Birth injury to mother
Birth injury (to the mother)
Birth injury (to the mother) | Pregnancy Birth and Baby beginning of content4-minute read
Listen
What is birth injury?
Birth injuries are physical injuries experienced during childbirth, and can affect either the mother or the baby. In newborn babies, a birth injury (often called 'neonatal birth trauma') can include many things, from bruising to a broken bone.
In mothers, birth injuries range from tearing in the vaginal area to damage to the pelvic floor.
Birth injuries in mothers typically fall into 2 main categories:
Injuries to the perineal area
- Perineal tears and episiotomy — around 3 in 4 women who give birth vaginally experience 'perineal trauma' (a tear or surgical cut to the area between the vagina and anus).
- Nerve damage — occasionally, nerves in the perineal area can get damaged during childbirth, which can lead to a painful condition called pudendal neuralgia.
- Haemorrhoids (piles) — these are swollen veins around the anus that you might feel as lumps. While they can be painful or itchy, they are usually not serious.
Injuries to the pelvic floor
- Muscle damage — the 'pelvic floor' is a group of muscles inside the pelvis that helps hold the uterus, bladder and bowel in place. In up to half of all women who give birth vaginally, there are permanent changes to the pelvic floor due to over-stretching or tearing (avulsion).
- Pelvic organ prolapse — if the pelvic muscles are damaged or weakened, the organs inside the pelvis can drop down towards the vagina, causing bladder and bowel problems.
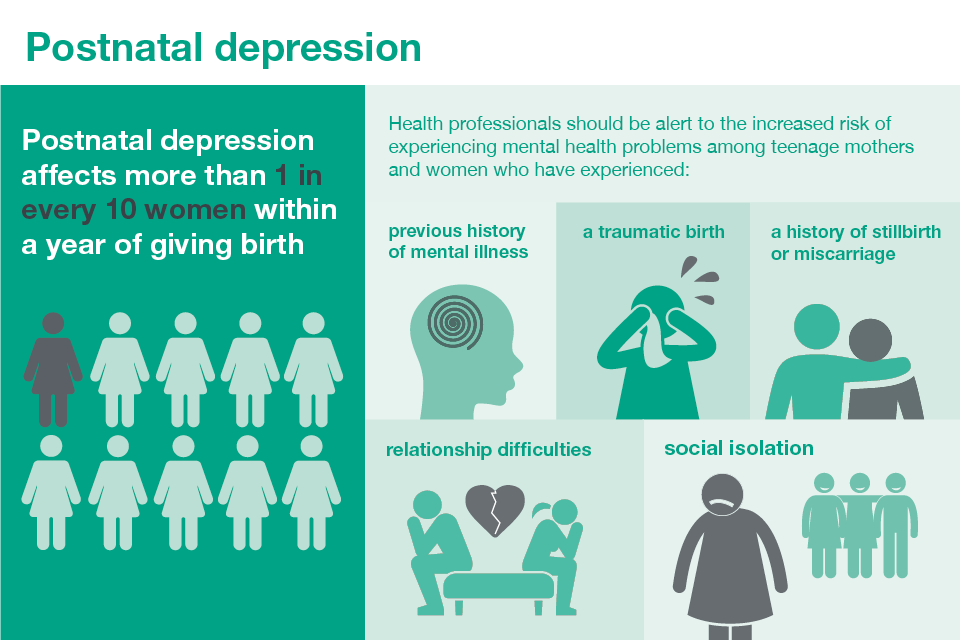
While these birth injuries are physical, many mothers can experience emotional or psychological distress — before, during or after the birth. This is known as birth trauma. There are ways to decrease your risk of birth trauma, and both treatment and support are available.
This is known as birth trauma. There are ways to decrease your risk of birth trauma, and both treatment and support are available.
What causes birth injury?
If you suffer a birth injury, the cause was most likely something out of your control.
Some of the main risk factors for birth injury include:
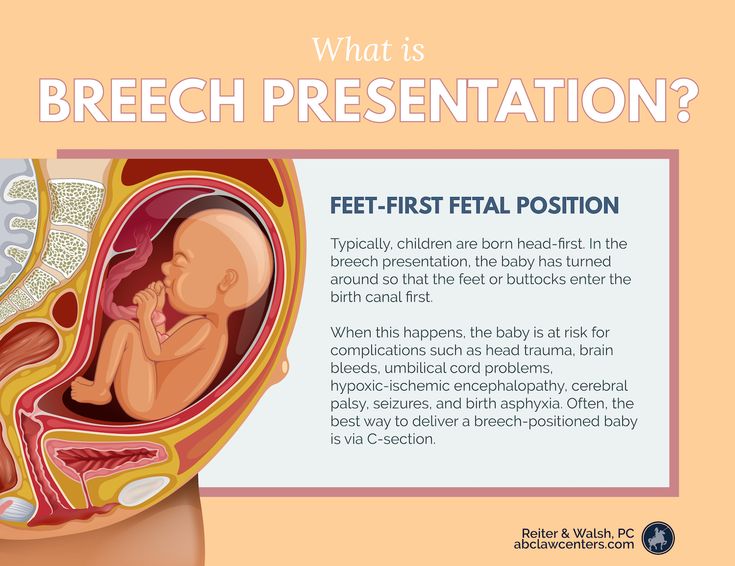
- the position of the baby, such as in a breech birth
- having a large baby (over 4kg)
- having a very quick or very long labour
- labour complications
- assisted delivery using forceps or ventouse (vacuum)
- having a small or unusually shaped pelvis
Can birth injury be prevented?
Although it's often not possible to prevent birth injury, there are some things you can do during pregnancy to reduce your risk:
- Exercise regularly (make sure you do pregnancy safe exercise).
- Strengthen your pelvic muscles with daily pelvic floor exercises.
- Avoid getting constipated or straining on the toilet, as this can weaken your pelvic muscles.

- Giving birth by caesarean could prevent some birth injuries, but this is major surgery so carries health risks of its own.
How is birth injury treated?
Some birth injuries are minor and may heal on their own — for example, a minor perineal tear or graze. Other injuries need treatment at the time, such as a deeper tear that needs stitches. You may also need some pain relief.
If you had a more serious birth injury, such as a significant tear or damage to the muscles of the pelvic floor, treatment may include physiotherapy and exercises to strengthen your pelvic floor muscles. Some women may need to use pessaries in their vagina or surgery to repair a prolapse.
Sometimes, signs of pelvic floor damage or prolapse are not detected and treated until much later.
If you have had a birth injury, you may be at more risk of it happening again with your next baby. Your doctor will talk to you about whether you should consider a planned caesarean section next time.
If you experience any ongoing symptoms, such as pelvic pain or bladder and bowel problems, you should see your doctor.
Resources and support
- Talk to your doctor, midwife or obstetrician.
- You can call Pregnancy, Birth and Baby on 1800 882 436 to speak with a maternal child health nurse (7 days a week, 7am to midnight AET).
- The Continence Foundation of Australia offers information and support to people with bowel and bladder problems. You can call the helpline on 1800 33 00 66 between 8am and 8pm (AEST), Monday to Friday.
