What cause thrush in toddlers
Causes, Treatment and When to See a Doctor
Nationwide Children’s Hospital
Thrush is an infection caused by a fungus called candida (CAN-did-ah). Candida is naturally present in the mouth and body and is usually harmless. But, if conditions are right, it can grow out of control and cause an infection.
- A candida infection in the mouth is called oral thrush; in the diaper area, a yeast diaper rash; in other places on or in the body, a yeast infection.
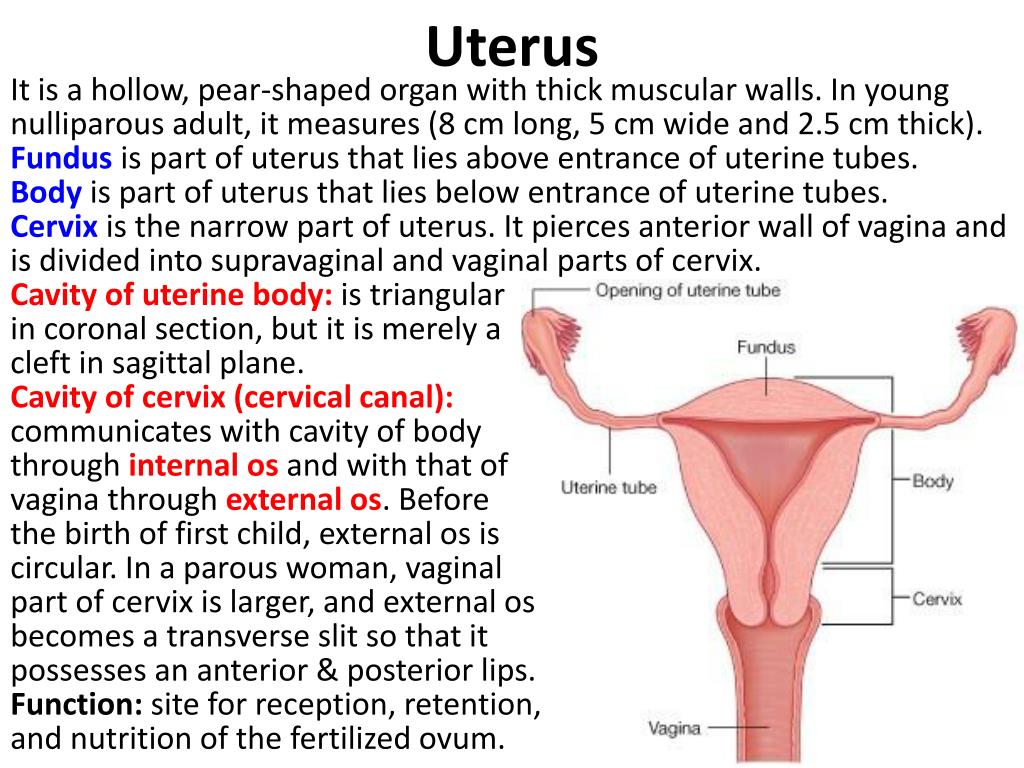
- Candida is the same fungus that causes vaginal yeast infections.
- Oral thrush is more common in infants and toddlers, but older children can get it too.
- Thrush is contagious (catching) and can be passed to others.
Risk Factors for Getting Thrush Are:
- Age – born early (premature) or younger than 6 months or low birth weight
- Getting it during birth from the parent who has an unknown vaginal yeast infection
- Breastfeeding with an untreated yeast infection of the breast
- Using human milk from a pump that has not been properly sterilized
- Sucking on a pacifier or bottle too often and for too long
- Using an inhaler for asthma without rinsing the mouth after use
- Recent history of child or nursing parent taking antibiotic medicine to treat a bacterial infection
- A weakened immune system
Signs and Symptoms
- Thrush in the mouth:
- Can be on the tongue, gums, roof of the mouth, or inside of the cheeks.
- Begins as tiny, flat, white, or creamy yellow spots. These spots come together and form cheesy patches that look like cottage cheese. The spots are often mistaken for milk patches. Sometimes it looks like a white coating.
- Cannot be removed with a soft cloth or a cotton-tipped swab without causing bleeding.
- May cause pain while sucking or swallowing. Your child may not drink or eat as much as usual.
- Can be on the tongue, gums, roof of the mouth, or inside of the cheeks.
- Yeast infections in the diaper area look like diaper rash. The skin can have:
- Small or big red patches, be entirely bright red, or have raised edges or small bumps
- Pimples that ooze pus
- A vaginal yeast infection can cause the skin to be red, itchy, and burn. Often, there is a creamy discharge from the vagina.
Treatment
- Thrush is easily treated with an antifungal medicine such as nystatin (Mycostatin®), fluconazole (Diflucan®), or itraconazole (Sporanox®).
 Your child may get these medicines as a syrup or a pill.
Your child may get these medicines as a syrup or a pill. - Thrush usually clears up in 4 to 5 days. It is important to use all of the medicine for the length of time that is recommended.
- An antifungal cream is usually recommended for yeast infections in the diaper area, in the vagina, or other places on the skin. You can buy some of these medicines without a prescription.
- Avoid using any home remedies without asking your child’s health care provider first.
How to Give Oral Drops
- A liquid medicine comes with a dropper in the box. Use it to give the oral drops.
- You will put the drops directly in the mouth on the sores. The medicine needs to stay in the mouth for a while. It will not hurt your child to swallow it.
- Plan to give the drops right after you feed your baby.
Follow These Steps:
- Wash your hands well.
- For an infant or young child, place them on their back.
 Turn their head sideways so that the cheek with the white patches faces down toward the bed (Picture 1).
Turn their head sideways so that the cheek with the white patches faces down toward the bed (Picture 1). - Gently open your child’s mouth and drop half of the medicine inside the cheek. Turn your child’s head the other way and repeat squirting the medicine inside the other cheek.
- Using a cotton-tipped swab, spread the medicine inside the mouth over the white patches.
- For an older child, have them swish the medicine in their mouth for 30 seconds and then swallow.
- Wait 30 minutes before giving your child anything to eat or drink.
- Always wash your hands well before and after touching your child’s mouth or things that have touched their mouth. This is so you do not pass the infection to others.
