When will baby turn head down
Symptoms of Baby Turning Head Down
Your baby kicks, squirms, and flips all day (and night!). But what exactly are they doing in there?
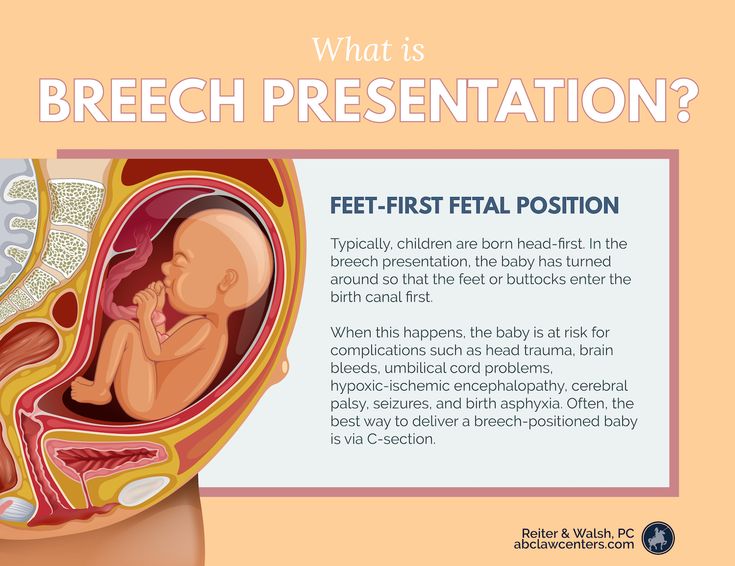
Well, toward the end of your pregnancy, your baby will likely get into a head-down position so that they can begin their descent into the birth canal. The exact timing of when your baby hits this position is individual. And some babies prefer other positions, like breech (head up) or transverse (side lying).
Regardless, some signs can serve as clues about how baby’s relaxing in there. Here’s more about when your baby will move head down, what the options are if they stay head up or in another position, and what to feel for when trying to determine your baby’s position at home.
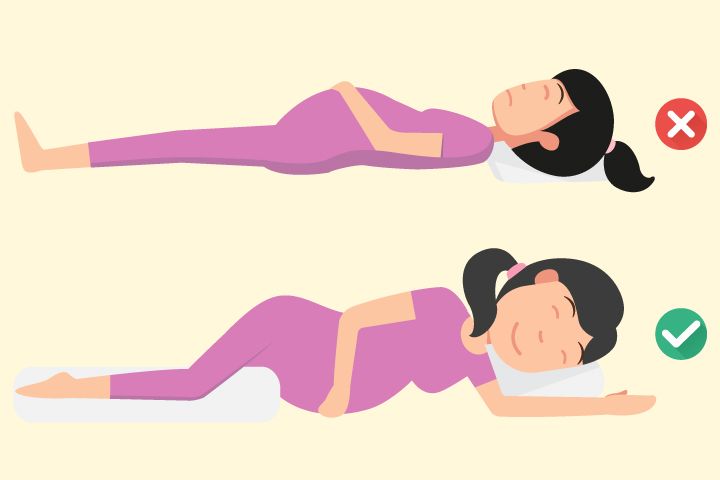
Related: What Sleeping Position Will Help Turn My Breech Baby?
Most babies tend to shimmy their way into a cephalic (head-first) presentation before birth.
Fast fact
At 28 weeks, around 25 percent of babies are breech (head up), but this number jumps down to just 3 or 4 percent at term.
Your baby may move all over the place in the first and second trimesters. Their position may change wildly early on in the third trimester as well.
However, if you’re between 32 and 36 weeks, you may notice your baby staying put in a head-down position. Your uterus grows to accommodate their size — but there’s only so much room. As time passes, your baby gets bigger and starts to run out of space to move into different positions.
Related: The Third Trimester of Pregnancy: Concerns and Tips
Being head down is just half of the equation when it comes to birth. There’s also the matter of which way your baby is facing.
Why does this make a difference? It comes down to geometry. Your baby’s head must fit through the pelvis on its way into the vaginal canal for delivery. Some positions make this journey easier than others, especially considering how different parts of your baby’s skull are wider and narrower than others.
- Occiput anterior: This position is the most common.
 It means that your baby is head down with their back against your stomach and their chin tucked into their chest.
