How to treat sticky eyes
Conjunctivitis symptoms & treatments - Illnesses & conditions
See all parts of this guide Hide guide parts
- 1. About conjunctivitis
- 2. Symptoms of conjunctivitis
- 3. Causes of conjunctivitis
-
4.
Diagnosing conjunctivitis
- 5. Treating conjunctivitis
- 6. Complications of conjunctivitis
About conjunctivitis
Conjunctivitis is a common condition that causes redness and inflammation of the thin layer of tissue that covers the front of the eye (the conjunctiva).
People often refer to conjunctivitis as red eye.
Other symptoms of conjunctivitis include itchiness and watering of the eyes, and sometimes a sticky coating on the eyelashes (if it's caused by an allergy).
Read more about the symptoms of conjunctivitis
Conjunctivitis can affect one eye at first, but usually affects both eyes after a few hours.
What causes conjunctivitis?
The conjunctiva can become inflamed as a result of:
- a bacterial or viral infection – this is known as infective conjunctivitis
- an allergic reaction to a substance such as pollen or dust mites – this is known as allergic conjunctivitis
- the eye coming into contact with things that can irritate the conjunctiva, such as shampoo or chlorinated water, or a loose eyelash rubbing against the eye – this is known as irritant conjunctivitis
Read more about the causes of conjunctivitis
Treating conjunctivitis
Treatment isn't usually needed for conjunctivitis, because the symptoms often clear up within a couple of weeks. If treatment is needed, the type of treatment will depend on the cause. In severe cases, antibiotic eye drops can be used to clear the infection.
Irritant conjunctivitis will clear up as soon as whatever is causing it is removed.
Allergic conjunctivitis can usually be treated with anti-allergy medications such as antihistamines. If possible, you should avoid the substance that triggered the allergy.
It's best not to wear contact lenses until the symptoms have cleared up. Any sticky or crusty coating on the eyelids or lashes can be cleansed with cotton wool and water.
Washing your hands regularly and not sharing pillows or towels will help prevent it spreading.
Read more about treating conjunctivitis
See your GP immediately if you have:
- eye pain
- sensitivity to light (photophobia)
- disturbed vision
- intense redness in one eye or both eyes
- a newborn baby with conjunctivitis
Eye problems self-help guide
Find out more about your symptoms, when you can use self-care, and what to do if your condition worsens and you need medical help.
Self-help guide: Eye problems
Work and school
Public Health Scotland (PHS) advises that you don't need to stay away from work or school if you or your child has conjunctivitis, unless you (or they) are feeling particularly unwell.
If there are a number of conjunctivitis cases at your child's school or nursery, you may be advised to keep them away until their infection has cleared up.
Generally, adults who work in close contact with others, or share equipment such as phones and computers, shouldn't return to work until the discharge has cleared up.
Complications
Conjunctivitis can be a frustrating condition – particularly allergic conjunctivitis – but in most cases it doesn't pose a serious threat to health.
Complications of conjunctivitis are rare, but when they do occur they can be serious and include:
- a severe case of allergic conjunctivitis can lead to scarring in the eye
- in cases of infective conjunctivitis, the infection can spread to other areas of the body, triggering more serious secondary infections, such as meningitis
Read more about the complications of conjunctivitis
Symptoms of conjunctivitis
The symptoms of conjunctivitis will depend on what's causing the condition.
However, the two main symptoms are usually:
- eye redness – as a result of the inflammation and widening of the tiny blood vessels in the conjunctiva (the thin layer of cells covering the front of the eyes)
- a discharge – the conjunctiva contains thousands of cells that produce mucus and tiny glands that produce tears – inflammation causes the glands to become overactive, so that they produce more water and mucus
Only one eye tends to be affected at first, but symptoms usually affect both eyes within a few hours.
Infective conjunctivitis
If you have infective conjunctivitis, you may also have:
- a burning sensation in your eyes
- a feeling of grit in your eyes
- a sticky coating on the eyelashes – usually when you first wake up in the morning
- an enlarged lymph node (gland) in front of the ear
Allergic conjunctivitis
You may have itchy eyes if you have allergic conjunctivitis.
The pattern of symptoms for allergic conjunctivitis depends on the substance you're allergic to.
Allergies to pollen (hay fever) occur during certain parts of the year. You can have an allergy to:
- tree pollen, released during spring
- grass pollen, released during the end of spring and beginning of summer
- weed pollen, released any time from early spring to late autumn
It's highly likely that the pollen will also cause other symptoms, such as sneezing and a runny or blocked nose.
Allergies to dust mites or animal fur cause symptoms throughout the year. Both eyes are usually affected and you may find the symptoms worse in the morning.
Some people develop an allergy to eye drops. This is known as contact dermatoconjunctivitis and it can also affect your eyelids, causing them to become dry and sore.
Some people are allergic to wearing contact lenses, which is known as giant papillary conjunctivitis. The symptoms progress much more slowly and you may also develop small spots on the inside of your upper eyelids. This type of conjunctivitis carries a high risk of complications, so you need to seek medical advice as soon as possible
When to seek medical advice
Most cases of conjunctivitis aren't a cause for concern, but you should contact your GP if you think you have it, particularly if you think it's related to wearing contact lenses.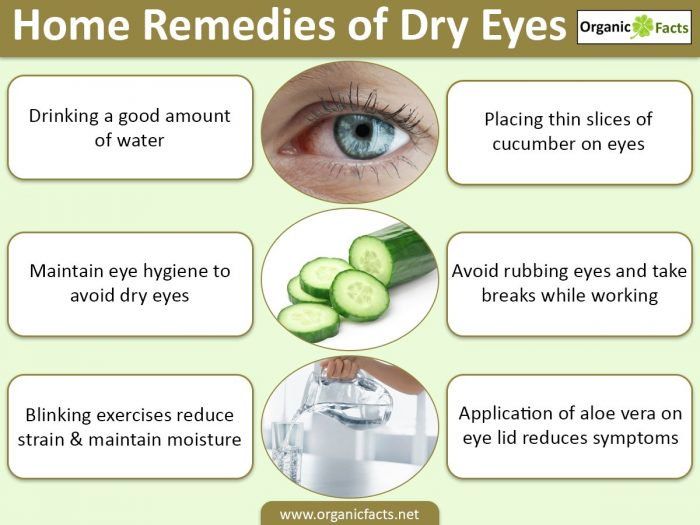
Your GP can check whether there's a more serious underlying cause of your symptoms.
When to seek immediate medical advice
The following symptoms could be the sign of a more serious eye condition:
- pain in your eyes
- sensitivity to light (photophobia)
- disturbed vision
- intense redness in one eye or both eyes
Contact your GP immediately if you experience any of these symptoms. If this isn't possible, visit your nearest accident and emergency (A&E) department.
Causes of conjunctivitis
Conjunctivitis is a condition that occurs when the conjunctiva (a thin layer of cells covering the front of your eyes) becomes inflamed.
The three most common causes of this inflammation are:
- infection (infective conjunctivitis)
- an allergic reaction (allergic conjunctivitis)
- something irritating the conjunctiva, such as a loose eyelash (irritant conjunctivitis)
These are discussed in more detail below.
Infective conjunctivitis
Eye infections are most commonly caused by:
- bacteria – for example, the strains of bacteria that often cause lung and ear infections
- a virus – most commonly an adenovirus that may also cause a sore throat and high temperature (fever)
- sexually transmitted infections (STIs) – such as chlamydia or gonorrhoea
Viral conjunctivitis causes a watery discharge, while the discharge from bacterial conjunctivitis contains pus. An eye swab can also determine the cause of the infection (read more about diagnosing conjunctivitis).
Spreading the infection
You're more likely to develop infective conjunctivitis if you've been in close contact with someone who's already infected with it.
It's therefore very important to wash your hands thoroughly after coming into contact with anyone who has infective conjunctivitis. You should also avoid sharing pillows or towels with anyone with the infection.
