Kick in the stomach
a kick in the stomach
a kick in the stomach - Examples:
1) Disappointing weekend. It was all a kick in the stomach for German Grand Prix organisers, who had to scrap the 2015 race at the ...
2) It is a kick in the stomach to students. The Government are reneging on the deal reached in 2010 ...
3) ... plan to close the branches, describing it as "a kick in the stomach" for both customers and staff in Northern Ireland.
4) Why should they treat generously a country that has given them a kick in the stomach?
5) It was a kick in the stomach to be told you're going to be living with this chronic condition as a . ..
6) This might be a kick in the stomach for Chelsea fans. Many didn't want to see Mourinho sacked midway through the ...
7) That was a kick in the stomach, and it took us a long time to get back from that.
8) We made it hard for ourselves and it was a kick in the stomach to concede in the first minute but in the second half we showed great character ...
9) ... has to be respected and making exceptions for celebrities would be a kick in the stomach to those who are not celebrities.
10) Slashing the time available to consider submissions is a kick in the stomach to the hundreds of very capable people who have spent a lot of time preparing . ..
..
11) ... which meant I was the alternate, which was kind of a kick in the stomach.
12) He gave me a kick in the stomach when he went, but I don't bear any animosity to him and I ...
13) ... not considered part of any contribution to the school? What a kick in the stomach for somebody that's done it for over 40 years.
14) ... they get housing. what do the homeless get? a kick in the stomach from what I have seen.
15) This is a kick in the stomach and just plain nasty.
16) RMS recently gave her competitors a kick in the stomach by unveiling not one, but four 24 hour vernacular TV stations.
17) ... cost of living increase. But what we do get is a kick in the stomach. Especially as they keep asking for more and more with less and less.
18) Losing to Donegal was a kick in the stomach for us because we had been quite optimistic going into the game.
19) Many see the destruction of the food as a kick in the stomach for this who are already spiraling into poverty.
20) Far from giving other women a kick in the stomach, female CEOs are more likely to give their female colleagues a hand up.
Jujitsu kick to the abdomen: a case of blunt abdominal trauma resulting in hematochezia and transient ischemic colitis
Case Reports
. 2011 Aug;58(2):189-91.
2011 Aug;58(2):189-91.
doi: 10.1016/j.annemergmed.2011.01.014. Epub 2011 Mar 9.
Hans Rosenberg 1 , Jeremy Beck
Affiliations
Affiliation
- 1 Department of Emergency Medicine, The Ottawa Hospital, University of Ottawa, 1053 Carling Avenue, Ottawa, Ontario, Canada. [email protected].
- PMID: 21392850
- DOI: 10.1016/j.annemergmed.2011.01.014
Case Reports
Hans Rosenberg et al. Ann Emerg Med. 2011 Aug.
. 2011 Aug;58(2):189-91.
doi: 10.1016/j.annemergmed.2011.01.014. Epub 2011 Mar 9.
Authors
Hans Rosenberg 1 , Jeremy Beck
Affiliation
- 1 Department of Emergency Medicine, The Ottawa Hospital, University of Ottawa, 1053 Carling Avenue, Ottawa, Ontario, Canada. [email protected].
- PMID: 21392850
- DOI: 10.1016/j.annemergmed.2011.01.014
Abstract
Blunt abdominal trauma is a common presentation to the emergency department. Ischemic colitis is a rare complication of this and its possible sequelae are important for an emergency physician to recognize. A 21-year-old man presented to the emergency department with abdominal pain and hourly episodes of bright red blood per rectum shortly after being kicked in the stomach at his jujitsu class. He had no significant medical history, and results of his systems review were otherwise unremarkable. On examination, he appeared well, with normal vital signs. He had mild lower abdominal tenderness, but there were no peritoneal signs present. There was blood on the digital rectal examination. His hemoglobin, platelet, and international normalized ratio levels were normal and his abdominal radiograph was unremarkable. The gastroenterology service was contacted because of the hematochezia and a flexible sigmoidoscopy was performed. The sigmoidoscopy showed erythema, ulceration, and edema of a segment in the left colon, consistent with ischemic colitis. This was later confirmed on biopsy.
Ischemic colitis is a rare complication of this and its possible sequelae are important for an emergency physician to recognize. A 21-year-old man presented to the emergency department with abdominal pain and hourly episodes of bright red blood per rectum shortly after being kicked in the stomach at his jujitsu class. He had no significant medical history, and results of his systems review were otherwise unremarkable. On examination, he appeared well, with normal vital signs. He had mild lower abdominal tenderness, but there were no peritoneal signs present. There was blood on the digital rectal examination. His hemoglobin, platelet, and international normalized ratio levels were normal and his abdominal radiograph was unremarkable. The gastroenterology service was contacted because of the hematochezia and a flexible sigmoidoscopy was performed. The sigmoidoscopy showed erythema, ulceration, and edema of a segment in the left colon, consistent with ischemic colitis. This was later confirmed on biopsy. A computed tomography (CT) scan of the abdomen was conducted, which revealed left colonic inflammation consistent with colonic ischemia. There was no mesenteric vascular thrombosis or mesenteric hematoma found on CT. His hematochezia and abdominal pain subsided spontaneously, and he was discharged home. This case illustrates transient ischemic colitis as a potential presentation of blunt abdominal trauma, and emergency physicians should consider this uncommon diagnosis in the differential diagnosis of patients presenting after abdominal trauma.
A computed tomography (CT) scan of the abdomen was conducted, which revealed left colonic inflammation consistent with colonic ischemia. There was no mesenteric vascular thrombosis or mesenteric hematoma found on CT. His hematochezia and abdominal pain subsided spontaneously, and he was discharged home. This case illustrates transient ischemic colitis as a potential presentation of blunt abdominal trauma, and emergency physicians should consider this uncommon diagnosis in the differential diagnosis of patients presenting after abdominal trauma.
Copyright © 2011 American College of Emergency Physicians. Published by Mosby, Inc. All rights reserved.
Similar articles
-
Computed Tomography and Magnetic Resonance Imaging Findings in a Case of Colonic Intramural Hematoma After Mild Blunt Abdominal Trauma.
Torres US, Cesar DN, DʼIppolito G.
 Torres US, et al. J Comput Assist Tomogr. 2016 Nov/Dec;40(6):896-898. doi: 10.1097/RCT.0000000000000534. J Comput Assist Tomogr. 2016. PMID: 27759601
Torres US, et al. J Comput Assist Tomogr. 2016 Nov/Dec;40(6):896-898. doi: 10.1097/RCT.0000000000000534. J Comput Assist Tomogr. 2016. PMID: 27759601 -
[Post-traumatic intramural hematoma of the colon].
Crema MD, Arrivé L, Monnier-Cholley L, Tubiana JM. Crema MD, et al. J Radiol. 2004 Dec;85(12 Pt 1):2039-41. doi: 10.1016/s0221-0363(04)97779-7. J Radiol. 2004. PMID: 15692417 French.
-
Acute colonic intramural hematoma due to blunt abdominal trauma.