It means that your baby is head down with their back against your stomach and their chin tucked into their chest. - Occiput posterior: This position means that your baby is head down but facing the opposite direction. In this position, your baby’s back is at your back.
Anterior is the ideal position for an uncomplicated vaginal delivery. When your baby’s chin is tucked, it helps the narrowest part of their head go through the birth canal. Posterior presentation can mean a longer or potentially more difficult delivery, sometimes requiring a vacuum, forceps, or cesarean section.
If your baby is posterior even in early labor, they may still turn throughout the process as contractions move them around in the womb. Some babies completely spin to an anterior position during labor while others are born posterior.
Related: What Your Baby’s Position in the Womb Means
You may not experience any signs that your baby has flipped into a head-down position. There’s really no easy way to tell just by looking at your bump. You need to get in there and feel around. But how?
There’s really no easy way to tell just by looking at your bump. You need to get in there and feel around. But how?
Fortunately, your doctor or midwife is trained to feel for your baby’s position using what are called Leopold’s maneuvers.
With this technique, your provider will feel for what part of your baby is presenting in the pelvis, then for your baby’s back, and then for what part of your baby is in your fundus (up high, near your rib cage). They’ll also feel around for your baby’s cephalic prominence, which simply means which way your baby is facing.
With a head-down presentation:
- baby’s head would be in your pelvis
- baby’s back position would depend on whether baby is anterior/posterior, but generally baby will have either their back to your belly (anterior) or your back (posterior)
- baby’s bottom/legs would be in your fundus
All these findings can also be confirmed via ultrasound to give you the clearest picture.
But how can you figure out your baby’s position at home? Pay close attention to the shapes in your belly, as well as the different movements you feel.
Your baby may be head down if you can:
- feel their head low down in your belly
- feel their bottom or legs above your belly button
- feel larger movements — bottom or legs — higher up toward your rib cage
- feel smaller movements — hands or elbows — low down in your pelvis
- feel hiccups on the lower part of your belly, meaning that their chest is likely lower than their legs
- hear their heartbeat (using an at-home doppler or fetoscope) on the lower part of your belly, meaning that their chest is likely lower than their legs
Belly mapping
It can be difficult to read the different lumps and bumps you feel on your stomach. With practice, you may start to understand what you’re feeling. You might even try belly mapping — a process to estimate baby’s position. It was created by Gaily Tully, certified professional midwife and author of SpinningBabies.com.
To use this technique, wait until you are at least 30 weeks pregnant. You may even want to try belly mapping following a prenatal appointment so your doctor can give you some guidance on baby’s position.
You may even want to try belly mapping following a prenatal appointment so your doctor can give you some guidance on baby’s position.
Lie down in bed or on the couch. Using a washable marker or finger paint, gently mark where you feel your baby’s head (it feels like a small bowling ball). The arms and hands are likely near the head, and their tiny movements give them away.
Then feel for the back, butt, and legs, as well as larger movements. You may find it helpful to use a baby doll to play with different possible positions. You can then lightly draw or paint your baby on your stomach to help you visualize how they’re lying.
Related: Can You Give Birth with Baby in the Vertex Position?
If you’re in late pregnancy and have concerns about your baby’s positioning, ask your doctor about it at your next prenatal appointment. Chances are that your healthcare provider is making a note of your baby’s position as well.
If your baby is breech or in some other position besides head down, there are several options for delivery. Factors at play here include:
Factors at play here include:
- whether your baby stays in a certain position as you reach term
- any other pregnancy complications you might have
- when you end up going into labor naturally
Wait-and-see approach
Again, your baby’s position isn’t usually a big concern until you reach between 32 and 36 weeks in your pregnancy. Before that point, the fluid in the uterus gives your baby plenty of space to move around. As you get closer to delivery and your baby hasn’t settled head down, they start to run out of room to make the switch.
Your doctor can monitor your baby’s position at your prenatal appointments by feeling your belly for where their head, back, and buttocks are. To confirm, you may also have an ultrasound or pelvic exam.
External cephalic version (ECV)
External cephalic version (ECV) is a procedure during which your doctor tries to move your baby into a head-down position to increase the chance you’ll have a vaginal birth. This is done in a setting in which baby can be monitored and you can have an emergency cesarean section (C-section) if needed.
This is done in a setting in which baby can be monitored and you can have an emergency cesarean section (C-section) if needed.