- Visit the Australasian Birth Trauma Association website for information and support, including peer-to-peer support.
- Visit the PANDA (Perinatal Anxiety & Depression Australia) website for information and support after a traumatic birth. You can call the PANDA national helpline on 1300 726 306 ((Mon to Fri, 9am to 7.30pm AEST).
Sources:
Mater Mothers Hospital (Labour and birth - assisted vaginal birth), Medical Hypotheses (The significance of incomplete skull fracture in the birth injury), Stanford Children's Health (Birth injury), Australian Commission on Safety and Quality in Health Care (Neonatal birth trauma), Cerebral Palsy Alliance Research Foundation (What causes cerebral palsy), Medscape (Birth trauma), Merck Manual (Birth injuries in newborns), Australian Institute of Health and Welfare (Australia's mothers and babies data visualisations perineal status), PANDA (Childbirth trauma)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Related pages
- When birth doesn't go to plan
- Birth injury (to the baby)
- Birth trauma (emotional)
Need more information?
Psychological Trauma - Birth Trauma
Read more on Australasian Birth Trauma Association website
What is Birth Trauma? - Birth Trauma
The delivery of a baby is a positive event for many women, but for some it can be a mixed experience or even very negative, resulting in physical and/or
Read more on Australasian Birth Trauma Association website
Birth trauma (emotional)
Birth trauma affects many women. But there are ways to reduce your risk of an emotionally traumatic childbirth, while support and treatment are available if you experience symptoms.
But there are ways to reduce your risk of an emotionally traumatic childbirth, while support and treatment are available if you experience symptoms.
Read more on Pregnancy, Birth & Baby website
Early Postnatal - Birth Trauma
The early postnatal period is a time of emotional change for most women. Some women may experience distress or symptoms of depression at this time if they
Read more on Australasian Birth Trauma Association website
Family & Friends - Birth Trauma
If you are reading this then you may have someone close to you that has been impacted by a difficult birth experience, be it a partner, loved one or someone
Read more on Australasian Birth Trauma Association website
Birth and beyond - Ngala
Exciting times are ahead!Birth comes after lots of anticipation and preparation
Read more on Ngala website
Looking after your body after having a baby
Over the last 9 months, your body has had to change to accommodate your growing baby and preparing to give birth.
Read more on Pregnancy, Birth & Baby website
Bladder weakness after birth
Leaking urine after childbirth is very common. It can be embarrassing and inconvenient, but there are ways to improve bladder weakness.
Read more on Pregnancy, Birth & Baby website
Birth injury (to the baby)
While some babies do experience birth injury, giving birth in Australia is very safe. Most birth injuries to babies are temporary, and in many cases treatment is available.
Read more on Pregnancy, Birth & Baby website
Symptoms of Perinatal Anxiety and Depression
Symptoms of Perinatal Anxiety and Depression and how to get help. You should consider seeking professional help if you have had one of more of the following feelings
You should consider seeking professional help if you have had one of more of the following feelings
Read more on Gidget Foundation Australia website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Common Birth Injuries to Mothers
Childbirth is widely considered one of life's most amazing, yet frightening, experiences. The excitement and joy that comes with the prospect of bringing a new child into the world often comes with the anticipation of pain. While the pain of labor and delivery is something that's widely discussed, there are other factors, such as maternal birth injuries, that new mothers are often unaware of. A birth injury, depending on the type, can range from minor discomfort to long-lasting pain or changes to certain bodily functions. For some, the consequences of these injuries may have a mild impact that affects them for only a few days, or they may be long-lasting, with pain or discomfort that stays with them for years. In some extreme cases, the impact of a birth injury may even cause a new mother or family to consider consulting a lawyer. For this reason, it's important that expecting mothers understand what can happen to their bodies when they deliver a baby either naturally or by cesarean section.
A birth injury, depending on the type, can range from minor discomfort to long-lasting pain or changes to certain bodily functions. For some, the consequences of these injuries may have a mild impact that affects them for only a few days, or they may be long-lasting, with pain or discomfort that stays with them for years. In some extreme cases, the impact of a birth injury may even cause a new mother or family to consider consulting a lawyer. For this reason, it's important that expecting mothers understand what can happen to their bodies when they deliver a baby either naturally or by cesarean section.
Vaginal Tears
During childbirth, a baby's head may encounter difficulties that can cause a tear in the vaginal area. This may happen when the vagina does not easily stretch to accommodate the baby's head. Tears may also be caused by births that happen too quickly, the baby's positioning, forceps-assisted deliveries, or being overweight. There are four degrees of tears, ranging from mild to severe. Some tears, only involve the perineal skin, which is the skin between the vaginal opening and the rectum. The tissue just beneath the perineal skin may also be torn, but stitches are not always required. Other lacerations involve tearing of the muscle as well and may extend down to the anus, the anal sphincter, or even the rectum. The greater the tear, the more likely it is that surgical repair will be required. These types of lacerations are not uncommon: Roughly 95 percent of women experience some degree of tearing when they deliver their first child. Additional problems that can stem from this type of injury include urinary and fecal incontinence and painful sexual intercourse.
Some tears, only involve the perineal skin, which is the skin between the vaginal opening and the rectum. The tissue just beneath the perineal skin may also be torn, but stitches are not always required. Other lacerations involve tearing of the muscle as well and may extend down to the anus, the anal sphincter, or even the rectum. The greater the tear, the more likely it is that surgical repair will be required. These types of lacerations are not uncommon: Roughly 95 percent of women experience some degree of tearing when they deliver their first child. Additional problems that can stem from this type of injury include urinary and fecal incontinence and painful sexual intercourse.
Broken Bones
Some women may experience bone injuries as a result of childbirth. A fractured coccyx or separated pubic symphysis are both examples of this type of problem. With a separated pubic symphysis, the baby's head may cause the pubic symphysis, which is the section of cartilage where the left and right bones of the pelvic girdle connect, to separate, causing a gap. This can cause pain and discomfort that may last as little as two months but can take as long as eight months to heal. With a fractured coccyx, the mother's tailbone may fracture or bruise as a result of pressure from the baby's head during delivery.
This can cause pain and discomfort that may last as little as two months but can take as long as eight months to heal. With a fractured coccyx, the mother's tailbone may fracture or bruise as a result of pressure from the baby's head during delivery.
Uterine Rupture
A uterine rupture is a rare condition that can happen before or during labor and delivery. This may occur when a baby is abnormally large and the strain causes a uterine scar from a previous C-section to rupture during a vaginal delivery, or it may happen as a result of trauma. When the uterus tears, the baby, the placenta, or both may go into the abdominal cavity of the mother. This can cause a number of additional complications, ranging from urologic injury to hemorrhaging to even death.
