Rash on baby face with fever
Causes and when to see a doctor
Toddlers can often get fevers when they are unwell, even when they have a cold or another minor illness. Several common childhood illnesses, including roseola and scarlet fever, can cause a rash to develop after the fever passes.
A fever is not a disease but a sign that the body’s immune system is fighting an infection. The body raises its core temperature to fight off the invading bacteria or viruses.
Children aged 1–3 years old, generally referred to as toddlers, often get illnesses because:
- their immune systems have not yet fully developed
- they have increased exposure to germs from other children, especially in day care or preschool
- they tend to put their hands or objects in their mouths
Fever usually goes away once the illness passes. However, toddlers sometimes develop a rash following a fever. Although this is rarely severe, it is important to see a doctor immediately.
In this article, we look at the possible causes of a rash after fever in toddlers, what to do about it, and when to see a doctor.
Several common childhood illnesses can cause a rash after fever. Most are not serious, but some do require medical treatment, so it is essential to discuss these symptoms with a doctor.
Common causes of post-fever rash in toddlers include:
Roseola infantum
Roseola infantum, which is also called roseola or sixth disease, is a viral infection. Babies and toddlers pass on the virus through saliva, coughing, and sneezing.
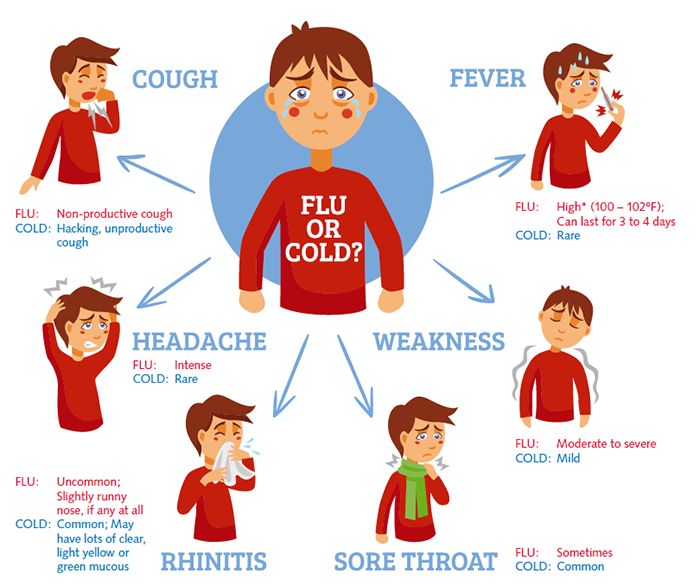
Roseola may cause a sudden, high fever of 102–105°F that lasts for 3–6 days. Some children are active and comfortable with no other symptoms during this stage of the illness, but others may also experience:
- decreased appetite or unwillingness to eat
- eye swelling or conjunctivitis, also known as pink eye
- a cough
- a runny nose
- diarrhea
- swollen lymph nodes
- sleepiness or irritability
Typically, the symptoms of roseola go away suddenly on the sixth or seventh day of illness. After these symptoms have cleared up, the rash appears.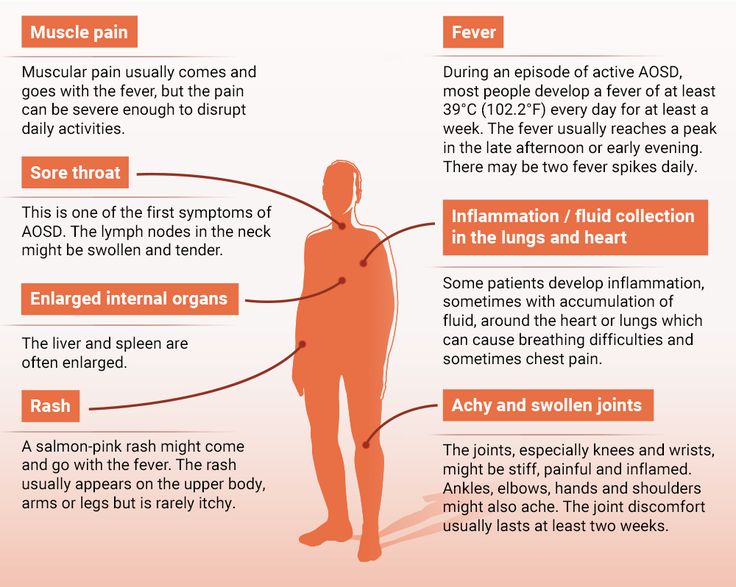
In most cases, the roseola rash:
- consists of small pink spots, about 2–5 millimeters (mm) wide
- may be slightly raised or flat
- starts on the trunk and may spread to the arms, neck, and face
- does not itch or hurt
- disappears when pressed, which is known as blanching
- fades after 1–2 days
The incubation period for roseola is 7–14 days, which means that symptoms may not appear until 1–2 weeks after becoming infected. Antibiotics do not work against roseola, but extra fluids and fever-reducing medicine can relieve symptoms.
