Epistaxis during pregnancy
What causes nosebleeds in pregnancy, and tips to manage them | Your Pregnancy Matters
Pregnant women are more likely to get nosebleeds due to increased blood volume, which may cause vessels in the nose to rupture.Pregnancy is full of quirky side effects – including nosebleeds. One in five patients get nosebleeds during pregnancy (epistaxis), compared with 6% of women who get them when not pregnant.
Over the course of pregnancy, your total blood volume doubles to support the growing baby. To accommodate this extra blood, the blood vessels in your body dilate. The pressure of the extra blood can sometimes cause the more fragile vessels to rupture and bleed more easily.
Your nose is rich in tiny blood vessels that can get dried out from normal breathing, which can lead to breakage and bleeding. For most pregnant patients, the occasional minor nosebleed is no cause for alarm. It’s mostly just annoying.
I've invited my colleague, Ashleigh Halderman, M.D., an ear, nose, and throat specialist from UT Southwestern's Otolaryngology Department, to talk about what causes nosebleeds during pregnancy, how women can prevent them, and how to stop them when they do occur.
Colds, medications, and unruly sinuses
Dr. Ashleigh HaldermanEven when you aren't pregnant, you're more likely to get a nosebleed with a cold, sinus infection, or allergies. But approximately 20% of women experience pregnancy rhinitis – inflammation and swelling of the mucous membranes in the nose.
Pregnancy rhinitis causes congestion, postnasal drip, and runny nose. And when you're constantly blowing your nose, you're more susceptible to having a bloody nose.
Certain medical conditions such as high blood pressure or clotting disorders can cause nosebleeds as well.
You may also get a nosebleed if the membranes in your nose dry out and crack due to cold weather, dry air, or intense air conditioning.
Pregnancy tumor: A rare cause of nosebleeds
Also known as a pyogenic granuloma, a pregnancy tumor is a noncancerous, rapidly growing mass of capillary blood vessels that bleeds easily. Research suggests the masses form due to the influx of hormones during pregnancy.
Approximately 5% of pregnant women develop pregnancy tumors, which typically form in the gums between the teeth but can also form in the nose. The masses can appear anywhere on the body and generally disappear after the baby is born.
Treatment usually consists of either a medicated gel or nasal spray, which helps control bleeding. Some women need to have the tumor removed if it is causing breathing problems or excessive nosebleeds. The exact procedure to remove the tumor depends on where the tumor is located. For pregnancy tumors of the nose, most can be removed endoscopically without any external incisions or stitches.
Related reading: 5 weird pregnancy symptoms you might not know about
How can I prevent nosebleeds during pregnancy?
While it’s not possible to prevent all nosebleeds, there are few things you can do to avoid irritating the sensitive blood vessels in your nose.
● Moisturize the inside of your nose: Use a bit of saline nasal gel to lubricate dry or irritated nasal passages.
● Use a humidifier: Because dry air increases the risk of nosebleeds, adding a little moisture to the air can do wonders.
● Drink plenty of fluids: This keeps your mucous membranes well hydrated and less likely to dry out and crack.
● Treat colds and allergies: Talk to your doctor about which over-the-counter medications may be best.
Be especially gentle after a nosebleed. Your nose needs to heal, so don’t blow it too hard or stuff tissues in the nostrils, which can prolong bleeding.
How to stop a nosebleed and when to see your doctor
If you do get a nosebleed during pregnancy (or any other time):
● Sit or stand up to keep your head higher than your heart
● Lean forward slightly to stop the blood from running down the back of your throat into your mouth
● Pinch both nostrils and maintain pressure for 10 to 15 minutes
● To help constrict the blood vessels and slow bleeding, you also can apply a cold pack or ice over the bridge of your nose or use a nasal spray such as Afrin before pinching the nostrils together
Call your health care provider if you experience more than a couple nosebleeds during pregnancy, or if:
● Bleeding doesn’t stop after 30 minutes
● Blood flow is heavy
● You have trouble breathing
● You become lightheaded or disoriented
Pregnancy can cause strange things to happen to your body. While nosebleeds generally are nothing to be overly concerned about, talk to your doctor if you are worried. We're always available to help you feel more comfortable during pregnancy.