Yin WY, Gueng MK, Huang SM, Chen HT, Chang TM. Yin WY, et al. Int Surg. 2000 Jan-Mar;85(1):51-4. Int Surg. 2000. PMID: 10817432 Review.
-
Delayed small bowel perforation following blunt abdominal trauma: A case report and review of the literature.

Hamidian Jahromi A, Johnson L, Youssef AM. Hamidian Jahromi A, et al. Asian J Surg. 2016 Apr;39(2):109-12. doi: 10.1016/j.asjsur.2013.01.006. Epub 2013 Mar 6. Asian J Surg. 2016. PMID: 27016786 Review.
-
Isolated unilateral adrenal gland hemorrhage following motor vehicle collision: a case report and review of the literature.
Lehrberg A, Kharbutli B. Lehrberg A, et al. J Med Case Rep. 2017 Dec 26;11(1):358. doi: 10.1186/s13256-017-1506-x. J Med Case Rep. 2017. PMID: 29277157 Free PMC article. Review.
See all similar articles
Cited by
-
Brazilian Jiu Jitsu, Judo, and Mixed Martial Arts Injuries Presenting to United States Emergency Departments, 2008-2015.

Stephenson C, Rossheim ME. Stephenson C, et al. J Prim Prev. 2018 Oct;39(5):421-435. doi: 10.1007/s10935-018-0518-7. J Prim Prev. 2018. PMID: 30043324
-
ACG clinical guideline: epidemiology, risk factors, patterns of presentation, diagnosis, and management of colon ischemia (CI).
Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ; American College of Gastroenterology. Brandt LJ, et al. Am J Gastroenterol. 2015 Jan;110(1):18-44; quiz 45. doi: 10.1038/ajg.2014.395. Epub 2014 Dec 23. Am J Gastroenterol. 2015. PMID: 25559486 No abstract available.
Publication types
MeSH terms
Blunt abdominal trauma - City Hospital No.
 12, Barnaul: Articles
12, Barnaul: Articles Blunt abdominal trauma is a closed traumatic injury to the abdominal organs and retroperitoneal space. It is manifested by pain in the abdomen, weakening of peristalsis, a violation of the general condition. Shock may develop. The condition poses a threat to life, urgent medical measures are required. The diagnosis is made on the basis of clinical symptoms, data from ultrasound, CT, radiography, laparoscopy and other studies. Surgical treatment - revision, suturing or removal of damaged organs.
ICD-10
General information
Blunt abdominal trauma - damage to internal organs located in the abdominal cavity and retroperitoneal space, while maintaining the integrity of the skin of the anterior abdominal wall, lumbar region and lateral parts of the abdomen. It poses a threat to the life of the patient, while external signs of severe damage are absent or minimal (the skin is intact, there are no visible deformations), the presence of a light gap is characteristic (the condition of the victim immediately after the injury may remain satisfactory).
All of the above in some cases causes late treatment of patients to specialists, complicates the provision of first aid and creates certain difficulties in the diagnostic process. Meanwhile, the probability of a successful outcome directly depends on the timely initiation of treatment. With the development of a serious condition, the effectiveness of medical care is significantly reduced, and the likelihood of death and the occurrence of dangerous complications increases dramatically.
Causes
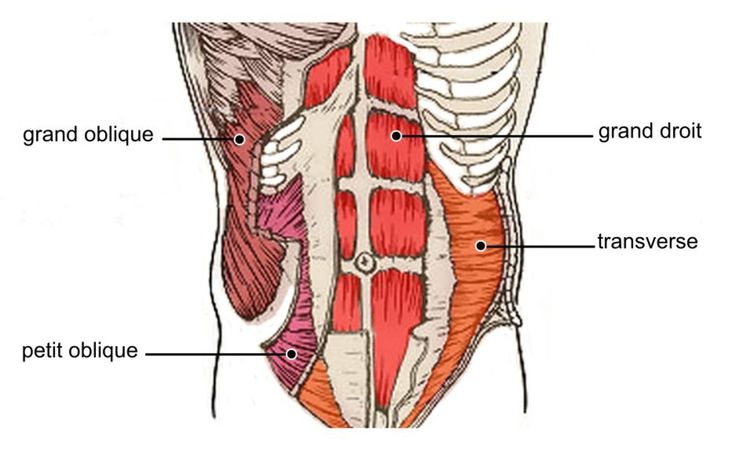
The direct cause of blunt abdominal trauma is a powerful concentrated blow to the anterior abdominal wall and lateral parts of the abdomen, less often to the lumbar region. Usually, at the moment of impact, the abdominal muscles are in a more or less relaxed state - this creates favorable conditions for "passing" the blow deep into the tissues. A similar mechanism of injury can be observed during criminal incidents (punching or kicking), car accidents, falls from great heights, natural or industrial disasters.
Most of the listed incidents are characterized by intense traumatic impact and the simultaneous occurrence of several injuries. Combinations of a closed abdominal injury with a pelvic fracture, rib fractures, fractures of the bones of the upper and lower extremities, fractures of the spine, TBI and injuries of various areas are possible. The presence of several injuries aggravates the patient's condition, provokes the rapid development of traumatic shock and increases the likelihood of massive blood loss.
Classification
Taking into account the characteristics of damage in abdominal surgery, the following types of blunt abdominal trauma are distinguished:
- No damage to internal organs. This group includes bruises, ruptures of the fascia and muscles of the abdominal wall.
- With damage to the abdominal organs. These include damage to the spleen, liver damage, intraperitoneal rupture of the bladder, rupture of the small and large intestine.

- With damage to organs located outside the abdominal cavity. This group includes extraperitoneal bladder rupture, kidney injury, pancreatic injury, and ruptures of some parts of the large intestine.
- With intra-abdominal bleeding. Similar injuries can occur with damage to the liver, spleen, vessels of the omentum and mesentery of the intestine.
- With the threat of early development of peritonitis. This includes injuries with rupture of hollow organs (stomach, intestines).
- With simultaneous damage to hollow and parenchymal organs.
Blunt abdominal trauma can be isolated (injury to one organ, such as only the liver or only the small intestine), multiple (injury to several organs, such as the spleen and colon), or combined (injury to several organs and systems, for example, rupture of the urinary bladder and pelvic fracture or pancreatic injury and shoulder fracture).
Symptoms
History reveals characteristic trauma, patient complains of abdominal pain. The absence of pain is not a reason to exclude the diagnosis of blunt abdominal trauma: in the light interval, the pain is insignificant, in the erectile phase of shock, the victim may underestimate the severity of his condition and not notice the pain; in the presence of other injuries (for example, fractures of the ribs or bones of the limbs), abdominal pain may fade into the background and not be realized due to intense pain in another part of the body; in the torpid phase of shock, complaints may be absent due to a decrease in sensitivity, depression and indifference of the patient, impaired consciousness, etc.
The absence of pain is not a reason to exclude the diagnosis of blunt abdominal trauma: in the light interval, the pain is insignificant, in the erectile phase of shock, the victim may underestimate the severity of his condition and not notice the pain; in the presence of other injuries (for example, fractures of the ribs or bones of the limbs), abdominal pain may fade into the background and not be realized due to intense pain in another part of the body; in the torpid phase of shock, complaints may be absent due to a decrease in sensitivity, depression and indifference of the patient, impaired consciousness, etc.
