How long to get pregnant with pcos
I have PCOS and I want to have a baby, what do I need to know?
This article is republished from The Conversation under a Creative Commons license.
Sara Holton, Deakin University and Karin Hammarberg, Monash University
Most women want and expect to have children. But women who have a chronic health condition such as polycystic ovary syndrome (PCOS) often have concerns about childbearing, including whether they can become pregnant.
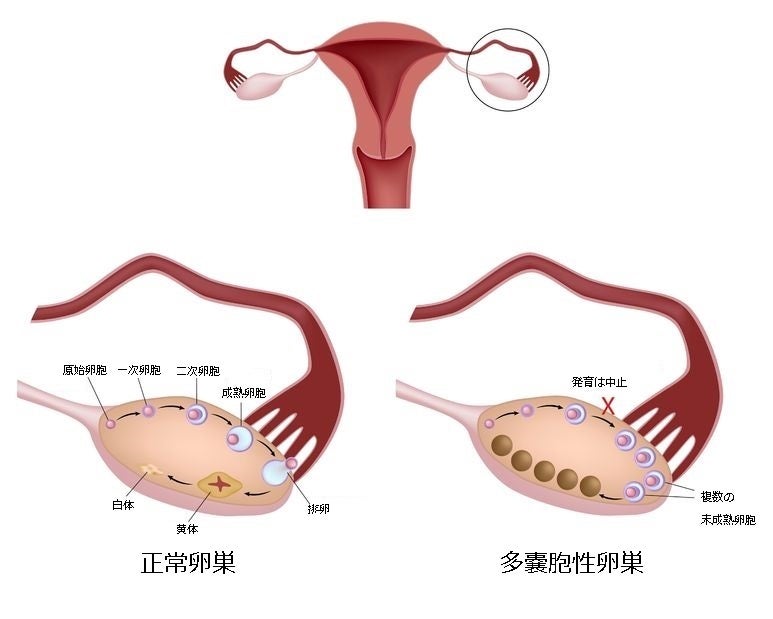
PCOS is a complex hormonal condition which affects up to one in five women of reproductive age. Most women with PCOS have elevated levels of a type of hormone called luteinising hormone, which brings about ovulation, and reduced levels of a hormone called “follicle stimulating hormone”, which is essential for pubertal development and the function of women’s ovaries and men’s testes.
Women with PCOS also have an underproduction of oestrogen (“female” hormones) and an overproduction of androgens (“male” hormones). This causes tiny cysts on the surface of the ovaries.
Due to these hormonal imbalances, women with PCOS often have irregular menstrual cycles because they don’t ovulate or ovulate only occasionally. So women with PCOS are more likely to have trouble conceiving than other women.
While most women who have PCOS become pregnant, they often take longer to fall pregnant and are more likely to need fertility treatment than women without PCOS.
In a recent study by Monash University, women with PCOS took part in an online discussion group. They talked about their concerns about pregnancy and what they could do to improve their chances of falling pregnant, the sort of information they would like about fertility and PCOS, and when they would like to receive this information.
Their greatest worry was about whether they would be able to get pregnant. They also wanted to know how best to prepare for pregnancy and what they should do before trying to conceive. They had trouble finding up-to-date, relevant and reliable information.
Read more: Explainer: what is polycystic ovary syndrome?
How to increase chance of pregnancy
As for all women, being in the best possible health before trying for a baby increases the chance of pregnancy and gives the baby the best start in life.
According to the international evidence-based guideline for the assessment and management of PCOS, adopting a healthy lifestyle – including being in the healthy weight range, not smoking, cutting back on alcohol, eating a healthy diet, getting plenty of regular exercise and enough sleep – is the first thing to do to improve a woman’s chances of becoming pregnant and having a healthy baby.
To get the right kind of advice and support, women planning to get pregnant should have a preconception health check with their GP. This is also an opportunity to discuss a plan of action in case the PCOS causes fertility difficulties.
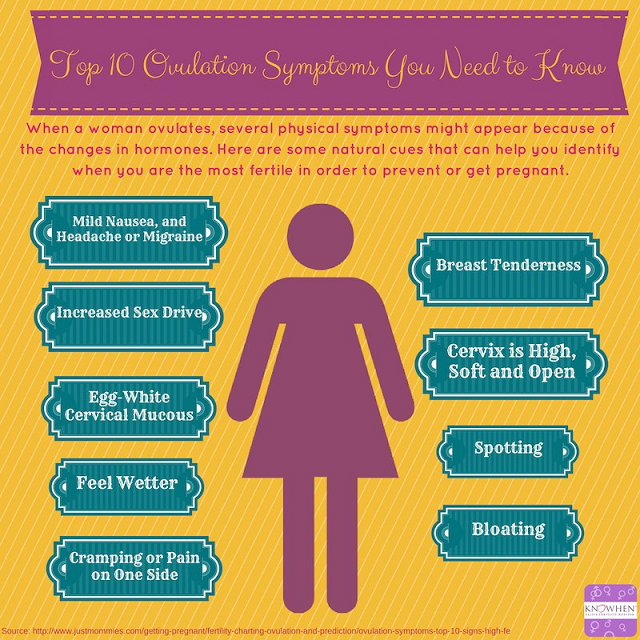
For women with PCOS who are overweight or obese, a modest weight loss sometimes results in more regular ovulation, which increases the chance of pregnancy.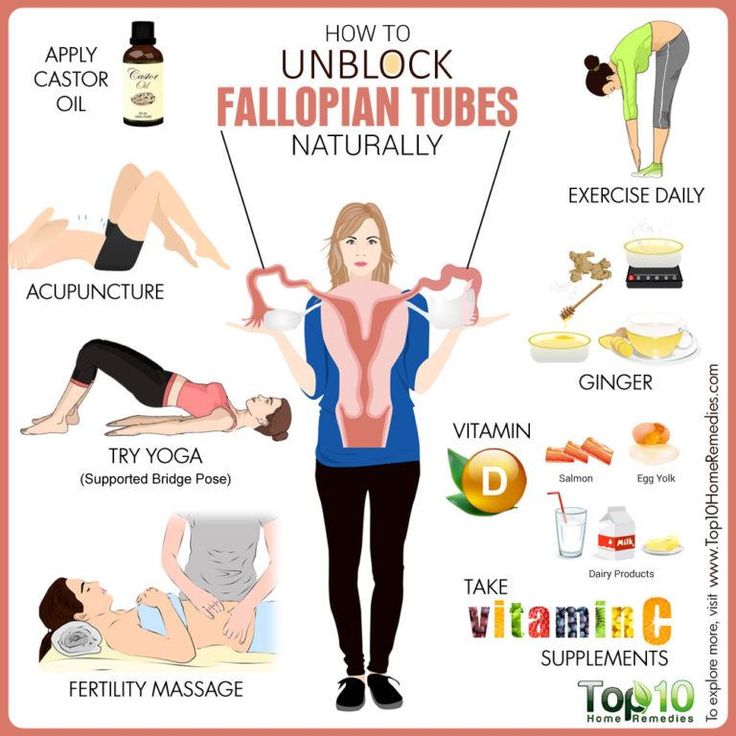 For those who know they ovulate, having sex during the “fertile window” (the five days leading up to and including ovulation) boosts the chance of conception.
For those who know they ovulate, having sex during the “fertile window” (the five days leading up to and including ovulation) boosts the chance of conception.
Overall, women with and without PCOS have a similar number of children. john looy unsplash
Read more: Women's fertility: does 'egg timer' testing work, and what are the other options?
What are my options?
If you have tried for a baby for 12 months without success (or six months if you are aged 35 or over) it’s time to seek medical advice. Your GP is your first port of call, but she might refer you to a fertility specialist.
If you have very irregular or only sporadic periods, this is an indication you are not ovulating and need medical help to have a baby. The first line of medical treatment is ovulation induction. This involves a course of tablets or injections to stimulate the ovaries to release an egg that can be fertilised, either during intercourse or through intra-uterine insemination (IUI).
If this doesn’t work, there may be other reasons why pregnancy can’t be achieved and more invasive treatments such as IVF may be needed.
IVF involves a course of injections to stimulate the ovaries to produce multiple eggs. When they’re mature the eggs are retrieved in an ultrasound-guided procedure under light anaesthetic. Sperm are added to the eggs in the laboratory for embryos to form.
A few days later, an embryo is placed in the uterus where it may implant and grow into a baby. If there is more than one embryo, these can be frozen for later use if there is no pregnancy.
While IVF is safe in the hands of specialists, there are some possible health effects to be aware of, including ovarian hyperstimulation syndrome. This is an over-response to the fertility drugs that are used to stimulate the ovaries to produce multiple eggs. This can lead to abdominal pain, nausea and vomiting, rapid weight gain and blood clots.
Read more: Better health and diet well before conception results in healthier pregnancies
For more information
The Your Fertility website has more information on PCOS and fertility.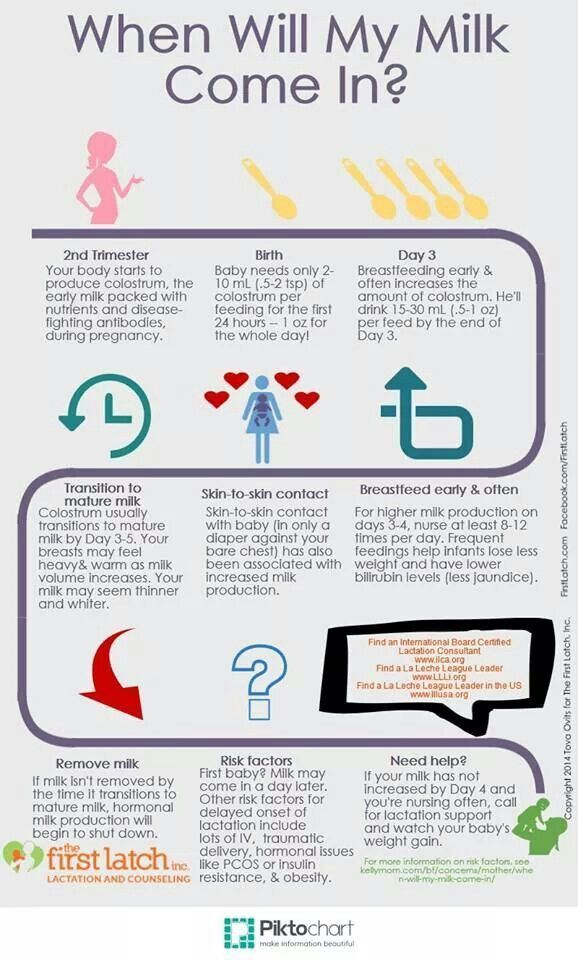 The Centre for Research Excellence in Polycystic Ovary Syndrome has also produced a list of questions for women with PCOS to use in conversations with their healthcare provider and a fact sheet about PCOS, fertility and pregnancy.