While nosebleeds generally are nothing to be overly concerned about, talk to your doctor if you are worried. We're always available to help you feel more comfortable during pregnancy.
To visit with an Ob/Gyn, call 214-645-8300 or request an appointment online.
Management of Severe Epistaxis during Pregnancy: A Case Report and Review of the Literature
- Journal List
- Case Rep Obstet Gynecol
- v.2019; 2019
- PMC6360570
Case Rep Obstet Gynecol. 2019; 2019: 5825309.
Published online 2019 Jan 20. doi: 10.1155/2019/5825309
,,,,,, and
Author information Article notes Copyright and License information Disclaimer
Background
Epistaxis is a common problem during pregnancy. Few cases of severe epistaxis, not associated with nasal lesions or clotting disorders, were described in the literature. We reported a case of severe epistaxis in a pregnant patient, exploring all the different possible management options.
Few cases of severe epistaxis, not associated with nasal lesions or clotting disorders, were described in the literature. We reported a case of severe epistaxis in a pregnant patient, exploring all the different possible management options.
Case
A 33-year-old primigravida, who was 38 weeks pregnant, presented with spontaneous severe left-sided epistaxis. Her blood pressure was into normal ranges. Clotting disorders and nasal lesions were excluded. The patient clinical worsening, due to severe anemia, and the failure of conservative treatment have imposed an emergency caesarean section, with an immediate resolution of the nasal bleeding.
Conclusion
Treatment of severe epistaxis must always consider conservative measures first-line with early recourse to otolaryngologist. In general, delivery of the fetus is considered curative.
Epistaxis is a common problem during pregnancy, due to an increased nasal mucosa vascularity. The prevalence in pregnant women is 20. 3% compared with 6.2% in nonpregnant ones [1]. Large volume epistaxis is rare for patients without preexisting risk factors or conditions, such as the use of anticoagulants or blood clotting disorders.
3% compared with 6.2% in nonpregnant ones [1]. Large volume epistaxis is rare for patients without preexisting risk factors or conditions, such as the use of anticoagulants or blood clotting disorders.
Few cases of severe epistaxis during pregnancy, not associated with nasal lesions or clotting disorders, were described in the literature, demonstrating a lack of familiarity regarding the appropriate management options in these clinical conditions.
We report a case of severe, prolonged epistaxis in a pregnant patient, during the third trimester, with no clear risk factors. We explored the different possible management options in this challenging case and we assume our experience may help in future similarly clinical situations.
A 33-year-old primigravida, who was 38 weeks pregnant, presented with spontaneous severe left-sided epistaxis. Her first episode had started the previous week, with about seven-eight episodes a day. Her medical history was unremarkable. She had no personal or family history of bleeding tendencies, and she was not taking any regular medications. Her blood pressure was into normal ranges. She reported no previous episodes of epistaxis in her life. Routine blood tests were normal during the pregnancy.
Her blood pressure was into normal ranges. She reported no previous episodes of epistaxis in her life. Routine blood tests were normal during the pregnancy.
We tried to control the bleeding first by administrating intravenous (IV) tranexamic acid, without resolution. So, we contacted the otolaryngologist, who performed an endoscopy, showing a left nasal floor bleeding varix. He decided for an anterior nasal packing: he inserted a tampon carefully along the floor of the left nostril, where it expanded on contact with blood. After the nasal tampon was been inserted, the otolaryngologist wetted it with a small amount of topical vasoconstrictor in order to hasten effectiveness. This procedure was repeated three times, inserting a total of six tampons (four in left nostril and two in the right one). Nevertheless, this conservative management of epistaxis failed. Within 4 hours of admission, patient haemoglobin had dropped from 12.5 to 7 mg/dl and she had a further bleed from the left nostril. The otolaryngologist did not consider a posterior nasal packing because the endoscopy showed an anterior bleeding site. A new endoscopy to locate the exact site of bleeding for direct cauterization was not indicated in acute setting due to vascular congestion and mucosal oedema. Patient clotting studies were within the normal range. A blood transfusion was required, using two packed red blood cells (PRBCs). The patient also started antibiotic therapy with IV Cephazolin 2 g every 8 hours. Cardiotocography (CTG), biophysical profile, and fetal Doppler demonstrated fetal well-being.