In the area of the anterior abdominal wall, lower ribs, lateral sections of the abdomen and lower back, hematomas and abrasions are sometimes visible. The muscles of the anterior abdominal wall are tense (it should be borne in mind that with exhaustion, muscle atrophy, as well as thickening of the fat layer and fatty degeneration of the muscles, the tension can be weak, barely noticeable). Soreness is detected on palpation of the abdomen, with intra-abdominal injuries, positive symptoms of peritoneal irritation are determined.
Soreness is detected on palpation of the abdomen, with intra-abdominal injuries, positive symptoms of peritoneal irritation are determined.
If available 500 ml or more. blood flowing from a damaged vessel or parenchymal organ, it is possible to determine the dullness of the sound during percussion of the abdomen. On auscultation, there is a decrease in peristalsis. Other symptoms may include nausea, vomiting, absence or changes in stools, blood in the urine, frequent painful urination, etc. Common non-specific signs include an increase in heart rate, a decrease in blood pressure, and an increase in shock index.
In some cases, characteristic symptoms allow a traumatologist or abdominal surgeon to suspect damage to a particular organ even before instrumental examinations. So, with ruptures of the small and large intestines, spreading, increasing pain in the abdomen, nausea and vomiting appear, and traumatic shock may develop. At the same time, with ruptures of the colon, the tension of the abdominal wall is more pronounced, signs of intra-abdominal bleeding are often revealed.
Liver injury usually results in profuse internal bleeding. The patient's condition rapidly deteriorates, hypovolemic shock develops, loss of consciousness is possible. If contact with the patient is maintained, complaints of pain in the right hypochondrium, radiating to the right shoulder girdle, are revealed. The pressure is reduced, breathing and pulse are quickened, the skin is pale. If the spleen is damaged, in some cases there are also signs of massive internal bleeding, but the pain is not on the right, but on the left. Sometimes (with subcapsular rupture) the patient's condition in the first days or even weeks may remain satisfactory.
In case of damage to the pancreas, the victim complains of sharp pain in the epigastric region, tension in the muscles of the abdominal wall and bloating. If the kidney is damaged, macrohematuria and pain in the lumbar region occur. With extraperitoneal ruptures of the bladder, swelling of the perineum and false urge to urinate are detected, with intraperitoneal injuries of the bladder, frequent false urges, pain in the lower abdomen, bloating and weakening of peristalsis are observed.
Diagnosis
A casualty with a suspected closed abdominal injury is immediately taken to a medical facility, blood and urine tests are prescribed, blood group and Rh factor are determined. The rest of the examination scheme is drawn up individually. Ultrasound, CT, MSCT are used to exclude intra-abdominal bleeding (including subcapsular) and assess the state of internal organs. If these studies are not available, if a rupture of hollow organs is suspected, an abdominal x-ray is used.
If bladder injury is suspected, catheterization is performed, and if necessary, ascending cystography is performed. The most accurate and effective method for diagnosing injuries of the abdominal organs is laparoscopy, which allows visually assessing the condition of internal organs, the degree of their destruction, the source and intensity of bleeding, and thus, as clearly as possible, determine the indications for surgical intervention and the tactics of surgical treatment.
Treatment of blunt abdominal trauma
Treatment of bruises, ruptures of the fascia and muscles of the abdominal wall is conservative. In case of damage to hollow and parenchymal organs, an emergency operation is indicated - suturing, resection or removal of the organ. The intervention is carried out against the background of intensive anti-shock measures: blood transfusion and blood substitutes, artificial respiration, stimulation of cardiac activity, control and stimulation of diuresis, etc. In the postoperative period, intensive therapy is continued, antibiotics and analgesics are prescribed.
In case of damage to hollow and parenchymal organs, an emergency operation is indicated - suturing, resection or removal of the organ. The intervention is carried out against the background of intensive anti-shock measures: blood transfusion and blood substitutes, artificial respiration, stimulation of cardiac activity, control and stimulation of diuresis, etc. In the postoperative period, intensive therapy is continued, antibiotics and analgesics are prescribed.
Prognosis and prevention
The prognosis is determined by the severity of blunt abdominal trauma, the presence of damage to certain organs, the general health of the victim, the time of the surgical intervention. With combined injuries, mortality reaches 70, with ruptures of the liver - 50%, with ruptures of the spleen - 5%. In the early postoperative period, the development of peritonitis is possible, in the remote period, adhesive disease may occur due to the presence of cicatricial adhesions in the abdominal cavity. Prevention involves taking measures to reduce the level of injuries.
Prevention involves taking measures to reduce the level of injuries.
3. Diagnosis and surgical tactics in closed abdominal trauma / Tomnyuk N.D., Ryabkov I.A., Zhigo P.T., Kembel V.R. // Bulletin of the VSNC SO RAMS - 2007 - No. 4
4. Optimization of the diagnosis of blunt abdominal trauma / Faizulina R.R., Nuzova O.B., Bobyleva E.O. // Health and education in the XXI century - 2017 - V.19, No. 5
GMS Clinic Gastroenterologist Alexey Golovenko answers frequently asked questions about this disease in his article.
What are diverticula?
A diverticulum is a protrusion of the intestinal wall, resembling a "hernia" on a soccer ball. Most often, diverticula are found in the large intestine - these are the last 1.5 meters of the digestive tube, where water is absorbed, which makes the stool from liquid to hard. Less common are diverticula in the esophagus and small intestine. The sex of a person does not affect whether diverticula appear, but with age, the likelihood of their occurrence increases.
Why do these diverticula appear?
There is no unified theory of the occurrence of diverticula. Diverticula appear in the "weak" places of the intestinal wall - places where blood vessels penetrate it. It has also been noted that diverticula appear more often in people with constipation and in Westerners, where the diet is low in dietary fiber - natural "softeners" of the stool. Apparently, if, due to a lack of dietary fiber, the stool becomes too dense and moves through the intestine not in one mass, but in solid fragments, the pressure in the lumen increases too much in certain parts of the colon. This leads to the protrusion of the mucous membrane and submucosal layer of the intestine towards the abdominal cavity through the muscle layer.
I have diverticula. I am sick?
Probably not. The mere presence of diverticula (in the absence of symptoms) is called "diverticulosis". Only every fifth person with diverticula has some manifestations of the disease, and not always they are associated with active inflammation of the diverticula.
Can diverticula cause stomach pain?
Maybe, but there are several reasons for this pain. Intense constant pain over the area of the intestine where the diverticula are located, often indicates inflammation of the diverticulum - diverticulitis. Inflammation occurs when the mouth of the diverticulum is blocked by a dense fragment of stool (coprolite). This disrupts the blood supply to the diverticulum, and also promotes the movement (translocation) of bacteria from the lumen of the colon to the wall of the diverticulum. Together, this leads to inflammation of the diverticulum, and sometimes to bleeding from it.