Risk groups
You may be more at risk of getting infective conjunctivitis if:
- you're old or young – it's more common in children and the elderly, possibly because children come into contact with more infections at school, and elderly people may have a weaker immune system
- you've recently had an upper respiratory tract infection – such as a cold
- you have diabetes or another condition that weakens your immune system – as you may be more vulnerable to infections
- you're taking corticosteroids (steroids) – which can weaken your immune system
- you have blepharitis (inflammation of the rims of the eyelids) – which can be caused by a bacterial infection and may lead to conjunctivitis
- you've been in a crowded place – such as a busy train
Allergic conjunctivitis
Allergic conjunctivitis is caused when your eyes come into contact with an allergen (a particular substance that causes your immune system to react abnormally). This is known as an allergic reaction.
This is known as an allergic reaction.
There are four main types of allergic conjunctivitis:
- seasonal allergic conjunctivitis
- perennial allergic conjunctivitis
- contact dermatoconjunctivitis
- giant papillary conjunctivitis
Seasonal and perennial conjunctivitis
Seasonal and perennial allergic conjunctivitis are usually caused by:
- pollen from grass, trees or flowers
- dust mites
- flakes of dead animal skin
These types of conjunctivitis are more common in people who also have other allergies, such as asthma, and often occur with allergic rhinitis.
Contact dermatoconjunctivitis
Contact dermatoconjunctivitis is usually caused by eye drops, but it can also be caused by make-up or chemicals.
Giant papillary conjunctivitis
Giant papillary conjunctivitis is caused by:
- contact lenses
- stitches used in eye surgery
- a prostheses (artificial) part of the eye that's fitted during eye surgery
Giant papillary conjunctivitis is estimated to affect around 1-5% of people who use soft contact lenses and 1% of people who use hard contact lenses.
Irritant conjunctivitis
Irritant conjunctivitis can have a wide range of potential causes. Some common causes include:
- chlorinated water used in swimming pools
- shampoo
- a stray eyelash rubbing against the conjunctiva
- smoke or fumes
Diagnosing conjunctivitis
Your GP should be able to diagnose conjunctivitis by asking about your symptoms and examining your eyes.
Describing how your conjunctivitis started can help your GP diagnose which type it is and decide whether it needs to be treated.
The most common symptoms of infective conjunctivitis are sticky, red and watery eyes. However, infective conjunctivitis can sometimes be confused with other types of conjunctivitis, which are treated differently.
Swab test
Your GP may suggest further tests, such as a swab test, if your conjunctivitis hasn't responded to treatment, or to help decide what treatment to use.
A swab looks similar to a cotton bud. It's used to collect a small sample of mucus from your infected eye, which is sent to a laboratory to find out the cause of your conjunctivitis.
It's used to collect a small sample of mucus from your infected eye, which is sent to a laboratory to find out the cause of your conjunctivitis.
If your symptoms are severe or don't respond to treatment, you may need to see an eye specialist (ophthalmologist).
Other conditions
Most cases of conjunctivitis clear up within one to two weeks without needing any medical treatment. In some cases, it can last for longer than two weeks, which is known as persistent infective conjunctivitis.
If you have any unusual symptoms, such as severe pain, blurred vision or sensitivity to light, it may mean that you have a more serious condition.
If you have any of these symptoms, it's very important to seek medical assistance immediately, either by contacting your GP or going to your nearest hospital.
Other more serious conditions include:
- acute glaucoma – a rare form of glaucoma that causes a painful build-up of pressure in your eye
- keratitis – where the cornea (the clear layer at the front of your eye) becomes swollen and develops open sores
- iritis – a type of uveitis (swelling of the middle layer of your eye) that causes pain, headaches and watery eyes
Newborn babies
Contact your GP straight away if you think your baby may have infective conjunctivitis (also called neonatal conjunctivitis).
If this isn't possible, call NHS 24's '111' service or your local out-of-hours service. Your GP will examine your baby closely to see if they have sticky eyes or infective conjunctivitis.
All newborn babies with infective conjunctivitis must be referred to an eye specialist straight away for treatment.
Read more about the symptoms of infective conjunctivitis
Treating conjunctivitis
The recommended treatment for conjunctivitis will depend on whether it's caused by infection, an allergic reaction or an irritant, such as a stray eyelash.
Each treatment option is discussed in more detail below.
Infective conjunctivitis
Most cases of infective conjunctivitis don't need medical treatment and clear up in one to two weeks.
Self care
There are several ways you can treat infective conjunctivitis at home. The advice below should help ease your symptoms.
- Remove your contact lenses – if you wear contact lenses, take them out until all the symptoms of the infection have gone; don't re-use old lenses after the infection has gone because they could be a potential source of re-infection; always use new lenses, solutions and cases after an infection.

- Use lubricant eye drops – these are available over the counter at pharmacies or they may be prescribed for you; they may help ease any soreness and stickiness in your eyes; always follow the manufacturer’s instructions.
- Gently clean away sticky discharge from your eyelids and lashes using cotton wool soaked in water.
- Wash your hands regularly – this is particularly important after touching your eyes and will stop the infection spreading to others.
Antibiotics
Antibiotics aren't usually prescribed for infective conjunctivitis because it usually clears up by itself and there's a very low risk of complications for untreated conjunctivitis.
However, if the infection is particularly severe or it has lasted for more than two weeks, you may be prescribed antibiotics. Some schools or playgroups may insist that a child is treated with antibiotics before they can return, although this is rare.
Chloramphenicol and fusidic acid are the two main types of antibiotics that may be prescribed.
Chloramphenicol
Chloramphenicol is usually the first choice of antibiotic and comes in the form of eye drops. It's available without a prescription from pharmacies to treat bacterial conjunctivitis.
Chloramphenicol needs to be used carefully to get the best results, so make sure you follow the advice of your pharmacist about how and when to use it, or check the patient information leaflet that comes with the medication so you know how to use it properly.
If eye drops aren't suitable for you, you may be prescribed the antibiotic as an eye ointment instead.
Fusidic acid
Fusidic acid may be prescribed if chloramphenicol isn't suitable for you. It's often better for children and elderly people because it doesn't need to be used as often. It's also the preferred treatment for pregnant women.
Like chloramphenicol, fusidic acid comes in the form of eye drops and should be used as advised by your doctor or as described in the instructions that come with the medication.
Side effects
Eye drops can briefly cause blurred vision. Avoid driving or operating machinery straight after using eye drops.
Chloramphenicol and fusidic acid can also cause other side effects, such as a slight stinging or burning sensation in your eye, although this shouldn't last long.
Further treatment
It's very important to go back to your GP if you still have symptoms after two weeks. You should also contact your GP immediately if you experience any of the following symptoms:
- eye pain
- sensitivity to light (photophobia)
- loss of vision
- intense redness in one eye or both eyes
Your GP may recommend that you're tested for sexually transmitted infections (STIs). Some STIs, such as chlamydia, can cause infective conjunctivitis. If this is the case, your symptoms may last for several months.
Allergic conjunctivitis
Your treatment will depend on the type of allergic conjunctivitis you have.
The four main types of allergic conjunctivitis are:
- seasonal conjunctivitis – typically caused by an allergy to pollen
- perennial conjunctivitis – usually caused by an allergy to dust mites or pets
- contact dermatoconjunctivitis – usually caused by an allergy to eye drops or cosmetics
- giant papillary conjunctivitis – usually caused by an allergy to contact lenses
Whatever the cause, you'll find that some self-help methods can ease your symptoms.
Self care
If you have allergic conjunctivitis, you can follow the guidelines below to treat your condition at home.
- If you wear contact lenses, take them out until all the signs and symptoms of the conjunctivitis have gone.
- Don't rub your eyes, even though they may be itchy. Rubbing your eyes can make your symptoms worse.
- Place a cool compress over your eyes. Wetting a flannel with cool water and holding it over your eyes will help ease your symptoms.
- Avoid exposure to the allergen, if possible.
Seasonal and perennial allergic conjunctivitis
If you have seasonal or perennial conjunctivitis, you may be prescribed the following medicines:
- antihistamines
- mast cell stabilisers
- corticosteroids
These are described in more detail below.