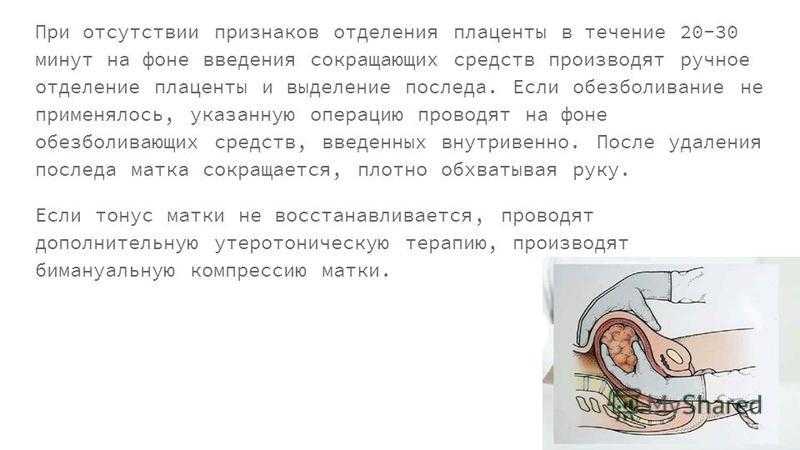
Uterine Inversion
Uterine inversion is a serious problem in which the placenta remains attached to the uterus, and upon its exit from the body, it tugs the uterus out with it, pulling it inside-out. This can lead to fatal hemorrhaging or shock. There are several grades of inversion, ranging from incomplete to total inversion. To treat this type of complication, the doctor has several options, which include manually reinserting the uterus, abdominal surgery, or an emergency hysterectomy, which may be necessary if the mother is at high risk of death.
There are several grades of inversion, ranging from incomplete to total inversion. To treat this type of complication, the doctor has several options, which include manually reinserting the uterus, abdominal surgery, or an emergency hysterectomy, which may be necessary if the mother is at high risk of death.
Nerve Injury
Nerve damage is another complication that mothers often don't think of before childbirth. Mothers can suffer from a range of problems depending on the nerves that are damaged. Injury to the femoral nerves can cause one to suffer from weakness or numbness in the legs that makes it difficult to feel or move them. Incontinence is another problem that stems from nerve damage, happening when pelvic and pudendal nerves are injured during delivery. Damage to one's nerves may be caused when they are compressed during delivery or when tissue is stretched.
Pelvic Organ Prolapse
Pregnancy and vaginal delivery may both contribute to prolapsed pelvic organs such as a prolapsed uterus. A prolapsed uterus occurs when the uterus slips down into the vagina because pregnancy, delivery, or both have weakened the pelvic floor muscles. Pelvic prolapse can occur with other pelvic organs as well, such as the bladder. The severity is defined in stages that range from 0 to 4. With a stage 4 prolapse, the organ will have slipped outside of the body entirely.
A prolapsed uterus occurs when the uterus slips down into the vagina because pregnancy, delivery, or both have weakened the pelvic floor muscles. Pelvic prolapse can occur with other pelvic organs as well, such as the bladder. The severity is defined in stages that range from 0 to 4. With a stage 4 prolapse, the organ will have slipped outside of the body entirely.
- The Risks of Birth by Cesarean Section
- Problems After Childbirth
- Millions of Women Are Injured During Childbirth
- Childbirth and Incontinence: Things You Should Know
- Pregnancy, Childbirth, and Bladder Control
- Prolapsed Uterus After Childbirth: What You Need to Know
- Pelvic Organ Prolapse Fact Sheet (PDF)
- Uterine Inversion
- Pregnancy Complications: Uterine Inversion
- Uterine Inversion (video)
- Uterine Rupture: What Family Physicians Need to Know
- Birth Complications: Uterine Rupture
- Medical Definition of Uterine Rupture
- Uterine Rupture
- Study Confirms Risk During Delivery After C-Section
- Risks of a Cesarean Procedure
- Postpartum Hemorrhage (PPH)
- Vaginal Tears in Childbirth
- Vaginal Tearing During Childbirth: What You Need to Know
- The Truth About Your Vagina Tearing During Childbirth
- After Childbirth: Pelvic Bone Problems
- Pelvic Bone Problems After Childbirth
- The Scary Truth About Childbirth
- Yes, You Can Break Your Tailbone During Labor
Birth trauma - causes, symptoms, diagnosis and treatment
Birth trauma - a collective concept that includes various damage to tissues and organs of a woman in labor or a newborn, caused by the action of birth forces. Among the birth injuries of the mother, there are hematomas, ruptures of the vulva, perineum and vagina, damage to the uterus, the formation of urogenital and enterogenital fistulas, and deformities of the pelvic bones. Many birth injuries can be life threatening. Diagnosis of birth injuries is based on external examination, gynecological examination, instrumental methods. Treatment of maternal birth injuries, as a rule, requires emergency surgical assistance and the involvement of narrow specialists (urologists, proctologists, traumatologists).
Among the birth injuries of the mother, there are hematomas, ruptures of the vulva, perineum and vagina, damage to the uterus, the formation of urogenital and enterogenital fistulas, and deformities of the pelvic bones. Many birth injuries can be life threatening. Diagnosis of birth injuries is based on external examination, gynecological examination, instrumental methods. Treatment of maternal birth injuries, as a rule, requires emergency surgical assistance and the involvement of narrow specialists (urologists, proctologists, traumatologists).
General information
Childbirth is a difficult test for the newborn fetus and mother. Therefore, after the birth of a child, experts often state the presence of various birth injuries and postpartum disorders in a woman in labor and a newborn. In obstetrics and gynecology, maternal and child birth injuries are distinguished. Birth injuries of a newborn include damage to the peripheral and central nervous systems of various nature and severity, injuries to bones and soft tissues, and internal organs.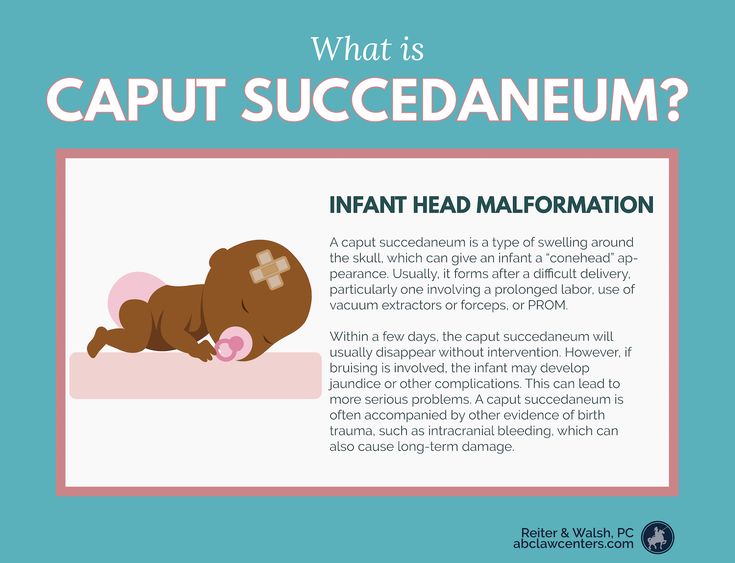 As part of this review, the main birth injuries that occur in women will be considered.
