Placenta stuck to uterus after birth
Types, Risks, Causes & Treatment
Overview
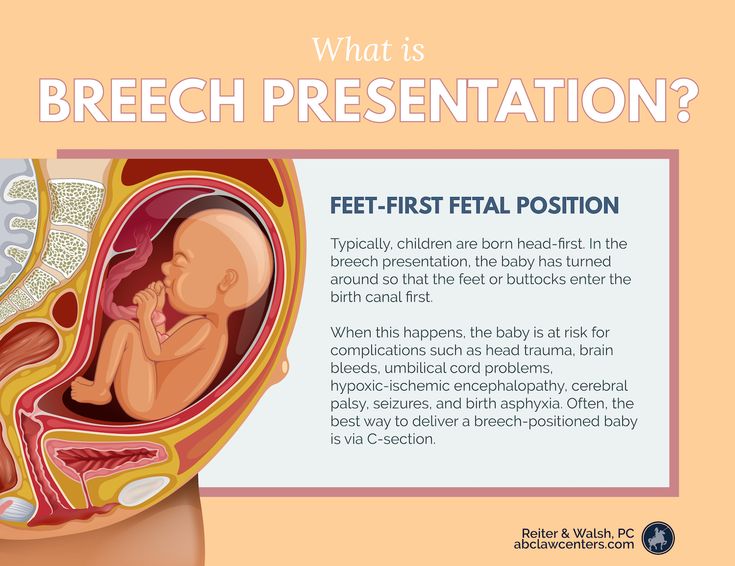
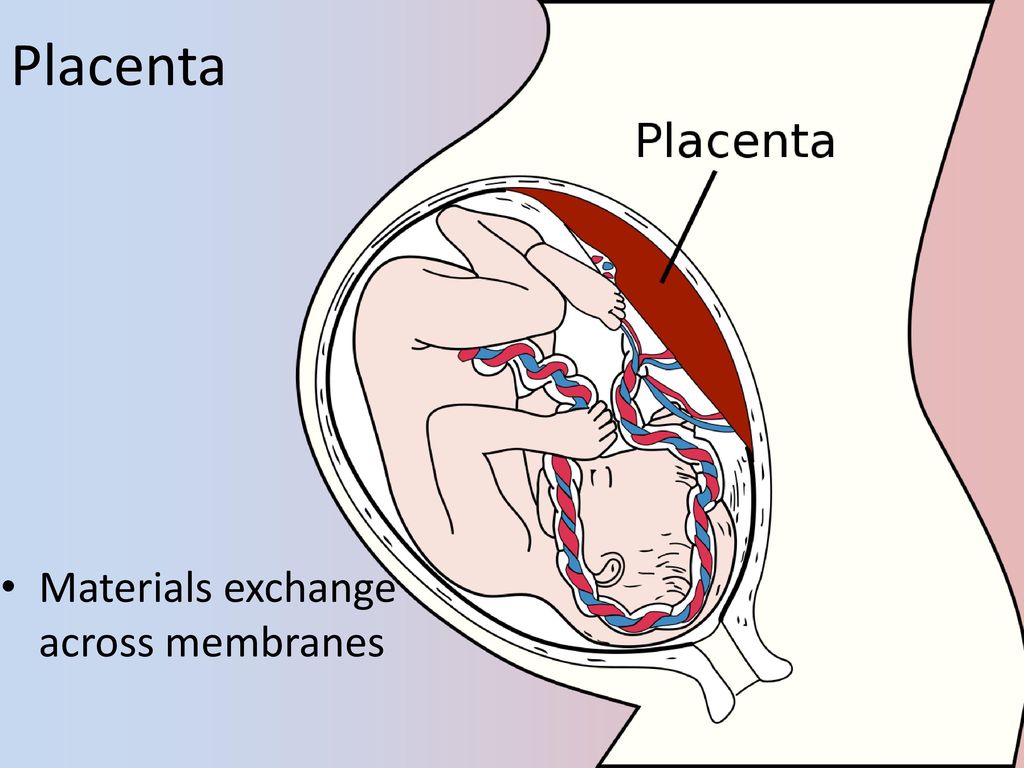
Placenta accreta is a pregnancy complication that occurs when the placenta embeds too deep in the uterine wall.What is placenta accreta?
Placenta accreta is a condition where the placenta (the food and oxygen source for a fetus) grows too deeply into the wall of your uterus. In a typical pregnancy, the placenta easily detaches from the wall of your uterus after your baby is born. In placenta accreta, the placenta has grown into your uterine wall and doesn’t separate easily following delivery. In severe cases, it can lead to life-threatening vaginal bleeding. It may require a blood transfusion and hysterectomy (removal of your uterus). Pregnancy care providers diagnose placenta accreta during pregnancy or during delivery. Treatment usually involves an early Cesarean delivery (C-section) followed by a hysterectomy to minimize the risk of severe complications.
What are the different types of placenta accreta?
There are three types of placenta accreta. Providers determine the type based on how deeply the placenta is attached to your uterus.
- Placenta accreta: The placenta firmly attaches to the wall of your uterus. It doesn’t pass through the wall of the uterus or impact the muscles of the uterus. This is the most common type.
- Placenta increta: In this type, the placenta is more deeply embedded in the wall of your uterus. It still doesn’t pass through the uterine wall but is firmly attached to the muscle of the uterus. Placenta increta accounts for about 15% of cases.
- Placenta percreta: The most severe of the types, placenta percreta happens when the placenta passes through the wall of your uterus. The placenta might grow through your uterus and impact other organs, such as your bladder or intestines. It accounts for about 5% of cases.
Who’s at risk for placenta accreta?
You’re at higher risk for placenta accreta if you:
- Have had previous Cesarean deliveries.

- Have a placenta in an abnormal location in your uterus.
- Have had previous surgeries on your uterus.
- Have had more than one pregnancy.
- Are pregnant via IVF.
Does placenta accreta harm the fetus?
Placenta accreta doesn’t directly harm the fetus. Placenta accreta often leads to preterm birth. Preterm birth carries risks such as respiratory problems or trouble gaining weight. Babies born before 37 weeks of pregnancy have a higher risk of being admitted to a neonatal intensive care unit (NICU) for specialized treatment.
What are the risks of placenta accreta to the birthing person?
- Premature delivery.
- Damage to your uterus and surrounding organs.
- Loss of fertility due to hysterectomy.
- Excessive bleeding that requires a blood transfusion.
- Blood clotting issues.
- Lung or kidney failure.
- Death.
How common is placenta accreta?
Placenta accreta may affect up to 1 in 533 pregnancies. The occurrence of placenta accreta has increased over the last several decades, mostly due to the increased rate of C-sections.
The occurrence of placenta accreta has increased over the last several decades, mostly due to the increased rate of C-sections.
Symptoms and Causes
What causes placenta accreta?
Abnormalities with the lining of your uterus cause placenta accreta. Your uterine lining can become damaged or scarred from prior uterine surgeries. It can also happen to people who haven’t had any uterine surgery.
The risk factors for placenta accreta are:
- Multiple C-sections: People who’ve had multiple C-sections have a higher risk of developing placenta accreta. This results from scarring of your uterus from the procedures. The more cesarean sections a woman has over time, the higher her risk of placenta accreta. Multiple cesareans are present in over 60% of cases.
- History of uterine surgeries: If you’ve had a uterine fibroid (a noncancerous growth or tumor of the uterine muscle) removed, the scarring could lead to placenta accreta.
 Surgeries such as curettage (removing tissue from your uterus) or endometrial ablation can also lead to scarring.
Surgeries such as curettage (removing tissue from your uterus) or endometrial ablation can also lead to scarring. - Placenta previa: This condition occurs when the placenta blocks your cervix. In people with placenta previa and a history of prior C-section deliveries, the risk for placenta accreta increases with the number of C-sections they’ve had.
What are the symptoms of placenta accreta?
