How to sleep in first trimester
Sleeping During Pregnancy (for Parents)
Reviewed by: Larissa Hirsch, MD
en español El sueño durante el embarazo
Why Does Pregnancy Sometimes Make Sleeping Difficult?
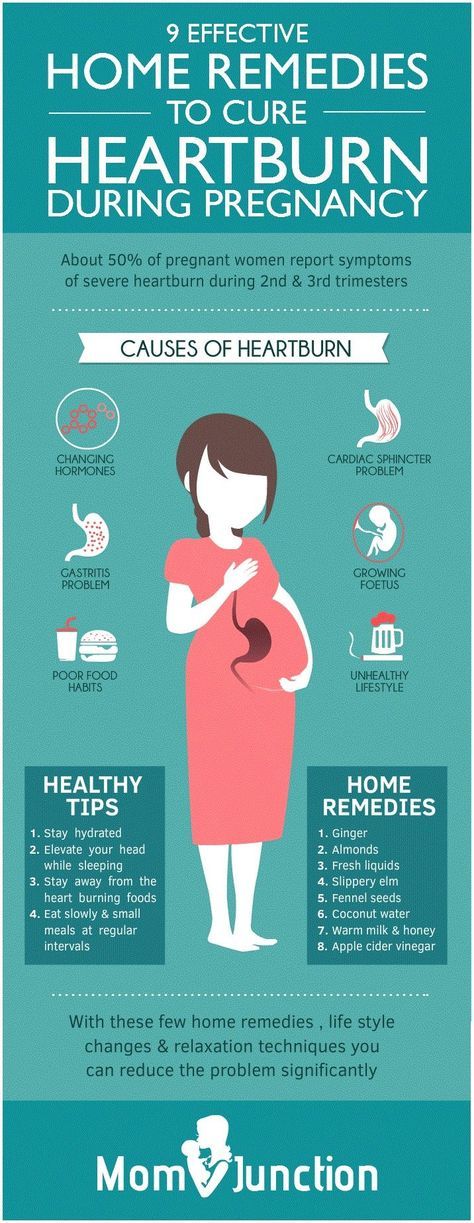
When you're pregnant, it can be hard to get a good night’s sleep. As you get bigger, it gets tougher to find a comfortable sleeping position. You may need to pee in the middle of the night. And heartburn can wake you up.
Some women have leg cramps and backaches, especially as they begin carrying more and more weight. Many pregnant women report that their dreams become more vivid than usual, and some even have nightmares.
Stress can interfere with sleep too. Maybe you're worried about your baby's health, anxious about your abilities as a parent, or feeling nervous about the delivery itself. All these feelings are normal, but they might keep you (and your partner) up at night.
How Can I Get a Better Night’s Sleep?
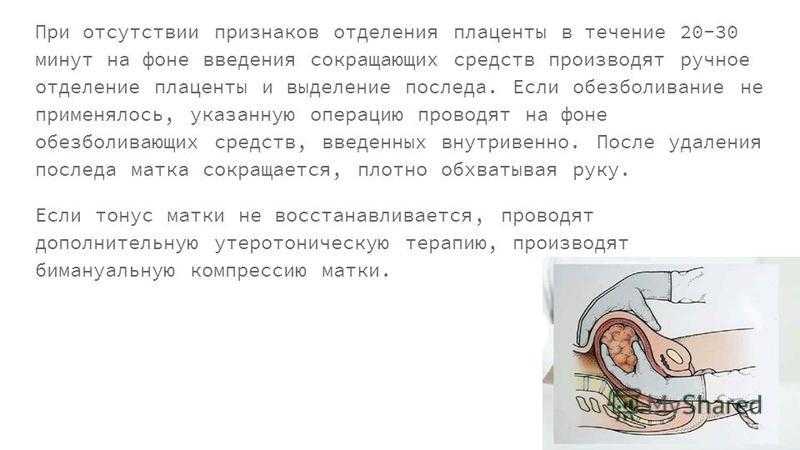
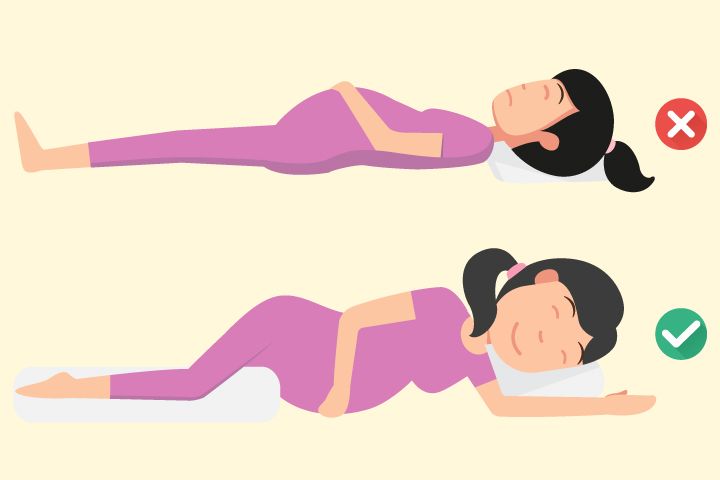
Early in your pregnancy, try to get into the habit of sleeping on your side. Lying on your side with your knees bent is likely to be the most comfortable position as your pregnancy progresses. It also makes your heart's job easier because it keeps the baby's weight from applying pressure to the large vein (called the inferior vena cava) that carries blood back to the heart from your feet and legs.
