Shape of the uterus
Anatomy of pregnancy and birth - uterus
Anatomy of pregnancy and birth - uterus | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What does the uterus look like?
One of the most recognised changes in a pregnant woman’s body is the appearance of the ‘baby bump’, which forms to accommodate the baby growing in the uterus. The primary function of the uterus during pregnancy is to house and nurture your growing baby, so it is important to understand its structure and function, and what changes you can expect the uterus to undergo during pregnancy.
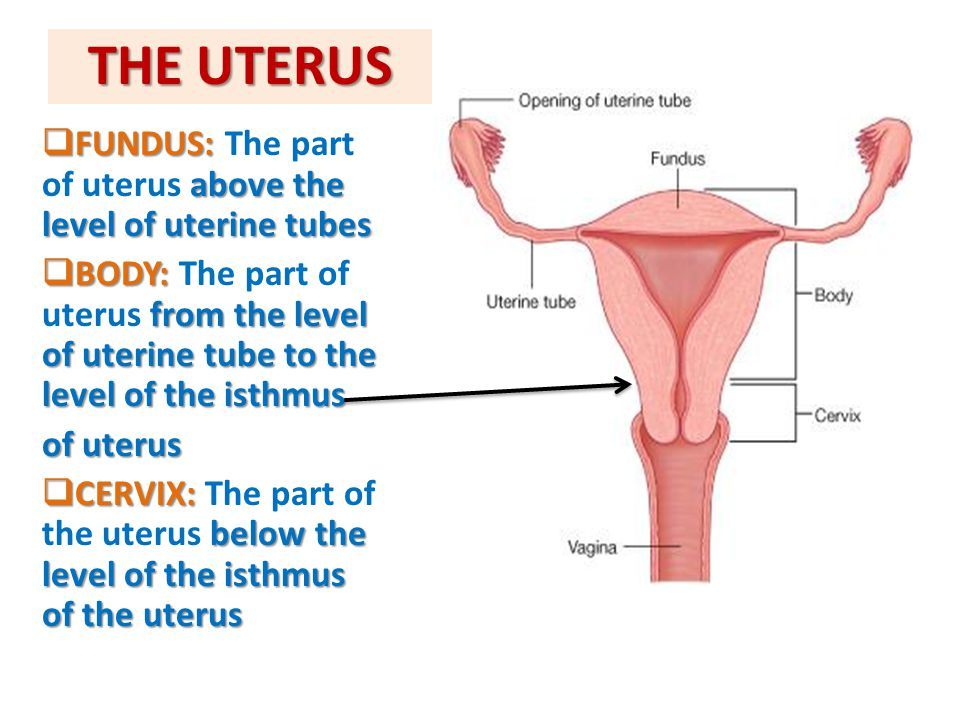
The uterus (also known as the ‘womb’) has a thick muscular wall and is pear shaped. It is made up of the fundus (at the top of the uterus), the main body (called the corpus), and the cervix (the lower part of the uterus ). Ligaments – which are tough, flexible tissue – hold it in position in the middle of the pelvis, behind the bladder, and in front of the rectum.
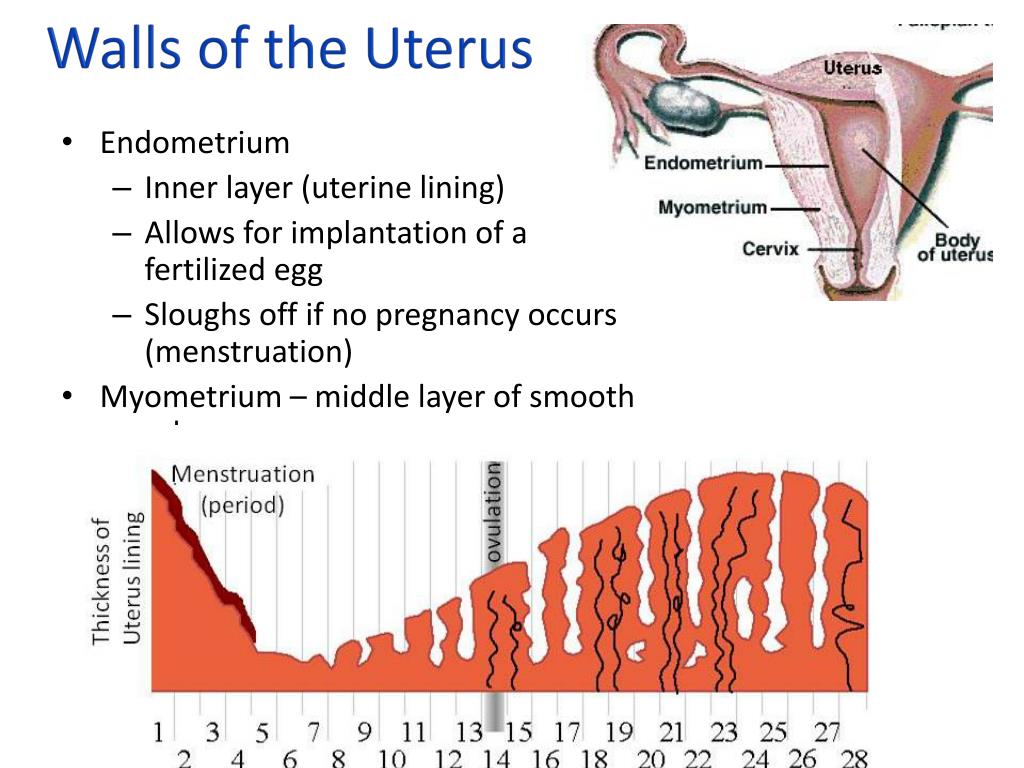
The uterus wall is made up of 3 layers. The inside is a thin layer called the endometrium, which responds to hormones – the shedding of this layer causes menstrual bleeding. The middle layer is a muscular wall. The outside layer of the uterus is a thin layer of cells.
Illustration showing the female reproductive system.The size of a non-pregnant woman's uterus can vary. In a woman who has never been pregnant, the average length of the uterus is about 7 centimetres. This increases in size to approximately 9 centimetres in a woman who is not pregnant but has been pregnant before. The size and shape of the uterus can change with the number of pregnancies and with age.
How does the uterus change during pregnancy?
During pregnancy, as the baby grows, the size of a woman’s uterus will dramatically increase. One measure to estimate growth is the fundal height, the distance from the pubic bone to the top of the uterus. Your doctor (GP) or obstetrician or midwife will measure your fundal height at each antenatal visit from 24 weeks onwards. If there are concerns about your baby’s growth, your doctor or midwife may recommend using regular ultrasound to monitor the baby.
Your doctor (GP) or obstetrician or midwife will measure your fundal height at each antenatal visit from 24 weeks onwards. If there are concerns about your baby’s growth, your doctor or midwife may recommend using regular ultrasound to monitor the baby.
Fundal height can vary from person to person, and many factors can affect the size of a pregnant woman’s uterus. For instance, the fundal height may be different in women who are carrying more than one baby, who are overweight or obese, or who have certain medical conditions. A full bladder will also affect fundal height measurement, so it’s important to empty your bladder before each measurement. A smaller than expected fundal height could be a sign that the baby is growing slowly or that there is too little amniotic fluid. If so, this will be monitored carefully by your doctor. In contrast, a larger than expected fundal height could mean that the baby is larger than average and this may also need monitoring.
As the uterus grows, it can put pressure on the other organs of the pregnant woman's body.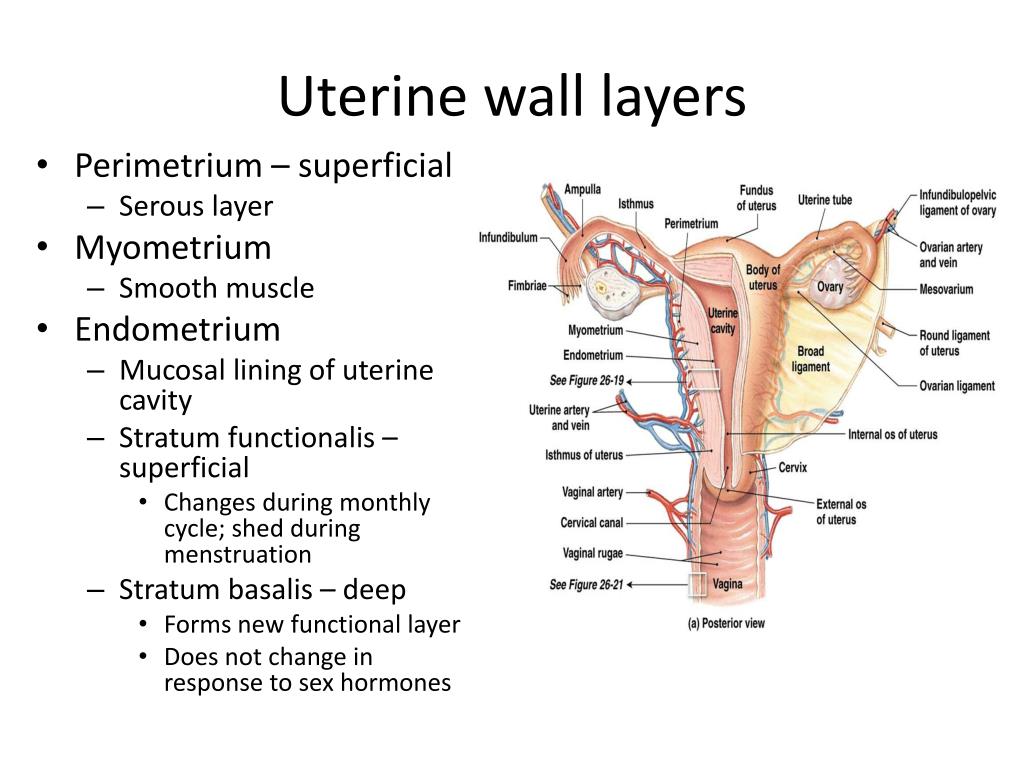 For instance, the uterus can press on the nearby bladder, increasing the need to urinate.