As part of this review, the main birth injuries that occur in women will be considered.
Significant stretching of the mother's birth canal during childbirth often leads to their damage. These injuries - birth injuries, can be superficial, non-rough in nature (for example, abrasions, cracks) and heal on their own in the early postpartum period, and remain unrecognized. In some cases, birth injuries are so significant that they can lead to serious postpartum complications, disability and even death of a woman. Among birth injuries of the mother there are hematomas; ruptures of the vulva, perineum, vagina, body and cervix; inversion of the uterus; sprains and ruptures of the joints of the pelvis; urogenital and enterogenital fistulas.
Birth injury
Common causes of maternal birth injury
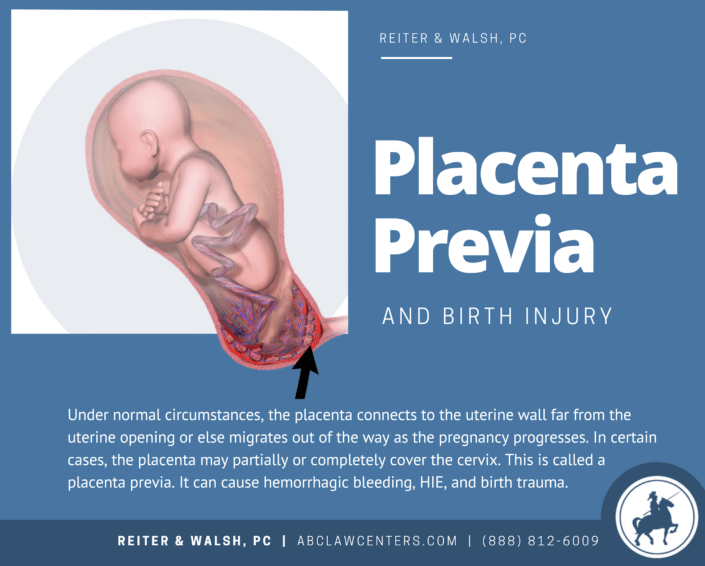
A variety of maternal birth injuries can be caused by various mechanical and histopathic causes. The mechanical factors in the occurrence of birth injuries include violent or discoordinated labor activity, the provision of operational aids during childbirth (the application of forceps, vacuum extraction of the fetus, manual separation of the placenta, fruit-destroying operations), excessive labor stimulation, irrational management of the straining period, inadequate protection of the perineum, etc. e. Post-term pregnancy, transverse position of the fetus, breech presentation of the fetus, premature birth, narrow pelvis, polyhydramnios, multiple pregnancy, placenta previa can contribute to birth injuries.
e. Post-term pregnancy, transverse position of the fetus, breech presentation of the fetus, premature birth, narrow pelvis, polyhydramnios, multiple pregnancy, placenta previa can contribute to birth injuries.
Histopathic causes of birth injuries are due to burdened obstetric and gynecological history of the woman in labor. So, the causes of birth injuries of the uterus can be surgical interventions in the past (caesarean section, metroplasty, conservative myomectomy, complete or partial perforation of the uterus during abortion, etc.), which lead to the formation of a scar on the uterus and, as a result, inadequate contractility of the myometrium in childbirth.
The likelihood of birth canal injuries increases in the presence of anatomical defects of the genitals (intrauterine septum, uterine hypoplasia, bicornuate uterus), cervical rigidity in late primiparas, uterine hyperanteflexia. Also, birth injuries can be caused by cervicitis, adenomyosis, endometritis, colpitis, cystic drift and chorionepithelioma. In the etiopathogenesis of birth trauma, there are often several aggravating factors.
In the etiopathogenesis of birth trauma, there are often several aggravating factors.
Birth injuries of the vulva and vagina
Hematomas of the vulva and vagina
Hematomas of the vulva and vagina are caused by stretching and rupture of blood vessels in the thickness of the soft tissues with intact integuments. In this case, the blood pouring out of the damaged vessel accumulates in the fiber and under the mucosa, forming a hematoma.
In case of birth injuries of soft tissues in the vulva and vagina, a blue-purple tumor appears, the size of which can reach the head of a newborn. Hematomas cause a feeling of discomfort (bursting, pressure), soreness. Large progressive hematomas extend to the pelvic tissue and may be accompanied by the development of hemorrhagic shock. Small hemorrhages usually resolve on their own; with large hematomas, their suppuration is possible. Recognition of birth injuries of soft tissues occurs during external examination and gynecological examination.
Surgical tactics are indicated for large (more than 4-5 cm in diameter) and progressive hematomas. At the same time, the tissues above the hematoma are opened, the accumulated blood is removed, the bleeding vessel is isolated and tied up, the wound is sewn up tightly. With an infected hematoma, the wound is not sutured. With a progressive hematoma, abdominotomy is sometimes required.
Tears of the vulva and vagina
Birth injuries of the vulva and vagina are most common in primiparas. Mild cracks and tears are usually asymptomatic and do not require intervention. Tears in the clitoris, urethra, vagina are accompanied by the formation of hematomas, massive bleeding, hemorrhagic shock.
Birth injuries of the vagina can be spontaneous and violent. In the latter case, the causes of birth injuries are various obstetric operations. Vaginal tears can occur in its upper, middle, or lower sections; be superficial or deep, reaching the tissue of the small pelvis and abdominal cavity.
Birth injuries of the tissues of the vulva are detected during examination. To exclude internal tears, it is necessary to examine the walls of the vagina with the help of mirrors.
The treatment of birth injuries of the vulva and vagina is exclusively surgical. After catheterization of the bladder with a metal catheter, the tears are sutured with catgut sutures. In the postoperative period, antimicrobial therapy and vaginal baths with antiseptics are prescribed. Unrecognized vaginal tears may heal uncomplicated or become infected. Deep tears can subsequently lead to secondary vaginal atresia, necessitating vaginoplasty.
Birth injuries of the perineum
Birth injuries of the perineum include violent or spontaneous ruptures of the skin, tissue and muscle-fascial tissues of the pelvic floor. Birth injuries of the perineum occur in 7-15% of women in labor, and much more often in primiparas. Perineal ruptures are often combined with birth injuries of the vagina.
Protrusion and cyanosis of the tissues of the pelvic floor, swelling and luster of tissues, cracks testify to the threat of birth injury of the perineum. If there is a threat of birth injury of the perineum, they resort to a median dissection of tissues - perineotomy or a lateral incision - episiotomy, followed by suturing.
Symptoms of perineal rupture
Depending on the depth of the birth injury, there are 3 degrees of perineal rupture.
In case of rupture of the perineum of the 1st degree, the integrity of the skin and subcutaneous tissue in the region of the posterior commissure is violated. II degree of perineal rupture is characterized by additional injuries of the pelvic floor muscles (including the muscles that lift the anus), the back or side walls of the vagina. With a birth injury of the perineum of the III degree, the rupture of the external sphincter, and sometimes the walls of the rectum, joins the above injuries.
Birth injuries of the perineum are manifested by violation of tissue integrity and bleeding.
