Help milk come in
What to Do, Causes, Treatments
Many expecting parents dream of the moment they’ll first cradle their little one in their arms and start providing for their most basic needs.
For some breastfeeding moms, this expectation may become a source of worry and anxiety if their milk supply doesn’t come in shortly after delivery.
First, take a deep breath. Your baby will be nourished and you’ll be OK. Whatever you’re providing your newborn with right now — be it a few drops of colostrum with formula supplementation or formula alone — your baby is benefiting.
If your milk volume doesn’t seem to be increasing 3 to 5 days after delivery, you may even be tempted to stop trying to breastfeed because you’re worried about your baby having enough food.
But before throwing in the towel on your milk supply or feeling like a failure, take a moment to keep reading — there are things you can do that may help. (And you’re not a failure, period.)
You may feel very alone and like you’ve done something wrong if you find that your breast milk hasn’t come in shortly after birth. But be gentle with yourself — you haven’t done anything wrong. You’re certainly not alone, and there’s a good chance more milk is on its way by in the next week or two.
There are plenty of reasons for a delay. Your breast milk supply may take a little longer to come in or increase if:
- It was a premature birth — particularly if your baby needed to be separated from you right after the birth.
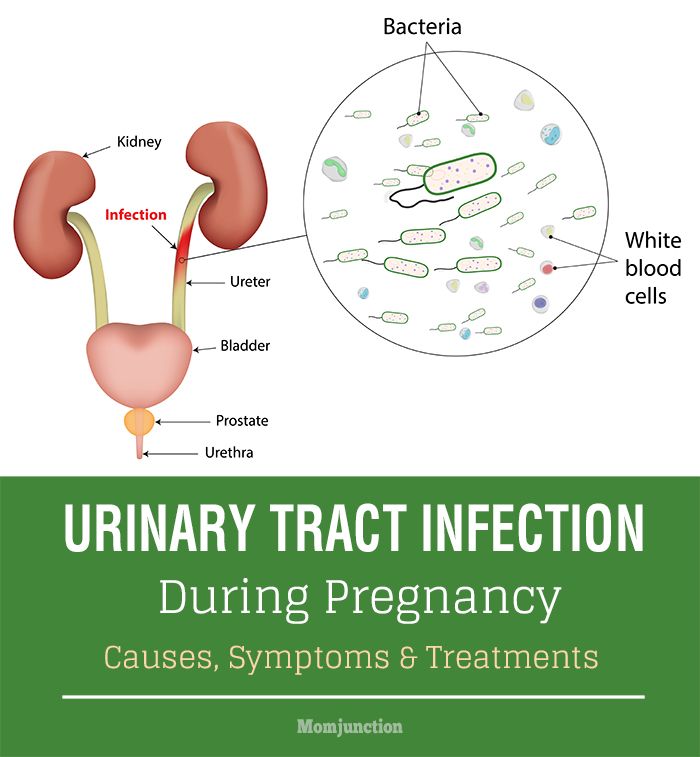
- You have a medical condition like diabetes or polycystic ovary syndrome (PCOS).
- You have obesity.
- You had/have an infection or illness that includes a fever.
- You had a cesarean delivery.
- Your pregnancy included a prolonged bed rest.
- You have a thyroid condition.
- You had a traumatic birth or a postpartum hemorrhage.
- You were unable to breastfeed in the first few hours after giving birth.
Because breast milk production is tied to demand (meaning, removal of milk from your breast), it’s important to make sure that you’re stimulating your breasts frequently and getting out as much milk and colostrum as possible.
Even if you’re making sure to drain your breasts frequently, there are many unique variables that can impact when your milk supply begins to increase.
It’s important to give yourself grace and take measures to encourage a strong supply whenever it does begin to change from colostrum to more mature milk. (See a little lower for some hints to help you with this!)
While it can be extremely frustrating waiting for your breast milk to increase, know that there’s still time for it to happen.
By consistently stimulating your breasts — either with a breast pump or manually — and offering your baby the opportunity to breastfeed, you’ll protect your milk supply and encourage your milk volume to increase sooner rather than later.
Getting help from a professional right away if your milk is coming along a little slower is important to ensure that you establish a healthy milk supply.