Antihistamines
If allergic conjunctivitis needs rapid relief, your GP will probably prescribe a medicine known as an antihistamine.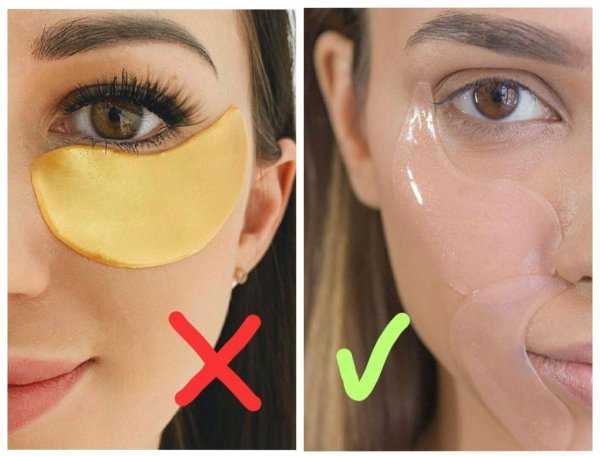
Antihistamines work by blocking the action of the chemical histamine, which the body releases when it thinks it's under attack from an allergen. This prevents the symptoms of the allergic reaction occurring.
Antihistamine eye drops
You may be prescribed antihistamine eye drops, such as:
- azelastine (not suitable for children under four years of age)
- emedastine (not suitable for children under three years of age)
- ketotifen (not suitable for children under three years of age)
- antazoline with xylometazoline (Otrivine-Antistin, not suitable for children under 12 years of age)
Antazoline with xylometazoline (Otrivine-Antistin) is also available over the counter from pharmacies without prescription. Always follow the manufacturer’s instructions.
If you're pregnant or breastfeeding, some antihistamine eye drops may not be suitable. Speak to your GP for advice.
Oral antihistamines
You may be prescribed an antihistamine such as:
- cetirizine
- fexofenadine
- loratadine
You'll usually only have to take an antihistamine once a day.
If possible, oral antihistamines shouldn't be taken if you're pregnant or breastfeeding. Speak to your GP for advice.
Although new antihistamines shouldn't make you drowsy, they may still have a sedating effect. This is more likely if you take high doses or drink alcohol while you're taking antihistamines.
Mast cell stabilisers
Mast cell stabilisers are an alternative type of medicine. Unlike antihistamines, they won't provide rapid symptom relief, but they are better at controlling your symptoms over a longer period of time.
It may take several weeks to feel the effects of a mast cell stabiliser, so you may also be prescribed an antihistamine to take at the same time.
Mast cell stabilisers that are commonly prescribed in the form of eye drops include:
- lodoxamide
- nedocromil sodium
- sodium cromoglicate
Corticosteroids
If your symptoms of allergic conjunctivitis are particularly severe, you may be prescribed a short course of topical corticosteroids (a cream, gel or ointment). However, these aren't usually prescribed unless absolutely necessary.
However, these aren't usually prescribed unless absolutely necessary.
Giant papillary conjunctivitis
As giant papillary conjunctivitis is usually caused by contact lenses, the symptoms often clear up after you stop wearing them. The spots that form on the inside of your upper eyelid may last slightly longer.
If you develop giant papillary conjunctivitis as a result of recent eye surgery, you'll be immediately referred to an ophthalmologist. This is so that your eyes can be carefully monitored and the most effective treatment given.
Irritant conjunctivitis
Most cases of irritant conjunctivitis don't need any treatment, as the condition should clear up once the irritant is removed from the eye.
An exception to this is if your eyes were exposed to harmful substances such as bleach or acid. This is usually regarded as a medical emergency and you'll need to be admitted to hospital so your eyes can be washed out with saline solution.
Complications of conjunctivitis
Complications of conjunctivitis depend on whether the condition is an infection (infective conjunctivitis) or an allergic reaction (allergic conjunctivitis).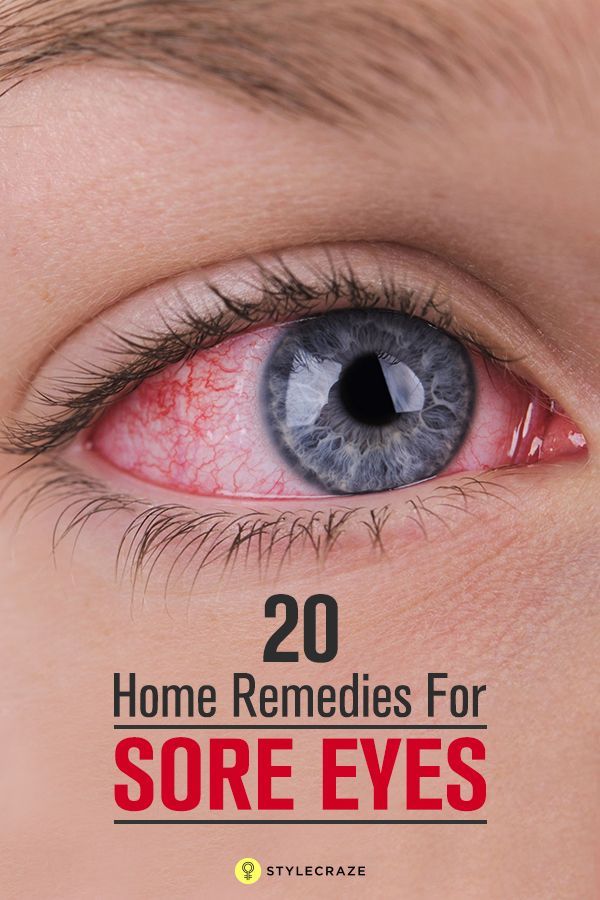
Infective conjunctivitis
If conjunctivitis has been caused by a sexually transmitted infection (STI), particularly chlamydia, the infection may last several months, rather than weeks.
Infective conjunctivitis caused by any type of bacteria can result in a number of complications, particularly in babies born prematurely (before week 37 of pregnancy).
Possible complications include:
- meningitis – an infection of the meninges (the protective layer of cells surrounding the brain and spinal cord)
- cellulitis – an infection of the deep layer of skin and tissue that causes the skin on the surface to become sore and inflamed. It's usually easily treated with antibiotics
- septicaemia – more commonly known as blood poisoning, septicaemia occurs when bacteria get into the bloodstream and attack the body's tissues
- otitis media – a short-term ear infection that affects around one in four children who have had infective conjunctivitis caused by the haemophilus influenzae bacteria
Neonatal conjunctivitis
In newborn babies (neonates) up to 28 days old, infective conjunctivitis can lead to a severe and rapidly progressive eye infection. If this isn't treated, it can cause permanent damage to the child’s vision.
If this isn't treated, it can cause permanent damage to the child’s vision.
If your newborn baby is found to have infective conjunctivitis, they'll immediately be referred for specialist assessment and treatment. Their condition will be closely monitored. Complications of infective conjunctivitis are rare and most babies make a full recovery.
After having infective conjunctivitis caused by chlamydia, around one in five babies may develop pneumonia. This is a potentially life-threatening condition in young babies and may need treatment in hospital.
Allergic conjunctivitis
If your conjunctivitis is caused by an allergic reaction to pollen, dust mites or similar (seasonal and perennial allergic conjunctivitis), it's very rare to experience any serious complications.
However, you may find your reoccurring symptoms frustrating. For example, if your conjunctivitis is caused by pollen, you may find it difficult to go outside during the spring and summer months without triggering your symptoms.
This type of allergic conjunctivitis can affect your daily life and could make it difficult for you to concentrate at work or school, particularly if your eyes are severely irritated. Although this can affect your quality of life, it shouldn't cause any long-term health problems.
Read more about living with an allergy.
Punctate epithelial keratitis
Some types of conjunctivitis can cause a condition called keratitis. Keratitis is where your cornea (the front of your eye) becomes swollen.
