Big blood clot after miscarriage
Miscarriage - Better Health Channel
What is a miscarriage?
A miscarriage is defined as the loss of a pregnancy before 20 weeks gestation. Miscarriage happens when a pregnancy stops growing. Eventually, the pregnancy tissue will pass out of the body. Some women will feel crampy, period-like pain and in most cases there will be vaginal bleeding.
Most spontaneous miscarriages (75 to 80 per cent) occur in the first 12 weeks of pregnancy. It is estimated that 1 in 4 pregnancies end in miscarriage. Many miscarriages are unreported or go unrecognised because they occur very early in the pregnancy.
Causes of a miscarriage
A miscarriage usually occurs because the pregnancy is not developing properly. The development of a baby from a female and a male cell is a very complicated process. If something goes wrong with the process, the pregnancy will stop developing. Miscarriages are more common in older women than younger women, largely because chromosomal abnormalities are more common with increasing age.
Another cause of miscarriage may be that the developing pregnancy did not embed itself properly into the lining of the uterus (womb). The natural reaction of the uterus is to expel the non-viable pregnancy.
Symptoms of a miscarriage
Pain and bleeding in early pregnancy can mean that you are having a miscarriage, but not always. Bleeding is very common in early pregnancy, affecting about one in four women, many of whom will go on to have a healthy baby. Early bleeding that does not lead to miscarriage will not have caused your baby any harm.
If the bleeding is being caused by a miscarriage, there is no treatment or therapy that can stop the miscarriage from occurring. However, it is still very important that you see a health professional.
Treatment for a miscarriage
Nothing can be done to stop a miscarriage once it has begun. Treatment is aimed at avoiding heavy bleeding and infection. It is also aimed at looking after you, physically and emotionally.
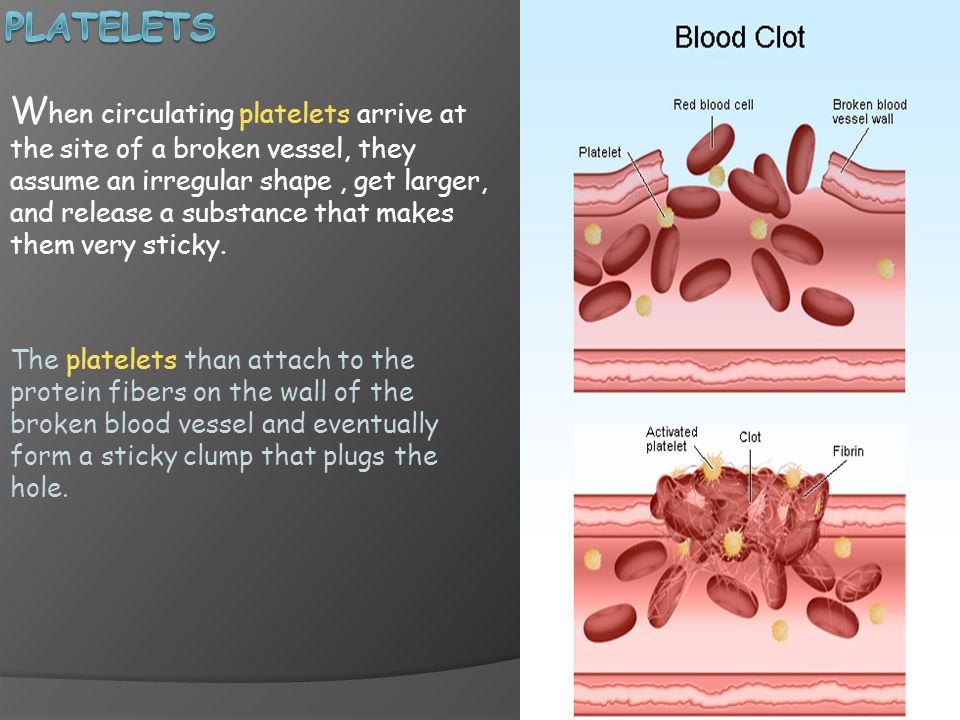
You may need to wait a short period of time before treatments begin. If you experience heavy bleeding with clots and crampy pain in that time, it is likely that you are passing the pregnancy tissue. The bleeding, clots and pain will usually settle when most of the pregnancy tissue has been passed.
Sometimes, the bleeding will continue to be heavy and you may need further treatment. If you think you are having, or have had, a miscarriage, you should see a doctor or go to an emergency department.
You should go to your nearest emergency department if you have:
- increased bleeding – for instance, soaking 2 pads per hour or passing golf ball-sized clots
- severe abdominal pain or shoulder pain
- fever or chills
- dizziness or fainting
- vaginal discharge that smells unpleasant
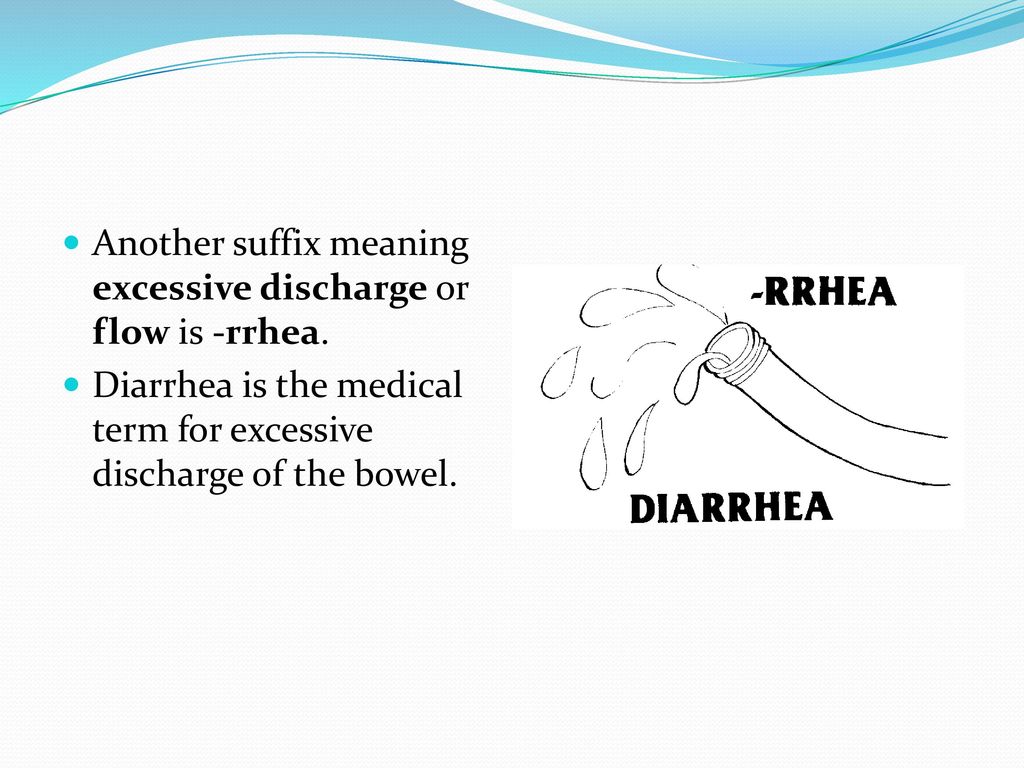
- diarrhoea or pain when you open your bowels.
