What can cause a yeast infection in pregnancy
Yeast Infections During Pregnancy - American Pregnancy Association
Yeast infections during pregnancy are more common than any other time in a woman’s life, especially during the second trimester of pregnancy. You may be noticing an increase in the amount of thin, white, odd smelling discharge. This is common and a normal symptom in the second trimester.
If you think you may be experiencing a yeast infection, the following information will prepare you to discuss the possibility with your doctor. Though yeast infections have no major negative effect on pregnancy, they are often more difficult to control during pregnancy, causing significant discomfort for you. Don’t wait to seek treatment!
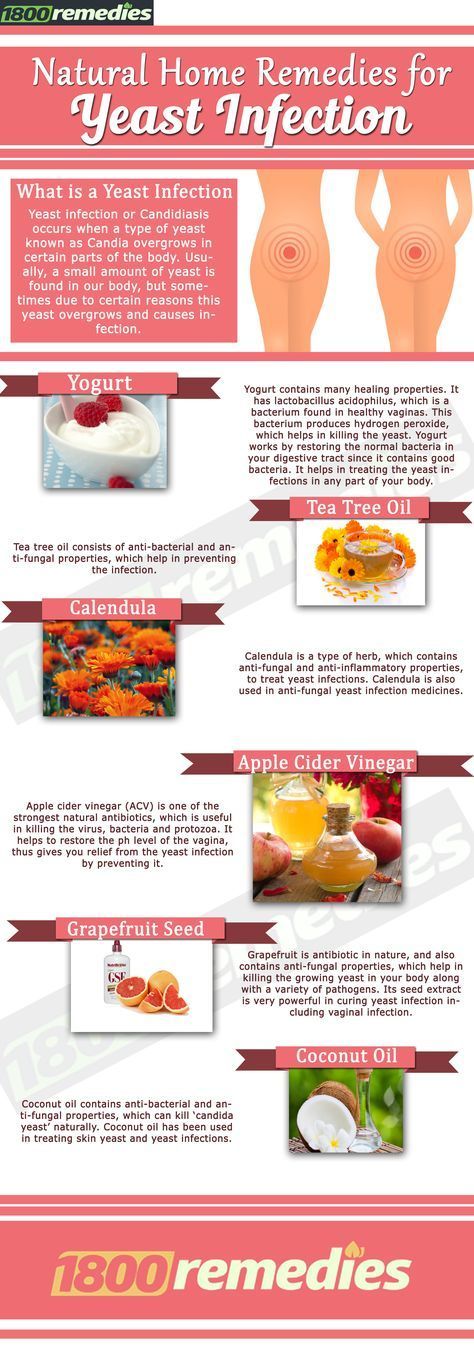
What is a yeast infection?
Yeast infection occurs when the normal levels of acid and yeast in the vagina are out of balance, which allows the yeast to overgrow causing an uncomfortable, but not serious, a condition called a yeast infection.
If you have never been diagnosed or treated by a physician for a yeast infection and have some of the symptoms, you should see your physician first for accurate diagnosis and treatment. Other infections have similar symptoms, so you want to make sure that you are treating the infection correctly. There are also treatments that are not appropriate during pregnancy.
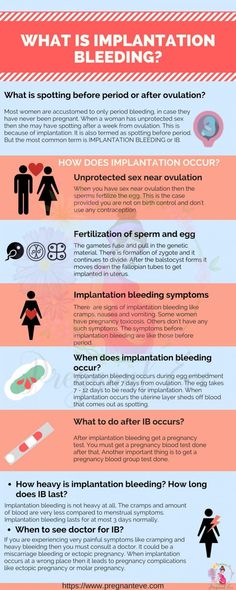
What causes yeast infections during pregnancy?
A yeast infection can be caused by one or more of the following:
- Hormonal changes that come with pregnancy or before your period
- Taking hormones or birth control pills
- Taking antibiotics or steroids
- High blood sugar, as in diabetes
- Vaginal intercourse
- Douching
- Blood or semen
Why are yeast infections more common during pregnancy?
Your body is going through so many changes right now, and it is difficult for your body to keep up with the chemical changes in the vagina. There is more sugar in vaginal secretions on which the yeast can feed, causing an imbalance which results in too much yeast.
What are the symptoms of yeast infections?
The symptoms of a yeast infection may include one or more of the following:
- Discharge that is usually white/tan in color, similar to cottage cheese and may smell like yeast/bread
- Other discharge may be greenish or yellowish, also similar to cottage cheese and may smell like yeast/bread
- An increase in discharge
- Redness, itching, or irritation of the lips of the vagina
- Burning sensation during urination or intercourse
What else could I be experiencing?
If you are experiencing symptoms similar to a yeast infection, but a physician has ruled this diagnosis out, you may have one of the following:
- Sexually Transmitted Diseases (STDs) like Chlamydia, Gonorrhea, & Trichomoniasis
- A vaginal infection called bacterial vaginosis
How do I know for sure if I have a yeast infection?
At your doctor’s office or medical clinic, a clinician will use a simple, painless swab to remove the discharge or vaginal secretions and examine it through a microscope. Usually, upon a simple examination of the vagina, a physician can diagnose a yeast infection. In rare cases, the culture may be sent to a lab.
Usually, upon a simple examination of the vagina, a physician can diagnose a yeast infection. In rare cases, the culture may be sent to a lab.
How are yeast infections treated during pregnancy?
During pregnancy, physicians recommend vaginal creams and suppositories only. The oral medication, Diflucan (a single-dose medication), has not been proven safe during pregnancy and lactation. Not all vaginal creams and suppositories are okay to use during pregnancy, so it is best to consult your doctor or pharmacist to get the right one. If left untreated, yeast infections can pass to your baby’s mouth during delivery. This is called “thrush” and is effectively treated with Nystatin.
It may take 10-14 days to find relief or completely clear up the infection while you are pregnant. After the infection has cleared up and any sores have healed, it may be helpful to use a starch-free drying powder, or Nystatin powder to prevent a recurring infection.
How can I prevent a yeast infection or recurring yeast infections?
Most yeast infections can usually be avoided by doing the following:
- Wear loose, breathable cotton clothing and cotton underwear.
- After regular, thorough washing (using unscented, hypoallergenic or gentle soap), use your blow dryer on a low, cool setting to help dry the outside of your genital area.
- Always wipe from front to back after using the restroom.
- Shower immediately after you swim. Change out of your swimsuit, workout clothes, or other damp clothes as soon as possible.
- Do NOT:
- douche
- use feminine hygiene sprays
- use sanitary pads and tampons that contain deodorant
- take a bubble bath/use scented soaps
- use colored or perfumed toilet paper
- Include yogurt with “lactobacillus acidophilus” in your diet.
- Limit sugar intake, as sugar promotes the growth of yeast.
- Get plenty of rest to make it easier for your body to fight infections.
When should I contact my doctor?
If you are experiencing the symptoms described in this article, call your doctor now. Yeast infections have similar symptoms of other infections, such as STDs.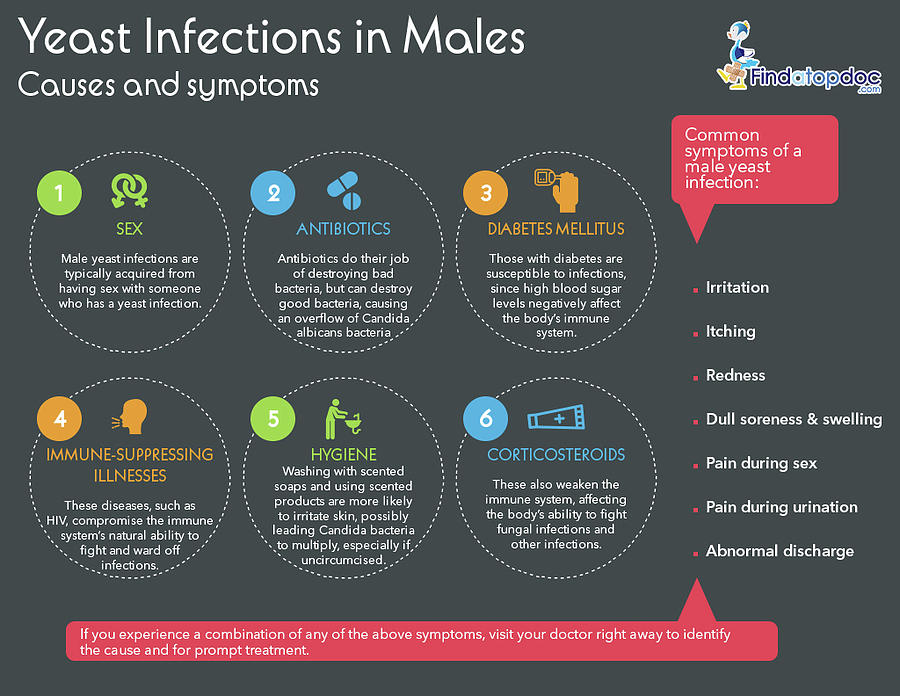 Proper diagnosis every time you experience these symptoms is vital for the most effective, immediate treatment, or your condition may worsen/not go away.
Proper diagnosis every time you experience these symptoms is vital for the most effective, immediate treatment, or your condition may worsen/not go away.
If you see no improvement within three days, or if symptoms worsen or come back after treatment, you should contact your healthcare provider again.
Want to Know More?
- Pregnancy Nutrition
- Medication and Pregnancy
Compiled using information from the following sources:
1. American Academy of Family Physicians
https://familydoctor.org
1. Mayo Clinic Complete Book of Pregnancy & Babys First Year. Johnson, Robert V., M.D., et al, Ch. 11.
Yeast Infections and Pregnancy: Causes, Symptoms & More
What’s a yeast infection?