There are usually no symptoms of placenta accreta. In some cases, you may experience bleeding in the third trimester of pregnancy (weeks 28 to 40) or pelvic pain (from the placenta pressing on your bladder or other organs).
Diagnosis and Tests
How is placenta accreta diagnosed?
A prenatal ultrasound can diagnose placenta accreta during pregnancy. Magnetic resonance imaging (MRI) can be helpful in some cases to show how deeply the placenta has penetrated your uterine wall.
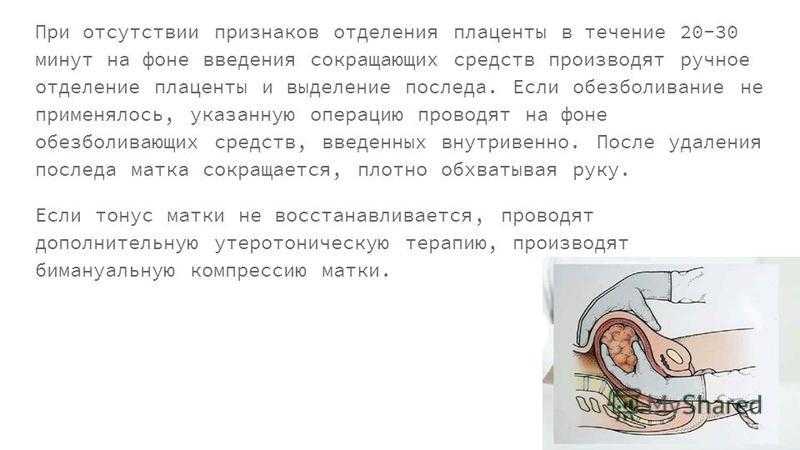
In other cases, pregnancy care providers discover placenta accreta after your baby is born.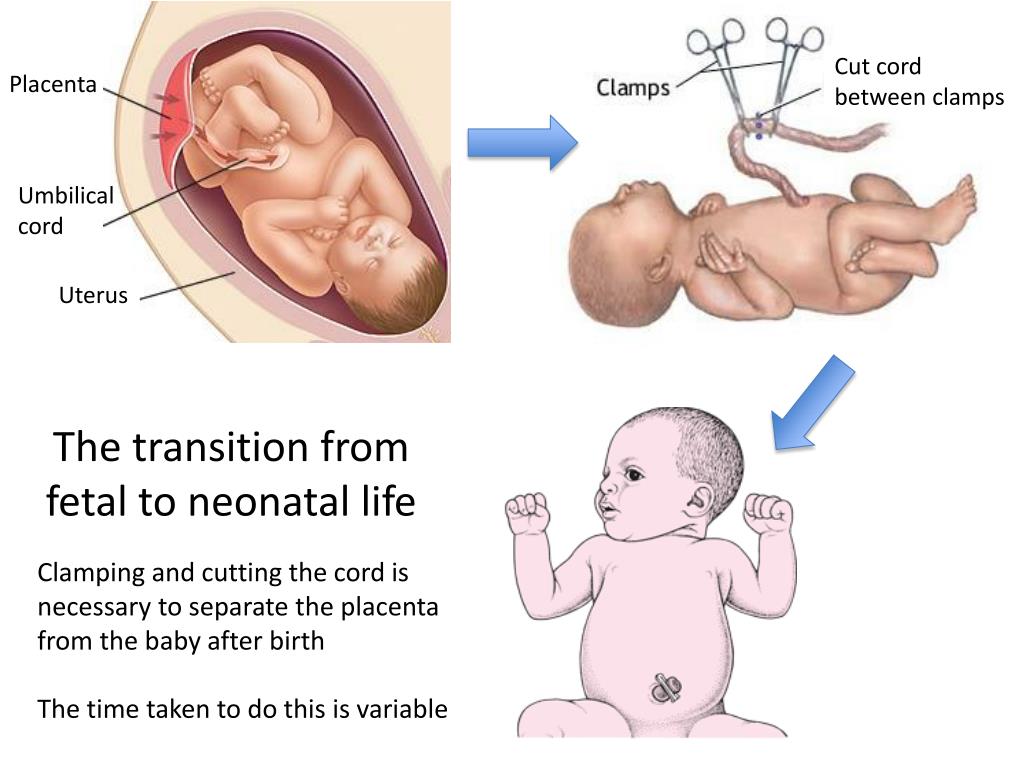 Ideally, uterine contractions expel the placenta within 30 minutes of delivery. When this doesn’t occur, your provider may suspect placenta accreta.
Ideally, uterine contractions expel the placenta within 30 minutes of delivery. When this doesn’t occur, your provider may suspect placenta accreta.
How important is an early diagnosis of placenta accreta?
An early diagnosis of placenta accreta is essential because it can allow multiple healthcare providers to become involved in your pregnancy and delivery care. For example, a neonatologist may be involved in your newborn’s care, or a perinatologist may be involved in yours. Your provider will monitor you closely to ensure the best results for you and your baby.
Having the right people involved could prevent the removal of your uterus (hysterectomy) or life-threatening blood loss. In some cases, providers can’t avoid a hysterectomy and blood transfusion despite an early diagnosis; however, risks for other complications decrease with early diagnosis.
Management and Treatment
How is placenta accreta treated?
Treatment of placenta accreta can vary. If your provider diagnoses it before delivery, they’ll monitor you closely for the rest of your pregnancy. You may be hospitalized or put on bed rest to prevent preterm labor. Your provider will schedule a C-section to deliver your baby, usually around between 34 and 37 weeks. This is done to decrease the risk of bleeding from contractions or labor. If you wish to have future pregnancies, your healthcare provider can try to save your uterus.
If your provider diagnoses it before delivery, they’ll monitor you closely for the rest of your pregnancy. You may be hospitalized or put on bed rest to prevent preterm labor. Your provider will schedule a C-section to deliver your baby, usually around between 34 and 37 weeks. This is done to decrease the risk of bleeding from contractions or labor. If you wish to have future pregnancies, your healthcare provider can try to save your uterus.
However, in severe cases where the placenta is deeply or firmly attached or invading into other organs, a hysterectomy (removal of the uterus) may be the safest option. A Cesarean hysterectomy is when your uterus is removed at the time of a C-section delivery. In this case, your provider will deliver your baby, your uterus and the placenta at the same time. Removing your uterus with the placenta still attached minimizes the risk of excessive bleeding (hemorrhaging).
Some healthcare providers will leave small parts of the placenta inside your uterus because the placenta dissolves over time.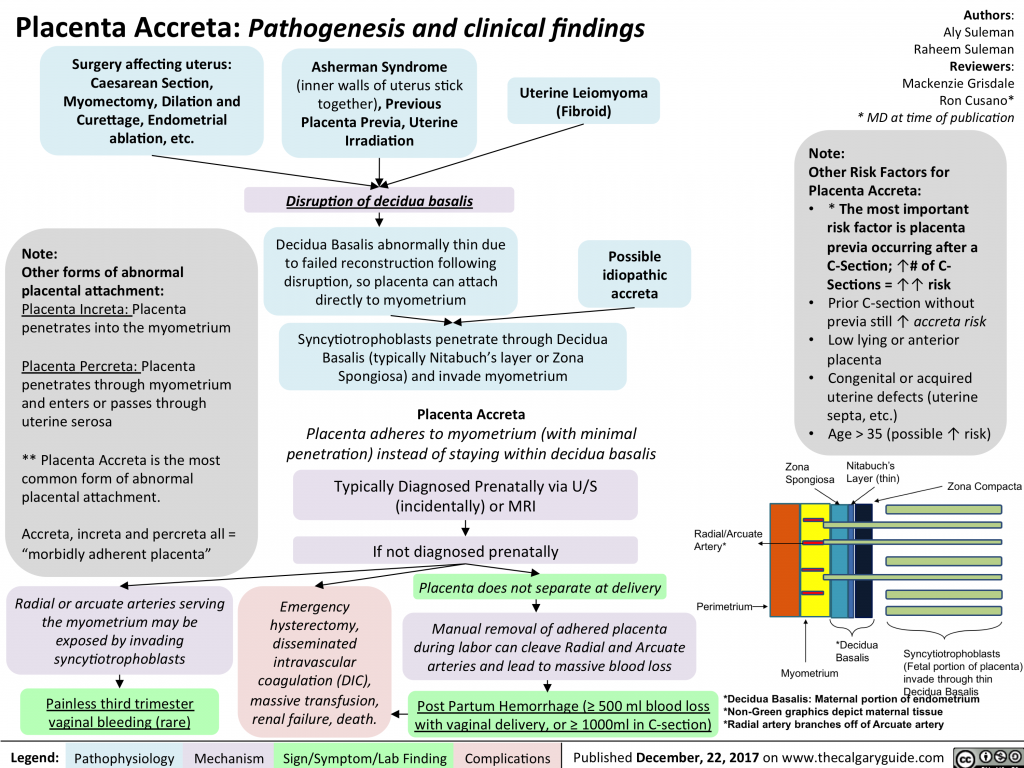 This also carries risks like severe vaginal bleeding, infection and blood clots. It may still be difficult to get pregnant in the future.