This can be painful and make your eyes sensitive to light (photophobia). Ulcers sometimes form on the cornea. If the ulcers scar your cornea, your vision may be permanently damaged.
If you experience any unusual symptoms, contact your GP immediately or visit your nearest accident and emergency (A&E) department.
Sticky eyes: Causes, treatment, and prevention
People may use the term sticky eyes to describe when a wet or sticky discharge causes the eyelid to feel as though it is stuck together. The condition can occur due to various conditions that affect the eyes, such as styes, conjunctivitis, and blepharitis.
The condition can occur due to various conditions that affect the eyes, such as styes, conjunctivitis, and blepharitis.
However, it is normal to have some crustiness around the eyes at times when waking up.
In this article, we discuss the possible causes of sticky eyes. We also look at the treatment options and ways to prevent sticky eyes from occurring.
“Sticky eyes” is one way a person may refer to discharge from the eyes that feels gooey, crusty, or sticky.
According to the American Academy of Ophthalmology, waking up with some sticky or crustiness around the eyes is normal. This discharge is the result of not blinking during the night and various debris and mucus depositing at the corners of the eyes.
In some cases, medical conditions may cause the eyes to develop a crusty, sticky layer of mucus.
Medical conditions such as blepharitis, dry eye, and conjunctivitis are common causes of sticky eyes.
Blepharitis is a common condition that causes the eyelids to become:
- red or discolored
- itchy
- swollen
It can also cause crusty flakes to appear on the eyelashes.
It typically occurs when a person has too much bacteria on their eyelids at the base of their eyelashes. It can also happen if the oil glands in the eyelids become blocked.
There are two types of blepharitis: anterior and posterior.
Anterior blepharitis develops due to bacteria on the skin or dandruff. It affects the outside of the eye, where a person’s eyelashes attach to the eyelid.
Posterior blepharitis occurs when the oil glands become clogged. It affects the inner edge of a person’s eyelid.
Other symptoms can include:
- light sensitivity
- excessive tearing
- foamy tears
- watery eyes
- itchy eyes
- a feeling of something being in the eye
- dry eye
- crusting of the eyelids
According to the American Optometric Association (AOA), without treatment, it can lead to other issues, such as blurry vision, missing eyelashes, inflammation, or secondary infections.
Learn more about blepharitis here.
Treatment
Treatment can vary depending on the type of blepharitis, but it typically involves:
- warm compresses
- keeping the eyelids clean
- antibiotics for bacterial infections
- eye drops
- dandruff shampoo
- keeping the glands clean and clear
Conjunctivitis, also known as pinkeye, is an infection that causes symptoms such as:
- swelling of the conjunctiva or eyelids
- pink or red color in the white of the eye
- the feeling of an object in the eye or the urge to rub the eye
- increased tear production
- difficulty wearing contacts
- crusting of the eyelids and lashes
- irritation, itching, or burning in the eye
- pus or mucus discharge
The Centers for Disease Control and Prevention (CDC) note that there are three main causes of pinkeye: allergens, viruses, and bacteria.
Learn more about infective conjunctivitis here.
Treatment
Treatment for the condition can vary depending on the cause.
For bacterial causes, a doctor may prescribe antibacterial ointment or eye drops.
A person can treat allergic conjunctivitis using topical antihistamines and vasoconstrictors in the form of eye drops.
Viral conjunctivitis will typically resolve without treatment. However, for more serious forms, a person may require antiviral medications.
A person should also avoid wearing contact lenses and use a cold compress to soothe symptoms.
Parents or caregivers of children with conjunctivitis should take them to see a doctor for a diagnosis and treatment.
Learn more about how to treat pinkeye at home.
A stye is a painful bump that appears on the eyelid due to a blocked oil gland or bacterial infection.
The symptoms of a stye include:
- a painful bump along the edge of the eyelid
- a small spot of pus at the center of the bump
- a scratchy sensation in the eye
- light sensitivity
- excess tearing
- crustiness along the margin of the eyelid
Learn more about styes here.
Treatment
Treatment includes warm compresses, but if there are signs of infection, it is important to see a doctor to get antibiotics.
Dacryocystitis is the infection of the lacrimal sacs, or tear sacs. It typically occurs just after birth or in adults who are older than 40 years.
In infants, it occurs due to abnormalities in the tear ducts, such as a blockage.
In adults, it can occur due to infection, trauma, nasal abscesses, and bacteria, such as Streptococcus.
The symptoms can include:
- tenderness and swelling
- excess tears
- fever
- thick discharge from the eye
- swelling near the inner corner of the eye
Learn more about dacryocystitis here.
Treatment
Treatment includes warm compresses and antibiotics.
A person can also perform a Crigler massage on themselves or the affected infant. They can do this by placing the index finger in the corner of the eye and rolling the finger downward. It is important to wash the hands thoroughly before and after doing this.
It is important to wash the hands thoroughly before and after doing this.
Chronic dry eye occurs when the eyes do not produce enough tears. According to the AOA, causes can include either poor quality tears or not enough tears. Common symptoms can include:
- blurry vision
- watery eyes
- burning or stinging sensation
- sensitivity to light
- redness on the whites of the eye
Learn more about dry eye here.
Treatment
Common treatments include:
- artificial tears
- conserving tears
- treating other conditions around the eyes causing the issue
- increasing tear production
Several other conditions may cause sticky eyes to form. These can include:
- foreign objects in the eye
- unclean contact lenses
- damage or injury to the eyes
A person should speak with a doctor if they experience sticky or crusty eyelids or lashes. A person’s doctor can diagnose and recommend treatment for the underlying condition, which will help the crusty eye clear.
Sticky eyes are common in newborns and young children. They can occur due to a blocked tear duct. According to the United Kingdom’s National Health Service (NHS), 1 in 5 babies are born with tear ducts that have not yet fully developed.
A parent or caregiver may notice sticky substances in the corner of the eyes or see that the eyelashes have clumped together. It can affect one or both eyes.
Although the blocked tear duct will usually clear up without any intervention, a parent or caregiver may need to clean the baby’s eyes using a clean piece of cotton wool.
In some cases, people may confuse a blocked tear duct with conjunctivitis. Anyone who notices discharge alongside red or pink whites of the eyes in a child in their care should take them to see a doctor.
If the whites of the eyes do not turn red or pink, the cause is likely to be a blocked tear duct.
Another cause of sticky eyes in babies is dacryocystitis. A parent or caregiver should contact a healthcare professional if they suspect this condition, as antibiotics may be necessary.
Hot or cold compresses can help soothe the symptoms of sticky eyes. A person can use a dampened washcloth using either hot or cold water for temporary relief. A cloth can also help with cleaning the eye. However, if only one eye is sticky, it is important to avoid using the washcloth to wipe the other eye, as doing this might spread the infection.
Artificial tears may also help in some situations. A person should speak with a doctor before using artificial tears if they are unsure of the exact cause of the irritation.
A person should avoid wearing contacts when their eyes or the areas around their eyes have become irritated. Contacts can further irritate the eyes.
If an infant or child has a new or persistent sticky eye, it is best to take them to see a doctor.
The prevention of sticky eyes is not always possible. A person should follow good hygiene routines when it comes to their eyes to avoid potential infections, such as pinkeye or blepharitis.
The American Academy of Ophthalmology recommends always cleaning the hands before touching or cleaning the eyes.
People who wear contacts should follow safety routines when handling their eyes and contacts. The CDC recommends that people protect their eye health by:
- rubbing and rinsing contacts in a clean solution after each use
- using only contact solution to clean the case or contacts
- disposing of excess solution and drying the case with a clean paper towel
- washing the hands thoroughly every time before handling the contacts or eyes
A person should contact a doctor if they have persistent symptoms of eye or eyelid irritation, such as discoloration or swelling that does not go away.
It is possible that home treatments, such as warm or cold compresses, may work to help treat any underlying condition without the need for additional treatment.
A person should let a doctor know if their eye condition is getting worse even after treatment. A doctor will likely want to examine the eye and determine the cause of the continued irritation.