Parents and caregivers should keep children with roseola out of school or day care until they have been free of fever for 24 hours without the use of medication. The rash from roseola is not contagious.
Up to 15 percent of children with roseola may also experience a febrile seizure, which can happen as a result of the high fever and the ability of the virus to cross into the brain.
During a febrile seizure, the child may:
- lose consciousness
- start shaking their arms and legs uncontrollably
- become stiff
- roll their eyes
- wet or soil themselves
- vomit
- froth at the mouth
Febrile seizures generally only last a few minutes. According to the National Institute of Neurological Disorders and Stroke, there is no evidence that short febrile seizures cause brain damage. Most children will recover without any problems.
According to the National Institute of Neurological Disorders and Stroke, there is no evidence that short febrile seizures cause brain damage. Most children will recover without any problems.
However, the parent or caregiver should immediately call an ambulance if:
- it is the child’s first febrile seizure
- the seizure lasts longer than 5 minutes
- the child has a stiff neck, is vomiting excessively, or is extremely lethargic
During the seizure, it is vital to:
- remain calm and time the length of the seizure
- carefully place the child in a safe location to protect them from accidental injury
- position the child on their side or front to prevent choking
- carefully remove any objects from the child’s mouth
Scarlet fever
Share on PinterestA person may contract scarlet fever through contact with infected skin lesions.Scarlet fever results from an infection with group A Streptococcus bacteria. This type of bacteria can also cause strep throat and specific skin infections, such as impetigo.
This type of bacteria can also cause strep throat and specific skin infections, such as impetigo.
Infected children can pass on the bacteria through:
- coughing and sneezing
- sharing food or drinks
- letting other people touch a skin lesion, where there is a skin infection
Symptoms of scarlet fever may include:
- a temperature of 101°F or higher
- red rash that starts on the neck, underarms, or groin area and spreads across the body
- red, sore throat
- white coating or red bumps on the tongue
- redness in skin creases, such as under the arms and inside the elbows and inner thighs
- a headache
- body aches
- nausea, stomach ache, or vomiting
The rash from scarlet fever feels rough like sandpaper. It usually appears 1–2 days after the fever starts but can present up to 7 days later.
The area around the mouth usually remains pale, even if the rest of the face looks red. After the rash has faded, the skin may peel.
A child with symptoms of scarlet fever should see a doctor as soon as possible. In rare cases, group A strep infections can cause severe complications, such as heart or kidney problems.
Doctors treat scarlet fever with antibiotics. A child may return to school or day care once they have been taking antibiotics for at least 24 hours.
Hand, foot, and mouth disease
Hand, foot, and mouth disease (HFMD) is common in children under 5 years old. Several different viruses can cause this illness, and children can pass on the infection through:
- saliva
- coughing and sneezing
- fluid from blisters
- poop
HFMD often starts with a fever, but it may also cause a sore throat, lack of appetite, and malaise.