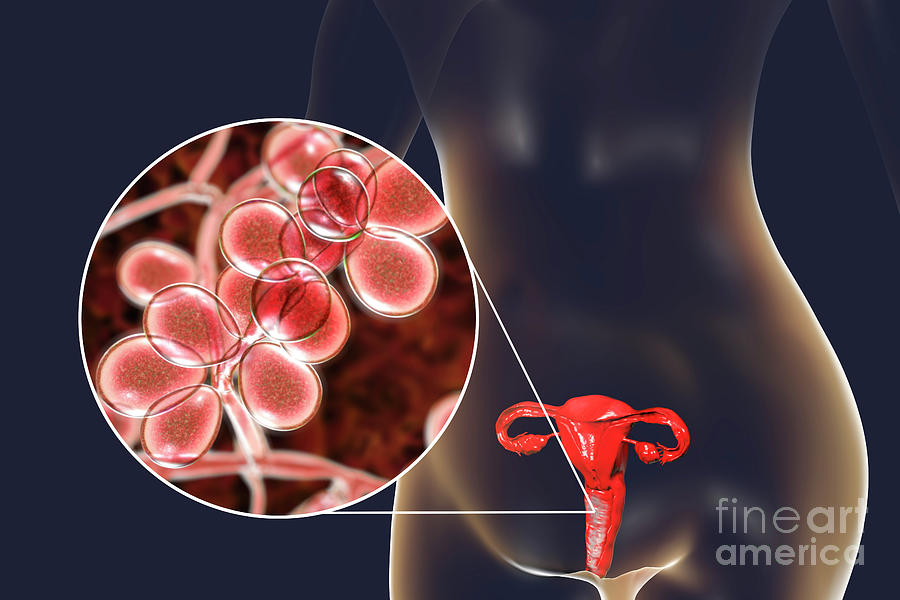
Vulvovaginal candidiasis, or moniliasis, is a yeast infection of the vulva and vagina. Yeast is a type of fungus. The yeast that most often causes these infections is Candida albicans, but other types of yeast — including Candida glabrata and Candida tropicalis — can also be responsible.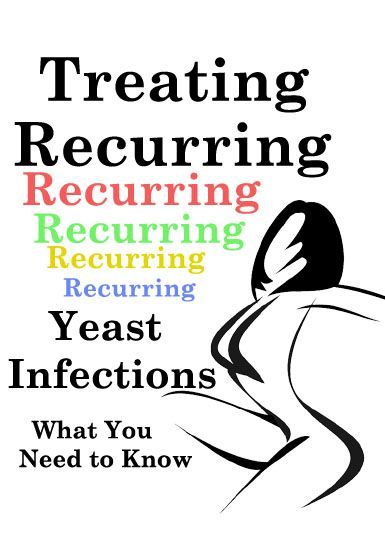
About three out of every four women will have at least one yeast infection in their lifetime, according to American Family Physician. Up to 45 percent will get two or more infections.
During pregnancy, Candida (and the infections it causes) is even more common. According to one study, about 20 percent of women have Candida yeast in their vagina normally. That number goes up to 30 percent during pregnancy. Yeast is more likely to cause infection during pregnancy due to hormone fluctuations.
Because you can pass the yeast to your baby during delivery, it’s important to get treated.
What causes candidiasis?
Candidiasis occurs when the normal number of fungi that reside in the vagina increases enough to cause symptoms. The most common factors that make a woman more likely to get yeast infections include:
- pregnancy
- diabetes
- use of birth control pills, antibiotics, or corticosteroids such as prednisone (Rayos)
- disorders that weaken the immune system, such as HIV
During pregnancy, shifting hormone levels change the pH balance in the vagina.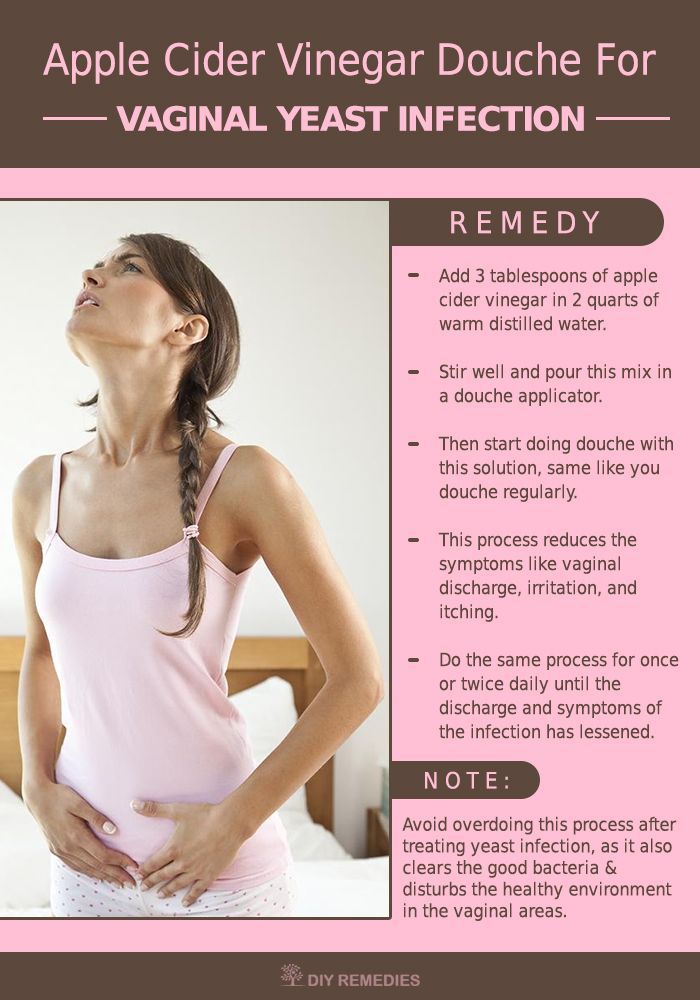 This creates an environment that’s more favorable for yeast to grow.
This creates an environment that’s more favorable for yeast to grow.
What complications are associated with yeast infections?
In nonpregnant women who have a normal immune system, yeast infections rarely lead to serious complications.
Even in pregnancy, yeast infections don’t usually cause harmful effects in the mother. However, you can pass the yeast to your baby during delivery.
Most babies who develop a yeast infection have it just in their mouths or diaper area. However, though rare, a yeast infection in babies can become very serious, because their immune systems aren’t yet well-developed. It can spread through the infant’s body and affect breathing and heart rhythm, for example. This happens most often in babies who have other things affecting their immune systems, such as prematurity or an underlying infection.
Yeast infections can also cause body-wide infections and serious complications in women who have a weakened immune system because of conditions such as HIV.
What are the signs and symptoms of candidiasis?
With candidiasis, you’ll most likely have itching in your vagina and vulva. You may also notice a white vaginal discharge. This discharge may look similar to cottage cheese and shouldn’t have an odor.
Other symptoms include:
- soreness or pain in the vagina or vulva
- burning when you urinate
- a rash on the vulva and the skin around it, which sometimes appears on the groin and thighs as well
These symptoms may last for a few hours, days, or weeks.
In newborn babies and in women who have a weakened immune system, candidiasis may occur in the mouth. This condition is known as thrush.
Other conditions can cause symptoms similar to a yeast infection, including:
- an allergic reaction to a product you’ve used in the vaginal area, such as soap or a condom
- sexually transmitted diseases (STDs) such as chlamydia and gonorrhea
- bacterial vaginosis, a type of infection
How can I prevent a yeast infection?
You can reduce your risk of future yeast infections by:
- keeping the vaginal area dry
- avoiding bubble baths, feminine hygiene sprays, and douches
- wearing cotton underwear
Although candidiasis isn’t an STD, oral sex may make your condition worse and affect your sexual partner.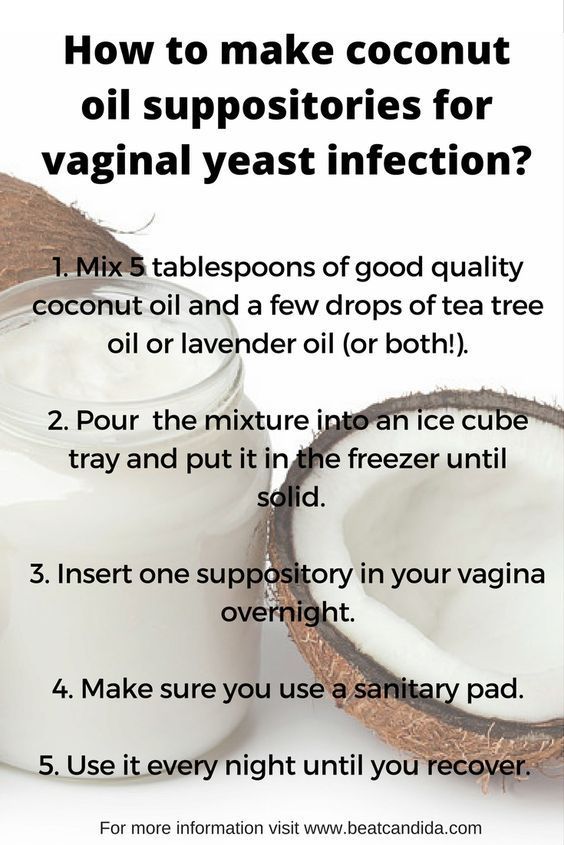
How is candidiasis diagnosed?
Your doctor will ask about your symptoms and do a physical exam. To confirm the diagnosis, your doctor will use a cotton swab to take a sample of the vaginal discharge. The sample will be checked under a microscope for signs of the yeasts that cause infections.
In certain cases, your doctor may want to culture — or grow in a lab — a sample of your vaginal discharge. Cultures help them rule out other types of yeast, such as C. glabrata and C. tropicalis.
How is candidiasis treated?
Most of the time, vulvovaginal candidiasis is easy to treat with an antifungal cream or suppository. The medicine should relieve your symptoms within seven days. However, during pregnancy, you should see your doctor before starting treatment. They can confirm that you actually have a yeast infection and ensure you get a treatment that’s safe to use during pregnancy.