The Centre for Research Excellence in Polycystic Ovary Syndrome has also produced a list of questions for women with PCOS to use in conversations with their healthcare provider and a fact sheet about PCOS, fertility and pregnancy.
While fertility problems are common among women with PCOS, it’s reassuring that, overall, women with PCOS and women without PCOS have similar numbers of children. And, although PCOS is associated with fertility difficulties, women with PCOS should also be aware conception is possible and effective contraception is needed to avoid pregnancy when it’s not wanted.
This article was co-authored by Louise Johnson, CEO of the Victorian Assisted Reproductive Treatment Authority (VARTA). Louise has no conflicts of interest to note.
Sara Holton, Research Fellow, Deakin University and Karin Hammarberg, Senior Research Fellow, Jean Hailes Research Unit, School of Public Health & Preventive Medicine, Monash University
This article is republished from The Conversation under a Creative Commons license.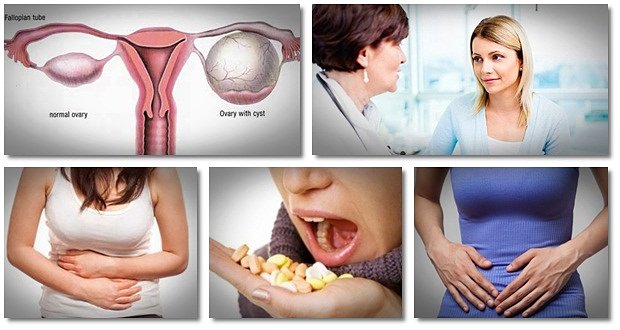 Read the original article.
Read the original article.
PCOS Fertility Pregnancy
How to Get Pregnant with PCOS
Polycystic ovary syndrome, or PCOS, is a hormonal condition that tampers with more than just your fertility, but you might first receive a diagnosis when you’re trying to get pregnant. This is because it’s a common — and treatable — cause of infertility in women.
According to the Centers for Disease Control (CDC), up to 12 percent of women in the United States have difficulty getting pregnant because of untreated PCOS. In reality, this number might be bigger because almost 50 percent of women with this syndrome don’t know they have it or are not diagnosed correctly.
Having PCOS doesn’t mean you can’t get pregnant. It just might be a bit trickier and you may need extra help. There is plenty that you can do at home and with medical treatment to keep PCOS symptoms at bay and raise your chances for a healthy pregnancy.
Getting pregnant with PCOS involves some of the same steps that women without PCOS should take for a healthy pregnancy.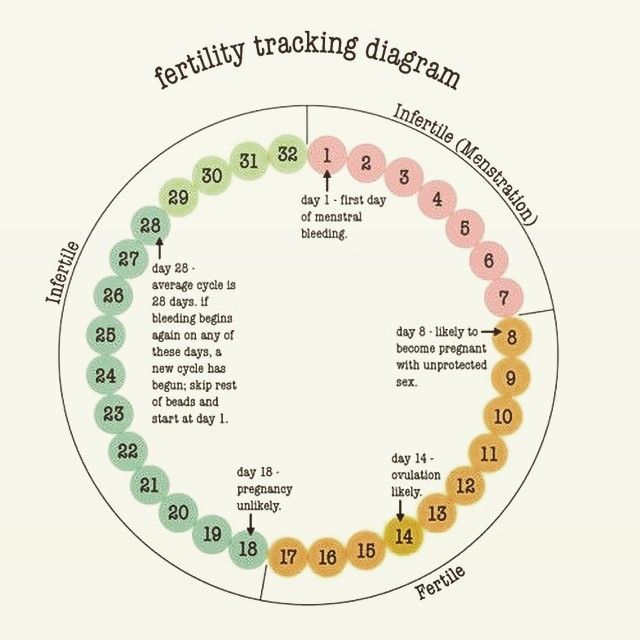
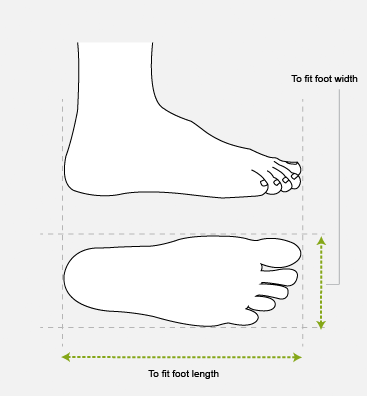
- Have your weight and body mass index (BMI) measured by your doctor. Your BMI shows whether you have a healthy body weight and how much of your body composition is fat. If you are carrying extra weight, talk to your doctor about how much weight you need to lose before you get pregnant.
- Start a healthy diet and exercise plan. Get into the habit of choosing healthier food choices and being more active.
- Use an ovulation calendar or app to track when you have your period. This helps you make a better guess about which days of the month you are more likely to get pregnant.
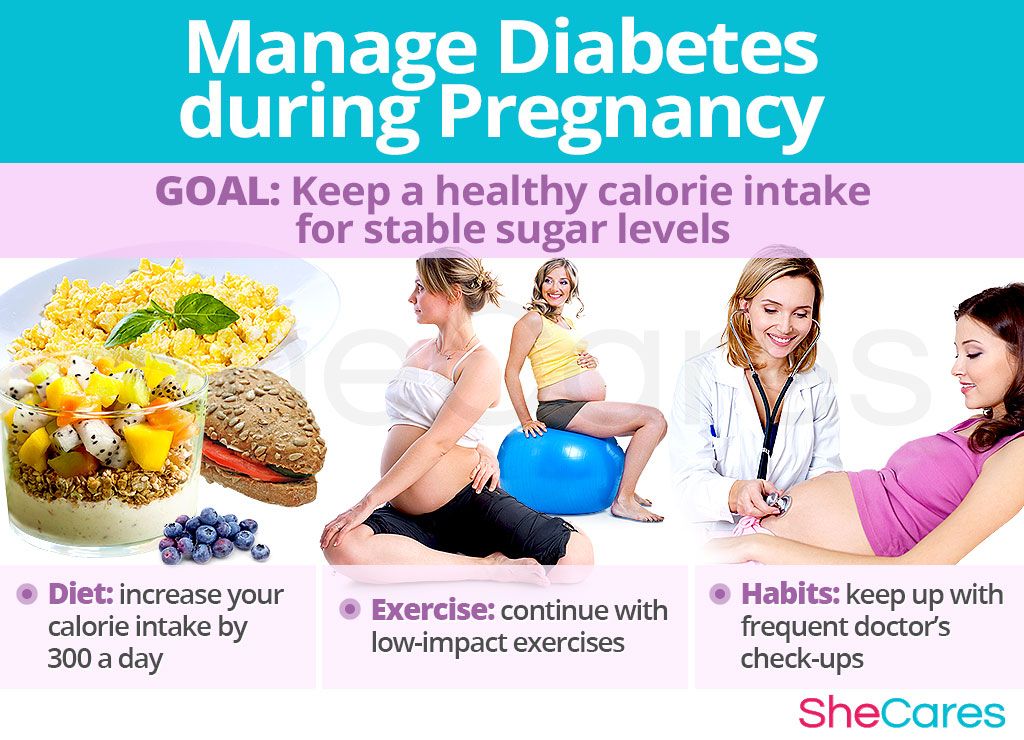
- Check your blood sugar levels. See your doctor to make sure your blood sugar levels are balanced. Your blood sugar levels are important in getting pregnant, having a healthy pregnancy, and even in your baby’s future health.
Being overweight has been linked to PCOS, but many women who have this condition are not overweight at all. Still, if you are carrying extra weight, you may improve your fertility and reduce other PCOS symptoms by losing just 5 percent of your weight.
Still, if you are carrying extra weight, you may improve your fertility and reduce other PCOS symptoms by losing just 5 percent of your weight.
Exercise daily by going for a walk and getting in your steps. Use a standing desk rather than sitting down while you’re working. Lift light weights while watching TV as building more muscle helps bring down PCOS symptoms and improves your health.