After about 1–2 days, sores and a rash may appear. The telltale signs of HFMD include:
- sores in the back of the mouth that are small initially but turn into painful blisters
- flat, red spots on the palms of the hands or the soles of the feet
- flat, red spots or blisters on the buttocks or groin
Some toddlers might get all of these symptoms, while others may only get mildly sick without any other problems.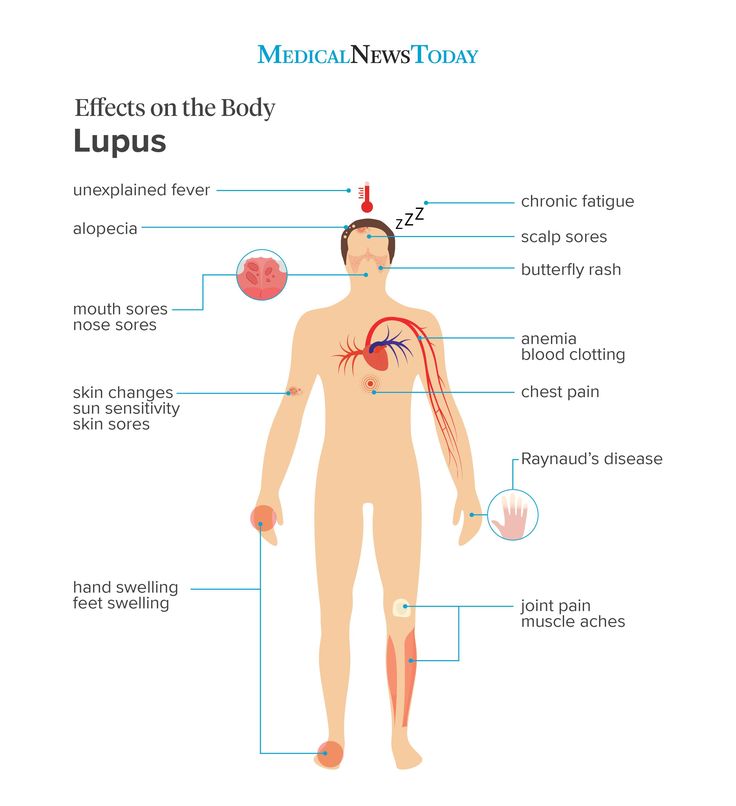 A parent or caregiver should get advice from a doctor on when a child with scarlet fever should return to school or day care.
A parent or caregiver should get advice from a doctor on when a child with scarlet fever should return to school or day care.
Although most cases of HFMD resolve on their own, the sores can be painful. If a child is unable to eat or drink, there is a risk of dehydration. Children who are not eating or drinking or who seem very ill should see a doctor.
Fifth disease
Fifth disease, known medically as erythema infectiosum, is a viral infection that commonly occurs in toddlers. Parvovirus B19 is the virus responsible for the infection, which spreads easily through coughing and sneezing.
Symptoms of fifth disease may include:
- fever
- a headache
- a runny nose
Fifth disease is sometimes called slapped cheek syndrome because the rash causes the cheeks to appear red. Some toddlers may get a red, blotchy rash on their trunk, buttocks, arms, and legs a few days after the redness becomes apparent in the cheeks.
The rash may cause itching and tends to form a lacy pattern as it starts to fade. It can last for several weeks.
It can last for several weeks.
Most children recover from fifth disease without any problems. However, both children and adults with weakened immune systems can develop long-term complications.
As it is a viral illness, antibiotics are not effective against fifth disease. Plenty of fluids, rest, and pain relievers may be beneficial.
Usually, children can go back to school or day care once they have been fever-free for at least 24 hours. The rash is not contagious.
Share on PinterestA pharmacist can offer advice about medication for children.
If a toddler is uncomfortable, medications that reduce pain and fever can relieve symptoms. Acetaminophen or ibuprofen are standard choices and are available over the counter (OTC).
When giving medication to a child:
- always follow the directions on the packaging carefully
- be sure to use the correct amount for the child’s age and weight
- if in doubt, check with a medical professional first
Encourage the child to drink plenty of fluids. Popsicles or children’s electrolyte drinks may be helpful if the child does not want water.
Popsicles or children’s electrolyte drinks may be helpful if the child does not want water.
Fevers in toddlers are often due to illnesses that get better on their own. However, parents and caregivers should observe young children when they get a fever, rash, or other symptoms of an illness.