Both oral and topical antifungal drugs are used to treat yeast infections in nonpregnant women. However, oral drugs may not be safe to use during pregnancy. A 2016 study in JAMA found an association between higher risk of miscarriage and oral fluconazole (Diflucan) use during pregnancy. Oral antifungal drugs have also been linked to birth defects.
However, oral drugs may not be safe to use during pregnancy. A 2016 study in JAMA found an association between higher risk of miscarriage and oral fluconazole (Diflucan) use during pregnancy. Oral antifungal drugs have also been linked to birth defects.
Topical antifungal drugs that are safe to use during pregnancy include:
How should repeat yeast infections be treated?
During pregnancy, you’re more likely to have repeated yeast infections. Four or more yeast infections in one year is called recurrent vulvovaginal candidiasis.
If you keep getting yeast infections, talk to your doctor. You may need to be evaluated for risk factors such as diabetes or an immune disorder. If pregnancy is the cause, the infections should stop after you deliver.
Research finds that taking an oral “azole” drug for six months reduces your chance of a repeat infection. However, oral antifungal medicines might not be safe to use during your pregnancy. You may have to wait until after you deliver to go on this treatment.
symptoms, treatment (1st, 2nd, 3rd trimesters)
Did you know that every third woman in the world suffers from candidiasis? At the same time, thrush occurs three times more often in pregnant women. Let's take a look at the causes of thrush together, and also talk about the main symptoms and methods of treating thrush at different stages of pregnancy.
Lyudmila Starichenko
doctor of the highest qualification category,
head doctor of the Clinic of Innovative Technologies
work experience 41 years
learn more on the website
Causes of thrush
Signs and symptoms of thrush in pregnant women
Treatment of thrush in pregnant women
What to avoid when treating thrush?
Why is thrush dangerous during pregnancy?
What if it doesn't go away?
Prevention
Causes of thrush
Thrush or vulvovaginal candidiasis is a common disease of the vaginal mucosa. The main reason for its appearance is a fungal infection.
The main reason for its appearance is a fungal infection.
Pregnant women are at particular risk. After all, in this position, the patient has a natural decrease in immunity, which can even lead to a decrease in local immunity. As a result, the inevitable growth of opportunistic microorganisms occurs. Among them are yeast-like fungi that cause candidiasis. Changes in the hormonal background, namely, an increase in the level of female sex hormones, can also affect the increased growth of yeast-like fungi. This is especially true for patients who have pregnancy complications.
Read more about the causes of candidiasis in our material.
learn more
Signs and symptoms of thrush in pregnancy
The signs and symptoms of thrush in pregnancy are no different from the usual symptoms of thrush. They differ only in what particular organ is affected by thrush.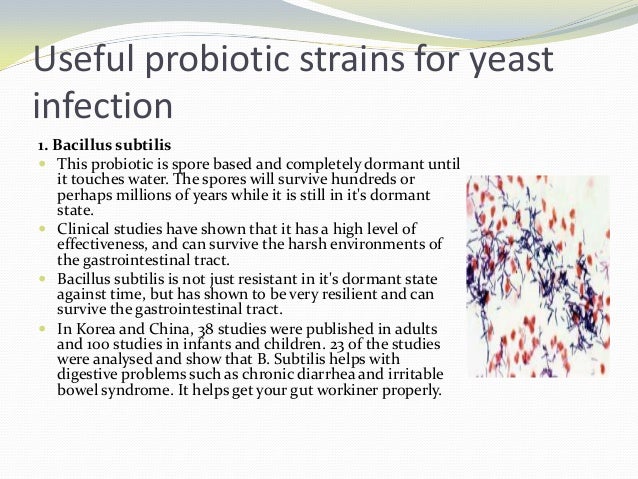
So, for example, with urogenital candidiasis, the most characteristic symptoms are discharge from the genital tract, itching, burning in the genital area and its intensification during sleep and water procedures.
Treatment of thrush in pregnant women
All medications during pregnancy must be selected by a doctor. Self-treatment is out of the question here, because by wrong actions a woman can harm not only herself, but also her child!
As a rule, only local therapy is prescribed during pregnancy at any time.
First trimester
In the first trimester, use Natamycin 100 mg intravaginally for 6 days. The drug refuses fungicidal and antifungal action. Thanks to the active substance, it binds to the sterols of the cell membrane of the fungus and disrupts its permeability. This leads to the destruction of the fungal cell as a result of damage or rupture of the membrane.
Thanks to the active substance, it binds to the sterols of the cell membrane of the fungus and disrupts its permeability. This leads to the destruction of the fungal cell as a result of damage or rupture of the membrane.
Natamycin is active against most yeast-like fungi, and especially against fungi of the genus Candida. The advantage of this drug is that it does not have a systemic effect and is not absorbed into the gastrointestinal tract, acting only locally on the damaged mucous membrane. Of the possible side effects with topical application - only irritation and burning sensation at the site of application.
Second and third trimesters
In the II and III trimester, Sertoconazole 300 mg is used intravaginally once. This drug has a powerful antifungal effect by increasing the permeability of the cell membrane, which leads to the destruction of the cells of the opportunistic fungus. Side effects do not differ from the previous drug. Of the side effects at the site of application of Sertoconazole, itching and burning may occur, which will pass on their own.
Side effects do not differ from the previous drug. Of the side effects at the site of application of Sertoconazole, itching and burning may occur, which will pass on their own.
Followed by Econazole 150 mg intravaginally for 3 days. The drug has a local antifungal and antibacterial effect. It stops the biosynthesis of ergosterol and other sterols that regulate the permeability of the fungal cell wall. With intravaginal administration, patients did not experience pregnancy complications or other undesirable effects of therapy on reproduction. Local reactions are possible: rash, burning, irritation, itching, redness and dryness of the skin.
The last stage of treatment is Clotrimazole 100 mg intravaginally for 6-10 days. The drug belongs to a broad spectrum antifungal agent. It is applied topically only by the intravaginal method. Clotrimazole inhibits the growth and division of microorganisms.
The mechanism of action of the drug is associated with a change in the permeability of cell membranes.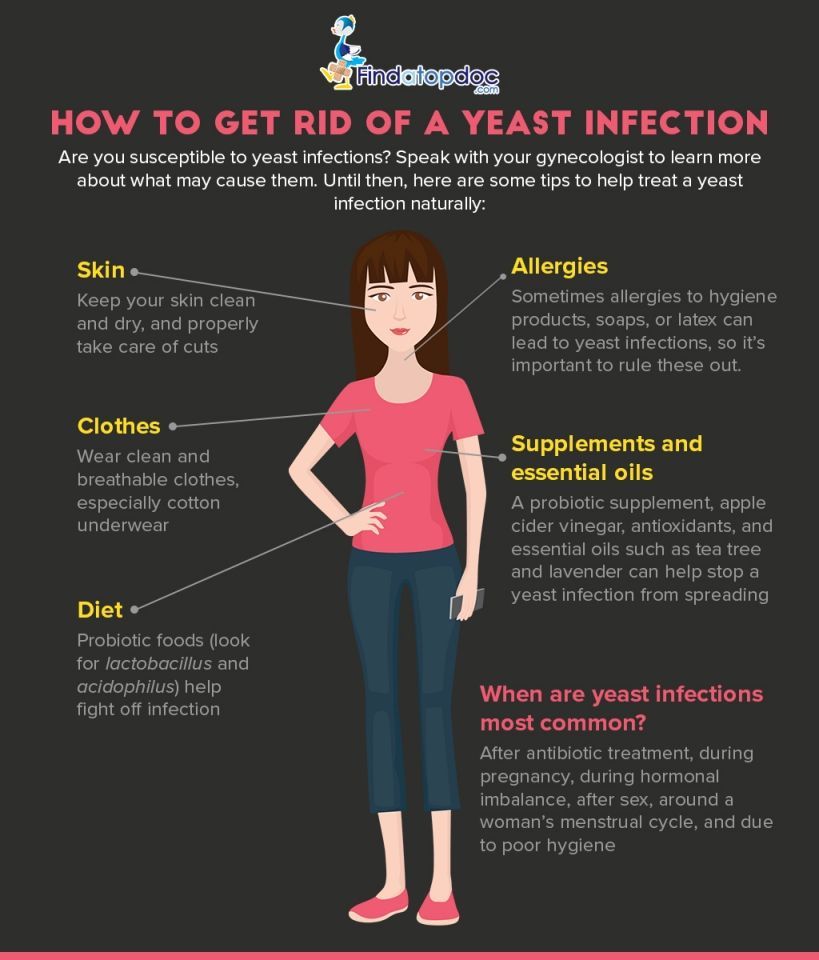 It inhibits the synthesis of proteins, fats, damages nucleic acids in fungal cells and accelerates the excretion of potassium. Very rarely, but sometimes there are yeast-like fungi that may be immune to the drug. In general, reviews of the drug are extremely positive, however, some patients may experience side effects that Clotrimazole has in abundance.
It inhibits the synthesis of proteins, fats, damages nucleic acids in fungal cells and accelerates the excretion of potassium. Very rarely, but sometimes there are yeast-like fungi that may be immune to the drug. In general, reviews of the drug are extremely positive, however, some patients may experience side effects that Clotrimazole has in abundance.
In addition, when treating candidiasis, it is recommended to follow a diet. About what foods can be consumed, and which are better not worth it, read our material.
Folk methods
It should be said that the doctor with whom we consulted does not advise the use of folk remedies for thrush, as they are simply not able to help with this disease. But on the Internet, some means are indicated. Among them: douching and tar soap, soda and chamomile, potassium permanganate and sea buckthorn oil.
For more information on how to use these folk remedies, look in our material.
However, we want to remind you once again that none of the folk remedies is a panacea for thrush. Alternative recipes can reduce the intensity of unpleasant symptoms, but can not cure candidiasis. Therefore, we recommend that you seek professional medical help without fail and do not self-medicate.
find out how to get diagnosed
What to avoid when treating thrush?
