Sleep habits of infants
Newborn sleep patterns: A survival guide
© 2008 – 2017 Gwen Dewar, Ph.D., all rights reservedAs every parent knows, the world of newborn sleep is exotic and strange. Babies rack up lots of sleep overall, averaging 16-18 hours a day during the first two weeks. Yet they awaken frequently, and rarely sleep more than 4 hours at a stretch, even at night. Their internal clocks aren’t yet synchronized with the external, 24-hour day.
It’s a recipe for exhaustion, but understanding the science of sleep can help you cope, and avoid mistakes that can delay your child’s development of more mature sleep rhythms.
In this article, you’ll learn about
- fundamental differences between newborn sleep and adult sleep;
- circadian rhythms, and how you can help your baby get in sync with the natural day;
- sleep cycles in the newborn, and how to work around them;
- tips for preventing newborns from waking up; and
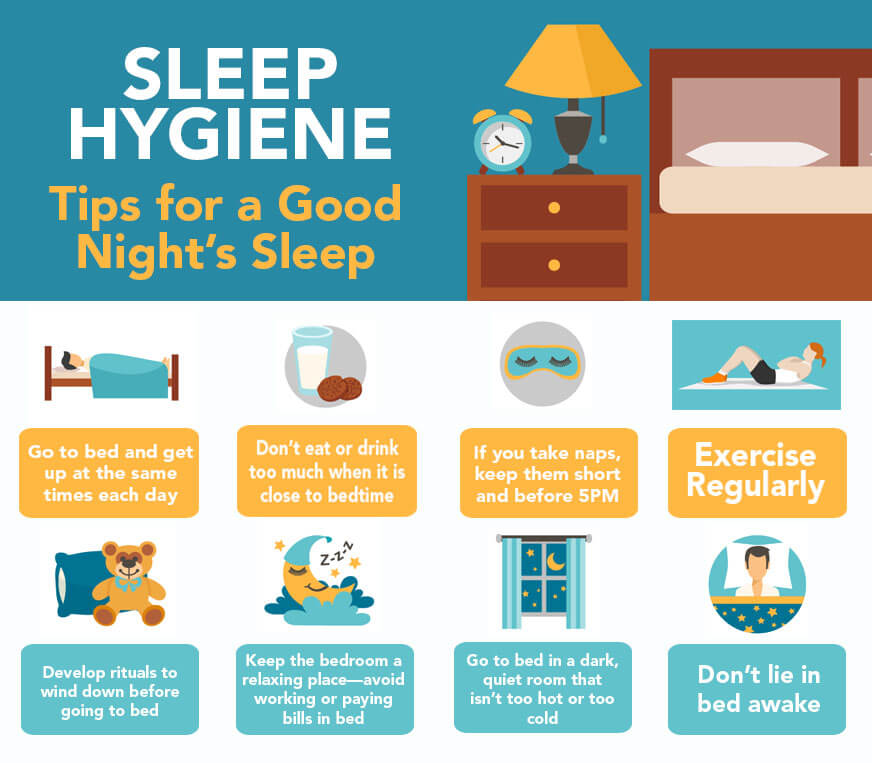
- advice for improving your own sleep.
Throughout, I focus on babies under four weeks of age. For information about older infants, see my article on baby sleep patterns.
If you are looking for information about newborn sleep safety, see these science-based tips for reducing the risk of SIDS.
Newborn sleep patterns: Are there any?
To the sleepless parent, newborn sleep might seem totally disorganized. For example, consider these points.
1. Newborns never sleep for long.
Newborns sleep in short bouts — typically ranging from 30 minutes to 4 hours — at seemingly random times throughout the day and night.
2. Newborns awaken easily.
In part, this is because they spend a large portion of their sleep time in “active sleep,” a light sleep state characterized by fluttering eyelids; rapid, irregular breathing; occasional body movements; and vocalizations (grunts or brief cries).
3. Newborn sleep times can vary widely.
In the first few days, the average newborn sleeps between 16-18 hours a day (Iglowstein et al 2002). By four weeks, newborn sleep averages about 14 hours. But the range is considerable. Some four-week-old babies sleep as little as 9 out of 24 hours. Others sleep for 19 hours a day (Iglowstein et al 2002).
By four weeks, newborn sleep averages about 14 hours. But the range is considerable. Some four-week-old babies sleep as little as 9 out of 24 hours. Others sleep for 19 hours a day (Iglowstein et al 2002).
If your baby doesn’t fit the typical profile, does that mean something is wrong?
Not necessarily. Some babies suffer from medical conditions that influence the way they sleep, so if you have concerns you should discuss them with your medical provider. But it appears that many healthy, normal newborns deviate several hours from the average duration of sleep.
Newborn sleep rhythms: Why newborns seem to sleep—and wake—around the clock
The timing of adult sleep is governed by circadian rhythms — physiological changes that follow a 24-hour cycle. Many of these changes are influenced by your exposure to light.
For instance, when you expose yourself to sunlight during the day, you are helping your body calibrate it’s internal clock. Even if you are sleep-deprived, morning light helps ensure that you will be more alert during the day than you are at night.
Conversely, the absence of light at night helps your body wind down. When darkness falls, your brain interprets this as a signal to start producing melatonin, a hormone that triggers relaxation, paving the way for sleep.
You can easily disrupt this process by exposing yourself to artificial light sources in the evening — especially sources of blue light (Wahnschaffe et al 2013). But as long as you stick with the program — bright light during the day, and darkness at night — you will likely find yourself in sync with the natural, 24-hour day.
And of course most adults are in sync. But it’s different for newborns.
Newborn sleep is not governed by strong circadian rhythms.
Things don’t begin that way. Not when babies are still in the womb. During pregnancy, fetuses are tuned into their mothers’ physiological cues about day and night.
Fetal heart and respiratory rates speed up when a mother is active. They slow down when a mother is sleeping (Mirmiran et al 2003). Such changes may be influenced by maternal hormones, particularly melatonin. Maternal melatonin passes through the placenta, and may direct the fetus’ internal clock (Torres-Farfan et al 2006).
Such changes may be influenced by maternal hormones, particularly melatonin. Maternal melatonin passes through the placenta, and may direct the fetus’ internal clock (Torres-Farfan et al 2006).
But after birth, this intimate hormonal connection is broken. Newborns must develop their own circadian rhythms of hormone production.
Unfortunately for us, this takes time (Kennaway 1996), and the process is complicated by the fact that newborns need to feed every few hours. As a result, newborn sleep episodes tend to be brief, and spaced at fairly regular intervals around the clock.
So when do babies develop mature circadian rhythms?
It’s normal for babies to take 12 weeks, or even longer.
Most infants take about 12 weeks to show day-night rhythms in the production of melatonin (Rivkees 2003). Circadian changes in cortisol, a hormone that helps regulate alertness, may take even longer to emerge (Rivkees 2003). And, overall, babies may take 3-5 months before they “settle” at night–meaning that they sleep for more than 5 hours at a stretch (Jenni et al 2006; Pinilla and Birch 1993).
Nevertheless, newborn sleep isn’t completely divorced from the natural rhythms of the 24-hour day. Studies show that circadian rhythms begin developing in the first days after birth.
For example, German and Japanese studies have reported that newborns sleep more at night than they do during the day (Freudigman and Thoman 1998; Korte 2004; Matsuoka et al 1991).
And scientific evidence suggests that even newborns are receptive to environmental cues about time. You can take advantage of this fact to help shape newborn sleep patterns.
How to help newborns get in sync with the natural, 24-hour day
1. Make your baby a part of your daily routine.
When parents include their newborns in their daily activities, newborn may adapt more rapidly to the 24-hour day (Custodio et al 2007; Lorh et al 1999).
One study took continuous measurements of mother-infant activity patterns for four months after birth. Newborns who were active at the same time of day as their mothers were quicker to develop mature circadian rhythms (Wulff and Siegmund 2002).
2. Reduce stimulation at night.
When your baby wakes for night time feedings, keep activity to a minimum. Make as little noise as possible, and avoid moving your baby around. Ideally, you want to avoid waking her “all the way up.” But if that isn’t possible, at least try to minimize the hustle and bustle. You want the baby to learn that nighttime is for sleep and quiet.
3. Expose your newborn to natural lighting patterns.
Light cues might not instantly synchronize newborn sleep patterns, but they help.