Call a doctor if a child of any age gets a rash after fever, or if the child is:
- younger than 3 months of age and has a rectal temperature of 100.4°F or higher
- aged 3–6 months and has a temperature of 102°F or higher
- over 6 months of age and has a fever of 103°F or higher
This is essential even if the child does not seem unwell.
Fever and rashes are common in toddlers. Most of the time, the child will recover without any long-term problems. However, it is important to monitor symptoms closely.
If symptoms become worse or do not go away, see a doctor. Parents and caregivers who have any concerns about a child’s illness should speak to a doctor.
Roseola (for Parents) - Nemours KidsHealth
What Is Roseola?
Roseola (roe-zee-OH-lah) is a viral illness that most commonly affects young kids between 6 months and 2 years old. It's also known as sixth disease, exanthem subitum, and roseola infantum.
It is usually marked by several days of high fever, followed by a distinctive rash just as the fever breaks.
Two common, closely related viruses can cause roseola, human herpesvirus (HHV) type 6 and type 7. These viruses belong to the same family as the better-known herpes simplex viruses (HSV), but do not cause the cold sores and genital herpes infections that HSV can cause.
What Are the Signs & Symptoms of Roseola?
Most children with roseola develop a mild upper respiratory illness, followed by a high fever (often higher than 103°F or 39.5°C) for up to a week. During this time, a child might be fussy or irritable, not eat as much as usual, and may have swollen lymph nodes (glands) in the neck.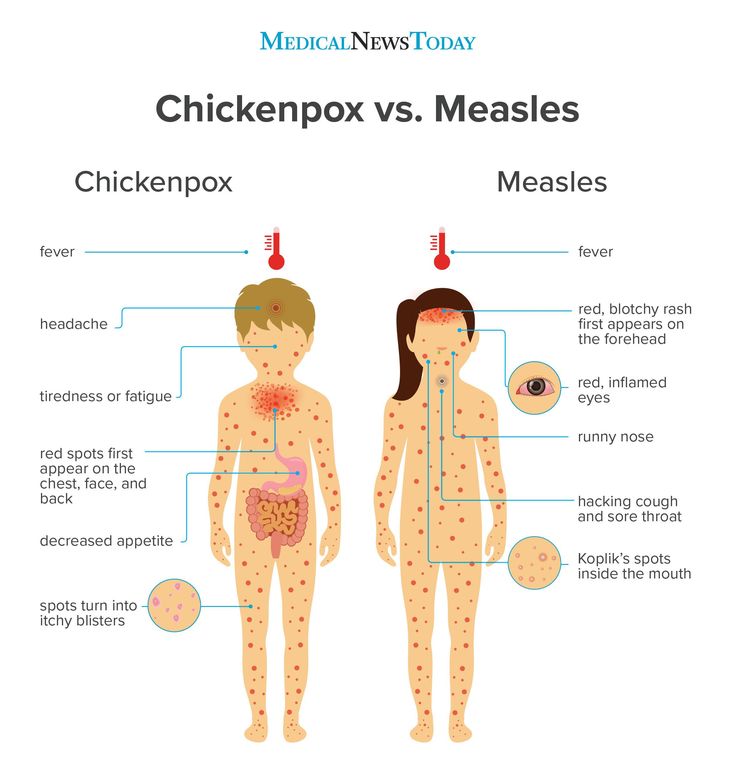
The high fever often ends abruptly, and at about the same time a pinkish-red flat or raised rash starts on the trunk. The rash's spots turn white when touched, and individual spots may have a lighter "halo" around them. The rash usually spreads to the neck, face, arms, and legs.
This fast-rising fever can trigger febrile seizures (convulsions caused by high fevers) in about 10% to 15% of young children who have roseola. Signs of a febrile seizure include:
- unconsciousness
- 2 to 3 minutes of jerking or twitching in the arms, legs, or face
- loss of control of the bladder or bowels
Is Roseola Contagious?