Sticky eyes occur when too much mucus or discharge from the eyes builds up on the eyelid and lashes, causing a crusty or sticky feeling.
The condition itself is easy to treat with a clean washcloth, but it is likely the result of an underlying condition that may need additional treatment.
In cases of infection, a person may need antibiotics or additional medications to help while the infection clears. When in doubt, a person should speak with a doctor about their symptoms to determine whether further treatment is necessary.
Why is there mucus in the eyes. How to treat eye discharge in a child.
From All About Vision
Eye discharge is a combination of mucus, fat, skin cells, and other particles that accumulate in the corners of the eyes during sleep." They may be wet and sticky or dried out, depending on how much fluid is present.
Mucous secretions have a protective function, flushing waste products and potentially dangerous particles from the tear film and the anterior surface of the eye.0003
Throughout the day, the eyes secrete mucus, but the ever-present tear film bathes your eyes with every blink, removing the secretions before they can harden.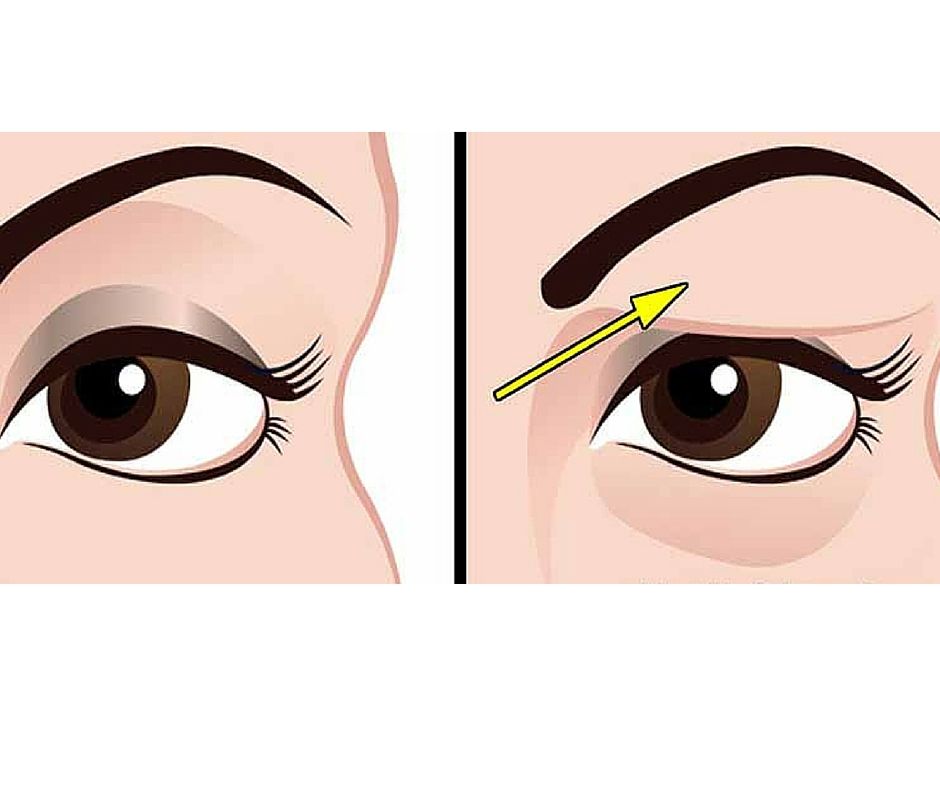
When you sleep and do not blink, the discharge accumulates and dries up in the corners of the eyes, and sometimes along the lash line. accompanied by blurry vision, sensitivity to light or eye pain may indicate a serious eye infection or eye disease. Therefore, you should immediately contact an optometrist.
FIND AN OCULIST OR OPTICS SHOP NEAR YOU : Whether you need an eye exam or are ready to buy eyeglasses or contact lenses, our locator will help you find a safe place nearby.
Where does eye discharge come from?
The discharge from the eyes consists mainly of a watery mucous secretion (mucin) produced by the conjunctiva and the secretion of the meibomian glands, an oily substance that helps to moisten the eyes between blinks.
Those impurities that are not washed away by tears accumulate in the inner corners of the eye and along the lash line. ""
Causes of discharge from the eyes the consistency, color, or amount of discharge, this may indicate an infection or eye disease.

Common eye conditions with abnormal eye discharge include:
Conjunctivitis. Discharge from the eyes is a common symptom Conjunctivitis Inflammation of the thin membrane that lines the "alkaline" of the eye (the sclera) and the inner surface of the eyelids.
In addition to itching, stinging, irritation and redness of the eyes , conjunctivitis is usually accompanied by white, yellow or green mucus that may form a crust along the eyelash line during sleep. In some cases, the crust formed on the eyelid can be so dense that it does not allow you to open your eyes.
There are three types of conjunctivitis:
Viral conjunctivitis
Viral conjunctivitis is highly contagious and is caused by the common cold or herpes simplex virus. Eye discharge from viral conjunctivitis is usually clear and watery, and may include white or yellowish mucus.
Bacterial conjunctivitis
Bacterial conjunctivitis, as the name suggests, is caused by a bacterial infection. If not promptly treated, it can pose a threat to vision. Eye discharge from bacterial conjunctivitis is usually thicker and purulent (like pus) than from viral conjunctivitis, and is usually yellow, green, or even gray in color. In the morning after sleep, patients often cannot open their eyelids, which are completely stuck together with secretions.
If not promptly treated, it can pose a threat to vision. Eye discharge from bacterial conjunctivitis is usually thicker and purulent (like pus) than from viral conjunctivitis, and is usually yellow, green, or even gray in color. In the morning after sleep, patients often cannot open their eyelids, which are completely stuck together with secretions.
Allergic conjunctivitis
Allergic conjunctivitis is triggered by allergens - pollen, dandruff, dust and other common irritants that cause eye allergies . It can also be caused by an allergic reaction to chemical pollutants, cosmetics, contact lens solutions, and eye drops. In allergic conjunctivitis, the discharge from the eyes is usually watery. Allergic conjunctivitis is not contagious and always affects both eyes.
Other eye infections
In addition to conjunctivitis, there are many eye infections that cause abnormal eye discharge. For example:
-
Herpes ocularis (recurrent viral eye infection)
-
Fungal keratitis (a rare but serious inflammation of the cornea)
-
while wearing contact lenses).

The discharge from an eye infection varies considerably - it can be clear and watery or thick, green and sticky, so you should see an eye doctor as soon as possible for diagnosis and treatment.
Blepharitis
A chronic disease of the eyelids, blepharitis, is either an inflammation of the eyelash hair follicles or an abnormal secretion of the meibomian glands at the inner edge of the eyelids.
Meibomian gland dysfunction
Also called MGD, this sebaceous gland disorder in the eyelid can cause foamy discharge from the eyes, sticky eyelids, yellow or green pus, and irritation and pain.
Barley
Barley is a blockage of the meibomian gland at the base of the eyelid, usually caused by an infected eyelash follicle. Also called hordeolum, it resembles a pimple at the edge of the eyelid and is usually accompanied by redness, swelling of the eyelids, and tenderness at the site of the lesion. Yellow pus, sticking of the eyelids, and discomfort when blinking may also occur.
Yellow pus, sticking of the eyelids, and discomfort when blinking may also occur.
SM. ALSO: How to get rid of stye
The tear duct system provides moisture and protection to the eyes.
Dry eye
Insufficient tear production or meibomian gland dysfunction can lead to dry eye syndrome , a frequently chronic condition in which the surface of the eye is not properly lubricated, becoming irritated and inflamed. Symptoms include reddened, bloodshot eyes, a burning sensation, blurred vision, and a foreign body sensation in the eye. "" Sometimes dry eyes can also cause very heavy watering.
Contact lenses
When wearing contact lenses, there may be more discharge from the eyes than usual. This can be due to a variety of reasons, including eye infection from contact lens wear, contact lens discomfort resulting in dry and irritated eyes, and contact lens wearers rubbing their eyes more frequently. If you notice more discharge due to contact lenses, remove your lenses and see an optometrist to rule out a potentially serious eye disease.