Your provider uses their hands to manually turn the baby head down. If you’ve reached 36 weeks and your baby still isn’t head down, your doctor may suggest an ECV.
The success rate of this procedure is around 58 percent. While that’s not a super impressive statistic, ECV may be worth a try if delivering vaginally is important to you.
It’s also worth noting that some babies that are flipped return to a breech position. You can have a repeat ECV, but space runs out the closer you get to birth, so it may be more difficult the second time.
Cesarean delivery (C-section)
A C-section is another option for delivering babies who aren’t head down. It involves major surgery that you may schedule ahead of time (if you know your baby isn’t head down) or that can be performed in the event you go into labor naturally.
Around 85 percent of breech babies are born via C-section. While this surgery is routine, it involves some risks, including:
While this surgery is routine, it involves some risks, including:
- infection
- postpartum hemorrhage
- blood clots
- issues with future pregnancies, like a risk of placenta previa or uterine rupture
Vaginal birth
The American College of Obstetricians and Gynecologists explains that some women may be candidates for a vaginal birth even if their babies are breech. This possibility is determined on a case-by-case basis and involves a review of your medical history and weighing the benefits of vaginal delivery versus the risks of C-section.
If you choose to go this route, you’ll need to follow any specific guidelines set up by your hospital or birth center.
Related: Midwives Are Growing in Popularity: Here’s What You Need to Know
Your baby moves a lot throughout your pregnancy. As you get closer to your due date, they’ll likely settle into a head-down position as they get ready for birth.
If you have concerns about your baby’s position, don’t hesitate to bring them up at your next prenatal appointment. Your healthcare provider is also keeping tabs on whether baby is head down and can help guide you with options for repositioning or an alternate birth plan, if necessary. You’ve got this, mama!
Your healthcare provider is also keeping tabs on whether baby is head down and can help guide you with options for repositioning or an alternate birth plan, if necessary. You’ve got this, mama!
Symptoms of Baby Turning Head Down
Your baby kicks, squirms, and flips all day (and night!). But what exactly are they doing in there?
Well, toward the end of your pregnancy, your baby will likely get into a head-down position so that they can begin their descent into the birth canal. The exact timing of when your baby hits this position is individual. And some babies prefer other positions, like breech (head up) or transverse (side lying).
Regardless, some signs can serve as clues about how baby’s relaxing in there. Here’s more about when your baby will move head down, what the options are if they stay head up or in another position, and what to feel for when trying to determine your baby’s position at home.
Related: What Sleeping Position Will Help Turn My Breech Baby?
Most babies tend to shimmy their way into a cephalic (head-first) presentation before birth.
Fast fact
At 28 weeks, around 25 percent of babies are breech (head up), but this number jumps down to just 3 or 4 percent at term.
Your baby may move all over the place in the first and second trimesters. Their position may change wildly early on in the third trimester as well.
However, if you’re between 32 and 36 weeks, you may notice your baby staying put in a head-down position. Your uterus grows to accommodate their size — but there’s only so much room. As time passes, your baby gets bigger and starts to run out of space to move into different positions.
Related: The Third Trimester of Pregnancy: Concerns and Tips
Being head down is just half of the equation when it comes to birth. There’s also the matter of which way your baby is facing.
Why does this make a difference? It comes down to geometry. Your baby’s head must fit through the pelvis on its way into the vaginal canal for delivery. Some positions make this journey easier than others, especially considering how different parts of your baby’s skull are wider and narrower than others.
- Occiput anterior: This position is the most common. It means that your baby is head down with their back against your stomach and their chin tucked into their chest.
- Occiput posterior: This position means that your baby is head down but facing the opposite direction. In this position, your baby’s back is at your back.
Anterior is the ideal position for an uncomplicated vaginal delivery. When your baby’s chin is tucked, it helps the narrowest part of their head go through the birth canal. Posterior presentation can mean a longer or potentially more difficult delivery, sometimes requiring a vacuum, forceps, or cesarean section.
If your baby is posterior even in early labor, they may still turn throughout the process as contractions move them around in the womb. Some babies completely spin to an anterior position during labor while others are born posterior.
Related: What Your Baby’s Position in the Womb Means
You may not experience any signs that your baby has flipped into a head-down position. There’s really no easy way to tell just by looking at your bump. You need to get in there and feel around. But how?
There’s really no easy way to tell just by looking at your bump. You need to get in there and feel around. But how?
