Breast milk allergy rash
Is your Baby Reacting to Breastmilk?
Read time: 8 minutes
What should I know about an allergy or intolerance in my breastfed baby?Learn the difference between an allergy and a food intolerance or sensitivity
Know the signs and symptoms of food allergy or intolerance in breastfed infants
Learn which foods are the most common allergens or culprits in food intolerances
How to manage your food intake to help alleviate your baby’s symptoms
Breastmilk is incredible – it offers a complete form of nutrition for infants, and offers a range of benefits for health, growth, immunity, and development.1 The nutrients in your breastmilk come directly from what’s circulating in your blood, meaning that the nutrients and compounds you absorb from the food you eat are then passed along to your baby.
While being truly allergic or reacting to something in mom’s milk is rare in babies, a small percentage of mothers do notice a difference in their babies’ symptoms or behavior after eating certain foods.
Sometimes these terms are used interchangeably, but an allergy and an intolerance/ sensitivity are very different. According to the American Academy of Allergy Asthma and Immunology (AAAI), an allergy is when the immune system reacts to a food, whereas an intolerance happens during digestion.2
Allergies generally have more severe symptoms, often causing skin reactions or difficulty breathing. Food intolerances occur when we have difficulty digesting a food, which often result in gastro-intestinal symptoms.
With an allergy, the culprit food often needs to be taken out of the diet completely to avoid symptoms.
Food intolerances however may allow for a small amount of the offending food to be eaten without any reactions. This is the ‘threshold’ amount: the lowest amount of the food you can eat without having symptoms.
Read more: Am I Able to Reduce the Risk of Allergies for my Baby while I’m Pregnant and Breastfeeding?
Which foods might cause an allergic reaction?In general, food allergens include cow’s milk, soy, eggs, peanuts, wheat, tree nuts, fish, and shellfish. 3
In children, the most common allergens are peanuts, milk, tree nuts, and shellfish.4,5
What are the symptoms of a food allergy in babies?Food allergies affect about 7.6% of children in the United States.4
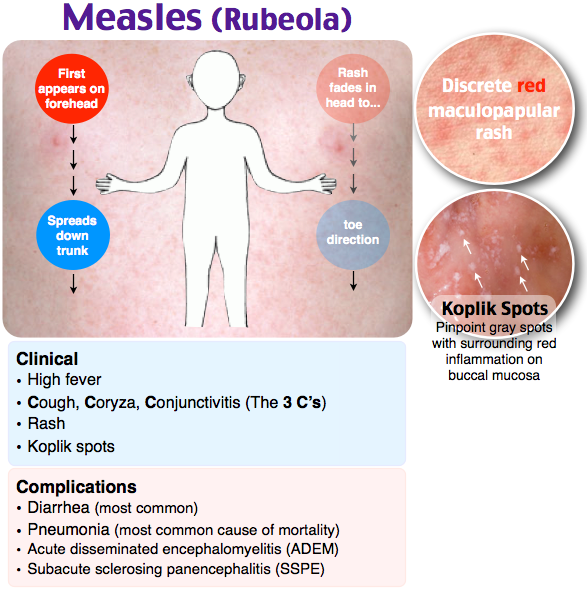
The most common symptoms of an allergy in breastfed infants are eczema (a scaly, red skin rash) and bloody stool (with no other signs of illness). You might also see hives, wheezing or other breathing problems, nasal congestion, swelling of a body part (tongue, lips, face), throat tightness, pale skin, vomiting or diarrhea.6
If you notice any of these symptoms, be sure to call baby’s pediatrician right away. While you can likely manage most food allergies in your breastfed infant by changing your diet, there are some cases in which using a hypoallergenic formula may be required.
Learn about: How Do I Manage Gas in My Breastfed Baby?
Which foods might cause a food intolerance or sensitivity reaction?You may have heard that eating foods that make you gassy will also cause gastrointestinal distress for your baby, or that eating foods like onion, garlic and cruciferous vegetables will cause colic. While there is no significant data to support such an association, there are some mothers who do notice certain foods make their babies fussier than usual. This may be a food intolerance or sensitivity.
There is a much wider variety of foods that may trigger a reaction when it comes to food intolerances; but it’s important to note that food sensitivities in babies are much less common than food allergies.
Foods that may cause reactions include: Fructose, lactose and other FODMAPs (easily fermented carbohydrates found in a variety of foods), wheat, histamine (often found in processed meats, cheeses, and some produce), and food additives. 7
The most common symptom of a food sensitivity in babies is a change in their bowel habits. Extra gas, bloating, diarrhea or constipation, fussy after eating, mucous in the stool, or crying excessively may indicated baby is not doing well with a food you’re eating.