- Be sure your child drinks plenty of liquids so that they do not get dehydrated (lose too much fluid).
- Sterilize baby bottle nipples after each use.
 Do this by placing the nipples in boiling water for 10 minutes. Let the nipples cool before using them.
Do this by placing the nipples in boiling water for 10 minutes. Let the nipples cool before using them. - Limit breastfeeding and bottle feeding to 20 minutes. Sucking for a long time can increase irritation.
- If your baby uses a pacifier:
- Let them use it only when they cannot be calmed in any other way.
- Buy several extras that can be sterilized between uses. Sterilize pacifiers the same way as the bottle nipples.
- Do not put your child’s pacifier in your mouth or let other children do this.
- Do not share bottles, cups, or toys that your child has used with others.
- If you are breastfeeding:
- Clean each breast with water and air-dry after each feeding.
- If your breasts show any signs of infection, such as soreness or redness, call your health care provider. You may need to be treated at the same time.
- If using human breast milk from a pump, all pump parts need to be sterilized.
Treatment of a Yeast Rash
If your baby has a yeast diaper rash or yeast infection on the skin, the health care provider will prescribe a cream or recommend an over-the-counter one.
- Wash your hands well before and after treating your child’s yeast infection.
- To help the skin heal, keep it clean and dry.
For a Yeast Diaper Rash:
- Change the diaper as soon as your baby pees or poops. You may also want to change the diaper once during the night.
- Rinse your baby’s bottom after each diaper change. Gently clean the diaper area from front to back and inside the skin folds with warm water and a soft washcloth (Picture 2).
- Try to avoid baby wipes, but especially those with alcohol, propylene glycol, and fragrances.
- Use mild soap and water only if the poop (stool) does not come off easily.
- Avoid scrubbing or rubbing. It can damage the skin more.
- If the rash is severe, use a squirt bottle of water to clean and rinse without rubbing.
 Or you can soak your baby’s bottom in a tub of warm water after each diaper change.
Or you can soak your baby’s bottom in a tub of warm water after each diaper change. - Pat the skin dry and let it air dry fully.
- Apply a thin layer of antifungal cream. Most should be used only 2 to 3 times a day.
- You can also use an over-the-counter skin barrier or zinc oxide cream over the antifungal cream on the baby’s bottom and in the skin folds. Apply a thick layer each time the diaper is changed. Popular ones are petroleum jelly (Vaseline®) or a cream with zinc oxide like Desitin®, Triple Paste®, A+D®, or Balmex®. These creams do not have to be completely washed off with each diaper change.
- Do not use steroidal creams, corn starch, talc, or baby powder on your baby’s bottom.
- Let your baby play or nap with their diaper off. The air helps dry and heal the rash (Picture 3).
- Avoid rubber pants or plastic liners over the diaper.
- Put the diaper on loosely so it does not rub against the skin as much.
- Call your child’s health care provider if thrush gets worse after 3 days of treatment, if it lasts more than 10 days, or you have any questions.
Thrush and Yeast Infections (PDF), Somali (PDF), Spanish (PDF)
HH-I-117 6/90, Revised 3/22 Copyright 1990, Nationwide Children's Hospital
Oral Thrush (for Parents) - Nemours KidsHealth
en español: Muguet (candidiasis oral)
Reviewed by: Michelle P. Tellado, MD
What Is Oral Thrush?
Oral thrush is a very common yeast infection in babies. It causes irritation in and around a baby's mouth.
What Are the Signs and Symptoms of Oral Thrush?
Oral thrush (also called oral candidiasis) can affect anyone, but is most common in babies younger than 6 months old and in older adults.
A baby with oral thrush might have cracked skin in the corners of the mouth or white patches on the lips, tongue, or inside the cheeks that look a little like cottage cheese but can't be wiped away.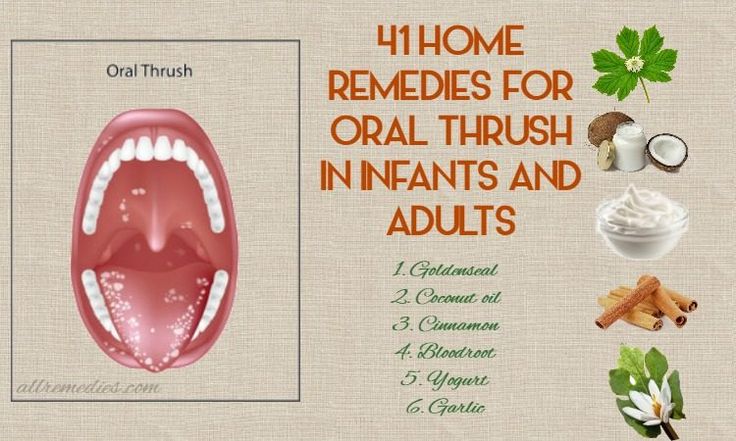
Some babies may not feed well or are uncomfortable when sucking because their mouth feels sore, but many babies don't feel any pain or discomfort.
What Causes Oral Thrush?
Oral thrush is caused by the overgrowth of a yeast (a type of fungus) called Candida albicans.
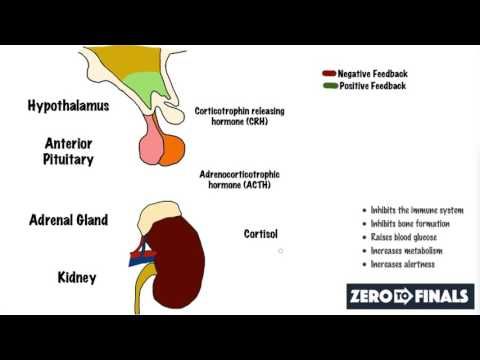
Most people (including infants) naturally have Candida in their mouths and digestive tracts, which is considered normal growth. Usually, a healthy immune system and some "good" bacteria control the amount of this fungus in the body.
But if the immune system is weakened (from an illness or medicines like chemotherapy) or not fully developed (as in babies), Candida in the digestive tract can overgrow and lead to an infection. Candida overgrowth also causes diaper rash and vaginal yeast infections. Babies can have oral thrush and a diaper rash at the same time.
Candida overgrowth also can happen after a baby has been given antibiotics for a bacterial infection because antibiotics can kill off the "good" bacteria that keep the Candida from growing. Oral thrush also can happen after the use of steroid medicines.