Roseola is contagious. The infection spreads when a child with roseola talks, sneezes, or coughs, sending tiny droplets into the air that others can breathe in. The droplets also can land on surfaces; if other children touch those surfaces and then their nose or mouth, they can become infected.
Roseola may be contagious during the fever phase, but does not spread by the time the rash breaks out.
Can Roseola Be Prevented?
There is no known way to prevent roseola. But because it affects young kids rather than adults, it's thought that a bout of roseola in childhood may provide some lasting immunity to the illness. Repeat cases of roseola can happen, but are uncommon.
How Long Does Roseola Last?
The fever of roseola lasts from 3 to 7 days, followed by a rash lasting from hours to a few days.
How Is Roseola Diagnosed?
To make a diagnosis, a doctor will take a
medical historyand do an exam. A diagnosis of roseola is often uncertain until the fever drops and the rash appears, so the doctor may order tests to make sure that the fever is not caused by another type of infection.
How Is Roseola Treated?
Roseola usually does not require professional medical treatment. When it does, most treatment is focused on lowering the high fever. Antibiotics can't treat roseola because viruses, not bacteria, cause it.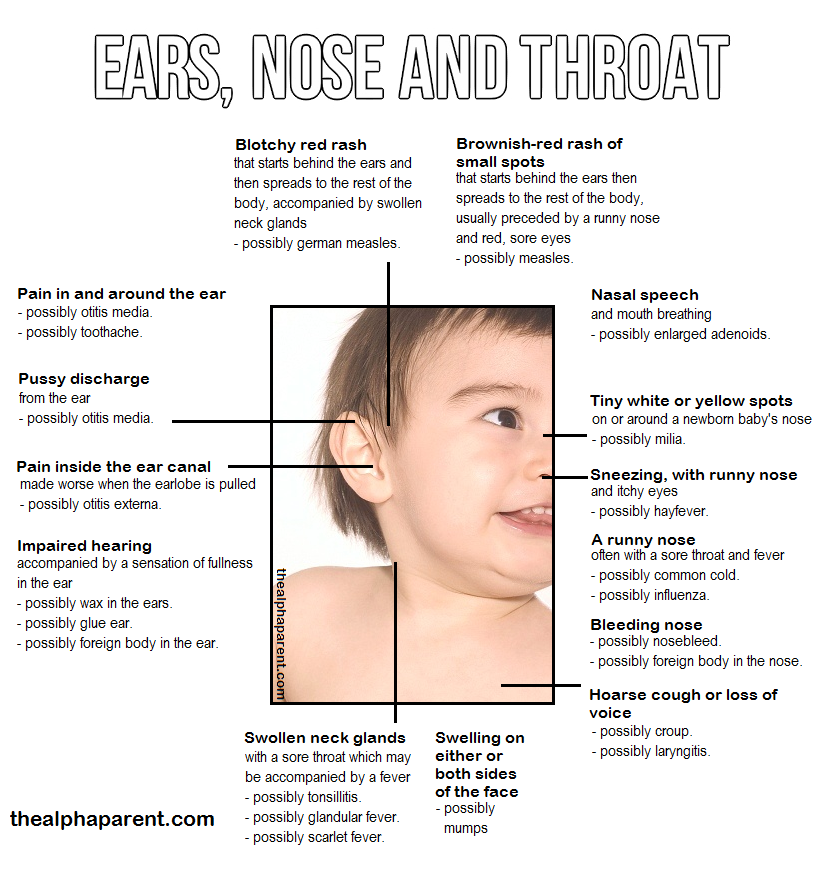
Home Treatment
Acetaminophen (such as Tylenol) or ibuprofen (such as Advil or Motrin) can help to ease a fever. Never give aspirin to a child who has a viral illness because its use in such cases has been associated with Reye syndrome, which can lead to liver failure and death.
While some parents use lukewarm sponge baths to lower fever, there is no proof that this really works. In fact, sponge baths can make children uncomfortable. Never give your child an icy or cold bath or alcohol rubs.
To prevent dehydration from the fever, encourage your child to drink clear fluids such as water with ice chips and Pedialyte (electrolyte oral replacement solution). Breast milk and formula can help prevent dehydration as well.