Any woman who is trying to get pregnant needs to have the right levels of nutrients. Switch out sugary foods, simple carbs, and unhealthy fats for healthier choices, including:
- fresh and cooked fruit and vegetables
- whole grains like brown rice, oats, and barley
- beans and lentils
- chicken
- fish
Certain vitamins and minerals are important for a healthy pregnancy and a growing baby. Ask your doctor about the best supplements for you. Supplements that may help fertility include:
- folic acid (vitamin B9)
- vitamin B6
- vitamin B12
- vitamin C
- vitamin D
- vitamin E
- coenzyme Q10
Your doctor will test your blood sugar levels if you’re having trouble getting pregnant.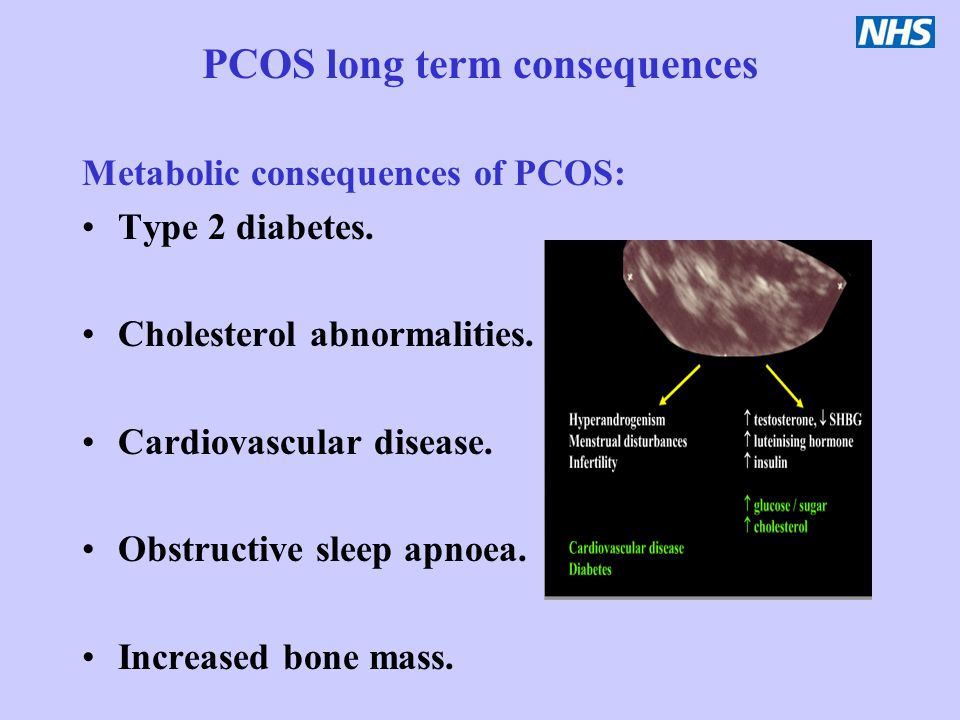 PCOS sometimes leads to high blood sugar levels or type 2 diabetes. This may cause fertility problems.
PCOS sometimes leads to high blood sugar levels or type 2 diabetes. This may cause fertility problems.
This happens because PCOS may change how your body uses insulin. This important hormone moves sugar (glucose) out of the blood and into the muscles and cells where it is burned for energy. PCOS makes your body less sensitive to insulin — making it harder for it to do its job.
Balancing your blood sugar levels may help you get pregnant. Eat a healthy diet with more fiber, protein, and healthy fats. Getting plenty of daily exercise and strength training can also help your body use insulin better.
In some cases, your doctor might recommend medications to help balance your blood sugar levels. A common type 2 diabetes drug called metformin (or Glucophage) makes your body use insulin better to help lower high blood sugar. This can also help you get pregnant with PCOS.
You might need to take metformin in low doses and only temporarily, depending on your blood sugar levels. For best results, eat a healthy diet and exercise regularly along with taking any prescribed medications to help you get pregnant.
For best results, eat a healthy diet and exercise regularly along with taking any prescribed medications to help you get pregnant.
If you have high blood sugar levels or type 2 diabetes, it’s important to check your blood sugar levels with a home monitor every day.
Your doctor will check your blood sugar levels with tests, including:
- random blood sugar test
- overnight fasting blood sugar test
- oral glucose tolerance tests (after fasting and drinking a sugary drink)
- hemoglobin A1C test (checks your blood sugar levels for the last two to three months)
If you have PCOS your body might make more of both the male hormone testosterone and the female hormone estrogen. Too much (or too little) of these hormones can make it tricky to get pregnant. Your doctor might recommend prescription medications to help balance your hormones.
Medications to help you get pregnant with PCOS include:
- metformin to balance insulin levels
- clomiphene citrate (or Clomid) to help balance estrogen levels
- birth control pills to balance estrogen and testosterone levels (before beginning fertility treatment)
- fertility medications to jump-start the ovaries to send out more eggs
You may need in vitro fertilization (IVF) treatment to help you get pregnant with PCOS. Your fertility doctor will give you a checkup that may include more blood tests, ultrasounds scans, and a physical exam.
Your fertility doctor will give you a checkup that may include more blood tests, ultrasounds scans, and a physical exam.
IVF is a process that can take months or even years whether you have PCOS or not. However, medical research shows that women with PCOS have a high success rate of getting pregnant with IVF treatment.
Some clinical studies found that women with PCOS who took birth control pills before the IVF treatment had better results. You may also need other mediations to help balance hormones and get your body ready for the IVF treatment.
For all women, the first step in IVF treatment is to eat a balanced diet and get plenty of exercise to reach a healthy weight. Women with PCOS who are a healthy weight are twice as likely to get pregnant with IVF than women with PCOS who are obese.
Before exploring IVF, your doctor might suggest a less-costly alternative called intrauterine insemination (IUI). This process increases the chance of pregnancy because it directly injects a high concentration of sperm closer to the egg.
PCOS may make it harder to get pregnant because it can impact your menstruation cycle (your monthly period). Symptoms include:
- too few menstrual periods
- having your period for longer than usual
- not getting your period
- very heavy periods
- higher levels of male hormones like testosterone
- acne breakouts
- getting facial hair and extra hair in other places
- small cysts or bundles of fluid in the ovaries
- fewer eggs released from the ovaries
If you don’t get treated for PCOS, it also raises your risk for other health conditions, like:
- type 2 diabetes
- sleep apnea (snoring)
- heart disease
- high blood pressure
- high cholesterol
- stroke
No one knows why some women get PCOS. Nothing you did — or didn’t do— caused you to have this condition. But getting an early diagnosis and treatment along with making other lifestyle changes may help you get pregnant and prevent health complications from PCOS.
If you are trying to get pregnant with PCOS, you may only need treatment with medications. A medical study found that almost 80 percent of women with PCOS treated with the drug clomiphene citrate successfully ovulated. Out of these, half of the women got pregnant naturally within six period cycles.
If medications don’t help you get pregnant, your doctor may recommend IVF treatments. Most women with PCOS have a 20 to 40 percent chance of getting pregnant with IVF treatment. Women who are 35 years old and older or who are overweight have a lower chance of getting pregnant.
You can get pregnant with PCOS. You will likely need to have moderate weight, balance your blood sugar levels, and treat other PCOS symptoms with healthy lifestyle changes and medications.
In some cases, fertility medications alone will help you get pregnant. If that doesn’t work, you may need IVF treatment.
But regardless of what treatment you explore, don’t lose hope. Success rates are optimistic. In time you may be smiling, positive pregnancy test in hand.
In time you may be smiling, positive pregnancy test in hand.
How to get pregnant with polycystic ovaries?
Polycystic disease is a common hormonal disease that affects the functioning of a woman's ovaries. The dangers of PCOS include irregular menstrual periods, excessive hair growth, acne, weight gain, and other problems. Left untreated, PCOS can even lead to infertility. In this article, we will tell you more about causes of polycystic , polycystic ovaries and pregnancy , and also give an answer to the question: “ Is it possible to give birth with polycystic ovaries? ".
What is polycystic ovary syndrome?
Polycystic ovary syndrome (PCOS) is a hormonal disorder common among women of reproductive age. Women with PCOS may have menstrual irregularities and elevated levels of male hormones (androgens). Numerous small collections of fluid (follicles) may form in the ovaries, and an egg may not be released regularly. This condition should not be confused with multifollicular ovaries, because with multifollicular ovaries, ovulation and a normal menstrual cycle can persist, unlike polycystic disease.
This condition should not be confused with multifollicular ovaries, because with multifollicular ovaries, ovulation and a normal menstrual cycle can persist, unlike polycystic disease.
50-75% of cases of endocrine infertility. 20-22% of marital infertility. It is detected in 5-16% of women of reproductive age. These are the figures for the diagnosis of "Polycystic Ovary".
Symptoms of polycystic ovary syndrome
Polycystic ovary syndrome is accompanied by characteristic symptoms, upon noticing which it is necessary to seek advice from an endocrinologist or gynecologist. For some women, symptoms begin around the time of their first menstrual period. Others discover symptoms of PCOS only after they have gained a lot of weight or have problems getting pregnant. In some cases, PCOS may be asymptomatic.
The most common symptoms of PCOS:
- Irregular periods. Lack of ovulation prevents the lining of the uterus from falling off every month.
 Some women with PCOS have fewer than eight periods a year, or none at all.
Some women with PCOS have fewer than eight periods a year, or none at all. - Severe bleeding. The lining of the uterus builds up over a longer period of time, so menstruation may be heavier than usual.
- Hair growth . More than 70 percent of women with this condition grow hair on their face and body, including on their back, abdomen, and chest. Excess hair growth is called hirsutism.
- Acne . Male hormones can make the skin more oily than normal and cause breakouts on areas such as the face, chest, and upper back.
- Weight gain. Up to 80 percent of women with PCOS are overweight or obese.
- Male pattern baldness. The hair on the scalp becomes thinner and may fall out.
- Darkening of the skin. Dark patches of skin may develop in body folds, such as the neck, groin area, and under the breasts.
- Headaches.
 Hormonal changes may cause headaches in some women.
Hormonal changes may cause headaches in some women.
Irregular periods
Infrequent, irregular periods, long or no periods are the most common symptom of PCOS. For example, with PCOS, you may have fewer than nine periods a year, more than 35 days between periods, and abnormally heavy periods.
Hyperandrogenism
Hyperandrogenism is a disease characterized by high levels of androgens. It is more common in women than in men. Symptoms of hyperandrogenism may include acne, seborrhea (inflammation of the skin), hair loss on the scalp, increased body or facial hair, and infrequent or absent periods.
Hyperandrogenism is a defining feature of women and young girls with PCOS. Polycystic disease causes a malfunction of the ovaries or adrenal glands, which leads to the production of excess androgens (male sex hormones).