Oral thrush also can happen after the use of steroid medicines.
How Is Oral Thrush Treated?
See your doctor if you think your baby may have thrush. Some cases go away without medical treatment within a week or two, but the doctor may prescribe an antifungal solution for your baby's mouth. This medicine is usually applied several times a day by "painting" it on the inside of the mouth and tongue with a sponge applicator.
Depending on your baby's age, the doctor also might suggest adding yogurt with lactobacilli to your baby's diet. The lactobacilli are "good" bacteria that can help get rid of the yeast in your child's mouth.
If your baby keeps getting oral thrush, especially if he or she is older than 9 months old, talk with your doctor because this might be a sign of another health issue.
Can Oral Thrush Be Prevented?
Oral thrush is a common infection in babies, but you can help prevent it:
- If you formula-feed your baby or use a pacifier, thoroughly clean the nipples and pacifiers in hot water or a dishwasher after each use.
 That way, if there's yeast on the bottle nipple or pacifier, your baby won't be reinfected. Store milk and prepared bottles in the refrigerator to prevent yeast from growing.
That way, if there's yeast on the bottle nipple or pacifier, your baby won't be reinfected. Store milk and prepared bottles in the refrigerator to prevent yeast from growing. - If you breastfeed and your nipples are red and sore, you might have a yeast infection on your nipples, which you and your baby can pass back and forth. Talk to your doctor, who might recommend using an antifungal ointment on your nipples while your baby is treated with the antifungal solution.
To prevent diaper rash, change diapers often.
Reviewed by: Michelle P. Tellado, MD
Date reviewed: September 2019
Share:
/content/kidshealth/misc/medicalcodes/parents/articles/thrush
Thrush in a child's mouth in the language of causes - symptoms and treatment of candidiasis
Candidiasis or thrush is an infectious pathology caused by yeast-like fungi of the genus Candida albicans.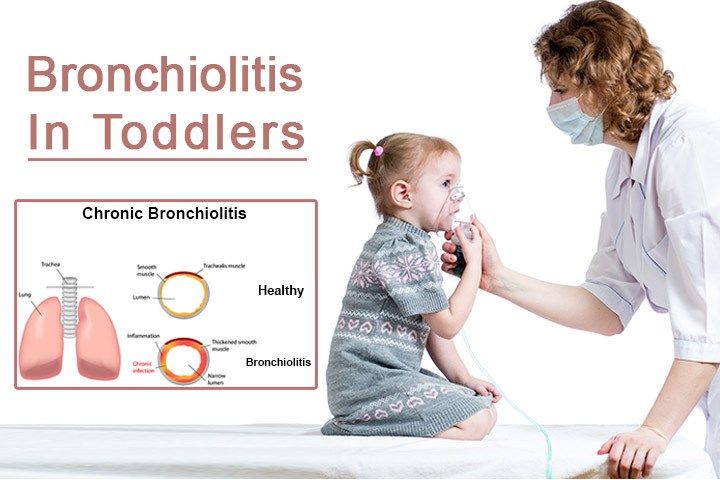 In infants, it manifests itself mainly in the form of candidal stomatitis. If a child shows signs of illness, it is necessary to visit a pediatrician. In a complicated form of the disease, a consultation with a dermatologist, ENT, urologist or gynecologist will be required.
In infants, it manifests itself mainly in the form of candidal stomatitis. If a child shows signs of illness, it is necessary to visit a pediatrician. In a complicated form of the disease, a consultation with a dermatologist, ENT, urologist or gynecologist will be required.
Causes of thrush in children
Fungi of the genus Candida belong to the opportunistic microflora of the oral cavity and small intestine. Uncontrolled reproduction of microorganisms begins with the weakening of the protective functions of the body. Pathogens damage the mucous membrane and nearby tissues.
Internal factors in the development of thrush:
- prematurity;
- artificial feeding;
- surgical interventions;
- beriberi;
- alimentary dystrophies;
- anemia;
- rickets;
- imbalance of intestinal microflora;
- thyroid dysfunction;
- SARS, HIV, chronic viral pathologies;
- violation of protein, carbohydrate, fat metabolism;
- vomiting and frequent regurgitation.
Internal factors include prematurity, formula feeding, surgery, hypo- and avitaminosis, alimentary dystrophy, anemia, rickets, disruption of normal intestinal microflora, SARS, chronic viral diseases (including HIV), protein and fat metabolism disorders and carbohydrates, endocrine pathologies (including diabetes mellitus), malignant neoplasms, frequent regurgitation and vomiting.
External factors of thrush include:
- frequent damage to mucous membranes;
- teething in a child;
- long-term use of antibacterial, hormonal or immunosuppressive drugs, cytostatics;
- non-compliance with the rules of oral care.
Candida vulvovaginitis in the mother, contact with a carrier of pathogenic strains of the fungus, and mechanical ventilation can provoke the development of thrush in a child.
Symptoms of thrush in children
The incubation period is 2–60 days, on average 3–6 days. Clinical manifestations depend on the severity of candidal stomatitis. The main symptom is a white coating on the tongue.
The main symptom is a white coating on the tongue.
Forms and characteristic signs of thrush in children:
- L Mild form - most often diagnosed in children. In the oral cavity, areas appear covered with a white coating of a curdled consistency. Localization - the inner surface of the cheeks, the upper surface of the tongue, sometimes - the soft and hard palate. Plaque is easily removed by scraping. The general well-being of the child is within the normal range, there is no specific sour smell from the mouth.
- Moderate form - the child has a dense cheesy coating on the tongue or in the form of a film. Nearby tissues are red and swollen. The plaque is hardly separated from the mucous membranes, after removal, the affected areas bleed. With this form of candidiasis in the mouth, the mood, sleep and appetite of the child worsens.
- Severe form - all mucous membranes of the oral cavity, gums, lips, posterior pharyngeal wall are affected in a child. The plaque is dense, it is practically not removed when scraped off, a light film remains under it.
 With this form of candidiasis, a pronounced sour smell from the mouth appears. The child is naughty, refuses breast or food, does not sleep well.
With this form of candidiasis, a pronounced sour smell from the mouth appears. The child is naughty, refuses breast or food, does not sleep well.