First of all, do not self-medicate. This advice is especially relevant during pregnancy. Not all drugs are compatible with pregnancy, and which of them can or cannot be taken - only the attending physician can decide!
As we said above, during pregnancy, only local therapy is prescribed.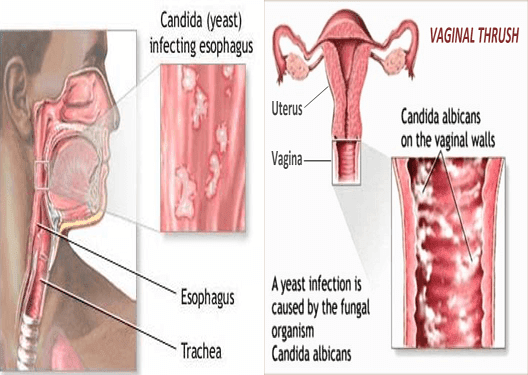 Ignorance of these features can adversely affect the fetus.
Ignorance of these features can adversely affect the fetus.
Why is thrush dangerous during pregnancy?
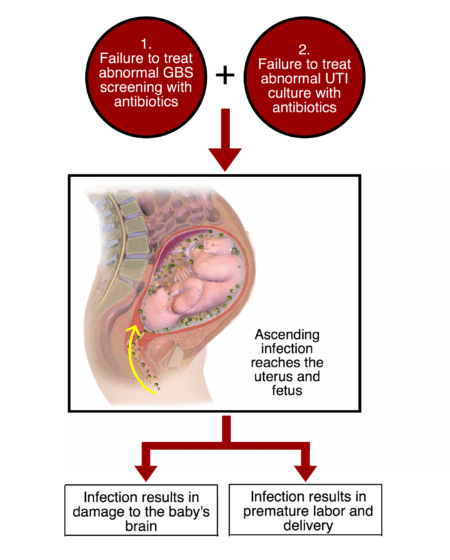
Thrush is dangerous during pregnancy. At this time, the development of an ascending infection with intrauterine infection of the fetus and a newborn with the development of intrauterine infection is possible.
Do not start this disease. This is fraught not only with unpleasant symptoms, but also with consequences for the body. Candidiasis carries the following complications: systemic damage to the pelvic organs, a significant decrease in the quality of life, constant discomfort, dysbiotic disorders of the microflora of the intestinal tract. During pregnancy, the effects may intensify.
What to do if it doesn't go away?
Unfortunately, thrush can easily develop from an active to a chronic form. This happens for a number of reasons. For example, hormonal disruptions and other health-related causes, which abound during pregnancy, can lead to the reappearance of candidiasis. In addition, a decrease in immunity, fatigue, and even climate change can provoke a relapse.
This happens for a number of reasons. For example, hormonal disruptions and other health-related causes, which abound during pregnancy, can lead to the reappearance of candidiasis. In addition, a decrease in immunity, fatigue, and even climate change can provoke a relapse.
If candidiasis does not go away during pregnancy or returns, you should not fight it yourself according to the prepared scheme from the last time. The patient needs to contact the attending physician again to select the most effective drugs.
This is especially true for pregnant women. Drugs used outside of pregnancy can not only not help, but also harm.
Prevention
How to avoid the unpleasant symptoms and consequences of thrush? It is not so difficult to do this if you strictly follow the basic rules of prevention and hygiene. Among them - the selection of comfortable underwear, personal hygiene, the rejection of scented pads and, of course, maintaining the immune system. The last point is, in principle, relevant for pregnant women.
Among them - the selection of comfortable underwear, personal hygiene, the rejection of scented pads and, of course, maintaining the immune system. The last point is, in principle, relevant for pregnant women.
Conclusion
During pregnancy, a woman has a natural decrease in immunity, which may, unfortunately, lead to thrush. And if you do not start a fight with it in time, then the disease can be transmitted to the child. However, with timely treatment and elimination of the factors that cause the disease, it is possible to forget about this disease once and for all. The main thing is not to start thrush to a chronic form. Only a medical specialist will be able to individually select for you a treatment that will cope with the disease.
If you still have questions, you can ask them to the specialists of the Innovative Technology Clinic.
Website: https://3dkit.ru/
Phone: +7 (963) 380-10-31 +7 (865) 257-76-05
. Dovatortsev, 53 B
Author: Ekaterina Vlasova
Photo: Anastasia Ryazhskaya
Treatment of thrush during pregnancy - KGBUZ City hospital No. 12, Barnaul: articles
Associate Professor, Department of Medicine, Medical University, Russian National Research University, Department of Obstetrics and Gynecology. N.I. Pirogov, obstetrics and gynecologist, the highest qualification category.
During pregnancy, infectious diseases and viruses can affect the fetus, so you must be more careful with health care. But it's not that easy. Changes in the body of pregnant women have reduced immunity and significantly increased the risk of disease. In other words, pregnant women's thrush and vulvar candidiasis are three times more.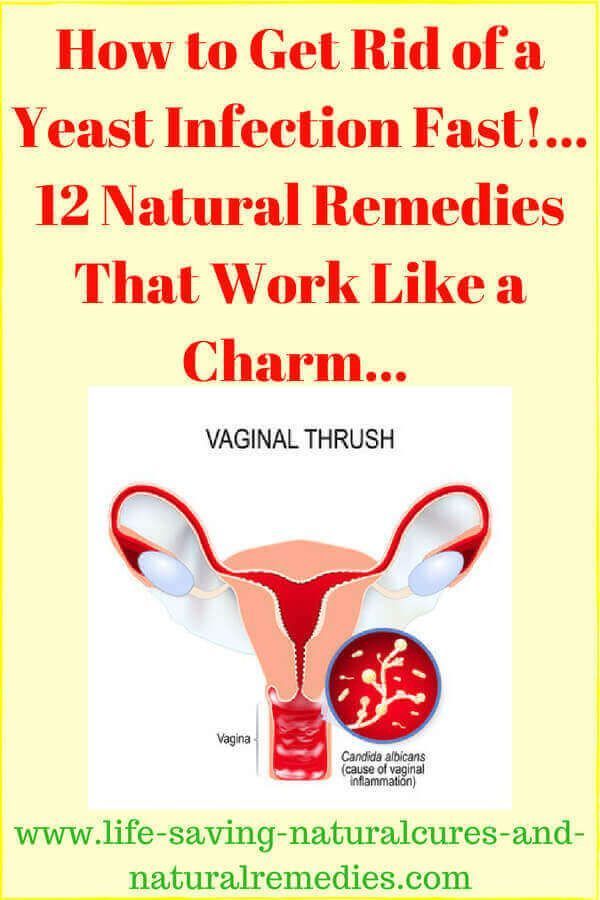 During pregnancy, choking is often a complication and can increase the risk of preterm labor and miscarriages. In addition, when passing by birth, infected during childbirth, you can be infected with candidiasis. As a result, damage to the oral cavity, esophagus and skin. In premature babies, it can be even more serious, such as candida pneumonia and fungal sepsis. Therefore, it is very important to quickly notice the disease and choose the right treatment. Fortunately, treatment can be started at any stage of pregnancy.
During pregnancy, choking is often a complication and can increase the risk of preterm labor and miscarriages. In addition, when passing by birth, infected during childbirth, you can be infected with candidiasis. As a result, damage to the oral cavity, esophagus and skin. In premature babies, it can be even more serious, such as candida pneumonia and fungal sepsis. Therefore, it is very important to quickly notice the disease and choose the right treatment. Fortunately, treatment can be started at any stage of pregnancy.
Pregnant female thrush: causes
- The main reason for the reproduction of Candida bacteria in pregnant women in the immune system is a decrease in the body's defense function. Reduced immunity for a physical reason to prevent the fetus from deviating from the mother. As a result, it is good for the development of the child, but mothers are more susceptible to infectious diseases such as thrush.
- Hormonal imbalance and pregnancy can significantly change hormonal imbalance and increase estrogen.
 As a result, the vaginal mucosa produces a lot of glycogen and activates the Candida genus.
As a result, the vaginal mucosa produces a lot of glycogen and activates the Candida genus. - Even those who love sugar prone foods need to be careful with their diet because carbohydrates develop a culprit. The glucose of pregnant women is used slowly and it is easier to reach the fetus.
- During the stress of pregnancy, the emotional background can become unstable, your mood will quickly change, and small problems can be illusions at the end of this world. Coltisol, the stress hormone, is also generated due to constant mental stress. It maintains the state of the body, but in some cases, it can impair the function of the immune system.
- Intimate high denim liner is an ideal breeding ground for Candida. To prevent this, replace hygiene regularly and remember at least once a day.
- Heavy underwear and dense synthetic fiber o-underwear is always sweaty, creating an ideal condition for fungal and bacterial growth.
- There is no problem with the antibacterial product only for antibacterial soap, but for example, the skin after wax hair removal can be taken with a disinfectant.
 However, antibacterial soap should not be used every day. Antibacterial soap is a rather aggressive composition, which increases the risk of excessive drying of the mucous membrane and the collapse of the vaginal flora. As a result, this can lead to an overgrowth of Candida bacteria.
However, antibacterial soap should not be used every day. Antibacterial soap is a rather aggressive composition, which increases the risk of excessive drying of the mucous membrane and the collapse of the vaginal flora. As a result, this can lead to an overgrowth of Candida bacteria. - Chronic disease undertreatment: Thyroid disorders, diabetes and insufficient genital inflammation also cause candidiasis.
Symptoms of the disease
Milk always appears in the same way.
- Vaginal secretion is usually thick, curly, white or yellowish in color. But sometimes it gives wet and transparency. Pregnant women may be frightened because such a large amount of secretion resembles amniotic fluid. If you notice such signs, be sure to consult your doctor and get tested to see if the amniotic fluid is leaking.
- Itching and burning and discomfort appear in the vulva and vagina and become worse during urination or water.
- Redness and swelling of the genitals and vaginal discharges, which always come out of the vagina, stimulate the lips and perineum.

- Some women feel discomfort and pain when chewing gum during intercourse when having intercourse.