For example, in one study, newborns slept longer at night if their parents observed a regular policy of turning out the lights by 9pm (Iwata et al 2017).
In another study, young babies tended to sleep longer at night if they had been exposed to lots of early afternoon light (Harrison 2004).
And time spent outdoors might make an important difference. Babies who go outside experience much higher daytime light levels than those kept indoors all day, and may develop stronger circadian rhythms as a result (Tsai et al 2012).
4. Try infant massage.
A recent experiment found that mothers assigned to massage their newborns with lotion at bedtime experienced better newborn sleep outcomes than mothers who massaged without lotion and mothers in a control group who didn’t massage at all.
After one month, newborns massaged with lotion were falling asleep faster, staying asleep longer, and awakening at night less often. Mothers using lotion actually massaged their infants more frequently, which may explain the results (Field et al 2016). An earlier study found that infant massage helped newborns develop more mature patterns of melatonin secretion (Ferber 2002).
The takeaway? More research is needed on this topic (Bennett et al 2013), but meanwhile, this seems worth a try.
5. Do you pump and store breast milk? Consider keeping a record of what time of day you express.
Breast milk contains tryptophan, an amino acid that is used by the body to manufacture melatonin.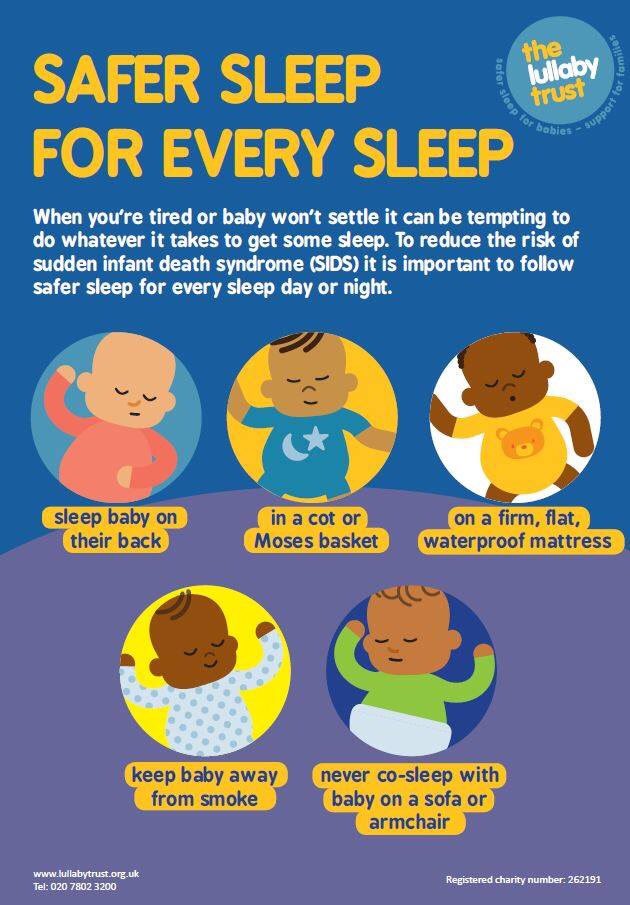 Tryptophan levels rise and fall according to maternal circadian rhythms, and when infants consume tryptophan before bedtime, they fall asleep faster (Steinberg et al 1992).
Tryptophan levels rise and fall according to maternal circadian rhythms, and when infants consume tryptophan before bedtime, they fall asleep faster (Steinberg et al 1992).
It’s therefore possible that breastfeeding helps newborn sleep patterns synchronize with the 24-hour day (Cubero et al 2005). This hypothesis was tested by feeding infants formula fortified with varying concentrations of tryptophan. When infants were given low levels of tryptophan during the day and high concentrations at night (mimicking the natural fluctuations of breast milk), infants fell asleep faster at night and got more sleep overall (Cubero et al 2007).
Newborn sleep cycles: Why newborns are light sleepers
When adults first fall asleep, we pass through a couple of light sleep stages, and then plunge into a bout of deep sleep.
Afterwards, we switch into REM, or “rapid eye movement” sleep, a sleep stage famous for its association with dreaming, and the loss of muscle tone. We don’t move much during REM.
We don’t move much during REM.
When REM is over, we either awaken, or return to light sleep and begin the cycle again. For the average adult, a single sleep cycle lasts about 90-100 minutes. We may partially awaken many times during the night. But we’re more likely to wake up “all the way” during transitions between stages, during light sleep, and during REM.
Newborn sleep is also characterized by sleep stages and cycles, but there are crucial differences.
First, babies typically begin their sleep bouts in the newborn equivalent of REM (sometimes called “active sleep”).
Second, newborns in REM don’t usually experience muscle atonia.
Unlike us, they may thrash around, stretch, twitch, and even vocalize. The results can fool parents into thinking their babies are waking up, when they are actually experiencing normal REM sleep.
Third, newborn sleep cycles are shorter — around 50-55 minutes for the average infant — and REM makes up a much bigger proportion of sleep.
It’s not unusual for newborns to spend more than half their total sleep time in REM (Grigg-Damberger 2016). Indeed, several studies suggest that, over the course of a 24 hour day, some newborns spent may spend as much as 75% of their sleep time in active sleep (e.g., Poblano et al 2007; Sadeh et al 1996).
Fourth, while newborns do experience something roughly analogous to deep sleep, this stage, called “quiet sleep,” is potentially dangerous.
Characterized by slower, more rhythmic breathing, quiet sleep appears more restful (Grigg-Damberger 2016). But it’s harder for babies to awaken from quiet sleep, which can cause trouble if the baby isn’t getting enough oxygen.
This may explain why newborns don’t oblige exhausted parents by lapsing into long periods of deep sleep. It’s too risky. Instead, the typical 50-55 minute newborn sleep cycle includes only about 20 minutes of quiet sleep. The rest of the time, babies are either in REM or in “transitional sleep,” a rather restless state that looks like a mash-up of active and quiet sleep, and which scientists don’t yet understand (Grigg-Damberget 2016).
Put this all together, and you can see why parents feel their babies are such light (and erratic) sleepers. Like adults, newborns are more likely to awaken during REM, and during transitions between sleep stages. But unlike adults, newborns spend a lot more time in REM, and they transition between cycles more frequently.
And parents may sometimes mistake REM restlessness for waking — and attempt to interact with or soothe a baby at the wrong time. In short, there are lots of opportunities for babies to wake up — or get awakened unnecessarily.
This sounds like a raw deal for parents. But newborns probably benefit from being light sleepers. Having a low threshold of arousal may protect babies from SIDS, and active sleep might be crucial for a newborn’s brain development (Heraghty et al 2008; Seigel 2005).
And if we understand the peculiar nature of newborn REM, we can learn to avoid jumping in too soon when we think a baby is awakening or signalling for us.
A baby who seems to be waking up may, if left alone, go back to sleep very rapidly.
How to keep your light sleeper from waking up all the way
1. Don’t rush in the moment you think your baby has awakened.
As noted above, babies experience frequent arousals, but that doesn’t mean they are doomed to wake up “all the way” every few minutes. Babies often jerk, sigh, or vocalize during partial arousals. If you avoid stimulating them during these moments, they may go back to sleep on their own.
2. Tank up the baby before you go to sleep.
Whether you breastfeed or bottle-fed, try to give the baby an especially large meal before your own bedtime. This will encourage your baby to sleep longer. To learn more about this approach, see this Parenting Science guide to “Dream feeding.”
3. If you feed your baby formula, try to find one that includes DHA.
DHA is a fatty acid found in fish oil and other dietary sources. It’s important for brain development, and may play a role in shaping sleep patterns as well.
In one study, children who consumed low levels of DHA had reduced amount of slow-wave (deep) sleep (Faglioli et al 1989). In another study, pregnant women with higher blood levels of DHA gave birth to babies who spent more time in quiet sleep (Cheruku et al 2002).
DHA is found in breast milk, so it’s plausible (though unproven) that boosting a nursing mother’s DHA intake could improve a newborn’s sleep patterns. If you use formula, it seems like a good idea to find a baby formula that contains DHA.
4. Check out my article on baby sleep aids.
There you’ll find tips for improving newborn sleep, and avoiding practices that are either unhelpful or potentially hazardous.