The otolaryngologist did not consider a posterior nasal packing because the endoscopy showed an anterior bleeding site. A new endoscopy to locate the exact site of bleeding for direct cauterization was not indicated in acute setting due to vascular congestion and mucosal oedema. Patient clotting studies were within the normal range. A blood transfusion was required, using two packed red blood cells (PRBCs). The patient also started antibiotic therapy with IV Cephazolin 2 g every 8 hours. Cardiotocography (CTG), biophysical profile, and fetal Doppler demonstrated fetal well-being.
During her second day of admission, repeated blood tests showed that her haemoglobin remained persistently low at 7.5 g/dl, despite the recent blood transfusion. The patient became tachycardic (rate 157 bpm), tachypnoeic (22 breaths per minute), and asthenic.
After accurate counselling with the patient and considering the failure of conservative treatment, we thereby decided for a surgical management of pregnancy. The patient delivered a healthy baby girl weighing 3.9 kg. The execution of caesarean section was followed by an immediate resolution of the nasal bleeding.
The patient delivered a healthy baby girl weighing 3.9 kg. The execution of caesarean section was followed by an immediate resolution of the nasal bleeding.
We discharged the patient from the hospital with nasal packing, in order to ensure the formation of an adequate clot. Five days later, the otolaryngologist performed an endoscopy to locate the exact site of bleeding for direct cauterization. The patient experienced no other episodes of epistaxis.
Epistaxis in pregnancy is common but the vast majority of cases do not require medical attention. The prevalence of epistaxis in pregnant women is more than three times that in nonpregnant ones [1].
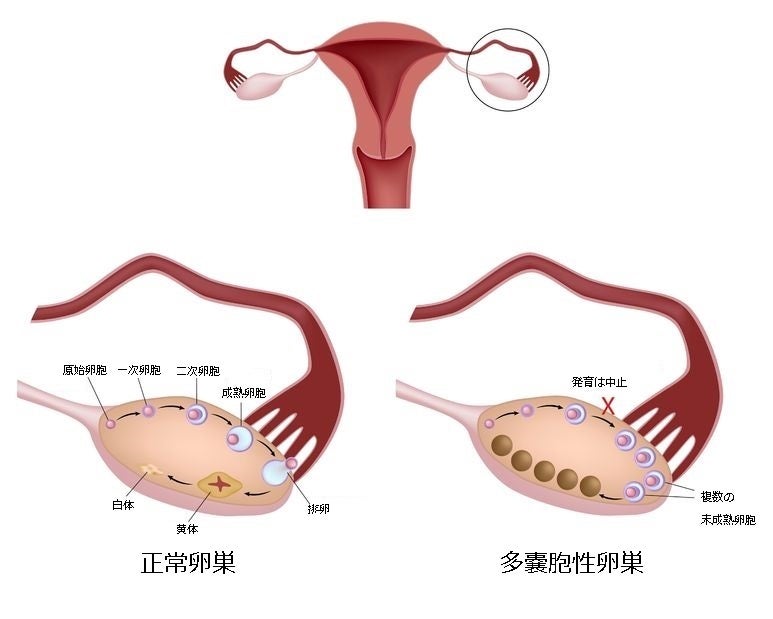
Several conditions predispose to epistaxis during pregnancy. In particular, the elevated oestrogen levels increase the vascularity of the nasal mucosa [10], which may potentiate and prolong the bleeding. Progesterone causes an increase in blood volume, which may exacerbate both vascular congestion and hence bleeding, and may mask blood loss in the event of severe epistaxis, due to apparently effective cardiovascular compensation [11]. Placental growth hormone has systemic effects, including vasodilation [11]. Indirect hormonal effects include vascular inflammatory and immunological changes that may predispose to nasal hypersensitivity and hence to problems such as nasal granuloma gravidarum [11]. In general, delivery or fetal death causes immediate cessation of the nasal bleeding, because some of the underlying factors, such as congestion and hyperemia, disappear.
Placental growth hormone has systemic effects, including vasodilation [11]. Indirect hormonal effects include vascular inflammatory and immunological changes that may predispose to nasal hypersensitivity and hence to problems such as nasal granuloma gravidarum [11]. In general, delivery or fetal death causes immediate cessation of the nasal bleeding, because some of the underlying factors, such as congestion and hyperemia, disappear.