Types of miscarriage
The types of miscarriage that can occur include:
- Missed abortion– occurs when the pregnancy has failed, although there has not been any bleeding or other signs.
 Occasionally, the aborted pregnancy may remain in the uterus for weeks or even months until bleeding commences. Missed abortion is suspected when pregnancy symptoms disappear and the uterus stops growing. It is diagnosed by an ultrasound examination.
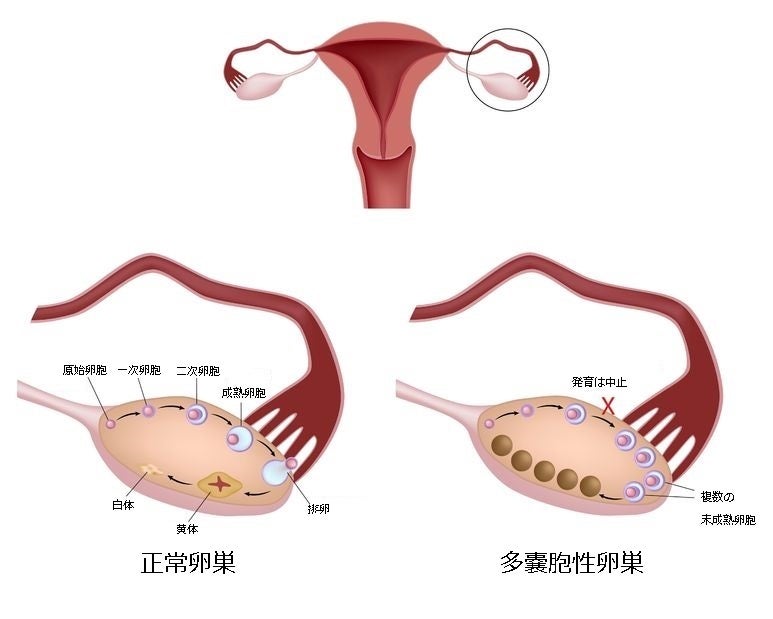
Occasionally, the aborted pregnancy may remain in the uterus for weeks or even months until bleeding commences. Missed abortion is suspected when pregnancy symptoms disappear and the uterus stops growing. It is diagnosed by an ultrasound examination. - Blighted ovum– this occurs when a pregnancy sac is formed, but there is no developing baby within the sac. This is diagnosed by ultrasound, usually after some bleeding.
- Ectopic pregnancy– this occurs when the developing pregnancy implants in the fallopian tubes rather than in the uterus. One to two per cent of all pregnancies are ectopic and without treatment, an ectopic pregnancy can seriously impact on your health and fertility.
Reactions to miscarriage
There is no ‘right way’ to feel after a miscarriage. A range of feelings is normal, and they often linger for some time after the miscarriage. Reactions may include feelings of:
- emptiness
- anger and disbelief
- disappointment
- sadness and a sense of isolation.

Some degree of grief is very common, even if the pregnancy wasn’t planned. Partners may react quite differently, just as people can respond differently to a continuing pregnancy. Try to take it a day at a time and acknowledge your feelings and reactions as they arise.
In addition to the grief you may feel, your body will be undergoing many hormonal changes, which may make you feel very emotional. Family or close friends can be a great source of support at these times. Alternatively, you may choose to seek professional support.
Don’t blame yourself for a miscarriage
Pathology tests are sometimes performed after a miscarriage, but usually, no cause can be identified. This can add to feelings of distress and disbelief, and may lead to feelings of guilt. However, doctors agree that a miscarriage is rarely caused by anything the mother did – or didn’t – do (for example, drank a glass of wine, ate a particular food, had sex or did not rest enough). In the majority of cases, the next pregnancy proceeds to full term.
After a miscarriage
Often, some of the pregnancy tissue remains in the uterus after a miscarriage. If it is not removed by scraping the uterus with a curette (a spoon-shaped instrument), you may bleed for a long time or develop an infection. Unless all the pregnancy tissue has been passed, your doctor will usually recommend that a curette (also called a ‘D&C’ – dilation and curettage) be performed. This is done under a light general anaesthetic and you can usually go home later the same day. A sample of tissue is usually sent for pathology tests.
After the curette
Most women bleed for 5 to 10 days following a curette. Contact your doctor if you experience:
- prolonged or heavy bleeding
- blood clots or strong abdominal pain
- changes in your vaginal discharge
- fever or flu-like symptoms.
Your next period after a miscarriage
Your ovaries will usually produce an egg about 2 weeks after your miscarriage. Your first period should occur within 4 to 6 weeks.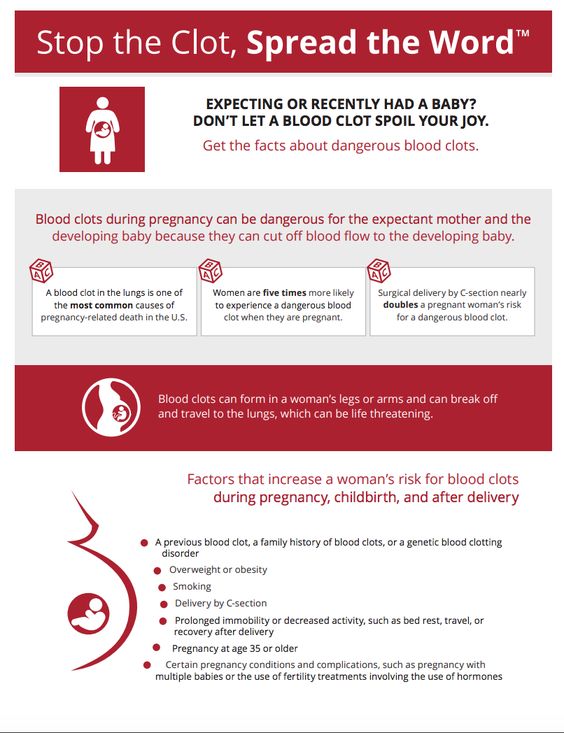 You should have a check-up with your doctor 6 weeks after your miscarriage to make sure there are no problems and to ensure your uterus has returned to normal size. You can also ask any questions about your miscarriage at this time, including the results of any pathology tests.