For instance, the uterus can press on the nearby bladder, increasing the need to urinate.
How does the uterus prepare for labour and birth?
Braxton Hicks contractions, also known as 'false labour' or 'practice contractions', prepare your uterus for the birth and may start as early as mid-way through your pregnancy, and continuing right through to the birth. Braxton Hicks contractions tend to be irregular and while they are not generally painful, they can be uncomfortable and get progressively stronger through the pregnancy.
During true labour, the muscles of the uterus contract to help your baby move down into the birth canal. Labour contractions start like a wave and build in intensity, moving from the top of the uterus right down to the cervix. Your uterus will feel tight during the contraction, but between contractions, the pain will ease off and allow you to rest before the next one builds. Unlike Braxton Hicks, labour contractions become stronger, more regular and more frequent in the lead up to the birth.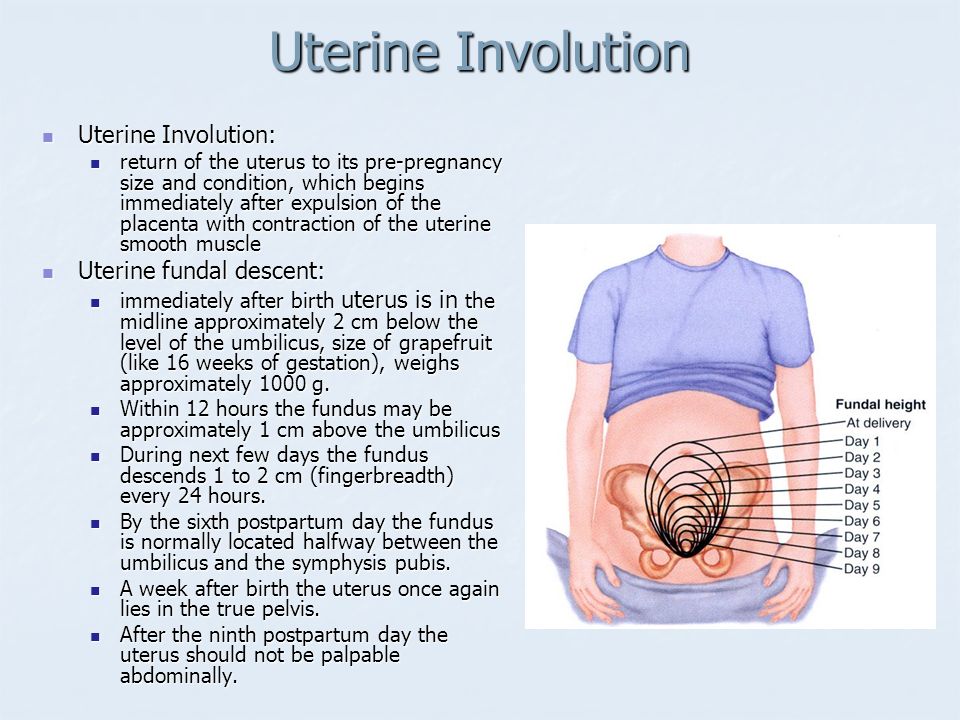
How does the uterus change after birth?
After the baby is born, the uterus will contract again to allow the placenta, which feeds the baby during pregnancy, to leave the woman’s body. This is sometimes called the ‘after birth’. These contractions are milder than the contractions felt during labour. Once the placenta is delivered, the uterus remains contracted to help prevent heavy bleeding known as ‘postpartum haemorrhage‘.
The uterus will also continue to have contractions after the birth is completed, particularly during breastfeeding. This contracting and tightening of the uterus will feel a little like period cramps and is also known as 'afterbirth pains'.
Read more here about the first few days after giving birth.
Sources:
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), StatPearls Publishing (Anatomy, Abdomen and Pelvis), Department of Health (Clinical practice guidelines: Pregnancy care), Better Health Channel Victoria (Pregnancy stages and changes), Mater Mother's Hospital (Labour and birth information), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (The First Few Weeks Following Birth), Queensland Health (Queensland Clinical Guidelines – maternity and neonatal), King Edward Memorial Hospital (Fundal height: Measuring with a tape measure), Royal Hospital for Women (Fetal growth assessment (clinical) in pregnancy), MSD Manual (Female internal genital organs)Learn more here about the development and quality assurance of healthdirect content.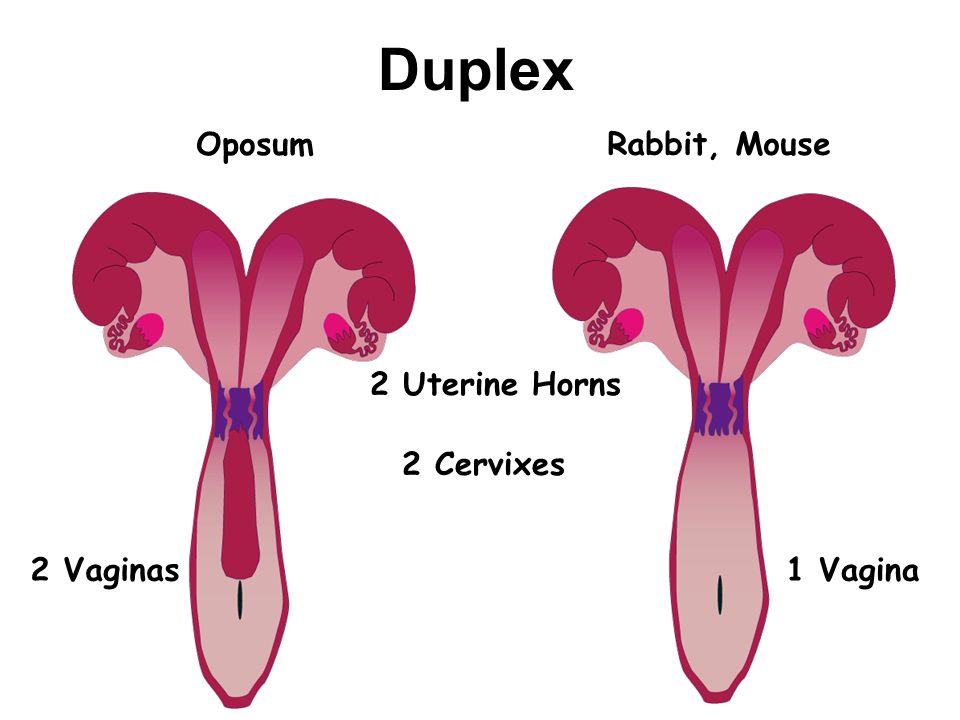
Last reviewed: October 2020
Back To Top
Related pages
- Anatomy of pregnancy and birth
- Anatomy of pregnancy and birth - abdominal muscles
- Anatomy of pregnancy and birth - cervix
- Anatomy of pregnancy and birth - pelvis
- Anatomy of pregnancy and birth - perineum and pelvic floor
Need more information?
Prolapsed uterus - Better Health Channel
The pelvic floor and associated supporting ligaments can be weakened or damaged in many ways, causing uterine prolapse.
Read more on Better Health Channel website
Uterus, cervix & ovaries - fact sheet | Jean Hailes
This fact sheet discusses some of the health conditions that may affect a woman's uterus, cervix and ovaries.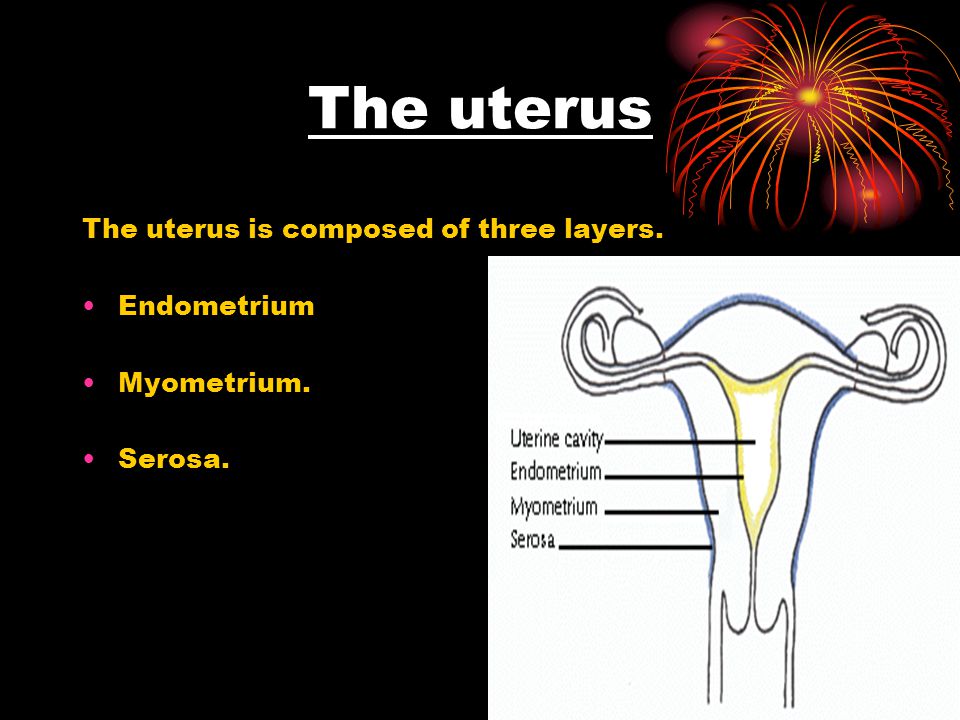
Read more on Jean Hailes for Women's Health website
Uterine differences
Some people have a uterus with a different shape. If your uterus has a different shape, you may have difficulties becoming pregnant, recurrent miscarriages or premature birth.
Read more on Pregnancy, Birth & Baby website
Dilatation and curettage (D&C)
A D&C is an operation to lightly scrape the inside of the uterus (womb).