Most often, diverticulitis resolves without a trace during antibiotic therapy. In some people, diverticulitis becomes chronic—the inflammation persists. This can lead to complications: abscesses (abscesses in the tissue surrounding the diverticulum), fistulas (purulent passages connecting the lumen of the diverticulum, for example, with neighboring organs), infiltrate (tumor-like accumulation of cells around the inflamed diverticulum) and stricture (narrowing of the intestinal lumen at the site of inflammation ). However, pain in colonic diverticula can occur without inflammation.
However, pain in colonic diverticula can occur without inflammation.
How so? There is no inflammation, where does the pain in an actually healthy intestine come from?
In the thickness of the colon wall there is a network of nerve fibers that control its motility - which segments of the intestine will contract, pushing out the stool. With an increase in pressure in the intestinal lumen (passage of stool or gas), special cells are activated that release neurotransmitters (for example, serotonin). This gives a signal to the nervous system to contract the intestine and free itself from the contents. Normally, we almost do not feel this "work" of the intestine.
When a diverticulum becomes inflamed, the balance of neurotransmitters is disturbed, which is partly facilitated by changes in the composition of bacteria within the diverticulum. The imbalance of neurotransmitters can remain even when the inflammation has already passed. This leads to increased sensitivity of the gut to stretch (doctors call this "visceral hypersensitivity"). This phenomenon is confirmed by experiments. If a healthy person and a patient with diverticular disease introduce a balloon into the intestine and begin to gently inflate it with air, then a person with a disease will experience discomfort earlier than a healthy person (that is, pain will occur with a smaller volume of the balloon). The same pain mechanism is described in irritable bowel syndrome.
This phenomenon is confirmed by experiments. If a healthy person and a patient with diverticular disease introduce a balloon into the intestine and begin to gently inflate it with air, then a person with a disease will experience discomfort earlier than a healthy person (that is, pain will occur with a smaller volume of the balloon). The same pain mechanism is described in irritable bowel syndrome.
How do you determine if there is inflammation or other complications?
Computed tomography is the best examination for suspected diverticulitis. In this study, several emitters rotate around the human body and numerous x-ray images are obtained. The computer program then uses these fragments to create whole "slices" of the body. Tomography allows not only to see changes in the contour of the intestinal wall (that is, diverticula proper), but also changes in the tissues surrounding the colon (for example, abscesses). A less accurate way to find diverticula is irrigoscopy or, in a simple way, an enema with barium sulfate, which is clearly visible in X-rays and allows you to see the internal contour of the intestine and some very gross complications (for example, strictures).
Instead of computed tomography, some centers use ultrasound (ultrasound), which, unlike tomography, is completely safe and, apparently (in experienced hands), has almost the same accuracy. The downside is that an ultrasound specialist must undergo special long-term training in order to learn how to diagnose diverticula, so, alas, not every clinic has such doctors.
What about a colonoscopy?
Colonoscopy - that is, the examination of the colon with a flexible apparatus with a video camera - is also a way to detect diverticula. Most diverticula are discovered incidentally during a routine colonoscopy, which is done to detect cancer early. However, if acute inflammation of the diverticulum (diverticulitis) is suspected, colonoscopy is not used as a primary diagnostic method. During colonoscopy, the intestine is inflated with gas from the inside, and this can lead to perforation (rupture) of the diverticulum.
At the same time, after the inflammation of the diverticulum has passed, a colonoscopy should be performed. Studies show that the likelihood of finding colon cancer increases during the first year after acute diverticulitis. Apparently, inflammation in some patients "masks" the tumor on x-rays, and immediately viewing the entire colon with an endoscope during acute inflammation is both unsafe and impossible due to pain.
Studies show that the likelihood of finding colon cancer increases during the first year after acute diverticulitis. Apparently, inflammation in some patients "masks" the tumor on x-rays, and immediately viewing the entire colon with an endoscope during acute inflammation is both unsafe and impossible due to pain.
Can I protect myself from diverticulitis and other complications?
Yes, if you have diverticula, you can reduce your risk of inflammation by getting soft stools every day. The consistency of the stool is most dependent on the content of dietary fiber. Try to eat at least a plate or cup of vegetables and fruits every day, add wheat bran to cereal and yogurt, and drink at least a glass of liquid (not necessarily water) with each meal. Instead of sweets and other sweets, try to eat dried fruits - this will also help keep weight under control.
It happens that due to the abundant intake of plant foods, gas formation increases. Then, to normalize the stool, they take balanced dietary fibers that are not so strongly fermented by bacteria, for example, psyllium is the husk of psyllium seeds, which can be consumed indefinitely. By the way, in vegetarians, who, refusing meat, begin to consume more plant foods, both the diverticula themselves and their complications occur less frequently than non-vegetarians.
By the way, in vegetarians, who, refusing meat, begin to consume more plant foods, both the diverticula themselves and their complications occur less frequently than non-vegetarians.
They say you can't eat sunflower seeds and popcorn - it all gets stuck in diverticula.
This is an old theory that has been completely refuted by modern research. American scientists observed 47,000 people who, during a routine examination at the age of 40 to 75, did not find any diseases of the large intestine, as well as diverticula. Participants filled out questionnaires every 2 years about their condition and talked about their diet for 18 years. It turned out that diverticulitis and bleeding from diverticula occurred with the same frequency in people who do not eat nuts, popcorn and seeds, and in people who eat well. Moreover: those who took nuts twice a week not only did not more often, but were less likely to be seen by doctors due to diverticulitis than people who eat nuts only once a month.
I was diagnosed with symptomatic uncomplicated diverticular disease. The stomach hurts on the left, and the doctors do not find inflammation. Is it curable?
Yes, due to similar pain mechanisms, the treatment of uncomplicated diverticular disease is similar to that of irritable bowel syndrome. Pain is eliminated by taking antispasmodics - drugs that relieve painful contraction of the intestine, which are often taken for a long time. A non-absorbable (non-absorbable) antibiotic is also sometimes prescribed to change the composition of the bacteria in the gut. Some patients may need a small dose of antidepressants to improve the exchange of serotonin, which regulates intestinal motility.
It's clear, what if today it hurts not from inflammation, but tomorrow - diverticulitis and peritonitis? When to run to the doctor?
Seek medical attention if the pain becomes severe and persistent, does not go away at night, or if it causes fever, chills, nausea or vomiting, or fainting. You should also always consult your doctor if there is blood in the stool. It is very important. Without timely treatment, diverticulitis can result in surgery. And even worse.
You should also always consult your doctor if there is blood in the stool. It is very important. Without timely treatment, diverticulitis can result in surgery. And even worse.
Gastroenterologist, hepatologist GMS Clinic Sergey Vyalov gave an interview to the stopkilo.net Internet portal and spoke about the problems and treatment of the gallbladder.
Introduction
The gallbladder is one of the "special" organs that can literally prepare surprises. Such surprises are an unexpected attack of severe pain in the abdomen on the right somewhere under the ribs, which we call "biliary colic."
The gallbladder serves as a kind of reservoir that collects and stores bile until the right moment, and then throws it away for the needs of digestion. If bile begins to be poorly “stored” or “stagnate”, then its composition changes. Then it all depends on how far the process has gone.