When Should I Call the Doctor?
Call the doctor if your child is lethargic or won't drink or breastfeed. If your child has a seizure, get emergency care right away.
Reviewed by: Julio E. Pajaro, MD
Date reviewed: January 2019
Parental leaflet on viral diseases
Parental leaflet.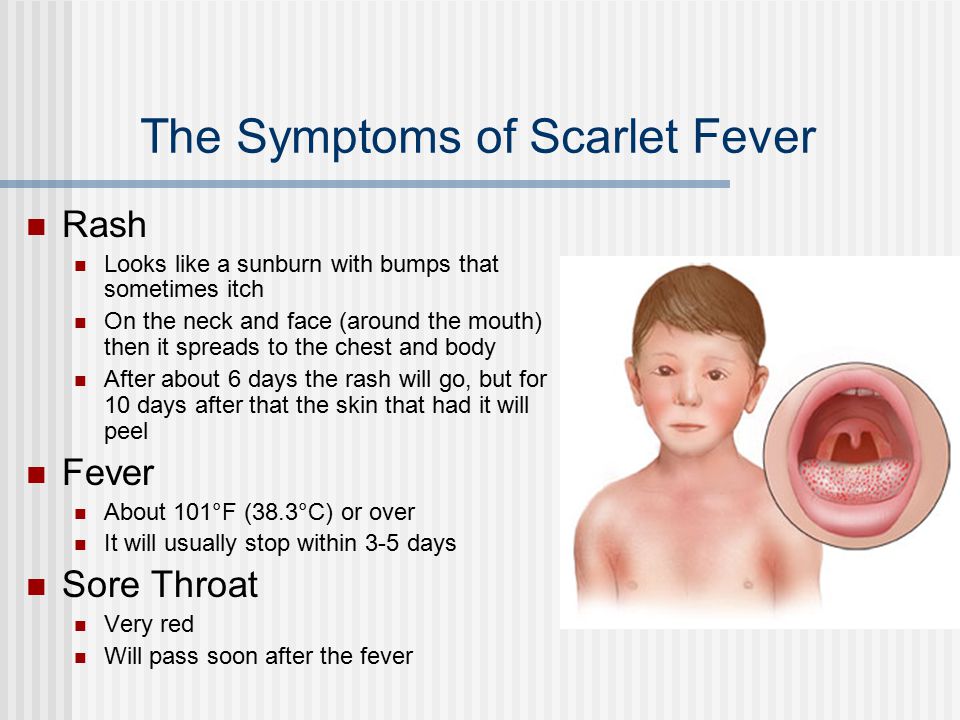
Measles is a viral infection with a very high susceptibility. If a person has not had measles or has not been vaccinated against this infection, then after contact with the patient, infection occurs in almost 100% of cases. The measles virus is highly volatile. The virus can spread through ventilation pipes and elevator shafts - at the same time, children living on different floors of the house get sick.
The period from contact with a person with measles to the appearance of the first signs of the disease lasts from 7 to 14 days.
The disease begins with a severe headache, weakness, fever up to 40 degrees C. A little later, a runny nose, cough and almost complete lack of appetite join these symptoms.
Very characteristic of measles is the appearance of conjunctivitis - inflammation of the mucous membrane of the eyes, which is manifested by photophobia, lacrimation, sharp redness of the eyes, and subsequently - the appearance of purulent discharge. These symptoms last 2 to 4 days.
These symptoms last 2 to 4 days.
On the 4th day of illness, a rash appears , which looks like small red spots of various sizes (from 1 to 3 mm in diameter), with a tendency to merge. The rash occurs on the face and head (it is especially characteristic of its appearance behind the ears) and spreads throughout the body for 3-4 days. It is very characteristic of measles that the rash leaves behind pigmentation (dark spots that persist for several days), which disappears in the same sequence as the rash appears.
Measles can cause serious complications . These include inflammation of the lungs (pneumonia), inflammation of the middle ear (otitis media), and sometimes such a formidable complication as encephalitis (inflammation of the brain).