Note that if your little one has excessive crying that continues on a daily basis and lasts for long periods, that may indicate colic rather than food sensitivity.8 Talk with your pediatrician about this possibility.
Read more: How Can I Manage My Baby's Colic?
What can I do if my baby is reacting to something in my diet?The ultimate goal is figuring out which food is affecting your baby. An elimination diet can help identify which food may be causing the allergy or food sensitivity.9 This means removing possible allergens from your diet for 2 to 3 weeks each while you continue breastfeeding.
If you plan on trying an elimination diet, especially a multi-food elimination, be sure to work with a registered dietitian nutritionist. This will help ensure you are still getting all the nutrition you and your baby need as well as help navigate hidden sources of allergens. Foods like milk, soy, and corn can hide in all sorts of pesky places.
It’s important to add a food back into your diet if no symptoms in your baby improve within a few weeks of eliminating it. If your baby’s symptoms has not improved, it is likely that the food is not the culprit.
Our Happy Baby Experts are registered dietitian nutritionists and infant feeding specialists, they can help you meet your breastfeeding goals while keeping both you and baby happy and healthy. Chat with them now!
Trying to figure out what to eat while also taking out all allergens? Here are some ideas: Meal Plan for Allergen Free Eating while Breastfeeding
Does breastfeeding help protect against allergies?While more research is needed, some studies have indicated that breastfeeding exclusively for at least four months may help to reduce the risk and severity of food allergies, even in families with a history of them. 11,12
So if your little one does show an intolerance or allergy early, know that it may resolve on its own before they turn one and that continued breastfeeding may help to safeguard against allergies later on.
What should I do if baby is reacting to my breastmilk?Contact your infant's pediatricianBring your baby in for a checkup. You’ll want to rule out any other causes for her symptoms, check baby’s growth and weight gain, and make sure baby is not losing excessive blood if your little one experiencing bloody stool. Your doctor can also discuss the possibility of confirming the presence of an allergy with a skin prick test.
If your child is diagnosed with a food allergy, remember to ask about reintroducing the food later. Most kids will grow out of food allergies, sometimes by their first birthday.
Keep a food and symptom journalWe know it’s hard to find time to eat in those first few months, let alone write down what made it into your mouth, but tracking your intake alongside your baby’s symptoms is a good way to shed light on any possible reactions.
Just remember that foods we eat may remain in our bodies for long periods of time. So while a journal can be helpful to pinpoint the onset of symptoms when you first eat the offending food, know that your baby’s symptoms can persist for several days, even if you don’t eat that particular food again.
Consider eliminating specific foodsIf you notice an adverse reaction in your baby after you eat certain foods, try removing that food from your diet and watch for improvement.
You may want to start with cow’s milk, as the most frequent allergic reaction in breastfed babies is a milk protein allergy.5 Remember, it takes time for your body to be completely free of the offending food, so make sure you’ve removed all sources of the food for at least two weeks.
Always speak with your health care provider before attempting to eliminate foods from your diet. Work closely with a registered dietitian nutritionists during this process to ensure you maintain a balanced diet and are getting all the nutrients you and your baby need.
Be sure to add foods back in when their elimination does not seem to impact your baby’s symptoms.
Seek supportChanging your diet can be hard. Finding a registered dietitian nutritionist who can help make adjustments to your diet will help take some stress out of this process. Additionally, may lactation consultants are familiar with helping make these adjustments as well and also ensuring baby is getting what they need.
Let’s Chat!We know parenting often means sleepless nights, stressful days, and countless questions and confusion, and we want to support you in your feeding journey and beyond.
Our Happy Baby Experts are a team of lactation consultants and registered dietitian nutritionist certified in infant and maternal nutrition – and they’re all moms, too, which means they’ve been there and seen that. They’re here to help on our free, live chat platform Monday through Friday, from 8am–6pm (ET). Chat Now!
Read more about the experts that help write our content!
For more on this topic, check out the following articles:How to Deal with Nursing Strikes while Breastfeeding
How much Should I Eat while Breastfeeding?
How do I Manage Gas in my Breastfeed Baby?
Which Foods Should You Avoid While Breastfeeding?
Infant Allergies and Food Sensitivities
Human breast milk typically does not cause allergic reactions in breastfeeding infants, but mothers sometimes worry that their babies may be allergic to something that they themselves are eating and passing into their breast milk. In fact, only two or three out of every one hundred babies who are exclusively breastfed demonstrate an allergic reaction—and that’s most often to the cow’s milk in their mother’s diet. In this case, the infant may show signs of severe colic, abdominal discomfort, or a skin rash such as eczema or hives, or may react with vomiting, severe diarrhea (often with blood in the stool), or difficulty breathing that lasts up to several hours after breastfeeding.