If you notice more discharge due to contact lenses, remove your lenses and see an optometrist to rule out a potentially serious eye disease.
Eye injury
A foreign body in the eye (such as dirt, particles or a chemical) or eye injury may cause watery discharge as a natural defense reaction. If after an eye injury you notice pus or blood in the eye (subconjunctival hemorrhage), contact your optometrist immediately for treatment. All eye injuries should be treated as an emergency.
Corneal ulcer
A corneal ulcer is a vision-threatening abscess-like infection of the cornea, usually caused by trauma to the eye or an advanced eye infection. If left untreated, corneal ulcers can lead to permanent vision loss. Corneal ulcers are characterized by pain, redness, swelling of the eyelids, and thick discharge from the eyes. The discharge of pus can be so strong that it causes clouding of the cornea and blurred vision.
Dacryocystitis
When the tear duct is blocked, inflammation and infection of the lacrimal sac in the drainage system of the lacrimal apparatus can occur, resulting in a painful and swollen bump under the inner eyelid. In addition to pain and redness, common symptoms of dacryocystitis include watery eyes, sticky discharge from the eyes, and blurry vision.
Treatment of eye discharge
A small amount of eye discharge is harmless, but if you notice changes in color, frequency, consistency and amount, contact your optometrist.
If mucus in the eyes is due to an eye infection, the optometrist may prescribe antibiotics or antiviral eye drops and ointments. If an eye allergy is causing watery eyes and irritation, over-the-counter antihistamine eye drops and decongestants may help relieve symptoms.
Warm compresses help soothe itching and general discomfort, and remove discharge from the eyes.
For sticky eyelids, soak a tea towel in warm water and place it over your eyes for a few minutes, then gently wipe the discharge. "
"
Home Checklist from them:
Avoid touching your eyes to avoid getting or spreading an eye infection.0003
Wash your hands frequently, especially if you have contagious conjunctivitis.
If you experience bleeding while wearing contact lenses, remove your lenses and see your optometrist. Sometimes switching to disposable contact lenses can reduce the risk of associated discharge.
If you have an eye infection, discard any cosmetics that can cause infection, such as mascara and eyeliner.
If you have watery eyes due to allergies, try to eliminate or minimize exposure to irritants. If you are sensitive to eye drops, try using products without preservatives.
Page published on Monday, November 16, 2020
Page updated on Friday, July 1, 2022
Why eye discharge occurs and what to do about it
You can listen to a short version of the article.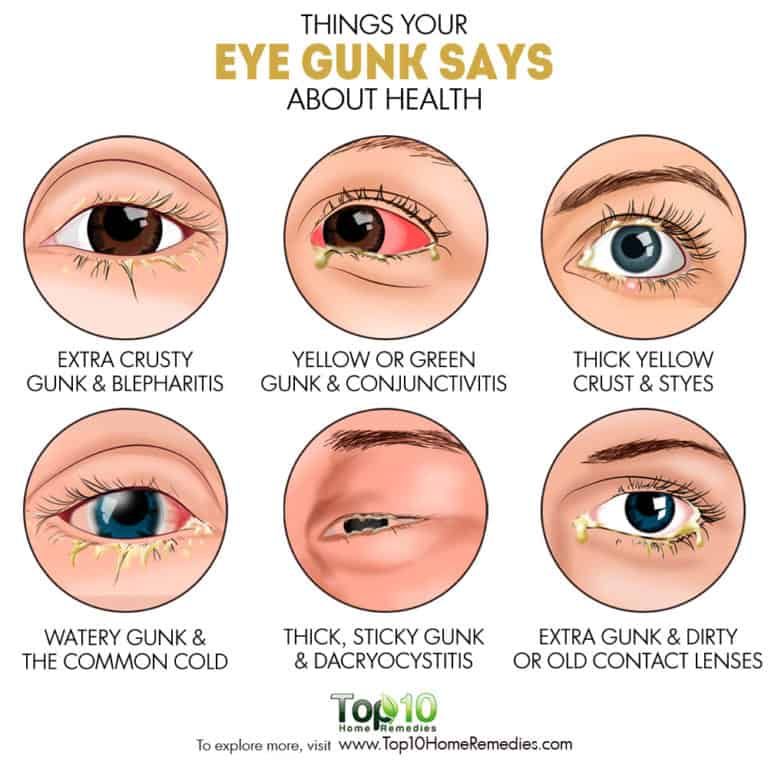 If it's more convenient for you, turn on the podcast.
If it's more convenient for you, turn on the podcast.
When to see a doctor
Schedule an appointment with a general practitioner or an optometrist if What Is Sleep Crust? / American Academy of Ophthalmology:
- discharge from the eyes is abundant and has a pronounced greenish-yellow or white color;
- you have washed away everything superfluous, but the discharge appears again and again - and there are so many of them that it can be difficult for you to open your eyes;
- vision became blurry;
- you become sensitive to light: it hurts to look at it;
- eye with discharge, very reddened or swollen;
- you feel pain in your eyes.
Any of these signs can be a symptom of a serious infection.
What causes eye discharge and what to do about it
Eye discharge can have Discharge From Eye / American Academy of Ophthalmology and more benign causes.
1. This is normal eye mucus
The best known secretions are normal mucus produced by the conjunctiva This is a thin transparent tissue that covers the outside of the eye and the back of the eyelids. It is she who produces the mucous and liquid part of tears .. Together with her, in the corners of the eyes, and sometimes along the lash line, they can What Is Sleep Crust? / American Academy of Ophthalmology accumulate and solidify fat, dead skin cells and dust. This cocktail is constantly formed on the surface of the eyes, but during the day, when we actively blink, tear fluid washes it away without a trace. At night, tears are produced less and we blink much less frequently.
It is she who produces the mucous and liquid part of tears .. Together with her, in the corners of the eyes, and sometimes along the lash line, they can What Is Sleep Crust? / American Academy of Ophthalmology accumulate and solidify fat, dead skin cells and dust. This cocktail is constantly formed on the surface of the eyes, but during the day, when we actively blink, tear fluid washes it away without a trace. At night, tears are produced less and we blink much less frequently.
What to do
Sleepy mucus looks unpleasant, but it is completely harmless and can be easily removed by simply washing with warm water.
2. Contact Lens Reaction
Contact lenses, even when worn as directed, may cause irritation or inflammation in some people. eye. The risk is increased if you forget to remove your lenses before bed.
What to do
Do not go to bed with contact lenses on. If for some reason this is not possible, ask the optometrist to choose a gas-permeable option suitable for night wear. Another option is to try disposable contact lenses.
Another option is to try disposable contact lenses.
If you are using your lenses exactly as instructed and there is more discharge from your eyes, also contact your optometrist as soon as possible. This is to rule out an eye infection or other disease.
2. Chronic dry eye
There are many reasons why the mucous membrane of the eyes can dry out. For example, this happens if you do not tear yourself away from gadgets for a long time or are in a room with low air humidity.
Dryness anyway What Is Dry Eye? Symptoms, Causes and Treatment / American Academy of Ophtalmology leads to the fact that the lacrimal fluid becomes small and does not have time to wash out the accumulated dust, fat, and dead skin cells from the eyes. Therefore, the number of allocations increases.