There are many things you can do to encourage a greater milk supply both at the hospital and when you’re at home:
Massage your breast area as well as pump or hand express milk
Stimulation of the breast can help in the creation of important milk receptor sites and increase the amount of milk you’re producing. It’s important to spend time engaging and massaging your breasts.
It’s important to spend time engaging and massaging your breasts.
Use a hospital grade pump
These types of pumps have extra suction that can make a big difference not only in the amount of milk that you’re able to extract from your breasts, but also the amount of stimulation your breasts feel. This can lead to a significant increase in the amount of future breast milk you’re able to produce.
Related: The 10 best breast pumps — and how to choose one
Express milk frequently — even if only a small amount comes out!
You should breastfeed, pump, or hand express every 2 to 3 hours in the beginning. Remember that your milk supply is based around supply and demand. It’s essential that you try to drain milk from your breast frequently, so that your body knows it should produce more for your baby.
Especially if your little one is separated from you for any reason, it’s important to use a good hospital grade pump to stimulate and drain milk/colostrum from your breasts.
Hospital staff and lactation consultants can work with you to develop a pumping and feeding plan that will encourage your milk volume to increase.
Use a heating pad or take a warm shower before expressing milk
Heat and massage are great ways to encourage your breast to let down more milk.
Listen to relaxing music
Hearing soothing tunes will help relax you and get the hormones flowing that you need to let down milk. If you’re pumping, looking at pictures of your baby may help as well.
Drink lots of water and get as much sleep as possible
Breast milk includes a lot of water, so just by increasing your water intake you may be able to increase the amount of breast milk you produce.
Many women find that they produce more milk after sleeping, since it offers their bodies a chance to relax and get the right milk-producing hormones flowing.
Bonus points for eating lots of healthy food, since you’ll also produce less breast milk if you get sick.
It may seem like the whole world is weighing on your shoulders as you wait for your milk volume to increase, but there are many ways to make sure that your baby stays healthy and fed.
If your premature baby isn’t putting back on weight after delivery or otherwise needs milk for some reason, don’t worry. Medical staff will feed your little one as much breast milk as you are able to produce and supplement with formula as needed.
Although you may be unhappy with the colostrum or small amount of breast milk you feel you have to offer after a pumping session, your baby will benefit from it! No amount is too little to share with your little one, and any milk that comes from you is specially formatted by nature for your baby.
Using formula for a brief window while your milk increases doesn’t mean that you’ll be unable to breastfeed your baby in the future. If you’re uncomfortable feeding your baby formula, you can speak to your doctor about using donor’s milk. This is milk from people who have produced more than their babies need. It’s screened and stored in milk banks.
It’s screened and stored in milk banks.
Your doctor or lactation consultant will be able to direct you to a local milk bank if you need donor’s milk.
Your baby may not be getting enough to eat if:
- They appear dehydrated (soft spot or eyes sunken in, skin losing elasticity).
- They have fewer wet and dirty diapers. Your baby should be having at least 6 to 8 wet diapers a day after their fifth day of life.
- They cry throughout and following feeds (e.g., no signs of happy milk-drunk baby).
- They’re not back to birth weight by 14 days of life. After an initial decrease in weight right after birth, your baby should be steadily gaining weight.
- They become lethargic or unresponsive.
If you notice signs that your baby isn’t getting sufficient milk, contact your pediatrician as soon as possible. They can determine if there are any other problems and work with you to ensure that your child stays healthy.
It can be both empowering and intimidating to think that breast milk is all your baby needs to stay nourished.
Especially if your breasts aren’t feeling engorged and your milk volume doesn’t seem to be increasing in the first few days after delivery, you may be worried that you’ll never be able to keep your baby full and that you’re somehow inadequate as a parent.
So listen: This is not true! (Read that again.) Remember that there are many reasons why your milk may be a little delayed. Work with a lactation consultant or your doctors and nurses to maximize the amount of milk you produce and ensure good, long breast milk producing potential. A rough start doesn’t have to mean the end to your breastfeeding expectations.
And in the event that your milk doesn’t come in at all due to a medical condition, don’t blame yourself. Your baby will be just fine, and you’re still doing a great job. Fed is best.
13 Ways To Help Milk Come In Faster After Birth — Milkology®
The first few days postpartum are SO overwhelming (and sometimes scary!)