- Since there is a lot of discharge from the strong odor genitals, it may smell moldy and sour.
Diagnosis
Women with position are characterized by vaginal discharge-vitiligo. It is white and has a rich concentration reminiscent of diluted cream. Hence, it is not possible to judge a pregnant female milkman with only one symptom.
Use a speculum to observe the mucous membrane of the vagina and cervix, determine the properties of the secretion and check for inflammation. Take ointment there. The analysis determines the level of white blood cells and the presence or absence of bacteria.
Culture may be required for recurrence of vulvar candidiasis. You can determine susceptibility to pathogens and various drugs.
Method of treatment
Candida Albikans is a pathogen of the daytime woman. Since it is always found in the mucous membrane of the mouth, intestines and vagina, it cannot be completely removed and is not necessary.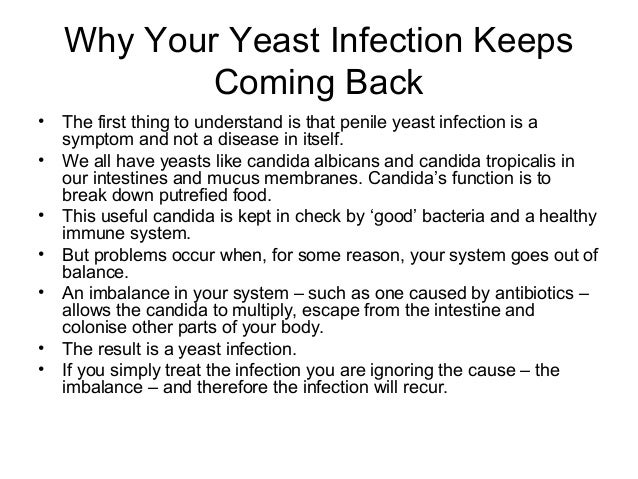 Usually bacteria do not appear. However, due to fluctuations in hormones and a decrease in immunity, it starts further, causing candidiasis. During pregnancy, you need to be treated under the direction of your doctor so that you do not harm your baby.
Usually bacteria do not appear. However, due to fluctuations in hormones and a decrease in immunity, it starts further, causing candidiasis. During pregnancy, you need to be treated under the direction of your doctor so that you do not harm your baby.
During every pregnancy we understand how to treat goose pimples.
Early pregnancy
Early pregnancy is not easy to treat with GOO. At present, important organs for children are beginning to form, so the choice of drugs is limited. External Medicine: Only vaginal sitting, suppositories and cream can be used. Gynecology is usually prescribed in medicines based on natamycin. In this case, the bacteria may be resistant to the tolerant, making it difficult to treat candidiasis.
Treatment of milkman in early pregnancy not only relieves the symptoms of throttling, but it is also necessary to stimulate local immunity and restore microbial activity in the vagina.
Intermediate Pregnancy
Treatment of milkman in the second stage of pregnancy has a wide range of approved drugs and can be used with black preparations. The choice of a particular drug should always be made by a doctor. It is dangerous to start treatment with self-condemnation. There is a risk of recurrence of thrush or complications during pregnancy.
The choice of a particular drug should always be made by a doctor. It is dangerous to start treatment with self-condemnation. There is a risk of recurrence of thrush or complications during pregnancy.
3 months pregnant
Within three months of pregnancy, the fetus is already fully formed and the list of approved units is expanding. Currently, most external antifungal or antifungal agents can be used with caution. At present, the most important thing is to completely remove the disease. Otherwise, the bacteria may be infected by babies at birth.
Pregnancy is one of the important and responsible stages in a woman's life. In many cases, this is Respect for the Elders Day, which means nine months of waiting to meet a child. However, during pregnancy, the hormonal background of a woman's body changes significantly, and at the same time, pleasure, pain and discomfort can be felt in various parts of the body. It can occur in intimate areas, including those with unpleasant symptoms.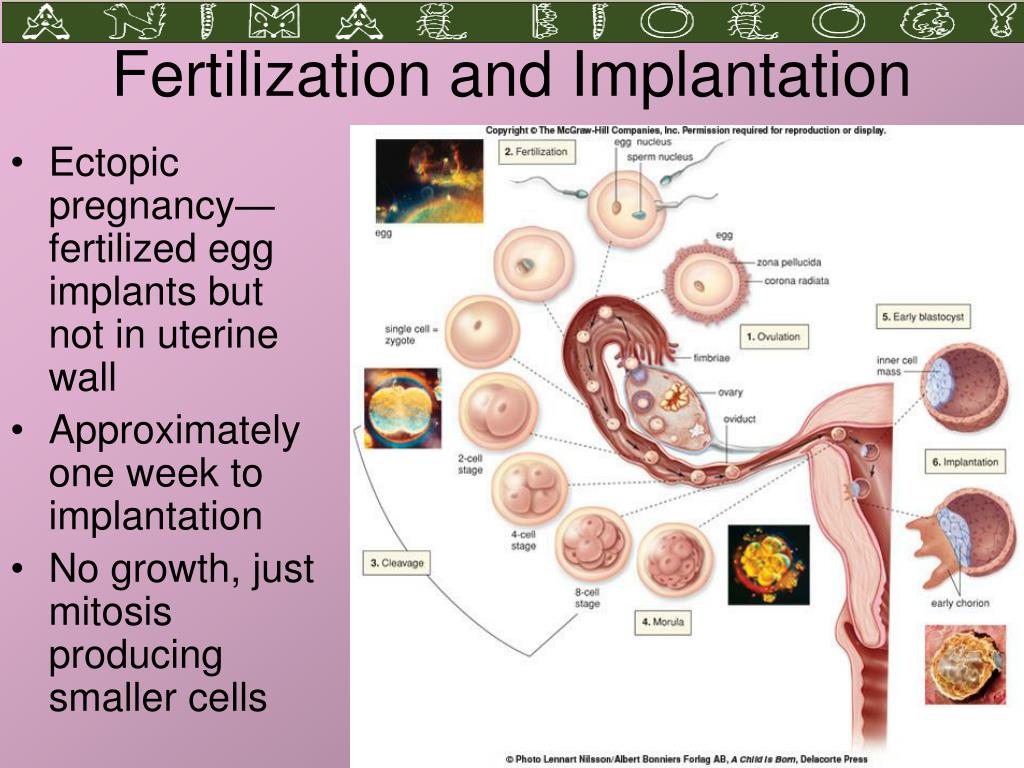
Vaginal discomfort often manifests as itching, burning, irritation and swelling. In short, understand that when these symptoms appear, there is a risk of harming the health of the fetus, so it is necessary to find out the cause as soon as possible and eliminate it.
Various venereal diseases affect the development of discomfort in the perineum. Unfortunately, pregnant women are prone to various infections. An increase in progesterone levels and a natural decrease in the activity of the immune system create favorable conditions for the exacerbation of chronic infections and the emergence of new ones.
How dangerous is the development of a vaginal or vulvar infection during a child's pregnancy? Usually during pregnancy, the fetus is protected from various infections such as amniotic sac, water bacteria, cervical mucosa, etc., so you can easily find your unborn baby.
If an infection is present in an interesting place in a woman's body and is not treated properly, it can adversely affect the course of pregnancy. For example, an untreated infection can damage the membranes of the fetus, the fluid that the fetus is in, or the fetus itself.
For example, an untreated infection can damage the membranes of the fetus, the fluid that the fetus is in, or the fetus itself.
They are also more likely to have physical contact with an infected baby during their passage through the birth canal. Therefore, with any discomfort in the intimate area during pregnancy, you should consult a specialist.
Vaginitis or vulvar appearance may be suspected by symptoms such as rubbing, itching, or burning. Sexually transmitted diseases often cause "vaginitis," an inflammation of the lining of the vagina and cervix. The corpse itself often gives discomfort in the perineal region in pregnant women. This can be caused not only by sexually transmitted diseases, but also by the endocrine system, chronic diseases, stress, poor hygiene.
Bacterial hell can also cause discomfort. This pathology is caused by a decrease in the number of lactobacilli in the vagina, which, as a result of their location, is always occupied by other microorganisms present in the vagina, but in excess leads to the development of dysbacteriosis. Bacterial hell may be asymptomatic, but sometimes progresses with clinical symptoms. Usually accompanied by white, gray or yellow-green vaginal discharge with an unpleasant fishy odor, as well as discomfort.
Bacterial hell may be asymptomatic, but sometimes progresses with clinical symptoms. Usually accompanied by white, gray or yellow-green vaginal discharge with an unpleasant fishy odor, as well as discomfort.
Bacterial hell can also adversely affect the course of pregnancy, causing inflammation of the pelvic organs, premature birth, choroiditis (inflammation of the amniotic membrane), infection of the amniotic fluid, and more.
Vulvovaginal candidiasis, infection of the mucous membranes of the vulva and vagina with Candida, can cause itching in the intimate areas during pregnancy. It should be borne in mind that the development of vulvar candidiasis first develops during pregnancy. This is due to changes in hormone levels, weakening of the immune system. In addition to discomfort, itching and flushing in the fossa, the disease is characterized by mild redness, thick white discharge resembling cottage cheese, a sour smell from the vagina, pain during intercourse and urination.
However, itching and flushing are not always symptoms of a serious illness. In rare cases, using inappropriate underwear or harsh pH soaps can cause discomfort.
If you feel discomfort in your groin, see a specialist. The specialist can conduct an examination, collect an anamnesis, and, if necessary, prescribe laboratory and other diagnostic tests. They help to confirm the diagnosis and choose an individual course of treatment.
To avoid discomfort in the intimate area and not spoil the comfortable additional waiting time, it is necessary to follow the recommendations for prevention.
- It is necessary to carry out external hygiene of intimate areas. Usually twice a day, no more, no less. Frequent washing can lead to “overdrying” of the skin and mucous membranes in intimate areas, and unsanitary conditions can lead to various irritations. Self-cleansing and vaginal douching are not recommended unless recommended by a specialist in specific cases.