This also carries risks like severe vaginal bleeding, infection and blood clots. It may still be difficult to get pregnant in the future.
How early do you deliver with placenta accreta?
Most healthcare providers will recommend a C-section between 34 and 37 weeks gestation if there are no complications. This prevents you from having contractions or going into labor, as these can cause significant bleeding. Your healthcare provider may give you corticosteroids to help develop the fetus's lungs.
Prevention
Can I prevent placenta accreta?
You can’t prevent placenta accreta. The risk of placenta accreta increases if you’ve had multiple C-sections or a placental disorder like placenta previa. Talk to your provider about your chances of developing placenta accreta based on your health history.
Outlook / Prognosis
What is the outlook for people with placenta accreta?
The outlook is generally good when pregnancy care providers diagnose placenta accreta during pregnancy.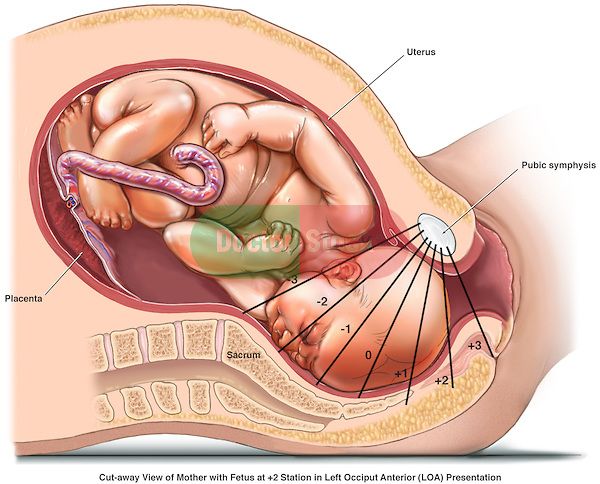 However, there will be complications associated with preterm labor and a possible hysterectomy. If your obstetrician removes your uterus, you’ll lose the ability to become pregnant again. This condition can also lead to massive blood loss, injury to the bowel or bladder and even death.
However, there will be complications associated with preterm labor and a possible hysterectomy. If your obstetrician removes your uterus, you’ll lose the ability to become pregnant again. This condition can also lead to massive blood loss, injury to the bowel or bladder and even death.
Can I have another baby after placenta accreta?
It depends on if you had a hysterectomy. Talk to your healthcare provider if you wish to become pregnant in the future. They may be able to prevent a hysterectomy to preserve your fertility.
What is the survival rate of placenta accreta?
The survival rate of placenta accreta is generally good. In most cases, this means you’ll have a hysterectomy to prevent postpartum hemorrhaging or other severe complications.
Living With
When should I call my healthcare provider?
Placenta accreta is a high-risk pregnancy condition. Your healthcare provider will monitor you closely and let you know what to expect for the rest of your pregnancy, delivery and recovery.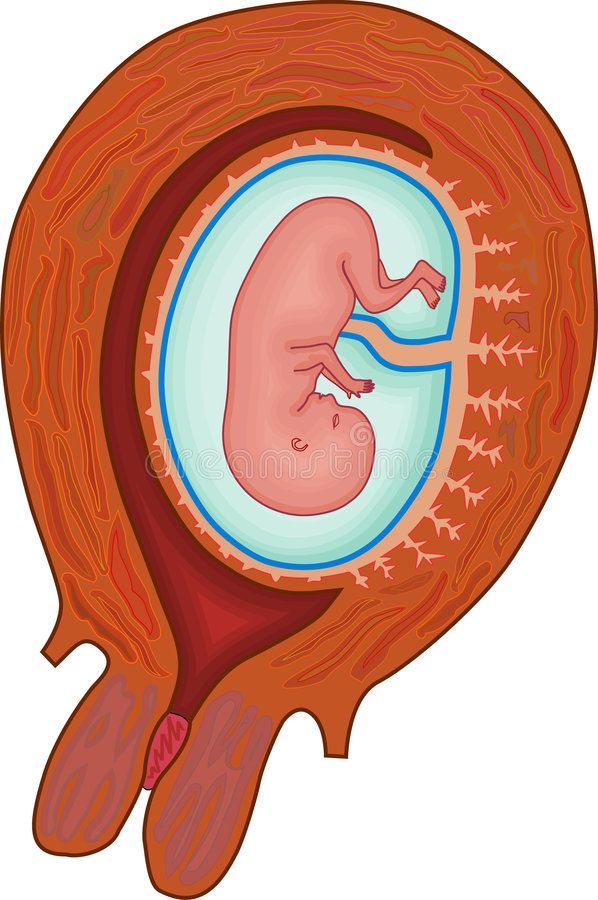 Contact them if you have questions about your diagnosis — they’re there to help you.
Contact them if you have questions about your diagnosis — they’re there to help you.
If at any point you begin bleeding heavily (soaking through a pad in less than an hour) or have pelvic pain, call 911.
What questions should I ask my obstetrician?
If you have placenta accreta, it’s normal to have questions. Some common questions to ask are:
- Will I have to give birth early?
- How is this condition treated?
- Do I need to be on bedrest or modify my daily activities?
- How do I know when to go to the hospital?
- Is a vaginal delivery possible?
- Will I be able to have a baby in the future?
- Will I need a hysterectomy?
Frequently Asked Questions
Does placenta accreta cause a hysterectomy?
Your healthcare provider makes every attempt to save your uterus; however, the risks of doing so may be too high. Most people with severe placenta accreta lose their uterus due to the life-threatening bleeding that can occur.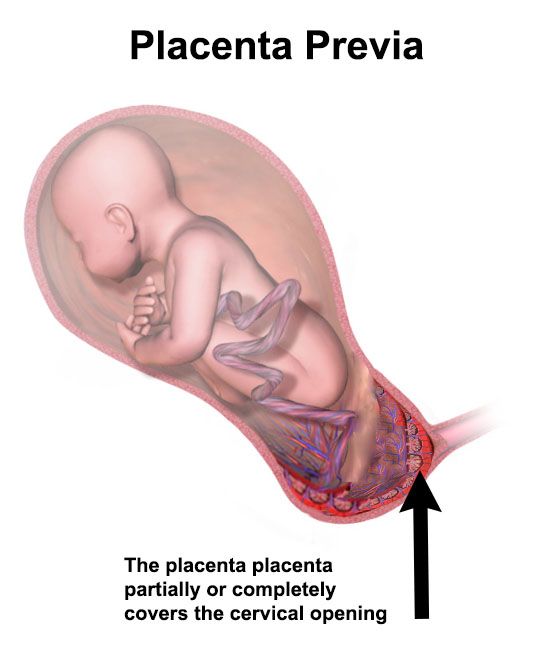 Talk to your healthcare provider about the likelihood of needing a hysterectomy based on your condition.