Newborn sleep patterns take their toll on parents. In a study tracking the sleep patterns of mothers from pregnancy through the postpartum period, maternal sleep worsened after childbirth and continued to deteriorate until about 12 weeks postpartum (Kang et al 2002)—-the time when newborn sleep patterns begin to show marked circadian rhythms (Nishihara et al 2000).
Twelve weeks isn’t forever, but it can seem like it when you are severely sleep restricted. As you struggle to cope with newborn sleep patterns, don’t forget to look after yourself. Here are some tips to help you cope.
1. Appreciate the power of a 30-minute nap
When you’re running up an enormous sleep debt, you might think a 30-minute nap will make little difference to your health.
But recent research confirms that all naps are not the same. When you’re sleep deprived, the brain compensates by rendering naps more restorative than usual.
In one study, volunteers permitted to sleep only 2 hours at night showed the typical abnormalities in their stress hormone and immune factor chemistry. But after just two 30-minute naps, those irregularities were entirely normalized (Faraut et al 2015b).
In another study, volunteers coping with a 2-hour nightly regimen experienced heightened pain sensitivity — a common symptom of sleep deprivation. But once again, the effect was reversed after just two 30-minute naps (Faraut et al 2015a).
2. Don’t assume that it’s pointless to lie down if you don’t fall asleep. You might pass into a state of drowsy, semi-conscious sleep — and reap some benefits.
Too wired to “sleep when the baby sleeps”? If so, keep in mind that quiet resting is better than nothing. In fact, if you are lying down with your eyes closed, you might be asleep without realizing it.
In numerous lab studies, subjects who were awakened from the first stage of sleep often denied that they were asleep at all (Dement and Vaughan 1999). A nap that consists only of stage 1 sleep might not help you improve your reaction times, but it will probably make you feel less tired. And if you manage to slip into the second stage of sleep — even for just 3 minutes — your nap may have recuperative effects (Hayashi et al 2005).
3. Don’t play the blame game.
Brooding about the situation will make it harder for you to fall asleep when you are given the opportunity. And it’s wrong-headed, too: You might be doing everything you can to get more sleep, and still be stuck with a baby who sleeps less than average.
Research suggests that the amount of sleep we get at night is strongly influenced by genetics (Touchette et al 2013), and, as mentioned above, there is a lot of individual variation among newborns.
4. Don’t assume that breastfeeding will make you more sleepless than formula feeding.
One study reported that the parents of breastfed babies averaged 40-45 minutes more sleep time than did the parents of formula-fed babies (Doan et al 2007).
5. If you are breastfeeding, you are likely to get more sleep if you keep your baby nearby.
The World Health Organization recommends that babies share a bedroom with their parents, and it’s a recommendation that makes breastfeeding less disruptive. A recent study found that breastfeeding women got more sleep when they co-slept with baby (Quillin and Glenn 2004). In fact, mothers who co-slept and breastfed got more sleep than did mothers who bottle-fed their babies (Quillin and Glenn 2004).
6. If your baby is asleep, don’t worry about changing diapers.

If your baby can’t sleep because she needs a diaper change, she’ll let you know. And a little urine is unlikely to awaken her anyway. In a recent experiment, researchers injected water into the diapers of sleeping infants to see if this would wake them up (Zotter et al 2007). It didn’t.
7. Get sunlight and avoid artificial lighting at night.
Make sure you expose yourself and your baby to bright light during the day. And keep lights out–or at least dimmed–after sunset.
As noted above, natural lighting helps influence newborn sleep patterns. But it also helps you keep your own circadian rhythms from drifting, which is important if you are going avoid insomnia and be a source of daytime cues for your newborn.
8. Let a friend or family member watch your baby while you take a nap, even if this means your breastfed baby will take some meals from a bottle.
Lactation experts often discourage breastfeeding mothers from bottle feeding babies for the first 3-4 weeks.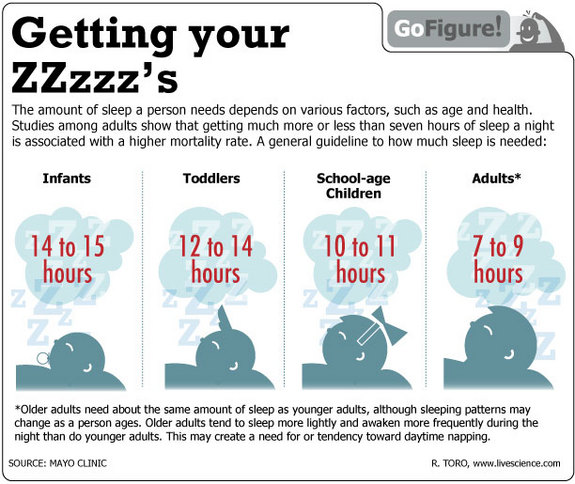 The worry is that supplemental feeds will lead to a decreased milk supply and endanger successful breastfeeding in the long-term.
The worry is that supplemental feeds will lead to a decreased milk supply and endanger successful breastfeeding in the long-term.
But you need to balance this against the negative effects of severe sleep restriction. Lack of sleep puts parents at increased risk of illness and postpartum depression, which is bad for parents and babies. If you are at the end of your rope, get help.
9. Trust your instincts, and get help when you feel stressed
If something feels wrong with you or the baby, talk to your physician. And remember that your own mental health is crucial.
Coping with sleep deprivation is very stressful, especially if your infant seems to be especially fussy or prone to crying. Watch for signs of postpartum stress and postpartum depression, and reach out to others for support.
10. Remember that things will get better
Newborns have special sleep patterns and special needs. But things will start to get better around 12 weeks postpartum.
More reading relevant to newborn sleep
For more information about babies and sleep, see these fully-referenced Parenting Science articles.
References: What scientific studies say about newborn sleep
Anders TF. 1979. Night-waking in infants during the first year of life. Pediatrics 63: 860-864.
Bennett C, Underdown A, and Barlow J. 2013. Massage for promoting mental and physical health in typically developing infants under the age of six months. Cochrane Database Syst Rev. 2013 Apr 30;4:CD005038. doi: 10.1002/14651858.CD005038.pub3.
Cheruku SR, Montgomery-Downs HE, Farkas SL, Thoman EB, and Lammi-Keefe CJ. 2002. Higher maternal plasma docosahexaenoic acid during pregnancy is associated with more mature neonatal sleep-state patterning. Am J Clin Nutr 76:608-13.
Cubero J, Valero V, Sánchez J, Rivero M, Parvez H, Rodríguez AB, Barriga C. 2005. The circadian rhythm of tryptophan in breast milk affects the rhythms of 6-sulfatoxymelatonin and sleep in newborn. Neuro Endocrinol Lett. 26(6):657-61.
Neuro Endocrinol Lett. 26(6):657-61.
Cubero J, Narciso D, Terrón P, Rial R, Esteban S, Rivero M, Parvez H, Rodríguez AB, Barriga C. 2007. Chrononutrition applied to formula milks to consolidate infants’ sleep/wake cycle. Neuro Endocrinol Lett. 28(4):360-6.
Custodio RJ, Junior CE, Milani SL, Simões AL, de Castro M, Moreira AC. 2007. The emergence of the cortisol circadian rhythm in monozygotic and dizygotic twin infants: the twin-pair synchrony. Clin Endocrinol (Oxf). 66(2):192-7.
Dement W and Vaughan C. 1999. The promise of sleep. New York: Random House.
Doan T, Gardiner A, Gay CL, Lee KA. 2007 Breast-feeding increases sleep duration of new parents. J Perinat Neonatal Nurs. 21(3):200-6.
Faglioli I, Barconcini P, Ricour C, and Salzarulo P. 1998. Decrease of slow-wave sleep in children with prolonged absence of essential lipids intake. Sleep 12: 495-499.
Faraut B, Léger D, Medkour T, Dubois A, Bayon V, Chennaoui M, Perrot S. 2015a. Napping reverses increased pain sensitivity due to sleep restriction. PLoS One. 10(2):e0117425.
PLoS One. 10(2):e0117425.
Faraut B, Nakib S, Drogou C, Elbaz M, Sauvet F, De Bandt JP, Léger D. 2015b. Napping reverses the salivary interleukin-6 and urinary norepinephrine changes induced by sleep restriction. J Clin Endocrinol Metab. 100(3):E416-26.
Ferber SG, Laudon M, Kuint J, Weller A, Zisapel N. 2002. Massage therapy by mothers enhances the adjustment of circadian rhythms to the nocturnal period in full-term infants. J Dev Behav Pediatr. 23(6):410-5.