But it all starts with a violation of the normal contractions of the gallbladder - it contracts either too quickly and strongly, or too weakly and slowly. Both of these disorders lead to improper bile secretion and changes in the composition of bile, and in the long term - to the formation of stones.
Both of these disorders lead to improper bile secretion and changes in the composition of bile, and in the long term - to the formation of stones.
Most often, errors in nutrition lead to this when we overeat or eat a lot of fatty, fried, smoked food. In some people, an additional contribution to the development of gallbladder diseases is made by high cholesterol, hormonal imbalance, taking certain medications, and hereditary predisposition. Stress, emotional and nervous tension also leads to dysfunction of the gallbladder. That is why the last stage, cholelithiasis, more often affects women after a critical age. Although in recent years, gallbladder diseases have become much “younger” and are very often detected even in children!
Sensations located in the upper abdomen (in the region of the stomach) or under the ribs on the right are most often associated with a disease of the stomach or gallbladder, and in rare cases even the intestines. It is very difficult to distinguish them from each other on your own. When examining the abdomen, the doctor can easily determine what exactly led to the onset of symptoms. A connection with food intake can suggest: if symptoms appear after eating, the problem is most likely related to the gallbladder or stomach. If the symptoms are not clearly related to eating, there is reason to assume a problem with the intestines.
When examining the abdomen, the doctor can easily determine what exactly led to the onset of symptoms. A connection with food intake can suggest: if symptoms appear after eating, the problem is most likely related to the gallbladder or stomach. If the symptoms are not clearly related to eating, there is reason to assume a problem with the intestines.
Symptoms
Typical symptoms of gallbladder disease are discomfort or pain in the upper abdomen or right under the ribs, often associated with eating. Many people experience mild nausea, a bitter taste in the mouth, heaviness under the ribs, or an aching sensation. Most often they occur when the gallbladder is provoked by fatty, fried, spicy or smoked foods. However, they can also develop a few days after taking antibiotics, antifungal and antiviral drugs.
Chronic cholecystitis develops for a long time and slowly, often manifests itself as discomfort and pain. Acute cholecystitis has more severe symptoms, the temperature may even rise, the pains make you sit bent over and hold on to your right side, sometimes even give to the dorsal. And I want to go to the doctor. Most often, these symptoms are quite typical in most people.
And I want to go to the doctor. Most often, these symptoms are quite typical in most people.
Cholecystitis, in its essence, is an inflammation of the gallbladder, which is accompanied by both a violation of its contractions and a violation of bile secretion.
It is the violation of normal bile secretion that leads to an increase in pressure in the bladder, concentration and thickening of bile. It begins to collect in clots, flakes and lumps appear, which crystallize in the form of stones in the bladder. If cholecystitis is not treated, it can become acute or stones will appear in the bladder. We call this sequential change of stages the "bilious continuum."
Lifestyle does NOT significantly affect the state of the gallbladder or the development of an inflammatory process in it. Of greater importance is nutrition, as well as taking medications that are excreted along with bile.
The relationship of stress and increased anxiety with contractions of the gallbladder is important. Very often, an emotional breakdown or nervous period can lead to the development of the disease.
Very often, an emotional breakdown or nervous period can lead to the development of the disease.
Recommendations
Table No. 5 is recommended for diseases of the gallbladder. It is also used in the treatment of diseases of the liver and pancreas. Nutrition for diseases of the stomach or intestines is different from the nutrition needed for diseases of the gallbladder. The main restrictions apply to fatty, fried, spicy and smoked foods, as well as alcohol. We have developed a special application for the phone "Table No. 5", which covers nutrition in detail.
Cold and hunger are used to treat the most acute period of acute pancreatitis, which sometimes occurs due to cholelithiasis. Therefore, there is such a stereotype. Also, hunger is sometimes used for biliary colic. With an exacerbation of cholecystitis (not acute cholecystitis!) The standard of care is drugs that restore contractions of the gallbladder and ursodeoxycholic acid preparations (ursosan). In the initial period of exacerbation, antispasmodics are used (mebeverine, drotaverine, gimecromon). Further, it is possible to use prokinetics (itomed), but they are not used for cholelithiasis, only in the early stages. These drugs normalize bile secretion. It is strictly forbidden to use cholagogue without ultrasound results!
Further, it is possible to use prokinetics (itomed), but they are not used for cholelithiasis, only in the early stages. These drugs normalize bile secretion. It is strictly forbidden to use cholagogue without ultrasound results!
This recommendation is not a guideline for treatment - treatment should be prescribed by a doctor after examination!
In some cases, indeed, diseases of other organs can lead to the development of cholecystitis. Duodenitis is the most common disease, which, due to the edema of the "exit" of the biliary tract, leads to a violation of the secretion of bile. This increases the pressure in the gallbladder, causing inflammation or gallstones. Also contributing to cholecystitis and gallbladder dysfunction is an excess of bacteria in the intestines, the so-called bacterial overgrowth. This condition can occur after food poisoning, with long-term constipation or prolonged diarrhea, as well as with inflammatory bowel disease and diverticular disease.
This unpleasant symptom can manifest itself in different ways: pain in the right side of the body is sharp, pulling, appearing during active movement or at rest. Why is this happening and how to understand that it's time to see a doctor? We tell together with GMS Clinic surgeon Bulat Yunusov.
Why can the right side hurt?
The causes of this symptom are usually related to the internal organs. “This is a sign that something located on the right side of the abdomen is suffering,” says Bulat Yunusov, a surgeon at GMS Clinics and Hospitals. “The cause of lesions of these organs can also be different, for example, inflammation, oncological processes, injuries, the consequences of previous operations, neurological disorders.”
However, there may be other reasons for this symptom. “An unpleasant sensation in the right side can be of a muscular nature, especially if it occurs after physical exertion. If a person has fallen on their right side, the pain may be associated with muscle contusion or injury, such as myositis. Gallstones can also cause an unpleasant tingling sensation in the side. The stones close the ducts, which leads to swelling of the bladder and, as a result, to the occurrence of calculous cholecystitis, that is, an inflammatory process. All this, of course, is accompanied by pain, ”commented an invited specialist from another medical center. Consider the main causes of pain in the right side.
Gallstones can also cause an unpleasant tingling sensation in the side. The stones close the ducts, which leads to swelling of the bladder and, as a result, to the occurrence of calculous cholecystitis, that is, an inflammatory process. All this, of course, is accompanied by pain, ”commented an invited specialist from another medical center. Consider the main causes of pain in the right side.
Inflammatory diseases of the gastrointestinal tract
Pain and cramps in the right side can be caused by a whole bunch of inflammatory processes in the gastrointestinal tract. “This is, for example, appendicitis, diverticulitis, colitis, gastroenteritis, gastric and duodenal ulcers,” says Bulat Yunusov.
Most often, with these diagnoses, the pain is felt as aching, moderate, with gradually increasing intensity. With appendicitis, pain can increase with walking, coughing, changing body position and decrease at rest. Also, with this diagnosis, there is an increase in temperature, nausea, vomiting.