You’re in charge of a new little human that you only just met, you’re surviving on little-to-no sleep, and you’re waiting (not so patiently) for your milk to come in.
Your milk “coming in” is actually not a great term, because (to get technical) you’ve actually been producing milk since the 2nd trimester of pregnancy!
Remember: you’ve got colostrum ready to go.
It’s just that colostrum comes out slowly and in small amounts. But you’ve gotta trust your body… your baby’s tummy is tiny and the colostrum is specifically made by your body to be the perfect food for newborns to tie them over until your milk transitions.
Your milk “coming in” is actually when colostrum transitions from a thicker, yellow fluid to a more voluminous, whiter, “mature” milk.
MOST women’s breast milk will transition from colostrum to mature milk about 2-5 days after birth. For some women, it can take even longer.
You might be thinking… “Is there anything I can DO to speed up the process?!”
Yes… yes, there is! Here are a few helpful tips on how to make your milk come in faster…
(this post may contain affiliate links)
How To Help Milk Come In Faster After Birth1. Try to take advantage of the golden hour.
Try to take advantage of the golden hour.The golden hour is the first hour after birth when your baby is awake, alert, and usually ready to latch. If possible, try to latch your baby as soon as possible.
Even if you’ve had a c-section, you can request to breastfeed in the recovery room. Babies usually get tired a couple hours after birth… so attempting to breastfeed early on is a great idea!
2. Skin-to-skin for the winYour baby CRAVES to be skin to skin with you and absolutely looooves it! It’s the most natural place for them to be and most closely mimics what it was like in the womb. (warm, comfy, hearing your heartbeat)
Skin-to-skin enables your baby to breastfeed more often because they’re close to the breast and can smell your milk. Plus, skin-to-skin boosts the milk-making hormones and reduces newborn crying.
The more you can be skin-to-skin with your baby after birth, the better! It speeds up your milk to come in because you’ll naturally breastfeed more often. (the key to speeding up the process!)
(the key to speeding up the process!)
Rooming in the same room with your baby in the hospital will ensure you’re breastfeeding on demand through the day, and night, and so you never miss a moment to respond to their hunger cues. Speaking of hunger cues…
4.
Recognize Hunger CuesBreastfeed on demand and respond to your baby’s hunger cues before they get too fussy.
Don’t worry about breastfeeding too much. (that’s not a thing!) Remember this: you can’t overfeed a breastfed baby, but you can UNDERFEED them.
5. Nurse On Demand Around the ClockA baby that nurses frequently will often bring in mom’s milk faster. The more you breastfeed, the more your breasts will produce… simple supply and demand!
Your newborn will need to feed every 2-3 hours around the clock… this translates to about 8-12 nursing sessions every 24 hours. And breastfeed every time they display a hunger cue… even if you just nursed them an hour ago!
And breastfeed every time they display a hunger cue… even if you just nursed them an hour ago!
If you and the baby are separated or baby isn’t latching well, you can hand express or pump to stimulate the breasts, get colostrum out, and help milk to come in. (note: hand expressing is more effective for colostrum removal than pumping) Learn it!
6. Hand ExpressThe more milk you remove, the more milk you’ll make. Hand expressing your colostrum can help speed up your milk coming in. And whatever colostrum you get out you can feed to your baby with a syringe.
Video on how to hand express
7. Breast MassageYou can incorporate breast massage and compressions while your newborn is nursing to ensure you get a lot of colostrum out.
Or you can use THIS handy little tool which uses vibration to encourage milk removal.
8. Expect a fussy baby
Like we said earlier, babies usually get sleep a couple hours after birth. But it seems like on day 2 (curing the night specifically), babies usually WAKE UP and the only thing that makes them happy is breastfeeding and cluster feeding. This is normal, and expected. Your baby will want to be nursing a ton and that’s actually a good thing! It’ll help signal your body to ramp up milk production and help your colostrum transition to mature milk faster. Days 3 and 4 postpartum might be a fussy time for them too. Put them to the breast whenever they display a hunger cue. Just keep feeding, your mature milk is on the way!
But it seems like on day 2 (curing the night specifically), babies usually WAKE UP and the only thing that makes them happy is breastfeeding and cluster feeding. This is normal, and expected. Your baby will want to be nursing a ton and that’s actually a good thing! It’ll help signal your body to ramp up milk production and help your colostrum transition to mature milk faster. Days 3 and 4 postpartum might be a fussy time for them too. Put them to the breast whenever they display a hunger cue. Just keep feeding, your mature milk is on the way!