Fortunately, your doctor or midwife is trained to feel for your baby’s position using what are called Leopold’s maneuvers.
With this technique, your provider will feel for what part of your baby is presenting in the pelvis, then for your baby’s back, and then for what part of your baby is in your fundus (up high, near your rib cage). They’ll also feel around for your baby’s cephalic prominence, which simply means which way your baby is facing.
With a head-down presentation:
- baby’s head would be in your pelvis
- baby’s back position would depend on whether baby is anterior/posterior, but generally baby will have either their back to your belly (anterior) or your back (posterior)
- baby’s bottom/legs would be in your fundus
All these findings can also be confirmed via ultrasound to give you the clearest picture.
But how can you figure out your baby’s position at home? Pay close attention to the shapes in your belly, as well as the different movements you feel.
Your baby may be head down if you can:
- feel their head low down in your belly
- feel their bottom or legs above your belly button
- feel larger movements — bottom or legs — higher up toward your rib cage
- feel smaller movements — hands or elbows — low down in your pelvis
- feel hiccups on the lower part of your belly, meaning that their chest is likely lower than their legs
- hear their heartbeat (using an at-home doppler or fetoscope) on the lower part of your belly, meaning that their chest is likely lower than their legs
Belly mapping
It can be difficult to read the different lumps and bumps you feel on your stomach. With practice, you may start to understand what you’re feeling. You might even try belly mapping — a process to estimate baby’s position. It was created by Gaily Tully, certified professional midwife and author of SpinningBabies.com.
To use this technique, wait until you are at least 30 weeks pregnant. You may even want to try belly mapping following a prenatal appointment so your doctor can give you some guidance on baby’s position.
You may even want to try belly mapping following a prenatal appointment so your doctor can give you some guidance on baby’s position.
Lie down in bed or on the couch. Using a washable marker or finger paint, gently mark where you feel your baby’s head (it feels like a small bowling ball). The arms and hands are likely near the head, and their tiny movements give them away.
Then feel for the back, butt, and legs, as well as larger movements. You may find it helpful to use a baby doll to play with different possible positions. You can then lightly draw or paint your baby on your stomach to help you visualize how they’re lying.
Related: Can You Give Birth with Baby in the Vertex Position?
If you’re in late pregnancy and have concerns about your baby’s positioning, ask your doctor about it at your next prenatal appointment. Chances are that your healthcare provider is making a note of your baby’s position as well.
If your baby is breech or in some other position besides head down, there are several options for delivery. Factors at play here include:
Factors at play here include:
- whether your baby stays in a certain position as you reach term
- any other pregnancy complications you might have
- when you end up going into labor naturally
Wait-and-see approach
Again, your baby’s position isn’t usually a big concern until you reach between 32 and 36 weeks in your pregnancy. Before that point, the fluid in the uterus gives your baby plenty of space to move around. As you get closer to delivery and your baby hasn’t settled head down, they start to run out of room to make the switch.
Your doctor can monitor your baby’s position at your prenatal appointments by feeling your belly for where their head, back, and buttocks are. To confirm, you may also have an ultrasound or pelvic exam.
External cephalic version (ECV)