You should have a check-up with your doctor 6 weeks after your miscarriage to make sure there are no problems and to ensure your uterus has returned to normal size. You can also ask any questions about your miscarriage at this time, including the results of any pathology tests.
The effect of miscarriage on future pregnancies
Most of the problems that cause miscarriage happen by chance and are not likely to happen again. One miscarriage does not significantly increase the risk of the same thing happening with your next pregnancy, as long as no specific cause has been found. Testing is not usually offered to women who have miscarried once or twice because it is very unlikely that anything would be found.
However, women who have had 3 consecutive miscarriages are at risk of miscarrying again. If you fall into this category, you can attend the Recurrent Miscarriage Clinic at The Royal Women’s Hospital for further investigations, counselling and management of future pregnancies.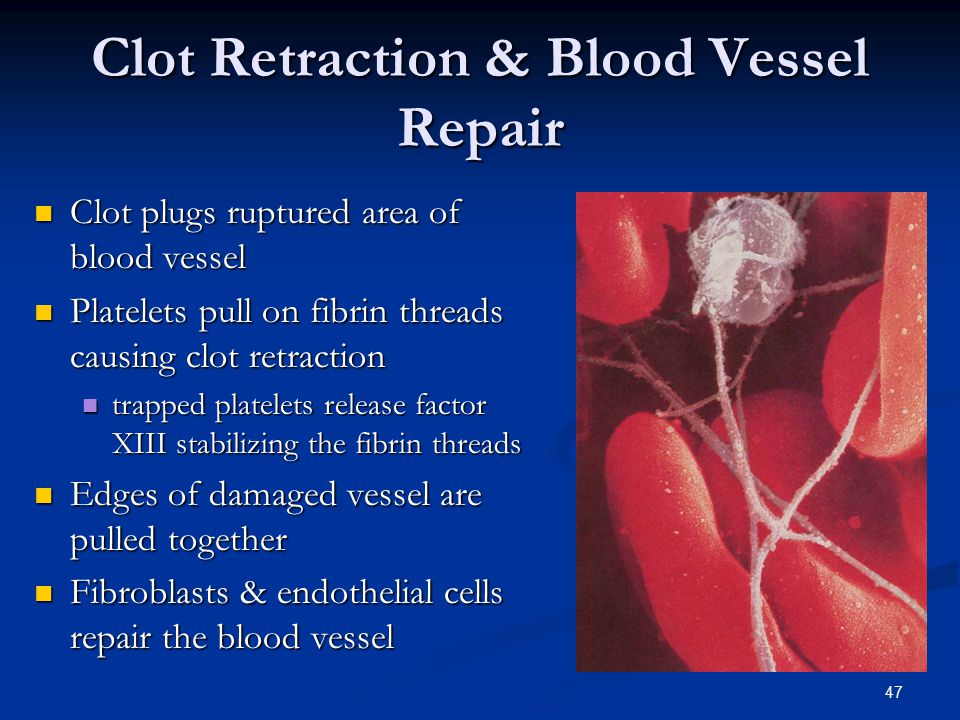
Trying for another pregnancy after miscarriage
There is no right time to try for another pregnancy. Some people decide they need time to adjust to their loss, while others want to try again right away. It is usually suggested you wait until after your next period before trying again. As it is possible to become pregnant again straight away, it is important to use contraception until you are ready to try again.
If you are Rh (Rhesus) negative
If you have an Rh negative blood group, you will require an injection of anti-D immunoglobulin following a miscarriage. This will prevent problems with the Rh factor in future pregnancies. Your doctor will discuss this with you further.
Preparing for another pregnancy after a miscarriage
Although the common reasons for miscarriage cannot be prevented, you can improve your chances for long-term fertility and a successful pregnancy by:
- stopping smoking
- taking regular exercise and having a balanced diet
- reducing stress
- maintaining your weight within recommended limits.
Take folic acid
It is recommended that all women planning a pregnancy take folic acid as it helps promote the normal development of a baby’s nervous system. You will need to take 0.5 mg per day for one month prior to pregnancy and up to 12 weeks gestation.
Where to get help
- In an emergency, call 000 for an ambulance
- Your GP (doctor)
- The Royal Women’s Hospital Tel. (03) 8345 2000
- Recurrent Miscarriage Clinic, The Royal Women’s Hospital Tel. (03) 8345 2000
- Stillbirth and Neonatal Death Support (SANDS) Tel. (03) 9899 0218
Miscarriage - Atlanta Gynecology and Obstetrics
Loss of pregnancy before 20 weeks is called a miscarriage. Spontaneous miscarriage is the most common complication of early pregnancy and the rate decreases as the pregnancy progresses.
Miscarriages occur in 8-20% of clinically-recognized pregnancies:
- 80% of these happen in the first 12 weeks of pregnancy
- The rate of loss for unrecognized or “chemical pregnancies” is 13-26%
- The overall risk of loss after 15 weeks is relatively low
Causes of miscarriage
Though it is difficult to identify what causes all miscarriages, most pregnancy losses are thought to be due to chromosomal defects.