Diagnosis and treatment of perineal tears
Birth injuries of the perineum are recognized after the birth of the placenta. To do this, the obstetrician-gynecologist spreads the genital gap, examines the walls of the vagina and the cervix. More often damage to the perineum during childbirth occurs not along the midline, but extramedially, but there is also a central gap between the posterior commissure and the muscle that lifts the anus.
Perineal tissue integrity is restored by suturing under local infiltration or general anesthesia. Separate catgut sutures are placed on the damaged walls of the vagina and rectum, pelvic floor muscles, subcutaneous tissue and perineal skin. In the postpartum period, sutures are processed, a thorough toilet of the wound after each defecation and urination, and constipation is prevented.
Birth injury of the uterus
Rupture of the uterus
Rupture of the uterus is one of the most severe birth injuries and occurs in 0.015%-0.1% of the total number of births. When the uterus ruptures, the integrity of the walls of its body is violated. The lethality of women with birth trauma of the uterus from shock, anemia and septic complications reaches 3-4%. Many women who have had uterine rupture develop hypoxic encephalopathy later on. Fetal death in uterine rupture is close to 100%.
Classification of uterine ruptures
There are uterine ruptures that occurred during pregnancy and during childbirth. According to the pathogenetic signs of birth trauma, spontaneous (mechanical, histopathic and mechanical-histopathic) and violent (traumatic, mixed) uterine ruptures are distinguished. According to the birth trauma clinic, uterine ruptures can be threatening, begun, completed.
According to the degree of damage to the walls of the uterus, birth trauma can take the form of a crack, incomplete rupture and complete rupture penetrating into the abdominal cavity. By localization, there is a rupture of the bottom of the uterus, its body, the lower segment, as well as a complete separation of the uterus from the vaginal vaults (colpoporexis) in the transverse position of the fetus.
By localization, there is a rupture of the bottom of the uterus, its body, the lower segment, as well as a complete separation of the uterus from the vaginal vaults (colpoporexis) in the transverse position of the fetus.
Symptoms of uterine rupture
The clinic of birth trauma of the uterus depends on the causes, stage, degree, localization of the rupture. The severity of manifestations and consequences are largely due to the accompanying background - in the presence of somatic diseases of the woman in labor, gestosis, physical and mental exhaustion, infection, etc., irreversible changes quickly develop in the body.
Threatening uterine rupture is characterized by excessive labor activity with painful strong contractions, hourglass uterine deformity, development of edema of the cervix, vagina and vulva, difficulty urinating, anxiety of the woman in labor. With the onset of uterine rupture, the listed symptoms are supplemented by convulsive contractions, the appearance of sanious or bloody discharge from the vagina, and hematuria.
When the uterus ruptures, after a sharp pain and burning sensation in the abdomen, labor activity stops, the woman in labor calms down, becomes depressed, apathetic. Due to the development of hemorrhagic and painful shock, pallor of the skin, hypotension, tachycardia rapidly increase, cold sweat, nausea and vomiting appear. After rupture of the uterus, parts of the fetus are partially or completely palpated in the abdominal cavity, there is no fetal heartbeat. External bleeding with this birth injury can be significant or scanty, depending on the size and location of uterine rupture.
Urgent care for uterine ruptures
If there is a threat of uterine rupture, immediate termination of labor and completion of labor by operative means - caesarean section or fruit-destroying operation. With the onset or completed uterine rupture, cerebrosection is performed, the fetus and placenta are removed, amniotic fluid and blood are removed, and hemostasis is performed.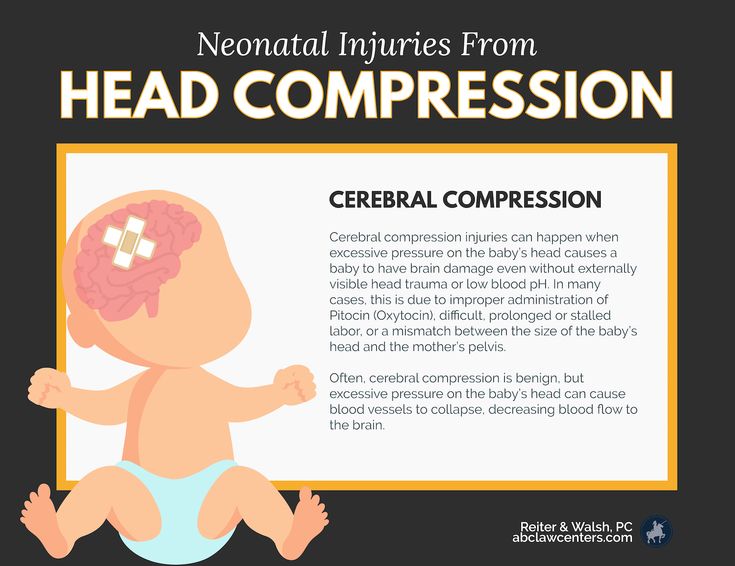 The volume of intervention for these birth injuries ranges from supravaginal amputation to hysterectomy. Uterine suturing is possible in young patients with recent and small ruptures of a linear nature, the absence of infection.
The volume of intervention for these birth injuries ranges from supravaginal amputation to hysterectomy. Uterine suturing is possible in young patients with recent and small ruptures of a linear nature, the absence of infection.
At the same time, it is necessary to carry out adequate replenishment of blood loss, anti-shock infusion-transfusion therapy, and correction of hemocoagulation. If birth injuries of the uterus were not recognized, bleeding or peritonitis may develop, as well as the death of the puerperal. With infectious complications, laparotomy, removal of the uterus with appendages (panhysterectomy), drainage of the abdominal cavity, and massive antibiotic therapy are undertaken.
Cervical tears
This type of birth injury occurs according to various authors in 3-60% of women in labor. Cervical ruptures (violent or spontaneous) are divided into 3 degrees according to the depth of damage: I - a defect of no more than 2 cm; II - defect more than 2 cm, but not reaching the vaginal vaults; III - a defect that reaches the vaults and passes to them.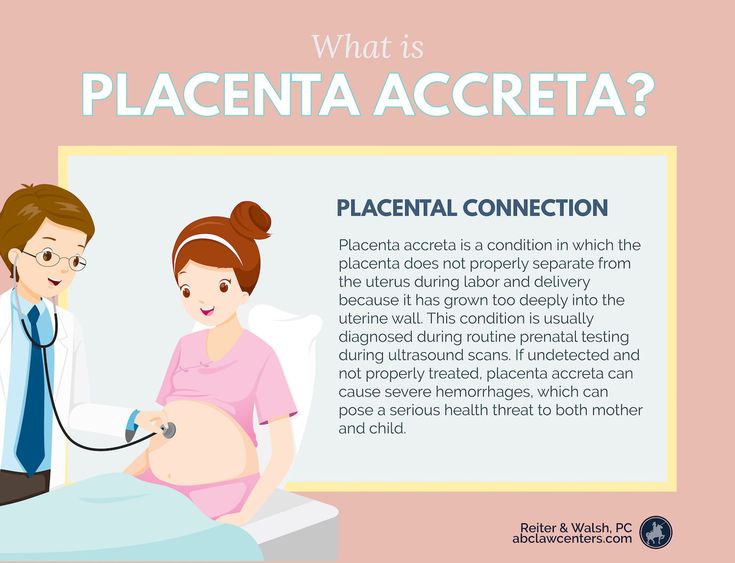 Cervical ruptures are usually localized in the lateral sections, more often on the left.
