Swollen vulva with yeast infection
Swollen Vulva: Causes, Other Symptoms, Treatment
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Was this helpful?
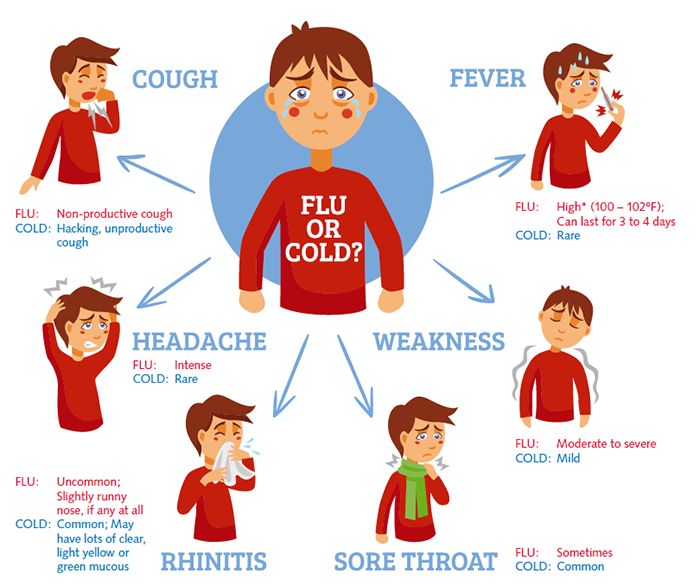
A swollen vulva is a common symptom of vaginitis, or an inflammation of the vagina. This often happens because of a bacterial, yeast, or viral infection or an imbalance in vaginal bacteria.
If you’re experiencing a swollen vulva, you could be experiencing a condition known as vaginitis. This is an inflammation of the vagina, and it can happen because several different health issues.
Vaginitis often results from a bacterial, yeast, or viral infection or an imbalance in vaginal bacteria. Certain skin disorders or low levels of estrogen can also cause the condition to occur.
When your vagina and vulva are both inflamed, it’s known as vulvovaginitis. In addition to a swollen vulva, vaginitis could lead to:
- unusual vaginal discharge
- itching
- irritation
- pain during sex
- pain while peeing
- light bleeding or spotting
If these symptoms last for more than a couple of days, see your doctor. They can figure out what’s causing your symptoms and develop a treatment plan suited to your needs.
Keep reading to learn more about what may be behind your symptoms.
An allergic reaction that causes your vulva to swell is known as noninfectious vaginitis.
This can result from chemicals in:
- clothing
- creams
- condoms
- perfumed soaps
- scented detergents
- douches
- lube
These and other products that come into contact with your vulva and vagina can cause irritation and inflammation.
What you can do
If you suspect an allergic reaction, stop using the product or wearing the item of clothing that may be causing irritation. Limiting your exposure to irritants should help ease the swelling.
You could also use an over-the-counter (OTC) cortisone cream to reduce your symptoms. If the swelling continues, you should see your doctor. They may recommend a sitz bath or a prescription topical cream for treatment.
Shop for cortisone cream.
A swollen vulva is normal after any sexual encounter. Sexual arousal causes increased blood flow to the area, causing it to swell and become puffy. Your clitoris may also enlarge.
Your clitoris may also enlarge.
Your vulva may swell if there wasn’t enough lubricant during penetration. This can irritate the area.
What you can do
Your vulva shouldn’t stay swollen for long, and you can use a cold compress to ease any swelling or puffiness.
Although swelling is a normal symptom of arousal, you can take some proactive measures to avoid serious swelling. Be sure to keep natural or store-bought lubricant on hand to avoid friction, and stay away from products that could cause an allergic reaction.
Shop for personal lubricant.
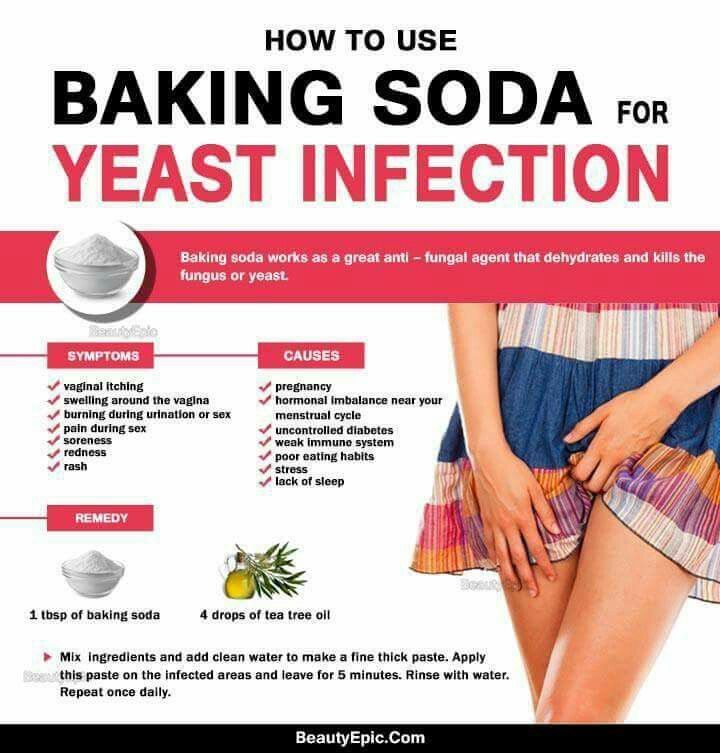
Vaginal yeast infections will affect up to 3 out of 4 women in their lifetime.
In addition to swelling, you may experience:
- irritation
- thick white discharge
- intense itchiness
- burning sensation
- pain or soreness
- rash
If your symptoms are severe, or you’ve had four or more infections in a year, you should see your doctor.
What you can do
You can use an OTC antifungal vaginal cream, ointment, or suppository to stop the reaction and alleviate the swelling.
If this is the first time you’ve had symptoms of an yeast infection — or if they don’t disappear with at-home treatment — you should make an appointment with your doctor.
Depending on your symptoms, your doctor will prescribe either a single-dose or multi-dose oral antifungal medication. They may also recommend maintenance therapy if you have recurring yeast infections.
Shop for antifungal vaginal cream.