Few cases of severe epistaxis during pregnancy were described in literature [2–8, 12] (). We excluded cases of epistaxis associated with nasal lesions, like granuloma gravidarum [9] and nasal polyp [13], or clotting disorders [14].
Table 1
Cases of severe epistaxis during pregnancy not associated with nasal lesion or clotting disorders.
| Author/year | Number of patients | Management of epistaxis | Management of pregnancy |
|---|---|---|---|
| Green L K 1974 [2] | 1 | Local pressure; nasal packing | Emergency caesarean section |
| | |||
| El Goulli M 1979 [3] | 1 | Nasal packing | Vaginal delivery |
| | |||
| Howard DJ 1985 [4] | 1 | Nasal packing; bipolar diathermy; external carotid artery ligation; nasal balloon | Emergency caesarean section |
| | |||
| Braithwaite J M [5] | 1 | Nasal packing; nasal balloon | Emergency caesarean section |
| | |||
| Cooley 2002 [6] | 1 | Nasal packing; nasal balloon | Emergency caesarean section |
| | |||
| Hardy 2008 [7] | 1 | Nasal packing; bipolar cautery; artery ligation | Vaginal delivery |
| | |||
| Cornthwaite K 2013 [8] | 1 | Nasal packing; bipolar diathermy | Elective caesarean section |
| | |||
| Crunkhorn RE 2014 [9] | 1 | Nasal packing; sphenopalatine artery (SPA) ligation; bipolar cautery; bipolar diathermy | Elective caesarean section |
| | |||
| Our case 2018 | 1 | IV∗ tranexamic acid nasal packing; bipolar cautery | Emergency caesarean section |
Open in a separate window
Footnotes: ∗ intravenous.![]()
Treatment of severe epistaxis must always consider conservative measures first-line, like IV tranexamic acid administration, anterior packing and bipolar cautery. If conservative treatment fails, two radical treatments have to be considered: the one is surgical, in the form of vessel ligation, and the other is obstetrical and is termination of the pregnancy.
In our case, the patient clinical worsening and the failure of conservative treatment imposed an emergency caesarean section. The cervix was unfavorable for easy induction and a long induction of labor was considered contraindicated for this patient. Valsalva maneuvers could also aggravate the bleeding during labor, increasing the risk of fetal hypoxia. The decision to deliver was also influenced by the gestational age; in fact in the case of a preterm pregnancy, when maternal and fetal conditions are good, a conservative management is preferred, in order to avoid the possible risks associated with preterm birth.
Fetal anemia is a well-known cause of antenatal fetal distress. The case report by Braithwaite JM et al. [5] demonstrated that rapidly developing severe maternal anemia, due to recurrent blood loss of nonplacental origin, even in the absence of maternal hypotension, can cause fetal distress. Severe epistaxis is potentially life-threatening to both mother and fetus.
The case report by Braithwaite JM et al. [5] demonstrated that rapidly developing severe maternal anemia, due to recurrent blood loss of nonplacental origin, even in the absence of maternal hypotension, can cause fetal distress. Severe epistaxis is potentially life-threatening to both mother and fetus.
This case highlights the importance of early recourse to ear, nose, and throat (ENT) referral, when epistaxis is unresponsive to simple measures. In general, when nasal lesions and clotting disorders cannot be identified, fetal delivery is considered curative, showing that hormonal changes during pregnancy may lead to significant alterations of nasal physiology, with oestrogen causing vascular congestion, mucosal oedema, and rhinitis, known as the “rhinitis of pregnancy”. Moreover, pregnancy is associated with significant anatomic and physiologic remodeling of the cardiovascular system. Starting at 6-8 weeks of gestation and peaking at 32 weeks, maternal blood volume increases by 40–50% above nonpregnant volumes [15, 16]. Termination of pregnancy resolves hypervolemia and hormonal changes; in fact in all the cases reported in , we can observe a nasal bleeding resolution after delivery.
Termination of pregnancy resolves hypervolemia and hormonal changes; in fact in all the cases reported in , we can observe a nasal bleeding resolution after delivery.
The authors declare that they have no conflicts of interest.