Cervical ruptures are usually localized in the lateral sections, more often on the left.
Symptoms of cervical rupture
Birth injuries of the cervix are manifested by postpartum bleeding from the vagina after the birth of the placenta and contraction of the uterus. Blood flowing from the genital tract has a scarlet color, is released in a continuous stream or in the form of a large number of clots in the absence of external damage to the birth canal. Sometimes there is little or no bleeding. If the branches of the uterine arteries are damaged, there is a massive outpouring of blood or the formation of hematomas in the paracervical tissue, a clinic of hemorrhagic shock.
If cervical ruptures remain unrecognized, in the future it can lead to the development of postpartum ulcers, parametritis, pelvioperitonitis, spontaneous abortions, cervical dysplasia.
Diagnosis and treatment of cervical tears
To recognize birth injuries of the cervix, all postpartum women need to be examined with the help of mirrors immediately after the completion of labor, and also 6-48 hours after swelling and stretching of the tissues have decreased.
Detected ruptures of the cervix are subject to suturing immediately or delayed, no later than 2 days after birth. The sutures are applied to the ruptures of the neck through all layers of tissues, starting from the upper corner of the defect in the direction of the external pharynx. Due to unfavorable conditions (the presence of lochia, edema, crushing of tissues), birth injuries of the cervix often heal by secondary intention.
Other birth injuries
Uterine inversion
The development of acute uterine inversion is due to improper management of the afterbirth period, weakness of the uterine ligaments, and atony of the uterus. Distinguish between partial and complete eversion of the uterus. This birth injury proceeds with the phenomena of pain shock.
Treatment of uterine inversion consists in anti-shock measures and reduction of the uterus to its anatomical place under general anesthesia.
Sprains and ruptures of the pelvic joints
These birth injuries develop with excessive softening of the joints of the pelvis (symphysiopathy, symphysitis), childbirth with a premature or large fetus, obstetric benefits. In this case, the pubic bones are stretched and separated at a distance of more than 0.5 cm from each other. Rupture of the pubic joint is often accompanied by displacement of bones, damage to the bladder, urethra, and clitoris. Stretching of the sacroiliac joints leads to hemorrhages and subsequent inflammation of the joints.
In this case, the pubic bones are stretched and separated at a distance of more than 0.5 cm from each other. Rupture of the pubic joint is often accompanied by displacement of bones, damage to the bladder, urethra, and clitoris. Stretching of the sacroiliac joints leads to hemorrhages and subsequent inflammation of the joints.
The clinic of birth injuries of the pelvic joints is manifested by pain in the womb, coccyx, sacrum, aggravated by abduction of the legs, walking; gait disturbance, skin hyperemia and swelling of surrounding tissues.
Birth injuries of the pelvic region are detected during a consultation with a traumatologist during examination, palpation, radiography of the pubic, sacroiliac joint, and pelvis. Treatment of sprains of the pelvic joints requires rest, tight bandaging, wearing special corsets. A rupture of the pubic symphysis or a significant divergence of the pelvic bones requires surgical intervention.
Urogenital and rectal-vaginal fistulas
Birth injuries with the formation of fistulas are caused by prolonged (more than 2 hours) standing of the baby's head in one plane, resulting in impaired blood circulation in tissues with their subsequent necrosis. Sometimes urogenital and rectal-vaginal fistulas are formed as a result of intraoperative damage to the walls of the bladder or rectum.
Fistulas are manifested by the release of urine or gases and feces through the vagina outside the acts of urination and defecation. Such disorders are always accompanied by the development of a local inflammatory reaction in the vagina (colpitis).
Diagnosis of urogenital fistulas is made during a gynecological examination, cystoscopy; rectal-vaginal fistulas are recognized by digital rectal examination, irrigoscopy, fistulography, and rectoscopy. When detecting urogenital and rectovaginal fistulas, their surgical closure (fistuloplasty) is usually required.
Prevention of birth injuries
Prevention of birth injuries of the uterus requires the study of a gynecological history of a pregnant woman in the early stages, ultrasound monitoring of the state of scars on the uterus during pregnancy, hospitalization of pregnant women with a threat of injuries in childbirth.
Prevention of birth injuries requires the rejection of forced delivery, the use of obstetric benefits strictly according to indications.
Birth trauma - causes, symptoms, diagnosis and treatment
Birth trauma is a collective concept that includes various damage to tissues and organs of a woman in labor or a newborn, caused by the action of birth forces. Among the birth injuries of the mother, there are hematomas, ruptures of the vulva, perineum and vagina, damage to the uterus, the formation of urogenital and enterogenital fistulas, and deformities of the pelvic bones. Many birth injuries can be life threatening. Diagnosis of birth injuries is based on external examination, gynecological examination, instrumental methods. Treatment of maternal birth injuries, as a rule, requires emergency surgical assistance and the involvement of narrow specialists (urologists, proctologists, traumatologists).
General information
Childbirth is a difficult test for the newborn fetus and mother. Therefore, after the birth of a child, experts often state the presence of various birth injuries and postpartum disorders in a woman in labor and a newborn. In obstetrics and gynecology, maternal and child birth injuries are distinguished. Birth injuries of a newborn include damage to the peripheral and central nervous systems of various nature and severity, injuries to bones and soft tissues, and internal organs. As part of this review, the main birth injuries that occur in women will be considered.
Therefore, after the birth of a child, experts often state the presence of various birth injuries and postpartum disorders in a woman in labor and a newborn. In obstetrics and gynecology, maternal and child birth injuries are distinguished. Birth injuries of a newborn include damage to the peripheral and central nervous systems of various nature and severity, injuries to bones and soft tissues, and internal organs. As part of this review, the main birth injuries that occur in women will be considered.
Significant stretching of the mother's birth canal during childbirth often leads to their damage. These injuries - birth injuries, can be superficial, non-rough in nature (for example, abrasions, cracks) and heal on their own in the early postpartum period, and remain unrecognized. In some cases, birth injuries are so significant that they can lead to serious postpartum complications, disability and even death of a woman. Among birth injuries of the mother there are hematomas; ruptures of the vulva, perineum, vagina, body and cervix; inversion of the uterus; sprains and ruptures of the joints of the pelvis; urogenital and enterogenital fistulas.
Birth injury
Common causes of maternal birth injury
A variety of maternal birth injuries can be caused by various mechanical and histopathic causes. The mechanical factors in the occurrence of birth injuries include violent or discoordinated labor activity, the provision of operational aids during childbirth (the application of forceps, vacuum extraction of the fetus, manual separation of the placenta, fruit-destroying operations), excessive labor stimulation, irrational management of the straining period, inadequate protection of the perineum, etc. e. Post-term pregnancy, transverse position of the fetus, breech presentation of the fetus, premature birth, narrow pelvis, polyhydramnios, multiple pregnancy, placenta previa can contribute to birth injuries.