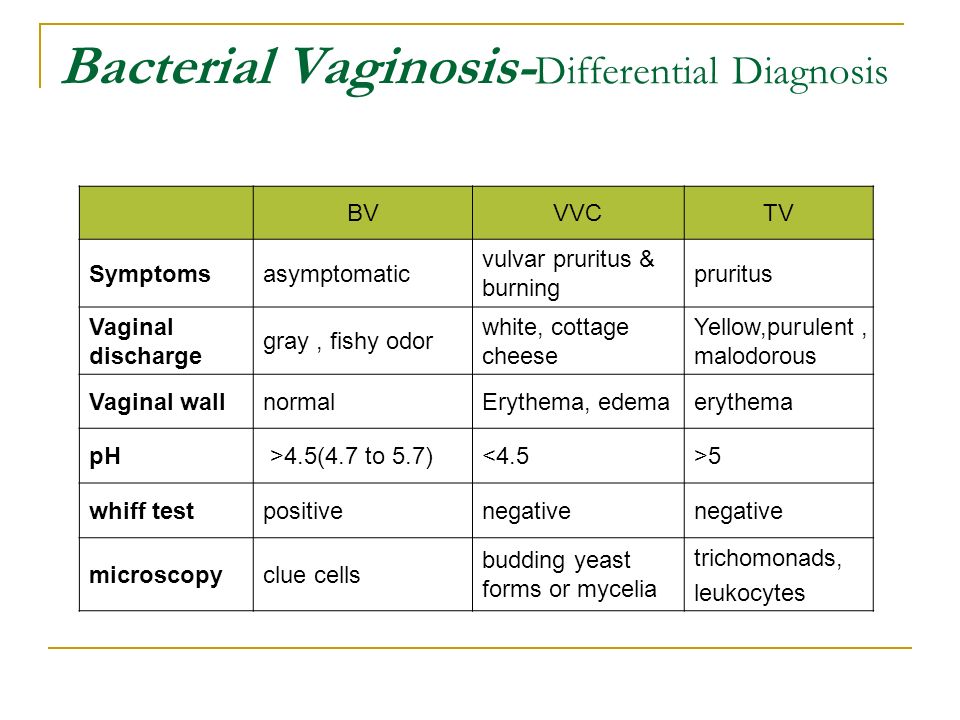
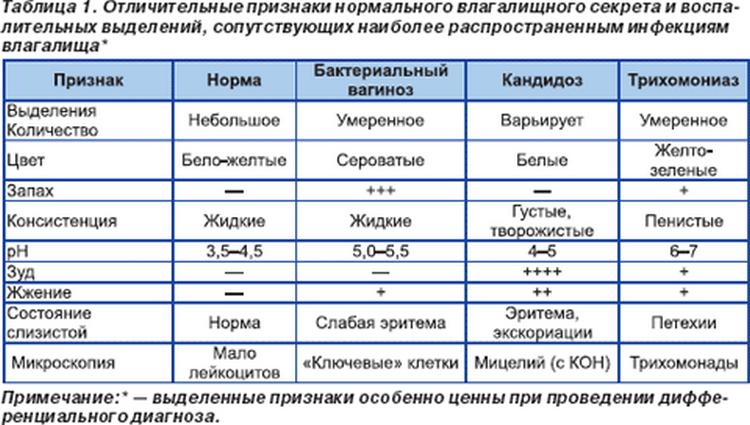
Bacterial vaginosis is the most common form of vaginitis, affecting up to a third of women in the United States. It’s caused by an imbalance in the bacteria found in your vagina, and it can lead to an off-white or gray discharge and a fishy smell. Although a swollen vulva isn’t a common symptom, it’s still possible.
What you can do
For some women, symptoms of bacterial vaginosis resolve on their own. You should never use OTC yeast products to treat bacterial vaginosis, because it could make the infection worse.
BV symptoms do mimic other forms of vaginitis, so you should see your doctor if your symptoms persist. They can rule out any other conditions and prescribe medication to help ease your symptoms.
They can rule out any other conditions and prescribe medication to help ease your symptoms.
A swollen vulva is a common symptom of pregnancy. Your growing uterus will block your blood flow in your pelvic region, causing your vulva and legs to swell. The swelling becomes worse as you go further along in your pregnancy.
But that’s not the only change to your vulva; because your uterus and embryo require more blood to flow in your genital area, your vulva will also change colors to a bluish tinge.
What you can do
You could try some home remedies to treat your swollen vulva. You could use a cold compress or cold water rinse to reduce swelling.
If you’re concerned about your symptoms or have any questions, make sure to bring them up to your doctor. Your doctor will be able to rule out any other underlying conditions, like cysts or bacterial vaginosis.
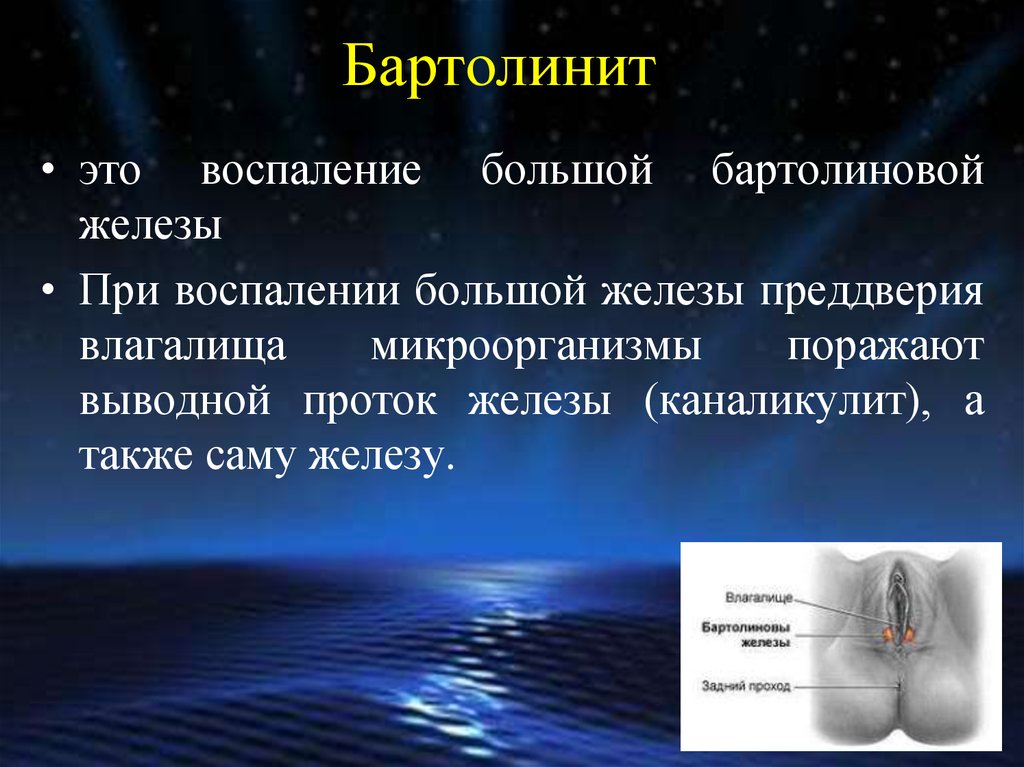
A Bartholin’s cyst is a small sac filled with fluid that appears just inside the vaginal opening. It’s soft and painless, and often doesn’t lead to any symptoms.