Complications in infants
In infants, thrush develops rapidly, the pathological process spreads to other parts of the body. Signs of candidiasis appear in the perineum, between the buttocks, symptoms of an intestinal fungal infection are observed. A severe form of thrush can cause sepsis.
Without proper treatment, candidiasis becomes chronic. Frequent exacerbations negatively affect the immune system and the general condition of the infant. The risk of developing allergic and atopic diseases increases. In children with chronic candidiasis, bronchial asthma is often detected.
Fungal tonsillitis is a common complication of oral candidiasis. A characteristic symptom is the appearance of a white cheesy plaque on the tonsils, burning, sore throat.
When a fungus affects the digestive tract, a child develops colic, and the process of food digestion slows down.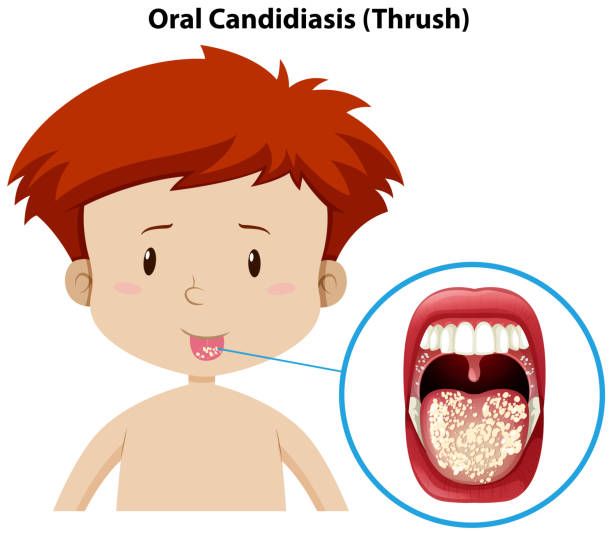 Disturbed by constipation, pain in the lower abdomen. Mycosis of the respiratory organs is accompanied by frequent bronchitis, prolonged SARS, pneumonia.
Disturbed by constipation, pain in the lower abdomen. Mycosis of the respiratory organs is accompanied by frequent bronchitis, prolonged SARS, pneumonia.
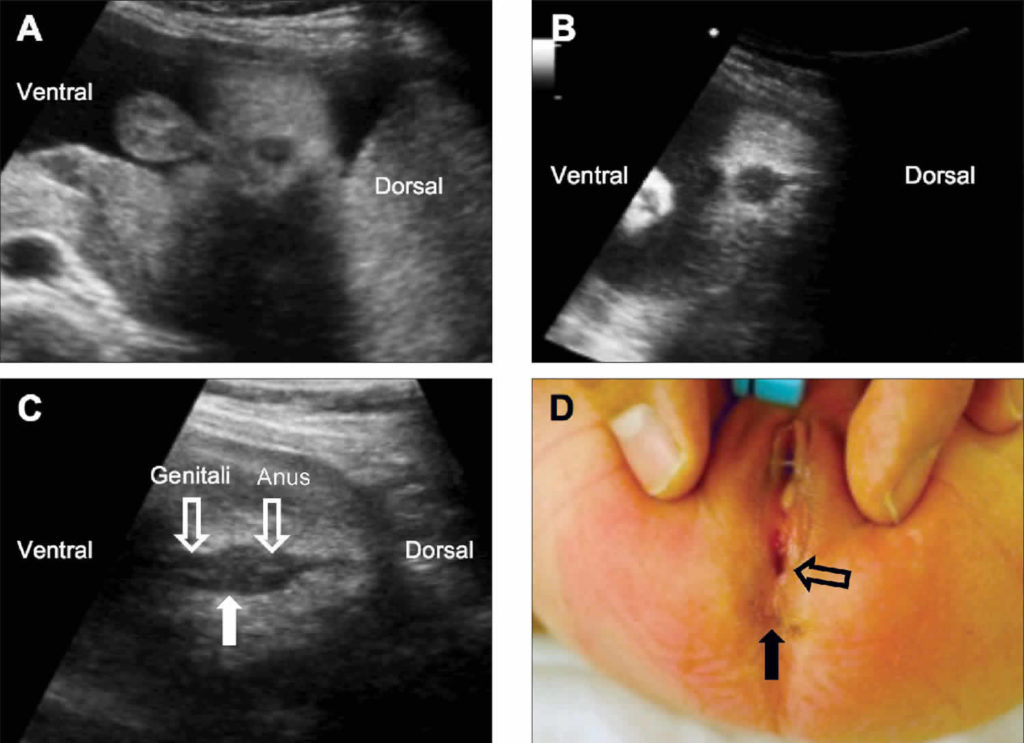
Girls with chronic oral thrush often develop vulvovaginal candidiasis. Signs - redness and swelling of the external genital organs, due to the dryness of the mucous membranes, erosions form. In infancy, due to the anatomical features of the structure of tissues, pathology can lead to fusion of the labia and vaginal walls. In such cases, long-term medical treatment and surgery will be required.
Fungal infection of the genital organs in boys is accompanied by redness of the head of the penis, a secret similar to sour cream is secreted from the urethra. Against the background of thrush, urethritis and cystitis often develop.