- Chromosomal Abnormalities > 60%
- Maternal: Structural Abnormalities
- Uterine Fibroids, Septums, and Adhesions
- Trauma
- Acute Infections
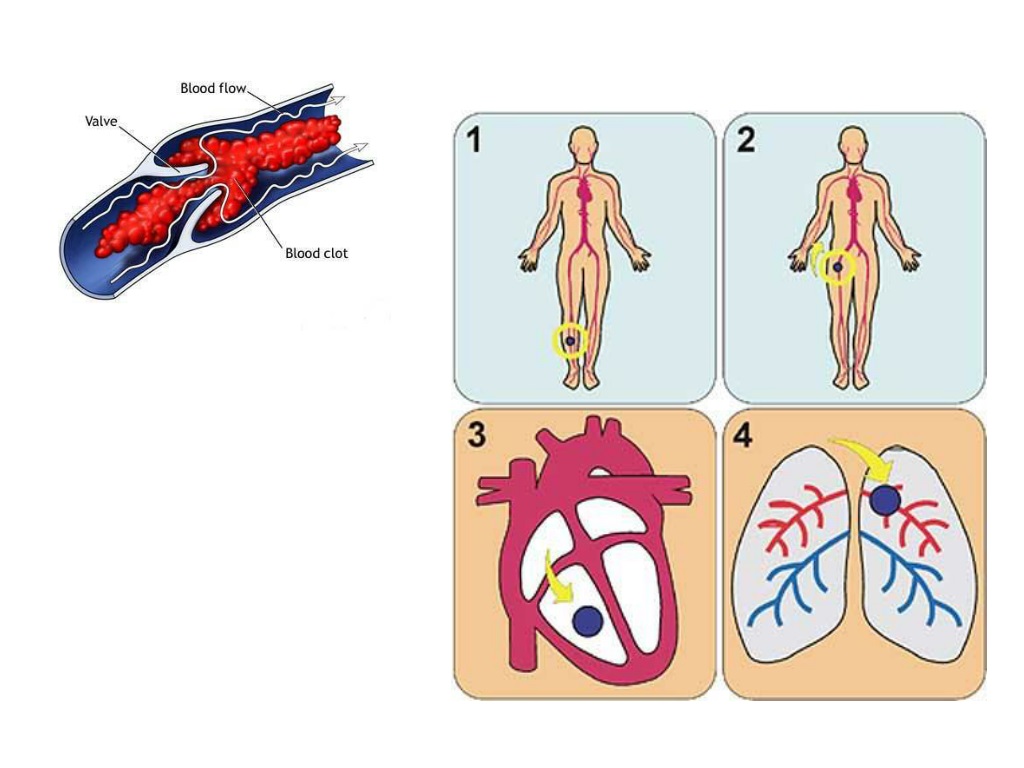
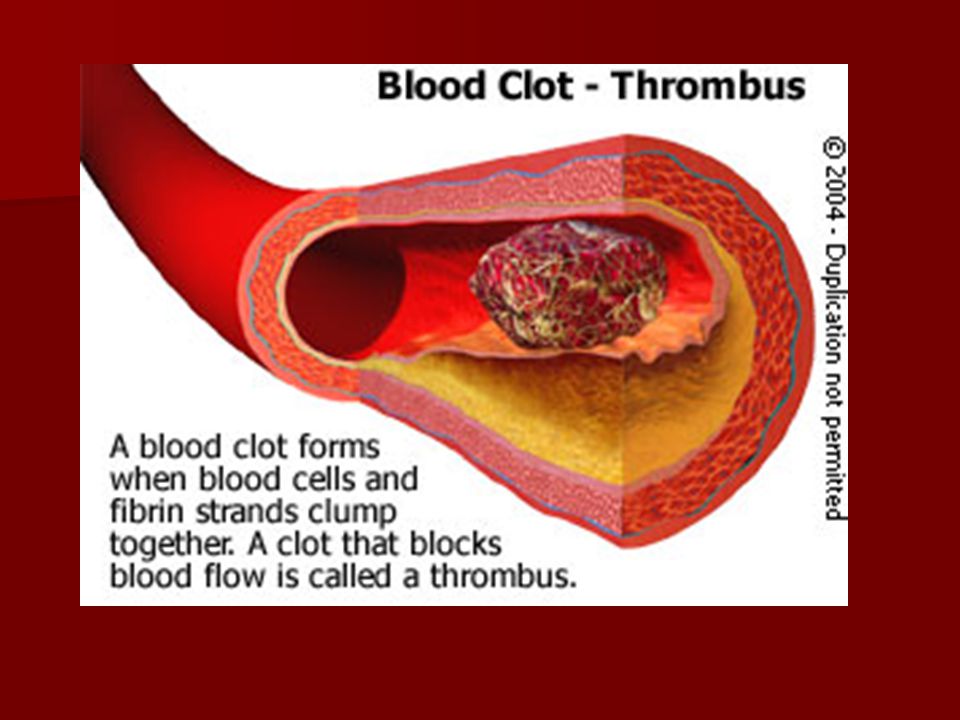
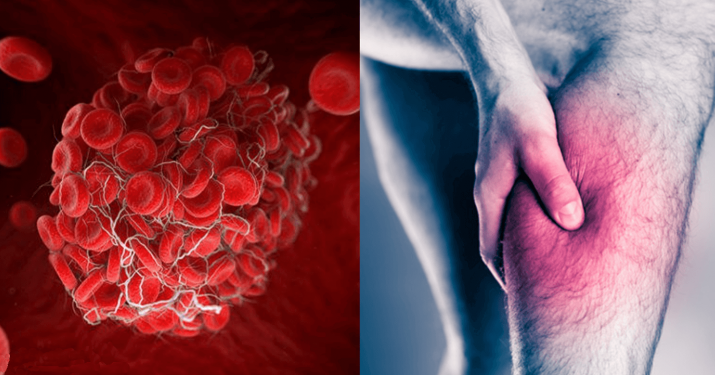
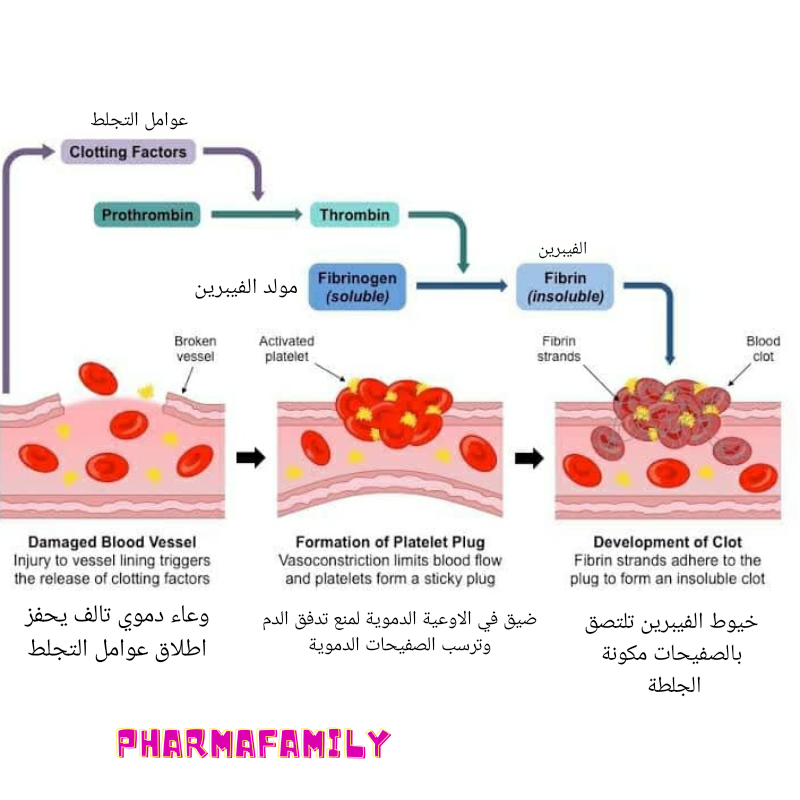
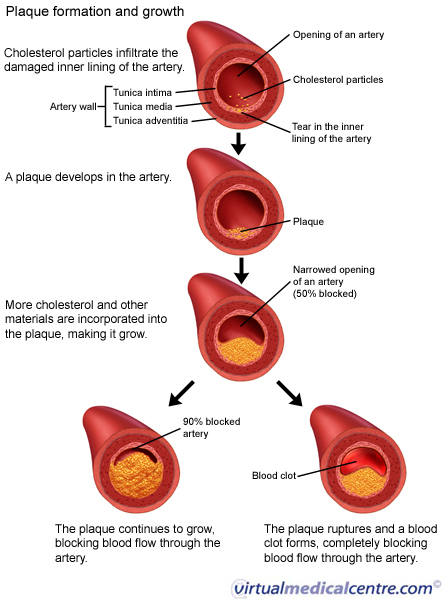
- Blood Disorders (Thrombophilia)
- Unexplained
Loss of viability of the pregnancy usually occurs between 6-12 weeks. Recognition may not occur until weeks later. The course of treatment that you take will depend on your current condition, your desires, the size of your pregnancy, and your provider recommendations.
Factors associated with miscarriage
There can be many factors that affect the probability of having a miscarriage. In many cases, there is more than one factor that comes into play. If you know what these factors are, you can be more cautious.
- Age: Miscarriage risk increases with age. The risk can be as high as 40% at 40 years old and 80% after 45 years old
- Previous miscarriage: The rate of miscarriage increases with the number of previous miscarriages: 20% after one, 28% after two consecutive, and 43% after three or more consecutive losses
- Smoking: Increases the risk of loss
- Alcohol use: Studies have been inconsistent in proving that alcohol can cause an increased rate of pregnancy loss.
 One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day
One study indicated that there was an increase in miscarriages among women who drank more than 3 drinks a day - Cocaine use