But if the Bartholin’s cyst grows large, it can become uncomfortable and lead to pain in your vulva when you have sex, walk, or sit down.
If your vulva is swollen, red, tender, and hot, that means the cyst has become infected and has caused an abscess in one of the Bartholin’s glands. These are pea-sized glands found on the left and right side of the vaginal opening.
What you can do
You should see your doctor right away if your vulva has become:
- swollen
- red
- hot
- tender
Your doctor may perform a swab test or biopsy to see if the cyst is infected and to rule out Bartholin’s gland cancer, a rare form of vulvar cancer.
After making a diagnosis, your doctor may recommend soaking in some warm water several times a day for up to four days, or holding a warm compress against the area to reduce the cyst and any swelling.
If you have an abscess, your doctor may prescribe antibiotics to kill the infection, and then drain the cyst.
Genital Crohn’s disease is the skin condition caused by granulomas developed from Crohn’s disease, an inflammatory bowel disease. It’s a rare disease that can cause persistent swelling of the vulva, in addition to cracks, erosions, and hollow cavities in the genital area.
What you can do
You should see your doctor if your vulva is swollen for more than a few days. They may prescribe a topical steroid or calcineurin inhibitor to help reduce any swelling. Your doctor may also recommend antiseptic cleansers to treat secondary infection or skin fissures.
You can ease — and even prevent — a swollen vulva by following these tips and tricks.
You can
- Practice good hygiene. Avoiding baths, hot tubs, and whirlpool spas will reduce exposure to bacteria and fungi. Also, make sure to wipe from front to back after going to the bathroom to prevent the spread of fecal bacteria to your vagina.
- Don’t use products that can cause irritation.
 Avoid harsh soaps, scented tampons, pads, douches, and scented soaps. Also, to prevent irritation, make sure to rinse soap thoroughly from your genitals after a shower and dry the area well.
Avoid harsh soaps, scented tampons, pads, douches, and scented soaps. Also, to prevent irritation, make sure to rinse soap thoroughly from your genitals after a shower and dry the area well. - Don’t douche. When you douche, you’re wiping out the good bacteria in your vagina. This allows the bad bacteria to overgrow and leads to vaginitis.
- Wear cotton underwear. Cotton underwear allows your genital area to breathe and will prevent yeast from growing.
- Always use a latex condom. Wearing a condom will prevent sexual infections from spreading.
Was this helpful?
You don’t have to wait for pain or discomfort to see your doctor. If your vulva is swollen for more than a few days, you should make a doctor’s appointment. But if you’re experiencing intense pain or discomfort, seek immediate medical attention. Your doctor will be able to diagnose the underlying condition causing your vulva to swell, and recommend the appropriate treatment option.
Vaginal swelling: 14 causes and treatment
Vaginal swelling can be uncomfortable. Possible causes include pregnancy, an infection, an allergy, or physical irritation.
People with vaginal swelling often assume they have a yeast infection, but this is just one of many possibilities. Vaginal swelling can be caused by allergies, sexually transmitted infections (STIs), cysts, or rough intercourse. Treatment will depend on the cause.
Anyone who experiences vaginal swelling should look for signs of infection and consult a doctor for a diagnosis and treatment.
Here are 14 possible causes of vaginal swelling, along with possible treatment options.
1. Allergy
Share on PinterestAn allergic reaction to certain substances may cause the vagina to swell.An allergic reaction may cause the vagina to swell. The vagina is a sensitive part of the body and may react to any number of ingredients found in personal care products such as:
- soaps
- lubricants
- vaginal washes and douches
- tampons and pads
- vaginal contraceptives
- body lotions and creams
- latex condoms
Swelling may appear in response to a new product, but a product the body is familiar with can also cause an allergic reaction.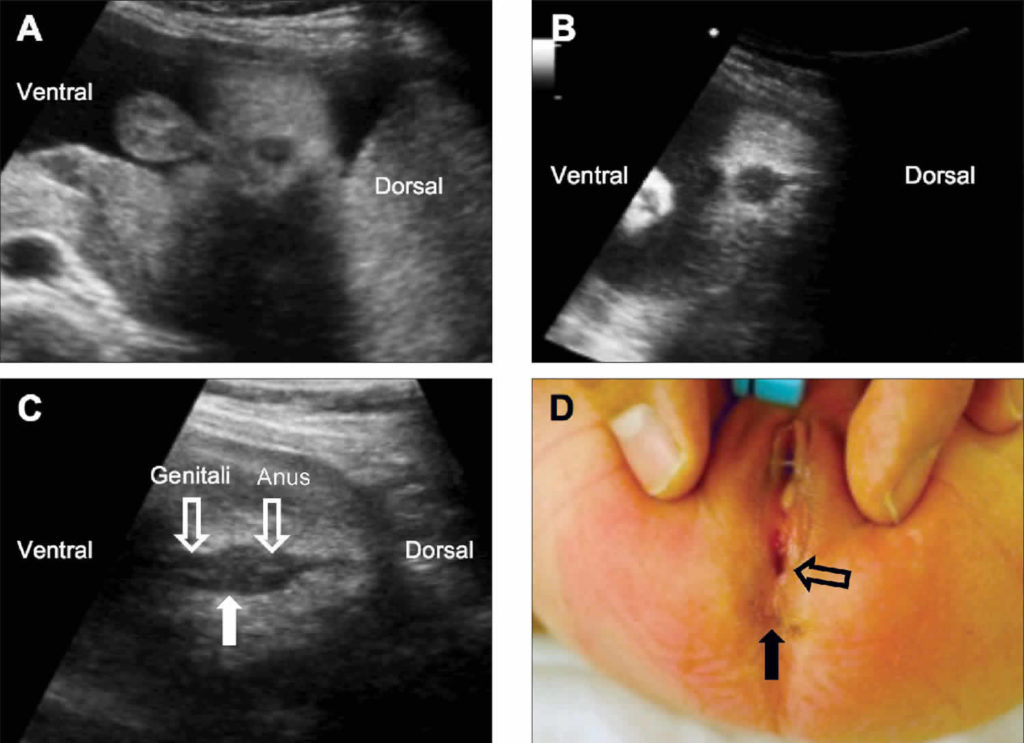 If a person suspects that they are allergic to a particular product, it may be a good idea to stop using it and consult a dermatologist.