Talk to your healthcare provider about the likelihood of needing a hysterectomy based on your condition.
A note from Cleveland Clinic
Placenta accreta is a potentially life-threatening condition that doesn’t typically cause symptoms during pregnancy. However, an early diagnosis via ultrasound and close monitoring can help lower your risk for complications from placenta accreta. In some cases, placenta accreta isn’t discovered until after your baby is delivered. Talk to your healthcare provider about what you can expect if you have placenta accreta. They’re there to keep you and your baby safe and healthy.
Types, Risks, Causes & Treatment
Overview
Placenta accreta is a pregnancy complication that occurs when the placenta embeds too deep in the uterine wall.What is placenta accreta?
Placenta accreta is a condition where the placenta (the food and oxygen source for a fetus) grows too deeply into the wall of your uterus. In a typical pregnancy, the placenta easily detaches from the wall of your uterus after your baby is born.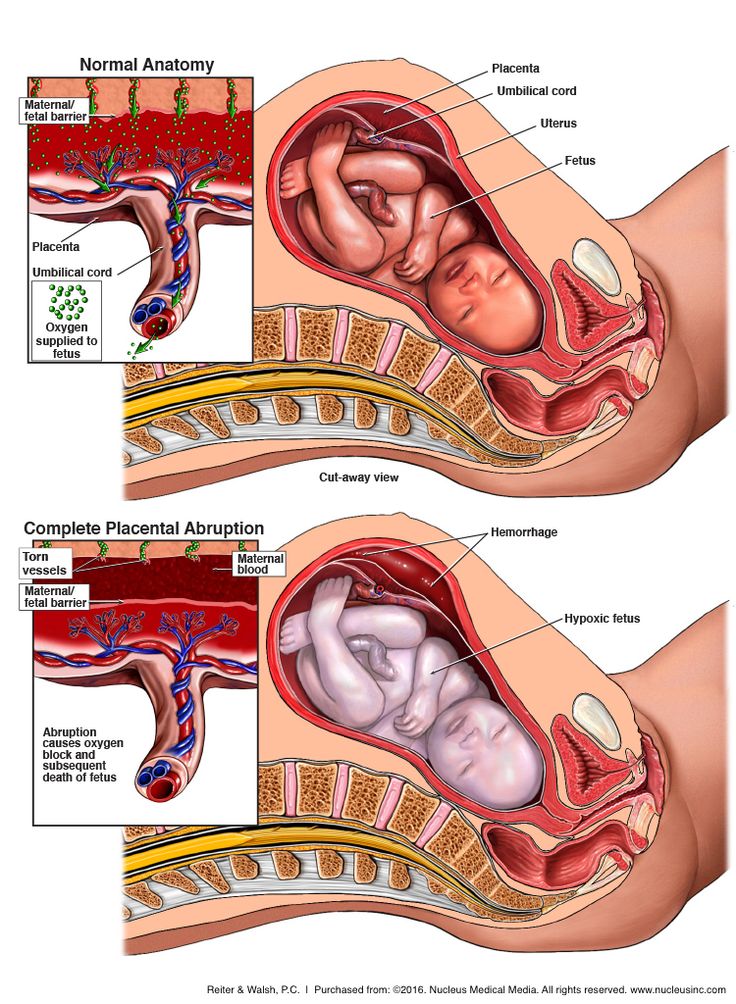 In placenta accreta, the placenta has grown into your uterine wall and doesn’t separate easily following delivery. In severe cases, it can lead to life-threatening vaginal bleeding. It may require a blood transfusion and hysterectomy (removal of your uterus). Pregnancy care providers diagnose placenta accreta during pregnancy or during delivery. Treatment usually involves an early Cesarean delivery (C-section) followed by a hysterectomy to minimize the risk of severe complications.
In placenta accreta, the placenta has grown into your uterine wall and doesn’t separate easily following delivery. In severe cases, it can lead to life-threatening vaginal bleeding. It may require a blood transfusion and hysterectomy (removal of your uterus). Pregnancy care providers diagnose placenta accreta during pregnancy or during delivery. Treatment usually involves an early Cesarean delivery (C-section) followed by a hysterectomy to minimize the risk of severe complications.
What are the different types of placenta accreta?
There are three types of placenta accreta. Providers determine the type based on how deeply the placenta is attached to your uterus.
- Placenta accreta: The placenta firmly attaches to the wall of your uterus. It doesn’t pass through the wall of the uterus or impact the muscles of the uterus. This is the most common type.
- Placenta increta: In this type, the placenta is more deeply embedded in the wall of your uterus.
 It still doesn’t pass through the uterine wall but is firmly attached to the muscle of the uterus. Placenta increta accounts for about 15% of cases.
It still doesn’t pass through the uterine wall but is firmly attached to the muscle of the uterus. Placenta increta accounts for about 15% of cases. - Placenta percreta: The most severe of the types, placenta percreta happens when the placenta passes through the wall of your uterus. The placenta might grow through your uterus and impact other organs, such as your bladder or intestines. It accounts for about 5% of cases.
Who’s at risk for placenta accreta?
You’re at higher risk for placenta accreta if you:
- Have had previous Cesarean deliveries.
- Have a placenta in an abnormal location in your uterus.
- Have had previous surgeries on your uterus.
- Have had more than one pregnancy.
- Are pregnant via IVF.
Does placenta accreta harm the fetus?
Placenta accreta doesn’t directly harm the fetus. Placenta accreta often leads to preterm birth. Preterm birth carries risks such as respiratory problems or trouble gaining weight. Babies born before 37 weeks of pregnancy have a higher risk of being admitted to a neonatal intensive care unit (NICU) for specialized treatment.
Babies born before 37 weeks of pregnancy have a higher risk of being admitted to a neonatal intensive care unit (NICU) for specialized treatment.
What are the risks of placenta accreta to the birthing person?
- Premature delivery.
- Damage to your uterus and surrounding organs.
- Loss of fertility due to hysterectomy.
- Excessive bleeding that requires a blood transfusion.
- Blood clotting issues.
- Lung or kidney failure.
- Death.
How common is placenta accreta?
Placenta accreta may affect up to 1 in 533 pregnancies. The occurrence of placenta accreta has increased over the last several decades, mostly due to the increased rate of C-sections.
Symptoms and Causes
What causes placenta accreta?
Abnormalities with the lining of your uterus cause placenta accreta. Your uterine lining can become damaged or scarred from prior uterine surgeries. It can also happen to people who haven’t had any uterine surgery.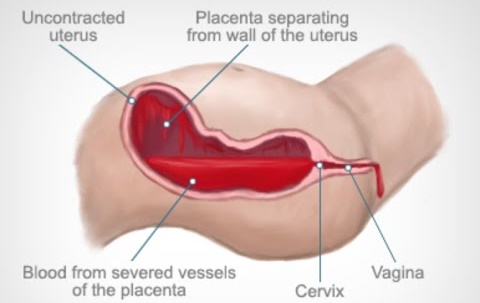
The risk factors for placenta accreta are:
- Multiple C-sections: People who’ve had multiple C-sections have a higher risk of developing placenta accreta. This results from scarring of your uterus from the procedures. The more cesarean sections a woman has over time, the higher her risk of placenta accreta. Multiple cesareans are present in over 60% of cases.
- History of uterine surgeries: If you’ve had a uterine fibroid (a noncancerous growth or tumor of the uterine muscle) removed, the scarring could lead to placenta accreta. Surgeries such as curettage (removing tissue from your uterus) or endometrial ablation can also lead to scarring.
- Placenta previa: This condition occurs when the placenta blocks your cervix. In people with placenta previa and a history of prior C-section deliveries, the risk for placenta accreta increases with the number of C-sections they’ve had.
What are the symptoms of placenta accreta?