Field T, Gonzalez G, Diego M, Mindell J. 2016. Mothers massaging their newborns with lotion versus no lotion enhances mothers’ and newborns’ sleep. Infant Behav Dev. 45(Pt A):31-37.
Freudigman KA and Thoman EB. 1998. Infants’ earliest sleep/wake organization differs as a function of delivery mode. Dev Psychobiol. 32(4):293-303.
Grigg-Damberger MM. 2016. The Visual Scoring of Sleep in Infants 0 to 2 Months of Age. J Clin Sleep Med. 12(3):429-45.
Iglowstein I, Jenni OG, Molinari L, Largo RH. 2003. Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics 111(2): 302-307.
Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics 111(2): 302-307.
Harrison Y. 2004. The relationship between daytime exposure to light and night-time sleep in 6-12-week-old infants. J Sleep Res. 13(4):345-52.
Hayashi M, Motoyoshi N, Hori T. 2005. Recuperative power of a short daytime nap with or without stage 2 sleep. Sleep. 28(7):829-36.
Heraghty JL, Hilliard TN, Henderson AJ, and Fleming PJ. 2008. The physiology of sleep in infants. Arch Dis Child. 2008 Nov;93(11):982-5.
Horne RSC, Parslow PM, Ferens D, Watts AM, and Adamson TM. 2004. Comparison of evoked arousability in breast and formula fed infants. Arch Dis Child 89: 22-25.
Hugelin A. 1982. Mechanisms of respiratory control during sleep and wakefulness: implications in newborn sleep apnoea. Electroencephalogr Clin Neurophysiol Suppl. 36:625-30.
Iwata S, Fujita F, Kinoshita M, Unno M, Horinouchi T, Morokuma S, Iwata O. 2017. Dependence of nighttime sleep duration in one-month-old infants on alterations in natural and artificial photoperiod. Sci Rep. 7:44749.
Sci Rep. 7:44749.
Jenni OG, DeBoer T, and Acherman P. 2006. Development of the 24h rest-activity pattern in human infants. Infant behavior and development 29: 143-152.
Kang MJ, Matsumoto K, Shinkoda H, Mishima M, Yeo YJ. 2002. Longitudinal study for sleep-wake behaviours of mothers from pre-partum to post-partum using actigraph and sleep logs. Psychiatry Clin Neurosci. 56(3):251-2.
Kato I, Franco P, Grosswasser J, Scaillet S, et al. 2003. Incomplete arousal processes in infants who were victims of sudden death. Am J Respir Crit Care Med 168: 1298-1303.
Kennaway DJ, Goble FC and Stamp GE. 1996. Factors influencing the development of melatonin rhythmicity in humans. Journal of Clinical Endocrinology & Metabolism, Vol 81, 1525-1532
Korte J, Hoehn T, Siegmund R. 2004. Actigraphic recordings of activity-rest rhythms of neonates born by different delivery modes. Chronobiol Int. 21(1):95-106
Lohr B, Siegmund R. 1999. Ultradian and circadian rhythms of sleep-wake and food-intake behavior during early infancy. Chonobiology international 16(2): 129-148.
Chonobiology international 16(2): 129-148.
Matsuoka M, Segawa M, and Higurashi M. 1991. The Development of Sleep and Wakefulness Cycle in Early Infancy and Its Relationship to Feeding Habit. The Tohoku Journal of Experimental Medicine 165 (2):147-154.
McNamara F, Lijowska AS, and Thach BT. 2002. Spontaneous arousal activity in infants during NREM and REM sleep. J Physiol 538: 263-269.
Mirmiran M, Maas YG, Ariagno RL. 2003. Development of fetal and neonatal sleep and circadian rhythms. Sleep Med Rev. 7(4):321-34.
Nishihara K, Horiuchi S, Eto H, Uchida S. 2000. The development of infants’ circadian rest-activity rhythm and mothers’ rhythm. Psychiatry Clin Neurosci. 54(3):305-6
Pinilla T and Birch LL. 1993. Help me make it through the night: Behavioral entrainment of breasfed infants’ sleep patterns. Pediatrics 91: 436-444.
Poblano A, Haro R, and Arteaga C. 2007. Neurophysiologic measurement of continuity in the sleep of fetuses during the last week of pregnancy and in newborns. Int J Biol Sci. 4(1):23-8.
Int J Biol Sci. 4(1):23-8.
Quillin SI and Glenn LL. 2004. Interaction between feeding method and co-sleeping on maternal-newborn sleep. J Obstet gynecol Neonatal Nurs 33(5): 580-588.
Rivkees SA, Mayes L, Jacobs H, Gross I. 2004. Rest-activity patterns of premature infants are regulated by cycled lighting. Pediatrics. 113(4):833-9.
Sadeh A, Dark I, and Vohr BR. 1996. Newborns’ sleep-wake patterns: the role of maternal, delivery and infant factors. Early Hum Dev. 44(2):113-26
Siegel JM. 2005. Functional implications of sleep development. PLoS Biology 3(5): 756-758.
Thomas KA and Burr R. 2002. Preterm infant temperature circadian rhythm: possible effect of parental cosleeping. Biol Res Nurs. 3(3):150-9.
Torres-Farfan C, Rocco V, Monsó C, Valenzuela FJ, Campino C, Germain A, Torrealba F, Valenzuela GJ, and Seron-Ferre M. 2006. Maternal melatonin effects on clock gene expression in a nonhuman primate fetus. Endocrinology. 147(10):4618-26.
Touchette E, Dionne G, Forget-Dubois N, Petit D, Pérusse D, Falissard B, Tremblay RE, Boivin M, and Montplaisir JY. 2013. Genetic and environmental influences on daytime and nighttime sleep duration in early childhood. Pediatrics 131(6):e1874-80.
Tsai SY, Thomas KA, Lentz MJ, Barnard KE.2012. Light is beneficial for infant circadian entrainment: an actigraphic study. J Adv Nurs. 68(8):1738-47.
Van Sleuwen BE, Englelberts AC, Boere-Boonekamp MM, Kuis W, Schulpen TWJ, and L’Hoir MP. 2007. Swaddling: A systematic review. Pediatrics 120: e1097-1106.
Wahnschaffe A, Haedel S, Rodenbeck A, Stoll C, Rudolph H, Kozakov R, Schoepp H, and Kunz D. 2013. Out of the lab and into the bathroom: evening short-term exposure to conventional light suppresses melatonin and increases alertness perception. Int J Mol Sci. 14(2):2573-89.
Wulff K, Siegmund R. 2002.[Emergence of circadian rhythms in infants before and after birth: evidence for variations by parental influence]. Z Geburtshilfe Neonatol. 206(5):166-71. Review. German.
Z Geburtshilfe Neonatol. 206(5):166-71. Review. German.
Zotter H, Urlesberger B, Pichler G, Mueller W, Kerbl R. 2007. Do wet diapers induce arousals in sleeping infants? Acta Paediatr. 96(3):452-3.
Content of “Newborn sleep patterns” last modified 9/17
Image credits for “Newborn sleep patterns”
title imagine of newborn sleeping by Raw pixel / istock
image of mother kissing newborn ©iStockphoto.com/Shawn Gearhart
image of tired mother with sleeping newborn by istock
Baby sleep patterns for the science-minded
© 2018 Gwen Dewar, Ph.D., all rights reserved
Baby sleep patterns vary from infant to infant, and they change over time. So there is no one, universal chart or instruction manual that can predict when and how your baby will sleep.
But scientific research can help us understand the range of variation, and the general trends.
Here I provide a timeline of quick facts, followed by a longer article that will help you understand what can speed up — or slow down — the development of baby sleep patterns.
I’ll also help answer questions like “how much sleep does a baby need?” and “when do babies start sleeping through the night?”
A developmental timeline of baby sleep patterns
0-3 months. Newborns sleep in short bouts scattered throughout the 24-hour day. As the days pass, they gradually develop a tendency to sleep more at night.
Total sleep duration varies; about half of all infants get between 13 and 16 hours of sleep every 24 hours.
Overall, their sleep is light and restless. Unlike older children and adults, young babies usually lapse into REM, or rapid eye movement sleep, immediately after dozing off, and they spend a lot more sleep time in REM than we do.