- Choose a good detergent.
 Dermatologically tested, hypoallergenic, with lactic acid and genital skin care ingredients are ideal. Epigen Intimate Hygiene Gel is ideal for daily groin hygiene during pregnancy and after childbirth. Epigen Intim Gel consists of activated glycyrrhizic acid and lactic acid. The pH is slightly acidic and corresponds to the normal acid-base balance of the skin in this area. This remedy helps relieve irritation (frustration) from wearing underwear or less comfortable underwear. It has a very pleasant smell and with constant use helps to neutralize unpleasant odors in intimate areas.
Dermatologically tested, hypoallergenic, with lactic acid and genital skin care ingredients are ideal. Epigen Intimate Hygiene Gel is ideal for daily groin hygiene during pregnancy and after childbirth. Epigen Intim Gel consists of activated glycyrrhizic acid and lactic acid. The pH is slightly acidic and corresponds to the normal acid-base balance of the skin in this area. This remedy helps relieve irritation (frustration) from wearing underwear or less comfortable underwear. It has a very pleasant smell and with constant use helps to neutralize unpleasant odors in intimate areas. - Skip synthetics and opt for natural fabrics. Cotton underwear does not create a "greenhouse effect", especially in the heat.
Discomfort in the intimate area is treated in different ways. The diagnosed disease influences the choice of treatment. Spray Epigen Intim can be included in the complex treatment for uncomfortable conditions such as nonspecific vaginitis (vaginitis), bacterial vaginosis, thrush and herpes.
epigene intim spray
epigen intim spray
This drug has an anti-inflammatory and anti-inflammatory effect. Thanks to its active ingredient, active glycyrrhizic acid, Epigen Intim spray can relieve itching and inflammation. It also helps reduce tissue inflammation, swelling, and redness. In addition, this drug can improve the local immunity of the vagina by promoting the production of its own interferon. Epigen Intim spray accelerates the healing and restoration of the integrity of damaged mucous membranes, which leads to the restoration of the protective functions of the mucous membranes and an increase in the number of lactobacilli.
This drug treats viral infections (intense human papillomaviruses, genital herpes), diseases related to local immunity (antiviral, antifungal agent, non-specific vaginitis with antibacterial agents) and these vaginas. Successful fire prevention.
By the way, during the pregnancy of a child, the use of many medicines sold in pharmacies is restricted or prohibited.
However, the familiar spray can be used for pregnancy and women's care and is available without a prescription. This applies to both external and to-eye, depending on the disease.
When the groin is itchy, hot, inflamed and swollen, women feel as uncomfortable as possible. For pregnant women, intimate discomfort can be a great experience. Follow the simple rules presented in the article to minimize the risk of uncomfortable feelings. If there is discomfort for the perineum, it is right to see a specialist. This is not medical help.
Pregnancy is a special situation in a woman's life, and nowadays many daily events take on different dimensions. Especially this disease.
Most pregnant nausea has the same causes for adults and young people. However, there is a specific term "rhinitis of a pregnant woman", which means a reaction to changes in hormones that occur in the body. This type of disease is quite difficult to treat, but in most cases it can be cured naturally or immediately after childbirth or immediately after childbirth. It is important to note that about a third of those who become mothers suffer from rhinitis, that is, that this problem cannot occur normally.
It is important to note that about a third of those who become mothers suffer from rhinitis, that is, that this problem cannot occur normally.
Other causes include:
- allergies
- Infectious diseases and due to viruses and bacteria
- The room is bad.
- Hypothermia
- Nasal mucosal wound
- Decreased immunity and due to diseases infected in the past
- Foreign body enters the nose
- Agro smell
Is a runny nose dangerous during pregnancy?
As a result, rhinitis of a woman in a special position is hardly a threat. As mentioned above, it is in the normal state. However, another threat may be hidden in a runny nose, so the cause must be found immediately.
The first obvious danger is that the treatment of a runny nose during pregnancy cannot be performed in the same way as a normal posture. Most drugs, especially the first few, have a very bad effect on the development of the fetus. For this reason, pregnant women need to choose and treat specific safe medications.
For this reason, pregnant women need to choose and treat specific safe medications.
Another is that a runny nose can be a bigger illness and if you are infected with viruses and bacteria, you will have a serious effect on the fetus. In particular, a severe runny nose and body temperature during pregnancy are dangerous. Therefore, women should catch this symptom and catch the disease at an early stage, which is much easier to treat.
Another argument to look for a doctor, if you have a runny nose during pregnancy in the early stages, then your own nose during pregnancy not only supplies the pregnant woman with oxygen, but also affects her development. that you cannot give. In severe cases, lack of oxygen can lead to underdevelopment of the nervous tissue and mental retardation.
Treatment of the common cold during pregnancy
The common cold is especially bothersome in the first month of pregnancy. At this time, the fetus is active and all major systemic positionings occur. Therefore, the use of drugs is highly discouraged, as this can cause serious harm to the fetus. What should I do? The first step is to see a doctor who can help determine the real cause and how to treat a runny nose during pregnancy. Allergies require complex samples designed to identify the allergen. After that, if possible, the runny nose should pass naturally. For colds and infections, folk remedies are recommended, as well as methods such as inhalation and rinsing the nose with special saline solutions. If the cause of a runny nose is dry air or a lot of dust, it is necessary to use a humidifier and carry out general cleaning. Washing the nose in this case is also good for moisturizing the mucous membranes.
Therefore, the use of drugs is highly discouraged, as this can cause serious harm to the fetus. What should I do? The first step is to see a doctor who can help determine the real cause and how to treat a runny nose during pregnancy. Allergies require complex samples designed to identify the allergen. After that, if possible, the runny nose should pass naturally. For colds and infections, folk remedies are recommended, as well as methods such as inhalation and rinsing the nose with special saline solutions. If the cause of a runny nose is dry air or a lot of dust, it is necessary to use a humidifier and carry out general cleaning. Washing the nose in this case is also good for moisturizing the mucous membranes.
Nasal irrigation during pregnancy is best started from the second month of pregnancy. The fetus is already well formed and the placenta reliably protects it from the invasion of substances. This period is considered the most calm. And in the doctor’s arsenal there are not only folk remedies, but they can also advise safe nasal drops during pregnancy. Of course, drugs are prescribed in minimal doses, sometimes even for children, so this can be ineffective. However, cleansing and inhalations are still effective, and moistening of the mucous membranes may not be necessary.
Of course, drugs are prescribed in minimal doses, sometimes even for children, so this can be ineffective. However, cleansing and inhalations are still effective, and moistening of the mucous membranes may not be necessary.
Runny nose at 3 months of pregnancy is still a serious cause and should be seen by a doctor. In any case, do not start on your own, even if you think you know the cause or a safe remedy. Your body is constantly reinventing itself, and what was right a few months ago can suddenly feel negative. However, rinsing the nose with salt water is currently not contraindicated.
This makes it easier for me to choose a medicine before visiting a specialist.
Treatment of sore throat and runny nose during pregnancy
If one day you suddenly have a sore throat or runny nose, this is an early symptom of a cold, therefore it is especially unpleasant. Remember that many conventional therapies are contraindicated during pregnancy. For example, what is prohibited.
- Increase your vitamin C intake.
- alcoholic drugs
- Yes, and in principle, most drugs except paracetamol, especially antipyretics.
Regular heat treatment should also be carried out carefully in its own position after prior consultation with a doctor. All heating devices are strictly prohibited if they are accompanied by body temperature.
Sore throat and runny nose that can conceive.
- Aqualol Nasal Cleansing Spray, which can be used by pregnant women.
- Drink plenty of hot drinks, preferably fruit drinks, teas, compotes, decoctions of roses.
- Warm the spots on the nose with heated salt or eggs.
- Warm milk with honey
- Inhalation (according to doctor's instructions).
- Bend your legs (handy with woolen socks).
- Ventilate regularly (you should be in another room at the moment).
- Place chopped onion and garlic in all rooms.
- You can wash your throat with kinsenka, chamomile, eucalyptus, and a small decoction every two hours.
 It can be used with a saline solution such as aquarol throat candy.
It can be used with a saline solution such as aquarol throat candy.
Aqualor Pregnancy Cold Spray
Aquarol is a unique tool based on sea water and contains no excipients. At the same time, sea water itself is a very unique complex of various macro and microelements that are beneficial for our body. The water fence was created in an ecological and clean place in the Atlantic Ocean near the coast of Brittany (France) and Lucesila (Sweden). After that, it is completed in a process of removal, sterilization of unwanted impurities, salt reduction, dilution and packaging in a conveniently anatomical aerosol bottle.
Aquarol Nasal Spray can be used not only to prevent airborne infection, but also to clean the nose and throat of pregnant women. The important thing is that the mother and unborn child are completely harmless. It can also be used for the runny nose of newborns. Also, it's just not possible, so don't be afraid to overdose at all. It is recommended to inject the drug solution into the holes in both nostrils in the required number of ways. Then you need to go carefully.
Then you need to go carefully.
It should be noted that this preparation does not belong to homeopathy, and its effectiveness is confirmed by clinical experience. Not only washing the pathogenic microbial plexus with the mucous membrane, but also moisturizing.
Prevention of the common cold
During pregnancy, a normal nose can turn into a serious health problem for mother and children, so this is the time to double and triple. Therefore, you need to pay special attention to disease prevention. We give tips to protect the body.
First of all, before going to bed, especially to regularly change the air in the room. At the same time, he is not in the draft. To prevent the drying contained in the heating, you should buy a humidifier or arrange some water containers throughout the room. Please wipe the water regularly to keep dust from collecting.