9. Wake your baby to feed if necessary
If your baby is sleeping through nursing sessions, you may need to wake them up. (especially if you had a medicated birth) You never want a newborn to go more than 3 hours without a feeding.
Related article: Baby Sleeping While Breastfeeding? 27 Ways To Keep Them Awake!
 Stay Hydrated
Stay HydratedWhile drinking extra fluids won’t increase your milk supply, being hydrated WILL decrease it. So you want to make sure you stay hydrated. Keep a water bottle nearby and drink whenever you think of it.
My midwife actually recommended drinking THIS after birth because it helps replace lost electrolytes during delivery.
11. Eat WellDid you know breastfeeding moms require an extra 500 calories per day? Making milk is hard work!
Make sure you don’t deprive yourself, especially as you’re recovering from birth. Eat a well-rounded diet and focus on fresh fruits, vegetables, and whole grains.
Also, a lactation cookie can’t hurt!
Lactation cookies contain galactagogues (foods that help milk supply). One of my favorite tips for pregnant mamas is to make and freeze some lactation cookies for postpartum. I encourage moms to bring some with them to the delivery room. Lactation cookies a great way to ensure you’re getting that extra 500 calories in a day and they’re easy to eat, one-handed snacks!
This is my favorite way to make lactation cookies ahead of time because you simply add butter, 2 eggs, and then bake!…
Buy on Amazon
12.
 Avoid Pacifiers
Avoid Pacifiers Although you might choose to use a pacifier later on, try to delay giving it to baby until you’re milk is well-established (about 4 weeks postpartum).
Your baby has a natural desire to suck and any suckling they do away from the breast is a missed chance for breast stimulation (and bringing your milk in faster!).
13. Connect with an IBCLC
IBCLCs (International Board Certified Lactation Consultants) are the best of the best for troubleshooting and support.
Most hospitals have them on staff so ask to see one when you’re in the recovery room. Ask them any questions you have and be sure to have them observe you and your baby breastfeeding to make sure baby is breastfeeding well
What triggers breast milk to come in?
After birth, when the placenta separates from the uterus, there will be a sharp drop in the hormone progesterone. This triggers the breast to ramp up milk production.
So no matter if you have a vaginal birth or a tummy birth (c-section), rest assured your milk WILL come in! (it’s just a matter of when)
Things that may delay your breast milk to come in after birth:A lot of bleeding after birth
Infection or illness with fever
Previous breast surgery
Strict or prolonged bed rest during pregnancy
Having a c-section or a traumatic birth experience like a long labor or a lot of interventions
Being a first time mom. Studies show 1st time moms often have a slight delay in milk production.
Certain medical conditions (diabetes, thyroid conditions, pre-eclampsia)
Stress
A high BMI (above 26-30)
Having any retained placenta fragments (your progesterone levels won’t drop to trigger milk production)
Being separated from baby or baby having a poor start to breastfeeding (remember: the more milk you remove, the more milk you’ll make… so you’ll need to get hand expressing or pumping to stimulate your breasts as soon as possible)
Try not to stress! Continue to breastfeed/hand express/pump as necessary and keep removing milk. Reach out to your healthcare provider if you have any concerns or if your baby isn’t having enough wet/dirty diapers.
Reach out to your healthcare provider if you have any concerns or if your baby isn’t having enough wet/dirty diapers.
Our 3
Fav breastfeeding products⭐1. To get more milk out. Frida Mom’s Lactation Massager is a cool little gadget that helps baby get more milk out during nursing and helps you express more milk when pumping.
⭐2. To boost supply and tone up postpartum. The protein powder Milk Dust is specially made to nourish and tone postpartum bodies (and contains milk boosting ingredients too!) Get 10% off Milk Dust using the code MILKOLOGY at checkout
⭐3. To soothe your nips. This nipple balm. (seriously, it’s the best).
Related Post:
35 Veteran Breastfeeders Give Their Best Advice To Newbies
BreastfeedingStacey Stewart
Breast milk production | Baby's needs
Did you know that the amount of breast milk adapts to your baby's needs? In this article, you will learn amazing facts about breast milk production in the first days, weeks and months.