Read more on WA Health website
Ectopic pregnancy
An ectopic pregnancy occurs when a fertilised egg implants outside the uterus (womb)
Read more on WA Health website
Hormonal IUD (intrauterine device, Mirena®) | Body Talk
The hormonal IUD is a type of contraception and is placed inside the uterus by a specially trained doctor or nurse.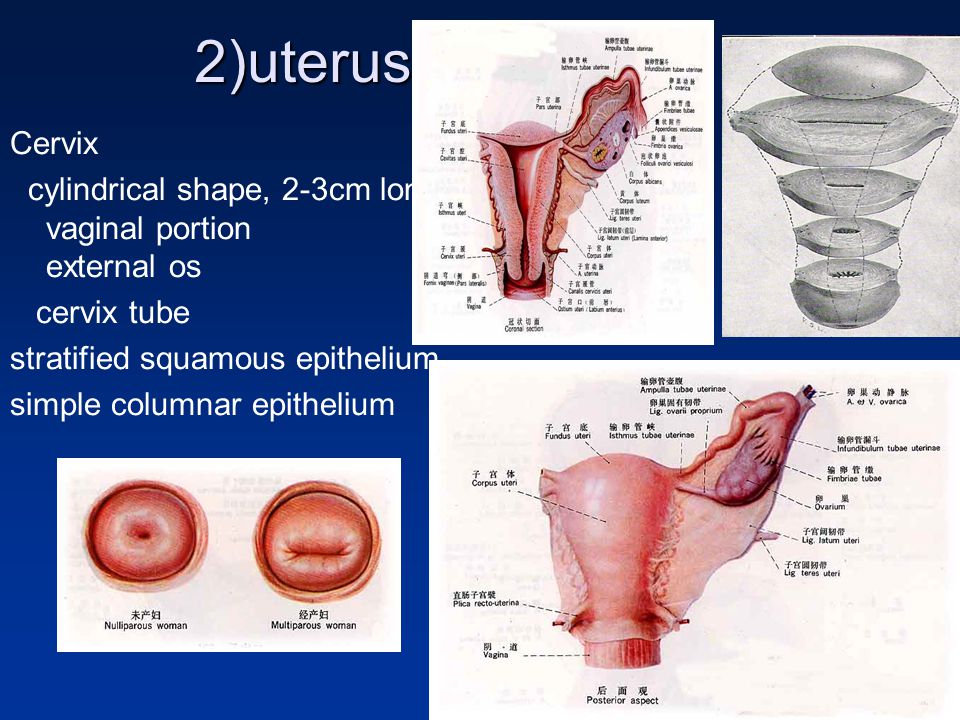 Find out all the facts here.
Find out all the facts here.
Read more on Body Talk website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
Copper IUD (intrauterine device) | Body Talk
The copper IUD is a type of contraception and is placed inside the uterus by a specially trained doctor or nurse. Find out all the facts here.
Read more on Body Talk website
Placenta previa - Better Health Channel
Placenta previa means the placenta has implanted at the bottom of the uterus, over the cervix or close by.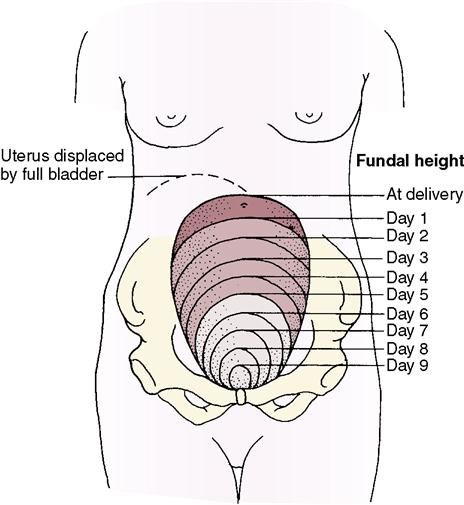
Read more on Better Health Channel website
Mirena IUD | Hormonal IUD Mirena | IUD Mirena insertion | IUD Mirena cost | Mirena IUD Melbourne - Sexual Health Victoria
The hormonal intrauterine device (IUD) is a small contraceptive device that is put into the uterus (womb) to prevent pregnancy.
Read more on Sexual Health Victoria website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.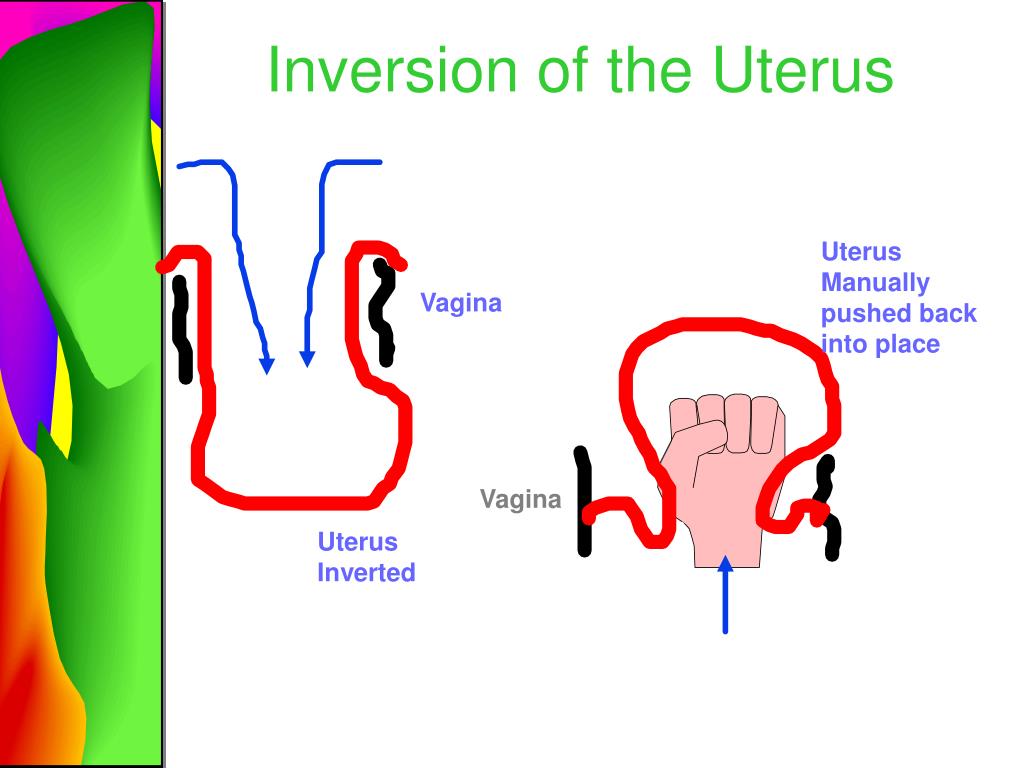
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care.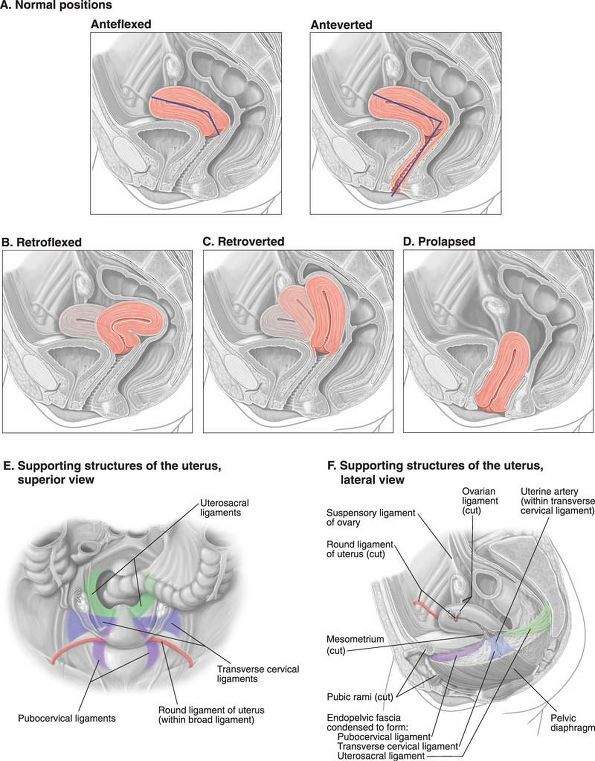 If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Abnormally Shaped Uterus | Reproductive Science Ctr.
 of New Jersey
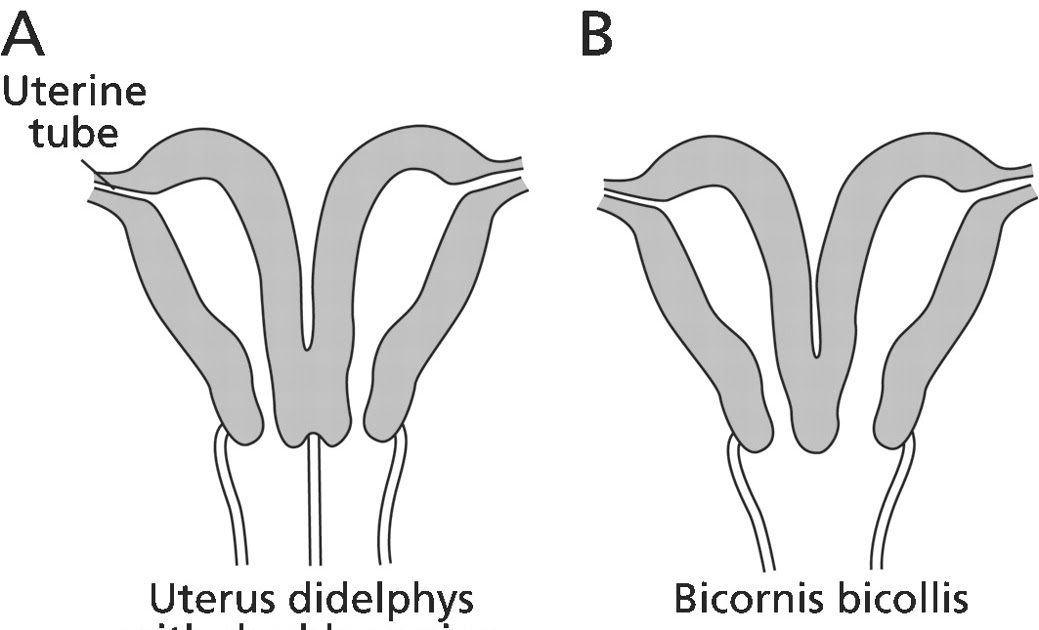
of New Jersey When a woman’s uterus, or womb, is abnormally shaped before birth (congenital), it can cause obstetric or infertility issues in her reproductive years. These abnormalities can complicate child birth and the child’s health. They can also result in irregular periods or not having any period. According to the March of Dimes, about 3 in 100 women are born with an abnormally shaped uterus.