Try walking in fresh air, trying to walk in a clean, smoke-free area. Please wear enough according to the weather.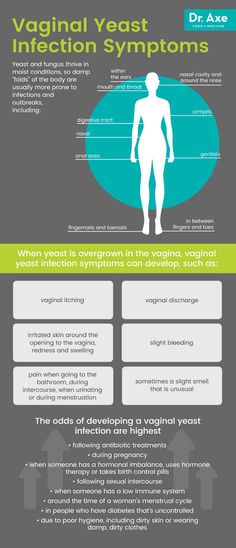 Avoid people with people: a place that seems to be compatible with sources of infection, such as clinics, public transport, and shopping malls. When you get pregnant with your baby, don't forget the mass event.
Avoid people with people: a place that seems to be compatible with sources of infection, such as clinics, public transport, and shopping malls. When you get pregnant with your baby, don't forget the mass event.
In the cold season, do not neglect garlic or onions. If these plants are not included in your regular meal, you can simply cut them up and put them in the room. Also remember that when I was a child, I put pieces of garlic in "kinder soppl as" capsules and wore how to hang up.
We will answer questions you frequently receive.
- What are dangerous inflammatory diseases during pregnancy?
- What tests do you need during pregnancy to prevent this problem?
Prevention of infectious diseases should begin before planning to become pregnant.
And so on. 1. 1.
Therefore, if ovulation occurs usually in the middle of the cycle, if there is chronic inflammation, the secretion of the ovulation hormone will be impaired, ovulation will be slow, and this will happen almost before menstruation, so the eggs are old.
2. A special iron called yolk is formed at the site of the egg after ovulation. This gland is the main factor that secretes a hormone called progesterone, ensures the onset of pregnancy and maintains early pregnancy. In chronic salivary glenitis (inflammation), ovulation occurs at an early stage, progesterone function is incomplete, and the amount of progesterone is insufficient. These factors can often end an early pregnancy. 3. The main cause of ectopic pregnancy is the inflammatory process. The result is stenosis of the junction of the tissue and the Fallopian tube. It also works to promote the progress of the eggs in the uterine cavity and the progress of the eggs in the uterine cavity.
Inflammation of inflammatory diseases during pregnancy
1. When the inner layer of the uterus is damaged, the defense system in the uterus changes. The inner layer of the uterus is rejected (melting) of the rotating solution of the fetus, because it recognizes the embryo from aggressive substances (microorganisms, a virus that causes inflammation) and in the same way as foreign substances (microorganisms). 。
。
2. However, if the eggs of the fetus attached, in most cases they stick to the lower part of the uterus, low adhesion or placenta formation. These conditions are dangerous factors for bleeding during pregnancy.
3. Chronic inflammatory processes can change the antigenic structure of infected endometrial cells. A certain process is the most common cause of the onset of dusty vascular syndrome. One symptom of this complication is the formation of blood clots. During pregnancy, the occurrence of microt-thrombosis in the placenta leads to placental splitting, fetal growth retardation in the setring, a tendency to such an atmosphere, determined during pregnancy complications, proteins in urine proteins, edema and blood pressure. It will be done. 4. In the process of chronic inflammation of the reproductive organs associated with pregnancy, the immune system arises, which is responsible for the recognition of foreign substances and depletion outside the body. The blood cells involved in the immune response are toxic to fetal development and placental formation.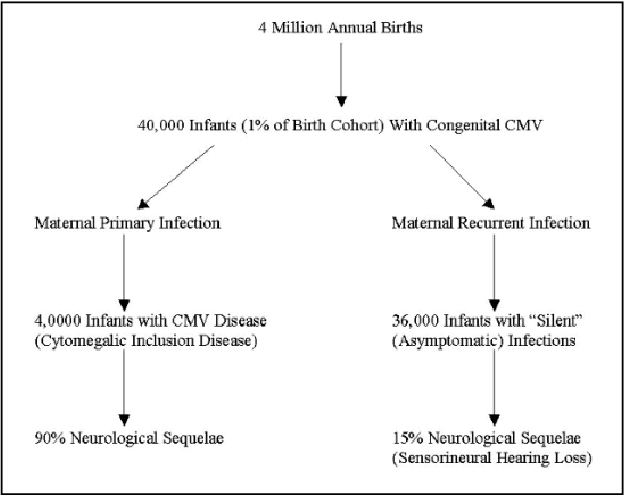
All disorders in the body in the inflammatory process of the female reproductive organ can lead to the following pathology.
- Without gestures
- Concession or frozen pregnancy (fetal death occurs).
- Natural miscarriage during each period of pregnancy.
- Premature birth
- The fetus died in the uterus.
- Subject to fetus.
If the inflammatory process is activated during pregnancy, there is a possibility of an internal infection.
The inclusion of infections in the early stages of pregnancy can form various malformations in the fetus.
After this fetal growth syndrome.
These postpartum babies may become maladjusted and sometimes require additional treatment.
For this reason, newborns whose mother suffers from chronic inflammatory diseases in the genitals, conduct additional interviews on infectious diseases.
During childbirth
1. Inflammatory diseases in various parts of the genital system can adversely affect the progress of childbirth. Complications associated with childbirth include early discharge and premature delivery of amniotic fluid.
Complications associated with childbirth include early discharge and premature delivery of amniotic fluid.
Most microorganisms have a number of specific enzymes that affect the fetal membrane and cause early growth. Usually, if the combat disease is already full scale, the cervix is completely open or almost completely open, if there is an inflammatory edema, pour water before starting the contraction. You can.
2. In addition, there may be a weakening of labor. Also, if the state without water lasts for a long time, the uterus, fetal sac and the fetus itself will be more likely to become infected. Multiple drivers are often accompanied by inflammatory processes, leading to primary or secondary labor. In this case, the uterus is overstretched so that it cannot be well reduced at birth. The need for water, associated with early assessment of amniotic fluid and the need for rolling when pain is relieved, will ultimately negatively affect the condition of the newborn.
Postpartum
a. Inflammation of the genital organs does not disappear after childbirth. After childbirth, the likelihood of endometritis is high, uterine contraction is insufficient, and symptoms such as fever, pain in the lower abdomen, increased blood secretions, and the appearance of characteristic eyebrow secretion.
Inflammation of the genital organs does not disappear after childbirth. After childbirth, the likelihood of endometritis is high, uterine contraction is insufficient, and symptoms such as fever, pain in the lower abdomen, increased blood secretions, and the appearance of characteristic eyebrow secretion.
- This symptom requires treatment in the hospital.
SO!
The chronic inflammatory process most often occurs in a latent form, causing significant changes in the immune system and hemostasis (coagulation system), causing pregnancy, childbirth and terrible complications after childbirth.
At birth, all women with genital inflammatory diseases are carried out to rule out infectious diseases, including sexually transmitted diseases. When a specific pathogen is identified, appropriate treatment is performed.
All women with chronic inflammatory diseases in the genitals are prescribed and treated with drugs to improve the circulation of the placenta to prevent oxygen deficiency (hypoxia) in the fetus.
All women must take responsibility for the pregnancy plan. By conducting pre-pregnancy tests and removing inflammatory nests, you can avoid complications during pregnancy, childbirth and postpartum origin.
Influenza is a dangerous viral infection that develops acutely, and progress is accompanied by typical respiratory disorders and is mainly reflected in lung function. Influenza infection can cause pneumonia, otitis media, and bronchitis, which is especially dangerous for pregnant women.
Symptoms of influenza infection
Influenza often develops one day after infection, despite the incubation period. This photo is closer to pregnant women. This is because the immunity of pregnant women decreases. The body feeds not only on itself, but also on the fetus and allows the strength of two people (mostly three). The level of pregnant women's hormones is different from girls who are not interested.
The lungs of a pregnant woman are heavy because they have to supply oxygen not only to the mother, but also to the tissues of the fetus.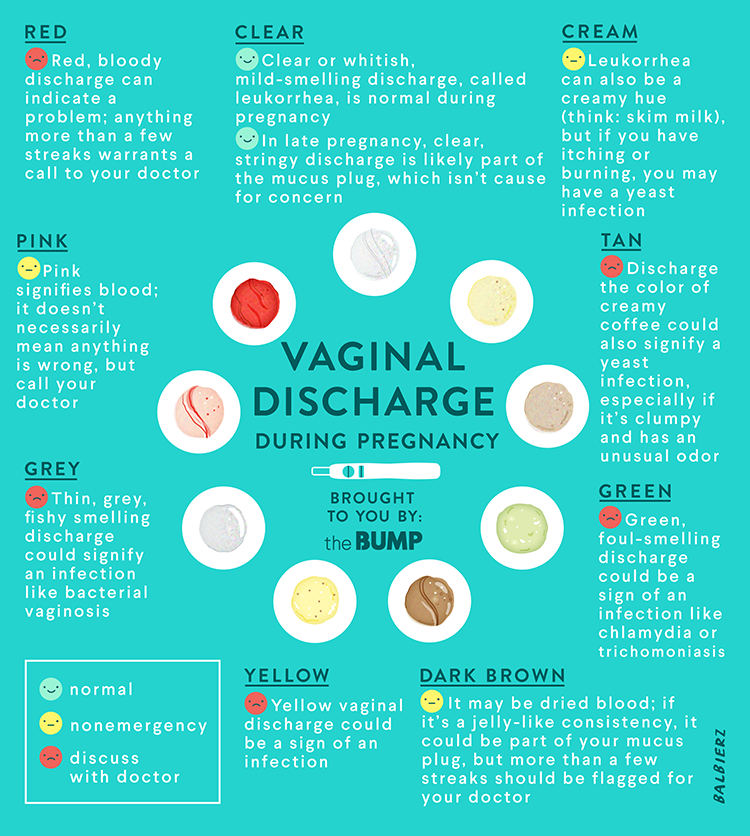 It is also difficult to make the lungs completely straight because the growth fetus compresses the lungs from below for a long time. When an infectious disease enters the respiratory function, it leads to a serious situation in the form of complications.
It is also difficult to make the lungs completely straight because the growth fetus compresses the lungs from below for a long time. When an infectious disease enters the respiratory function, it leads to a serious situation in the form of complications.