If you note any of these symptoms, contact your pediatrician right away. While rare—especially among breastfed babies—milk allergies can be severe or fatal. Most babies eventually outgrow their allergy to cow’s milk, although food allergies to other substances may be lifelong.
Breastfeeding exclusively for the first six months of life has been shown to significantly lessen the risk and severity of
food allergies in families with a strong history of them. Exclusive breastfeeding or breastfeeding in combination with partially or extensively hydrolyzed infant formula also reduces the risk for
eczema, a condition of excessively dry and easily irritated skin.
So far, there is no evidence that avoiding certain foods while breastfeeding can help prevent your child from developing allergies or asthma. The exception to that might be eczema: some studies suggest that avoiding certain foods may reduce your baby’s risk for developing eczema. Still, if your family has experienced severe food allergies, you might consider limiting your intake of milk and dairy products, fish, eggs, peanuts, and other nuts during pregnancy and while breastfeeding. Monitor your baby carefully for skin rashes, breathing problems, unusual stools, or other allergic symptoms, and be sure to tell your pediatrician about your family’s medical history.
A few mothers notice minor reactions to other foods in their diet. Some babies cry, fuss, or even nurse more often after their mother has eaten spicy or "gassy" foods (such as cabbage). These reactions differ from allergies in that they cause less-serious symptoms (no rashes or abnormal breathing) and almost always last less than twenty-four hours.
If your baby reacts negatively every time you eat a certain type of food and you find this troubling, you can just avoid that particular food temporarily. If these symptoms continue on a daily basis and last for long periods, they may indicate colic rather than food sensitivity. Talk with your pediatrician about this possibility, if eliminating various foods has no effect on your child’s symptoms.
- Last Updated
- 11/2/2009
- Source
- New Mother's Guide to Breastfeeding, 2nd Edition (Copyright © 2011 American Academy of Pediatrics)
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
causes, treatment, diet - Dobrobut Clinic
Main
Medical Library Dobrobut
Publication date: 2020-03-09
How an allergy manifests itself in infants
Allergy is a pathological reaction of the body to various substances of a foreign nature. Clinically, such reactions are expressed in the form of allergic diseases: atopic dermatitis, food allergies, urticaria, allergic rhinitis, Quincke's edema, bronchial asthma.
Allergic diseases (AD) have long turned into a "disease of civilization". The increase in the number of allergy sufferers is most noticeable among children of the first year of life. One of the causes of allergies in an infant is the early rejection of the mother's breast or the lack of breastfeeding. In this case, the baby does not receive the necessary protective elements with mother's milk. You will learn about other causes of allergic diseases, about how to treat allergies in an infant, from our article.
Causes of allergies in infants
The direct cause of allergies is the child's contact with an allergen - a foreign substrate.
One of the factors contributing to the development of allergic diseases is hereditary predisposition. If one of the parents has an allergy, then the probability of its occurrence in a child is 60-70%, if both parents are ill, then the probability of developing AZ increases to 90%. The early development of allergic diseases in children is also facilitated by the unreasonable use of antibacterial drugs, especially in the first months of life. Bad habits of the mother (alcohol, drugs, smoking) increase the risk of developing allergic diseases in the child. The question of whether the diet of a pregnant woman affects the development of AD in a child is still under discussion.
How do babies develop allergies? Its main symptoms are:
- peeling of the skin,
- various rashes,
- diaper rash,
- profuse regurgitation,
- nasal congestion,
- shortness of breath,
- loose stool.
Angioedema may also develop (very rare).
Breastfeeding allergy
Allergy to breast milk is usually associated with the diet of a breastfeeding mother. In 85% of cases, food allergens are: cow's milk, fish and seafood, eggs, wheat, soybeans, hazelnuts, peanuts, honey. At the first sign of an allergy in a baby, a nursing mother should write down the names of the foods she consumed daily to determine what the child has an allergic reaction to. The list of products must be shown to the allergist.
CMP (cow's milk protein) is usually the first complementary food protein that infants come into contact with. It can also cause allergies.
There are three groups of reactions to CMP:
- Skin rash. Swelling of the face.
- Gastrointestinal symptoms (diarrhea, vomiting).
Symptoms of atopic dermatitis may appear 1-5 days after the food test.
A well-adjusted diet for breastfeeding mothers has been shown to reduce the risk of developing allergies in babies.