Anovulation
Anovulation occurs when an egg is not released from the ovary during the menstrual cycle. The egg is essential for pregnancy. Since several hormones are involved in ovulation, there are many causes of anovulation, one of which is PCOS. Chronic anovulation is a common cause of infertility.
The egg is essential for pregnancy. Since several hormones are involved in ovulation, there are many causes of anovulation, one of which is PCOS. Chronic anovulation is a common cause of infertility.
Diagnosis
There is no test to definitively diagnose polycystic ovary syndrome (PCOS). The doctor will likely begin by discussing your medical history, including menstrual periods and weight changes. A physical exam will include checking for signs of excessive hair growth, acne, and weight gain.
Your doctor may recommend:
- Gynecological examination. A physician visually and manually examines the reproductive organs for growths or other abnormalities.
- Blood tests. A blood test is given to determine the level of hormones. This will help rule out possible causes of menstrual irregularities or excess androgens that mimic PCOS. An additional blood test may also be needed to measure insulin resistance as well as fasting cholesterol and triglyceride levels.
- Ultrasound examination (ultrasound). The doctor will check the appearance of the ovaries and the thickness of the lining of the uterus. A rod-shaped device (sensor) (transvaginal ultrasound) is inserted into the vagina, which emits sound waves and converts them into images on a computer screen.
Is it possible to get pregnant with PCOS
How to get pregnant with PCOS? Getting pregnant with PCOS can be difficult, but that doesn't mean it's impossible. While PCOS can affect your hormones and therefore your fertility, there are medical treatments and lifestyle changes you can make to improve your chances of pregnancy.
Is it possible to get pregnant with polycystic ovaries? To get pregnant, you must ovulate, which PCOS most often prevents. Women who do not ovulate regularly with PCOS do not release enough eggs for fertilization. Pregnancy with PCOS is further complicated by the fact that PCOS causes a hormonal imbalance that changes the quality of cervical fluid, making it difficult for sperm to survive.
It is impossible to say categorically that PCOS is infertility, but PCOS is one of the main causes of infertility in women.
Is it possible to get pregnant with PCOS? And although there are no exact statistics on the chances of pregnancy, 70 to 80 percent of women with PCOS have fertility problems. PCOS disrupts the normal menstrual cycle and makes it difficult to conceive.
Is it possible to get pregnant with PCOS? Polycystic ovary syndrome is not a sentence and it is possible to get pregnant, albeit problematic. However, if PCOS is left untreated, the chances of getting pregnant decrease with age.
It is possible to get pregnant with polycystic disease, but most often pregnancy with polycystic disease is difficult. This condition can increase the risk of pregnancy complications. Women with PCOS are twice as likely to have a preterm birth than women without. They are also at greater risk of miscarriage, high blood pressure, and gestational diabetes. However, by managing the symptoms, many women with PCOS can become pregnant and have a healthy baby.
How to get pregnant with PCOS? Women with PCOS can become pregnant using fertility treatments that improve ovulation. Losing weight and lowering your blood sugar can increase your chances of a healthy pregnancy.
Pregnancy planning for PCOS
How to get pregnant with PCOS? While your chances of getting pregnant with PCOS may be lower, there are a few things you can do to increase those chances.
- Call your doctor. How to get pregnant with polycystic ovaries? Normalization of hormones and menstruation is the first step. Your doctor may prescribe medications to help your body deal with insulin better and regulate your menstrual cycle.
- Maintain a healthy weight. Is it possible to get pregnant with PCOS? Weight loss can lower insulin levels, androgen levels, and restore ovulation. Ask your doctor about a weight management program and meet with a nutritionist regularly for help with your weight loss goals.

- Eat right. Polycystic Ovarian Diet includes sugary foods, simple carbohydrates and unhealthy fats. Add to your menu: fresh and cooked fruits and vegetables, whole grains such as brown rice, oats and barley, beans and lentils, chicken, fish.
- Be active. Exercise helps lower blood sugar levels. How to get pregnant with insulin resistance? If you have PCOS, increasing daily activity such as walking, exercising, walking can help treat or even prevent insulin resistance, control your weight, and avoid developing diabetes.
- Lead a healthy lifestyle. Follow a healthy lifestyle with PCOS, give up bad habits, unhealthy diet, lack of sports and irregular sleep.
Treatment for PCOS
Treatment for PCOS focuses on your individual problems such as infertility, acne or obesity. Also, the direction of PCOS treatment largely depends on whether a woman is planning a pregnancy or not. Specific treatment may include lifestyle changes or medications.
How to treat PCOS?
Lifestyle changes
Your doctor may recommend weight loss through a low-calorie diet combined with moderate exercise. Even small weight loss - like losing 5 percent of your body weight - can improve your condition. Can you get pregnant with PCOS? Losing weight can also increase the effectiveness of medications your doctor recommends to treat PCOS and help with infertility.
Treatment with drugs for polycystic ovaries
To regulate the menstrual cycle, the doctor may recommend:
Combination birth control pills. Estrogen and progestin tablets reduce androgen production and regulate estrogen. Hormone regulation can reduce the risk of endometrial cancer and correct abnormal bleeding, excess hair growth, and acne. Instead of pills, you can use a skin patch or vaginal ring containing a combination of estrogen and progestin.
Progestin therapy. Daily progestin may: restore normal hormonal balance, regulate ovulation, stop excessive hair growth, protect against endometrial cancer, and help get pregnant with sleep deprivation.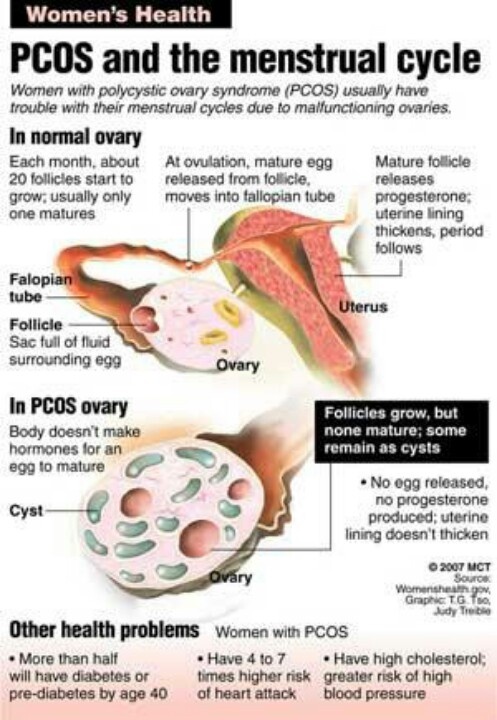
How to induce ovulation in PCOS? To help induce ovulation in PCOS, your doctor may recommend:
Clomiphene is a fertility medication that can help women with PCOS get pregnant.
Metformin is a drug used to treat type 2 diabetes. It also treats PCOS by increasing insulin levels.
Operation
How to get pregnant with PCOS? Surgery may be an option to improve fertility if other treatments don't work. Ovarian drilling is a procedure in which tiny holes are made in the ovary using a laser or a thin, heated needle to restore normal ovulation and the possibility of pregnancy with PCOS.
Important! To determine the right treatment and choose the right drug, you need to consult a doctor!
Help Doc.ua: you can make an appointment with a gynecologist-endocrinologist on the website.
What is polycystic ovary syndrome and how to treat it
Overweight, excessively thick, coarse and dark hair, severe acne and androgenic alopecia - sometimes at first sight you can understand that a woman suffers from polycystic ovary syndrome. It is believed that this syndrome is the cause of up to 70% of cases of infertility in women, as well as the source of many of the complications associated with the occurrence of this disease.
It is believed that this syndrome is the cause of up to 70% of cases of infertility in women, as well as the source of many of the complications associated with the occurrence of this disease.
What is PCOS, what are its symptoms and how is it treated?
The symptoms of PCOS are obvious
Polycystic Ovary Syndrome, or PCOS for short, is an endocrine disease that is a growing problem in the female population of modern civilization. This disease affects approximately 5-10% of women of reproductive age and is the most common cause of ovulatory disorders.
PCOS is an ovarian dysfunction that leads to irregular menstruation, ovulation disorders and eventually infertility. Sometimes the intervals between cycles reach six months or a year, which, of course, complicates pregnancy.
The hormonal changes that cause this condition are manifested by low levels of FSH, but increased levels of androgens and LH. As a result, male hormones increase in the female body, which is called hyperandrogenism.
What does it look like in practice? When androgens are produced by the ovaries and adrenal cortex, a woman develops male sexual characteristics. They mainly include hirsutism, which is excessive hair growth on the arms, legs, chin, neck, above the upper lip, and around the nipples. On the other hand, male-pattern baldness, deepening of the voice, clitoral hypertrophy, thyroid disorders, decreased libido, and the aforementioned menstrual dysregulation can be observed.
Another important symptom that affects up to 50% of patients with PCOS is obesity (especially abdominal), which occurs due to insulin resistance, a metabolic disorder that indicates a decrease in the body's sensitivity to insulin, which is the cause of diseases such as diabetes and et al.
In addition, PCOU contributes to the development of hyperprolactinemia - an increase in prolactin in the blood, which, in turn, leads to increased depression and problems with conception.
Terms used in the description of PKU:
- Androgens are male sex hormones.
- Hyperedrogen is an excess of androgens.
- Hyperprolactinemia is an excess of the hormone prolactin in the blood.
- Hirsutism is excessive hair growth that occurs in women in unusual places for them (beard, abdomen, chest).
- Insulin resistance is a condition in which body tissues are not sensitive to insulin and the pancreas produces too much of it.
Causes of PCOS development
The formation of the disease, of course, is affected by long-term use of contraceptive pills without interruptions.
The second very important factor is the very high amount of harmful chemicals consumed daily in food, such as hormones and steroids found in meat, harmful chemicals and preservatives, or any sweeteners such as glucose-fruit syrup.