Stomach ulcer pain becomes more noticeable after eating fatty, spicy or fried foods, alcohol, and intense physical exertion. Additional symptoms may include heartburn, nausea, and vomiting.
In colitis (inflammation of the intestines), the pain may be pulling or paroxysmal. The disease is also accompanied by diarrhea, fever, general weakness, headaches, and the presence of mucus in the feces.
With diverticulitis (protrusion of the walls of the intestine), there is a sharp pain to the right of the navel, the temperature rises, diarrhea appears (with blood and mucus).
In gastroenteritis (inflammation of the mucous membrane of the stomach and small intestine), pain in the right side is accompanied by lack of appetite, nausea, vomiting, abdominal cramps, etc.
In pancreatitis (inflammation of the pancreas), pain begins suddenly and is constant and intense. Sometimes it can "give" to the left side or intensify after eating heavy, fatty or spicy foods.
Diseases of the urinary system
Often the side on the right side hurts because of the organs of the excretory system. “These include urolithiasis and pyelonephritis,” says Bulat Yunusov.
Pyelonephritis is an inflammatory disease of the kidneys, in which, in addition to pain in the right side, weakness, nausea, vomiting, “jumping” pulse, dry mouth, high temperature can also occur.
Pain in the side with urolithiasis may be constant or undulating, dull or sharp, may only bother at rest or worse when walking. It depends on the location of the stone, but sometimes pain can first be felt in the lumbar region (the so-called "renal colic"), and only then "settle" in the right side.
Liver diseases
“Pain in the right side can occur with damage to the liver and organs of the hepatobiliary system,” notes Bulat Yunusov. “Such diseases include cholecystitis, obstructive jaundice, liver cysts, hepatitis, cirrhosis.” All these diagnoses are characterized by a rather sharp pain in the right side, which can “radiate” to the right shoulder, neck or shoulder blade.
Often on the right side below it hurts in women due to malfunctions of the pelvic organs. “Such disorders in work include inflammatory diseases (salpingitis, salpingoophoritis) and non-inflammatory diseases (corpus luteum cyst, ovarian tumors, endometriosis, ovarian cysts, ectopic pregnancy),” notes Bulat Yunusov.
With salpingitis (inflammation of the fallopian tubes) and salpingo-oophoritis (inflammation of the fallopian tubes and ovaries), the pain is most often felt as pulling in the groin area, but can also “give” to the right or left side. Accompanied by fever, nausea, severe headache, vaginal discharge and aggravated during sexual intercourse.
With ovarian or corpus luteum cysts, drawing or stabbing pain is mainly localized in the lower abdomen or lower back, but can also be felt in the right side.
With endometriosis, the pain is most often acute, cramping, and may disappear and return. It is felt, as a rule, in the lower abdomen, in the left or right side (closer to the lower back).
Reaction to physical activity
Sometimes the right side hurts not because of failures in the internal organs (which we discussed above). If you feel pain on the right during (or immediately after) physical activity, there is a possibility that it is:
- Muscle spasm due to weakness of the muscles of the back or peritoneum.
- Spasm of the diaphragm. It is most often encountered while running: rapid breathing causes the diaphragm to contract faster, which can cause it to spasm and "give" pain in the right side.
- Increased liver function. This organ is considered the "blood" depot of the body. During training, the liver may increase slightly in volume and “press” on its outer capsule, where there are many nerve endings, which will be felt as pain in the right side. And such discomfort can also arise due to an improper diet: for example, if you “went over” with carbohydrates or fats before training. In this case, during the session, the liver will be forced to work with an increased load, which can also provoke pain.

How to determine why you have pain in your right side
Of course, you cannot make an accurate diagnosis on your own. However, you can get some idea about it, starting from how exactly your right side hurts. “In acute diseases, pain occurs suddenly, increasing in intensity in a short period of time (hours, sometimes days), Bulat Yunusov notes. “If the cause is some kind of chronic disease, then the pain syndrome is either permanent or undulating, without being very intense.”
It is also important to check for additional symptoms. “In order to correctly determine the cause of pain in the right side, it is necessary to listen to the nature of this pain. For example, pain of a muscular nature, as a rule, is dull and aching, - commented the invited specialist. - However, muscle pain can be acute, because in addition to the muscles in the right side there are intervertebral joints, which can be a source of discomfort. In cholelithiasis or acute cholecystitis, fever is added to the pain. This situation can be called "pain-plus" - pain and temperature. The discomfort caused by renal colic can also be “pain-plus”, but already pain plus frequent urination or the presence of blood in the urine. Pain caused by bowel problems - pain plus diarrhea.
This situation can be called "pain-plus" - pain and temperature. The discomfort caused by renal colic can also be “pain-plus”, but already pain plus frequent urination or the presence of blood in the urine. Pain caused by bowel problems - pain plus diarrhea.
What to do if you have pain in your right side
As you can see, pain in your side can be a symptom of a variety of health problems. Therefore, you should not ignore it - be sure to see a doctor. “Not always the severity of the disease that caused the situation can be determined by the nature of the pain syndrome. This applies, first of all, to the elderly and patients suffering from diabetes mellitus - serious diseases of the abdominal cavity can be erased (the pain syndrome may not be expressed at all or disappear completely), says Bulat Yunusov. – Thus, if abdominal pain does not go away within a few hours and is accompanied by fever, nausea, vomiting, loss of appetite, stool disorders (constipation or diarrhea), discomfort when urinating, lowering blood pressure, then the only right decision is a face-to-face consultation doctor. "
"
Can you take medicine if you have severe pain in your right side? Yes, but with caution. “You should not resort to taking analgesics on your own, as this can “lubricate” the clinical picture of the disease, which will lead to an untimely correct diagnosis,” says Bulat Yunusov. “The only thing is that it is possible to take antispasmodics (for example, no-shpy): these drugs relieve spasm of the muscles of the internal organs and are aimed at eliminating the cause of the pain syndrome, while in inflammatory diseases they, as a rule, do not give an analgesic effect.”
In general, doctors have a negative attitude towards self-medication. “At home, it is impossible to guarantee pain relief without harm to the body as a whole. You can dull the feeling of discomfort, thereby alleviating your torment only for a while. In addition, by self-medicating, quite unintentionally, you can cripple some other organ, which initially had nothing to do with pain in the right side. Treating at home is not a safe remedy for the problem. ”
”
The best way out is to make an appointment with a general practitioner and discuss your condition with him. Sometimes you can solve the problem "on a remote site". “To understand the conditions that are accompanied by an undulating course with dull pain for a long time, it is possible with a remote consultation,” sums up Bulat Yunusov.
Sudden severe abdominal pain (also known as acute abdominal pain) is a symptom of many diseases.
This is usually sudden and severe pain. Sometimes the discomfort gets worse over several days. Often the pain is well limited and worsens with coughing, movement, or changes in body position. Such pain usually indicates an acute illness requiring urgent medical attention, including in some cases emergency surgery.