Diagnosis of thrush
Thrush has characteristic symptoms. Therefore, there are no diagnostic problems. When collecting an anamnesis, the doctor determines the time of the onset of the disease.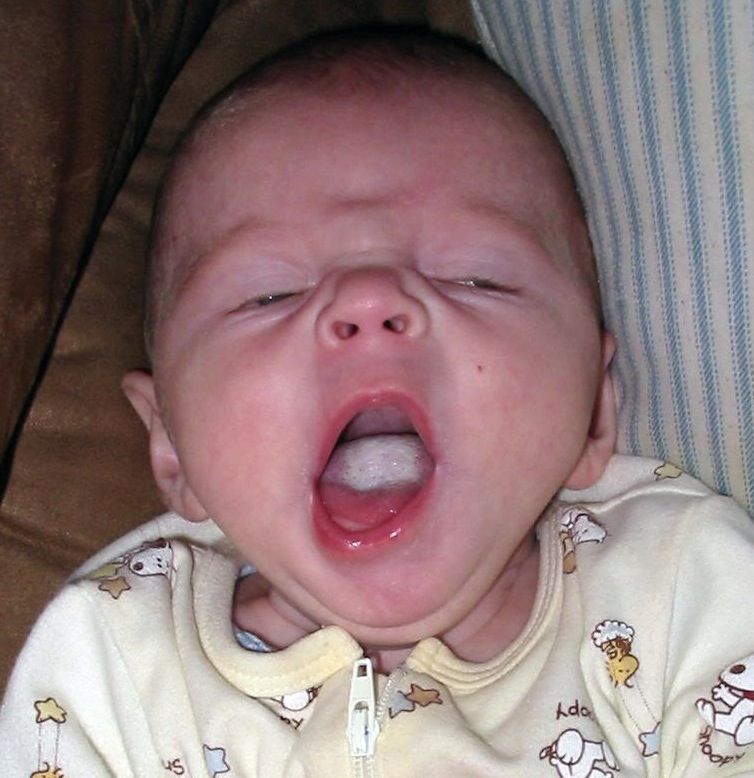 Assesses the general condition of the child, finds out the presence of fungal infections in the mother during pregnancy and childbirth.
Assesses the general condition of the child, finds out the presence of fungal infections in the mother during pregnancy and childbirth.
During a physical examination of a child, the doctor performs a number of necessary procedures:
- examines the condition of the oral mucosa;
- detects the presence of specific plaque in the mouth;
- determines the severity of the pathological process.
Be sure to check other parts of the body that may have been infected by fungus.
Laboratory methods for the diagnosis of thrush:
- Microscopy. A scraping is made from the affected area, the resulting biomaterial is studied under an electron or light microscope. The analysis reveals yeast-like cells and mycelial filaments.
- Culture method. Carried out to determine the type of pathogen, its sensitivity to antimycotic drugs.
- Serological research methods are used in the absence of clear clinical manifestations, lack of information of other diagnostic methods.
For fungal angina, sputum is analyzed to identify the type of pathogen. With candidiasis of the genital organs, it is necessary to pass a smear on the microflora. If mycosis of the internal organs is suspected, an analysis of feces, blood and urine is prescribed.
Be sure to carry out differential diagnosis to exclude diphtheria, acute herpetic stomatitis, acute tonsillitis.
Treatment of thrush
The choice of drugs for the treatment of thrush depends on the severity of the pathological process.
Peculiarities of therapy:
- In case of mild form, the oral cavity is irrigated with antifungal solutions with clotrimazole, nystatin. Soda or boric solution removes plaque well. Apply local disinfectants and antiseptics - methylene blue, Lugol's solution, Miramistin. When breastfeeding, the mother must treat the breast with a solution of soda, a decoction of calendula or oak bark before each feeding. The average duration of treatment is 2 weeks.

- For moderate to severe disease, oral or parenteral antifungals are prescribed. Additionally, symptomatic treatment of concomitant diseases is carried out.
Older children are given a diet. From the diet it is necessary to exclude sweet and salty dishes, flour. These products create favorable conditions for the reproduction of fungi. Additionally, it is necessary to take folic and ascorbic acid to restore the balance of microflora, drugs to strengthen the immune system.
With timely treatment, you can completely get rid of thrush in your mouth. Recovery occurs within 7-10 days. Severe forms of the disease and complications occur only in the complete absence of antifungal therapy.
Prevention of thrush in infants
Prevention of candidiasis in children is either specific or non-specific.
Non-specific methods of prevention:
- correct and regular care of the child's skin and mucous membranes;
- proper and rational nutrition of the mother during breastfeeding;
- with artificial feeding, choose high-quality mixtures with probiotics and vitamins;
- rational use of antibiotics during pregnancy;
- timely treatment of fungal infections during childbearing;
- do not give sweets to a child under one year, older children - sugar and sweets in limited quantities;
- strengthen immunity - hardening, exercise, long walks in the fresh air, adherence to the daily routine.

Specific prophylaxis is necessary in case of burdened gynecological and obstetric anamnesis. These are prematurity, intrauterine malformations, birth injuries, disorders in the work of the respiratory and central nervous systems. Newborns who are at risk, within a week after birth, undergo microscopy and bacteriological analysis of scrapings from the mucous membranes, analysis of feces. If it is necessary to take antibiotics, a prophylactic course of taking antimycotic agents is prescribed.
Oral candidiasis is a dangerous disease for children. Do not self-medicate, postpone a visit to the doctor. Call the clinic, the administrator will select a convenient time for a visit to the therapist. With frequent recurrences of thrush, consult an immunologist.
Thrush in infants. What is Thrush in Infants?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests.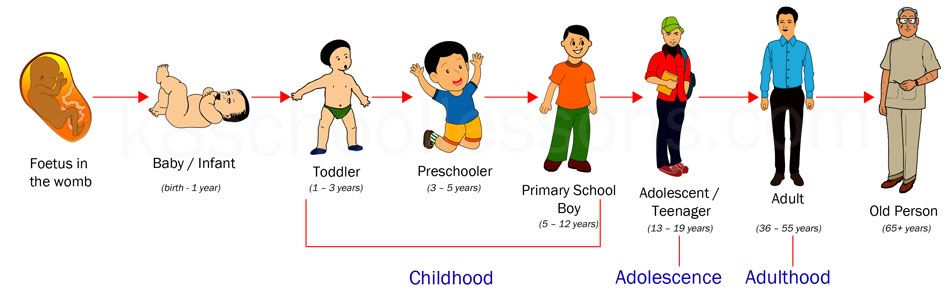 For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor.
Thrush is one of the clinical variations of fungal diseases caused by yeast-like fungi from the genus Candida. In infants, the most common oral form is candidal stomatitis. Clinical manifestations include a white cheesy coating on the mucous membranes of the cheeks, tongue and palate. In severe cases, the entire oral cavity is affected, the general condition of the child is disturbed. Diagnosis involves the identification of specific symptoms during examination, confirmation of the diagnosis by microscopic, bacteriological and cultural methods. Treatment is carried out with the help of local and systemic application of antimycotic drugs.