A woman has no idea what a huge impact on her weight and hormonal balance is the chemicals included in her daily diet. Meanwhile, insulin resistance, which is one of the causes of PCO, is more common in overweight and obese women suffering from arterial hypertension. And sometimes in patients with a genetic predisposition to diabetes.
And sometimes in patients with a genetic predisposition to diabetes.
How to treat polycystic ovary syndrome?
It is best to start pharmacological treatment by eliminating each of the problems of the syndrome in turn:
- hypertension.
- hypertension; hypertension; insulin resistance.
- hyperprolactinemia.
Treatment includes monitoring the patient's condition through regular examinations such as vaginal ultrasounds, blood tests, and hormonal fluctuations, while taking appropriate medications. Even if a woman with COV finds uniformly sized multipolar ovaries on ultrasound, none of them are large enough to mature and ovulate.
It is very important not to treat PCOS too early if you want to become pregnant in the future. If treatment is started too early, it may not be effective when the mother is about to become a mother. SPCA does not threaten the life or health of the patient, but is primarily a disease of fertility and appearance. Therefore, women planning a pregnancy should wait for treatment until they are ready for it.
Therefore, women planning a pregnancy should wait for treatment until they are ready for it.
The most important thing about PCOS is to recognize that time is against those who want to conceive.
Potentially harmful contraceptives are not recommended for the treatment of PCOS. There are birth control pills that are effective in contraception and at the same time remove excess testosterone from the body and regulate menstruation. However, prolonged use of contraceptives is one of the causes of PCOS, and we must not forget that it is easy to fall into the so-called vicious circle.
On the other hand, problems with insulin resistance, hypertension and hyperprolactinemia should be treated as separate diseases and treated as early as possible.
Pregnancy during treatment has a significant impact on relapse rates after treatment. Then the symptoms will disappear. Otherwise, PCO may reoccur. Unfortunately, patients with PCOS do not complete treatment and may need to take sex hormone balancing and anti-diabetic drugs for the rest of their lives.
Polycystic ovaries is a serious gynecological disease and one of the causes of infertility. The trigger for the development of polycystic vesicles is a violation of humoral regulation, the mechanisms of hormonal regulation of the internal and external secretory glands. Unlike men, the female reproductive organs are cyclical, and if the rhythm is disturbed, this can lead to serious disorders, so it is referred to as polycystic.
About the cost of treating polycystosis in our hospital in St. Petersburg
Toll-free number: 8-800-707-1560
* The clinic is licensed to provide these services.
How polycystic ovaries develop
The main reason is that women of reproductive age for some reason do not ovulate (the release of eggs into the fallopian tubes). The mechanism of occurrence of polycystic disease is as follows.
- Even at the stage of intrauterine development, female embryos and eggs are laid, but up to a certain point they are inactive.
 During puberty, the eggs develop and become available for participation in fertilization, but not all at once, but one (rarely two or three) every month.
During puberty, the eggs develop and become available for participation in fertilization, but not all at once, but one (rarely two or three) every month. - From the first day of menstruation, some follicles are activated, but after a week the dominant follicle is determined and breaks on the 12-15th day. It releases a mature egg. This process is called ovulation.
- After the eggs are released, the hormonally affected follicle sheaths secrete a hormone that is necessary to maintain progesterone, that is, to maintain the uterine layer of the endometrium, which is optimal for the implantation of the connection. Temporary endocrine gland.
- In the event of fertilization, luteil will continue to work for 16 weeks, demonstrating various functions to maintain the embryo in the uterus. In a healthy woman, if fertilization does not occur, the lutea will decrease and disappear when a new period begins.
If an egg is not shed for any reason, the follicle regenerates without breakage and a cyst of fluids accumulates around the egg (immature egg).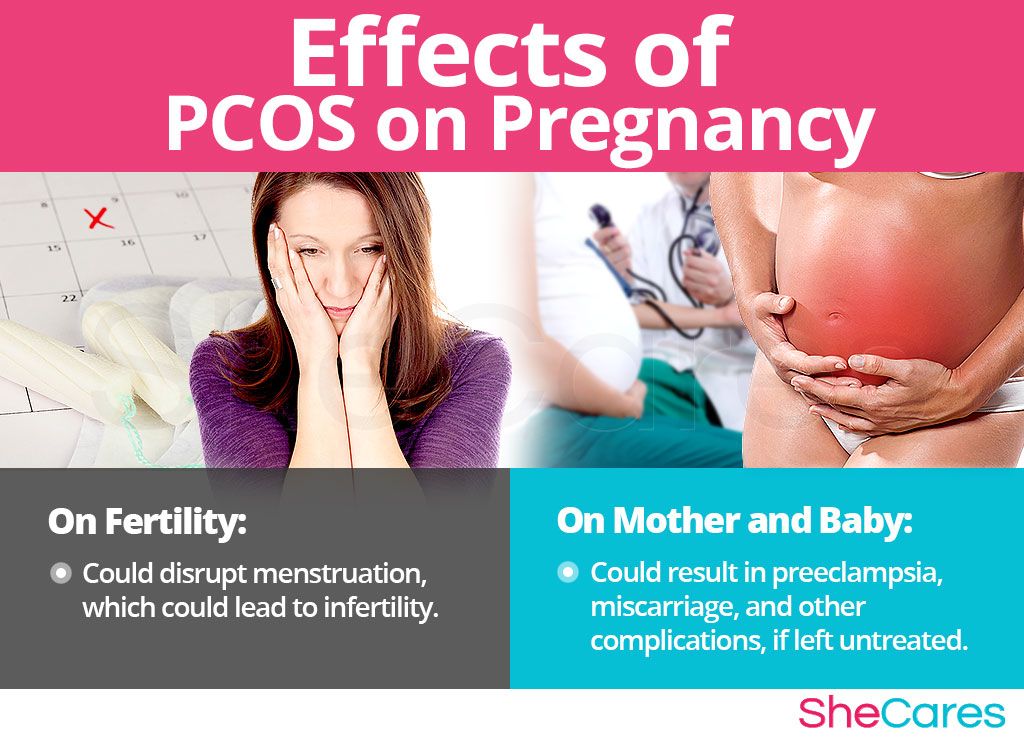 The next month, ovulation does not occur again, new follicles are reborn, and cysts form.
The next month, ovulation does not occur again, new follicles are reborn, and cysts form.
If the body fluid adjustment continues for a long time, the ovaries form a group of cysts that can be seen alone or in a group.
Initial polyglycolic diseases can be well treated because the cause is mainly abnormal hormones. The development of this disease can lead to a complete stop of ovulation and the development of infertility.
Causes of polycystic ovaries
What is the true cause of polycystic ovaries? However, the cause of the onset is known and has been confirmed by observation and medical statistics.
Insulin-resistant insulin refers to a condition in which the cells in the body cannot be detected. Consequently, the body cannot control blood sugar levels. It seems, but what is the link between ovarian disease and diabetes? It turns out right.
Insulin is produced in a special part of the body called "Langel Hansken" in the tail of the pancreas.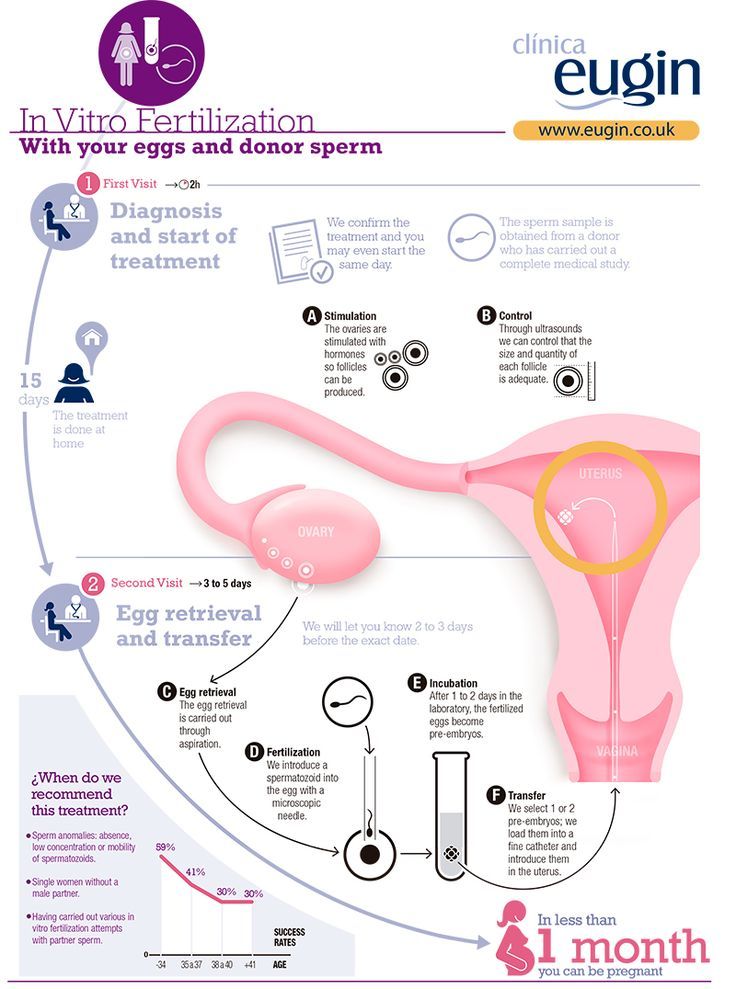 When this hormone enters the bloodstream, the cells are used by taking in sugar or stored as glycogen. Insulin resistance does not respond to insulin, and hyperglycemia has a detrimental effect on the body.
When this hormone enters the bloodstream, the cells are used by taking in sugar or stored as glycogen. Insulin resistance does not respond to insulin, and hyperglycemia has a detrimental effect on the body.
If there is no insulin sensitivity, the pituitary, adrenals, and ovaries only respond to high-dose insulin, resulting in a lack of glucose. To normalize this situation, these organs secrete large amounts of the hormone progterin and androgen.
Insulin resistance develops in 50% of cases with a higher weight, metabolic (metabolic) and a large amount of visceral fat (the layer of fat that surrounds the internal organs).