But don't drive yourself crazy worrying that you might roll over onto your back during the night. Shifting positions is a natural part of sleeping that you can't control.
Try experimenting with pillows to find a comfortable sleeping position. Some women place a pillow under their abdomen or between their legs. Also, using a bunched-up pillow or rolled-up blanket at the small of your back may help to relieve some pressure. In fact, you'll see many "pregnancy pillows" on the market. If you're thinking about buying one, talk with your doctor first about which might work for you.
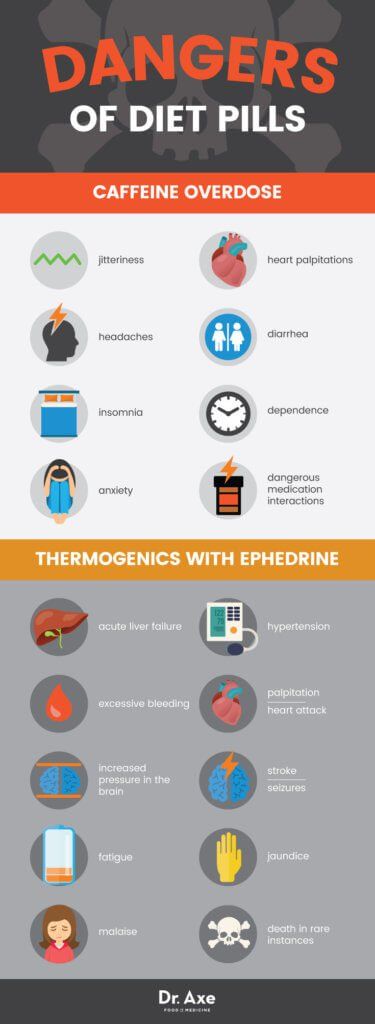
Over-the-counter sleep aids, including herbal remedies, are not recommended for pregnant women.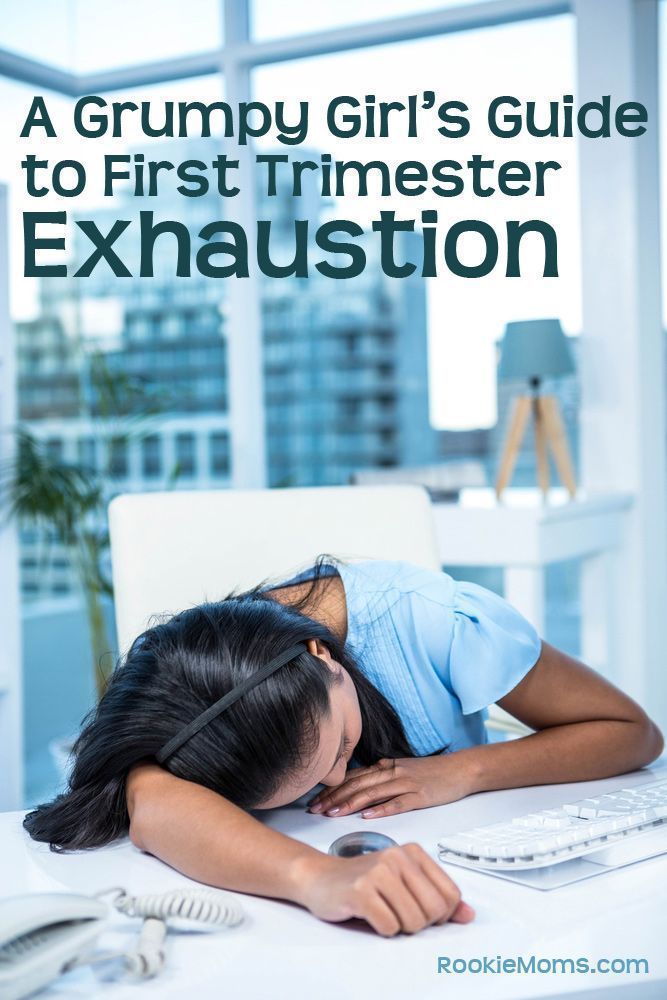
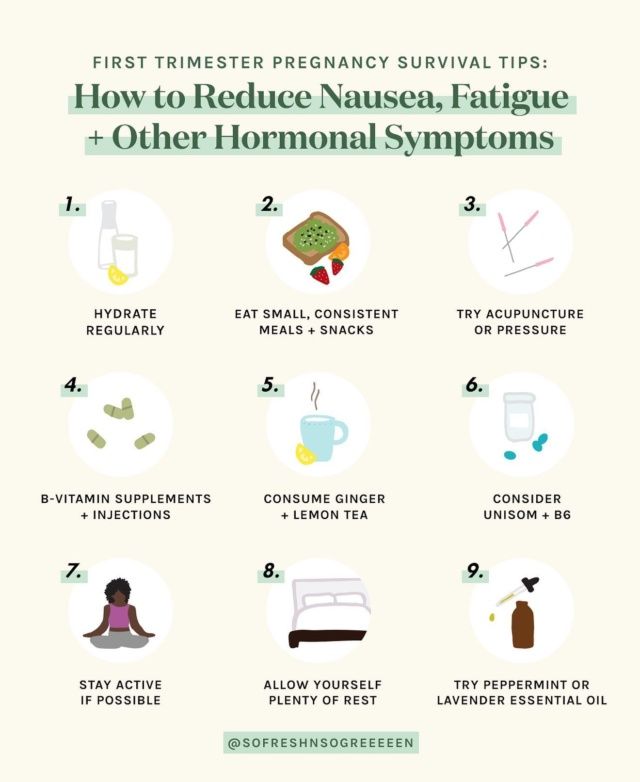
Instead, these tips may safely improve your chances of getting a good night's sleep:
- Cut out caffeinated drinks like soda, coffee, and tea from your diet as much as possible. Restrict any intake of them to the morning or early afternoon.