Histopathic causes of birth injuries are due to burdened obstetric and gynecological history of the woman in labor. So, the causes of birth injuries of the uterus can be surgical interventions in the past (caesarean section, metroplasty, conservative myomectomy, complete or partial perforation of the uterus during abortion, etc. ), which lead to the formation of a scar on the uterus and, as a result, inadequate contractility of the myometrium in childbirth.
), which lead to the formation of a scar on the uterus and, as a result, inadequate contractility of the myometrium in childbirth.
The likelihood of birth canal injuries increases in the presence of anatomical defects of the genitals (intrauterine septum, uterine hypoplasia, bicornuate uterus), cervical rigidity in late primiparas, uterine hyperanteflexia. Also, birth injuries can be caused by cervicitis, adenomyosis, endometritis, colpitis, cystic drift and chorionepithelioma. In the etiopathogenesis of birth trauma, there are often several aggravating factors.
Birth injuries of the vulva and vagina
Hematomas of the vulva and vagina
Hematomas of the vulva and vagina are caused by stretching and rupture of blood vessels in the thickness of the soft tissues with intact integuments. In this case, the blood pouring out of the damaged vessel accumulates in the fiber and under the mucosa, forming a hematoma.
In case of birth injuries of soft tissues in the vulva and vagina, a blue-purple tumor appears, the size of which can reach the head of a newborn. Hematomas cause a feeling of discomfort (bursting, pressure), soreness. Large progressive hematomas extend to the pelvic tissue and may be accompanied by the development of hemorrhagic shock. Small hemorrhages usually resolve on their own; with large hematomas, their suppuration is possible. Recognition of birth injuries of soft tissues occurs during external examination and gynecological examination.
Hematomas cause a feeling of discomfort (bursting, pressure), soreness. Large progressive hematomas extend to the pelvic tissue and may be accompanied by the development of hemorrhagic shock. Small hemorrhages usually resolve on their own; with large hematomas, their suppuration is possible. Recognition of birth injuries of soft tissues occurs during external examination and gynecological examination.
Surgical tactics are indicated for large (more than 4-5 cm in diameter) and progressive hematomas. At the same time, the tissues above the hematoma are opened, the accumulated blood is removed, the bleeding vessel is isolated and tied up, the wound is sewn up tightly. With an infected hematoma, the wound is not sutured. With a progressive hematoma, abdominotomy is sometimes required.
Tears of the vulva and vagina
Birth injuries of the vulva and vagina are most common in primiparas. Mild cracks and tears are usually asymptomatic and do not require intervention. Tears in the clitoris, urethra, vagina are accompanied by the formation of hematomas, massive bleeding, hemorrhagic shock.
Tears in the clitoris, urethra, vagina are accompanied by the formation of hematomas, massive bleeding, hemorrhagic shock.
Birth injuries of the vagina can be spontaneous and violent. In the latter case, the causes of birth injuries are various obstetric operations. Vaginal tears can occur in its upper, middle, or lower sections; be superficial or deep, reaching the tissue of the small pelvis and abdominal cavity.
Birth injuries of the tissues of the vulva are detected during examination. To exclude internal tears, it is necessary to examine the walls of the vagina with the help of mirrors.
The treatment of birth injuries of the vulva and vagina is exclusively surgical. After catheterization of the bladder with a metal catheter, the tears are sutured with catgut sutures. In the postoperative period, antimicrobial therapy and vaginal baths with antiseptics are prescribed. Unrecognized vaginal tears may heal uncomplicated or become infected. Deep tears can subsequently lead to secondary vaginal atresia, necessitating vaginoplasty.
Deep tears can subsequently lead to secondary vaginal atresia, necessitating vaginoplasty.
Birth injuries of the perineum
Birth injuries of the perineum include violent or spontaneous ruptures of the skin, tissue and muscle-fascial tissues of the pelvic floor. Birth injuries of the perineum occur in 7-15% of women in labor, and much more often in primiparas. Perineal ruptures are often combined with birth injuries of the vagina.
Protrusion and cyanosis of the tissues of the pelvic floor, swelling and luster of tissues, cracks testify to the threat of birth injury of the perineum. If there is a threat of birth injury of the perineum, they resort to a median dissection of tissues - perineotomy or a lateral incision - episiotomy, followed by suturing.
Symptoms of perineal rupture
Depending on the depth of the birth injury, there are 3 degrees of perineal rupture.
In case of rupture of the perineum of the 1st degree, the integrity of the skin and subcutaneous tissue in the region of the posterior commissure is violated. II degree of perineal rupture is characterized by additional injuries of the pelvic floor muscles (including the muscles that lift the anus), the back or side walls of the vagina. With a birth injury of the perineum of the III degree, the rupture of the external sphincter, and sometimes the walls of the rectum, joins the above injuries.
II degree of perineal rupture is characterized by additional injuries of the pelvic floor muscles (including the muscles that lift the anus), the back or side walls of the vagina. With a birth injury of the perineum of the III degree, the rupture of the external sphincter, and sometimes the walls of the rectum, joins the above injuries.
Birth injuries of the perineum are manifested by violation of tissue integrity and bleeding.
Diagnosis and treatment of perineal tears
Birth injuries of the perineum are recognized after the birth of the placenta. To do this, the obstetrician-gynecologist spreads the genital gap, examines the walls of the vagina and the cervix. More often damage to the perineum during childbirth occurs not along the midline, but extramedially, but there is also a central gap between the posterior commissure and the muscle that lifts the anus.
Perineal tissue integrity is restored by suturing under local infiltration or general anesthesia. Separate catgut sutures are placed on the damaged walls of the vagina and rectum, pelvic floor muscles, subcutaneous tissue and perineal skin. In the postpartum period, sutures are processed, a thorough toilet of the wound after each defecation and urination, and constipation is prevented.
Separate catgut sutures are placed on the damaged walls of the vagina and rectum, pelvic floor muscles, subcutaneous tissue and perineal skin. In the postpartum period, sutures are processed, a thorough toilet of the wound after each defecation and urination, and constipation is prevented.
Birth injury of the uterus
Rupture of the uterus
Rupture of the uterus is one of the most severe birth injuries and occurs in 0.015%-0.1% of the total number of births. When the uterus ruptures, the integrity of the walls of its body is violated. The lethality of women with birth trauma of the uterus from shock, anemia and septic complications reaches 3-4%. Many women who have had uterine rupture develop hypoxic encephalopathy later on. Fetal death in uterine rupture is close to 100%.
Classification of uterine ruptures
There are uterine ruptures that occurred during pregnancy and during childbirth. According to the pathogenetic signs of birth trauma, spontaneous (mechanical, histopathic and mechanical-histopathic) and violent (traumatic, mixed) uterine ruptures are distinguished. According to the birth trauma clinic, uterine ruptures can be threatening, begun, completed.