- Non-steroid anti-inflammatories (NSAIDs: Ibuprofen, Advil, Motrin): May be associated with an increased risk of miscarriage if used around the time of conception. The prostaglandin in NSAIDs may interfere with proper implantation
- Caffeine: The risks of miscarriage increase with high levels of consumption (>300mg /day)
Miscarriage at home
You may first note mild vaginal spotting and/or cramping. This bleeding and cramping will increase, at which point you may expel the tissue of the pregnancy. During the miscarriage, you may bleed heavily with large clots, soaking a pad every 10-20 minutes. The cramping may be significant. Tylenol and a heating pad are okay to use at this time. You should call the office or the on-call doctor if the heavy bleeding does not improve after two hours.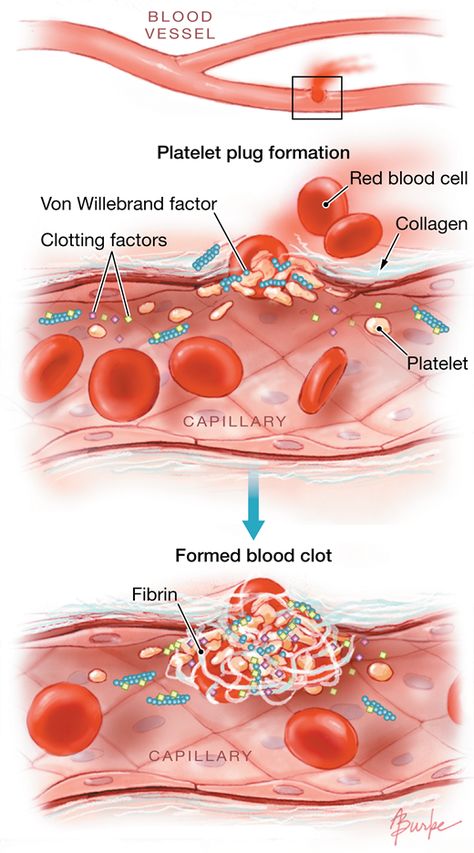
Once you have passed the pregnancy tissue, you will notice a decrease in bleeding and cramping. You may collect the passed tissue and store it in a clean and dry container and bring it to the office so that it may be sent out for pathological identification. You may call the office or the on-call doctor at any time for direction and advice.
Office Number: 404-299-9724 | After Hours Number: 404-487-2450
D&C at the hospital
A D&C is a surgical procedure performed under anesthesia to remove tissue from the uterus that has not started to or that has not entirely come out.
A D&C is an outpatient procedure that lasts for about 15-20 minutes. You usually go home about 1-2 hours after the procedure is completed. Most women return to light duties and activity the next day. Cramping and bleeding are common after a D&C. You may have bleeding for up to 2 weeks after your procedure.