What to do
Pay attention to symptoms. When the mucosa dries out, they are obvious: fatigue, burning, the appearance of broken capillaries, blurred vision, a regular feeling that something has got into the eye.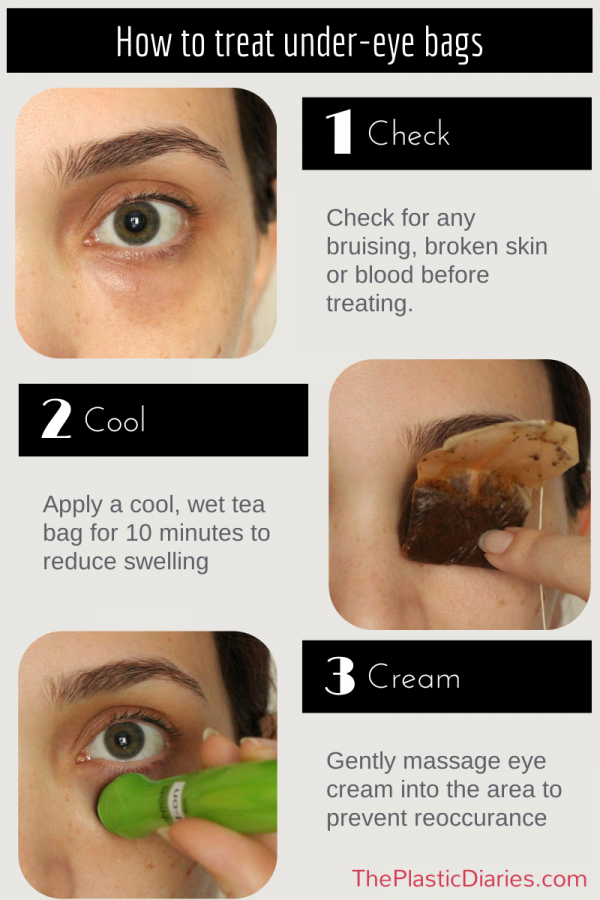 If there are such signs, consult with an ophthalmologist how you can restore healthy moisture to your eyes.
If there are such signs, consult with an ophthalmologist how you can restore healthy moisture to your eyes.
Your doctor will most likely advise you to use over-the-counter artificial tear eye drops as a first aid. But other appointments may be required.
3. Injury or damage to the eye
Any foreign substance, from the occasional sharp speck of dust to cosmetics and perfumes, if it gets into the eyes, can damage their mucous membrane. Lachrymation and profuse discharge is one of the most striking signs of Diagnosis and Management of Red Eye in Primary Care / American Family Phisician that the eye is injured.
What to do
If the damage does not look significant (say, you accidentally splashed deodorant on your face), try rinsing your eye with clean, warm water.
However, if you notice bleeding or pus after an injury, contact your optometrist immediately.
4. Allergic conjunctivitis
This is the name given to the reaction of the conjunctiva to allergen substances — plant pollen, pet dander, house dust.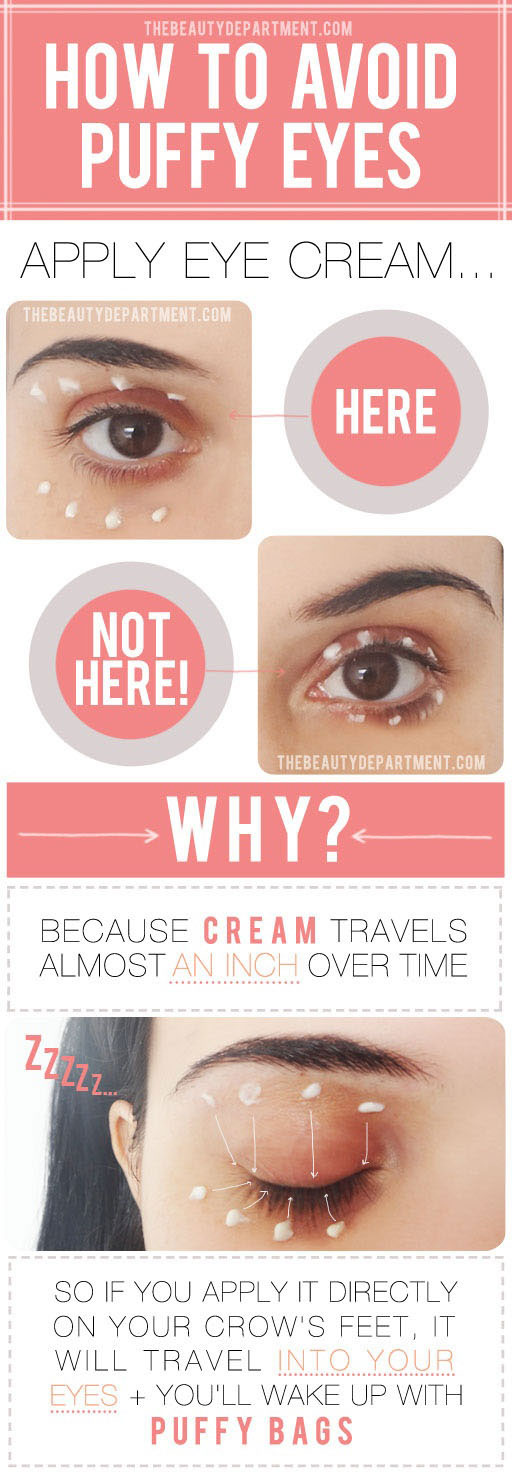 You can recognize allergic conjunctivitis Conjunctivitis: What Is Pink Eye? / American Academy of Ophthalmology for watery, reddened, swollen and itchy eyes. Sometimes discharges are added to these signs.
You can recognize allergic conjunctivitis Conjunctivitis: What Is Pink Eye? / American Academy of Ophthalmology for watery, reddened, swollen and itchy eyes. Sometimes discharges are added to these signs.
What to do
Allergic conjunctivitis is treated in the same way as allergic reactions in general, by taking antihistamines. For the eyes, such funds are available in the form of drops. Ideally, if a doctor helps you choose them.
5. Conjunctivitis
The conjunctiva becomes inflamed not only because of allergies. The cause of redness, itching, cramps, pain and other manifestations of conjunctivitis can be viral and bacterial infections, as well as irritants that have entered the eye.
What to do
Be sure to contact an ophthalmologist. Left untreated, the infection can spread and cause more serious eye damage. The doctor will make an accurate diagnosis and prescribe the necessary medications. For example, prescription eye drops.
6. Blepharitis
This is the name given to Blepharitis / NHS eyelid margin inflammation. Blepharitis causes swelling, pain, peeling around the roots of the eyelashes, and increased secretion of sebum around the follicles.
Sometimes the discharge is so abundant that the eyelashes stick together and the person cannot open his eyes.
What to do
Soak a cotton pad or gauze in warm clean water and apply to the eye for 10 minutes. Then, using a disc, gently massage the secretions.
If blepharitis persists, and even more so if additional symptoms occur, such as pain in the eyes and watery eyes, consult an ophthalmologist. The doctor will select the most suitable treatment for you. May recommend antibiotic creams or drops.
7. Keratitis
Keratitis Keratitis / Johns Hopkins Medicine is an inflammation of the cornea. It can be caused by various reasons: a bacterial or herpes infection, a fungus, an amoeba, or, for example, an ultraviolet burn if you forgot to put on your sunglasses on a hot and clear summer afternoon.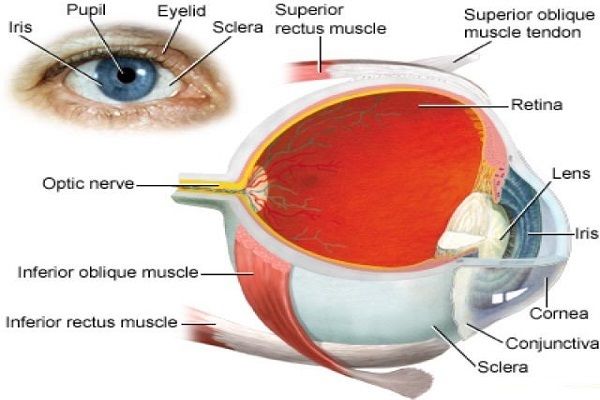
Symptoms of keratitis are similar to signs of conjunctivitis or mechanical damage: the eye turns red, watery, sore, vision may be reduced.
What to do
If left untreated, keratitis can lead to corneal scarring and temporary or even permanent loss of vision. Therefore, contact an ophthalmologist as soon as possible.