If a person suspects that they are allergic to a particular product, it may be a good idea to stop using it and consult a dermatologist.
2. Irritation
Even if an allergy is not present, the body may react adversely when it comes into contact with specific products. Even the most popular and most widely used chemical ingredients may cause vaginal swelling.
Chemical fragrances are often to blame. They can be found in many products that come into contact with the vagina, including:
- laundry detergent
- perfumes
- toilet paper
- body washes
- bath bombs and soaps
Some types of cloth may also cause vaginal irritation and swelling. Lace or polyester underwear, in particular, may irritate the skin.
Sometimes, the cut of underwear is responsible for the swelling. Thin thongs or G-strings may not cover the labia entirely, which may cause unnecessary friction in the area throughout the day that can lead to swelling.
It is important to identify and avoid irritants. If a person stops using a specific product and the swelling goes down, they may have found the culprit.
If a person stops using a specific product and the swelling goes down, they may have found the culprit.
Anyone unable to identify the cause of vaginal swelling should visit a doctor or dermatologist.
3. Rough intercourse
Sexual intercourse can cause the vagina to swell. If the vagina is not sufficiently lubricated, added friction may lead to discomfort or pain during sex, and swelling of the vagina after sex.
Rough intercourse can also tear vaginal tissues, putting a person at higher risk of infection.
If a person suspects that rough intercourse has caused vaginal swelling, they may want to spend more time engaging in foreplay or use a lubricant to reduce friction.
An over-the-counter pain reliever or nonsteroidal anti-inflammatory drug (NSAID) may help if the swelling is causing pain. Pain relievers, such as ibuprofen, are available for purchase online.
4. Gartner’s duct cysts
A duct that forms in fetuses when the urinary and sexual organs are developing usually disappears after birth.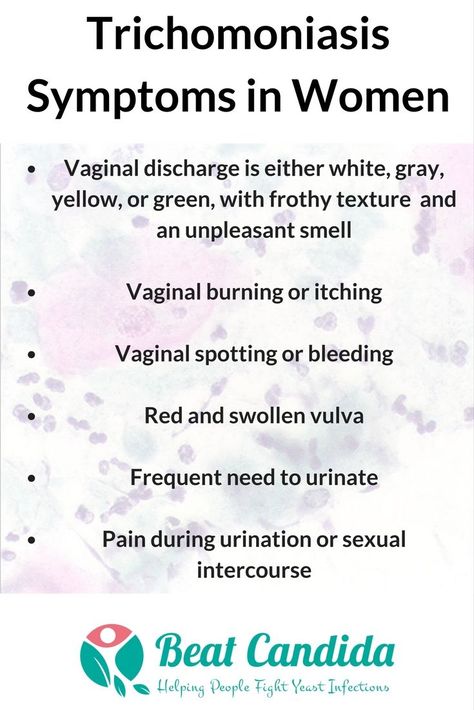 If part of this duct remains, it is known as a Gartner’s duct. The remaining tissue may attach to the vaginal wall and develop into a cyst.
If part of this duct remains, it is known as a Gartner’s duct. The remaining tissue may attach to the vaginal wall and develop into a cyst.
Gartner’s duct cysts tend to be harmless, but they can become problematic when they grow. A Gartner’s duct cyst may become infected or cause pain and swelling in the vagina.
In some cases, the cyst will appear as a growth on the outside of the vagina.
Surgery is often necessary to remove a troublesome Gartner’s duct cyst. Once the cyst is gone, symptoms should diminish.
5. Bartholin’s cysts
The Bartholin glands are on either side of the vaginal opening. They secrete moisture and help to provide lubrication.
A cyst on one of these glands may go unnoticed until it becomes infected, at which point an abscess may form. Also, the skin around the vagina may become inflamed and painful. In some cases, there may be a burning sensation or bleeding.
If the cyst or abscess is small, it may drain on its own. A warm, shallow bath may help to ease the pain, and over-the-counter medications can reduce pain and swelling.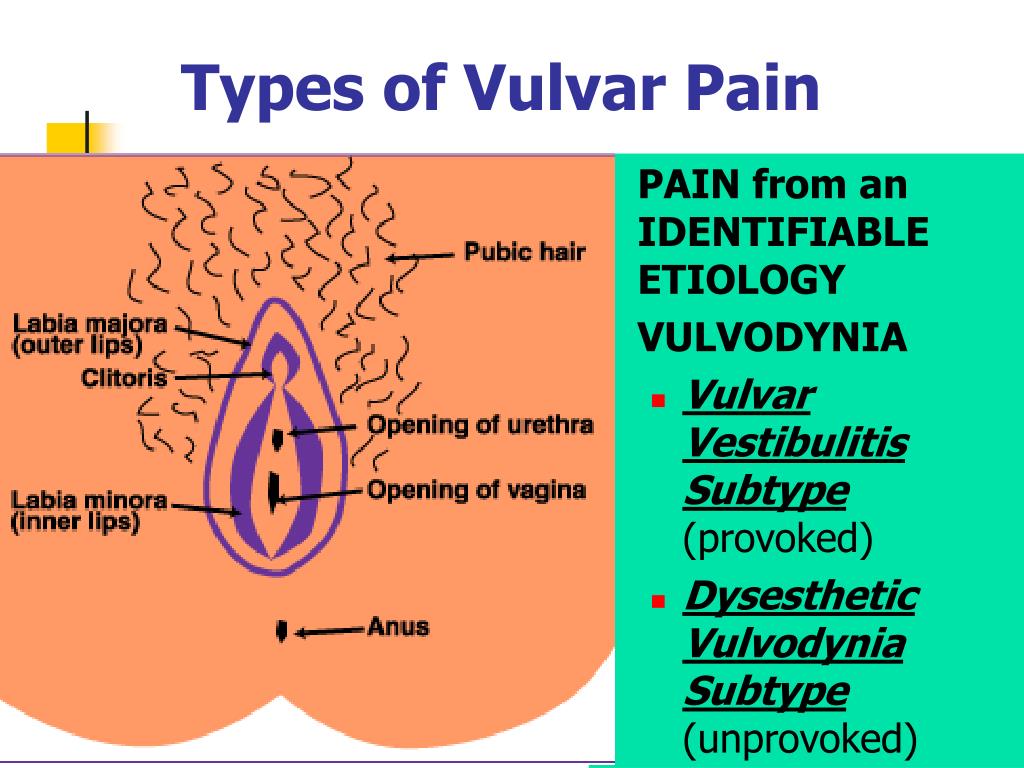
In more severe cases, a doctor may recommend antibiotics, surgical drainage, or removal of the cyst.