- Avoid drinking a lot of fluids or eating a full meal within a few hours of going to bed. (But make sure that you also get plenty of nutrients and liquids throughout the day.) Some women find it helpful to eat more at breakfast and lunch and then have a smaller dinner. If nausea keeps you up, try eating a few crackers before you go to bed.
- Get into a routine of going to bed and waking up at the same time each day.
- Avoid rigorous exercise right before you go to bed. Instead, do something relaxing, like reading a book or having a warm, caffeine-free drink, such as milk with honey or a cup of herbal tea.
- If a leg cramp awakens you, it may help to press your feet hard against the wall or to stand on the leg.
 Some women find that stretching their calf muscles before bed helps. Also, make sure that you're getting enough calcium and magnesium in your diet, which can help reduce leg cramps. But don't take any supplements without checking with your doctor.
Some women find that stretching their calf muscles before bed helps. Also, make sure that you're getting enough calcium and magnesium in your diet, which can help reduce leg cramps. But don't take any supplements without checking with your doctor. - Take a yoga class or learn other relaxation techniques to help you unwind after a busy day. (Be sure to discuss any new activity or fitness regimen with your doctor first.)
- If fear and anxiety are keeping you awake, consider enrolling in a childbirth class or parenting class. More knowledge and the company of other pregnant women may help to ease the fears that keep you awake at night.
What If I Still Can't Sleep?
Of course, there will be times when you just can't sleep. Instead of tossing and turning, worrying that you're not asleep, and counting the hours until your alarm clock will go off, get up and do something calm: read a book, listen to music, or look at a magazine. Eventually, you'll probably feel tired enough to get back to sleep.
And if possible, take short naps (30–60 minutes) during the day. Naps can help you have energy to get through the day and give your body the rest it needs.
Reviewed by: Larissa Hirsch, MD
Date reviewed: May 2022
Sleeping While Pregnant 1st Trimester
1.
Ku, C. W., Allen, J. C., Jr, Lek, S. M., Chia, M. L., Tan, N. S., & Tan, T. C. (2018). Serum progesterone distribution in normal pregnancies compared to pregnancies complicated by threatened miscarriage from 5 to 13 weeks gestation: a prospective cohort study. BMC pregnancy and childbirth, 18(1), 360. https://doi.org/10.1186/s12884-018-2002-z
2.
Won C. H. (2015). Sleeping for Two: The Great Paradox of Sleep in Pregnancy. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 11(6), 593–594. https://doi.org/10.5664/jcsm.4760
3.
Martin-Fairey, C. A., Zhao, P., Wan, L. , Roenneberg, T., Fay, J., Ma, X., McCarthy, R., Jungheim, E. S., England, S. K., & Herzog, E. D. (2019). Pregnancy Induces an Earlier Chronotype in Both Mice and Women. Journal of biological rhythms, 34(3), 323–331. https://doi.org/10.1177/0748730419844650
, Roenneberg, T., Fay, J., Ma, X., McCarthy, R., Jungheim, E. S., England, S. K., & Herzog, E. D. (2019). Pregnancy Induces an Earlier Chronotype in Both Mice and Women. Journal of biological rhythms, 34(3), 323–331. https://doi.org/10.1177/0748730419844650
4.
Baumgartel, K. L., Terhorst, L., Conley, Y. P., & Roberts, J. M. (2013). Psychometric evaluation of the Epworth sleepiness scale in an obstetric population. Sleep medicine, 14(1), 116–121. https://doi.org/10.1016/j.sleep.2012.10.007
5.
Lee, K. A., Zaffke, M. E., & McEnany, G. (2000). Parity and sleep patterns during and after pregnancy. Obstetrics and gynecology, 95(1), 14–18. https://doi.org/10.1016/s0029-7844(99)00486-x
6.
Neau, J. P., Texier, B., & Ingrand, P. (2009). Sleep and vigilance disorders in pregnancy. European neurology, 62(1), 23–29. https://doi.org/10.1159/000215877
7.
Okun, M. L., Buysse, D. J., & Hall, M.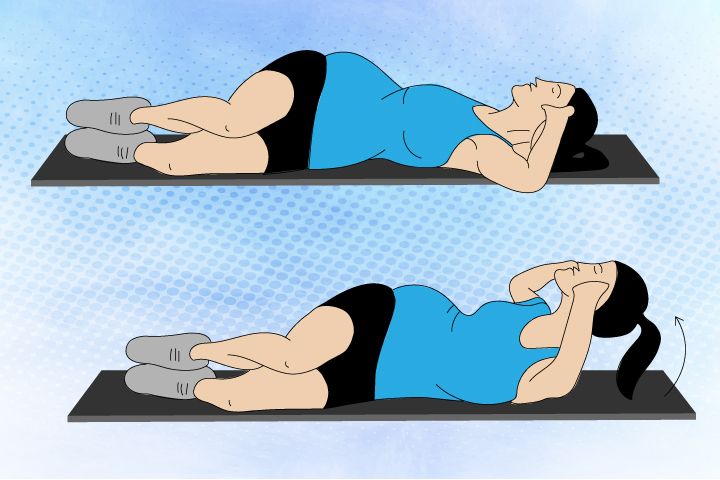 H. (2015). Identifying Insomnia in Early Pregnancy: Validation of the Insomnia Symptoms Questionnaire (ISQ) in Pregnant Women. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 11(6), 645–654. https://doi.org/10.5664/jcsm.4776
H. (2015). Identifying Insomnia in Early Pregnancy: Validation of the Insomnia Symptoms Questionnaire (ISQ) in Pregnant Women. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 11(6), 645–654. https://doi.org/10.5664/jcsm.4776
8.