Abnormal pituitary gland The pituitary gland is a part of the brain that plays a role in the secretion of certain hormones, including sex hormones. The pituitary gland controls the hypothalamus, which is a category of the brain, and the hypothalamus is connected to all parts of the nervous system by nerve cells. The hypothalamic-pituitary gland system supports the body's metabolism and endocrine.
Pituitary hormone secretion is problematic for various reasons. These reasons are as follows.
- Malignant and benign brain tumors.
- Injury trauma to the brain and damage to the brain and due to surgery.
- Gamma a-line irradiation.
- Infectious disease of the brain (encephalitis, meningitis).
- Pituitary disease (ITSENKO syndrome-pieces, hypothyroidism, diabetic diseases, hyperprolactinemia).
- Stroke, pituitary tissue necrosis
- Effects of steroids and antiepileptic drugs.
- Chemotherapy in the treatment of cancer
- Long-term and uncontrolled use of oral contraceptives.
A pituitary defect is manifested by increased production of male hormones (androgens) and a decrease in the level of follicle-stimulating hormone that regulates egg maturation.
Adrenal disorders. These organs, along with the ovaries, are controlled by the anterior pituitary gland and their functions are interrelated. Along with polycystic ovaries, it is often combined with hyperplasia of the adrenal cortex. This disorder interferes with the production of certain hormones, including sex hormones.
Along with polycystic ovaries, it is often combined with hyperplasia of the adrenal cortex. This disorder interferes with the production of certain hormones, including sex hormones.
Diseases of the thyroid gland. Hypothyroidism (deficiency of thyroid hormones) has symptoms similar to polycystic but requires different treatment.
genetic factors. If relatives such as mother, aunt or sister have the disease, the risk of developing PCOS is much higher.
sensual things. Overweight women develop insulin resistance over time. A high percentage of subcutaneous fat also causes less secretion of the hormone FSH, which contributes to the formation of androgens that do not turn into estrogens. In addition to the development of polycystic disease, women experience increased hair loss, weight gain, sweating, unhealthy appetite, oily skin and hair.
Types of polycystic ovaries
According to the mechanism of occurrence, polycystic disease is divided into two types.
- Primary Primary Occurs in 85% of cases. The disease is hereditary and is caused by a violation of the production of many enzymes. This disease is characterized by a violation of the ratio of the secretion of luteinizing hormone and follicle-stimulating hormone. The condition is often associated with insulin resistance and is indicative of severe metabolic disorders.
- secondary. Caused by dysfunction of the adrenal cortex. This type of polycystosis develops as a result of past infections, miscarriages, dystocia, hormonal therapy, stress, etc. The main cause of polycystitis is a violation of the secretion of gonadotropins that disrupt metabolic processes.
Signs and symptoms of the disease
Primary polycysts due to dysfunction of the hypothalamus are less pronounced than secondary polycysts due to pathology of the adrenal glands. The main complaint of the patient is the impossibility of conception.
Patients may also have symptoms of PCOS, including:
- If you have an irregular menstrual cycle or if your periods are more than 35 days apart.

- The growth of excess hair on the face and body due to increased male hormones in the blood.
- alopecia or hair loss
- Rapid weight gain, increased appetite.
- coarse voice
- Rough skin, oily sheen, acne.
- Prediabetes or hyperglycemia.
- Mastosis - proliferation of connective tissue in the mammary glands.
Diagnosis of polycystic ovaries
Polycystic ovaries are fully visualized on ultrasound. First, the size of the ovaries is noticeable. Normally, dimensions of 2 × 3 cm and a volume of up to 10 cm3 are desirable.
During the first phase of the cycle, several 6-8 mm follicles can be seen in the outer layer. In the ovulatory period (12-15 days after the onset of menstruation), the dominant follicle is already clearly visible, and blond body hair appears in its place. All this is displayed on the screen of the ultrasound monitor when examining a healthy woman.
In polycystic properties, the volume of the ovaries increases to 13 cm3, and in case of severe diseases, the size of the uterus exceeds the size of the uterus. Instead of follicles, cysts up to 12 mm in diameter are randomly arranged and look like a "pile of grapes". The ovaries are thick and the increase in tissue junction is noticeable. Dopalatography shows that blood flow to the ovaries is increased.
Instead of follicles, cysts up to 12 mm in diameter are randomly arranged and look like a "pile of grapes". The ovaries are thick and the increase in tissue junction is noticeable. Dopalatography shows that blood flow to the ovaries is increased.
An ultrasound examination of the ovaries alone cannot be accurately diagnosed. Diseases thought to be similar to polycystic ovaries include Cushing's syndrome, hyperprolactinemia, and hypothyroidism. Illuminations are also effective in revealing the extent of cystic lesions. Therefore, you must be tested for hormones.
Which hormones influence the development of PCOS
If you are diagnosed with PCOS, you need to have a hormonal test. By establishing the overall picture, the extent of hormonal abnormalities can be understood and can also help design optimal hormonal therapy.
It is diagnosed based on the following hormone test results.
Lutein (LH)
This peptide hormone is produced before the pituitary gland, along with hormones that cause follicles. In the first half of the cycle, LH promotes estrogen secretion and promotes lutein growth. Thanks to LH, follicles develop.
In the first half of the cycle, LH promotes estrogen secretion and promotes lutein growth. Thanks to LH, follicles develop.
The standard value of the hormone in the first 9-10 days of the menstrual cycle is 1.45-10 MEI/ml. By the time the egg matures, the amount of estrogen peaks, sends a signal to the hypothalamus and commands the pituitary gland to increase follicle secretion (FSH). Lutein hormones increase to 6.15-16.8 ml/ml markers.
When the concentration of LH and FSH increases, the follicle sheaths are torn and the eggs are discharged. From the 16th day from the beginning of menstruation, the LH value decreases from 1.07 to 9.1 ml / ml. Lutein, a polycystic hormone, is produced in large quantities, so the production of androgen (male hormone) flourishes.
FSH (Follicle Start Gormone)
Sugar protein secreted from the pituitary gland. Hormones play a role in the conversion of testosterone to estrogen. The standard value is 3.5-12.5 MEI/ml. If the FSH is below the reference value, the egg cannot be turned into an egg.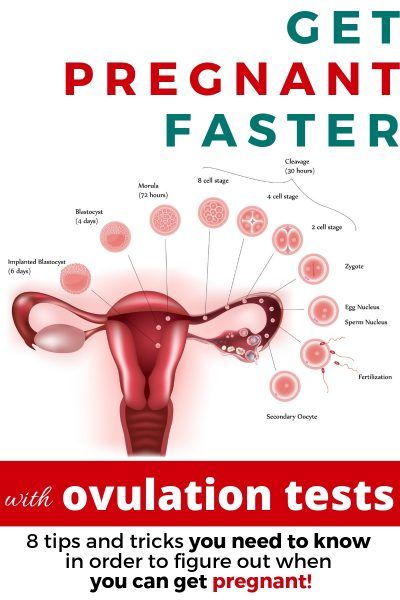 On days 14-16, when ovulation occurs, FSG indicators will be 21.5 mol/ml.
On days 14-16, when ovulation occurs, FSG indicators will be 21.5 mol/ml.
At the same time that the follicle sheath is broken, the concentration of the follicle stimulating hormone drops sharply, and its index is from 1.7 to 9 mol/ml. Hormones are secreted in a pulsed form every hour for the first two phases of the cycle, and then decrease every four hours.
FSG operates in parallel with LH and it is important that the ratio of LH and FSH is 1.5:1-2:1 for prosperity. In polysia, a typical deviation of 2.5:1 or more is, but the same results can be obtained in early pituitary and benign tumors and menopause. Therefore, more accurate diagnosis requires information about other hormones.
testosterone
This is an androgenic male hormone, and without it, the female reproductive organs do not work. Pituitary dysfunction will result in androgen rejection as it begins to move for the first time under the influence of tropical hormones (FSH, LH) secreted from the pituitary gland.
Half of testosterone is produced in adipose tissue and 25% in the adrenal cortex and ovaries, respectively. Under the influence of FSH, testosterone is converted into estrogen, preparing the body for a possible pregnancy. With polycystic ovaries, the balance of luteinizing hormone is disturbed, which leads to an overproduction of the hormone and increased activity of the adrenal cortex. Compared to men, women have lower testosterone levels, on average 0.29-3.17 mU/ml.
insulin
An association has been established between insulin resistance and PCOS, but the exact cause has not been established. However, more than 50% of patients with polycystic ovaries have insulin resistance in adipose muscle tissue with preserved ovarian sensitivity to glucose. As a result, the level of insulin in the blood decreases, which leads to hyperstimulation of the ovaries.
Excessive production of androgens and estrogens disrupts the menstrual cycle. Scientists believe that this type of insulin resistance is genetic and not caused by sugar cravings. Insulin resistance cannot be detected by routine blood glucose measurement. To do this, you must take the HOMA test (homostasis-based insulin resistance assessment model). It is calculated using a special formula and the result should not exceed 2.7.
Insulin resistance cannot be detected by routine blood glucose measurement. To do this, you must take the HOMA test (homostasis-based insulin resistance assessment model). It is calculated using a special formula and the result should not exceed 2.7.
cortisol
A hormone secreted by the adrenal cortex. Participating in many important processes, it is responsible for maintaining energy resources and carbohydrate metabolism. Cortisol is released disproportionately throughout the day. It peaks in the morning and declines in the evening. But under stress, cortisol simply rolls off. The result is palpitations, sweating, anxiety and fear.
When cortisol surges, the pituitary gland suppresses the secretion of convective hormones and, accordingly, less testosterone and estrogen, which are involved in the menstrual cycle. Nature's protection consists in the fact that an increase in cortisol leads to suppression of the secretion of sex hormones, since the birth of a new life in adverse conditions is unfavorable.