1. Dugan-Kim M., Connell S., Stika C., Wong C. A., Gossett D. R. Epistaxis of pregnancy and association with postpartum hemorrhage. Obstetrics & Gynecology. 2009;114(6):1322–1325. doi: 10.1097/AOG.0b013e3181bea830. [PubMed] [CrossRef] [Google Scholar]
2. Green L. K., Green R. S., Harris R. E. Life-threatening epistaxis associated with pregnancy. American Journal of Obstetrics & Gynecology. 1974;120(8):1113–1114. doi: 10.1016/0002-9378(74)90159-8. [PubMed] [CrossRef] [Google Scholar]
3. El Goulli M., Chelli M. Severe epistaxis during pregnancy. A case history. Journal de Gynécologie Obstétrique et Biologie de la Reproduction. 1979;8:437–439. [PubMed] [Google Scholar]
4. Howard D. J. Life-threatening epistaxis in pregnancy. The Journal of Laryngology & Otology. 1985;99(1):95–96. doi: 10.1017/S002221510009633X. [PubMed] [CrossRef] [Google Scholar]
The Journal of Laryngology & Otology. 1985;99(1):95–96. doi: 10.1017/S002221510009633X. [PubMed] [CrossRef] [Google Scholar]
5. Braithwaite J. M., Economides D. L. Severe recurrent epistaxis causing antepartum fetal distress. International Journal of Gynecology and Obstetrics. 1995;50(2):197–198. doi: 10.1016/0020-7292(95)02438-I. [PubMed] [CrossRef] [Google Scholar]
6. Hardy J. J., Connolly C. M., Weir C. J. Epistaxis in pregnancy - not to be sniffed at! International Journal of Obstetric Anesthesia. 2008;17(1):94–95. doi: 10.1016/j.ijoa.2007.09.003. [PubMed] [CrossRef] [Google Scholar]
7. Cornthwaite K., Varadharajan K., Oyarzabal M., Watson H. Management of prolonged epistaxis in pregnancy: Case report. The Journal of Laryngology & Otology. 2013;127(8):811–813. doi: 10.1017/S0022215113001576. [PubMed] [CrossRef] [Google Scholar]
8. Crunkhorn R. E. M., Mitchell-Innes A., Muzaffar J. Torrential epistaxis in the third trimester: A management conundrum. BMJ Case Reports. 2014;2014 doi: 10.1136/bcr-2014-203892.203892 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
BMJ Case Reports. 2014;2014 doi: 10.1136/bcr-2014-203892.203892 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
9. Noorizan Y., Salina H. Nasal septal haemangioma in pregnancy. Medical Journal of Malaysia. 2010;65(1):70–71. [PubMed] [Google Scholar]
10. Goldstein G., Govindaraj S. Rhinologic issues in pregnancy. Allergy & Rhinology. 2012;3(1):13–15. doi: 10.2500/ar.2012.3.0028. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
11. Sobol S. E., Frenkiel S., Nachtigal D., Wiener D., Teblum C. Clinical manifestations of sinonasal pathology during pregnancy. Journal of Otolaryngology. 2001;30(1):24–28. doi: 10.2310/7070.2001.20906. [PubMed] [CrossRef] [Google Scholar]
12. Cooley S. M., Geary M., O'Connell M. P., Keane D. P. Hypovolaemic shock secondary to epistaxis in pregnancy. Journal of Obstetrics & Gynaecology. 2002;22(2):229–230. [PubMed] [Google Scholar]
13. Scott P. M. J., Van Hasselt A. Case report of a bleeding nasal polyp during pregnancy. Ear, Nose & Throat Journal. 1999;78(8):p. 592. [PubMed] [Google Scholar]
Case report of a bleeding nasal polyp during pregnancy. Ear, Nose & Throat Journal. 1999;78(8):p. 592. [PubMed] [Google Scholar]
14. Aynağolu G., Durdağ G. D., Özmen B., Söylemez F. Successful treatment of hereditary factor VII deficiency presented for the first time with epistaxis in pregnancy: A case report. The Journal of Maternal-Fetal and Neonatal Medicine. 2010;23(9):1053–1055. doi: 10.3109/14767050903440463. [PubMed] [CrossRef] [Google Scholar]
15. Hytten F. E., Paintin D. B. Increase in plasma volume during normal pregnancy. Obstetrical & Gynecological Survey. 1963;70:602–607. doi: 10.1097/00006254-196408000-00008. [CrossRef] [Google Scholar]
16. Costantine M. M. Physiologic and pharmacokinetic changes in pregnancy. Frontiers in Pharmacology. 2014;5(65) doi: 10.3389/fphar.2014.00065. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Articles from Case Reports in Obstetrics and Gynecology are provided here courtesy of Hindawi Limited
reasons how to stop, is it dangerous?