Bai, G., Korfage, I. J., Groen, E. H., Jaddoe, V. W., Mautner, E., & Raat, H. (2016). Associations between Nausea, Vomiting, Fatigue and Health-Related Quality of Life of Women in Early Pregnancy: The Generation R Study. PloS one, 11(11), e0166133. https://doi.org/10.1371/journal.pone.0166133
9.
Oyiengo, D., Louis, M., Hott, B., & Bourjeily, G. (2014). Sleep disorders in pregnancy. Clinics in chest medicine, 35(3), 571–587. https://doi.org/10.1016/j.ccm.2014.06.012
10.
Gartland, D., Brown, S., Donath, S., & Perlen, S. (2010). Women's health in early pregnancy: findings from an Australian nulliparous cohort study. The Australian & New Zealand journal of obstetrics & gynaecology, 50(5), 413–418. https://doi.org/10.1111/j.1479-828X.2010.01204.x
https://doi.org/10.1111/j.1479-828X.2010.01204.x
11.
Nazik, E., & Eryilmaz, G. (2014). Incidence of pregnancy-related discomforts and management approaches to relieve them among pregnant women. Journal of clinical nursing, 23(11-12), 1736–1750. https://doi.org/10.1111/jocn.12323
12.
Bradley, C. S., Kennedy, C. M., Turcea, A. M., Rao, S. S., & Nygaard, I. E. (2007). Constipation in pregnancy: prevalence, symptoms, and risk factors. Obstetrics and gynecology, 110(6), 1351–1357. https://doi.org/10.1097/01.AOG.0000295723.94624.b1
13.
Gomes, C. F., Sousa, M., Lourenço, I., Martins, D., & Torres, J. (2018). Gastrointestinal diseases during pregnancy: what does the gastroenterologist need to know?. Annals of gastroenterology, 31(4), 385–394. https://doi.org/10.20524/aog.2018.0264
14.
Malfertheiner, S. F., Malfertheiner, M. V., Kropf, S., Costa, S. D., & Malfertheiner, P. (2012). A prospective longitudinal cohort study: evolution of GERD symptoms during the course of pregnancy. BMC gastroenterology, 12, 131. https://doi.org/10.1186/1471-230X-12-131
A prospective longitudinal cohort study: evolution of GERD symptoms during the course of pregnancy. BMC gastroenterology, 12, 131. https://doi.org/10.1186/1471-230X-12-131
15.
Bourjeily, G., Chambers, A., Salameh, M., Bublitz, M. H., Kaur, A., Coppa, A., Risica, P., & Lambert-Messerlian, G. (2019). Anthropometric Measures and Prediction of Maternal Sleep-Disordered Breathing. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 15(6), 849–856. https://doi.org/10.5664/jcsm.7834
16.
Sweet, L., Arjyal, S., Kuller, J. A., & Dotters-Katz, S. (2020). A Review of Sleep Architecture and Sleep Changes During Pregnancy. Obstetrical & gynecological survey, 75(4), 253–262. https://doi.org/10.1097/OGX.0000000000000770
17.
Doyon, M., Pelland-St-Pierre, L., Allard, C., Bouchard, L., Perron, P., & Hivert, M. F. (2020). Associations of sleep duration, sedentary behaviours and energy expenditure with maternal glycemia in pregnancy. Sleep medicine, 65, 54–61. https://doi.org/10.1016/j.sleep.2019.07.008
Sleep medicine, 65, 54–61. https://doi.org/10.1016/j.sleep.2019.07.008
18.
Okada, K., Saito, I., Katada, C., & Tsujino, T. (2019). Influence of quality of sleep in the first trimester on blood pressure in the third trimester in primipara women. Blood pressure, 28(5), 345–355. https://doi.org/10.1080/08037051.2019.1637246
19.
Okun, M. L., Kline, C. E., Roberts, J. M., Wettlaufer, B., Glover, K., & Hall, M. (2013). Prevalence of sleep deficiency in early gestation and its associations with stress and depressive symptoms. Journal of women's health (2002), 22(12), 1028–1037. https://doi.org/10.1089/jwh.2013.4331
20.
Lee, E. K., Gutcher, S. T., & Douglass, A. B. (2014). Is sleep-disordered breathing associated with miscarriages? An emerging hypothesis. Medical hypotheses, 82(4), 481–485. https://doi.org/10.1016/j.mehy.2014.01.031
21.
Medical Encyclopedia: A.D.A.M Medical Encyclopedia.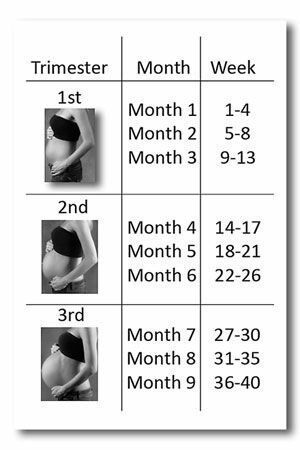 (2018, April 19). Problems sleeping during pregnancy. Retrieved August 27, 2020. https://medlineplus.gov/ency/patientinstructions/000559.htm
(2018, April 19). Problems sleeping during pregnancy. Retrieved August 27, 2020. https://medlineplus.gov/ency/patientinstructions/000559.htm
22.