Share this information
Your body is capable of producing breast milk for your baby at every stage of development. Understanding how milk production “turns on”, what happens to milk when you feed your baby, and why production adjusts to his needs as he grows, will help you start this amazing process in the right way.
Day one: milk production at birth
The baby is usually ready to breastfeed from birth. When he grabs the breast and begins to suck rhythmically, the milk-producing cells “turn on” and the formation of the first breast milk, colostrum, starts. 1 Try to feed your baby as much as possible in the first hour of his life, and then as soon as he shows interest in feeding. This will help lay the foundation for good milk production later on. 2
The first days: the arrival of milk
At this stage, your body's level of progesterone, the
pregnancy hormone, which begins to fall after the placenta comes out, is reduced, and the hormones responsible for milk production - prolactin, insulin and hydrocortisone - are included in the work. These hormones will help start milk production. 3 Around the third day of your baby's life, milk will begin to come in and you will feel that your breasts have filled up and become noticeably firmer. 1
These hormones will help start milk production. 3 Around the third day of your baby's life, milk will begin to come in and you will feel that your breasts have filled up and become noticeably firmer. 1
First month: shaping milk production
During the first weeks, your body will be especially sensitive to the amount of milk produced as it learns to produce the right amount. Prolactin levels increase dramatically each time you empty your breasts, thereby helping shape the lactation process. It also contributes to the maturation of your milk in terms of composition. At this stage, transitional milk is produced and the amount continues to grow. 3.4
For good long-term milk production, it is very important that you are close to your baby during the first few weeks. The more often you breastfeed, the more milk will be produced. This process resembles the law of supply and demand. Each time after emptying the breast, whether it is feeding the baby or pumping, even more milk will be produced.
Remember that it is normal for newborns to eat frequently, perhaps even every 45 minutes, and this does not mean that they are not getting enough milk. Frequent feedings help shape milk production, so feed your baby on demand, not on a schedule.
“In the first few weeks you may feel like you don’t have enough milk because your baby will be feeding all the time, but that’s okay,” says UK mom-of-two Jo, “We tend to think that the baby wants to eat every few hours, but that is not necessarily the case."
Don't forget that babies also breastfeed for comfort. Breastfeeding helps them calm down and adjust to their new life outside the womb. In addition, feeding helps to establish a connection between you.
Stable milk production in the first month
If you follow your baby's needs and feed him as often and for as long as he wants, milk production should adjust. 5
Some mothers try to increase the period between feedings so that the breasts can produce more milk during this time, but this should not be done, as this may have the opposite effect. 2
2
If you are unable to breastfeed directly for the first two weeks, express your milk to build and maintain your milk supply during this critical period and beyond.
Did you know that feeding your baby extra formula unnecessarily can reduce your milk production? The chest will not receive a signal to increase production, because it will not be emptied. In addition, if the baby sleeps longer after formula, he may miss his usual next feeding time.
This is a kind of “supplementing trap”. After three to four days of formula supplementation, during which the breasts have emptied less, the body will receive a signal that breastfeeding has stopped, and the amount of milk produced will begin to decrease. As a result, the baby will remain hungry and will need additional formula supplementation. And so on in a circle ... As a result, this will lead to really low milk production, and the baby will eat mainly the mixture.
Breast milk production after six weeks
After a month of breastfeeding, post-feeding bursts of prolactin secretion begin to decrease, milk matures, and the body gets used to producing as much milk as your baby needs. In fact, the chest begins to work "on autopilot." 4 You may also notice at this time that your breasts are softer and your milk flow has stopped.
In fact, the chest begins to work "on autopilot." 4 You may also notice at this time that your breasts are softer and your milk flow has stopped.
At this stage, women often have fears of "losing milk".
However, this only means that milk production has been established and now fully meets the needs of the child. It is noteworthy that although the baby continues to grow, he will consume approximately the same amount of milk both at six weeks and at six months. You may notice that the baby began to suckle the breast longer, but less often. On some days he may eat a little less than usual - his appetite changes in the same way as an adult.
Now your body will produce exactly the amount of milk,
as much as your baby needs. Therefore, the more milk the baby
drinks (or you express), the more it will produce.