Allergy Diet
Since breastfeeding allergies can be associated with errors in the nutrition of a nursing mother, it is necessary to completely eliminate foods that cause an allergic reaction in a baby from her diet.
The most common cause of allergies is:
- chicken meat,
- eggs,
- milk and dairy products,
- fish,
- seafood,
- peanuts,
- citrus fruits,
- honey,
- nuts,
- red vegetables, fruits and berries.
Allergy diet is one of the main components of AD prevention and treatment. Drug therapy for allergic diseases in an infant should be prescribed by a doctor. Read about skin care for a child with atopic dermatitis on our website Dobrobut.com.
To avoid allergic reactions in your baby, you should follow some rules:
- introduce complementary foods only after consulting a pediatrician;
- mother should try any product literally drop by drop and after feeding the child, carefully monitor the reaction of his body;
- maintain optimal temperature and humidity in the children's room;
- choose hypoallergenic baby care products;
- wash children's things with special means.
By following these recommendations, you can reduce the risk of allergic diseases in your baby.
Do you want to get an online explanation from the doctor of the Dobrobut MS?
Download our Google Play and App Store app
Our doctors
See all doctors 748
Our certificates
Certificate no. QIZ 804 468 C1
Certificate no. QIZ 804 469 C1
Certificate No. QIZ 804 470 C1
Certificate no. QIZ 804 471 C1
View all certificates
Request a call back
Enter your phone number
Other articles
Causes of tremor of the hands and other parts of the body. Signs, treatment tactics
Causes and symptoms of tremor in infants and adults. Varieties of tremor, pathologies in which it often occurs. Action tactics. How to treat essential tremor in a child.
Indications for inhalation in children. Features of the procedure
How to use inhalation for children. Features of the procedure. In what cases is inhalation given to a child and what means are used
Burning, redness, dryness - discomfort in the eyes and how to get rid of it
What does redness and dry eyes mean. In which cases we are talking about the development of inflammatory processes, and in which - about the banal irritation of the eyes. How to choose drops for redness and inflammation of the eyes.
Causes, varieties, signs, treatment of hypoplasia
Causes of underdevelopment of organs and tissues. Hypoplasia of the brain and other organs. Treatment of hypoplasia: general principles. replacement therapy.
View all articles
Request a call back
Enter your phone number
Allergy to breast milk components: problems of overdiagnosis
PUBLICATIONS
New study shows symptoms listed in international guidelines for milk allergy in primary care (iMAP) do not indicate immunoglobulin E.
(IgE)-mediated milk allergy is very common in infants.
Examples of symptoms include vomiting, regurgitation of milk, loose or more frequent stools, colic, and irritability.
Materials and methods
The study was published in the journal Clinical & Experimental Allergy.
The results come from a secondary analysis of 1,303 infants from the EAT study, a population-based, randomized controlled trial in the United Kingdom that looked at whether introducing allergenic foods to a child's diet reduces the risk of developing allergies to those foods later on.
Results
-
Nearly 3/4 (74%) of participants reported at least 2 symptoms listed in the guidelines (published in 2017 and 2019) of mild to moderate severity, and 9% reported at least 2 severe symptoms of at least within one month at the age of 3 to 12 months.
-
However, the study states that the prevalence of non-IgE-mediated CMP allergy in infants in European countries is less than 1%.
-
In the study, 25% of families reported 2 or more mild to moderate symptoms of non-IgE allergy to CMP, and 1.4% reported severe symptoms each month between 3 and 12 months of age.
-
These symptoms peaked at 38% with at least two mild to moderate symptoms and 4.3% with at least two severe symptoms at 3 months when participants did not directly consume cow's milk.
-
The researchers write that by 6 months there was no significant difference in the proportion of children with at least two symptoms between those who consumed and did not consume cow's milk.
-
The authors note that “small levels of lactoglobulin are found in breast milk; however, these amounts are below the threshold that would cause a reaction in more than 99% of infants with an IgE-mediated cow's milk allergy."
-
The authors also note that when reviewing recent recommendations for CMP allergy, "3 of 9 recommendations were directly supported by formula manufacturers or marketing consultants, and 81% of all recommendation authors reported conflicts of interest with formula manufacturers."
Conclusion
Overdiagnosis of milk allergy can lead to additional costs, unnecessary tests, and reduced breastfeeding. Cow's milk protein is usually found in standard infant formula or milk-containing products.
Misdiagnosis is likely to lead to an increase in prescription formulas that are not warranted, increased costs to patients and healthcare systems, and the use of untested allergy tests.
As far as overdiagnosis of milk allergy is concerned, reintroducing cow's milk later is one way to improve the diagnosis to see if the child has a reaction.