According to the birth trauma clinic, uterine ruptures can be threatening, begun, completed.
According to the degree of damage to the walls of the uterus, birth trauma can take the form of a crack, incomplete rupture and complete rupture penetrating into the abdominal cavity. By localization, there is a rupture of the bottom of the uterus, its body, the lower segment, as well as a complete separation of the uterus from the vaginal vaults (colpoporexis) in the transverse position of the fetus.
Symptoms of uterine rupture
The clinic of birth trauma of the uterus depends on the causes, stage, degree, localization of the rupture. The severity of manifestations and consequences are largely due to the accompanying background - in the presence of somatic diseases of the woman in labor, gestosis, physical and mental exhaustion, infection, etc., irreversible changes quickly develop in the body.
Threatening uterine rupture is characterized by excessive labor activity with painful strong contractions, hourglass uterine deformity, development of edema of the cervix, vagina and vulva, difficulty urinating, anxiety of the woman in labor. With the onset of uterine rupture, the listed symptoms are supplemented by convulsive contractions, the appearance of sanious or bloody discharge from the vagina, and hematuria.
With the onset of uterine rupture, the listed symptoms are supplemented by convulsive contractions, the appearance of sanious or bloody discharge from the vagina, and hematuria.
When the uterus ruptures, after a sharp pain and burning sensation in the abdomen, labor activity stops, the woman in labor calms down, becomes depressed, apathetic. Due to the development of hemorrhagic and painful shock, pallor of the skin, hypotension, tachycardia rapidly increase, cold sweat, nausea and vomiting appear. After rupture of the uterus, parts of the fetus are partially or completely palpated in the abdominal cavity, there is no fetal heartbeat. External bleeding with this birth injury can be significant or scanty, depending on the size and location of uterine rupture.
Urgent care for uterine ruptures
If there is a threat of uterine rupture, immediate termination of labor and completion of labor by operative means - caesarean section or fruit-destroying operation. With the onset or completed uterine rupture, cerebrosection is performed, the fetus and placenta are removed, amniotic fluid and blood are removed, and hemostasis is performed. The volume of intervention for these birth injuries ranges from supravaginal amputation to hysterectomy. Uterine suturing is possible in young patients with recent and small ruptures of a linear nature, the absence of infection.
With the onset or completed uterine rupture, cerebrosection is performed, the fetus and placenta are removed, amniotic fluid and blood are removed, and hemostasis is performed. The volume of intervention for these birth injuries ranges from supravaginal amputation to hysterectomy. Uterine suturing is possible in young patients with recent and small ruptures of a linear nature, the absence of infection.
At the same time, it is necessary to carry out adequate replenishment of blood loss, anti-shock infusion-transfusion therapy, and correction of hemocoagulation. If birth injuries of the uterus were not recognized, bleeding or peritonitis may develop, as well as the death of the puerperal. With infectious complications, laparotomy, removal of the uterus with appendages (panhysterectomy), drainage of the abdominal cavity, and massive antibiotic therapy are undertaken.
Cervical tears
This type of birth injury occurs according to various authors in 3-60% of women in labor. Cervical ruptures (violent or spontaneous) are divided into 3 degrees according to the depth of damage: I - a defect of no more than 2 cm; II - defect more than 2 cm, but not reaching the vaginal vaults; III - a defect that reaches the vaults and passes to them. Cervical ruptures are usually localized in the lateral sections, more often on the left.
Cervical ruptures (violent or spontaneous) are divided into 3 degrees according to the depth of damage: I - a defect of no more than 2 cm; II - defect more than 2 cm, but not reaching the vaginal vaults; III - a defect that reaches the vaults and passes to them. Cervical ruptures are usually localized in the lateral sections, more often on the left.
Symptoms of cervical rupture
Birth injuries of the cervix are manifested by postpartum bleeding from the vagina after the birth of the placenta and contraction of the uterus. Blood flowing from the genital tract has a scarlet color, is released in a continuous stream or in the form of a large number of clots in the absence of external damage to the birth canal. Sometimes there is little or no bleeding. If the branches of the uterine arteries are damaged, there is a massive outpouring of blood or the formation of hematomas in the paracervical tissue, a clinic of hemorrhagic shock.
If cervical ruptures remain unrecognized, in the future it can lead to the development of postpartum ulcers, parametritis, pelvioperitonitis, spontaneous abortions, cervical dysplasia.
Diagnosis and treatment of cervical tears
To recognize birth injuries of the cervix, all postpartum women need to be examined with the help of mirrors immediately after the completion of labor, and also 6-48 hours after swelling and stretching of the tissues have decreased.
Detected ruptures of the cervix are subject to suturing immediately or delayed, no later than 2 days after birth. The sutures are applied to the ruptures of the neck through all layers of tissues, starting from the upper corner of the defect in the direction of the external pharynx. Due to unfavorable conditions (the presence of lochia, edema, crushing of tissues), birth injuries of the cervix often heal by secondary intention.
Other birth injuries
Uterine inversion
The development of acute uterine inversion is due to improper management of the afterbirth period, weakness of the uterine ligaments, and atony of the uterus. Distinguish between partial and complete eversion of the uterus. This birth injury proceeds with the phenomena of pain shock.
Distinguish between partial and complete eversion of the uterus. This birth injury proceeds with the phenomena of pain shock.
Treatment of uterine inversion consists in anti-shock measures and reduction of the uterus to its anatomical place under general anesthesia.
Sprains and ruptures of the pelvic joints
These birth injuries develop with excessive softening of the joints of the pelvis (symphysiopathy, symphysitis), childbirth with a premature or large fetus, obstetric benefits. In this case, the pubic bones are stretched and separated at a distance of more than 0.5 cm from each other. Rupture of the pubic joint is often accompanied by displacement of bones, damage to the bladder, urethra, and clitoris. Stretching of the sacroiliac joints leads to hemorrhages and subsequent inflammation of the joints.
The clinic of birth injuries of the pelvic joints is manifested by pain in the womb, coccyx, sacrum, aggravated by abduction of the legs, walking; gait disturbance, skin hyperemia and swelling of surrounding tissues.
Birth injuries of the pelvic region are detected during a consultation with a traumatologist during examination, palpation, radiography of the pubic, sacroiliac joint, and pelvis. Treatment of sprains of the pelvic joints requires rest, tight bandaging, wearing special corsets. A rupture of the pubic symphysis or a significant divergence of the pelvic bones requires surgical intervention.
Urogenital and rectal-vaginal fistulas
Birth injuries with the formation of fistulas are caused by prolonged (more than 2 hours) standing of the baby's head in one plane, resulting in impaired blood circulation in tissues with their subsequent necrosis. Sometimes urogenital and rectal-vaginal fistulas are formed as a result of intraoperative damage to the walls of the bladder or rectum.
Fistulas are manifested by the release of urine or gases and feces through the vagina outside the acts of urination and defecation. Such disorders are always accompanied by the development of a local inflammatory reaction in the vagina (colpitis).