The first thing a pregnant woman with influenza feels is shortness of breath. However, upon noticing the anomaly, many women ignore the symptoms and waste them entirely. Taking it within 24-48 hours of infection can stop the virus from spreading throughout the body, which means protecting the mother and fetus from serious situations. Be careful not to have shortness of breath, allowing women to let the flu take over more organs and tissues.
The second important symptom is intense weakness. Also, if it has been revealed for a long time, it is often ignored. Being completely powerless and wanting to sleep all day is a necessity for a doctor.
What a pregnant woman can do to self-diagnose
Influenza infection spreads from person to person. And due to airborne infection, there is a risk of infection by contacting sick people and in a closed room.
And due to airborne infection, there is a risk of infection by contacting sick people and in a closed room.
Therefore, if you are convinced that pregnant women have terrible weakness and shortness of breath, and at the same time you are not sure that they are not in contact with those who are sick or simply unknown, the possibility of influenza may be low. Otherwise, it is urgent to visit a therapist, point out the symptoms and report contact with the patient.
Is the flu dangerous for the fetus
Influenza can have a negative effect on the organs of the fetus, but is said to have little to do with influenza and fetuses folded by the mother.
What is dangerous for the fetus is that the mother's body temperature is high. If the body temperature is 38°C or higher, preterm labor or miscarriage may begin. To prevent this from happening, it is important to control the temperature level from the high point of view of pregnant women. As the indicators begin to approach dangerous levels, you need to take Parasettemor, an anti-framing agent.
Is the flu dangerous for a pregnant woman
The complexity of treating a future mother from influenza is the fact that the effect of a medicine for a doctor to save a pregnant woman's life is many times greater than the degree of harm to the fetus and due to the flu itself. Pregnant women are vulnerable to viral infection. The number of deaths when pregnant women are infected with the flu is much higher than that of consummate women. Therefore, it is very important for women in an interesting position to do as much as possible to reduce the risk of infection.
How to protect pregnant women from the flu
The only reliable way to protect people from the flu is to get vaccinated early. The myth that vaccines harm the fetus is created by inappropriate medical warriors.
Every year the influenza virus mutates and changes its system. Immune scientists and virus scientists are conducting special studies to study changes in the virus and predict more accurate types. As a result of the study, a certain conclusion came out, and the institute created an effective vaccine for certain types of influenza. Vaccines can include both a weak toxic virus and fragments with all the genetic information about the pathology. The body that receives the enemy sample forms an active antibody so that the virus that entered during the infection does not spread and does not affect the internal organs.
As a result of the study, a certain conclusion came out, and the institute created an effective vaccine for certain types of influenza. Vaccines can include both a weak toxic virus and fragments with all the genetic information about the pathology. The body that receives the enemy sample forms an active antibody so that the virus that entered during the infection does not spread and does not affect the internal organs.
This vaccine is also effective in fetal immunity, and the newborn has its own flu antibodies after a few months. However, vaccines have nothing to do with fetal malformations or infectious diseases.
How to treat a pregnant woman for influenza
Pregnant women stay at home and because of their high risk, but strictly under the guidance of doctors. It is strictly forbidden to take medicine without the permission of a doctor. A notable example is that aspirin, which is harmless and popular with adults taking headaches and fevers, causes fetal malformations such as puckering of the lips.
Pregnant women must strictly maintain their rest. Regardless of the weather outside, try regular ventilation and do a wet cleaning on the surface. We aim to create an organism that can compete with infectious diseases by consuming enough water and eating rich vitamins and dietary fiber. It is better to eliminate fatty things and fried foods from meals. If a pregnant woman has swelling, it is necessary to inform the obstetrician and gynecologist as soon as possible. As the amount of water consumed increases, it accumulates in the tissues and is slowly discharged from the kidneys. To solve this problem, doctors may prescribe safe diuretics such as Kaneflon.
When complications develop, women use antiviral therapy while hospitalized and maintain water balance.
All materials listed on this site are for educational purposes only and are not intended for medical advice, diagnosis or treatment. The site operator, the author and the author of the article are not responsible for any consequences and losses caused by the use of materials on the site.
Breast burning during pregnancy is very common and often occurs in cases where you never experienced before pregnancy. In most cases, the breasts of pregnant women begin to worry in the second half of 2-3 months of pregnancy. What are the causes of breasts during pregnancy and how to deal with them?
Causes of heartburn during pregnancy
Breast burns (acid indigestion) bring an unpleasant burning sensation to the chest and mouth. In the case of pregnant women, burns may be accompanied by nausea, vomiting, throat, abdomen, abdominal pain and swallowing mechanisms. In addition, breasts during pregnancy are accompanied by sleep disorders and eating disorders.
Think about the main causes of breasts during pregnancy.
Changes in hormones
When you become pregnant, the secretion of progesterone (called pregnancy) increases. It has the function of relaxing the uterine muscles and preventing pregnancy. The difficulty lies in the fact that the effects of this hormone extend to the esophagus, stomach and intestines.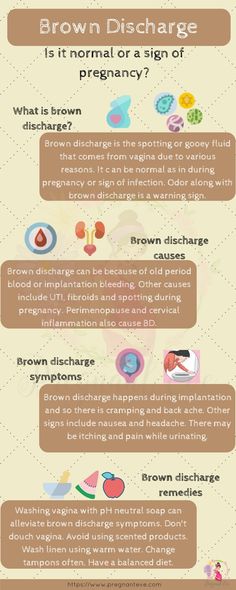
There is a sphincter between the esophagus and the stomach, and after food enters the stomach, it must be closed. However, due to the influence of progesterone, the sphincter characteristic decreases, food returns to the esophagus with hydrochloric acid, and the situation worsens. In addition, the acidity of the gastric juice can increase due to hormonal imbalance, causing burns in the chest.
Mechanical exposure
After the middle of pregnancy, the size of the uterus increases, so the gastrointestinal tract is used. This is due to the fact that the volume of the stomach decreases and the state of the contents of the stomach enters the esophagus.
Chest may occur because you are gaining weight. This is due to the fact that blood pressure begins to affect the abdominal cavity under the excess pound. Clothing compresses the stomach and secretes stomach acid, so tight clothing is best avoided.
Use specific product.
During pregnancy, breasts may also occur due to the following foods.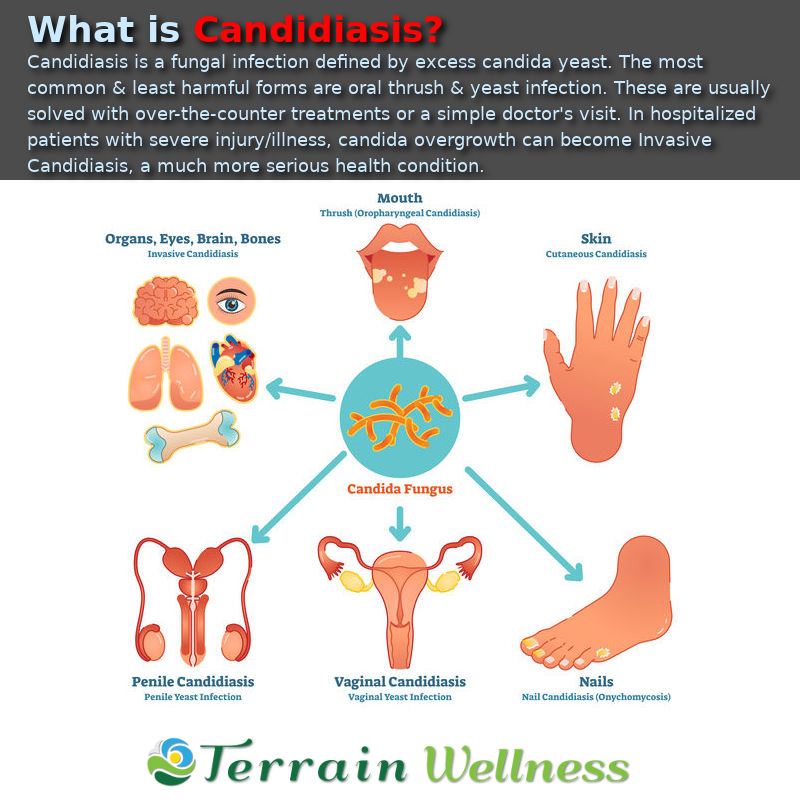
- High fat food (fish, meat).
- Sou r-Dairy Products (fermented foods, kefirs, etc.).
- Bakery.
- Fast food.
- Some types: citrus, kiwi, blue apple, honey harvest, raisins.
- History of tomatoes.
- chocolate
- Smoked meat.
- Sailor.
- soda drink.
- Hard boiled egg.
Treatment of heartburn during pregnancy
To cure breasts during pregnancy from soft, it is enough to fulfill the following points:
- pregnant. There is a certain limit for vegetable products in the chest diet, so it may not be enough for the minerals and vitamins that the body needs. To avoid this situation, it is recommended to take vitamins and minerals exclusively for pregnant women. Such preparations include, for example, "Mom/Pernoton Complex". It contains folic acid, omega a-3, iron liposomes, iodine, selenium, biotin, zinc and vitamins. All these substances are necessary for the proper formation and development of the fetus.
 This medication is provided in softgel form that is easy to drink. So even if you restrict your diet, you can get all the nutrients moms and babies need.
This medication is provided in softgel form that is easy to drink. So even if you restrict your diet, you can get all the nutrients moms and babies need. - In addition to avoiding lifestyle changes, it is usually necessary to stop cigarettes, including alcohol and e-cigarettes, during pregnancy. After eating, walk a little or sit quietly. Horizontal posture, bending and stretching are strictly prohibited. №
- Proper sleep. Pregnant women are supposed to sleep on the edge of the bed to prevent thoroughness. It is convenient to have a spare pillow here.
- Proper food - chew well and eat well. Even if the quantity decreases, it is best to increase the number of meals.
How to quickly get rid of heartburn during pregnancy?
Effective for heartburn: folk remedies
- Using baking soda for pregnancy breasts is one of the most common "private" methods for treating breasts. This method does get results right away, but it will pass quickly.