6. Cellulitis
Cellulitis is a bacterial infection of the inner layers of the skin that may cause the skin to become swollen, red, and tender. A person can develop cellulitis when the bacteria enter a cut, such as one sustained when shaving the pubic area.
Cleaning a cut regularly may help to combat infection. In some cases, a doctor will recommend antibiotics.
7. Bacterial vaginosis
Share on PinterestAntibiotics are usually prescribed to treat bacterial vaginosis.An overgrowth of harmful bacteria in the vagina may lead to vaginosis. Symptoms may include swelling and a grayish discharge with a foul smell.
Many cases resolve on their own, but a doctor may recommend antibiotics to speed up recovery.
Cleaning the vaginal area regularly and avoiding potential irritants can help to prevent bacterial vaginosis.
It may also be a good idea to avoid products such as douches, which disrupt the bacterial balance in the vagina.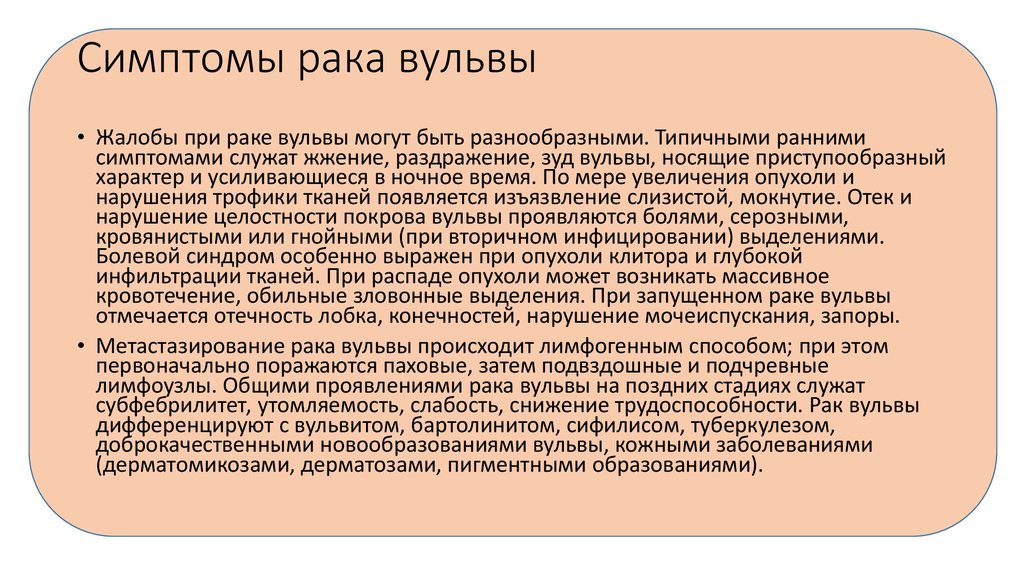
8. Yeast infection
A yeast infection is caused by an overgrowth of the Candida fungal species. It can cause vaginal swelling, and other symptoms may include:
- burning
- pain during sex and urination
- redness
- thick, chunky discharge
- irritated skin
Yeast infections are treated with antifungal medications. However, it is a good idea to see a doctor for a diagnosis because other conditions have similar symptoms.
9. STIs and cervicitis
Some of these infections can cause inflammation of the cervix, which is called cervicitis. Symptoms of cervicitis can include pain during intercourse, bleeding between periods, and abnormal discharge.
Below are some STIs that can cause vaginal swelling.
- Chlamydia: This can seriously damage a woman’s reproductive system and may also lead to painful urination and unusual discharge.
- Gonorrhea: Symptoms in women are often mild and are easily confused with those of an infection in the urinary tract or bladder.
 Other symptoms include bleeding between periods and increased discharge.
Other symptoms include bleeding between periods and increased discharge. - Trichomoniasis: This is caused by a parasite and may have no symptoms. When they appear, symptoms can include itching, soreness, pain while urinating, and changes in discharge.
Anyone who suspects that they have an STI should see a doctor.
10. Genital herpes
The herpes simplex virus often causes clusters of tiny, painful blisters to appear near the vagina. These can burst and become painful sores.
While some people notice no symptoms, others find that swelling, pain, and body aches accompany these sores.
There is currently no cure for genital herpes, but prescription medication may shorten or prevent outbreaks.
11. Edema
The term edema describes a collection of water or fluid in the body. Edema in the vagina is usually caused by lymph nodes or veins failing to drain.
Conditions that enlarge the uterus or put pressure on the veins in the pelvis, such as uterine fibroids or pregnancy, can cause edema to form.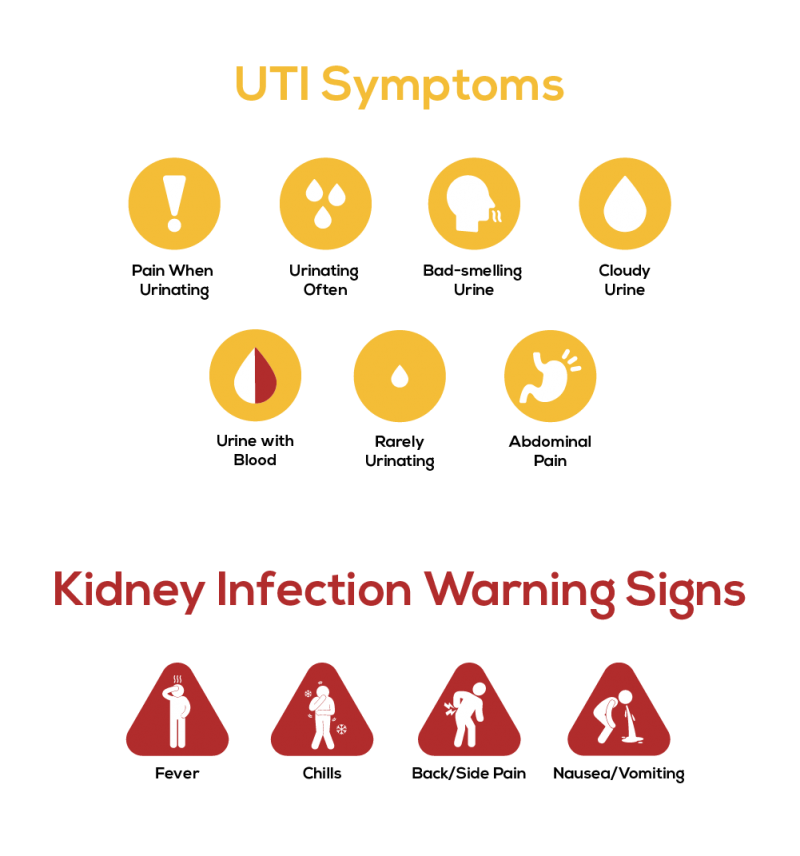
A doctor has to identify the cause of the edema to treat it. Gently massaging the area may help to reduce swelling in some cases, but this should be done under the guidance of a doctor.