Many times a woman only finds out about this congenital abnormality when a doctor examines her. The primary types of abnormalities in uterine shape include:
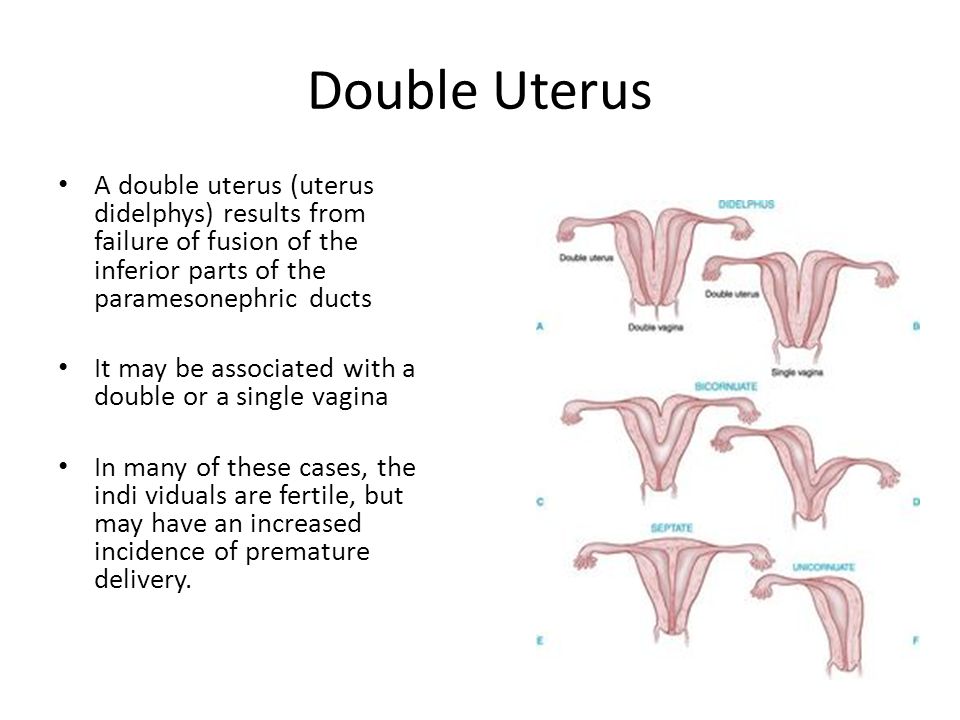
- Bicornuate uterus is partially split so that it has a heart shape. This occurs when the two tubal structures that normally join to form the womb do not unify during fetal development. Bicornuate uterus is sometimes associated with poor obstetric outcomes like miscarriage and preterm labor.
- Septate uterus occurs when the tissue of the residual septum wall is not absorbed into the single uterine cavity, as it is during the normal final stage of development.
 This results in a septum wall in the center that divides the space into two uterine cavities. This abnormality is associated with recurrent pregnancy loss.
This results in a septum wall in the center that divides the space into two uterine cavities. This abnormality is associated with recurrent pregnancy loss. - Unicornuate uterus is when only one side of the womb develops fully, usually with the cervix connected to the vagina. This cannot be corrected and can cause premature delivery and difficulties in childbirth.
- Didelphic uterus, or double uterus, is when a woman has two separate uterine cavities, each having a separate cervix. This type of abnormality has not been shown to be effectively corrected by surgical treatment.
Many women with an abnormally shaped womb do not have problems conceiving or delivering a healthy child. However, some uterine abnormalities benefit from treatment, which is usually by minimally invasive surgical correction.
Other conditions in the uterus can affect fertility, such as uterine fibroids. Sometimes surgery can result in a uterine problem as well.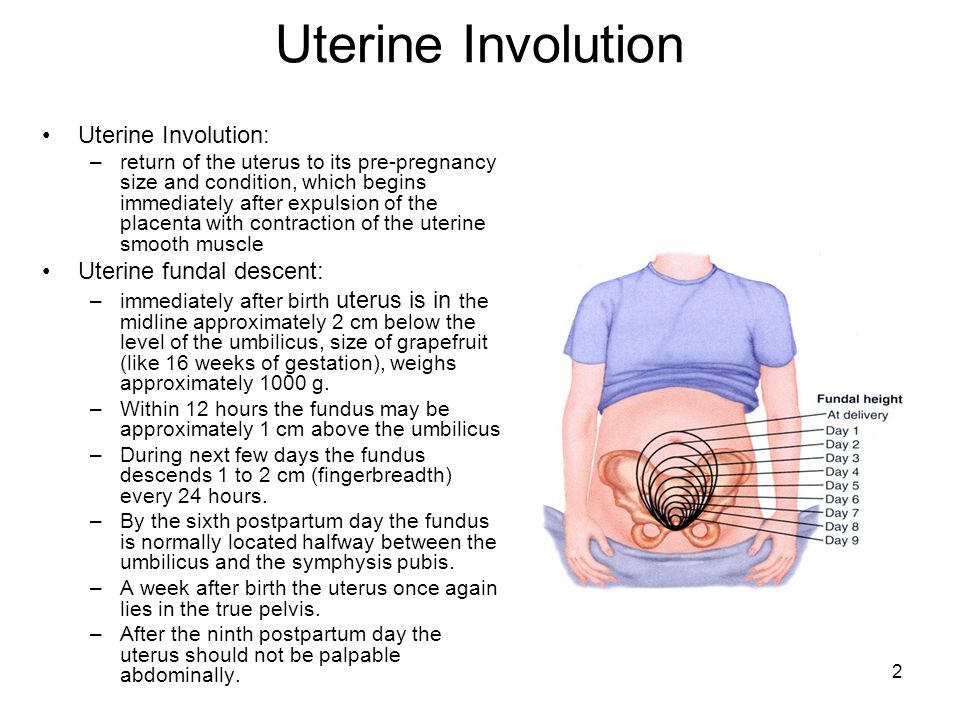 This page only deals with congenital, structural uterine problems.
This page only deals with congenital, structural uterine problems.
How the bicornuate uterus and other uterine abnormalities form
An uterine abnormality occurs when the fetus is in the mother’s womb. During development of the female fetus, the Müllerian ducts begin the formation of the female reproductive tract that includes the uterus, fallopian tubes, the cervix and the part of the vagina that connects to the cervix. Malformation during development can result in different types of abnormally shaped uteri and can similarly affect the vagina.
At about 10 weeks into a female fetus’ development, two Müllerian duct tubal structures form side by side and then unify to create the uterine cavity. At that point, there is still a section of a septum wall, which is tissue that is normally eliminated in the final stage of the womb’s development.
An obstructive abnormality can form when the uterus and the vagina have not unified together. This is called a transverse vaginal septum.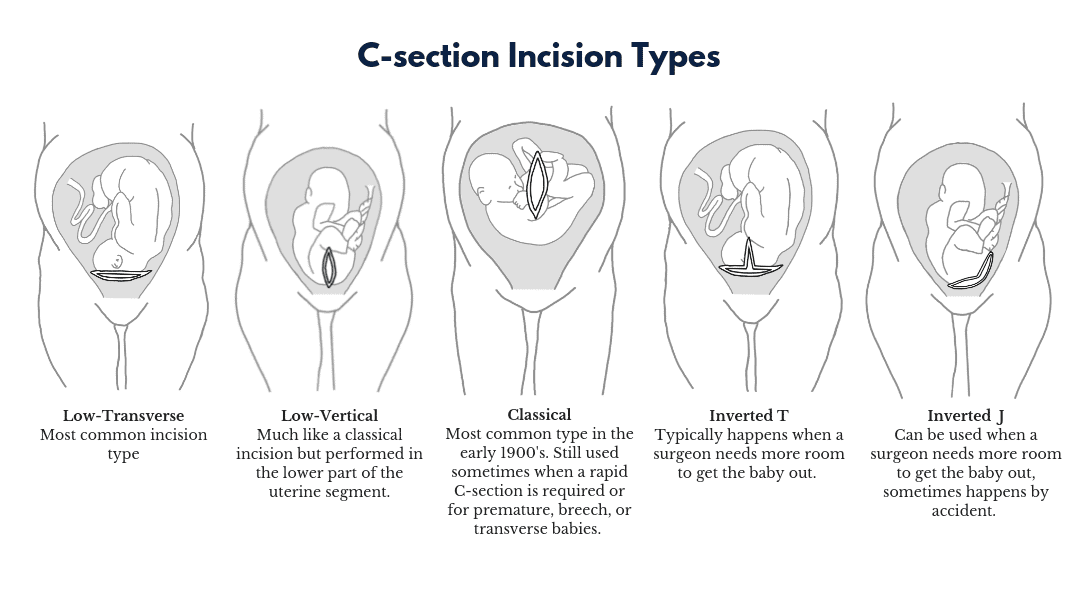 Such obstructive abnormalities cause the menstrual blood to remain in the uterus and not leave the body through the vagina. This accumulation can cause severe pelvic pain.
Such obstructive abnormalities cause the menstrual blood to remain in the uterus and not leave the body through the vagina. This accumulation can cause severe pelvic pain.
Nonobstructive abnormalities include the bicornuate, unicornuate, septate and didelphic uteri mentioned above. These do not prevent the proper outflow of menstrual blood.
Aside from infertility problems from a uterine abnormality, birthing complications and child health issues may arise. These include:
- Miscarriage.
- Breech or other baby positioning problems in the womb.
- Need for Cesarean section birth.
- Premature birth.
- Slower baby growth.