Is nosebleed during pregnancy a cause for concern?
How to stop a nosebleed if it starts?
How to avoid nosebleeds?
Do I need to see a doctor?
Video
« I am pregnant and my nose bleeds all the time. Is it normal? »
Is it normal? »
Absolutely! And you are not alone. Nosebleeds affect one out of every five pregnant women and occur six times more frequently than non-pregnant women.
Of course you don't feel comfortable when this happens. But let me reassure you that in most cases, nosebleeds do not harm either your health or the health of your unborn child.
Why is nosebleed so common during pregnancy?
As usual, all the bad things that happen during pregnancy are due to hormones.
This is important to know!
As early as the first trimester of pregnancy, estrogen and progesterone levels rise and cause the tiny blood vessels inside the nose to dilate.
To provide both you and your baby with enough oxygen, the amount of blood circulating in the body increases and the heart works harder. All this together can sometimes damage the vessels of the nose and cause them to rupture, which leads to bleeding from the nose.

Is nosebleed during pregnancy a cause for concern?
In most cases, nosebleeds will not harm you or your baby.
Attention!
If the bleeding continues without stopping for more than 20 minutes or is very intense, it is a good idea to immediately go to the nearest medical facility where you will receive emergency treatment by stopping the bleeding with nasal packing or electrocoagulation.
How to stop a nosebleed if it has started?
- Sit comfortably and don't be nervous - stress raises blood pressure and can lengthen bleeding time.
- Keep your head upright - this will reduce the pressure in the blood vessels inside the nose and help slow down the bleeding. Do not tilt your head back - this can lead to blood entering the respiratory tract and coughing.
- Pinch the soft part of the nose under the bony part between the thumb and forefinger - both sides of the nose should be firmly pressed against each other.

- If the blood is coming out too hard and running down your throat so that you have to swallow it, lean forward a little - swallowed blood may cause vomiting.
- Have someone place an ice pack or frozen vegetables on the back of your head and hold it.
- After 10 minutes (you can set the timer on your phone), release the sides of your nose and check if there is still blood.
- If so, try pinching your nose again and wait another 10 minutes.
Note
If bleeding occurs frequently and you find it difficult to wait 20 minutes each time, you can purchase a hemostatic sponge from a pharmacy and use it. It is a combination of collagen, hemostatic and antimicrobial agents.
Contraindications for the use of a hemostatic sponge during pregnancy and lactation have not been identified.
How to avoid nosebleeds?
- Dry nasal mucosa makes nosebleeds more likely.
 Use a humidifier in your home, especially during the winter months.
Use a humidifier in your home, especially during the winter months. - Avoid mucosal injury when picking or blowing your nose. Try to open your mouth when sneezing so that air does not forcefully escape through your nose.
- Immediately after the bleeding stops, refrain from vigorous physical exercise so that it does not reopen.
- Handle your nose carefully, avoid punching or even playful nose-pulling.
Do I need to see a doctor?
If the nose bleeds for the first time, this is desirable. The doctor will check your blood pressure and, if the bleeding was significant, may order blood tests - general and clotting.
Seek medical attention if subsequent nosebleeds occur:
- your blood pressure is higher than usual;
- you are taking blood thinners;
- the bleeding was very difficult to stop;
- bleeding occurred after a blow to the head, not even a very strong one;
- after bleeding you have difficulty breathing, you feel dizzy or very pale;
- you think your nose might be broken.

If the medical examination has ruled out all serious causes of nosebleeds, but they continue to haunt you, use our advice and just try to wait out the bleeding like bad weather.
videos
Photo: © Depositphotos
* The information provided cannot be used for self-diagnosis, treatment determination and does not replace a visit to a doctor!
