriage
- Gallery
- News
- Blog
- Reviews
- Jobs
- Licenses
- Insurance partners
- Controlling organizations
- Schedule of reception of citizens on personal appeals
- What you need to know about coronavirus infection?
- Rules for patients
- Online doctor's consultation
- to corporative clients
- The documents
A miscarriage is always associated with serious consequences for the whole body of a woman and for her reproductive organs in particular, it also affects the family situation, disrupts the woman's work schedule. An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
An unfavorable outcome of pregnancy requires great mental and physical costs on the part of parents. Therefore, contacting doctors to find out the causes of the problem is the very first and correct step towards the birth of a child.
Any competent gynecologist will tell you that the problem of miscarriage can be solved. With proper preparation for pregnancy and its management, the next time you will have a successful pregnancy. Most girls after a miscarriage go to extremes: they try to get pregnant again as soon as possible. And if this succeeds, then the miscarriage is very often repeated. And you need to give the body a rest for 2-3 months, then identify and eliminate the cause. And only then try.
Causes of miscarriage
Many are convinced that miscarriages are due to a fall, bruise, or some other physical shock. Any woman who has had a miscarriage can remember that not long before she either fell or lifted something heavy. And I am sure that she lost her unborn child precisely because of this. However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
However, those women whose pregnancy was normal also fall and lift heavy things. Most sudden miscarriages do not occur for this reason. The reason is in violations of the pregnancy itself. Approximately half of miscarriages are due to abnormal genetic development of the fetus, which can be hereditary or accidental. Merciful nature, following the principles of natural selection in everything, destroys the defective and unviable fetus. But you should not be afraid of this. The fact that there is a defect in one embryo does not mean at all that all the others will be the same.
The woman's body is almost always to blame for the other half of miscarriages. They are caused by various known and unknown factors, such as: acute infectious diseases suffered in the first trimester of pregnancy, poor environment or difficult working conditions, excessive psychological or physical stress, abnormal development of the uterus, radiation, alcohol, smoking and certain types of drugs.
The causes of early and late miscarriage may differ, although they may overlap. The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
The most important thing is to find out and eliminate or compensate for your own cause of miscarriage. Having discovered the cause, the gynecologist will tell you how to avoid another loss.
Miscarriage
Miscarriage statistics also include “missed pregnancy”. Sometimes it happens that the embryo dies and lingers in the uterine cavity. Most often, this fact is detected by ultrasound. The dead fetus may begin to decompose, and this, thereby, will lead to poisoning of the mother's body.
Doctors resort to surgical curettage, which is associated with a risk of inflammation and complications. With such a miscarriage, the next pregnancy is planned after the body is fully restored - not earlier than a year. During this year, you will have to find out the cause of the missed pregnancy and treat it.
Miscarriage up to 6 weeks
The main causes of miscarriage on this line are malformations of the embryo itself. Statistics say that from 70-90% of embryos had chromosomal abnormalities: they are random and will not occur in other pregnancies. You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
You may have been ill, taken medication, or were under the influence of other harmful factors. Fate saved you from a child with malformations.
The human body is perfect and finds a way to correct the situation by miscarriage. Today is a tragedy for you. The real tragedy would be the preservation and birth of a sick, non-viable child. So don’t cry and understand: everything is for the best, you won’t help grief with tears ... And after three months, try again - it will almost certainly turn out to be successful.
It should also be noted that the fact of a miscarriage does not mean that you have lost something. So for a period of 7-8 weeks, the absence of an embryo in the fetal egg is found - "anembryony". It is believed that in 80-90% of cases, miscarriages are undiagnosed non-developing pregnancies.
Miscarriage between 6 and 12 weeks
Miscarriage during this period is also considered early. Its most common causes are:
Endocrine disorders
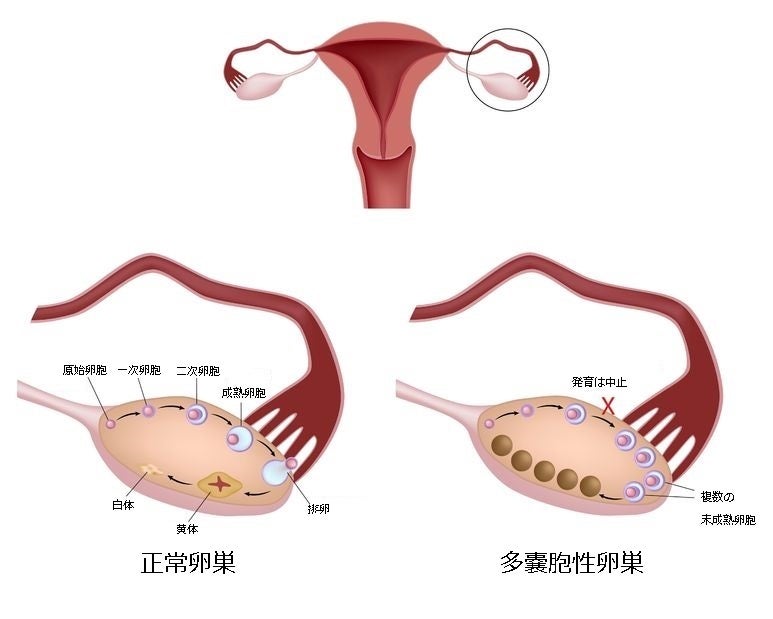
Endocrine disorders, when the ovaries do not synthesize enough hormones to keep the fetus in the womb, or the amount of male sex hormones is increased, is one of the most common causes of miscarriage and miscarriage.
Imbalance of hormones in a woman's body is highly likely to lead to an early termination of pregnancy. With a lack of the main hormone progesterone produced by the ovaries, this happens most often. Another hormonal problem is an increase in the tone of the uterus, which provokes the expulsion of the fetus.