- Causes of thrush in infants
- Symptoms of thrush in infants
- Complications of thrush in infants
- Diagnosis of thrush in infants
- Treatment of thrush in infants
- Prognosis and prevention of thrush in infants
- Prices for treatment
General
Candidiasis or thrush in infants is a fungal pathology that is caused by opportunistic or pathogenic strains of fungi of the genus Candida.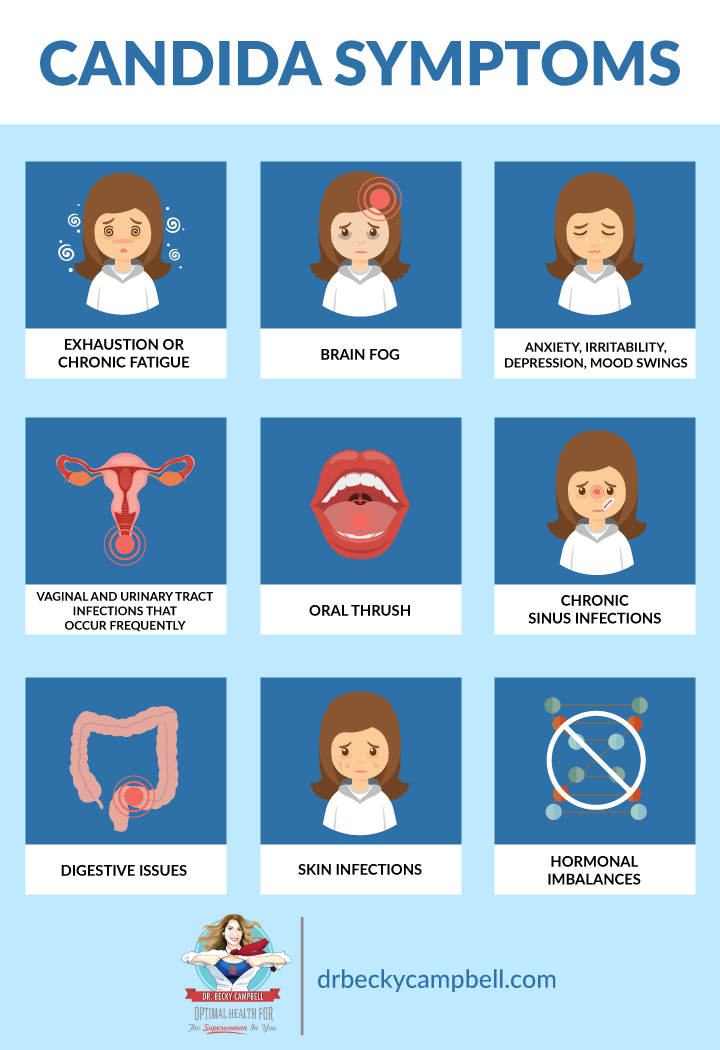 At 80-90% of her cases are caused by C. albicans. For newborns and infants, oral candidiasis is most common. Candidiasis stomatitis was first described by Hippocrates around 400 BC. The pathology got the name "thrush" because of the white plaque on the mucous membranes, which looks like curdled milk, and also because of the curdled discharge. The incidence depends on a decrease in immunity against the background of underlying pathologies or external circumstances: candidiasis develops in 20-25% of children with type I diabetes, in 25-30% of oncological patients and in 70-90% of babies with AIDS.
At 80-90% of her cases are caused by C. albicans. For newborns and infants, oral candidiasis is most common. Candidiasis stomatitis was first described by Hippocrates around 400 BC. The pathology got the name "thrush" because of the white plaque on the mucous membranes, which looks like curdled milk, and also because of the curdled discharge. The incidence depends on a decrease in immunity against the background of underlying pathologies or external circumstances: candidiasis develops in 20-25% of children with type I diabetes, in 25-30% of oncological patients and in 70-90% of babies with AIDS.
Thrush in infants
Causes of thrush in infants
The cause of thrush in infants, as in adults, are fungi from the genus Candida. Most often, C. albicans acts as the causative agent, less often - C. tropicalis, C. parapsilosis, C. glabrata, C. krusei. These yeast-like fungi are included in the list of opportunistic agents, since they are contained in the normal microflora of the oral cavity and small intestine. With the full functioning of the immune system, they do not have a negative effect. Against the background of a decrease in the body's resistance, fungi begin to grow and multiply rapidly, damaging the mucous membrane and underlying tissues.
With the full functioning of the immune system, they do not have a negative effect. Against the background of a decrease in the body's resistance, fungi begin to grow and multiply rapidly, damaging the mucous membrane and underlying tissues.
Many exogenous and endogenous factors can contribute to the development of thrush in infants. Internal factors include prematurity, formula feeding, surgeries, hypo- and beriberi, alimentary dystrophy, anemia, rickets, disruption of normal intestinal microflora, SARS, chronic viral diseases (including HIV), metabolic disorders of proteins, fats and carbohydrates , endocrine pathologies (including diabetes mellitus), malignant neoplasms, frequent regurgitation and vomiting. External factors provoking the development of candidiasis are chemical or physical damage to the mucous membrane, prolonged antibiotic therapy, taking immunosuppressive drugs, hormonal drugs and cytostatics, vulvovaginal candidiasis during pregnancy and / or childbirth in the mother, contact with patients with candidiasis or carriers of pathogenic strains, IVL and being in the conditions of the RIT department.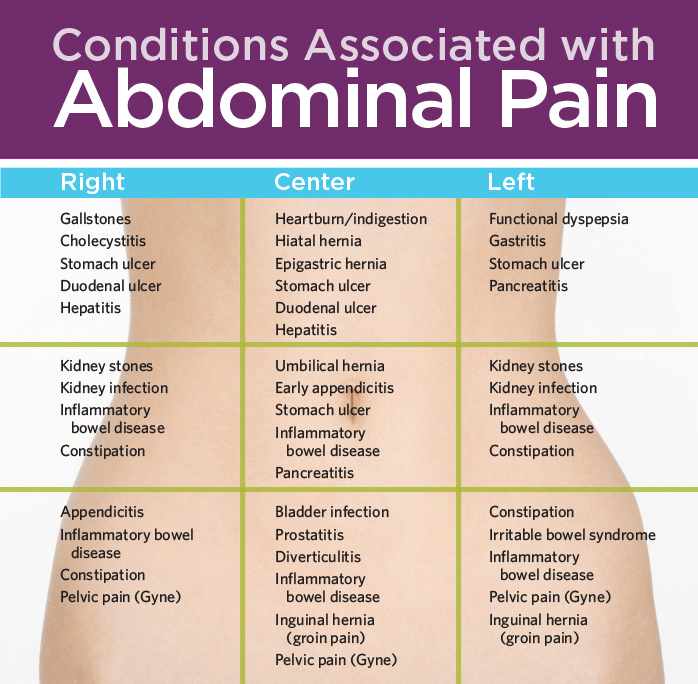
Symptoms of thrush in infants
The incubation period for thrush in infants ranges from 2 days to 2 months, with an average of 3-6 days. The clinical picture depends on the severity of the lesion. There are mild, moderate and severe forms of candidal stomatitis. The mild form is the most common. It is characterized by damage to the oral cavity in the form of foci of curdled plaque. The most common localization is the inner surface of the cheeks, the upper part of the tongue, less often the hard and soft palate. Formations are effortlessly separated by scraping. The general condition of the child is not disturbed, there is no discomfort, no specific smell is observed.