The doctor will clarify the diagnosis and prescribe treatment. In mild cases, if keratitis is not caused by an infection, you can get by with drops like “artificial tear”. In the case of infectious inflammation, you will need antiviral, antifungal agents or antibiotics, depending on the cause of the infection.
8. Trachoma
Trachoma is a bacterial eye infection caused by What Is Trachoma? / American Academy of Ophthalmology specific bacterium: Chlamydia trachomatis. In the early stages, trachoma resembles the symptoms of conjunctivitis: the eyes swell, itch, and discharge may appear on them.
As the disease progresses, pain and blurred vision appear. Scars form inside the eyelid, and this leads to the fact that the eyelashes seem to be wrapped inside the eye. This condition is called trichiasis and is one of the most characteristic signs of trachoma.
Scars form inside the eyelid, and this leads to the fact that the eyelashes seem to be wrapped inside the eye. This condition is called trichiasis and is one of the most characteristic signs of trachoma.
What to do
Trachoma is the leading cause of infectious blindness in the world. Therefore, at the slightest suspicion of an infection, you should contact an ophthalmologist as soon as possible.
9. Styes
Styes is an inflammation that can appear on the outer or inner side of the eyelid. In the first case, it is caused by infection of the eyelash follicle (the sac from which it grows). In the second - a blockage of the meibomian gland, which is located on the inside of the eyelid and secretes a secret that protects the mucous membrane from drying out.
A stye usually looks like a hard, round pimple at the edge of the eyelid. The eye may become red, sore and increase the amount of discharge.
What to do
Styes most often go away on their own in Sty / Mayo Clinic in 7-10 days. Compresses can be used to speed up and facilitate its maturation and removal. Soak a cotton pad or piece of gauze in warm water and place on the affected eye. Change the compress to a new warm one as it cools down.
Compresses can be used to speed up and facilitate its maturation and removal. Soak a cotton pad or piece of gauze in warm water and place on the affected eye. Change the compress to a new warm one as it cools down.
Be sure to consult a general practitioner or ophthalmologist if, after a week and a half, the barley does not disappear and does not decrease in size. In this case, you may be prescribed antibiotics: in the form of eye drops or a special cream. The doctor may also make a tiny incision in the barley to drain the pus. In no case do not try to do this operation yourself: this often leads to the fact that the infection spreads to the entire eye.
10. Dacryocystitis
Dacryocystitis is a condition Dacryocystitis / MSD Manual where a blocked lacrimal sac becomes infected and inflamed. The result usually looks like a swollen, reddened bump under the lower eyelid on the inside of the eye.
Lachrymation, pain in the eye, sticky discharge, blurred vision are all associated symptoms of dacryocystitis.
What to do
Often things go away on their own. To speed up and facilitate this process, you can apply a warm compress to the inflammation for 10-15 minutes. For example, gauze soaked in warm water.
However, dacryocystitis can have dangerous complications, up to the spread of infection to the brain. Therefore, it is best to contact an optometrist as soon as possible.
The doctor will examine the eye, ask you about your symptoms, clarify the diagnosis and prescribe the appropriate treatment. These are usually antibiotics in the form of ointments or tablets, as well as over-the-counter pain relievers that help reduce discomfort.
11. Corneal ulcer
Corneal ulcer What Is a Corneal Ulcer (Keratitis)? / American Academy of Ophthalmology is an infection that causes an open sore on the cornea. Associated symptoms: pain, tearing, sensitivity to light, difficulty opening the eye, profuse sticky discharge.
What to do
See an ophthalmologist as soon as possible. The cornea must be treated, otherwise the ulcers may spread over its entire surface or penetrate deeper. Usually treated with antibiotics.
The cornea must be treated, otherwise the ulcers may spread over its entire surface or penetrate deeper. Usually treated with antibiotics.
12. Endophthalmitis
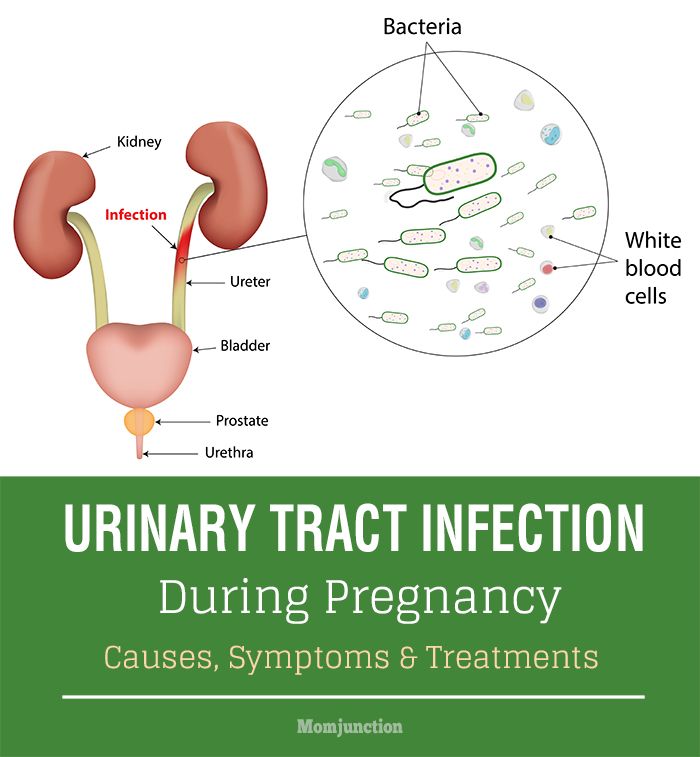
Endofalmitis What is Endophthalmitis? / American Academy of Ophthalmology is an infection of the tissues or fluids inside the eyeball.
Bacteria or fungi are most commonly introduced into the eye after a poorly performed operation, injection into the eye, or injury. But sometimes endofalmitis is a complication of an infectious process in another part of the body. For example, this can happen with a urinary tract infection or blood poisoning.
This condition has very pronounced symptoms: increasing pain in the eyes, distinct redness and swelling, a sharp decrease or loss of vision. And white or yellow (purulent) discharge from the eyes.
What to do
Endofalmitis is a medical emergency. If you do not quickly stop the inflammation, you can be left without vision. Therefore, if you suspect such an infection, you should immediately go to the emergency room or to an ophthalmologist.
13. Shingles
Herpes zoster What Is Shingles (Herpes Zoster)? / American Academy of Ophthalmology (lat. Herpes zoster). This disease, as a rule, is a complication of chickenpox transferred many years ago.
Usually, shingles is a painful red rash that most often appears in the lower back - hence the name of the disease. But if the herpes virus has affected the optic nerves, a painful rash can also appear in the eye area - mainly on the upper and lower eyelids. Among other things, herpes causes swelling of the eyes, decreased vision and the appearance of discharge.
What to do
Herpes zoster needs to be treated urgently or it can Shingles (Herpes Zoster) Symptoms / American Academy of Ophthalmology lead to corneal scarring, glaucoma or cataracts. Therefore, you need to see an ophthalmologist as soon as possible: the doctor will assess the degree of eye damage and prescribe the most effective treatment.
14. Covid
In some cases, coronavirus infection affects the eyes and can cause symptoms Is It COVID‑19 or Allergies? / American Academy of Ophthalmology, similar to signs of allergic conjunctivitis.
To distinguish between these conditions, check with your state of health. If signs of conjunctivitis arose against the background of high fever, cough, severe weakness and other manifestations of covid, it is most likely that the inflammation of the eyes has a coronavirus nature.
What to do
Apply compresses to the eyes to relieve Get Rid of Pink Eye Fast With These Home Remedies / American Academy of Ophthalmology. For example, a clean cotton sponge soaked in warm water. You can also apply a cool, damp towel to your eyes.
Over-the-counter pain relievers such as ibuprofen and antihistamines or artificial tears are acceptable.
If signs of conjunctivitis persist, consult your physician or ophthalmologist. With confirmed covid - by phone.
What to do so that the discharge does not appear
Surely you will not be able to protect yourself from infections and injuries. But you can reduce the risks.
- Wash your hands regularly.