Causes of severe abdominal pain
There are many possible causes of sudden severe abdominal pain. The most common of these are intra-abdominal or pelvic diseases, for example:
- appendicitis;
- perforation of the gastrointestinal tract;
- diverticulosis of the colon;
- acute gastroenteritis;
- biliary colic;
- acute cholecystitis;
- acute cholangitis;
- acute pancreatitis;
- stones in the kidneys;
- acute pyelonephritis;
- acute cystitis;
- mesenteric artery embolism;
- visceral vein thrombosis;
- abdominal aortic aneurysm.

In addition, in women, acute abdominal pain can cause:
Occasionally, sudden severe abdominal pain is a symptom of metabolic or non-abdominal diseases, such as:
- myocardial infarction;
- inflammation of the heart muscle or pericardium;
- pneumonia and pleurisy;
- pulmonary embolism;
- elevated blood calcium levels;
- thyroid or adrenal crisis;
- food hypersensitivity;
- porphyria;
- ketoacidosis.
There are many more causes of acute abdominal pain, so diagnosing the cause of the pain can be difficult.
How common is sudden severe abdominal pain?
Sudden severe abdominal pain is relatively common. Considering how many diseases can lead to acute abdominal pain, it would be fair to say that most patients experience it at least once in their lives.
How does sudden severe abdominal pain present?
Acute abdominal pain is characterized by a sudden onset. Usually it is a strong, well-defined pain, which is most felt in the affected area. It worsens when you move, cough, breathe, or change body position. The pain may be accompanied by other symptoms, such as fever, vomiting, diarrhea, gas, and pain when urinating.
Usually it is a strong, well-defined pain, which is most felt in the affected area. It worsens when you move, cough, breathe, or change body position. The pain may be accompanied by other symptoms, such as fever, vomiting, diarrhea, gas, and pain when urinating.
When examining a patient with acute abdominal pain, a doctor may find increased abdominal muscle tone as well as other abnormalities depending on the cause of the symptoms (eg, palpable abdominal resistance in case of swelling, symptoms consistent with renal colic, or cholecystitis).
What should I do if I have sudden severe abdominal pain?
In case of sudden severe pain in the abdomen, seek immediate medical attention. If symptoms get worse over several days and are not very severe, you may want to visit a gastroenterologist first, who will decide if further diagnosis and treatment is needed. However, if the pain is very severe and is accompanied by other alarming symptoms, you should go to the hospital or call an ambulance.
How does a doctor diagnose sudden severe abdominal pain?
How a doctor diagnoses sudden severe abdominal pain
A doctor diagnoses acute abdominal pain based on symptoms reported by the patient and a physical examination of the abdomen.
Sudden severe abdominal pain is only a non-specific symptom of many diseases. Therefore, it is necessary to diagnose the cause of the pain. This usually requires laboratory tests (including morphology, C-reactive protein, urinalysis, and others depending on the specific clinical situation) and imaging tests.
The main imaging study is an abdominal ultrasound. Sometimes it is also necessary to perform other tests, such as an abdominal CT scan, an x-ray of the abdomen or chest.
How to treat sudden severe abdominal pain?
Treatment of acute abdominal pain depends on the underlying cause.
- Pain medication can be given to each symptomatic patient.
- In addition, antibiotic therapy or other causative measures may be required.
 For example, the treatment of a heart attack, manifested in the form of epigastric pain.
For example, the treatment of a heart attack, manifested in the form of epigastric pain. - Some conditions presenting with acute abdominal pain require surgical treatment. For example, an aneurysm of the abdominal aorta, perforation of the gastrointestinal tract, or acute appendicitis.
Is it possible to completely cure sudden severe abdominal pain?
Acute abdominal pain usually disappears after symptomatic treatment - painkillers, diastolic drugs. However, first of all, it is important to effectively treat the cause of the pain.
As a rule, treatment with appropriate means leads to the recovery of the patient. However, some diseases that present with severe abdominal pain should be considered life-threatening, such as abdominal aortic aneurysm, mesenteric artery embolism.
What to do after stopping treatment for sudden severe abdominal pain?
Further treatment depends on the cause of acute abdominal pain. Some patients may not require further diagnosis and treatment, such as a single episode of acute cystitis in a healthy woman. However, most patients will need to be monitored in the clinic. The frequency of visits and control tests is determined by the attending physician individually.
However, most patients will need to be monitored in the clinic. The frequency of visits and control tests is determined by the attending physician individually.
Sudden severe abdominal pain (also known as acute abdominal pain) is a symptom of many diseases.
This is usually sudden and severe pain. Sometimes the discomfort gets worse over several days. Often the pain is well limited and worsens with coughing, movement, or changes in body position. Such pain usually indicates an acute illness requiring urgent medical attention, including in some cases emergency surgery.
Causes of severe abdominal pain
There are many possible causes of sudden severe abdominal pain. The most common of these are intra-abdominal or pelvic diseases, for example:
- appendicitis;
- perforation of the gastrointestinal tract;
- diverticulosis of the colon;
- acute gastroenteritis;
- biliary colic;
- acute cholecystitis;
- acute cholangitis;
- acute pancreatitis;
- kidney stones;
- acute pyelonephritis;
- acute cystitis;
- mesenteric artery embolism;
- visceral vein thrombosis;
- abdominal aortic aneurysm.

In addition, in women, acute abdominal pain can cause:
Occasionally, sudden severe abdominal pain is a symptom of metabolic or non-abdominal diseases, such as:
- myocardial infarction;
- inflammation of the heart muscle or pericardium;
- pneumonia and pleurisy;
- pulmonary embolism;
- elevated blood calcium level;
- thyroid or adrenal crisis;
- food hypersensitivity;
- porphyria;
- ketoacidosis.
There are many more causes of acute abdominal pain, so diagnosing the cause of the pain can be difficult.
How common is sudden severe abdominal pain?
Sudden severe abdominal pain is relatively common. Considering how many diseases can lead to acute abdominal pain, it would be fair to say that most patients experience it at least once in their lives.
How does sudden severe abdominal pain manifest itself?
Acute abdominal pain is characterized by a sudden onset. Usually it is a strong, well-defined pain, which is most felt in the affected area. It worsens when you move, cough, breathe, or change body position. The pain may be accompanied by other symptoms, such as fever, vomiting, diarrhea, gas, and pain when urinating.
Usually it is a strong, well-defined pain, which is most felt in the affected area. It worsens when you move, cough, breathe, or change body position. The pain may be accompanied by other symptoms, such as fever, vomiting, diarrhea, gas, and pain when urinating.
When examining a patient with acute abdominal pain, a doctor may find increased abdominal muscle tone as well as other abnormalities depending on the cause of the symptoms (eg, palpable abdominal resistance in case of swelling, symptoms consistent with renal colic, or cholecystitis).
What should I do if I have sudden severe abdominal pain?
In case of sudden severe pain in the abdomen, seek immediate medical attention. If symptoms get worse over several days and are not very severe, you may want to visit a gastroenterologist first, who will decide if further diagnosis and treatment is needed. However, if the pain is very severe and is accompanied by other alarming symptoms, you should go to the hospital or call an ambulance.
How does a doctor diagnose sudden severe abdominal pain?