- Birth defects due to restrictions on the fetus’ growth in the womb.
Uterine abnormality symptoms & diagnosis
Most of the time, a uterine abnormality (also called a uterine anomaly or uterine defect) doesn’t cause the woman to experience any symptoms. Discovering an abnormally shaped uterus in these women generally only happens when they get a pelvic exam or ultrasound, either as a routine screening or to determine a cause for possible infertility.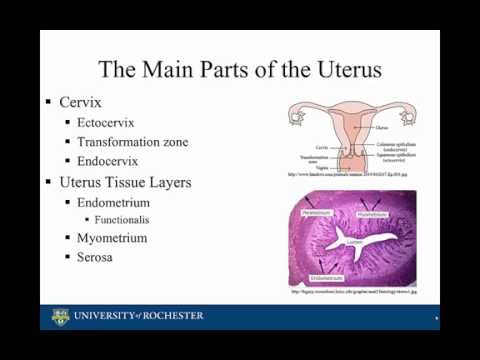
When symptoms do occur from an abnormality, they can include:
- Recurrent miscarriages.
- Not ever having a period.
- Pain: inserting a tampon, during sex, with menstruation.
- Monthly abdominal pain, in the case of an obstructive uterine abnormality.
Diagnosis & treatment
A physician will first do a physical examination, if one hasn’t already been conducted. We generally use different types of diagnostic testing to identify if a woman has an abnormally shaped uterus, what kind it is, and what is the best course of action and treatment. Sometimes we will need to conduct more than one of these tests, which include the following.
- Sonohysterogram (SIS). This involves placement of a catheter into the uterus to allow distention of the uterine cavity with saline. Then while the catheter is inside, a transvaginal ultrasound is performed to visualize the cervix, uterus and ovaries.
- Hysterosalpingogram (HSG).
 A contrast dye is injected into the cervix and uterus and X-rays are taken of those areas and the fallopian tubes. The dye results in better images of these organs. Sonohysterogram is often used to distinguish between a septate or bicornuate uterus.
A contrast dye is injected into the cervix and uterus and X-rays are taken of those areas and the fallopian tubes. The dye results in better images of these organs. Sonohysterogram is often used to distinguish between a septate or bicornuate uterus. - Laparoscopy and/or Hysteroscopy. This uses a thin tube with a camera that’s inserted through very small incisions in the woman’s abdomen or through the vagina and cervix (for the latter procedure) to view into the uterus. The images are relayed to a computer screen. If surgical correction needs to be done, it can be done at this time with special surgical instruments inserted through the tube.
- MRI. A magnetic resonance imaging (MRI) test gives us very good images of the womb and surrounding structures. It is very accurate in diagnosing most uterine abnormality issues.
If these tests result in a diagnosis of an abnormally shaped uterus, the physician will discuss next steps with the patient.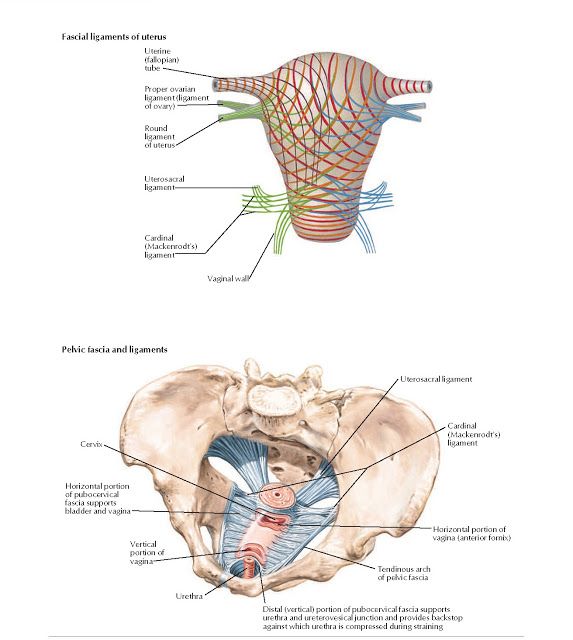
Treatment of an abnormally shaped uterus
Surgery is the only treatment to correct an abnormally shaped uterus, yet many women with such abnormalities don’t need the issue to be surgically corrected. We generally recommend a surgical correction if the woman has had recurrent miscarriages or has compromised fertility due to the uterine abnormality. We may also recommend surgery to correct the issue if she experiences uncomfortable pain regularly.
When appropriate, surgeons will most often perform minimally invasive surgery via laparoscopy or hysteroscopy.
Surgically correcting a septate uterus can improve the chances of a successful pregnancy in a woman with recurrent miscarriages. In the past, surgery could be considered on a bicornuate uterus; however, surgery these days is not the norm for this condition and is reserved mostly for recurrent adverse obstetric outcomes. Additionally, surgical corrections of unicornuate uterus and didelphic uterus have not been shown to be effective treatments at improving pregnancy outcomes.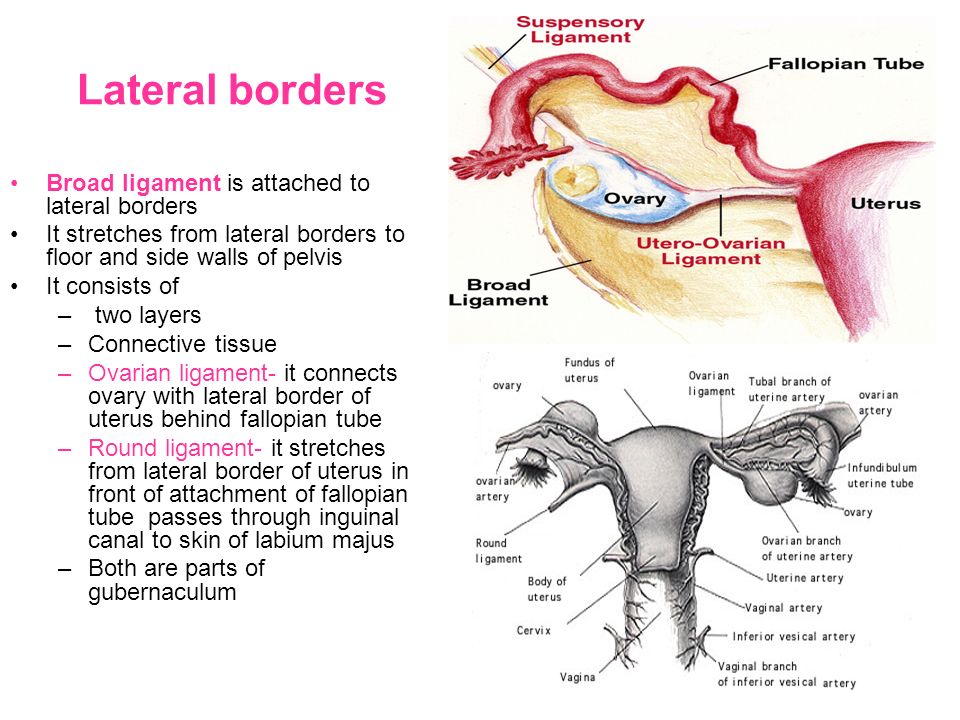
ᐈ Anomalies of the uterus and their impact on the onset and gestation of pregnancy - Reproductive medicine, gynecology, pregnancy monitoring, urology
Laser treatment and vaginal rejuvenation
More details
Once again about hormones or the list of must-haves for the week
More details
Visit card urologist. For or Against?Read more
Reproductive health care
Read more
Pregnancy with uterine fibroids
More details
Practical skills in examining infertile couples
More details
Pregnancy with endometriosis: a modern view
More details
Fighting breast cancer
More details
varicocele
003
More
Secretory and obstructive infertility in men
Learn more
Controlled Ovarian Stimulation (COS) protocols
Learn more
Miscarriage.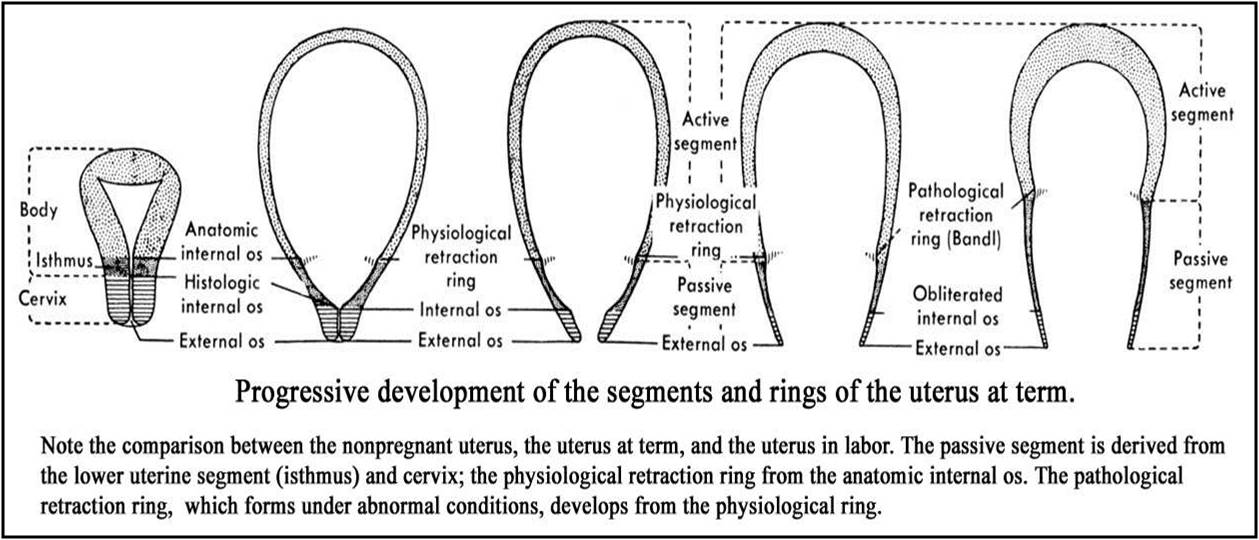 What is the reason?
What is the reason?