Alternatively, we offer appropriate candidates a procedure called a Mechanical Vacuum Aspiration (MVA).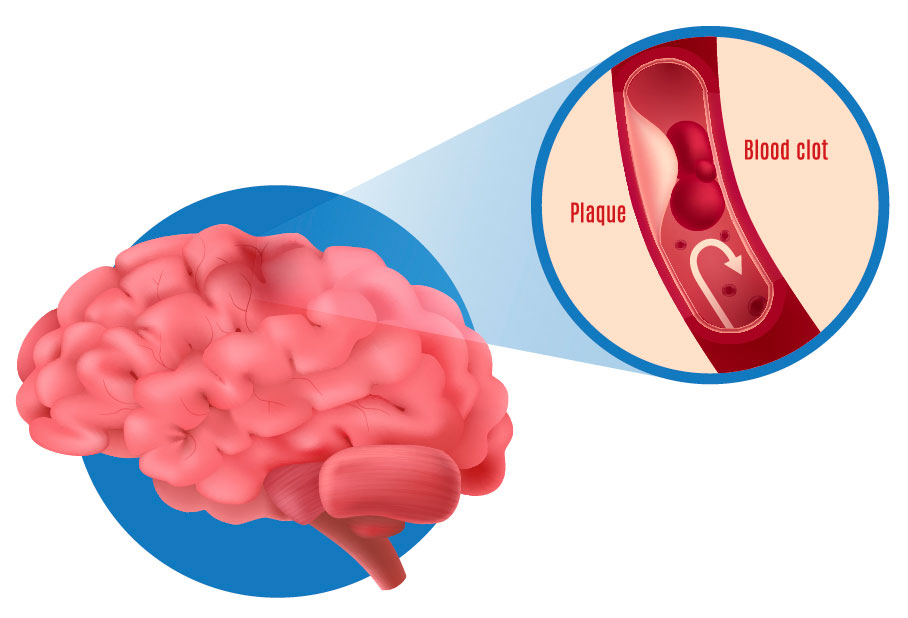 This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
This procedure is similar to the D&C, but it can be done in the office under local anesthesia. Recovery and warning signs are similar to those of the D&C procedure.
With either of these procedures, we recommend that you do not put anything in the vagina (no tampons, douching, or intercourse) until you are seen again in the office.
Warning signs after a miscarriage or D&C
Call the office if you have:
- Temperature > 100.4
- Nausea and vomiting for > 12 hours
- Increasing pain or bleeding
- Foul-smelling vaginal discharge
Coping with the loss of pregnancy
Emotional healing can take longer than physical healing. Grief after a pregnancy loss is a normal response. In the days and weeks after your pregnancy loss, you may experience a loss of appetite, emotional changes, irritability, sleep disturbances, and inability to focus on daily tasks. This is all normal and should resolve in a few weeks or months. If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
If you find that these symptoms are severe or that you are unable to cope with these feelings, please call and make an appointment to talk to a provider in our practice. We will be able to help you and make any other referrals you may need.
The next pregnancy
Your next period should come within 4-6 weeks after your miscarriage. We recommend that you use contraception until after you have had a normal period. You may continue prenatal vitamins during and after this time. You may also discuss birth control at your post-miscarriage visit if you do not desire to become pregnant again.
Thrombogenic risk factors in pregnant women.
220045, Minsk, st. Semashko, 10
This email address is being protected from spambots. You must have JavaScript enabled to view.
Version of the site for the visually visible
Healthcare Institution
Minsk Clinical Consulting and Diagnostic Center
Coll-Center (Registration)
| +375 17 311 10 19 (10 lines) | |
| +375 17 355 94 50 (7 lines) | |
| +375 29 238 00 90 (mobile MTS 4 lines) | |
| +375 44 550 00 90 (mobile A1 4 lines) |
Apply online
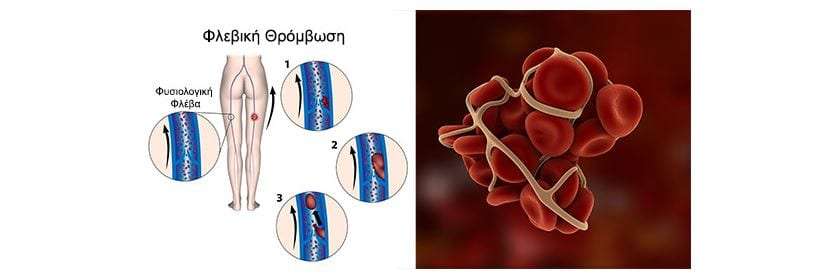
Minsk Clinical Consultative and Diagnostic Center Book online If a woman has a history of recurrent miscarriage or fetal loss in late pregnancy, second toxicosis half pregnancy, intrauterine growth retardation, placental abruption or placental infarction, she is indicated for testing for thrombophilia. Hyperhomocysteinemia, which sometimes develops under the influence of hereditary genetic polymorphism, is associated with late toxicosis and is involved in the development of infarcts and placental abruption. Inflammation of the endothelial lining of blood vessels associated with elevated levels of homocysteine causes an increased risk of both venous and arterial thrombosis. Hyperhomocysteinemia can be caused by the presence in the body of altered forms of the enzyme methylenetetrahydrofolate reductase (MTHFR), which is normally involved in the conversion of homocysteine to methionine. Hereditary polymorphism of factor Leiden (V), which has a strong predisposition to thrombosis, occurs with an increased frequency in women with recurrent miscarriage. Among patients with recurrent miscarriage, abnormal forms of factor V Leiden are most common in women who have miscarriages in the second trimester of pregnancy. Hyperhomocysteinemia itself does not have a significant association with early fetal loss, suggesting that folic acid deficiency and MTHFR polymorphism may act through additional as yet unknown factors. Elevated levels of homocysteine are also detected during pregnancies complicated by preeclampsia, and this increase persists after childbirth. Other causes of placental thrombosis. Pregnancy may contribute to the manifestation of a genetic defect, as it develops the following features: The risk of thrombosis in inherited forms of thrombophilia can be reduced by the use of small doses of aspirin, heparin, folic acid, intravenous immunoglobulin G, or hematogenous factor concentrates. In all pregnant and non-pregnant individuals, folic acid intake significantly reduces homocysteine levels. Efficiency is high in cases where pre-treatment homocysteine levels were highest and lowest if homocysteine levels were relatively low. A decrease in homocysteine levels has been observed with the use of folic acid at a dose of 0.5 mg to 5 mg per day in combination with vitamin B6. There is a high probability of thromboembolic complications and in the presence of cardiovascular diseases, overweight, anemia, late toxicosis. The risk of thrombosis also increases in women in the age group after 40 years, in the presence of malignant tumors, a sedentary lifestyle. Causes of thrombosis First of all, the development of postpartum thrombosis is associated with changes in the blood coagulation system. During natural childbirth or caesarean section, blood is lost. The volume of blood loss can be different - from minimal (physiological) to significant (pathological), which depends on the specific situation. In any case, the body seeks to stop further blood flow, producing a large number of factors that increase blood coagulation by forming clots-plugs in the lumen of blood vessels. And the more blood loss, the more active these processes. In addition, when the placenta passes or due to mechanical tissue damage during the operation, the vessel wall is also damaged, special proteins and enzymes of the endothelium (the inner lining of the vessel) are released into the blood, which is also important for shifting processes towards increased blood coagulation. To reduce the risk of venous thromboembolic complications during pregnancy, the use of low molecular weight heparins (LMWH) in prophylactic and intermediate doses in the form of subcutaneous injections is recommended. However, at present, the decision to prescribe LMWH to pregnant women is made only on the basis of a thrombotic history or if a particular thrombophilia is detected (factor V Leiden mutations, prothrombin mutations, antithrombin deficiency, carriage of antiphospholipid antibodies, etc.). These indications for the appointment of LMWH are subjective, since they are not based on accurate laboratory data measuring excessive (thrombotic) activation of blood coagulation at different stages of pregnancy. Accordingly, the use of these indications leads to unreasonably widespread use of heparins during pregnancy. Congenital thrombophilia (a condition of increased blood clotting), caesarean section, advanced age of the mother and overweight increase the likelihood of blood clots during pregnancy. It is important to note that the risk of blood clots persists for up to