Moderate and severe forms of thrush in infants are less common, since they develop only in the absence of regular preventive examinations by a pediatrician or a conscious refusal of parents to treat. Candidiasis stomatitis of moderate severity is manifested by a cheesy or film-like plaque, diffusely spreading over all typical lesions. Adjacent tissues are sharply hyperemic. When trying to separate plaque from the mucous membrane, only some of its parts are removed, in place of which drops of blood remain. The general condition is somewhat disturbed: restless sleep, the child is naughty.
Adjacent tissues are sharply hyperemic. When trying to separate plaque from the mucous membrane, only some of its parts are removed, in place of which drops of blood remain. The general condition is somewhat disturbed: restless sleep, the child is naughty.
In a severe form of thrush in infants, a total lesion of all mucous membranes of the oral cavity, including the posterior pharyngeal wall, gums, and lips, is revealed. The plaque is tightly soldered to the underlying tissues, therefore, when scraping, it is possible to separate only small areas, under which a whitish film remains. On examination, a strong unpleasant odor is detected from the mouth. The general condition of the child is sharply disturbed: he is restless, sleeps badly, often cries, refuses his mother's breast.
Complications of thrush in infants
In children, unlike adults, there is a tendency to the rapid development and spread of pathological processes. Because of this, candidal stomatitis is often accompanied by damage to other parts of the body - candidiasis of the perineum, intestines, intergluteal and inguinal-femoral folds, candidal vulvovaginitis occur. In severe forms of thrush in infants, hematogenous and lymphogenous dissemination of fungi often occurs - sepsis develops. Ineffective treatment of acute candidiasis can lead to its transition to a chronic form. In addition to constant exacerbations and violations of the general condition of the child, this condition causes a further decrease in immunity, a tendency to allergic reactions and atopic diseases, such as bronchial asthma.
In severe forms of thrush in infants, hematogenous and lymphogenous dissemination of fungi often occurs - sepsis develops. Ineffective treatment of acute candidiasis can lead to its transition to a chronic form. In addition to constant exacerbations and violations of the general condition of the child, this condition causes a further decrease in immunity, a tendency to allergic reactions and atopic diseases, such as bronchial asthma.
In girls, against the background of oral thrush, vulvovaginal candidiasis very often develops. Clinically, it is manifested by hyperemia, swelling and dryness of the external genital organs with erosions of the mucous membranes. In pediatrics and neonatology, this pathology is of great danger, since in infancy, due to the special tenderness of tissues, there is a high risk of fusion of the labia and vaginal walls with each other. Such a complication, in addition to massive pharmacotherapy, requires surgical intervention.
Diagnosis of thrush in infants
Diagnosis of thrush in infants is based on a full collection of anamnestic data, an objective and laboratory examination of the child. Instrumental studies are usually not required. When collecting an anamnesis, the pediatrician establishes the etiological and contributing factors, determines the time of the onset of the disease, and evaluates the characteristics of the child's condition. The specialist must pay attention to the fungal pathologies of the mother during pregnancy and childbirth. The physical examination includes a thorough examination of the oral cavity, identifying characteristic deposits, determining the severity of the process, and examining other parts of the body that can potentially develop candidiasis. The leading role is played by laboratory diagnostics, which consists in microscopy, bacteriological and serological examination.
Instrumental studies are usually not required. When collecting an anamnesis, the pediatrician establishes the etiological and contributing factors, determines the time of the onset of the disease, and evaluates the characteristics of the child's condition. The specialist must pay attention to the fungal pathologies of the mother during pregnancy and childbirth. The physical examination includes a thorough examination of the oral cavity, identifying characteristic deposits, determining the severity of the process, and examining other parts of the body that can potentially develop candidiasis. The leading role is played by laboratory diagnostics, which consists in microscopy, bacteriological and serological examination.