The optimal value of cortisol is 138-625nmol/L. Deviations from the norm inhibit the development of follicles and eggs. Prolonged stress can sometimes completely stop menstruation and lead to the development of polycystic ovaries.
17-OH-progesterone
It is an intermediate product of the steroid group and is produced in the female and male body. As a result of metabolism, normal progesterone is converted into 17-hydroxypregnenolone (17-OH-progesterone), from which androgens (testosterone and estradiol) and cortisol are produced.
Concentrations range from 0.2 to 1.2 ng/ml during the first phase of the cycle, rising to 1-4.5 ng/ml after ovulation. In polycystic disease, both elevated and decreased levels of 17-OH-progesterone are observed. In the first case, we can talk about congenital dysfunction of the adrenal cortex.
Under these conditions, the arms and legs gradually become bald, the antennae lengthen, and the back and chest become hairy. At the same time, women have problems with insulin resistance and pressure. Elevated 17-OH-progesterone is a classic example of polycystic ovaries.
At the same time, women have problems with insulin resistance and pressure. Elevated 17-OH-progesterone is a classic example of polycystic ovaries.
Sulfuric acid DEA
dayoxyeproosterone sulfate (DGEAS) is an androgen produced by the adrenocortical and ovarian. DHEAS is converted to testosterone and estrogen by an enzyme called hosfatase. In the case of polycystic ovaries, testosterone is generated in the body instead of female hormones because the concentration of sulfuric acid dehydrocosterone increases. Appears in improvement of appetite, over weight, menstrual disorder, etc.
Ciloxin (T4), trio-stronin (T3), thyroid stimulant (TS)
The pituitary gland secretes thyroid hormone (TSH), which activates the activity of the thyroid gland. Translated between triode silones and siroins, a deficiency in these hormones desensitizes T3 and T4, causing hypothyroidism. Against this background, the production of prolactin increases. If this hormone has a high concentration, it will not only be able to get pregnant, but also cause polycystic ovaries.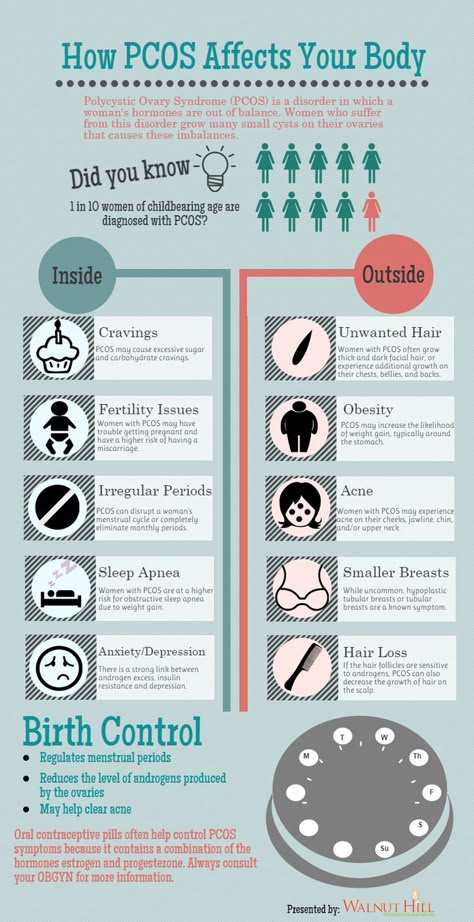
Diagnosis of the causes that caused the development of polycystic ovaries
The onset of polycystic ovaries mainly differs between a decrease in adrenocortical function and damage to the pituitary gland. The doctor performs the following diagnostic tests in order to perform the correct treatment and to make sure that the hormonal preparations are not mistaken.
Dexametazon dexametazon is a synthetic glucocorticosteroid that is active in the body's metabolism. In the Decisametazon epinephrine (secondary polycystic) trial, a polycystic ovary can be confirmed or refuted.
If significant cortical sampling hypercalism is caused by dexamethasone consumption, the adrenal cortex hormone that activates adrenal function is less likely to be secreted. Blood tests show that the level of androgens and metabolites in the urine drops sharply. If the cause of polymeia is not an adrenocortical disorder, the decrease in blood concentration is negligible.
Bark irritation test. The essence of this method is the same as the previous sample, introducing another drug into the blood. With the introduction of adrenocortical stimulating hormone (ACTH), the concentration of androgen in the blood increases sharply, and in polycystic ovaries, the increase is insignificant.
The essence of this method is the same as the previous sample, introducing another drug into the blood. With the introduction of adrenocortical stimulating hormone (ACTH), the concentration of androgen in the blood increases sharply, and in polycystic ovaries, the increase is insignificant.
Implemented a metabolic test. There is a metabolic abnormality in polycystic ovaries. To identify it, an analysis of the lipid composition in the blood is carried out, and the following disorders are detected as confirmation of the diagnosis.
- High density fats have decreased.
- Increasing extremely low density lipid fractions.
- Increased lipopuncture distribution with low density.
Abnormal lipid metabolism causes arteriosclerosis, coronary arteries, thrombosis and renal failure.
Hyperstotic ovaries are not necessarily synonymous with infertility. Multicular infertility accounts for less than one third, and the remaining 70% is well treated with hormonal and surgery.
Ovarcholic cystoria is one of the most common hormonal diseases in women of reproductive age. This can cause irregular menstrual cycles, infertility, or abnormal hair.
Hyper-ovaries are polygonal endocrine diseases that develop under the influence of heredity and harmful environmental factors. This disease is accompanied by an increase in androgen (a type of male hormone).
Diagnosed by objective tests (male culture), ultrasound tests (characteristic changes in the ovaries) and clinical tests (increased testosterone levels).
Treatment is with hormonal agents and must be forced to lose weight (excess). To increase pregnancy, you can use irritation drugs, laparoscopic eggs and IVF for serious illnesses.
Types of polycystic ovaries
It is divided into two types according to the occurrence of polycystic ovaries.
- Primarily e-there is a pathological change since the formation of menstrual function.
- After menstrual function or sometimes after childbirth, a secondary change in hormone adjustment occurs for some reason.
 As expected, this is a more preferred form over primary polycystic properties.
As expected, this is a more preferred form over primary polycystic properties.
Symptoms of polycystic ovaries
Symptoms of polycystic ovaries are as follows.
- Menstrual abnormalities in which the menstrual cycle gradually becomes shorter or ovulation occurs.
- Androjenesi s-mal e-Type Hair removal, hair loss, acne.
- Insulin resistance y-darkening of the skin inside the waist and pubis, accumulation of facial characteristics and relative expansion of the limbs, accompanied by a certain hypertrophy of the muscles.
Such patients often have emotional disorders such as depression, depression, anxiety and desire is always there, and the metabolic disorder is even worse because they always gain weight.。
Causes of polycystic ovaries
The cause of onset is ultimately unknown. It is believed that multiple cysts develop under poor conditions in hereditary characteristics.
The deterioration of inheritance is manifested in the violation of various endocrine connections.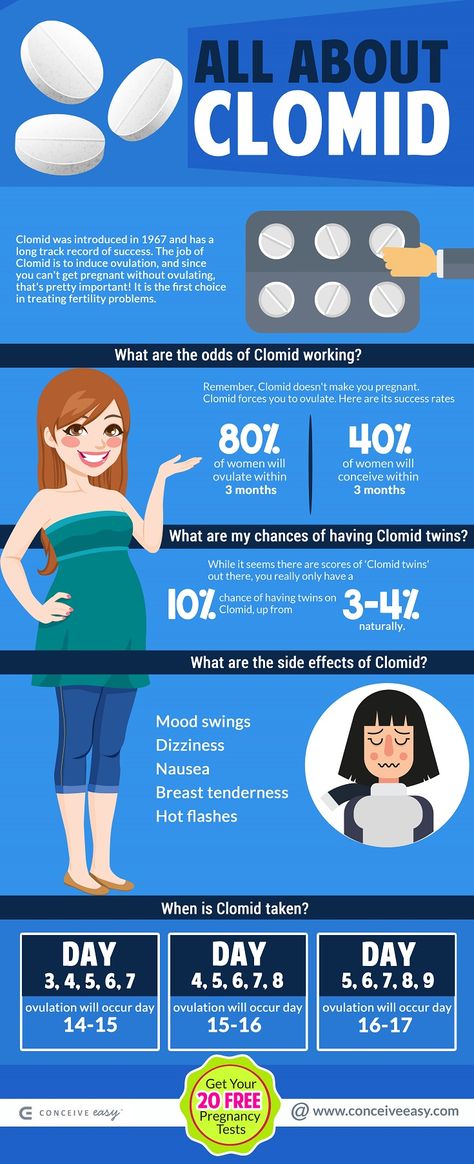 In such patients, the secretion of gonadotropins and insulin changes, causing energy exchange and metabolism of sex hormones. As a side effect factor
In such patients, the secretion of gonadotropins and insulin changes, causing energy exchange and metabolism of sex hormones. As a side effect factor
- Bad unbalanced food; - unbalanced meals; - unbalanced diet.
- Fatty tissue in the body increases.
- Sedentary life; passive lifestyle;
- Stressful situation.
- The ecosystem is bad.
Get advice
If you have any of these symptoms, we recommend that you see a doctor. Business advice prevents negative impact on health.
Details of illness, treatment costs, specialist consultations, etc. can be done by phone.
Why SM-Clinic?
Diagnosis of polycystic ovaries
By diagnosing polycystic ovaries early, you can take the necessary measures in time. Typical complaints associated with this condition are as follows.
- Menstrual delay (menstrual cycle is 35 days or more).
- Start of menstruation too early (cycle shorter than 21 days).

- Those with upper lip hair along the linea alba, i.e. male type
- Hair loss has increased.
- Get pimples or get sick with your skin.
- I gain too much weight and my weight loss is very slow.
- Do not be pregnant for more than 12 months despite regular close relationships.