There are usually no symptoms of placenta accreta.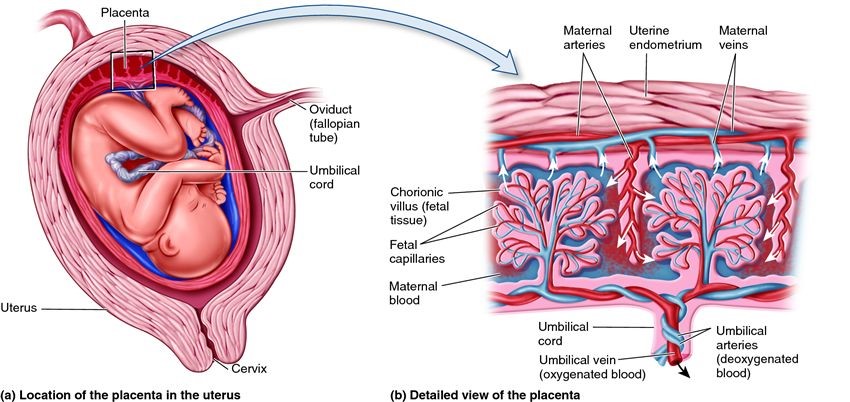 In some cases, you may experience bleeding in the third trimester of pregnancy (weeks 28 to 40) or pelvic pain (from the placenta pressing on your bladder or other organs).
In some cases, you may experience bleeding in the third trimester of pregnancy (weeks 28 to 40) or pelvic pain (from the placenta pressing on your bladder or other organs).
Diagnosis and Tests
How is placenta accreta diagnosed?
A prenatal ultrasound can diagnose placenta accreta during pregnancy. Magnetic resonance imaging (MRI) can be helpful in some cases to show how deeply the placenta has penetrated your uterine wall.
In other cases, pregnancy care providers discover placenta accreta after your baby is born. Ideally, uterine contractions expel the placenta within 30 minutes of delivery. When this doesn’t occur, your provider may suspect placenta accreta.
How important is an early diagnosis of placenta accreta?
An early diagnosis of placenta accreta is essential because it can allow multiple healthcare providers to become involved in your pregnancy and delivery care. For example, a neonatologist may be involved in your newborn’s care, or a perinatologist may be involved in yours.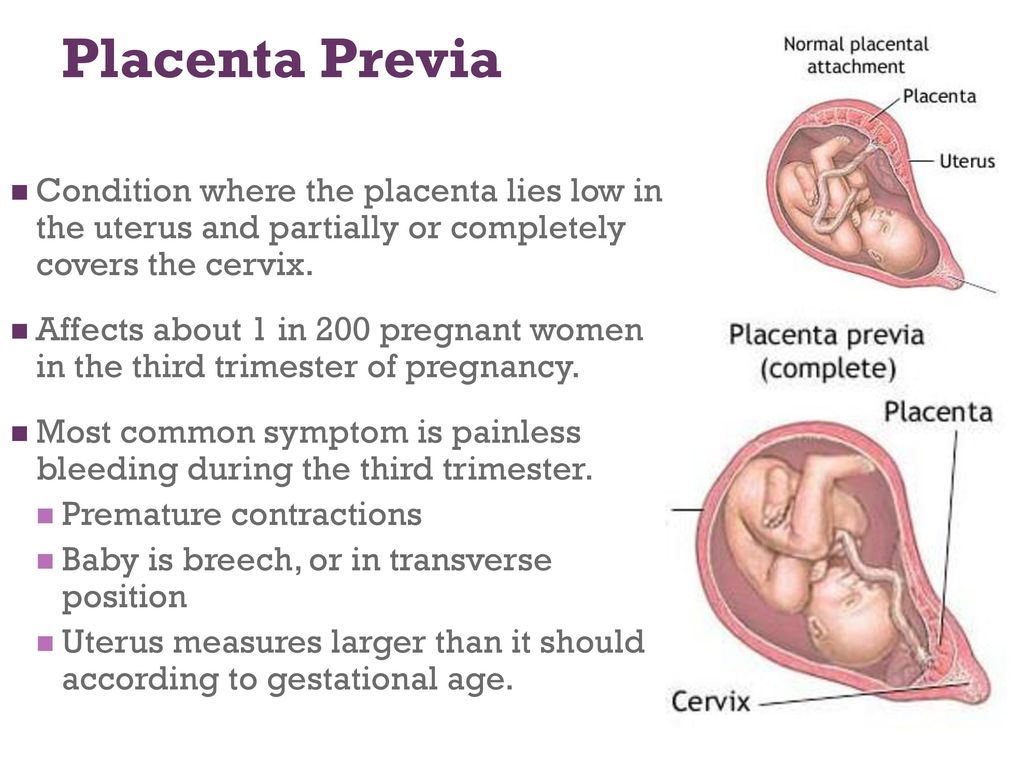 Your provider will monitor you closely to ensure the best results for you and your baby.
Your provider will monitor you closely to ensure the best results for you and your baby.
Having the right people involved could prevent the removal of your uterus (hysterectomy) or life-threatening blood loss. In some cases, providers can’t avoid a hysterectomy and blood transfusion despite an early diagnosis; however, risks for other complications decrease with early diagnosis.
Management and Treatment
How is placenta accreta treated?
Treatment of placenta accreta can vary. If your provider diagnoses it before delivery, they’ll monitor you closely for the rest of your pregnancy. You may be hospitalized or put on bed rest to prevent preterm labor. Your provider will schedule a C-section to deliver your baby, usually around between 34 and 37 weeks. This is done to decrease the risk of bleeding from contractions or labor. If you wish to have future pregnancies, your healthcare provider can try to save your uterus.
However, in severe cases where the placenta is deeply or firmly attached or invading into other organs, a hysterectomy (removal of the uterus) may be the safest option.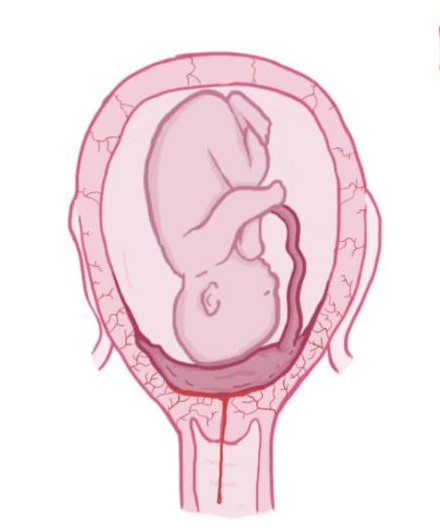 A Cesarean hysterectomy is when your uterus is removed at the time of a C-section delivery. In this case, your provider will deliver your baby, your uterus and the placenta at the same time. Removing your uterus with the placenta still attached minimizes the risk of excessive bleeding (hemorrhaging).
A Cesarean hysterectomy is when your uterus is removed at the time of a C-section delivery. In this case, your provider will deliver your baby, your uterus and the placenta at the same time. Removing your uterus with the placenta still attached minimizes the risk of excessive bleeding (hemorrhaging).
Some healthcare providers will leave small parts of the placenta inside your uterus because the placenta dissolves over time. This also carries risks like severe vaginal bleeding, infection and blood clots. It may still be difficult to get pregnant in the future.
How early do you deliver with placenta accreta?
Most healthcare providers will recommend a C-section between 34 and 37 weeks gestation if there are no complications. This prevents you from having contractions or going into labor, as these can cause significant bleeding. Your healthcare provider may give you corticosteroids to help develop the fetus's lungs.
Prevention
Can I prevent placenta accreta?