They move around a lot, and sometimes even vocalize. Learn more in my article about newborn baby sleep patterns.
3-4 months. Baby sleep patterns are becoming more adult-like. Infants no longer plunge directly into REM after falling asleep, and their sleep cycles begin to include longer stretches of slow-wave, “deep” sleep (Schechtman et al 1994).
In addition, babies are more likely to sleep for extended periods at night.
For example, in one study, approximately 50% of parents reported infant sleep bouts lasting 5 hours or more (Henderson et al 2010).
But multiple daytime naps are still common, and there is still a lot of individual variation. For most babies this age, total sleep duration is likely in the range of 12-16 hours.
5-6 months. Around this age, most parents report that their babies are sleeping without interruption at night for 5 hours or more, and many claim their babies sleep for more than 10 hours at night (Mindell et al 2016; Iglowstein; Jiang et al 2007).
Nevertheless, it’s not unusual for parents to report that their babies awaken at least once during the night, and some babies don’t settle into 5+ hour sleep bouts until they are considerably older (see below).
Babies typically take several naps during the day, and average total sleep duration remains in the range of 12-16 hours.
7-12 months. If your baby still isn’t sleeping for at least 5 hours at a stretch, you’re in good company. In one study of American infants, more than 15% of parents reported that their 12 month old babies hadn’t yet reached this milestone (Henderson et al 2010).
But for most families, nights have quieted down. It isn’t that these babies don’t experience night wakings. On the contrary, it’s normal for infants this age to awaken 3-4 times each night. But many babies have learned to fall back to sleep quietly on their own, so that their parents aren’t even aware that their infants had awakened (Goodlin-Jones et al 2001; Dias et al 2018).
By the end of the first year, babies tend to spend less time napping. But naps appear to remain helpful, and babies typically take one or two each day. Most babies continue to get sleep approximately 12-16 hours every 24 hours.
Factors that affect the timeline — or temporarily shake things up
Baby sleep patterns are shaped by a mix of genetic and environmental factors. For instance, in two studies of 6-month old babies, almost half the individual variation in nighttime sleep duration could be explained by genetic factors (Dionne et al 2015; Touchette et al 2013).
For instance, in two studies of 6-month old babies, almost half the individual variation in nighttime sleep duration could be explained by genetic factors (Dionne et al 2015; Touchette et al 2013).
By contrast, individual differences in the trajectory of napping — whether babies decreased napping from 6 months onward — were almost entirely explained by environmental factors, like whether parents promote or discourage napping.
How do genes influence baby sleep patterns? One route is by shaping infant temperament. If your baby tends to be less adaptable and more irritable, it’s going to be harder to quiet him or her down, and studies confirm that such babies sleep less overall (Weissbluth and Liu 1983; Van Tassel 1985; Scher et al 1992; Sadeh et al 1994; Scher et al 1998).
It’s also likely that some babies need less sleep than others, and that specific aspects of sleep — like how easily an infant is awakened — are shaped by genes.
But it’s clear that parents can affect baby sleep patterns. We’ve already noted the effects parents have on napping. In addition, parents can influence the development of circadian rhythms, and help babies learn to resettle themselves after waking at night (see below).
We’ve already noted the effects parents have on napping. In addition, parents can influence the development of circadian rhythms, and help babies learn to resettle themselves after waking at night (see below).
Finally, it appears that baby sleep patterns vary from one country to the next. For example, studies suggest that babies in Japan and Italy tend to sleep less than their counterparts in Switzerland and Canada (Kohyama et al 2011; Bruni et al 2014; Iglostein et al 2003; Mindell et al 2010).
And motor milestones — like learning to crawl, learning to stand, and learning to walk — tend to disrupt baby sleep patterns (Atun-Einy Scher 2016; Scher and Cohen 2015). If your baby is mastering a new physical skill, you might observe temporary changes.
Digging deeper: What makes baby sleep patterns different from our own, and how can we help babies develop more mature sleep habits?
The foregoing summary offers some quick answers. But it pays to learn more about baby sleep patterns. It can help you avoid mistakes, and support the development of more mature sleep rhythms.
It can help you avoid mistakes, and support the development of more mature sleep rhythms.
Here’s a look at baby sleep patterns in greater detail — focusing on circadian rhythms, sleep stages, sleep cycles, night wakings, and sleep duration.
Circadian rhythms: How long does it take for babies to synchronize with the natural, 24-hour day?
Young babies are notorious for sleeping and waking at awkward times. In part, this is because their circadian rhythms — recurring, 24-hour cycles of physiological activity — aren’t synchronized with the natural rhythms of daylight and darkness.
You may have heard that it takes 3-4 months for babies to develop mature circadian rhythms. But research confirms that the timing varies, and that babies synchronize sooner when we provide them with the right environmental cues.
Light has the biggest impact on your baby’s “inner clock,” so use it wisely.
During the day, expose your baby to natural, bright light. And as evening approaches, dim the artificial lights, and take care to avoid nighttime exposure to blue light, which is especially disruptive of sleep. Research suggests that newborns sleep for longer stretches at night when their parents stick with a policy of “lights out” after 9pm (Iwata et al 2017).
And as evening approaches, dim the artificial lights, and take care to avoid nighttime exposure to blue light, which is especially disruptive of sleep. Research suggests that newborns sleep for longer stretches at night when their parents stick with a policy of “lights out” after 9pm (Iwata et al 2017).
In addition, involve your baby in your daily activities, and avoid the temptation to turn nighttime feedings into social events.
When you attend to your baby in the middle of the night, be soothing, but avoid engaging your baby with eye contact and conversation. Keep the lights off, and your behavior low key.
Sleep stages and sleep cycles: How do baby sleep patterns unfold over the course of the night, and when are infants most likely to awaken?
To answer this, it helps to review what adult sleep is like.
For us, sleep isn’t a single continuous state of coma-like unconsciousness. We pass through a series of sleep stages, beginning with light sleep, progressing to deep sleep, and ending with rapid eye movement sleep, or REM — the sleep stage associated with busy brain activity, dreaming, and the loss of muscle tone.
We don’t move around during REM unless we suffer from certain sleep disorders.
The whole sequence takes approximately 90-100 minutes, after which we either awaken or repeat the cycle. Sleep lab research shows that we’re especially prone to awaken during or immediately after REM (Akerstedt et al 2002).
But throughout each sleep cycle, we also experience multiple arousals — brief, partial awakenings.
These are a normal part of sleep, fleeting “check ins” that help the brain keep tabs on potential threats. If there is nothing to attract our interest or concern, the arousal process is aborted, and the brain goes back to sleep.
For infants, things are much the same.
Babies experience distinct sleep stages, including an infant version of REM, called “active sleep.”
They also experience many brief arousals during the night, fleeting moments of drowsy wakefulness that you might not even notice.
And these arousals are especially common during the baby equivalent of REM, sometimes called “active sleep” (Grigg-Damberger et al 2007; Montemitro et al 2008).
But baby sleep patterns differ in crucial ways.
Baby sleep cycles are shorter — on average, about 50-60 minutes long (Jenni and Carskadon 2000; Jenni et al 2004; Grigg-Damberger 2017). And for the youngest babies — those under 3 months of age — the average sleep cycle looks like this:
- Active sleep (REM)
- Transitional sleep
- Quiet sleep
That is, babies begin a sleep bout in REM, next switch into a sleep stage called transitional sleep, and then finally arrive at a sleep stage called “quiet sleep” (Parslow et al 2003).
Another difference is that babies spend a lot more time in REM than we do.
Whereas average adult spends only 20% of total sleep time in REM, for newborns the percentage is higher than 50% (Grigg-Damberger 2017). Time spent in REM declines as babies get older, but the change my come slowly. For some 9-month-old babies, REM still makes up 50% of their total sleep hours (Montemitro et al 2008).
But perhaps the most consequential difference for new parents is that baby sleep patterns can deceive us. During REM and transitional sleep, babies can sometimes appear to be awake.
During REM and transitional sleep, babies can sometimes appear to be awake.
As noted, we adults don’t move around during REM. We experience sleep paralysis. But for young babies — especially babies under the age of 3 months — this isn’t the case. They usually retain muscle tone, and they use it. A lot.
They twitch, wiggle, stretch, and thrash. They may frown or smile, or launch into a burst of sucking movements. They may vocalize too (Grigg-Damberger 2017; Barbeau and Weiss 2017).