two months after delivery. The treatment of thrombosis is a complex process that must necessarily take place under the supervision of a physician. Therefore, in the presence of risk factors, thrombosis prophylaxis is recommended. Prevention can be non-drug and drug. The doctor determines the degree of risk for each patient - low, moderate, high. After that, a method of prevention is selected. As a rule, one non-drug prophylaxis is not enough for people with an increased risk of developing thrombosis, therefore, drug prophylaxis is carried out along with it. In this case, special drugs are used that prevent the formation of blood clots. Antiphospholipid syndrome (APS) is the cause of many obstetric complications such as fetal loss syndrome, HELLP syndrome, preterm birth. The high risk of adverse obstetric outcomes in APS necessitates pregnancy planning and the selection of adequate therapy for a pregnant woman with this pathology. Today, APS is one of the urgent problems in obstetric practice. Clinical manifestations of APS in obstetrics are fetal loss syndrome, intrauterine growth retardation, HELLP syndrome, oligohydramnios, fetoplacental insufficiency, preterm birth, preeclampsia (preeclampsia and eclampsia). Fetal loss syndrome is currently considered as a specific marker of APS. Termination of pregnancy in APS can occur at any stage of pregnancy, and very often spontaneous miscarriage is the only symptom to suspect APS in a patient. The high risk of adverse obstetric outcomes in APS dictates the need for pregnancy planning in these patients, careful selection of drug therapy and constant monitoring of the mother and fetus. At the stage of pregnancy planning in a patient with APS, it is necessary to exclude concomitant risk factors for thrombosis. The range of preventive measures includes correction of excess weight, treatment of concomitant arterial hypertension, correction of lipid disorders, smoking cessation, as well as the use of compression stockings for post-thrombophlebitic syndrome. Pregnant women with APS from the moment of conception are prescribed low doses of ASA (50-100 mg per day, but not more than 150 mg per day) and low molecular weight heparins until delivery. Cancel low molecular weight heparins 12-24 hours before delivery. Treatment with heparins is resumed 12 hours after delivery for a period of at least 4-6 weeks. Timely diagnosis and adequate therapy of APS in pregnant women, careful monitoring of hemostasis system parameters, regular monitoring of the fetal condition, joint management of pregnancy by an obstetrician-gynecologist and related specialists can improve perinatal outcomes. Deep vein thrombosis is the formation of a clot (thrombus) in the lumen of a vessel (in this case, deep veins located in the thickness of the muscles of the lower extremities), which causes a violation of blood circulation. The disease is manifested by arching pain, redness and swelling at the site of thrombosis. The disease can be asymptomatic or lead to a life-threatening complication - pulmonary embolism 1 . Women are less at risk of developing venous thrombosis, however, during pregnancy, the likelihood of its occurrence increases significantly. This is due to changes in hormonal levels, compression of the pelvic veins by an enlarged uterus, imbalance of the blood coagulation system, which can lead to pathological thrombosis in the veins 2 . From the first days of pregnancy, the body of the expectant mother undergoes serious changes: hormonal changes occur, hemoglobin, ferritin, vitamin B12 levels may decrease, cholesterol, insulin, alkaline phosphatase levels increase, the volume of circulating blood changes (in this way the body adapts to the development of the fetus and subsequent childbirth), the circulatory system is rebuilt, and the organs begin to work “for two”. Thrombotic complications are the main direct cause of maternal death during pregnancy and the postpartum period: 12.8% of all maternal deaths 3.6 . Therefore, it is necessary to closely monitor the health of a woman during pregnancy. Major risk factors for thrombosis in pregnant women Congenital vessels of blood vessels and blood coagulation systems The use of oral contraceptives and hormonal therapy Oncological diseases Varicose veins Pressure of the veins of the pelvis Chronic diseases of the cardiovascular system Pregnancy and the postpartum period years of age more than 35 years Sedentary lifestyle Major risk factors for thrombosis in pregnant women Main risk factors for thrombosis in pregnant women Key symptoms of thrombosis 4 Almost always, the disease in the early stages is without symptoms. However, some common signs of thrombosis can be identified: How to protect yourself? Avoid oral contraceptives and other drugs that affect blood clotting 6 months before the planned pregnancy to reduce the risk of blood clots. During the planning and course of pregnancy, regularly consult with your doctor, carefully following all his recommendations aimed at improving the health of mother and baby 4 . Pregnancy visit schedule 3.5 Preparing for the visit 3 When planning a pregnancy, in addition to your doctor, you can also consult a hematologist or any other specialist who deals with the problem of thrombosis and hemostasis during pregnancy. It is worth remembering which of the tests you have taken in the last couple of months: this will help the doctor track the dynamics of your condition. Laboratory study of the hemostasis system To prevent thrombotic complications during pregnancy, in some cases, doctors may recommend that some pregnant patients undergo a laboratory study with an assessment of the blood coagulation system - Coagulogram with indicators of coagulation factors such as 2-4 : Show your doctor a list of all the drugs you have taken regularly over the past two months. This information is very important! It is necessary to find out in advance whether your relatives had any diseases associated with increased blood clotting and the formation of blood clots in the venous system, as well as diseases of the kidneys and the cardiovascular system. If you track fitness activity, you can provide this data to your healthcare provider. Tips for pregnant women During pregnancy, if there are no contraindications, it is worth maintaining a fairly active lifestyle if possible. +375 17 355 94 50 (Hor. 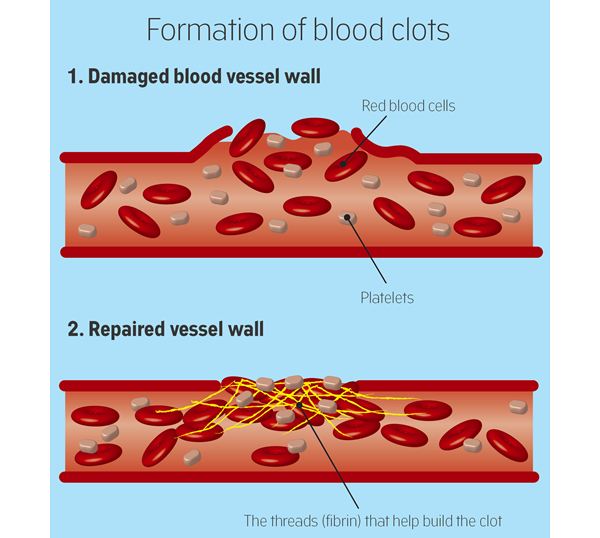 )
) +375 29 238 00 90 (mobile MTS) +375 44 550 00 90 (mobile A1) You are here:

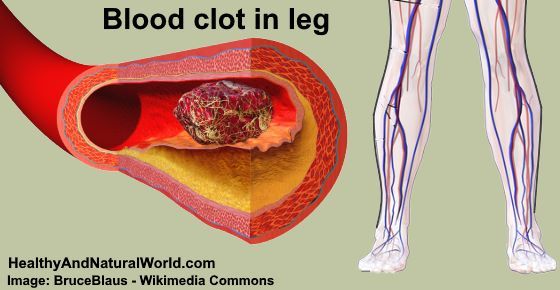 For carriers of inherited thrombophilia with recurrent adverse pregnancy outcomes, two prophylactic treatment options deserve attention: administration of low molecular weight heparin (enoxaparin) to women with recurrent late fetal loss and folic acid treatment for severe toxicosis of the 2nd half of pregnancy.