External cephalic version (ECV) is a procedure during which your doctor tries to move your baby into a head-down position to increase the chance you’ll have a vaginal birth.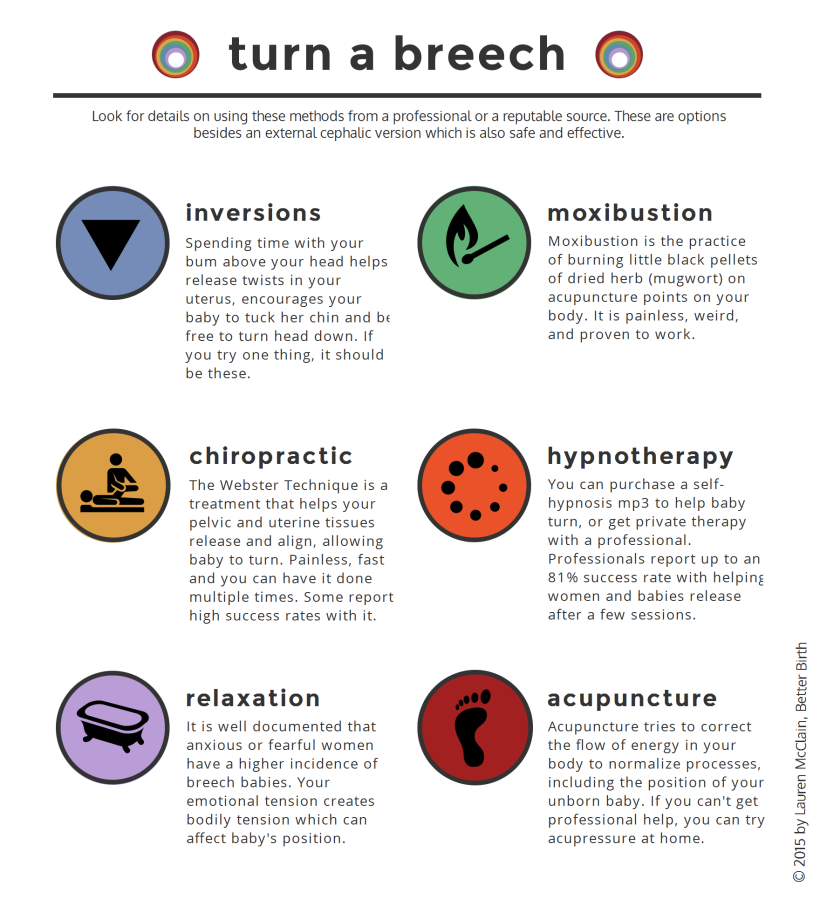 This is done in a setting in which baby can be monitored and you can have an emergency cesarean section (C-section) if needed.
This is done in a setting in which baby can be monitored and you can have an emergency cesarean section (C-section) if needed.
Your provider uses their hands to manually turn the baby head down. If you’ve reached 36 weeks and your baby still isn’t head down, your doctor may suggest an ECV.
The success rate of this procedure is around 58 percent. While that’s not a super impressive statistic, ECV may be worth a try if delivering vaginally is important to you.
It’s also worth noting that some babies that are flipped return to a breech position. You can have a repeat ECV, but space runs out the closer you get to birth, so it may be more difficult the second time.
Cesarean delivery (C-section)
A C-section is another option for delivering babies who aren’t head down. It involves major surgery that you may schedule ahead of time (if you know your baby isn’t head down) or that can be performed in the event you go into labor naturally.
Around 85 percent of breech babies are born via C-section. While this surgery is routine, it involves some risks, including:
While this surgery is routine, it involves some risks, including:
- infection
- postpartum hemorrhage
- blood clots
- issues with future pregnancies, like a risk of placenta previa or uterine rupture
Vaginal birth
The American College of Obstetricians and Gynecologists explains that some women may be candidates for a vaginal birth even if their babies are breech. This possibility is determined on a case-by-case basis and involves a review of your medical history and weighing the benefits of vaginal delivery versus the risks of C-section.
If you choose to go this route, you’ll need to follow any specific guidelines set up by your hospital or birth center.
Related: Midwives Are Growing in Popularity: Here’s What You Need to Know
Your baby moves a lot throughout your pregnancy. As you get closer to your due date, they’ll likely settle into a head-down position as they get ready for birth.
If you have concerns about your baby’s position, don’t hesitate to bring them up at your next prenatal appointment. Your healthcare provider is also keeping tabs on whether baby is head down and can help guide you with options for repositioning or an alternate birth plan, if necessary. You’ve got this, mama!
Your healthcare provider is also keeping tabs on whether baby is head down and can help guide you with options for repositioning or an alternate birth plan, if necessary. You’ve got this, mama!
Non-Children's Baby Neck Problems - Into-Sana
I think that many people have encountered such a problem as the incorrect position of the baby's head. When a child constantly turns his head in the same direction, or tilts it to the same shoulder. In medicine, this condition is called torticollis. According to statistics, every 4-5 newborns have certain signs of an incorrect head position. Parents voice a lot of explanations for this phenomenon: either the child was “lying down”, laying on one side all the time, then they were “tightly swaddled”, then “dad also had it”, then he, that is, the child, “loves so much”). Often, parents do not even think about the true cause of this rather significant problem that requires immediate treatment. And all this postpones a timely visit to the orthopedist for a long time.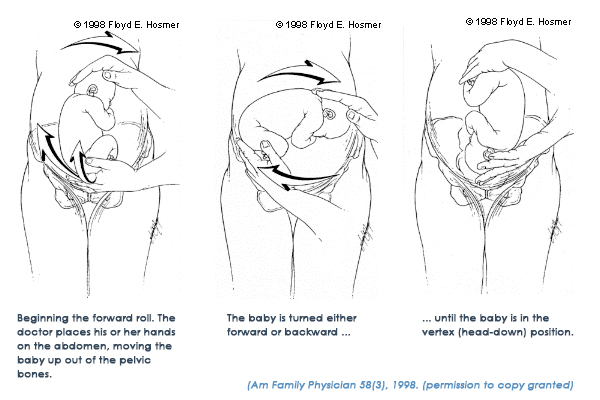
Now more about the pathology itself. There are several reasons for the formation of torticollis in children. It can be congenital and acquired. Today I would like to dwell on the most common cause of acquired torticollis in newborns - this is an injury to the cervical spine during childbirth.