Miller, M. A., Mehta, N., Clark-Bilodeau, C., & Bourjeily, G. (2020). Sleep Pharmacotherapy for Common Sleep Disorders in Pregnancy and Lactation. Chest, 157(1), 184–197. https://doi.org/10.1016/j.chest.2019.09.026
23.
Lee, K. A., Zaffke, M. E., & Baratte-Beebe, K. (2001). Restless legs syndrome and sleep disturbance during pregnancy: the role of folate and iron. Journal of women's health & gender-based medicine, 10(4), 335–341. https://doi.org/10.1089/152460901750269652
24.
McParlin, C., O'Donnell, A., Robson, S. C., Beyer, F., Moloney, E., Bryant, A., Bradley, J., Muirhead, C. R., Nelson-Piercy, C., Newbury-Birch, D., Norman, J., Shaw, C., Simpson, E., Swallow, B., Yates, L., & Vale, L. (2016). Treatments for Hyperemesis Gravidarum and Nausea and Vomiting in Pregnancy: A Systematic Review.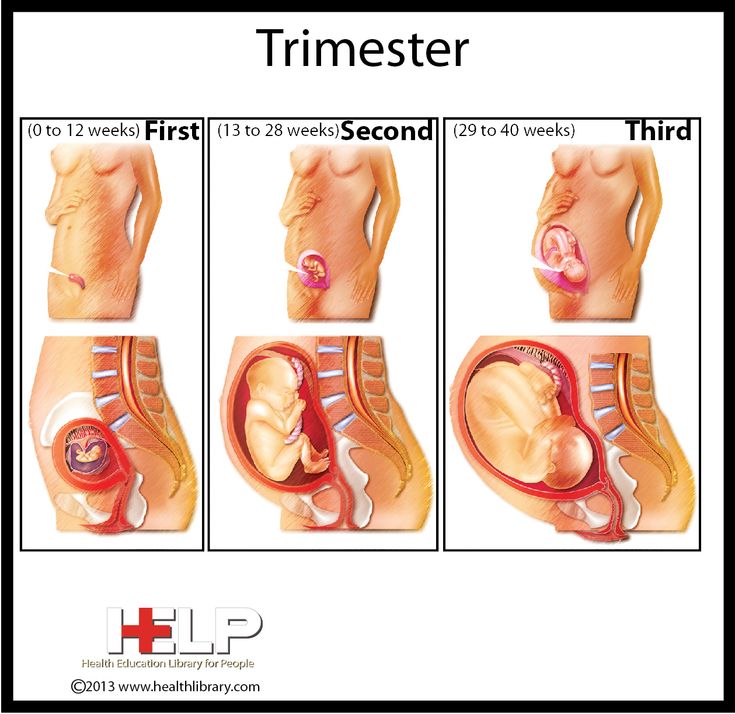 JAMA, 316(13), 1392–1401. https://doi.org/10.1001/jama.2016.14337
JAMA, 316(13), 1392–1401. https://doi.org/10.1001/jama.2016.14337
25.
Lindblad, A. J., & Koppula, S. (2016). Ginger for nausea and vomiting of pregnancy. Canadian family physician Medecin de famille canadien, 62(2), 145. https://pubmed.ncbi.nlm.nih.gov/26884528/
26.
Quach, D. T., Le, Y. T., Mai, L. H., Hoang, A. T., & Nguyen, T. T. (2020). Short Meal-to-Bed Time Is a Predominant Risk Factor of Gastroesophageal Reflux Disease in Pregnancy. Journal of clinical gastroenterology, 10.1097/MCG.0000000000001399. Advance online publication. https://doi.org/10.1097/MCG.0000000000001399
27.
Izci Balserak, B., Jackson, N., Ratcliffe, S. A., Pack, A. I., & Pien, G. W. (2013). Sleep-disordered breathing and daytime napping are associated with maternal hyperglycemia. Sleep & breathing = Schlaf & Atmung, 17(3), 1093–1102. https://doi.org/10.1007/s11325-013-0809-4
28.
Gaston, A., & Prapavessis, H.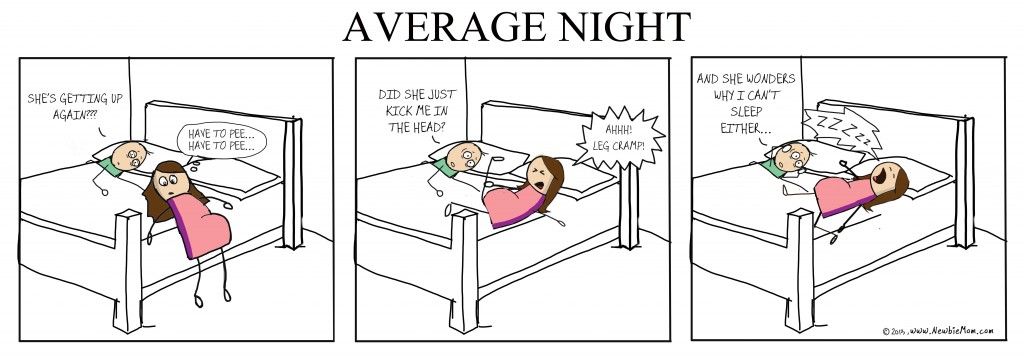 (2013). Tired, moody and pregnant? Exercise may be the answer. Psychology & health, 28(12), 1353–1369. https://doi.org/10.1080/08870446.2013.809084
(2013). Tired, moody and pregnant? Exercise may be the answer. Psychology & health, 28(12), 1353–1369. https://doi.org/10.1080/08870446.2013.809084
29.