Heading Pregnancy
Important: experts told how and when it is best to get vaccinated against COVID-19for pregnant women
Hypoplasia of the uterus: is pregnancy possible
Motherhood is an exquisite inconvenience of being everything for another person
Comments
Learn and participate
- when everyone is healthy! New technologies in the field of education How to help a child with a choice of profession? Safe Internet for a child Bulling at school: how to protect a child?0005
Why does the nose bleed during pregnancy - tips in the pregnancy calendar on Babyblog.
 ru
ru During pregnancy, a woman undergoes a lot of external and internal changes. Some of them are absolutely natural in nature and should not cause concern to the expectant mother, while others require an urgent appeal to specialists. If you read somewhere on the forums that a nosebleed during pregnancy is a trifle and quite normal, you should hardly trust such words. And the thing is that there can be a huge number of reasons for this phenomenon, and not all of them are harmless. Therefore, you still have to contact a qualified specialist if you have a problem with nosebleeds.
The main reasons why this happens
Against the backdrop of revolutionary changes in the entire body of the future mother and its hormonal changes, there is such a phenomenon as increased blood circulation in the vessels, including in all mucous membranes. For this reason, the inner shell of the nose of a pregnant woman becomes hypersensitive to every outside influence. For the same reason, expectant mothers often complain about nasal congestion. Of course, under such circumstances, bleeding is more frequent than usual, but each case still needs to be considered on an individual basis.
Of course, under such circumstances, bleeding is more frequent than usual, but each case still needs to be considered on an individual basis.
A more dangerous cause of such a phenomenon as nosebleeds during pregnancy may be a sharp increase in blood pressure. To accurately determine this, it is enough to use a tonometer during the next hemorrhage. Even a slight increase in the readings of the mercury column (by 10-20 mm) should already be a reason for an immediate visit to the doctor. The thing is that such a phenomenon necessarily negatively affects the uteroplacental blood flow, and this can cause spontaneous abortion. When such a threat becomes real, it is usually accompanied by other signs: dizziness, headache, flashing in the eyes.
Doctor's recommendation
Many doctors recommend that pregnant women have a blood clotting test if they bleed frequently. Such a simple procedure helps to accurately determine the cause of this unpleasant ailment. If the analysis turns out to be normal and does not show any pathological changes in the body, then you will be offered to limit yourself to taking Ascorutin-type vitamins. If blood clotting is below normal, then you will have to go for a consultation with a hematologist. Usually in such cases, patients are treated in a hospital.
If blood clotting is below normal, then you will have to go for a consultation with a hematologist. Usually in such cases, patients are treated in a hospital.
A very important point - do not self-medicate! This applies not only to such a serious illness as nosebleeds during pregnancy, but even to the most common rhinitis. Especially avoid any chemicals - aerosols, nose drops, etc. Not only will they not help, but they are quite capable of harming your little one. But what can really become your salvation is the installation of a high-quality air humidifier in an apartment. It will bring particular health benefits in winter, when the air in the room is extremely dry.
In addition, frequent nosebleeds can be helped by drinking plenty of fluids all the time. But in general - listen to what the doctor says - if he believes that your condition is within the acceptable range, then you should not be upset - both a runny nose and bleeding will go away on their own almost immediately after childbirth. Just be patient a little, because you have to endure not such inconveniences for the sake of the baby.
Just be patient a little, because you have to endure not such inconveniences for the sake of the baby.
What to do when bleeding?
Sit on a chair and hold your bleeding nostril closed for a few minutes. At the same time, tilt your head down a little, allowing the blood to flow out calmly. In no case should you lie down and raise your head up - too. Blood can enter the stomach and cause nausea, vomiting, and even stomach cramps. Naturally, if the blood from the nose during pregnancy cannot be stopped in the simple way described above, then this may indicate more serious problems.
How can this unpleasant phenomenon be prevented?
1. Ventilate the apartment more often. Thanks to such a simple action, you can prevent the nasal mucosa from drying out, which means that bleeding will not threaten you;
2. When you blow your nose or sneeze, do it carefully, because the vessels in your nose are already very fragile, besides weakened by the current general condition of your body;
3.