Not only a woman, but also a man knows that childbirth is a difficult process, often very traumatic, and there is always a danger, even during normal childbirth, of mechanical damage to the fetus. And besides the mistakes of obstetricians, this is also facilitated by objective reasons, the pathology of the labor activity itself, a change in the shape and size of the head of the child and the birth canal of the mother.
However, in the process of even physiological childbirth, the generally accepted manipulations of the midwife are often dangerous for the fetus, especially for its cervical spine.
Significantly increase the risk of traumatization of the cervical spine of the newborn:
or, conversely, prolonged labor with drug stimulation
7. emergency caesarean section
emergency caesarean section
8. delivery of a large fetus
9. multiple pregnancy.
One or more of these conditions greatly increase the likelihood of mechanical impact on the fragile neck of the newborn.
But even if there is a minimal deformity of the cervical vertebrae, and it is not detected and treated in time, then in the future it can lead to completely unexpected disorders in the development of brain structures. During growing up and life, the child will experience disturbances in the functions of attention, memory, emotional sphere, complications of the auditory, cardiovascular, endocrine and even immune systems.
With age, these children develop delayed speech development, speech understanding, headaches, behavioral disorders in the form of excessive capriciousness, aggression, and increased motor activity. Autism-like states can form, etc. Muscle tone in these children is usually reduced. With an injury to the upper cervical spinal cord, gait and coordination disorders, vicious foot installations, various types of posture disorders and spinal deformities can be observed, and myopia develops.
What parents should pay attention to
The first thing parents should pay attention to after discharge from the hospital is how the child behaves during any manipulations with the head and neck. Due to provoking pain in the neck, these children do not like to swim, wear caps, prefer the same breast during feeding. The neck in the first days of the child can be shortened, with an abundance of transverse folds, as if pressed into the shoulders, or elongated. The head can be sharply thrown back or turned to the side. These two symptoms may be combined. When you try to bring the head into the correct position, the child cries. There may be tension, soreness, swelling and hardening of the trapezius and posterior cervical muscles.
Sometimes these changes are not rough at first and go unnoticed. Later, under the influence of certain provocations, the previous minimal symptoms become more obvious. As a rule, these children later begin to hold their head in a prone position. They form an asymmetry of the occipital and frontal regions. Due to different muscle tone, infantile scoliosis and asymmetry of the pelvic girdle appear. Gradually, from the stage of rotation, the torticollis passes into the stage of inclination. During this period, attention is drawn to the different distance of the location of the auricles in relation to the shoulders. The head seems to fall to one side.
They form an asymmetry of the occipital and frontal regions. Due to different muscle tone, infantile scoliosis and asymmetry of the pelvic girdle appear. Gradually, from the stage of rotation, the torticollis passes into the stage of inclination. During this period, attention is drawn to the different distance of the location of the auricles in relation to the shoulders. The head seems to fall to one side.
All these symptoms should alert the parents and the family doctor, should serve as a reason for an immediate visit to a pediatric orthopedist.
Remember! The neonatal period determines the entire subsequent life of the child, his mental and physical abilities, and even many of his future illnesses .
However, these neuroorthopedic symptoms are often overlooked or misunderstood. As a result, the most precious days and weeks are missed, when it is still possible to change something, to fix it.
As one of the leading figures in medicine, pediatric neurologist Alexander Yurievich Ratner, said: “Many diseases of older children and even adults are a late retribution for unrecognized troubles of the neonatal period” .
I want to give advice to expectant mothers to prepare the female body for childbirth even at the stage of pregnancy planning.