Kusaka, M., Matsuzaki, M., Shiraishi, M., & Haruna, M. (2016). Immediate stress reduction effects of yoga during pregnancy: One group pre-post test. Women and birth : journal of the Australian College of Midwives, 29(5), e82–e88. https://doi.org/10.1016/j.wombi.2016.04.003
30.
Rodriguez-Blanque, R., Sánchez-García, J. C., Sánchez-López, A. M., Mur-Villar, N., & Aguilar-Cordero, M. J. (2018). The influence of physical activity in water on sleep quality in pregnant women: A randomised trial. Women and birth : journal of the Australian College of Midwives, 31(1), e51–e58. https://doi.org/10.1016/j.wombi.2017.06.018
How to sleep during pregnancy
It is difficult to overestimate the role of sleep in the life of every person. A complete healthy rest allows you to fully restore the functioning of the nervous system, relieve stress, improve performance and increase activity. Chronic sleep deprivation is the cause of many diseases. What can we say about a woman who is at the stage of bearing a baby. During this period, more than ever, she needs a healthy, long and full sleep. However, unfortunately, it is during this period that one can only dream of a restful sleep.
Chronic sleep deprivation is the cause of many diseases. What can we say about a woman who is at the stage of bearing a baby. During this period, more than ever, she needs a healthy, long and full sleep. However, unfortunately, it is during this period that one can only dream of a restful sleep.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
The cause of insomnia can be :
- Anxiety;
- Frequent urination;
- Fears and phobias before a new stage of one's life;
- Nervousness and irritability;
- Digestive disorder;
- Toxicosis;
- Physical indisposition;
- Uncomfortable posture.
During the period of bearing a child, the female body experiences an extraordinary load, especially in the last trimester.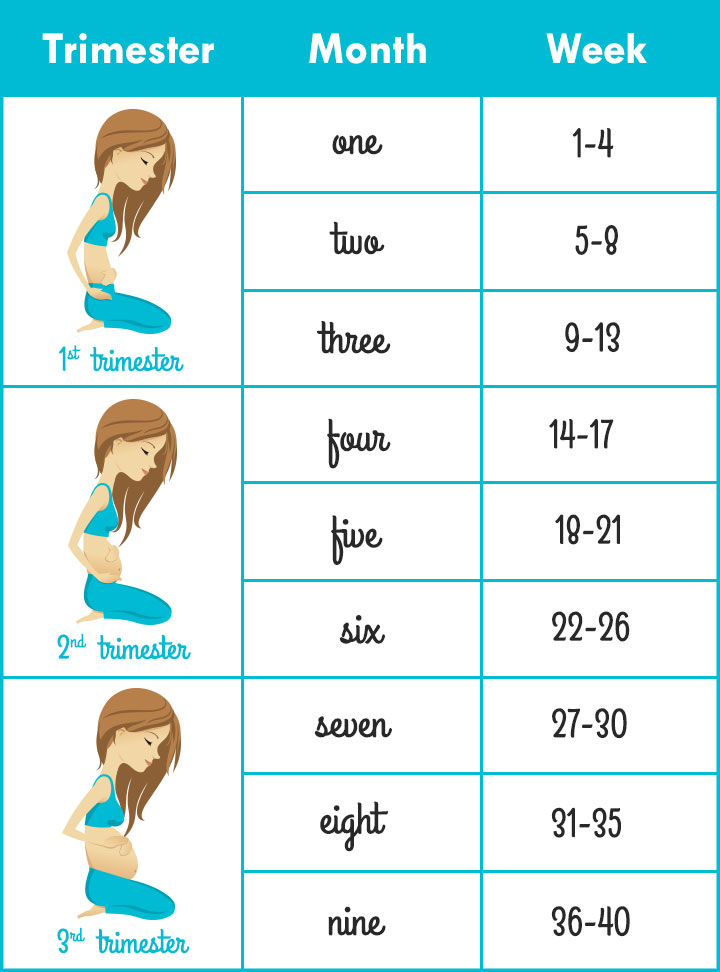 The need for more sleep increases, because the body expends much more energy. Therefore, healthy sleep and pregnancy are inextricably linked.
The need for more sleep increases, because the body expends much more energy. Therefore, healthy sleep and pregnancy are inextricably linked.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
Let's try to figure out how to sleep during pregnancy, so as not only not to harm the health of your unborn baby, but to sleep well.
Looking for a comfortable sleeping position
Each person has his own favorite position, in which it is easy to fall asleep and sleep. Many do not imagine a comfortable rest on their backs, accustomed to sleeping on their stomachs. This habit will have to be sacrificed, as it is unsafe for the normal development of the fetus. If in the first three months of pregnancy a woman can still sleep in the position in which she is used to and feels comfortable, then after the first trimester the growing belly will not allow her to lie safely in this position. Despite the natural protection of the baby in the form of amniotic fluid, there is a high probability of injuring the baby in a dream, squeezing it. But what is the right way to sleep during pregnancy?