More details
Hysteroscopy and its role in the treatment of infertility
More details
Why it is not possible to get pregnant
More details
How to calculate the sex of a child before conception
More details
Uterine obstruction004 Read more
Ovarian hyperstimulation syndrome: modern a look at the problem
More details
Pregnancy with endometriosis - a modern view
Read more
Immunological infertility and the role of antisperm antibodies in it
Read more
What is cervical pathology?
More details
IVF in the natural cycle: pros and cons
More details
Practical skills in examining infertile couples
More details
Artificial insemination
More details
skin.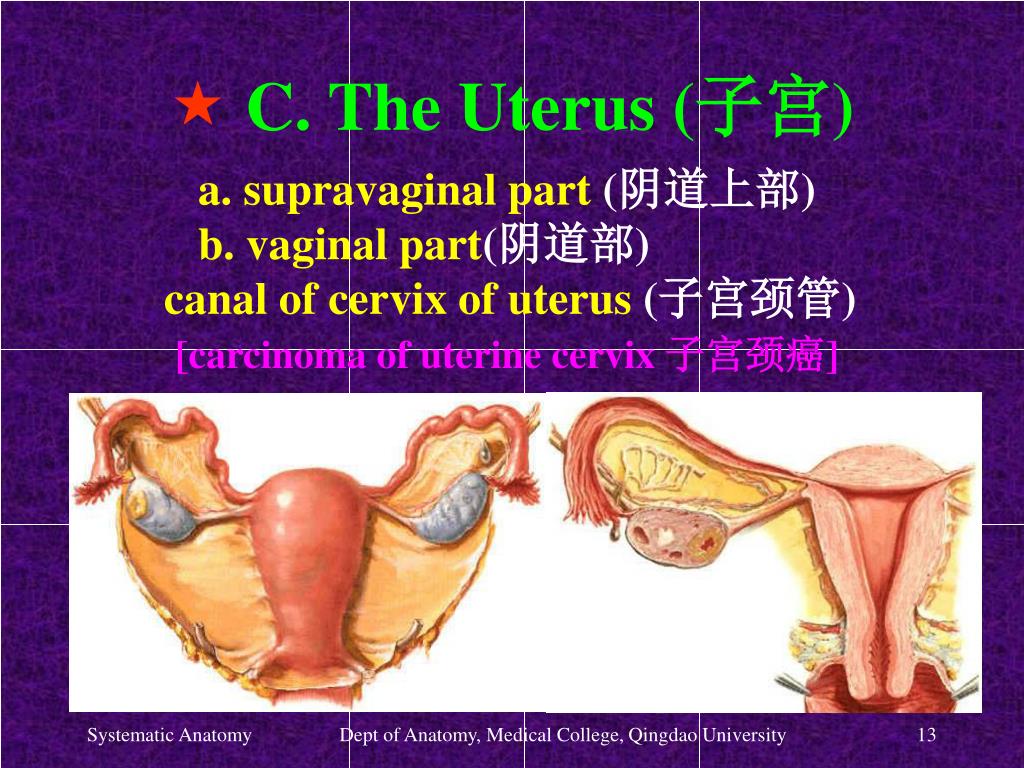
More
Unable to get pregnant. Where to run? Where to begin?
Read more
What future parents need to know (most popular questions)
Read more
Endometriosis. Some important questions
Read more
Prolactin increase. Should I be afraid?
Read more
Obstruction of the fallopian tubes, what to do next?
More
Human papillomavirus. Basic information
Details
KAMALIYA: “I consider Vladimir Kotlik the godfather of my children”
More details
Infertility and cancer: why men should definitely visit a reproductive specialist chances with IVF
Read more
Portrait of a female doctor: 5 signs of a good gynecologist
Read more
Is sex during IVF a good idea?
Read more
Never say never.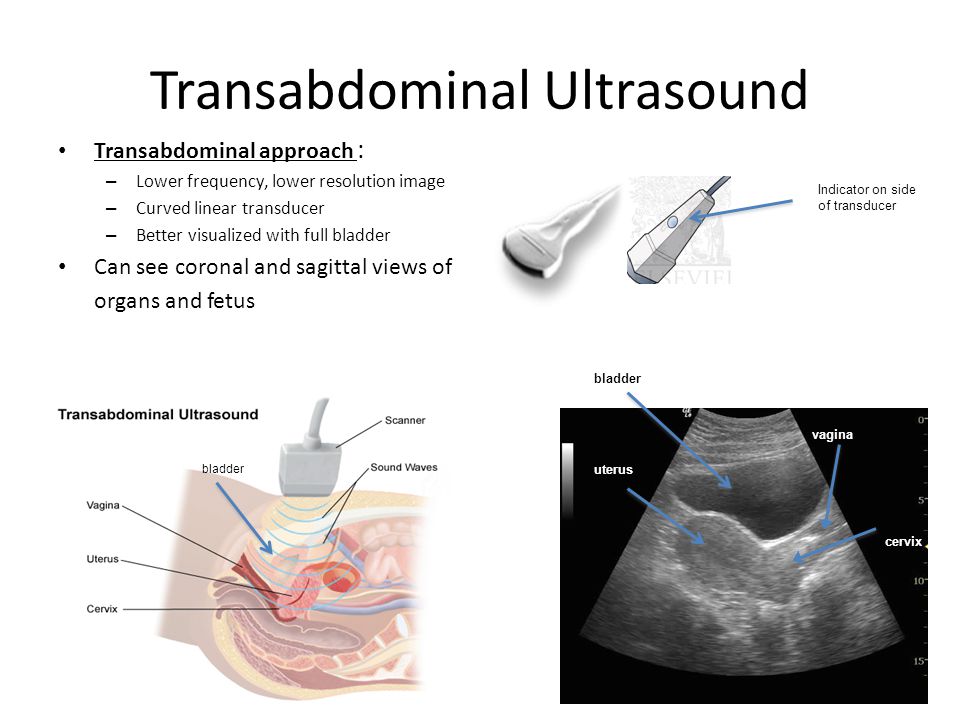 Why childfree is dangerous and why it is worth leaving a “part of yourself” in a cryobank
Why childfree is dangerous and why it is worth leaving a “part of yourself” in a cryobank
More details
How to plan for health, longevity and parenthood: practical advice from doctors for 2020
More details
From virus to cancer: hidden threats to women's health
More details
Signs, causes and risk factors of miscarriage003
Read more
Reproductive health of adolescent girls: what children and their parents need to know
Read more
Life is like magic: how to believe in a miracle if you are a pragmatist - a doctor's story
Read more
Beautiful skin in youth is the key to happy motherhood
Read more
Charged for success. What determines the effectiveness of ART
More
Why do not all eggs become embryos?
More details
Maxim Gapchuk in "Mother and child" ambitious future
More details
Unsuccessful IVF, how to survive? Expert advice
Read more
What should an Rh-negative woman know?
Read more
9 tips for future parents
Read more
IVF: modern methods and approaches in the treatment of female infertility
Read more
ICSI: male infertility is not a sentence
Read more
advantages over traditional surgery 0003Read more
Uterine examination: what you need to know about hysteroscopy
Read more
Artificial intrauterine insemination: the essence of the method, stages and results
More details
Diagnosis of infertility in men
More details
10 reasons to see an andrologist for a man
More details
Cryotechnologies as a way of family planning
More details
Read more
Monalisa Touch — what kind of technology is this
More
Premature menopause in men: how to recognize and what is dangerous
More
Why visit a gynecologist for preventive examinations
More details
Laser therapy in gynecology: without anesthesia and pain
More details
Outpatient gynecology - timely seeking qualified help
More details
why additional tests are needed after pregnancy and examinationMore details
Causes and prevention of female infertility
More details
One-day surgery: a modern approach to treatment
3
More details
Pregnancy management: to keep the baby healthy and mother's well-being
More details
Pregnancy after IVF: what future parents need to remember
More details
Anomalies of the uterus and their impact on the onset and carrying of pregnancy.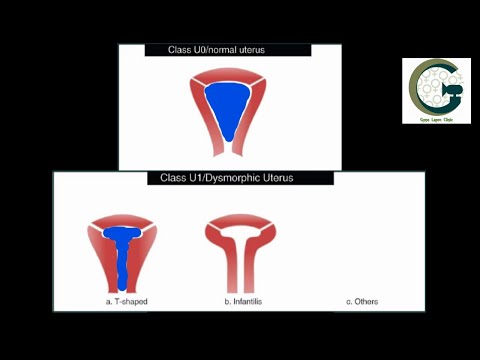
Read more
Scar on the uterus after caesarean section
Read more
The most common mistakes during pregnancy
Read more
Varicose veins and hemorrhoids during pregnancy
More details
Pregnancy planning (lifestyle)
More details
First aid kit for pregnant women during the war
More details
Periods disappeared during the war. What to do?
More details
Freezing of husband's sperm before the war
More details
A visit to a reproductive specialist during the war
More details
I learned that I was pregnant before the war. What to do?
Read more
What does vaginal discharge mean
Read more
Why can't I get pregnant?
Read more
How to get pregnant if you don't ovulate?