You can’t prevent placenta accreta.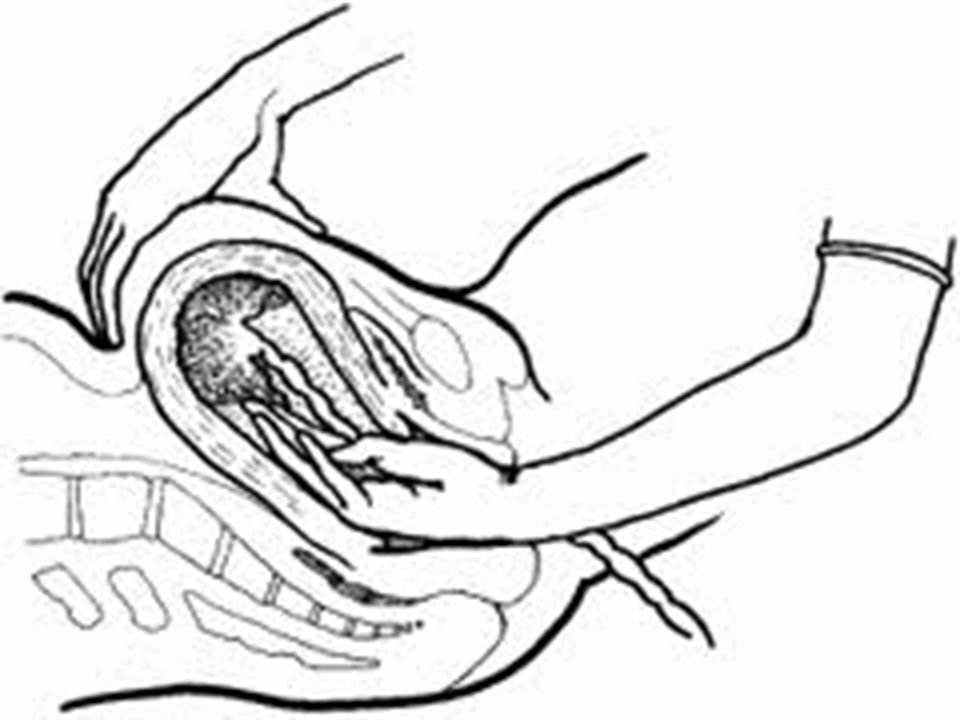 The risk of placenta accreta increases if you’ve had multiple C-sections or a placental disorder like placenta previa. Talk to your provider about your chances of developing placenta accreta based on your health history.
The risk of placenta accreta increases if you’ve had multiple C-sections or a placental disorder like placenta previa. Talk to your provider about your chances of developing placenta accreta based on your health history.
Outlook / Prognosis
What is the outlook for people with placenta accreta?
The outlook is generally good when pregnancy care providers diagnose placenta accreta during pregnancy. However, there will be complications associated with preterm labor and a possible hysterectomy. If your obstetrician removes your uterus, you’ll lose the ability to become pregnant again. This condition can also lead to massive blood loss, injury to the bowel or bladder and even death.
Can I have another baby after placenta accreta?
It depends on if you had a hysterectomy. Talk to your healthcare provider if you wish to become pregnant in the future. They may be able to prevent a hysterectomy to preserve your fertility.
What is the survival rate of placenta accreta?
The survival rate of placenta accreta is generally good. In most cases, this means you’ll have a hysterectomy to prevent postpartum hemorrhaging or other severe complications.
In most cases, this means you’ll have a hysterectomy to prevent postpartum hemorrhaging or other severe complications.
Living With
When should I call my healthcare provider?
Placenta accreta is a high-risk pregnancy condition. Your healthcare provider will monitor you closely and let you know what to expect for the rest of your pregnancy, delivery and recovery. Contact them if you have questions about your diagnosis — they’re there to help you.
If at any point you begin bleeding heavily (soaking through a pad in less than an hour) or have pelvic pain, call 911.
What questions should I ask my obstetrician?
If you have placenta accreta, it’s normal to have questions. Some common questions to ask are:
- Will I have to give birth early?
- How is this condition treated?
- Do I need to be on bedrest or modify my daily activities?
- How do I know when to go to the hospital?
- Is a vaginal delivery possible?
- Will I be able to have a baby in the future?
- Will I need a hysterectomy?
Frequently Asked Questions
Does placenta accreta cause a hysterectomy?
Your healthcare provider makes every attempt to save your uterus; however, the risks of doing so may be too high.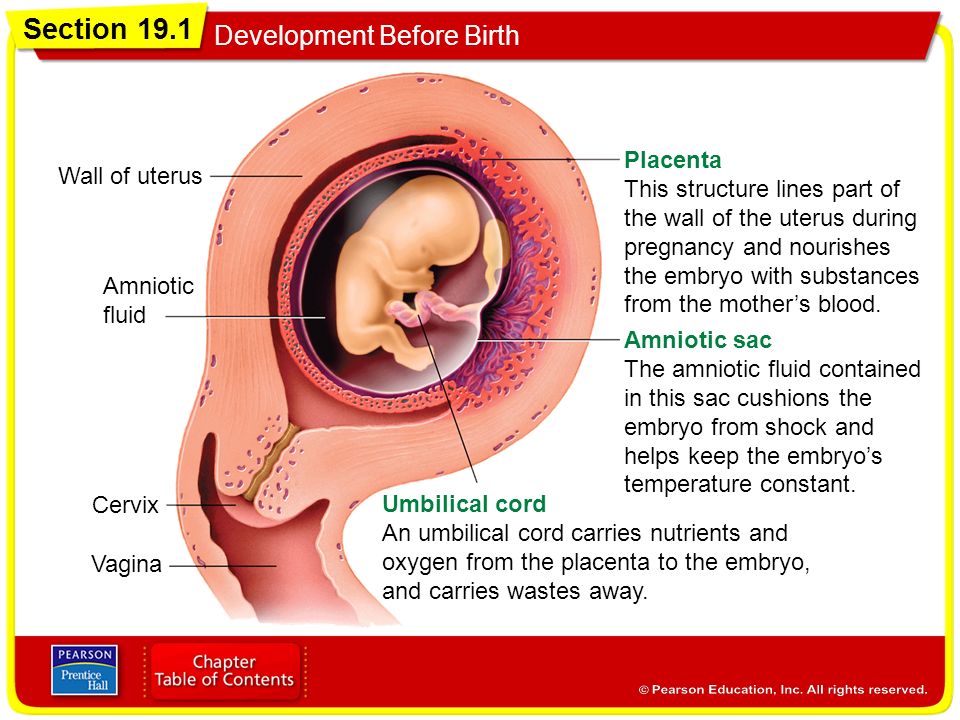 Most people with severe placenta accreta lose their uterus due to the life-threatening bleeding that can occur. Talk to your healthcare provider about the likelihood of needing a hysterectomy based on your condition.
Most people with severe placenta accreta lose their uterus due to the life-threatening bleeding that can occur. Talk to your healthcare provider about the likelihood of needing a hysterectomy based on your condition.
A note from Cleveland Clinic
Placenta accreta is a potentially life-threatening condition that doesn’t typically cause symptoms during pregnancy. However, an early diagnosis via ultrasound and close monitoring can help lower your risk for complications from placenta accreta. In some cases, placenta accreta isn’t discovered until after your baby is delivered. Talk to your healthcare provider about what you can expect if you have placenta accreta. They’re there to keep you and your baby safe and healthy.