Despite the natural protection of the baby in the form of amniotic fluid, there is a high probability of injuring the baby in a dream, squeezing it. But what is the right way to sleep during pregnancy?
Back position
Even if you are used to sleeping in a Spartan position, on your back, with your arms spread wide, from the 28th week you will have to radically change your lifestyle. The fact is that as the fetus grows, the load on the intestines and vena cava will increase significantly, blocking the access of oxygen to the baby.
As soon as a woman finds out about her new position, she has to give up a lot for the sake of the health of her unborn baby. And you need to give up not only bad habits: alcohol, cigarettes, coffee, but also from a comfortable sleep.
If you sleep on your back during pregnancy, you may experience the following problems:
- Dizziness;
- Nausea;
- Convulsions;
- Numb limbs;
- Pressure reduction;
- Hemorrhoids;
- Heaviness of breathing.
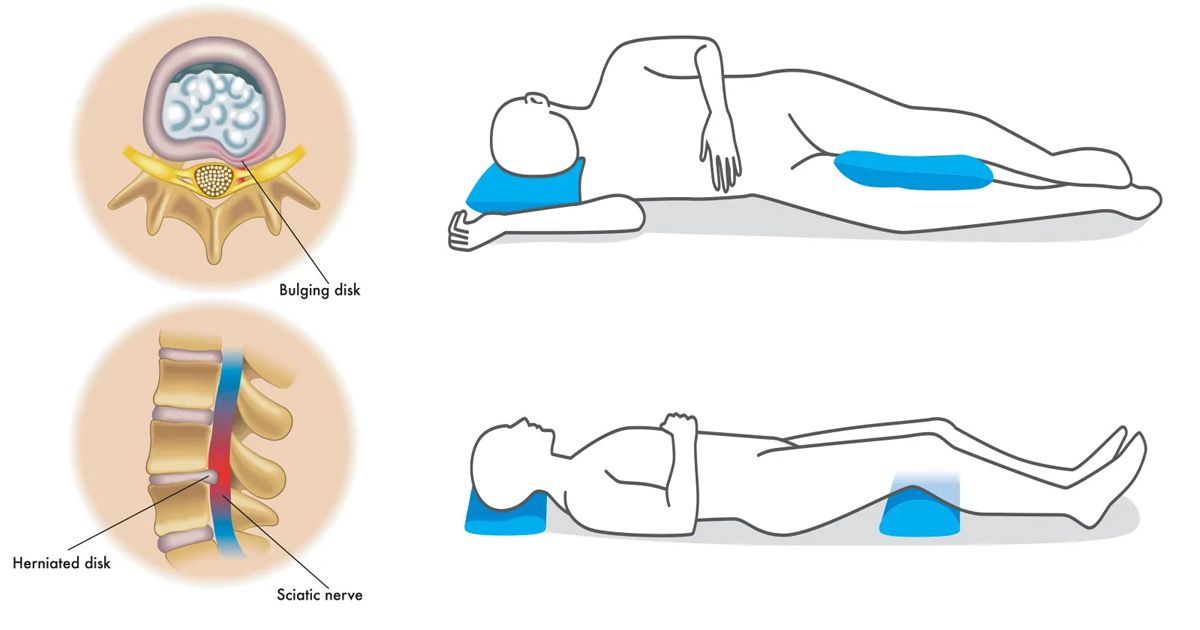
If you feel these symptoms or the baby gives persistent signals, you need to urgently change your position, so squeezing the vena cava is fraught not only with poor health for the mother, but also with a lack of oxygen supply to the fetus.
Stomach position
One of the most beloved positions for many people, which allows you to quickly fall asleep while hugging a pillow. Many women, as soon as they find out about the change in their lives, are interested in the question, is it possible to sleep on your stomach during pregnancy? Doctors recommend abandoning this position already in the first weeks, even before the enlarged belly makes it impossible to fall asleep peacefully.
If you are afraid during sleep, without controlling your movements, to arbitrarily roll over on your stomach, you can put a large pillow that does not allow you to change position.
Side position
In order to normalize your sleep and not harm the health of the baby, experts recommend sleeping on your side during pregnancy. And if at first this option seems unacceptable to many, after the second trimester, lying on your side is the only possible one. But here the question arises, on which side to sleep in order to ensure the safety of the fetus?
And if at first this option seems unacceptable to many, after the second trimester, lying on your side is the only possible one. But here the question arises, on which side to sleep in order to ensure the safety of the fetus?
Sleeping on the right side can cause squeezing of the kidney, which can have dire consequences. The ideal posture is lying on the left side. Thus, you not only do not injure the unborn baby, but also improve blood flow along with oxygen to the placenta.