So babies in REM may appear deceptively awake, and the same can be said for babies in transitional sleep. During transitional sleep, newborns become more likely to vocalize, and sometimes even open their eyes (Barbeau and Weiss 2017).
It’s really only during “quiet sleep” that young babies present us with reliable cues that they are asleep: Aside from the occasional sigh, their breathing becomes slow and regular, and they scarcely move at all. But young babies spend only a minority of their time in quiet sleep — approximately 20 minutes per sleep cycle (Grigg-Damberger 2017).
This can lead the exhausted parent to make an understandable but unfortunate mistake: You misread your baby’s cues, and end up disrupting your infant’s sleep.
It happens innocently enough.
You hear your baby whimper. You observe movement. You might even see that your baby’s eyes are open. So you bow to the inevitable, and swoop in to soothe him or her.
You start talking, or you pick your baby up.
It seems like a good idea at the time. Isn’t it better to be proactive, to jump in before your baby has become really noisy or agitated?
But your basic premise was faulty. Your baby wasn’t awake, but rather in REM or transitional sleep. Or perhaps what you mistook for waking was one of those brief arousals — a fleeting moment of drowsy wakefulness that would quickly transitioned back into sleep if you’d left your baby alone.
Either way, you’ve intervened unnecessarily, and added a night waking to the schedule that might not otherwise have happened. And you may have denied your baby the experience of falling back to sleep on his or her own, without any fuss or distress.
And you may have denied your baby the experience of falling back to sleep on his or her own, without any fuss or distress.
If you make this mistake regularly, you may be teaching your baby to turn brief arousals into full-blown waking sessions — and to expect lots of interaction with you.
To avoid this, be patient and observant before responding to your baby at night.
Get to know your baby’s quirks. And be aware that your social cues — especially the sound of your voice — can have particular powerful effect. Babies can awaken quickly when they hear us talk.
In fact, researchers note that babies “arouse more easily in response to their mother’s voice than to a smoke alarm” (Grigg-Damberger et al 2007).
Why do babies spend so much time sleeping light?
It might seem like Mother Nature made a terrible mistake. Wouldn’t it be better if our babies slept soundly and deeply all night? But REM may be important for a baby’s brain development (Siegel 2005). According to one theory, it could be a time for the brain to test its wiring — including the nerves that run to the skeletal muscles.
According to one theory, it could be a time for the brain to test its wiring — including the nerves that run to the skeletal muscles.
In addition, it’s likely that active sleep — and a tendency to awaken easily — helps protect babies from oxygen deprivation.
When a sleeping individual isn’t getting enough oxygen, it’s crucial to wake up immediately. Being slow to respond puts babies at higher risk for sudden infant death syndrome, or SIDS.
So there is a crucial survival advantage to sleeping light, and that’s what REM sleep delivers.
Researchers have demonstrated this in experiments on sleeping infants. They subjected the babies to mild reductions in oxygen. Would the infants promptly awaken?
Babies did arouse quickly — if they had been in REM sleep. But if the oxygen levels dropped while babies were in quiet sleep, the outcome was different. Babies aroused more slowly, or failed to awaken altogether (Parslow et al 2003; Richardson et al 2007).
It appears, then, that long bouts of quiet sleep could be hazardous, at least for infants young enough to be at risk for SIDS. For the first 6 months, sleeping relatively light — and being easily aroused — is a good thing. It makes babies safer.
As a result, we must be thoughtful when we’re evaluating sleep advice. A given tactic isn’t automatically desirable because it results in babies sleeping more deeply or for longer stretches of time.
On the contrary, experts recommend some practices because they support more frequent arousals in young infants.
For example, babies who are breastfed tend to experience more frequent arousals than babies who are formula-fed. Researchers suspect this is one reason why breastfed infants have lower rates of SIDS (Horne et al 2004b; Franco et al 2000).
You can read more about environmental risk factors for SIDS — and sleep practices to avoid — here.
So how much sleep do babies need?
This is a surprisingly difficult question to answer, especially for younger babies.
We know what international surveys tell us about typical baby sleep patterns. Among parents with babies under the age of 3 months, approximately 50% say their infants sleep between 13-16 hours over the course of a 24 hour day (Iglowstein et al 2003; Bruni; Netsi et al 2017; Kohyama et al 2011).
This might suggest that 13-16 hours is what most young babies need. But the surveys have limitations.
First, they are based on parental reports, which can be inaccurate. When scientists measure sleep objectively, they find disparities between parental perceptions and reality. Parents tend to overestimate total sleep duration, and underestimate the frequency of night wakings (Goodlin-Jones et al 2001; Galland et al 2016).
Second, even if we could be certain about the numbers, the numbers wouldn’t constitute proof about what babies need. Maybe the babies in these surveys aren’t getting enough sleep. Or maybe they’re getting too much.
What’s needed is research that addresses the health consequences of sleep, and unfortunately such research is in short supply (Paruthi et al 2016).
Citing this lack of evidence, the American Academy of Sleep Medicine has declined to issue any specific recommendations about sleep duration for babies under the age of 4 months (Paruthi et al 2016).
For older babies (4-12 months), the Academy notes that some studies have found links between emotional or behavioral problems and short sleep. On this basis, the Academy advises that 4- to 12-month-old babies are at a lower risk for problems if they get between 12-16 hours of sleep every 24 hours (Paruthi et al 2016).
For more information, see my page about baby sleep requirements, as well as this Parenting Science sleep chart.
What about sleeping through the night? When do babies begin sleeping in long, uninterrupted nighttime bouts?
Understandably, parents want their babies to “sleep through the night.” But, as we’ve already noted, nobody truly sleeps through the night — not in the sense of remaining in a constant sleep state for hours on end.
Instead, what’s normal — both for babies and adults — is to experience many partial arousals throughout the night, and to occasionally wake up, if only very briefly.
Researchers have captured this in video recordings: Babies under the age of 12 months awaken, on average, 3-4 times a night (Goodlin-Jones et al 2001).
So it isn’t realistic to expect your baby to stop awakening at night. Nor would that be a good idea. As we’ve seen, arousals serve an important function.
Instead, a more reasonable goal is for your baby to settle down at night for at least 5 hours at a stretch. When your baby experiences an arousal, he or she quickly falls back to sleep — without your assistance.
That’s what’s really going on when parents say their babies sleep for long periods of time. The infants are experiencing normal arousals and night wakings, but their parents aren’t aware of these interruptions. Babies are staying quiet, and returning to sleep on their own.
So when does this happen? At what age do babies keep quiet for at least 5 hours? Between, say, midnight and 5am?
The answer is that it varies.
Some babies achieve this milestone at two months postpartum. But most babies don’t get there until 4-6 months, or even later.
But most babies don’t get there until 4-6 months, or even later.
We can see this pattern in a study that tracked 75 American infants over time. Jacqueline Henderson and her colleagues asked their parents to keep sleep diaries — 6 days per month — throughout the first 12 months postpartum.
Most parents didn’t record long stretches of sleep, not when their babies were very young. At two months, only 8% of parents reported that their babies were sleeping uninterrupted between the hours of midnight and 5am.
But by 4 months, approximately 50% of parents made this claim. And by 5-6 months, the majority of parents — about 70% — said their babies were sleeping without any perceived interruptions during these potentially crucial hours. At 12 months, the percentage had increased to 84% (Henderson et al 2010).
But what if your baby isn’t a “good sleeper”? Is there something you can do to improve baby sleep patterns?
We’ve already seen that you can help your baby develop mature circadian rhythms.
If your baby isn’t sleeping well at night, make sure your baby is getting the right environmental cues — bright light during the day, darkness before bedtime, and a boring, peaceful nighttime atmosphere. This will help your baby get sleepy at the right time — and spend more time sleeping at night.
We’ve also seen that there are mistakes parents can make during the night — mistakes that can prevent babies from learning to fall back to sleep on their own.
If you can resist the urge to interact with a baby who seems to be waking — and wait to make sure the baby isn’t really asleep, or about to go back to sleep without your assistance — you’ll help your baby learn to sleep for longer periods.
In addition, you can troubleshoot for common sleep problems. Check out my overview of the causes of infant sleep problems, as well as my Parenting Science article about illnesses and physical ailments that can disrupt baby sleep patterns.