Read more
Male Infertility Diagnosis
Read more
When to See a Gynecologist
Read more
Fertility Program Guide
Learn more
cells
Read more
You are given a chance.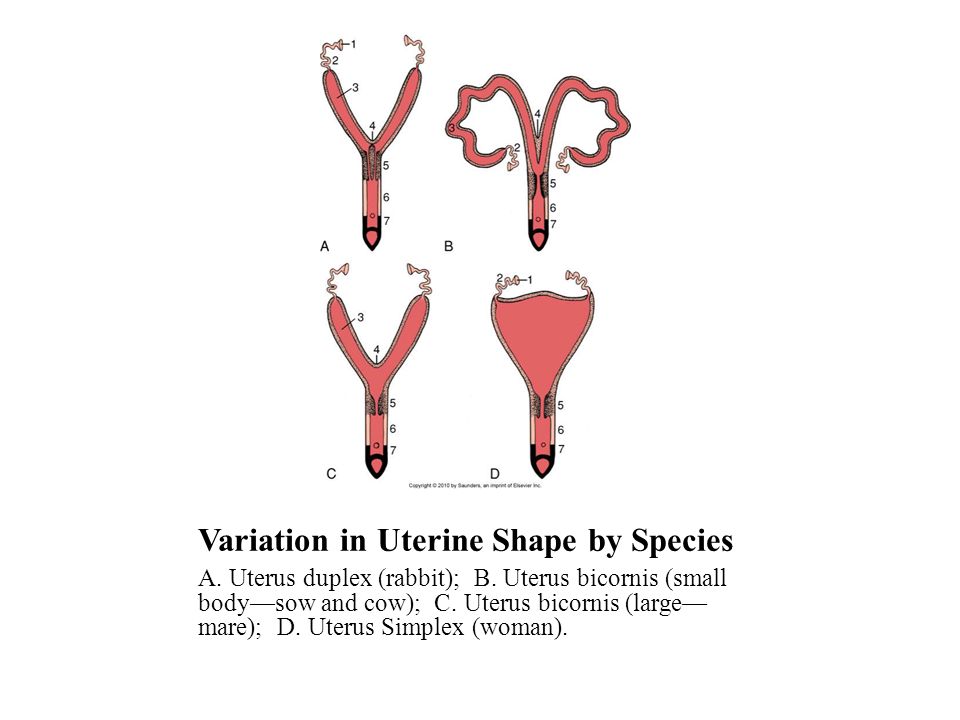 What you need to know about artificial insemination
What you need to know about artificial insemination
More
What causes thrush and why it comes back
More
Myths about egg donation
More
How to prepare for a gynecological examination More
2 Pregnancy during the warRead more
What tests are done during pregnancy and when
Read more
1st, 2nd and 3rd Trimester Prenatal Screenings
More details
Invasive Prenatal Diagnostics
More details
Non-Invasive Prenatal Diagnostics
More details
Bicornuate Pregnancy3
How ovulation is stimulated
More details
Embryo implantation, or what determines the success of IVF
Read more
When is it better to transfer the embryo - on the third or fifth day?
Read more
How to distinguish the onset of labor from a false alarm
Read more
Saddle uterus.
 What is a saddle uterus?
What is a saddle uterus? IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
The saddle uterus is a type of bicornuate uterus; a malformation in which the fundus of the uterus is split in the form of a saddle. The degree of splitting of the bottom of the uterus into two horns varies, but in all cases the shape of the uterus in the section resembles a saddle. The presence of a saddle uterus may not manifest itself in any violations or be accompanied by an increased risk of miscarriage, premature birth, weakness and incoordination of labor, postpartum hemorrhage. The saddle uterus is often combined with other malformations. The saddle uterus is detected, as a rule, by chance - during ultrasound, hysteroscopy, MRI.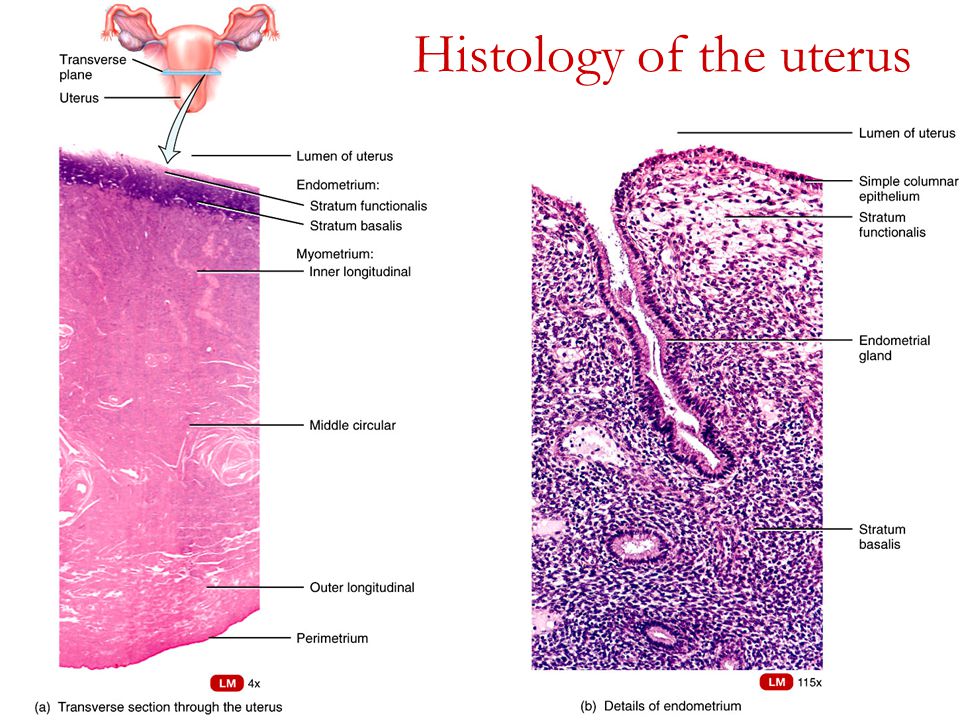 Surgical correction of the saddle uterus is indicated in case of impaired pregnancy.
Surgical correction of the saddle uterus is indicated in case of impaired pregnancy.
- Causes of saddle uterus
- Symptoms of saddle uterus
- Diagnostics
- Saddle uterus treatment
- Prices for treatment
General
The saddle uterus is a particular manifestation of the bicornuate uterus. With a saddle uterus, a small concave depression in the form of a saddle is formed on the outer surface of the bottom of the organ. In gynecology, of the total number of anomalies in the development of the uterus, the saddle uterus accounts for about 23% of cases. The degree of splitting of the bottom of the uterus into two horns varies: expansion of the transverse size, flattening of the bottom, a slight divergence of the bottom into two horns. In all cases, the shape of the uterus in section resembles a saddle.
The saddle uterus is often combined with malformations of the urinary system, intrauterine septum, and narrow pelvis.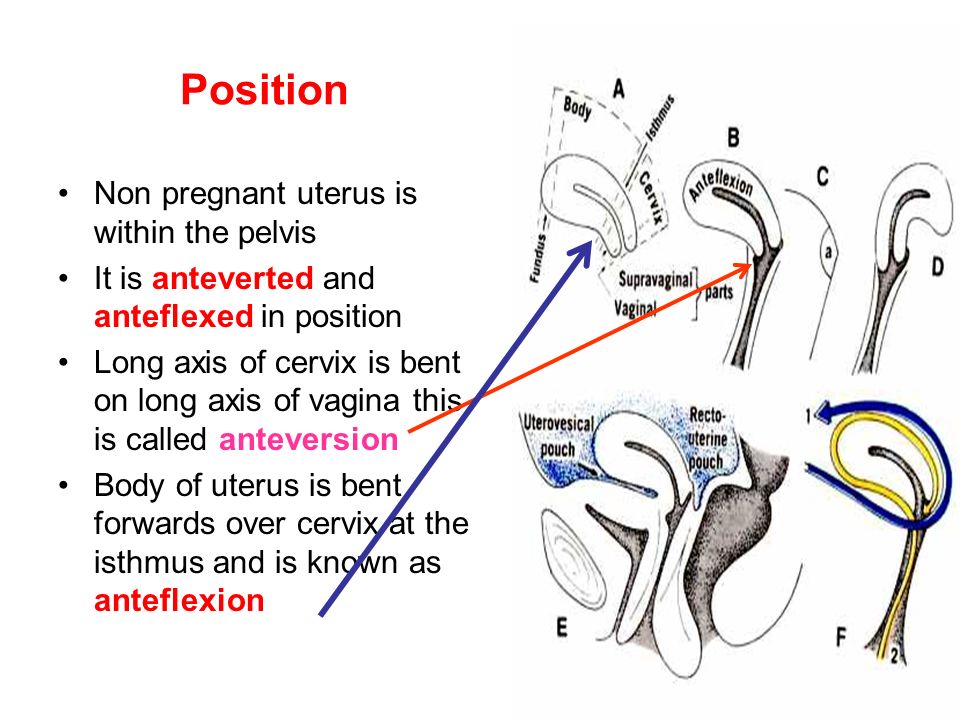 Therefore, the presence of a saddle uterus can be dangerous for the development of primary infertility, various pathologies of pregnancy, birth injuries, postpartum complications, intrauterine fetal death.
Therefore, the presence of a saddle uterus can be dangerous for the development of primary infertility, various pathologies of pregnancy, birth injuries, postpartum complications, intrauterine fetal death.
Saddle uterus
Causes of saddle uterus formation
Saddle shaped deformity of the uterus is formed between the 10th and 14th weeks of embryogenesis during the fusion of the mesonephric ducts. At the stage of embryonic development, the uterine cavity is initially represented by two uterovaginal cavities separated by a median sagittal septum. By the time of the birth of the female fetus, the septum gradually resolves, i.e., the initially bicornuate uterus first takes on a saddle shape, and then a normal, pear-shaped single cavity. In cases of incompleteness of the formation of the uterus, by the time the girl is born, the concavity in the bottom area remains, which leads to a congenital defect - the saddle uterus.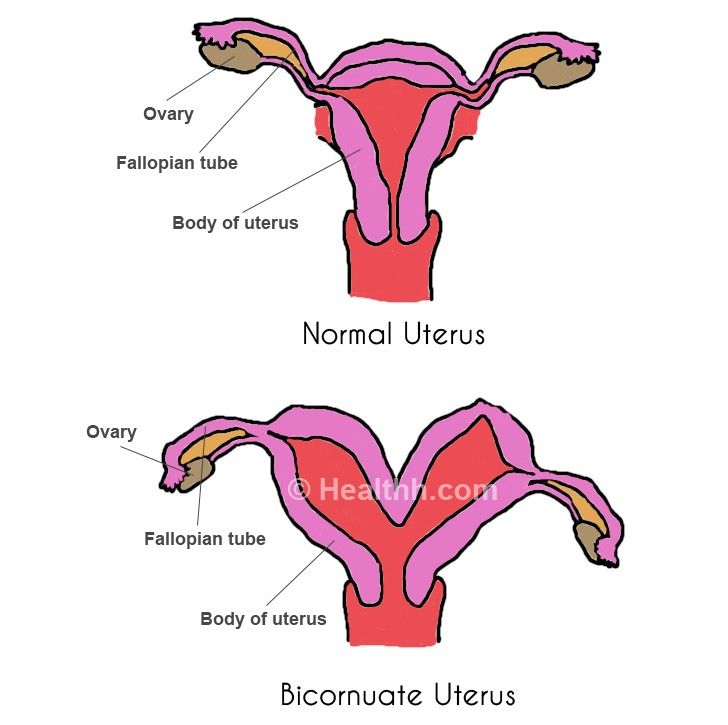 In addition to splitting the bottom with a saddle uterus, there is always its expansion in diameter.