How does this happen? The reason for this is thought to be the so-called "feedback lactation inhibitor" that controls milk production. The more milk in the breast, 2 the higher the inhibitor level, so a full breast produces less milk than one that has been emptied.
The more milk in the breast, 2 the higher the inhibitor level, so a full breast produces less milk than one that has been emptied.
What is the rate of milk production?
Mothers often worry about their milk supply and think about how to increase it. However, if the baby is healthy and growing well, problems usually do not arise.
“I was worried that my newborn daughter was not getting enough milk as she was feeding very quickly and always from one breast even though I offered both,” says Marjorie, mother of two in the UK, “But when I pumped from using a breast pump, I was surprised at how much milk I produced, and calmed down. I just had to keep feeding her little and often.”
Keep in mind, however, that not all mothers are able to express a lot of milk right away. You can also try hand expressing milk and see if there is a change in breast fullness.
If you're worried about your milk supply, read our tips for symptoms of too little or too much milk.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet Gynecol Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". F Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
3 Ostrom KM. A review of the hormone prolactin during lactation. Prog Food Nutr Sci . 1990;14(1):1-43. - Ostrom KM, "Review of the role of the hormone prolactin during lactation." Prog Food Nutr Sai. 1990;14(1):1-43.
1990;14(1):1-43. - Ostrom KM, "Review of the role of the hormone prolactin during lactation." Prog Food Nutr Sai. 1990;14(1):1-43.
4 Cox DB et al. Blood and milk prolactin and the rate of milk synthesis in women. Exp Physiol. 1996;81(6):1007-1020. - Cox D.B. et al., Effects of blood and milk prolactin on milk production in women. Exp Physiol. 1996;81(6):1007-1020.
5 Kent JC et al. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-95. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3): e 387-95.
Transitional milk | Stages of breast milk production
During the first couple of weeks after birth, the composition of breast milk changes dramatically. Learn about the amazing properties of this transitional milk.
Share this information
A newborn changes literally every day, and the same can be said about breast milk. With the advent of milk, the breast can increase to an impressive size, and changes occur not only on the outside, but also inside. During the first week, the milk-producing cells and the connections between them are rebuilt and prepare the breast for the upcoming feeding. 1 From now until about the end of the second week, they will produce what is called transitional milk. 2
“After the placenta is delivered, levels of progesterone, the pregnancy hormone, begin to decline rapidly,” explains Professor Peter Hartmann of the University of Western Australia, a leading authority on the composition of breast milk. “As progesterone levels decrease, milk synthesis increases and the composition is approaching the norm, although a couple more weeks are needed for the full maturation of the milk.
Breastmilk Stages: An Intermediate Phase
If colostrum is your baby's very first food and mature milk is his main food for a long time, then transitional milk is a kind of bridge between them.
They should be considered as three different stages of milk production, not three types of milk. The main components remain unchanged throughout breastfeeding, only their quantity changes depending on the circumstances. During the transition period, the composition of milk undergoes the most significant changes, and this happens every day in accordance with the changing needs of the child.
Milk changes because it contains bioactive components, including cells, hormones and beneficial bacteria. The transition to mature milk does not happen all at once: the composition changes gradually and in strict accordance with the developmental needs of the baby. 3.4
“The amount of milk produced by the mother has a major influence on the composition of milk,” says Professor Hartman. “The composition of milk at low and higher levels of production is different.”
“The composition of milk at low and higher levels of production is different.”
Transitional milk: increase in quantity
As the baby grows, it needs more food and a different ratio of nutrients. The amount of milk produced during this period also increases significantly. You can produce 600-700 ml per day, 5 which is a very impressive amount compared to the small amount of colostrum that was produced in the early days.
"The composition of milk in all mammals varies according to the needs of the young"
Your breasts are now in “boosting” mode: your body is learning to produce the amount of milk your baby needs. The breast becomes more mature, as does the milk. Compared to colostrum, transitional milk contains more fat and lactose, a natural sugar that gives your baby energy. 2
“The level of lactose rises sharply in the first two or three days after birth,” says Prof. Hartmann, “The composition of fats also changes: the content of medium-chain fatty acids C10 and C12 increases. They are an easily digestible source of energy and have antiviral properties. In addition, sodium and chloride levels are greatly reduced during this period, so that the milk has a very low salt content.”
They are an easily digestible source of energy and have antiviral properties. In addition, sodium and chloride levels are greatly reduced during this period, so that the milk has a very low salt content.”