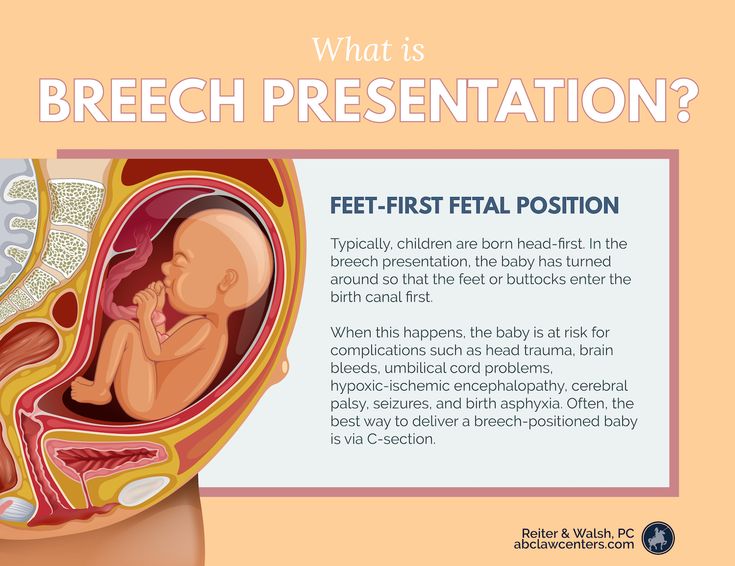
But one should not ignore the individual characteristics of each organism and the position of the fetus in the uterus. When the baby is in a transverse position, choose the side where the baby's head is. And with a breech presentation, doctors recommend changing the position several times a night.
If you still cannot improve your sleep, you feel unwell and you are tormented by insomnia, then it is better to consult a specialist. A good gynecologist will analyze the situation and help solve the problem. If necessary, he will prescribe a safe sedative that stabilizes the emotional state and helps to fall asleep calmly, resting and restoring the nervous system in a dream.
If necessary, he will prescribe a safe sedative that stabilizes the emotional state and helps to fall asleep calmly, resting and restoring the nervous system in a dream.
Help pillow
Fortunately, now modern manufacturers help women survive the pregnancy period with great comfort by offering special pillows. They are made taking into account the physiological characteristics of a woman in this period and allow you to find a comfortable position for relaxation.
You can buy two pillows and put one under your stomach and the other under your knees, looking for your best option. And you can buy a long banana-shaped pillow, which allows you to throw your leg on it while sleeping, which improves well-being and relieves the main load from the lower back and abdomen. Already in the last weeks of pregnancy, when the growing belly does not allow you to breathe normally, the pillow will allow you to take a comfortable half-sitting position.
Remember that pregnancy is your opportunity to gain strength and fully relax before the most crucial period in your life. Childbirth and the first weeks of caring for your baby will require a lot of energy from you, so good luck and sound sleep!
Childbirth and the first weeks of caring for your baby will require a lot of energy from you, so good luck and sound sleep!
Is it possible to sleep on your stomach during pregnancy
Subscribe to our Instagram! Useful information about pregnancy and childbirth from leading obstetricians and gynecologists in Moscow and foreign experts: https://www.instagram.com/roddompravda/
Tips and opinions from leading child professionals: https://www.instagram.com/emc.child/
Many girls like to sleep on their stomachs, moreover, many of them can fall asleep only in this position. When planning a future pregnancy, many people have reasonable questions about whether it is possible for pregnant women to sleep in this position and for how long can this be done? Obstetrician-gynecologist EMC Olga Panfilova answers these and other questions.
Can I sleep on my stomach in the first trimester?
Of course, for good health and mood, a calm and complete rest at night is very important. This is especially true for a woman who is expecting a baby, because it is she who often has problems with sleep, not least related to the positions that she usually takes in a dream. Including the posture on the stomach. However, in the early stages of pregnancy, you can safely continue to do this. The uterus is still so small and, moreover, so well protected by the bones of the pubis, that this position of the body is not capable of causing any harm to the developing baby. If the usual posture began to cause you discomfort, then most likely this is due to the so-called inflection of the uterus, which occurs due to the fact that the tissues of this organ soften, especially in the isthmus zone. Another cause of inconvenience may be the mammary glands, which begin to gradually increase in size, become painful. If you're having similar problems, it's time to find more comfortable sleeping positions, such as trying to fall asleep lying on your back. And even better already in the early stages to accustom yourself to sleep on your side.
This is especially true for a woman who is expecting a baby, because it is she who often has problems with sleep, not least related to the positions that she usually takes in a dream. Including the posture on the stomach. However, in the early stages of pregnancy, you can safely continue to do this. The uterus is still so small and, moreover, so well protected by the bones of the pubis, that this position of the body is not capable of causing any harm to the developing baby. If the usual posture began to cause you discomfort, then most likely this is due to the so-called inflection of the uterus, which occurs due to the fact that the tissues of this organ soften, especially in the isthmus zone. Another cause of inconvenience may be the mammary glands, which begin to gradually increase in size, become painful. If you're having similar problems, it's time to find more comfortable sleeping positions, such as trying to fall asleep lying on your back. And even better already in the early stages to accustom yourself to sleep on your side. You will definitely appreciate the benefits of the newly acquired habit later, when your stomach has reached such a size that even the very thought of trying to sleep on it seems ridiculous.
You will definitely appreciate the benefits of the newly acquired habit later, when your stomach has reached such a size that even the very thought of trying to sleep on it seems ridiculous.
Can I sleep on my stomach in the second trimester?
In the second trimester of pregnancy, the expectant mother can already boast of a voluminous belly, which means that the baby inside has grown up. And even though it is reliably protected by the fetal membranes, amniotic fluid, the muscles of the uterus and the press, laying on the stomach, you still put pressure on the baby. And just imagining that you are lying on your child, you are unlikely to be able to sleep peacefully. At this stage of pregnancy, you can still sleep on your back, but it is best to lie on your side, so you arrange your stomach as comfortably as possible.
Can I sleep on my stomach in the third trimester?
In the third trimester of pregnancy, sleeping on the back of the expectant mother is no longer recommended.