12. Pregnancy
Share on PinterestA developing fetus may put pressure on blood vessels and muscles, leading to vaginal swelling.Pregnancy may also cause the vagina to swell.
As the fetus grows, it can place pressure on the pelvis and nearby muscles and blood vessels.
This pressure can cause inflammation and affect the return of blood and fluid from the lymphatic system, which may lead to swelling.
If a person suspects they are pregnant, they can take a pregnancy test. Pregnancy tests are available for purchase over the counter or online.
Anyone experiencing uncomfortable vaginal swelling during pregnancy should consult a doctor about safe medications.
13. Sexual assault
Injury from rape or sexual assault may also cause vaginal swelling and bleeding, as well as pelvic pain.
Resources are available for people who have been forced into sexual activity. Organizations like the Rape, Abuse, & Incest National Network (RAINN) in the United States offer free, confidential support. The organization’s 24-hour hotline also connects callers with local services that can help. The number for the RAINN hotline is 800-656-HOPE (4673).
People who have experienced rape or sexual abuse should consider visiting a doctor to discuss options and receive any necessary treatment.
14. Foreign objects in the vagina
When the body tries to expel a foreign object lodged in the vagina, symptoms may include:
- pain
- swelling
- itching
- irritation
- fever
- foul discharge
In some cases, a doctor may need to remove a foreign object.
Regularly cleaning the vagina may prevent objects from becoming stuck in it.
Swelling of the vagina is usually not the result of a severe medical condition. Anyone uncertain of the cause should visit a doctor.
Seek a professional diagnosis if the following symptoms are present:
- signs of infection, such as fever or chills
- painful or unbearable symptoms
- persistent symptoms
Anyone who suspects that they have an STI should see a doctor.
To discover the cause of vaginal swelling, a doctor may perform a physical exam or a blood test. Many medications are available to treat vaginal swelling, and most incidences can be treated quickly and effectively.
Read the article in Spanish
Vulvovaginal candidiasis | Dikul Center
Vulvovaginal candidiasis is a fungal infection that causes irritation, discharge, and severe itching in the vagina and vulva, the tissues at the entrance to the vagina.
Vaginal yeast infection develops in up to 70% of women during their lifetime, and many of these episodes may occur several times.
Vaginal candidiasis is not a sexually transmitted infection. But the first regular sex life significantly increases the risk of developing candidiasis. Also, candidiasis can be associated with oral-genital sex.
Also, candidiasis can be associated with oral-genital sex.
Vaginal yeast infections respond well to treatment. In the presence of recurrent yeast infection - four or more times during the year - the patient may need long-term maintenance therapy.
Symptoms
Symptoms of candidiasis can range from mild to moderate and include:
- Feelings of itching and irritation in the vagina and vulva
- Burning sensation when urinating or during intercourse.
- Redness and swelling of the vulva
- Vaginal pain and tenderness
- Vaginal rash
- Odourless thick white cheesy vaginal discharge.
- Watery vaginal discharge
Complicated candidiasis
A woman may have a yeast infection if:
- There are severe symptoms such as extensive redness, swelling, and itching that are complicated by tears, cracks, or sores.
- If yeast infection develops more than four times a year
- Infection due to an atypical fungus
- Pregnancy
- Uncontrolled diabetes
- Weakening of the immune system due to the use of certain medications or the presence of serious diseases such as HIV infection.
When to see a doctor?
You need to make an appointment with a doctor if:
- Symptoms of a yeast infection appear for the first time
- It is doubtful that this is a fungal infection
- Symptoms do not improve after taking over-the-counter antifungal vaginal creams or suppositories.
- Other symptoms appear
Causes
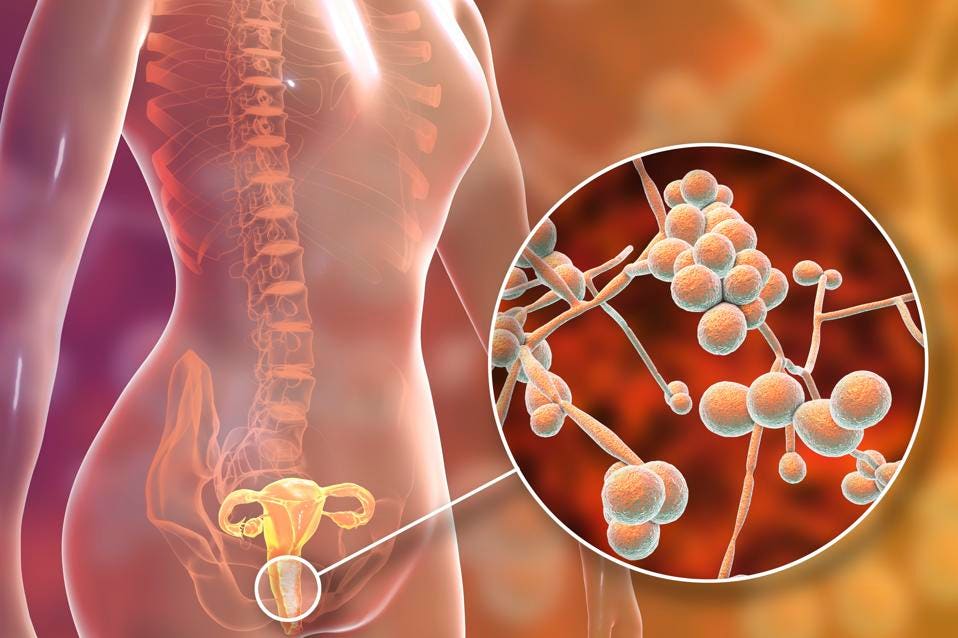
Candida albicans is the main cause of most vaginal yeast infections.
The vagina is known to naturally contain a balanced mixture of yeast, including Candida, and bacteria. Some bacteria (lactobacilli) prevent yeast from growing.
But this balance can be upset. Overgrowth of fungi or their penetration into the deeper layers of the mucous tissue of the vagina can lead to the development of symptoms of a yeast infection.