Gynecological tests can determine if the ovaries are enlarged to the left and right. But the final diagnosis can help you establish an additional method of examination.
- (Ovary volume exceeds 10 ml, follicles increase from 2 to 9mm), but on the day of the menstrual cycle (ovulation is confirmed in 2 cycles in 3 cycles. If not, then it is considered ovulation).
- An assessment of hormonal profiles is an increase in the concentration of free testosterone in the blood and total testosterone.
However, the test looks simple at first glance, but to determine the diagnosis of polycystic ovaries, a huge number of diseases that show similar symptoms (thyroid dysfunction, increased prolactin, androgen syndrome and premature baby disorder. This must be ruled out). For this reason, gynecologists and endocrine scientists have a wide range of studies, including hormonal tests (measuring levels such as thyroid, thyroid, triloxin, prolactin, 17-oxygenogenone, etc.) for each patient. Write down the program.
This must be ruled out). For this reason, gynecologists and endocrine scientists have a wide range of studies, including hormonal tests (measuring levels such as thyroid, thyroid, triloxin, prolactin, 17-oxygenogenone, etc.) for each patient. Write down the program.
Patients diagnosed with polycystic fibrosis should have a sugar-tolerant test or glycosylated hemoglobin level (reflecting blood sugar levels over the past three months). These tests allow you to evaluate carbohydrate metabolism over time and diagnose insulin resistance or type 2 diabetes.
Expert opinion
Histological ovaries are accompanied by hormonal imbalance because they have chronic ovulation. Such disorders can cause hyperactive endometrial processes and endometrial cancer. These risks increase, especially as you gain weight. Another risk of polykisticularity lies in physical handicaps. This condition is often associated with the perfection of the insulin receptor, which is the basis for type 2 diabetes and cardiovascular lesions (atheromas, hardlatosclerosis and coronary artery heart disease).
In the near future, women should consult a gynecologist and correct hormonal abnormalities in time to protect their bodies. Hyposis is harmless, but it can lead to serious complications without eliminating pathological connections. Therefore, it is very important to become a “friend” with a gynecologist and an endocrinologist and to normalize menstrual and reproductive functions in a timely manner.
Treatment methods for polycystic ovaries
Basic ovarian treatment is performed in a preserved manner. Laparoscopic surgery is only recommended for the purpose of improving male disorders when stimulation of ovulation inducers is ineffective. EVO may be needed.
Conservative treatment
At the first stage, the menstrual cycle is corrected, the skin condition improves, and anti-androgenic effects are prescribed by gynecologists and endocrine scientists for the prescription of compound hormonal contraceptives. These drugs reduce the concentration of male hormones in the blood. The treatment period is at least 3 to 6 months. Immediately after the cancellation, the start mechanism can be resigned, so it is saved repeatedly.
The treatment period is at least 3 to 6 months. Immediately after the cancellation, the start mechanism can be resigned, so it is saved repeatedly.
If you are diagnosed with insulin resistance, you will also be prescribed medicines that improve sugar metabolism. Appropriate nutrition with low activation is recommended to reduce excess weight.
Countermeasures with cosmetics are intensified as countermeasures against hair growth. Evaluate the best photo recognition skills. There are also specialized antiandrogens, but they have serious side effects and are prescribed under strict indications.
Ovulation induction is used to treat infertility. If you don't get the results you want after 6 menstrual cycles, your doctor will change your medication. In this case, if pregnancy has not occurred, the gynecologist recommends considering surgery and, possibly, in vitro fertilization.
Surgical treatment of polycystic ovaries
Laparoscopic perforation is recommended for patients in whom conservative treatment has failed and who wish to give birth. Because the eggshell is polycystic, it becomes so thick that it interferes with the natural production of eggs. After laparoscopic puncture, ovulation is not only facilitated, but also stimulated.
Because the eggshell is polycystic, it becomes so thick that it interferes with the natural production of eggs. After laparoscopic puncture, ovulation is not only facilitated, but also stimulated.
The maximum performance of the function lasts for one year, so it is recommended to start a normal sexual life as soon as possible.
Statistics show that polycystic ovary syndrome is diagnosed in 1 out of 10 women of reproductive age. The disease causes an irregular menstrual cycle, infertility and many other complications. Let's take a closer look at its causes, symptoms, and treatments.
Causes of pathology
Polycystic ovary syndrome (PCOS) is an endocrine pathological disease associated with structural changes and dysfunction of the ovaries. Violation of the menstrual cycle, in which the egg does not mature and leaves the follicle (a structural element of the ovary).
As a result, the follicle transforms into a cyst (abnormal cavity with walls and fluid). A story that repeats every month. As a result, many cysts form in the ovaries.
A story that repeats every month. As a result, many cysts form in the ovaries.
It is divided into two types depending on the cause and time of occurrence.
- Primary SPCU. Primary primary SPCU. With this type of syndrome, the first clinical manifestations appear during puberty.
- Average SPKU. This refers to an acquired disease. This occurs as a result of chronic endocrine disorders such as dysfunction of the hypothalamus, pituitary, thyroid and pancreas.
What symptoms accompany polycystic ovaries?
Its symptoms are varied. However, there are signs that are seen in most women with PCOS.
irregular menstrual cycle
In case of illness, the menstrual cycle is usually prolonged, at least 35 days. In some cases, menstruation is very rare and can last from 3 to 6 months.
In 20% of women with this disease, the menstrual cycle is not disturbed, but ovulation has not yet occurred.
Reproductive dysfunction in polycystic ovaries
With this disease, 80% of patients have reproductive dysfunction.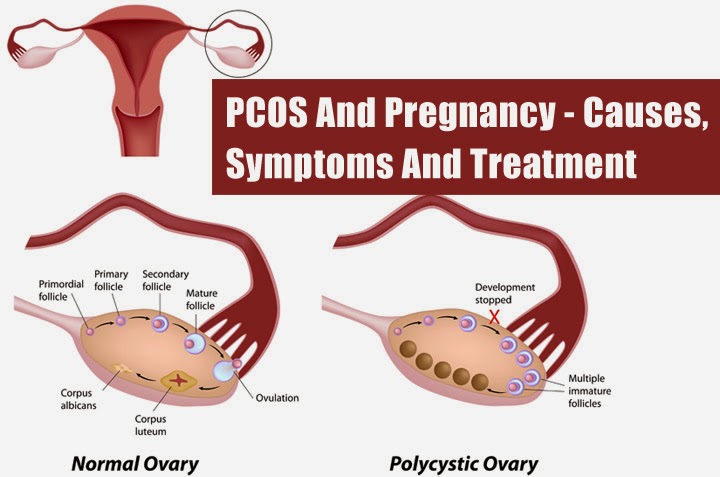 In most cases, infertility is primary and is characterized by the absence of a previous pregnancy.
In most cases, infertility is primary and is characterized by the absence of a previous pregnancy.
If you manage to get pregnant, you are at high risk of miscarriage or premature delivery.
hyperendrogenic
This condition is characterized by excessive secretion of male hormones. A characteristic sign of a violation is the appearance in a woman of male secondary sexual characteristics.
- Development of male terminal hair. It grows excessively on the jaw, upper chest, abdomen, back, etc.
- coarse voice
- Increase perspiration with stimulating fragrance.
- Breast reduction
- The clitoris is enlarged.
Deterioration of the skin and hair condition
Pathology negatively affects the appearance of women, as well as health. Increase the fat and density of the skin, the pores open large, and the face becomes unhealthy gray. There are closed frames and open frames, and inflammation appears on the skin. Age spots can be formed inside the buttocks and underarms.
Age spots can be formed inside the buttocks and underarms.
In addition, there are also gosun ah-glubal lards. The sebum membrane is different from advanced pores, and even with normal care, the hair is immediately infected.
Excessive body
Insulin resistance is a disturbance of the metabolic response to insulin secreted from the pancreas and, in principle, insulin resistance is recognized in patients with this disease. And insulin resistance leads to obesity.
Type 2 diabetes, which is chronic insulin resistance, can cause cardiovascular complications.
Other symptoms of polycystic ovaries
Against the background of rare menstruation, the endometrium causes hyperplasia and appears with thickening of the terminal skin. Observing such disorders and women
- Pain in the lower abdomen
- Discomfort in close relationships.
- Dizziness; dizziness.
- Fatigue increase
- Appetite reduction
- The diagnosis of this disease consists of several elements.
How is the disease diagnosed?
Gynecological tests can detect ovarian growth and tightness for doctors. In addition, the characteristics of the menstrual cycle, genetic diseases, infectious diseases, hair type, skin condition and women's weight are also considered.
- Inspections may be ordered to determine the level of hormones produced by clinical glands, thyroid and testosterone. Inspections are also carried out to study proteins, glucose and blood cholesterol values.
- How to use it as a research device. One of the most information about the diagnostic method is the ultrasound diagnosis. Ultrasound psychological tests include an increase in ovarian size, film thickness, hard layer and due to increased blood flow and at least 12-9 mm in diameter in one ovary.
- Treatment is as follows.
Methods of treatment
Hormonal agents are prescribed for the treatment of endocrine disorders, the formation of the menstrual cycle and the suppression of the effects of androgen.
- A non-historical antagenic drug based on chromifene is used to restore normal ovulation.
- Use a carbohydrate agent when blood glucose levels are high.
- Low-calorie foods and spreading meals (5-6 times a day) are prescribed to normalize weight. Those with high carbohydrates and fat are excluded from the menu. The basis of food are protein and dietary fiber products. Boil, bake and steam food. Moderate exercise is recommended for women.
- Surgery will appear if there is no result in conservative therapy. Surgical treatment is possible.
Use of ovarian extermination. This promotes normal follicles and the surviving egg survives.
- Accompanied by ovarian resection. During the operation, a partially removed tissue of the damaged ovary is performed. As a result, the formed eggs are released from the ovaries.
- Internal Coagulation Method: This is a way to heal ovarian tissue in a place where many follicles accumulate.