Case of successful completion of pregnancy with placenta accreta
Placenta ingrowth in patients with a uterine scar after previous caesarean section operations is an extremely important problem that is actively discussed in modern obstetrics.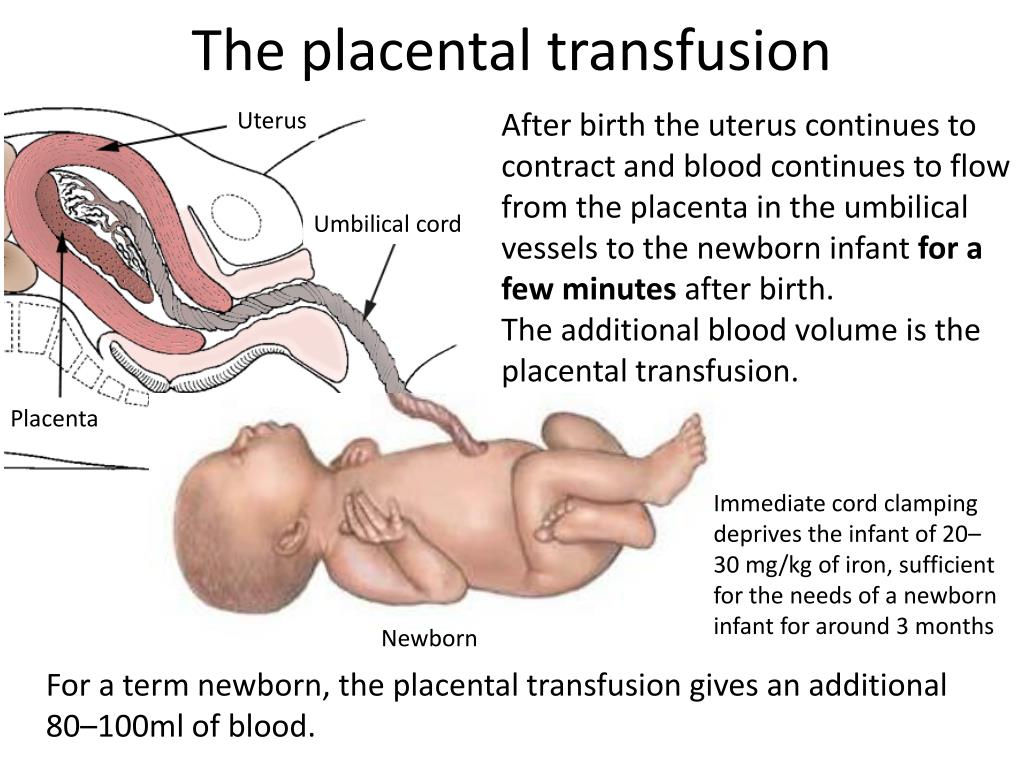 This type of complication is increasingly being diagnosed in women with repeated pregnancies after caesarean section operations, the number of which continues to be high due to the expansion of indications for operative delivery. During delivery, massive bleeding inevitably occurs, which poses a danger to the life of the mother.
This type of complication is increasingly being diagnosed in women with repeated pregnancies after caesarean section operations, the number of which continues to be high due to the expansion of indications for operative delivery. During delivery, massive bleeding inevitably occurs, which poses a danger to the life of the mother.
Previously, when placenta accreta, surgeons made a radical decision - they removed the uterus, which, however, did not reduce blood loss and, moreover, deprived the patient of reproductive function in the future.
Today it is possible to perform organ-preserving surgeries using methods of temporary reduction of the blood supply to the uterus (devascularization), such as temporary occlusion of the common iliac arteries with balloon catheters, embolization of the uterine arteries, ligation of the internal iliac arteries, creation of tunnels in the broad ligament of the uterus with temporary placement of a Folley catheter on lower segment area. An innovative organ-preserving surgical technique is used - a bottom caesarean section with metroplasty (excision of a section of the uterus with placenta ingrowth). Blood loss is replenished by reinfusion of own blood using the Cell Saver apparatus.
Blood loss is replenished by reinfusion of own blood using the Cell Saver apparatus.
Clinical case: Pregnant D., 37 years old, was admitted to the maternity hospital with a referral from the antenatal clinic doctor for delivery. The patient had a history of a caesarean section, during this pregnancy an ultrasound examination diagnosed placenta previa and suspected placenta ingrowth. On an outpatient basis, additional diagnostics were performed - MRI, the diagnosis was confirmed.
Considering placenta previa and suspected placenta accreta, a decision was made at 37-38 weeks of gestation to perform a planned delivery by caesarean section in an X-ray operating room.
Delivery was carried out by two teams of doctors: obstetrician-gynecologists - Ivan Osokin and Vasily Grabovsky - and X-ray surgeons Alexander Vanyukov and Sergey Bondarenko. During the operation, placenta ingrowth was confirmed on a fairly large (6 cm in size) area of the anterior wall of the uterus.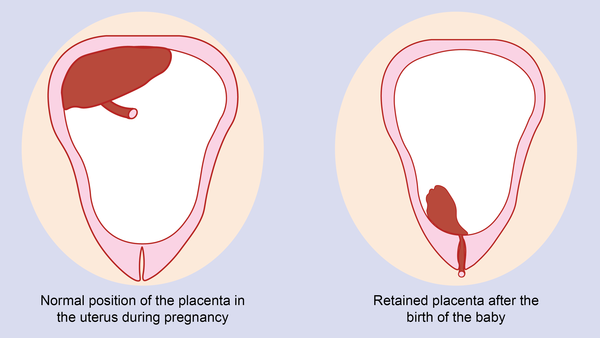 Given this feature, a caesarean section was performed in the area of the uterine fundus, as a result of which a live full-term baby was born.
Given this feature, a caesarean section was performed in the area of the uterine fundus, as a result of which a live full-term baby was born.
After the birth of the child, the doctors had to perform an operation to excise a section of the uterus with an ingrown placenta. To avoid massive bleeding, radiologists performed a temporary occlusion of the common iliac arteries.
Comments by the head of the Department of X-ray Surgical Methods of Diagnosis and Treatment Alexander Evgenievich Vanyukov:
- Usually, for this procedure, a puncture of the left and right common femoral arteries is performed. However, the puncture of the femoral arteries is associated with severe discomfort for the patient, because. requires prolonged immobilization of the limb and tight bandaging in the area of the surgical wound with median access for caesarean section. Also, for the puncture of the femoral artery, a greater number of postoperative hematomas and bleeding. Based on this, we decided to use the left and right radial arteries as arterial access.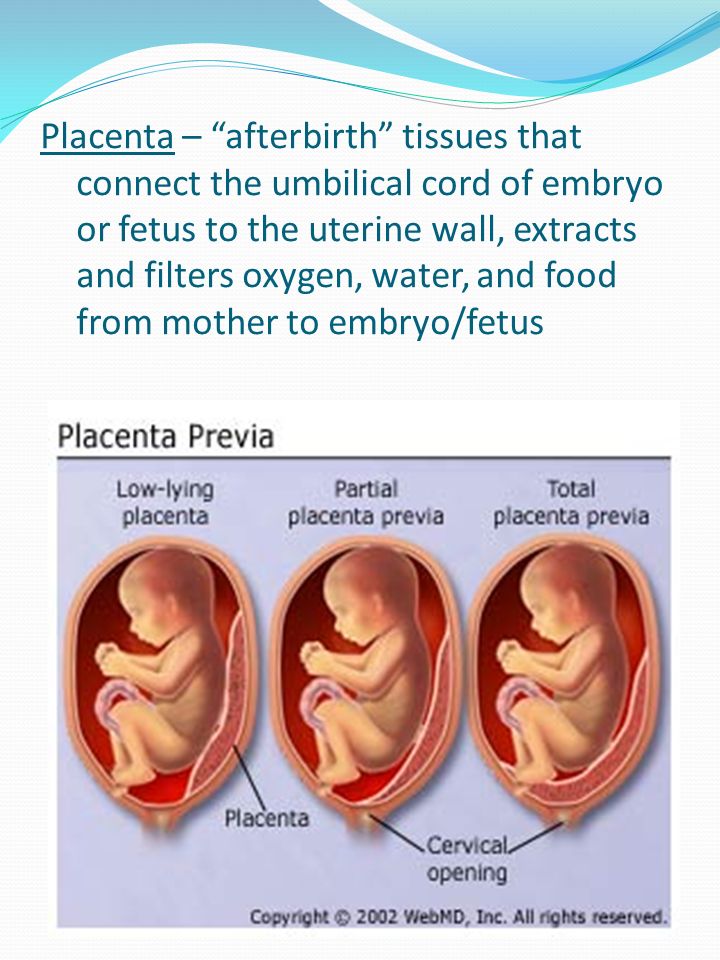 These are the arteries of the hand. Our part of the work begins after the birth of the child, so as not to expose the newborn to radiation exposure. Under x-ray navigation using a C-arm, a puncture of the left and right radial arteries was performed. Balloon catheters were passed through the aorta and placed in the left and right common iliac arteries. From that moment on, we were ready to perform intra-arterial hemostasis (ie stop bleeding) at any second. This time, emergency hemostasis was not required, and before surgeons began to separate the ingrown part of the placenta from the uterine body, we inflated the balloon catheters in the common iliac arteries, thereby cutting off the blood flow in the vessels supplying the uterus. When the placenta was removed and the body of the uterus was sutured, the balloons were deflated to ensure there was no bleeding. Then the balloons and guiding catheters were removed, and bandages were applied to the puncture site. This technique made it possible to preserve the uterus and avoid massive blood loss.