It must be remembered that after suffering from measles for a sufficiently long period of time (up to 2 months), there is a suppression of immunity, so the child can get sick with some cold or viral disease, so you need to protect him from excessive stress, if possible from contact with sick children.
Long-lasting immunity develops after measles. All those who have had measles become immune to this infection.
The only reliable protection against the disease is vaccination against measles, which is included in the National Immunization Schedule.
Reminder for parents.
Rubella is an airborne viral infection. As a rule, children who stay in a water room for a long time with a child who is a source of infection get sick. Rubella in its manifestations is very similar to measles, but it is much easier.
The period from contact to the appearance of the first signs of illness lasts from 14 to 21 days.
Rubella begins with an increase in the occipital lymph nodes and an increase in body temperature up to 38 degrees C. A little later, a runny nose joins, and sometimes a cough. A rash appears 2 to 3 days after the onset of the disease. Rubella is characterized by a pink, punctate rash that begins with a rash on the face and spreads throughout the body. Rubella rash, unlike measles, never merges, there may be a slight itch. The period of rashes can be from several hours, during which there is no trace of the rash, up to 2 days.
Rubella rash, unlike measles, never merges, there may be a slight itch. The period of rashes can be from several hours, during which there is no trace of the rash, up to 2 days.
The treatment of rubella is to relieve the main symptoms - the fight against fever, if any, the treatment of the common cold, expectorants.
Complications from rubella are rare.
After rubella, immunity also develops, re-infection is extremely rare, but can occur.
It is therefore very important to get the rubella vaccine, which, like the measles vaccine, is included in the National Immunization Schedule.
Note for parents.
Mumps (mumps) is a childhood viral infection characterized by acute inflammation in the salivary glands.
Infection occurs by airborne droplets. Susceptibility to this disease is about 50-60% (that is, 50-60% of those who were in contact and who were not ill and not vaccinated get sick).
It can take 11 to 23 days from contact with a sick mumps to the onset of illness.
Mumps begins with an increase in body temperature up to 39 degrees C and severe pain in or under the ear, worse when swallowing or chewing. At the same time, salivation increases. Swelling quickly grows in the area of the upper part of the neck and cheeks, touching this place causes severe pain in the child. Unpleasant symptoms disappear within three to four days: body temperature decreases, swelling decreases, pain disappears.
However, quite often mumps ends inflammation in glandular organs such as pancreas (pancreatitis), gonads. Past pancreatitis in some cases leads to diabetes mellitus . Inflammation of the gonads (testicles) is more common in boys. This significantly complicates the course of the disease, and in some cases may result in infertility. In especially severe cases, mumps can be complicated by viral meningitis (inflammation of the meninges), which is severe.
After a disease, a strong immunity is formed, but complications can lead to disability.
The only reliable protection against the disease is vaccination against mumps, which is included in the National Immunization Schedule.
Reminder for parents.
Varicella (chickenpox) is a common childhood infection. Mostly young children or preschoolers are ill. Susceptibility to the causative agent of chickenpox (the virus that causes chickenpox refers to herpes viruses) is also quite high. About 80% of contact persons who have not been ill before develop chickenpox.
From the moment of contact with a patient with chickenpox until the first signs of the disease appear, 14 to 21 days pass.
The disease begins with a rash. Usually it is one or two reddish spots, similar to a mosquito bite. These elements of the rash can be located on any part of the body, but most often they first appear on the stomach or face. Usually the rash spreads very quickly - new elements appear every few minutes or hours. Reddish spots, which at first look like mosquito bites, the next day take the form of bubbles filled with transparent contents. These blisters are very itchy. The rash spreads throughout the body, to the limbs, to the scalp. In severe cases, there are elements of the rash on the mucous membranes - in the mouth, nose, on the conjunctiva of the sclera, genitals, intestines. By the end of the first day of the disease, the general state of health worsens, the body temperature rises (up to 40 degrees C and above). The severity of the condition depends on the number of lesions. If there are elements of the rash on the mucous membranes of the pharynx, nose and on the conjunctiva of the sclera, then pharyngitis, rhinitis and conjunctivitis develop due to the addition of a bacterial infection. Bubbles open in a day or two with the formation of sores, which are covered with crusts. Headache, feeling unwell, fever persist until new rashes appear.