Yeast overgrowth can be caused by:
- The use of antibiotics, which can upset the balance of the natural vaginal flora
- Pregnancy
- Uncontrolled diabetes
- Immune system disorders
- Taking contraceptives or hormone therapy, which can increase the level of estrogen in the blood.
Candida albicans is the most common type of fungus that causes yeast infections. Yeast infections caused by other types of Candida are much more difficult to treat and usually require more aggressive treatments.
Risk factors
Factors that increase the risk of fungal infection include:
- Taking antibiotics. A yeast infection is not uncommon in women who take antibiotics. Broad-spectrum antibiotics kill not only a number of bacteria, but also the normal microflora in the vagina, which can cause yeast overgrowth.
- Increased estrogen levels contribute to the development of yeast infections. This can be both pregnant women and women who use high-dose estrogen birth control pills or if estrogen hormone therapy is being performed.
- Uncontrolled diabetes. Women with poor control and high blood sugar levels are more at risk of developing fungal infections than women who control their blood sugar levels.
- Immune system disorders.
Women who are immunosuppressed, such as after corticosteroid therapy or HIV infection, are more at risk of yeast infections.
Prevention
To reduce the risk of vaginal yeast infections, it is recommended to wear underwear that is not too tight with a cotton gusset.
Also recommended:
- Do not use tight fitting tights
- Douche as this flushes out some of the normal bacteria in the vagina that protect against infection.
- Use scented products for women frequently, such as bubble baths, pads, and tampons.
- Very hot and whirlpool baths are not recommended
- Do not take antibiotics unnecessarily, such as for colds or other viral infections.
- Avoid prolonged exposure to wet clothing such as swimwear and sportswear.
Diagnosis
To diagnose thrush, the doctor can:
- Ask questions about symptoms and medical history. It is important for the physician to collect information about past vaginal or sexually transmitted infections.
- Perform a gynecological examination. The doctor will examine the external genitalia to look for signs of a fungal infection. Then the doctor will examine the vagina and cervix using a special speculum.
- Collect vaginal secretions. The doctor may send a sample of vaginal fluid for analysis to determine the type of fungus that caused the yeast infection. Identifying the fungus can help your doctor decide on the appropriate treatment, especially if you have recurrent yeast infections.
Treatment
Treatment for yeast infections depends on the severity and frequency of infections.
For mild to moderate symptoms and infrequent episodes, your doctor may recommend:
- Short-term vaginal therapy. Taking antifungal medications for three to seven days usually clears up the yeast infection. Antifungal drugs, in the form of creams, ointments, tablets and suppositories, include miconazole (monistat 3) and terconazole. Some of these medicines can be purchased without a prescription, while others are available by prescription only.

- Single oral dose. Your doctor may prescribe a single oral dose of fluconazole (Diflucan). But taking such drugs is contraindicated during pregnancy. In the presence of severe symptoms, it is possible to take two single doses with an interval of three days.
Seek medical attention again if treatment does not relieve symptoms or if symptoms return within two months.
If you have severe symptoms or have frequent yeast infections, your doctor may recommend:
- Long-term vaginal therapy. Your doctor may prescribe antifungal medications taken daily for two weeks and then once a week for six months.
- Multi-dose oral preparation. Your doctor may prescribe two or three doses of an oral antifungal instead of vaginal therapy. However, this treatment is not recommended for pregnant women.
- Azol-resistant therapy. A doctor may recommend boric acid capsules to be inserted into the vagina. This medication should not be taken orally as it is toxic and is only used to treat Candida that is resistant to conventional antifungals.
- Correction of the underlying disease, such as diabetes or immunodeficiency, to avoid relapses.
Thrush in women
| Thrush or candidiasis in women - a disease caused by fungi of the genus Candida. If these microorganisms have developed on the mucous membrane of the vagina and external genital organs, then they speak of vaginal candidiasis |
This disease affects not only women of childbearing age who are sexually active, but also young girls and those who have reached respectable years. The reason is simple: candidiasis occurs not only after contact with a sick sexual partner. It can be the result of active reproduction of Candida, which used to be part of the normal microflora. With candidiasis, women complain of abundant cheesy discharge from the vagina and itching in the genital area.
Causes of thrush
Why thrush occurs is one of the most common questions women have.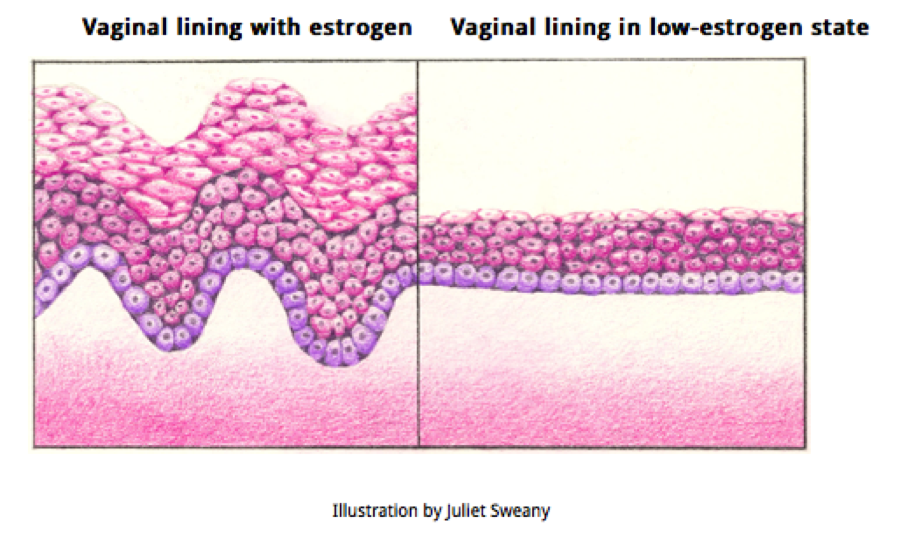 After all, this problem is very common. Unpleasant sensations arise at the most inopportune moment. This fungal disease nullifies intimate relationships and spoils everyday life.
After all, this problem is very common. Unpleasant sensations arise at the most inopportune moment. This fungal disease nullifies intimate relationships and spoils everyday life.
You can get candidiasis from a sexual partner. Especially if a man has obvious signs of this disease or he is a carrier of fungi. However, this reason is far from the most common. Much more often, thrush occurs as a result of a decrease in immunity and a violation of the natural balance of the microflora of the genital organs.
There are many factors that trigger the development of vaginal candidiasis in women.