Progesterone prepares the uterine mucosa for implantation and is the hormone for maintaining pregnancy in the first months. If conception occurs, the fetus cannot properly establish itself in the uterus. As a result, the fertilized egg is rejected. But pregnancy can be saved with the help of progesterone preparations if this problem is detected in time.
An excess of male sex hormones that suppress the production of estrogen and progesterone can also be the cause of an early miscarriage. Often, the cause of recurrent miscarriages are androgens that affect the formation and development of pregnancy; as well as thyroid and adrenal hormones. Therefore, a change in the function of these glands can lead to miscarriage.
Undertreated sexual infections
This problem must be solved before conception. Often the cause of miscarriage is sexually transmitted infections: syphilis, trichomoniasis, toxoplasmosis, chlamydia, cytomegalovirus and herpetic infections. Their effect on the fetus and the course of pregnancy is different for each woman and depends on the timing of infection, the activity of the microorganism, the degree of immune protection and the presence of other adverse factors. Depending on the situation, they can lead to the formation of fetal malformations, intrauterine infection, feto-placental insufficiency, early miscarriage or premature birth. Infection of the fetus and damage to the membrane of the fetus leads to miscarriage. To avoid this, infections should be treated before pregnancy. The use of therapy is possible during pregnancy as prescribed by a doctor.
Viral infections and other diseases
Any disease accompanied by intoxication and fever above 38 o C can lead to a miscarriage. Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Rubella, influenza and viral hepatitis occupy a leading position in this list. At a period of 4-10 weeks for pregnancy, ordinary tonsillitis can also become tragic, pneumonia carries a more serious risk. Pyelonephritis and appendicitis can cause early labor. When planning a pregnancy, it is imperative to undergo a medical examination in order to identify and treat foci of infections.
Extremely dangerous during pregnancy rubella - it leads to severe fetal malformations, so infection during pregnancy is an indication for medical abortion.
Any disease during pregnancy can lead to non-viability of the fetus. And the body, through a miscarriage, insures you against unwanted offspring. With such a miscarriage, the next pregnancy has every chance of going well.
Immune causes of miscarriage
Sometimes antibodies that are hostile to the fetus are formed in the blood of a pregnant woman. This cause can be predicted and eliminated in advance. Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Most often, the conflict occurs when the embryo inherits the positive Rh factor of the father, and the negative Rh factor, the mother's body rejects the embryonic tissues that are alien to it. Constant monitoring of antibody titer and the introduction of anti-Rhesus immunoglobulins allows you to maintain and maintain pregnancy. In case of an immune conflict, progesterone preparations are also used to prevent miscarriage, which in this case has an immunomodulatory effect.
Reduced immunity
Reduced immunity during pregnancy is also an immune cause. The body is simply not able to grow a new life in itself. You need to take care of yourself and recover before the next conception.
Anatomical causes of miscarriage
Anatomical causes of miscarriage are the most intractable. Malformations of the uterus are a serious reason for miscarriage. Sometimes you just have to deal with it.
Miscarriage at 12 to 22 weeks
Such a miscarriage is considered late. Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
Its causes coincide with the causes of miscarriages in the early stages (anatomical, immune, infectious, endocrine).
At this time, miscarriage also occurs due to isthmic-cervical insufficiency - a weak cervix cannot hold the fetus and opens. For this reason, a miscarriage can occur in the 2nd or 3rd trimester. Isthmic-cervical insufficiency is observed in 15.0-42.7% of women suffering from miscarriage. Careful monitoring of the pregnant woman allows you to identify the problem in time and make surgical correction of the cervix before the onset of childbirth.
There is only one method of treatment for isthmic-cervical insufficiency - mechanical narrowing of the cervical canal. To do this, the neck is either sewn up or a special ring is put on it. However, the latter method is less efficient, because the ring can easily slide off the neck, then it will no longer hold back the process of opening it.
After suturing, if necessary, it is possible to use antibiotics and drugs that normalize the microflora of the vagina. The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
The treatment of the vagina and the control of the state of the seams are carried out daily for 5 days. Stitches are removed at 37-38 weeks and with premature onset of labor.
Isthmic-cervical insufficiency may be primary (for no apparent reason), may be the result of abortion or hormonal disorders (increased levels of androgens - male sex hormones or their precursors).
Miscarriage after 22 weeks
Such a loss is hard to forget. Obstetricians talk about premature birth after the 28th week of pregnancy. Traditionally, a child born after this period is considered viable. But medicine knows many cases when it was possible to save the life of earlier children.
We recommend that you be carefully examined for miscarriage, check the above factors. In addition to them, the cause of a miscarriage can be antiphospholipid syndrome, while the woman's body perceives the child as something alien and rejects it. This disease, like the others listed, can be corrected; you have a very real chance of bearing a child.
Miscarriage due to impaired hemostasis
All of the above causes account for only 30-40%. Up to 70% of miscarriages are caused by disorders in the blood coagulation system (hemostasis).
Disorders of the blood coagulation system leading to pregnancy loss can be divided into thrombophilic (increased clotting) and hemorrhagic (a tendency to bleed). Both of these extremes are dangerous to the fetus. Various disorders leading to the formation of small blood clots lead to the fact that the fetus loses sufficient blood supply, development is disturbed and the fetus is rejected.
The main hemorrhagic changes can appear even in childhood in the form of increased bleeding during cuts, tooth extractions, the onset of menstruation. But sometimes they declare themselves only during pregnancy and are the cause of a miscarriage. Bleeding in the early stages and detachment of the chorion is difficult to stop.
You may not guess, but incomprehensible headaches, weakness, fatigue, temporary loss of smell or hearing may be symptoms of disorders in the blood coagulation system.