Particular attention should be paid to the entire pelvic girdle of a woman, its muscles and ligaments, and consult an orthopedist in time to rule out problems in this area responsible for childbirth. It is the presence of a twisted pelvis in the expectant mother that makes it difficult for the fetus to pass through the birth canal. Love your future child right now and do everything so that he is born and grows up healthy.
Dear parents, be attentive to your children, watch the position of your child's head! Better yet, show it to an orthopedist as soon as possible! Especially after complicated childbirth! And together with you we will do our best to keep your child healthy!
Children's orthopedist of the Into-Sana multidisciplinary polyclinic
Mironova Marina Aleksandrovna
Torticollis in children
The baby turns his head to one side all the time - is it torticollis or not?
In the womb, the embryo is in a cramped position and does not have the ability to change the position and tilt of the head. After birth, you can also often notice that the baby always lies with his head turned to one side. This is a habitual tilt of the head (adjusting torticollis). It is corrected by the simplest actions of the parents: you need to put the child to sleep alternately with his head in one or the other direction, take him to the chest from different sides, come up and bring him toys from the “unaccustomed” side.
After birth, you can also often notice that the baby always lies with his head turned to one side. This is a habitual tilt of the head (adjusting torticollis). It is corrected by the simplest actions of the parents: you need to put the child to sleep alternately with his head in one or the other direction, take him to the chest from different sides, come up and bring him toys from the “unaccustomed” side.
Torticollis, as a pathology, is characterized by a constant inclination of the head to one side and its simultaneous turn in the opposite direction. The baby cannot hold his head straight, cries if he tries to turn it in the other direction, the neck can be different from the healthy side and from the damaged side. This is a very common problem, often congenital and diagnosed in the first months of life. It is more common in girls and more often on the right side.
Why does torticollis occur?
In itself, the incorrect position of the head is a symptom that affects both bones, nerve fibers, and soft tissues. The task of a pediatric orthopedist at the first examination is to establish the cause that causes this phenomenon. Torticollis can be:
The task of a pediatric orthopedist at the first examination is to establish the cause that causes this phenomenon. Torticollis can be:
- muscular. The most common option is congenital underdevelopment of the sternocleidomastoid muscle. However, there is also an acquired muscular form associated with muscle injury;
- osteogenic (that is, the root cause lies not in the muscle, but in the bones), when we are dealing with deformed or fused vertebrae;
- neurogenic, caused by muscle hypertonicity, the root cause of which is compression of the nerve roots.
There are other causes of acquired torticollis - for example, a child may turn his head to one side because he hears worse in one ear, or because he has suffered an injury or illness; almost all of them are acquired. Whatever the type of question, you should immediately make an appointment with a pediatric orthopedic doctor. If necessary, a neurologist, traumatologist and other specialists can be involved in the diagnosis.
How is torticollis treated
Only a qualified pediatrician should prescribe any procedures to correct torticollis. Any self-activity in this matter can harm the child. However, parents need to know the main points related to the correction process.
First, the sooner the better. With timely diagnosis, you can get rid of the problem even in infancy and forget about it forever. Therefore, if something worries you in the position of the child's head, it is better to play it safe and go to the children's clinic, without waiting until it goes away on its own. Even if you made a mistake and everything is fine with the child, the price of the mistake is much lower than in the opposite case - there is a problem, but the child was not shown to a specialist.
Second: in the vast majority of cases, conservative treatment is sufficient. children's massage gives the best results. Unfortunately, this procedure does not cause delight in most babies (nerve endings are close, and the baby can cry during the massage), but with each next time it will be easier and easier to bear. Most often, a course or several is enough to get rid of torticollis.
Most often, a course or several is enough to get rid of torticollis.
Massage is sometimes combined with physiotherapy (electrophoresis, paraffin therapy) and exercise therapy. Toddlers with orthopedic problems are often recommended to visit the pool with their mother.
Third: the protocol of conservative treatment sometimes (optionally) includes devices that fix the head in the correct position, especially when the child is lying - a bandage, a helmet. There is no need to be afraid of this: such a device does not cause discomfort to the child, and the protest that the baby expresses is more often associated with the fact that he is not used to wearing it.
Finally, the fourth. Rarely, in the case of congenital muscular torticollis, if conservative treatment fails, surgery may be necessary. Before a year, such operations are not performed. As a rule, the operation is prescribed in the region of 3 years. It is performed by plastic lengthening of the sternocleidomastoid muscle.