In addition to splitting the bottom with a saddle uterus, there is always its expansion in diameter.
The causes of disembryogenesis and the formation of a saddle uterus can be various damaging factors that disrupt the proper formation of organs during pregnancy: maternal intoxication (alcohol, nicotine, narcotic, drug, chemical), beriberi, stress, endocrinopathies (thyrotoxicosis, diabetes mellitus), heart defects. Infectious diseases of a pregnant woman - measles, influenza, rubella, syphilis, toxoplasmosis, etc. - have an extremely unfavorable effect on organogenesis. Pregnancy under conditions of toxicosis, chronic fetal hypoxia can contribute to the formation of a saddle uterus.
Saddle uterus symptoms
Outside of pregnancy, a woman may not be aware of the presence of a saddle uterus. A slight saddle-shaped deformity of the uterine fundus does not prevent the onset of pregnancy, does not complicate the bearing of the fetus and childbirth.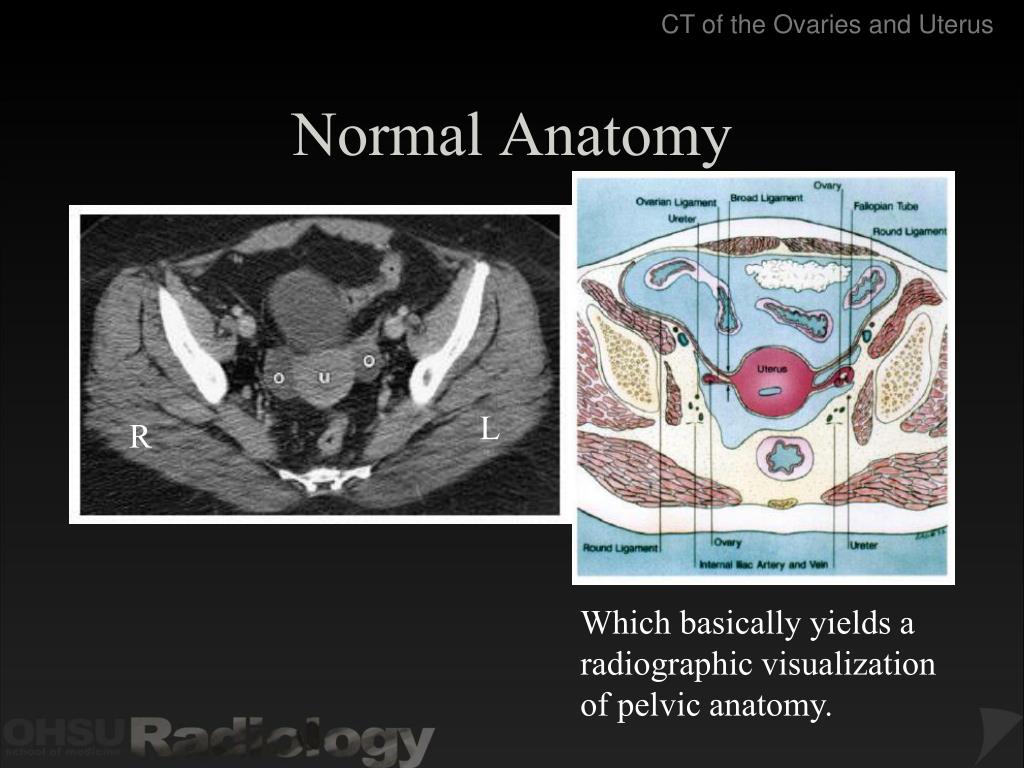 With more pronounced changes, there may be a threat of spontaneous abortion, pathology of the placenta (lateral or low location, placenta previa, premature detachment), transverse position of the fetus, pelvic presentation of the fetus, premature birth.
With more pronounced changes, there may be a threat of spontaneous abortion, pathology of the placenta (lateral or low location, placenta previa, premature detachment), transverse position of the fetus, pelvic presentation of the fetus, premature birth.
During childbirth, the saddle uterus can be a factor in the development of abnormal labor activity - weakness or discoordination. Often, with a saddle uterus in obstetrics, one has to resort to a caesarean section. Anatomical and functional inferiority of the uterus can provoke postpartum hemorrhage. In the absence of proper monitoring of a woman during pregnancy, the risk of perinatal mortality increases. In cases of severe deformation of the uterine fundus, primary infertility may occur.
Diagnostics
In the diagnosis of the saddle uterus, a decisive role is played by instrumental studies - ultrasound, USGSS, hysteroscopy, hysterosalpingography, magnetic resonance imaging. A standard gynecological examination with a saddle uterus is not informative.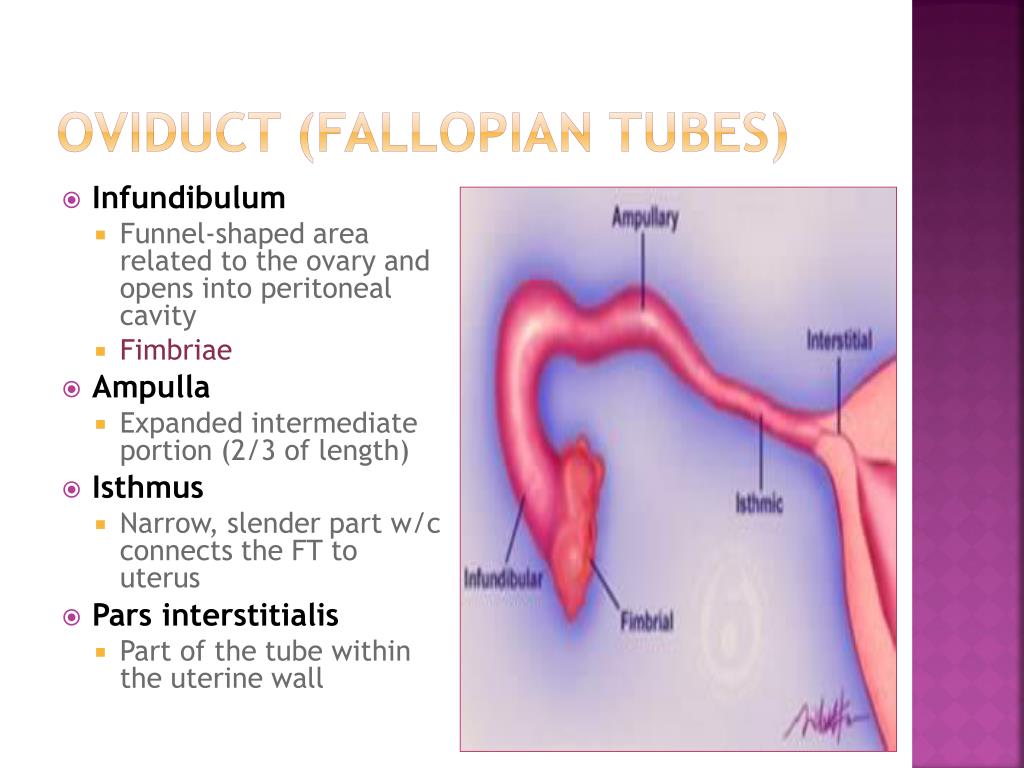
In the process of echography of the small pelvis (ultrasound), the saddle uterus is not always detected. With significant deformation, transverse scanning reveals an increase in the width of the fundus of the uterus up to 68 mm, thickening of the myometrium of the fundus wall up to 10-14 mm and its bulging into the cavity of the organ. To detect a saddle uterus, it is preferable to conduct an ultrasound scan with a vaginal probe in the second phase of the cycle with a sufficiently pronounced thickness of the endometrium.
The most reliable characteristic signs of the saddle uterus are found during hysterosalpingography: on radiographs, 2 mouths of the fallopian tubes are determined, in the bottom area, a small depression in the form of a saddle protruding into the uterine cavity is clearly read. Similar signs are detected during MRI. Hysteroscopy is used to directly visually examine the uterine cavity. In the process of pregnancy management in patients with a saddle uterus, dopplerography of the uteroplacental blood flow is monitored, cardiotocography, and fetal phonocardiography are performed.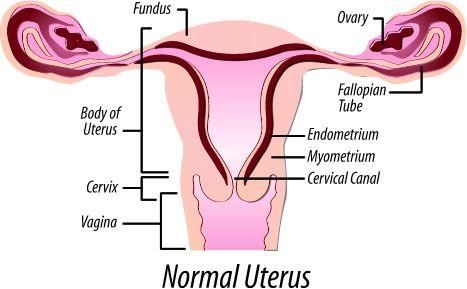
Saddle uterus treatment
Surgical tactics in the saddle uterus is used only if conception is impossible (in the absence of other reasons) or habitual miscarriage of the fetus. Reconstruction of the uterine cavity is often performed in the process of hysteroscopy through natural routes, without incisions. After correcting the defect, the chances of a normal pregnancy increase tenfold.
Patients with a saddle uterus should be under the close supervision of an obstetrician-gynecologist from the early stages of pregnancy, strictly follow all the recommendations, and if the slightest violations appear, be hospitalized in a maternity facility. In the case of a complicated pregnancy in patients with a saddle uterus, bed rest, antispasmodics, herbal sedatives, gestagens, deproteinized calf blood hemoderivat, essential phospholipids are prescribed. Tactics regarding the upcoming birth in pregnant women with a saddle uterus is decided in advance.