Protein: the right ratio
The protein content of breast milk does not stay the same either. There are two types of proteins in human milk: casein and whey. Under the influence of acid in the child's stomach, casein turns into a solid mass (cottage cheese) and gives a feeling of satiety for a longer time. It also has antimicrobial properties. Whey, on the other hand, is rich in antibodies and remains liquid, so it is easily absorbed, which is especially important for newborns. As the child's gastrointestinal tract strengthens, the ratio of casein to whey in milk gradually changes. If in colostrum it is about 90:10, then after a month it reaches 60:40, and after a year of breastfeeding, the balance is set at 50:50. 6
This ratio of proteins is ideal for humans, as our body grows relatively slowly and the brain is constantly growing and becoming more complex.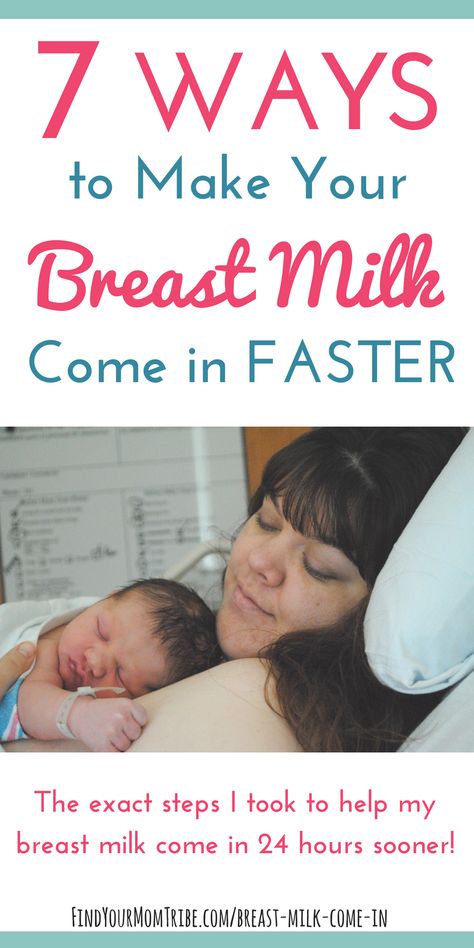 In addition, it promotes the supply of all the essential amino acids that a child needs for the healthy development of the brain, eyes and other organs.
In addition, it promotes the supply of all the essential amino acids that a child needs for the healthy development of the brain, eyes and other organs.
The amount of whey protein in human milk is significantly higher than that of other mammals. In cow's milk, the ratio of whey and casein is the opposite: 20:80 (therefore, it is not suitable for feeding children under one year old). 7
“Milk is designed to perform a specific task,” continues Professor Hartmann, “Some components are present in all milk, such as proteins and fats, but if you look at which proteins and which fats, it becomes clear which animal belongs to milk. The composition of milk in all mammals varies depending on the needs of the young.
Changing the protective properties of transitional milk
Although your baby is still very young, already in the first couple of weeks he begins to develop his own immune system, and now he needs your direct protection a little less.