For carriers of inherited thrombophilia with recurrent adverse pregnancy outcomes, two prophylactic treatment options deserve attention: administration of low molecular weight heparin (enoxaparin) to women with recurrent late fetal loss and folic acid treatment for severe toxicosis of the 2nd half of pregnancy. 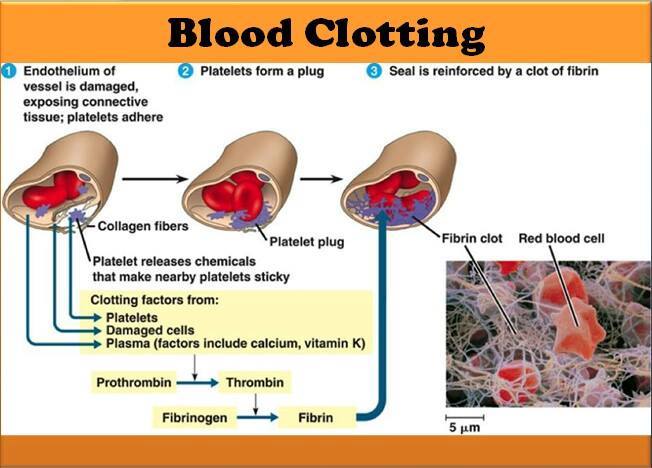 Prolonged, prolonged labor, caesarean section also predispose to complications. The group of very high risk for the development of thrombosis, including in the postpartum period, includes women with varicose veins of the lower extremities.
Prolonged, prolonged labor, caesarean section also predispose to complications. The group of very high risk for the development of thrombosis, including in the postpartum period, includes women with varicose veins of the lower extremities. 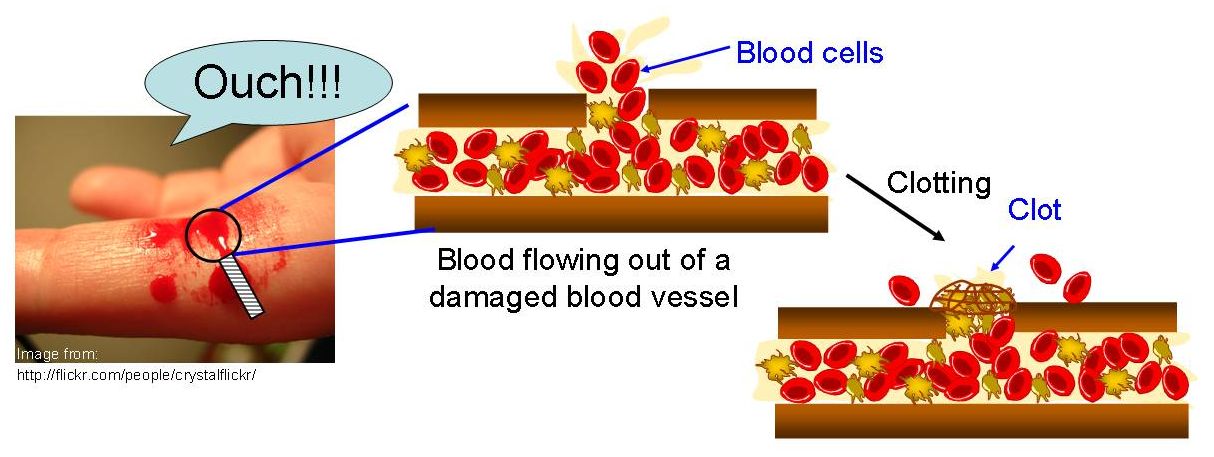
 If a woman has previously given birth three or more times or has multiple pregnancies (twins or more), the risk of thrombosis also increases. Additional risk factors for blood clots are: hypertension, cardiovascular disease and diabetes; use of oral contraceptives before pregnancy; dehydration.
If a woman has previously given birth three or more times or has multiple pregnancies (twins or more), the risk of thrombosis also increases. Additional risk factors for blood clots are: hypertension, cardiovascular disease and diabetes; use of oral contraceptives before pregnancy; dehydration. 

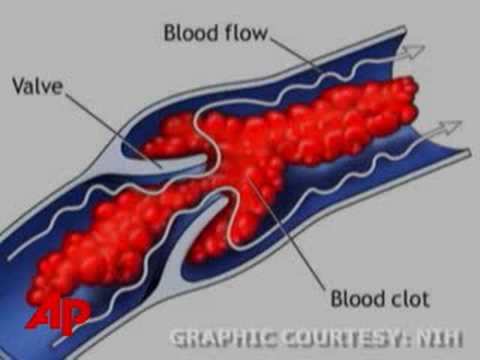
Risk of thrombosis during pregnancy