Microscopic diagnosis is the first stage at which the material obtained during scraping is examined under a light or electron microscope. It makes it possible to identify the characteristic filaments of mycelium and yeast-like cells. The cultural method allows you to determine the type of fungus and its sensitivity to specific antimycotic drugs.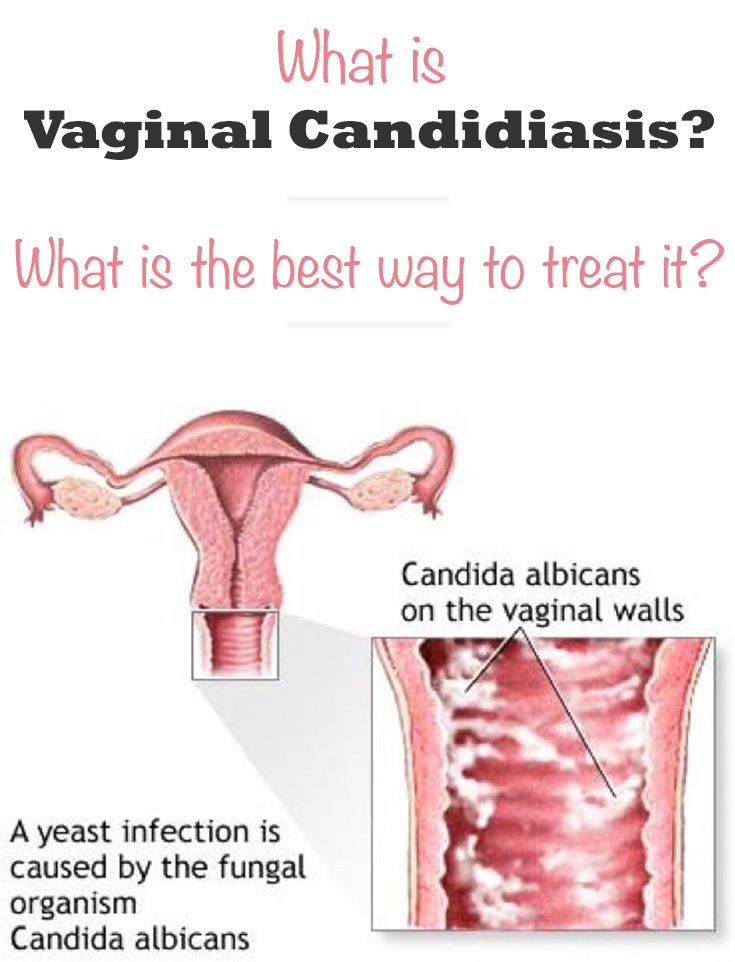 This method is also used when initial empiric treatment with common agents has failed. Serological reactions (most often RSK) are indicated in the absence of a clear clinical picture and low informativeness of other studies. Based on the above studies, differential diagnosis of candidal stomatitis with acute tonsillitis, diphtheria and acute herpetic stomatitis in children is carried out.
This method is also used when initial empiric treatment with common agents has failed. Serological reactions (most often RSK) are indicated in the absence of a clear clinical picture and low informativeness of other studies. Based on the above studies, differential diagnosis of candidal stomatitis with acute tonsillitis, diphtheria and acute herpetic stomatitis in children is carried out.
Treatment of thrush in infants
Treatment of thrush in infants depends on the prevalence of the pathological process. In the early stages, with a local lesion, local therapy is indicated - the oral cavity is irrigated with anti-candidiasis (clotrimazole, nystatin) alkalizing (2% baking soda solution, 0.25% boron solution) and disinfectant (aniline dyes - Lugol's solution, methylene blue) means. When breastfeeding, the mother's breast is treated with a 2% soda solution and herbal infusions (oak, calendula, and others). Such treatment is carried out until the complete recovery of the child, but for a period of at least 14 days.
In moderate and severe forms, systemic therapy is recommended by oral or parenteral administration of antimycotic drugs. When using anti-candidiasis drugs through the mouth, preference is given to powders for injection (fluconazole), since the prepared solution has not only a general, but also a local effect on the mucous membranes of the oral cavity. In parallel, the treatment of concomitant diseases and symptomatic therapy according to indications is carried out in full. According to current recommendations, this approach should also be used for mild forms, since it allows to reduce the treatment time to 3-6 days.
Prognosis and prevention of thrush in infants
The prognosis for thrush in infants is favorable. With timely rational therapy, complete recovery occurs within 7-10 days. Severe forms and the development of complications are observed only against the background of the complete absence of antifungal treatment. Nonspecific prevention of candidal stomatitis consists in the full care of the skin and mucous membranes of the child, especially against the background of severe pathologies that reduce immunity.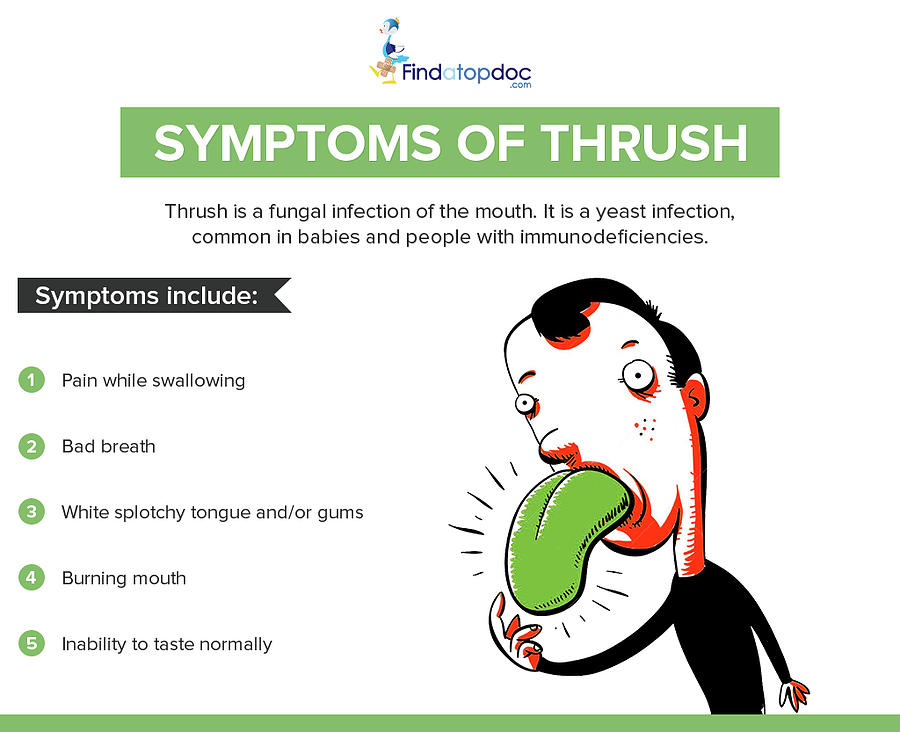 An important role is given to the rational use of antibacterial agents and the treatment of fungal diseases in the mother during the period of bearing a child.
An important role is given to the rational use of antibacterial agents and the treatment of fungal diseases in the mother during the period of bearing a child.
Specific prevention of thrush in infants is necessary if there are indications that include a burdened obstetric and gynecological history of the mother, prematurity and intrauterine malformations of the child, respiratory disorders, birth injuries of newborns, CNS pathologies. Newborns included in this group, the first 7 days of life, microscopy and bacteriology of samples of mucous membranes and feces are performed. For infants on antibiotic therapy, a prophylactic course of an antifungal drug, usually fluconazole, is given.
You can share your medical history, what helped you in the treatment of thrush in infants.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.