And keep these tips in mind:
1. Remember that soothing, supportive, emotional communication is the key to getting babies settled.
Remember that soothing, supportive, emotional communication is the key to getting babies settled.
Whether your baby shares a room with you, or sleeps elsewhere, you can make it a point reassure and calm your baby before bedtime. Being sensitive and responsive to your baby’s moods is called “emotional availability,” and studies show that it has an important impact on the way infants sleep. When parents show emotional availability at bedtime, babies wind down more easily, and they experience fewer sleep problems (Teti et al 2010; Jian and Teti 2015).
2. If you baby doesn’t seem to be sleepy at bedtime, don’t try to force it.
Getting pushy doesn’t make babies any sleepier. If anything, it makes them more excitable. And you don’t want your baby to associate bedtime with conflict. That can be a difficult lesson to unlearn!
So instead, try the technique known as “positive routines and faded bedtime,” which you can read about here. It’s a method for resetting your infant’s inner clock, and overcoming bedtime resistance.
3. If your baby seems to cry inconsolably, or seems otherwise distressed, discuss this with your doctor.
It’s not clear if excessive, inconsolable crying disrupts baby sleep patterns, but it definitely stresses out parents. And when parents are stressed out, they suffer more sleep problems. Read more about inconsolable crying and its possible causes in this Parenting Science article.
4. Watch out for those late naps.
Naps are good for babies, but poorly-timed naps can cause trouble. A long snooze in the late afternoon can delay drowsiness for hours, wrecking havoc with your baby’s bedtime.
References: Baby sleep patterns
For a complete list of the studies and publications cited in this article, click here.
Written content last modified 4/2018; new image added 3/2022
image of father holding sleepy infant by monkeybusinessimages / istock
Small portions of the text appeared in an older article, “Baby sleep patterns: A guide for the science minded,” last published in 2014.
THE SCIENCE OF SLEEP - articles from the experts at the Mother and Child Clinic
Advice #1 Don't try to get your baby to sleep through the night.
Features of the nervous and digestive system of a child of the first year of life, especially if he is breastfed, do not allow him to sleep all night.
In the first months of life, he can sleep at night without waking up for no more than five hours. Usually the interval between feedings is from 2.5 to 5 hours. For a complete nutrition of the baby, his daytime sleep should not exceed 2-3 hours. Only after 6 months do babies mature physiologically to sleep for 6-8 hours without waking up.
Advice #2 Don't write off baby's restless behavior as "colic, teeth, growth spurts".
Parents often explain the crying and restlessness of the baby before and during sleep with colic, teeth, or the transition to a new stage of development. In fact, the reason in most cases lies elsewhere. Try to record all the intervals of sleep and wakefulness during the day, as well as the behavior of the child during these periods. Analyze whether the baby is “walking” - at this age it is extremely important not to exceed the norms for wakefulness, and also to sleep the required number of hours so that fatigue from lack of sleep does not accumulate. In addition, sometimes children are sensitive to errors in their mother's diet. Observe, change those factors that disturb the baby, and the child will probably sleep better.
Try to record all the intervals of sleep and wakefulness during the day, as well as the behavior of the child during these periods. Analyze whether the baby is “walking” - at this age it is extremely important not to exceed the norms for wakefulness, and also to sleep the required number of hours so that fatigue from lack of sleep does not accumulate. In addition, sometimes children are sensitive to errors in their mother's diet. Observe, change those factors that disturb the baby, and the child will probably sleep better.
Tip #3 Don't let your child get tired.
It is important for a mother to learn to recognize the first signs of fatigue and “catch” these moments in time to put the baby to bed.
Tip #4 Set up a sleep ritual.
The rhythm of life in the city, unfortunately, implies that in the evening, when it is time for the child to go to bed, the whole family finally gathers at home after work, the baby’s emotions “go off scale”, albeit positive ones..jpg) It is important to adjust the child's regimen to the routine in the family, so that in the evening a quiet calm atmosphere is maintained in the house and the set time for falling asleep is observed. The ritual can be as follows: after bathing, give the baby a light relaxing massage, feed, turn on white noise or sing a lullaby, put your favorite soft toy next to it, and put the baby to bed. The ritual of repetitive actions will set the child up for sleep and help form the right habit.
It is important to adjust the child's regimen to the routine in the family, so that in the evening a quiet calm atmosphere is maintained in the house and the set time for falling asleep is observed. The ritual can be as follows: after bathing, give the baby a light relaxing massage, feed, turn on white noise or sing a lullaby, put your favorite soft toy next to it, and put the baby to bed. The ritual of repetitive actions will set the child up for sleep and help form the right habit.
Lack of sleep can lead to chronic fatigue and disruption of the child's nervous system. Scientific studies show that children who sleep less than the norm for their age have an increased risk of hyperactivity and attention deficit disorder .
Advice #5 Try to adjust the sleep time to the child's biological rhythms.
Baby's biorhythms are programmed for daylight hours, that is, for early bedtime and early rise. As practice shows, children adjust to daylight hours, and morning awakening has almost no effect on going to bed. So basically the kids wake up between 6.00-8.00. Sleep experts recommend that babies, especially those older than 4 months, be put to bed between 19until 9 pm (in summer, when it gets dark later, you need to darken the room with curtains). So you can avoid fatigue and lack of sleep. To re-arrange your baby for early bedtime, move your bedtime 15 minutes earlier each day.
So basically the kids wake up between 6.00-8.00. Sleep experts recommend that babies, especially those older than 4 months, be put to bed between 19until 9 pm (in summer, when it gets dark later, you need to darken the room with curtains). So you can avoid fatigue and lack of sleep. To re-arrange your baby for early bedtime, move your bedtime 15 minutes earlier each day.
Tip #6 Get outside more.
Many children sleep much better outside in a stroller. There are children who sleep little and restlessly at home, and sleep soundly for hours in a stroller. This is normal, so stock up on audiobooks and a thermos of tea and go out on your "distance" in the park.
Tip #7 Don't try to introduce complementary foods early for a good night's sleep.
This can backfire as the baby's immature digestive system is not ready to digest "adult" food.
Tip #8 Sing lullabies to your baby.
Even if it seems to you that you are deprived of vocal abilities, sing to your child. Psychologists say that the mother's voice and her heartbeat are the main soothing sounds for the baby. Studies of infants' responses to music have shown that because infants' hearts beat faster than adults, they enjoy the faster rhythm of musical compositions. They also prefer female vocals and high timbre.
Psychologists say that the mother's voice and her heartbeat are the main soothing sounds for the baby. Studies of infants' responses to music have shown that because infants' hearts beat faster than adults, they enjoy the faster rhythm of musical compositions. They also prefer female vocals and high timbre.
Tip #9 Create all the conditions in the bedroom.
Let the very atmosphere in the room set you up for relaxation. Ventilate it well before going to bed, and also darken it with curtains and try to ensure silence.
Tip #10 Cultivate good habits.
Try not to let the baby fall asleep on the breast, so that from the very beginning he will separate feeding and sleep. Place your baby in your crib regularly so that he gets used to having his own place to sleep. It’s good if he regularly spends some part of the night at his place.
Strictly follow the age norms of sleep and wakefulness - these are the main conditions for sound sleep, which means good mood and proper development of the baby.
Tips
pediatrician
Svetlana
Vladimirovna
Petina, Chief
doctor of the children's center of the clinic "Mother
and child" Kuntsevo
1. Consider your child's needs
Many babies sleep well
after bathing,
however, there are babies,
on whom a bath,
even with the addition of relaxing
herbs, acts,
on the contrary, exciting. Be guided by your own
child - if
after a bath his sleep
as if by hand,
postpone bathing
in the morning or afternoon.
2. Consult physicians
If your child
is not enough and restless
sleeps, then it is worth it to consult
with a pediatrician and a neurologist, as well as
, make the necessary examinations,
For example, ultrasound
brain,
To check
intracranial pressure. Doctors will evaluate
Doctors will evaluate
psychosomatic
baby status and
his psychomotor
development.
3. Prepare
room
First month of life
child keep the temperature in the bedroom
24-25 °C. Then you can reduce this figure to 20-22 ° C.
Make sure that the cot is not standing in a
draft, do not turn on the air conditioner.
Mattress choose
rigid, with natural filling
coconut fiber
.