The concentration of protective enzymes and antibodies in breast milk changes accordingly.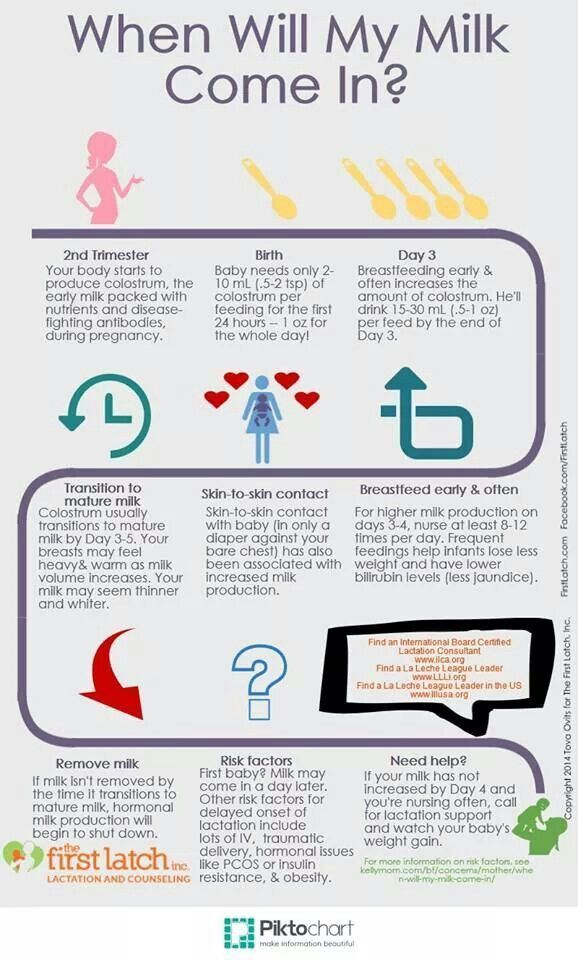 The content of some substances, in particular lactoferrin (protective enzyme) and secretory immunoglobulin A (antibody), decreases, while other substances, such as the antibacterial enzyme lysozyme, on the contrary, increase. 8
The content of some substances, in particular lactoferrin (protective enzyme) and secretory immunoglobulin A (antibody), decreases, while other substances, such as the antibacterial enzyme lysozyme, on the contrary, increase. 8
“The protein content of milk decreases around the same time,” says Prof. Hartmann, “The synthesis of protective proteins occurs at the same rate, but they are more diluted due to increased milk production.”
The concentration of minerals such as zinc, copper and magnesium, which support the development of the child's immune system, also decreases as the immune system strengthens. 9
When breast milk becomes fully mature
During the transition period, the composition of breast milk changes significantly. By the end of the first month, it becomes fully mature. This means that the child will be able to eat them further as they grow. The composition of milk will no longer change much, no matter how long you continue breastfeeding - a few months, a year or more.
Would you like to know more? Read our free e-book Surprising Breast Milk Facts or article on mature milk.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." F Mammary Gland Biol Neoplasia. 2007;12(4):211-221. 2 Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am . 2013;60(1):49-74. - Ballard O., Morrow A.L., "Composition of breast milk: nutrients and biologically active factors." Pediatrician Clean North Am. 2013;60(1):49-74. 3 Munblit D et al. 4 Pons SM et al. Triacylglycerol composition in colostrum, transitional and mature human milk. Eur J Clin Nutr . 2000;54(12):878-882. — Pons SM, "Triacylglycerol in colostrum, transitional and mature human milk". Yur J Klin Nutr. 2000;54(12):878-882. 5 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation. Am J Clin Nutr . 1988;48(6):1375-1386. 6 Kunz C, Lönnerdal B. Re-evaluation of the whey protein/casein ratio of human milk. Acta Paediatr. 1992;81(2):107-112. Kunz S, Lonnerdal W. Act Pediatr.1992;81(2):107-112. - Kuntz S., Lönnerdahl B., "New Evaluation of Whey Protein/Casein in Breast Milk". Akta Pediatr. 1992;81(2):107-112. 7 Martin CR et al. Review of infant feeding: key features of breast milk and infant formula. Nutrients. 2016;8(5). - Martin S.R. et al., Review of Infant Feeding Issues: Key Features of Breast Milk and Infant Formula. Nutrients. 2016;8(5). 8 Lönnerdal B et al. Longitudinal evolution of true protein, amino acids and bioactive proteins in breast milk: a developmental perspective. Colostrum and mature human milk of women from London, Moscow, and Verona: determinants of immune composition. Nutrients. 2016; 8(11): 695. - Moonblit, D. et al., "Colostrum and mature breast milk from women in London, Moscow, and Verona: major factors in immune composition." Nutrients. 2016; 8(11): 695.
Colostrum and mature human milk of women from London, Moscow, and Verona: determinants of immune composition. Nutrients. 2016; 8(11): 695. - Moonblit, D. et al., "Colostrum and mature breast milk from women in London, Moscow, and Verona: major factors in immune composition." Nutrients. 2016; 8(11): 695.  - Neville M.S. et al., "Female Lactation Study: Milk Quantity in Lactating Women at the Beginning and Peak of Lactation." Am F Clean Nutr. 1988;48(6):1375-1386.
- Neville M.S. et al., "Female Lactation Study: Milk Quantity in Lactating Women at the Beginning and Peak of Lactation." Am F Clean Nutr. 1988;48(6):1375-1386.