These are the arteries of the hand. Our part of the work begins after the birth of the child, so as not to expose the newborn to radiation exposure. Under x-ray navigation using a C-arm, a puncture of the left and right radial arteries was performed. Balloon catheters were passed through the aorta and placed in the left and right common iliac arteries. From that moment on, we were ready to perform intra-arterial hemostasis (ie stop bleeding) at any second. This time, emergency hemostasis was not required, and before surgeons began to separate the ingrown part of the placenta from the uterine body, we inflated the balloon catheters in the common iliac arteries, thereby cutting off the blood flow in the vessels supplying the uterus. When the placenta was removed and the body of the uterus was sutured, the balloons were deflated to ensure there was no bleeding. Then the balloons and guiding catheters were removed, and bandages were applied to the puncture site. This technique made it possible to preserve the uterus and avoid massive blood loss.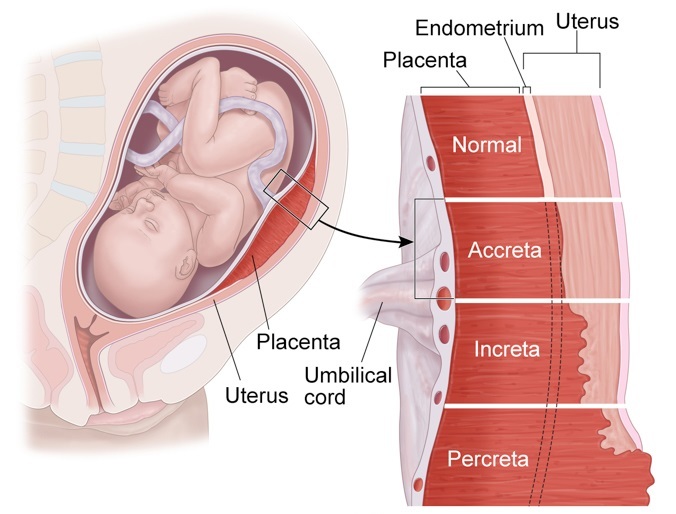 In addition, radial access allows you to maintain mobility in the limbs and is much safer than the femoral one.
In addition, radial access allows you to maintain mobility in the limbs and is much safer than the femoral one.
This story ended happily for the mother and the newborn thanks to the well-coordinated work of obstetrician-gynecologists and doctors from the Department of Endovascular Surgery.
Operating team:
Obstetrician-gynecologists: Grabovsky V. M., Osokin I. P.
X-ray endovascular surgeons: Vanyukov A. E., Bondarenko S. A. Sizova I.Yu.
Operating nurse: Rzyankina O.
Obstetrician-gynecologists: Yu. A. Bogatyrev, A. N. Efremov
Birth history: Placenta accreta
If you are told that the best decision is to terminate the pregnancy, seek a second opinion. Sometimes it helps to save a whole life - the life of an unborn baby. This was the case with our patient.
A 43-year-old woman came to the EMC for a consultation and a decision on the issue of delivery.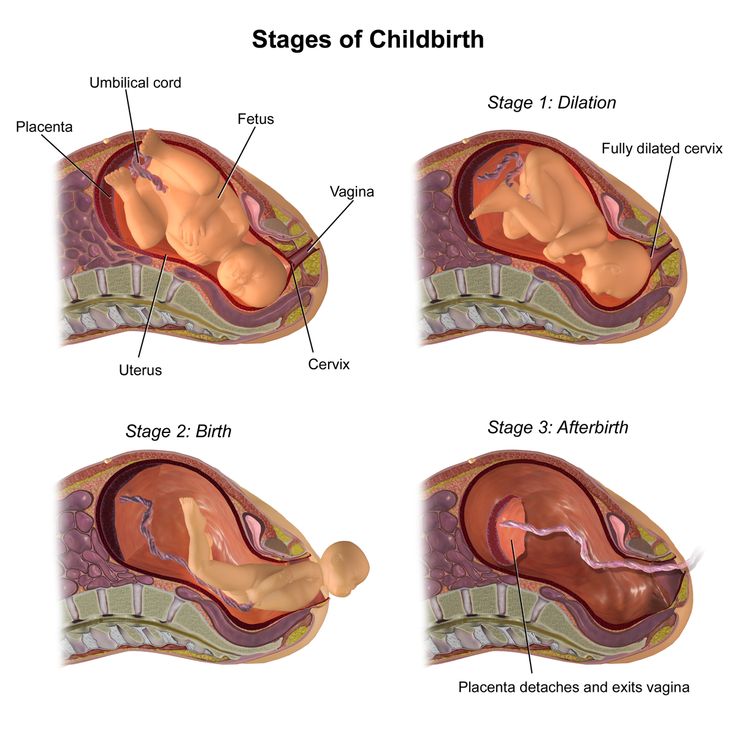
The patient had a third pregnancy, but a second birth was coming. The first pregnancy was non-developing. The second ended with operative delivery with removal of the myomatous node in the region of the lower uterine segment.
The third pregnancy occurred 6 months after delivery. Maria and her husband were happy to find out that they were expecting a girl. However, the pregnancy was difficult. Doctors in my hometown recommended terminating the pregnancy: it came too early after the first birth and the chorion was located in the area of the scar after a cesarean section - there was a risk of placenta ingrowth. The family did not want to put up with such a difficult decision. And the couple turned to the EMC Perinatal Center for help.
Placenta accreta is a terrible complication of pregnancy, in which placental vessels grow into the muscular layer of the uterus and even the bladder wall. In most cases, placenta ingrowth is diagnosed in patients who have undergone a caesarean section!
Doctors performed all the necessary examinations, including ultrasonography of the scar with dopplerometry, MRI of the scar to assess the degree of ingrowth.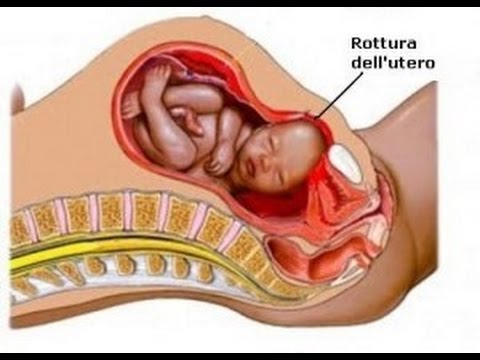 The diagnosis of placenta previa and placenta ingrowth into the scar after CS was confirmed.
The diagnosis of placenta previa and placenta ingrowth into the scar after CS was confirmed.
Based on the results of the survey, a consultation was held consisting of all the necessary EMC specialists. The experts came to the conclusion that with a certain tactics of managing the patient and extremely careful observation, it is absolutely realistic to carry out a successful delivery. The team of obstetricians, vascular surgeons, anesthesiologists and transfusiologists was ready to start the operation at any time. She was scheduled for 36 weeks, but labor began 4 days earlier. Thanks to an individual approach to each of our patients and round-the-clock readiness of the team, within minutes after hospitalization, the pregnant woman was ready for urgent delivery.
The patient underwent an inferomedian laparotomy, clipping (clamping) of the internal iliac arteries, a fundus caesarean section, metroplasty (plastic of the uterus), balloon tamponade of the uterus (intrauterine insertion of a special balloon that creates compression of the uterus from the inside and minimizes the risk of bleeding in the postoperative period), hardware reinfusion of autologous blood (transfusion of one's own blood during surgery from an operating wound, using special equipment).