How a doctor diagnoses sudden severe abdominal pain
A doctor diagnoses acute abdominal pain based on symptoms reported by the patient and a physical examination of the abdomen.
Sudden severe abdominal pain is only a non-specific symptom of many diseases. Therefore, it is necessary to diagnose the cause of the pain. This usually requires laboratory tests (including morphology, C-reactive protein, urinalysis, and others depending on the specific clinical situation) and imaging tests.
The main imaging study is an abdominal ultrasound. Sometimes it is also necessary to perform other tests, such as an abdominal CT scan, an x-ray of the abdomen or chest.
How to treat sudden severe abdominal pain?
Treatment of acute abdominal pain depends on the underlying cause.
- Pain medication can be given to each symptomatic patient.
- In addition, antibiotic therapy or other causative measures may be required.
 For example, the treatment of a heart attack, manifested in the form of epigastric pain.
For example, the treatment of a heart attack, manifested in the form of epigastric pain. - Some conditions presenting with acute abdominal pain require surgical treatment. For example, an aneurysm of the abdominal aorta, perforation of the gastrointestinal tract, or acute appendicitis.
Is it possible to completely cure sudden severe abdominal pain?
Acute abdominal pain usually disappears after symptomatic treatment - painkillers, diastolic drugs. However, first of all, it is important to effectively treat the cause of the pain.
As a rule, treatment with appropriate means leads to the recovery of the patient. However, some diseases that present with severe abdominal pain should be considered life-threatening, such as abdominal aortic aneurysm, mesenteric artery embolism.
What to do after stopping treatment for sudden severe abdominal pain?
Further treatment depends on the cause of acute abdominal pain. Some patients may not require further diagnosis and treatment, such as a single episode of acute cystitis in a healthy woman. However, most patients will need to be monitored in the clinic. The frequency of visits and control tests is determined by the attending physician individually.
However, most patients will need to be monitored in the clinic. The frequency of visits and control tests is determined by the attending physician individually.
Punched in the stomach. In Kudrovo, a woman sent her daughter's 10-year-old classmate to the hospital - December 17, 2021
Society
Incidents
December 17, 2021, 16:30
10 commentsIn the Vsevolozhsk district of the Leningrad region, a fourth-grader was hospitalized with a bruised abdomen. According to preliminary data, the child was crippled by the mother of one of her classmates.
As it became known on December 17 to the regional portal 47news, the night before, a 10-year-old girl was taken from the Kudrovo school to the Rauhfus hospital in St. Petersburg. Doctors examined the juvenile, they did not record any threats to her health.
The police said that the incident was registered with the wording "punched in the stomach. " The prosecutor's office of the Leningrad region is conducting an investigation, at the moment the circumstances of the injury are being clarified.
" The prosecutor's office of the Leningrad region is conducting an investigation, at the moment the circumstances of the injury are being clarified.
The administration of the Vsevolozhsk district gave details of the incident. The parents were waiting for the children at the school. When the classes ended, one of the parents burst into the vestibule and pushed the girl away.
“There is no information about the fact that someone beat someone. According to preliminary information, there is no conflict between the child of this mother and the girl who was injured. We find out what happened, ”said Irina Fedorenko, chairman of the Vsevolozhsk District Education Committee.
The journalists were unable to contact the principal at the time of publication.
Related
- A Petersburger was fined for the second time for forceful education of his beloved. The woman did not live to see the sentence
December 17, 2021, 16:48
- Inflicted 23 stabs while drunk.
 Near Kaliningrad, a man was accused of the brutal murder of a teenage relative
Near Kaliningrad, a man was accused of the brutal murder of a teenage relative December 10, 2021, 16:20
- Petersburger has been looking for a wife for 15 years. All this time she rested in the forest after being hit with a hammer
10 December 2021, 10:12
- A family quarrel near St. Petersburg ended with a katana strike
09 December 2021, 10:53
- A blow to the temple in response to spitting Details of the death of a teenager at school
December 02, 2021, 14:13
- She ran through the window, but did not escape from 85 blows. In St. Petersburg, they sentenced a jealous woman who cut the girl in the bathroom
December 01, 2021, 16:56
- schoolchildren who hit the teacher in the Perm Territory with a knife, they want to send for compulsory treatment
November 30, 2021, 19:06
Surprising2 9000
sad
Comments 10
read all commentsadd a commentJOIN
The brightest photos and videos of the day are in our groups in social networks
- VKontakte
- Telegram
- Yandex.
 Zen
Zen
Did you see a typo? Select a fragment and press Ctrl+Enter
Media news2
report news
Send your news to the editor, tell us about a problem or suggest a topic for publication. Upload your video and photos here.
- Vkontakte group
Company news
Comments10
Company news
1+1 show on OUR Radio with a new presenter!
From October 3, "1 + 1 show" on the air of OUR Radio in St. Petersburg comes out with new headings and in an updated composition. Katya Vinogradova has joined Denis Krasin! Every weekday, from 11 a.m. to 3 p.m., Denis and Katya will share their wonderful mood and good news with the audience, raffle even more prizes and continue to predict fate in rock divination. What will change in the show with the arrival of a new presenter? We decided to ask Katya Vinogradova herself: “I am a very expansive person, so the 1 + 1 show will now acquire a new emotional coloring . ..
..
Union Pay card from Primorye Bank: there is a card - there are no borders!
Recently, we have become accustomed to living in restrictions that make adjustments to our usual way of life. In particular, this applies to trips abroad, where for some time now there has been no usual possibility of paying for trips and accommodation, paying for purchases and withdrawing cash abroad. After it became known that the Visa and MasterCard payment systems were suspending their activities in Russia, the cards of these systems stopped working outside of our country. So how to travel, make work and business trips abroad in the usual way ...
When size matters. In St. Petersburg, a courier carries groceries in a giant backpack
Netizens are actively discussing an unusual way of delivering groceries in St. Petersburg. The footage shows how the courier is carrying a package in a huge, two-meter thermal box. Obviously, a particularly thrifty resident of St. Petersburg appeared in the city. In public transport, the courier turned out to be the most difficult, at rush hour he switched to a scooter. Judging by the inscriptions on the backpack, this is a delivery of the METRO grocery chain. We contacted the press office and learned that couriers with large backpacks are continuing an advertising campaign announcing a massive price reduction that METRO...
Petersburg. The footage shows how the courier is carrying a package in a huge, two-meter thermal box. Obviously, a particularly thrifty resident of St. Petersburg appeared in the city. In public transport, the courier turned out to be the most difficult, at rush hour he switched to a scooter. Judging by the inscriptions on the backpack, this is a delivery of the METRO grocery chain. We contacted the press office and learned that couriers with large backpacks are continuing an advertising campaign announcing a massive price reduction that METRO...
TOP 5
1Last excursion. What were the St. Petersburg guides who died on the Crimean bridge
1,031,863
462In St. Petersburg, the first case of a new terrorism is brewing. In the sight - a physician who returned from Georgia
156 343
583Putin named who blew up the Crimean bridge
152 137
1224SBU declared Sergey Shoigu and Dmitry Medvedev
149 078 9000 105
The sky is again.