- Reduced body defenses as a result of chronic diseases or after infections.
- Hormonal changes during pregnancy and before menstruation.
- Hormonal changes during menopause.
- Use of hormonal contraceptives .
- Long-term use of antibiotics, corticosteroids and cytotoxic drugs.
- Intestinal dysbacteriosis , where fungi can be introduced into the vagina.
- Climate change , which entails adaptation to new conditions, water composition.
- Use of intimate hygiene products : intimate gels, soaps, shower gels containing a lot of alkali and fragrances.
- Using panty liners . They violate the access of air to the genitals, increases humidity.
- Deodorized tampons and pads cause allergic reactions and mucosal damage.
- Wearing underwear made of synthetic fabrics, narrow and tight . The most common culprit for thrush is thongs.
- Food rich in confectionery and carbohydrate dishes, strong coffee, carbonated drinks, yeast baked goods, spicy and fatty delicacies, ketchup and mayonnaise.
- Avitaminosis entails a decrease in the body's resistance and a deterioration in the condition of the skin and mucous membranes.
- Obesity - in the folds of the body, favorable conditions are created for the reproduction of fungi.
- Metabolic disorders . A prime example is diabetes. It not only weakens local immunity, but also increases the amount of carbohydrates in cells, which is a good breeding ground for microorganisms.
- Smoking causes vasospasm and disrupts blood circulation, including in the genitals.
- Sexual intercourse with a dry vagina and other activities that can lead to microtrauma on the genital mucosa. Through them, Candida can penetrate deep into the tissues.
- Chronic stress , severe mental and physical stress, overwork, lack of sleep.
What are the symptoms of thrush and what are they associated with?
- Pain during intercourse. The most common reproduction of Candida begins on the mucous membrane of the vagina.
 They destroy the upper epithelial cells, gradually affecting the deeper layers. In this case, the smallest lesions resembling sores are formed. The mucous membrane of the vaginal walls becomes inflamed and painful. Therefore, during intercourse, a woman experiences pain and other unpleasant sensations.
They destroy the upper epithelial cells, gradually affecting the deeper layers. In this case, the smallest lesions resembling sores are formed. The mucous membrane of the vaginal walls becomes inflamed and painful. Therefore, during intercourse, a woman experiences pain and other unpleasant sensations. - Swelling of the genitals. Inflammation causes the walls of the vagina to swell. This is due to the fact that small vessels on the surface of the mucosa expand. In this way, the body tries to eliminate the toxins released by Candida. Blood circulation is enhanced, and the tissue of the genital organs is saturated with fluid that has escaped through the walls of the capillaries.
- White coating and cheesy discharge. Gradually, the number of fungi increases and colonies grow. They look like a whitish coating on the genitals. An inflammatory process begins, which is accompanied by abundant discharge from the vagina. They look like white curdled masses or curdled milk.
 These are mainly fungal mycelium, leukocytes and damaged mucosal cells.
These are mainly fungal mycelium, leukocytes and damaged mucosal cells. - Itching and burning. Candida feed on glycogen stores in cells. When this carbohydrate is broken down, acids are formed. Just they cause itching and burning in the vagina and irritate the skin of the genital organs damaged by Candida, while the woman feels severe discomfort. These symptoms are worse after urinating or washing. Therefore, every time the skin in this area must be dried. Preferably with soft paper towels, so as not to further injure.
- Rash with thrush. The inflammatory process in thrush also extends to the vestibule of the vagina, large and small labia. On the skin of the genital organs, the epidermis is stratified as a result of the activity of fungi, and small burgundy pimples-vesicles with liquid contents inside are formed - vesicles. After a day or two, they burst and small erosions and crusts form in their place.
- Spread to nearby skin areas.
 Signs of candidiasis: redness, small rash, itching, white plaque formation can also occur in the perineum, on the skin of the intergluteal and inguinal folds. More often this form of the disease occurs in women who are overweight.
Signs of candidiasis: redness, small rash, itching, white plaque formation can also occur in the perineum, on the skin of the intergluteal and inguinal folds. More often this form of the disease occurs in women who are overweight. - Deterioration of the general condition. Itching, constant discomfort and unpleasant sensations cause nervousness, bouts of bad mood, and sleep disturbance. The latter is due to the fact that the burning sensation intensifies at night. Unpleasant symptoms increase after a long walk and during menstruation.
- Urethritis and cystitis in thrush. Frequent urination and the appearance of pain indicates that Candida has entered the urinary system and caused urethritis and cystitis. Another sign that the inflammatory process has spread to other organs is the appearance of aching pains in the lower abdomen. In this case, an increase in temperature is possible. If you notice such symptoms, then be sure to consult a doctor and do not self-medicate.
The composition of the normal microflora of the vagina and external genitalia
The genital organs of girls begin to be colonized by microorganisms within a few hours after birth. This is the moment when the microflora begins to form. From the first day of life, various types of bacteria constantly live in the vagina and on the external genitalia. There are more than 60 of them. Usually these microorganisms do not cause disease and do not harm the body. This set varies depending on the woman's age, the phase of the menstrual cycle, pregnancy, and the presence of a permanent sexual partner. Periodically, pathogenic bacteria enter the vagina. But if their number is not large, then representatives of the microflora and immunity cells destroy these microorganisms. The vagina contains:
- lactobacilli
- bifidobacteria
- streptococci
- enterococci
- clostridia
- coagulase-negative staphylococci
- coliform bacteria
- candida
The majority of microorganisms in the body of a healthy woman are various types of lactobacilli and bifidobacteria - up to 90%. They provide an optimal level of acidity pH up to 3.8–4.5 (in adult women). If their number falls, then the vaginal environment becomes slightly alkaline and the pH exceeds 6. This leads to the multiplication of pathogenic bacteria and the development of inflammatory processes.
They provide an optimal level of acidity pH up to 3.8–4.5 (in adult women). If their number falls, then the vaginal environment becomes slightly alkaline and the pH exceeds 6. This leads to the multiplication of pathogenic bacteria and the development of inflammatory processes.
In almost 80% of cases, Candida is present in the microflora of a woman. They are represented by single inactive round cells and do not form filaments of mycelium (pseudo-mycelium).
The normal microflora in a woman's body performs important functions:
- Releases beneficial enzymes that provide the necessary acidity
- Promotes the formation of vitamins
- Supports the tension of local immunity
- Prevents the penetration of foreign bacteria that can cause disease.
The vaginal microflora has a balanced composition. At the same time, some bacteria regulate the number of others. So lactic acid bacteria produce acid, which inhibits the excessive reproduction of Candida.