90,000 bad habits and sleep-Baby-sleep.ru04/17/2019
11745
17
How to establish a dream
Irina Zavalko
Irina Zavalko
Neurologist-Summar senior sleep consultant for children and adults
Mom of two children
Many children, when falling asleep or in the superficial stages of sleep, perform actions that seem to parents to be bad habits: pulling on their navel, twisting their mother's hair around their finger, rocking on all fours, grinding their teeth.
Part of these actions the child performs consciously and could (with sufficient development of control over his actions and desire) not to do, while others are involuntary movements that occur during sleep or during the transition to sleep (falling asleep).
These activities often annoy or disturb parents. Regardless of whether it's just a habit or an involuntary movement, an important pattern works for them. Their frequency and duration increase in the following situations:
- Stressful events (moving, divorce of parents, birth of another child in the family).
- Increased emotional stress during wakefulness (even going to the mall or to a developmental activity can be redundant for the baby).
- Inappropriate sleep pattern for the child, which leads to prolonged falling asleep.
Child's crisis calendar
Before dealing with an unwanted action, reduce the emotional burden, help the child survive stress and adjust his sleep schedule.
How to help a child?
A child before going to bed twists his mother's hair around his finger or pulls at the navel - at first glance, the actions are harmless. But they can become a habit and become an association for falling asleep. Several times a couple of minutes this can be safely endured, but when does the child get used to doing this for a long time with each laying down? Especially if he falls asleep for a long time. Of course, you can act directly: simply forbid the baby to twist his hair or close and not let him touch the navel.
But there is a more effective and more pleasant strategy. Replace an unpleasant action with another: buy a doll with long hair or a lion with a long mane and offer to switch to this hair. Find a toy, diaper, or just a washcloth that is comfortable to fiddle with. Offer this item to your baby each time you put it down. So you gradually replace one ritual action with another. An important point: for safety reasons, a child younger than 6-7 months. you can’t put a soft toy in the crib, and up to 2-3 years old toys with small parts that the baby can tear off or bite off are excluded, as well as ropes and ribbons with free ends longer than 20 cm.
you can’t put a soft toy in the crib, and up to 2-3 years old toys with small parts that the baby can tear off or bite off are excluded, as well as ropes and ribbons with free ends longer than 20 cm.
Thumb sucking
The need to suck in children fades around 2 years of age and sometimes persists longer. Sucking often helps babies relax and fall asleep. This is why a baby may suck on a finger, the edge of a blanket, or a toy. It may start on its own or as a reaction to the separation of food and sleep, or weaning from a pacifier.
This habit, although it may be unpleasant for parents, is actually not harmful. Research has shown that nonnutritive sucking during sleep (i.e., sucking for other than nutritional purposes, such as breast or bottle sucking) promotes brain development in young children and reduces the risk of the dangerous sudden infant death syndrome in the first year of life[1].
Also, sucking on a finger or other object may help the child fall asleep faster when lying down and fall asleep without the help of parents during nighttime awakenings.
Sucking on various objects can lead to malocclusion, but these problems usually disappear soon after the baby stops sucking anything. Like licking objects and fingers while awake, sucking can increase the risk of gastrointestinal infections and oral thrush. After the age of 2–3 years, suckling doubles the risk of otitis media.
Weigh the pros and cons and decide whether it is right for you to wean your baby from thumb sucking. Maybe this will allow the whole family to sleep better? Or is it better for you to spend time and effort and wean the baby? Remember that any sudden change in the conditions and ritual of falling asleep can cause a protest in the child.
If your baby is used to sucking part of a toy, you can arrange a new place for her to sleep and always put her there before going to bed, because "the bunny likes to sleep in her comfortable bed." Buy your baby a new "adult blanket" that will not be as comfortable to suck on, and have a growing-up celebration when the old baby blanket "goes" to some baby. Take out your finger when falling asleep, take the baby's hand in yours and tell him a nursery rhyme, do a play massage.
Take out your finger when falling asleep, take the baby's hand in yours and tell him a nursery rhyme, do a play massage.
Masturbation
Parents may be even more frightened if the child rubs the genitals, that is, masturbates, before falling asleep. I hasten to reassure you: masturbation before puberty does not have a sexual connotation, the baby is just interested in exploring and touching his genitals. It causes pleasant sensations and therefore can be fixed in a habit.
In the XIX century. masturbation began to be sharply condemned, which was fixed in the ideas of people. However, modern psychology and medicine consider masturbation to be normal. Therefore, when raising a child, it is recommended not to prohibit the process itself, but only to teach the child that it is not worth pulling the genitals in the presence of other people.
Rhythmic movements
Some children before falling asleep and even during the superficial stages of sleep get up on all fours in bed and begin to rock back and forth, sometimes the child rubs his groin on the bed, and relatives begin to think that the baby is masturbating like this (although this is not so ). Other babies shake their head or their whole body from side to side, or even bang their heads against the pillow or the side of the crib, often causing the mother to be frightened.
Other babies shake their head or their whole body from side to side, or even bang their heads against the pillow or the side of the crib, often causing the mother to be frightened.
The baby performs these movements involuntarily. Somnologists call such actions rhythmic movements during sleep or falling asleep, or yactation. It is not known exactly why babies do this, one of the opinions is that the child helps himself to relax before going to bed and fall asleep, as if rocking himself.
Rhythmic movements are a normal phenomenon for children of the first years of life: about 70% of babies under one year old at least sometimes behave this way when falling asleep. With age, the prevalence of this phenomenon decreases and after 4 years only every 10th child behaves this way before going to bed. Rhythmic movements are not dangerous, and often, on the contrary, are useful, as they help the baby fall asleep on his own.
All parents need to do is to secure the child's sleeping area so that the child does not fall out of bed, become entangled or injured during these movements. Most often, parents worry that the child will injure the head if it hits the bed rails or the wall. This happens very rarely: no injuries or concussions occur in a child during rhythmic movements, only in the case of very pronounced beats, when the baby knocks his head against the wall with great intensity, it is worth fixing something soft at the site of impact or putting a soft one on the child before going to bed. head helmet.
Most often, parents worry that the child will injure the head if it hits the bed rails or the wall. This happens very rarely: no injuries or concussions occur in a child during rhythmic movements, only in the case of very pronounced beats, when the baby knocks his head against the wall with great intensity, it is worth fixing something soft at the site of impact or putting a soft one on the child before going to bed. head helmet.
In some cases, rhythmic movements can become a kind of association for falling asleep. If the baby falls asleep for a long time and at the same time sways on all fours or hits his head on the pillow, evaluate how suitable his sleep schedule is. For example, the reason may be in going to bed too early, when the child is not yet ready to sleep.
Rhythmic movements may appear or intensify against the background of a stressful situation (moving, divorce of parents, etc.), then it is necessary to help the child "digest" this situation on his own or with the help of a psychologist.
Teeth grinding
Another "bad habit" is bruxism . Parents are often frightened and sometimes annoyed by the unpleasant sound of teeth grinding that occurs shortly after falling asleep and sometimes repeats itself in the middle of the night. This phenomenon is called bruxism and also occurs involuntarily. Among children aged 2–3 years, every sixth teeth grind in their sleep, with age, many “outgrow” this phenomenon, and in most children by the age of 6–7 years, bruxism disappears by itself, while in some children it persists and may continue or resume in adulthood. .
Bruxism is also harmless, except in rare cases when it leads to abrasion of tooth enamel or provokes frequent awakenings.
It is widely believed that worms (parasitic worms that live in the intestines) cause children to grind their teeth while sleeping, but studies do not support this. According to scientific data, some malocclusion, interrupted sleep, and emotional overload lead to bruxism.
Therefore, if your child does not grind his teeth in his sleep very often, and you do not see a clear abrasion of the teeth, you can not worry and wait until he outgrows it. If bruxism still bothers you and your baby, contact your dentist to check the bite and the integrity of the enamel. When erasing teeth, the doctor can make a special protective cover - a mouthguard, which is put on the teeth during sleep. Try to reduce emotional stress and work out possible stressful situations. If your baby has adenoids in addition to bruxism, it is worth checking to see if he has pauses in breathing during sleep (apnea), which disturb sleep and provoke bruxism.
If you wake up frequently during the night, the first thing to do is to improve your sleep by contacting a sleep consultant.
And one more universal, but not always effective advice is to chew hard (for example, carrots) before going to bed. This advice is related to the notion that bruxism can cause the masticatory muscles to become underactive when chewing soft and pureed foods in modern humans.