This usually happens within 3 to 5 days. Within 5-7 days after the last sprinkling, the rash disappears.
Treatment of chickenpox is to reduce itching, intoxication and prevent bacterial complications. The elements of the rash must be lubricated with antiseptic solutions (as a rule, this is an aqueous solution of brilliant green or manganese). Treatment with coloring antiseptics prevents bacterial infection of rashes, allows you to track the dynamics of the appearance of rashes. It is necessary to monitor the hygiene of the mouth and nose, eyes - you can rinse your mouth with a solution of calendula, the mucous membranes of the nose and mouth also need to be treated with antiseptic solutions.
Complications of chickenpox include myocarditis - inflammation of the heart muscle, meningitis and meningoencephalitis (inflammation of the meninges, brain matter), inflammation of the kidneys (nephritis). Fortunately, these complications are quite rare. After chickenpox, as well as after all childhood infections, immunity develops. Re-infection happens, but very rarely.
Reminder for parents.
Scarlet fever is the only childhood infection caused not by viruses but by bacteria (group A streptococcus). This is an acute disease transmitted by airborne droplets. Infection through household items (toys, dishes) is also possible. Children of early and preschool age are ill. The most dangerous in terms of infection are patients in the first two to three days of the disease.
Scarlet fever begins very acutely with fever up to 39 degrees C, vomiting, headache. The most characteristic symptom of scarlet fever is tonsillitis, in which the mucous membrane of the throat has a bright red color, swelling is pronounced. The patient notes a sharp pain when swallowing. There may be a whitish coating on the tongue and tonsils. The tongue subsequently acquires a very characteristic appearance ( “crimson ”) - bright pink and coarsely granular.
By the end of the first beginning of the second day of illness, 9 appears0003 the second characteristic symptom of scarlet fever is a rash. It appears immediately on several parts of the body, most densely located in the folds (elbow, inguinal). Its distinguishing feature is that the bright red punctate scarlatinal rash is located on a red background, which gives the impression of a general confluent redness. Pressing on the skin leaves a white line . The rash may be spread over the whole body, but there is always a clean (white) area of skin between the upper lip and nose, and also the chin. Itching is much less pronounced than with chicken pox.
Rash lasts up to 2 to 5 days. The manifestations of sore throat persist a little longer (up to 7-9 days).
Scarlet fever is usually treated with antibiotics because the causative agent of scarlet fever is a germ that can be eliminated with antibiotics and strict adherence to bed rest . Also very important is the local treatment of angina and detoxification (removal of toxins from the body that are formed during the vital activity of microorganisms - for this they give plenty of drink). Vitamins, antipyretics are shown. Scarlet fever also has enough serious complications . Before the use of antibiotics, scarlet fever often resulted in the development of rheumatism with the formation of acquired heart defects or kidney disease. Currently, subject to well-prescribed treatment and careful adherence to recommendations, such complications are rare.
Almost exclusively children suffer from scarlet fever, because with age a person acquires resistance to streptococci. Those who have been ill also acquire strong immunity.
Note for parents.
Whooping cough is an acute infectious disease characterized by a long course. The hallmark of the disease is a spasmodic cough.
The mechanism of infection transmission is airborne. A feature of whooping cough is the high susceptibility of children to it, starting from the first days of life.
From the moment of contact with a whooping cough patient until the first signs of the disease appear, 3 to 15 days pass. Whooping cough feature is a gradual increase in cough within 2 to 3 weeks after its onset.
Typical signs of whooping cough:
- · persistent intensifying cough, gradually turning into spasmodic cough attacks (a series of coughing shocks rapidly following each other on one exhalation) with a convulsive breath, accompanied by a whistling lingering sound. In infants, such a cough can lead to respiratory arrest. Attacks of coughing are worse at night and end in the release of a small amount of viscous sputum, sometimes vomiting;
- puffiness of the face, hemorrhages in the sclera;
- ulcer on the frenum of the tongue (due to injury from the edges of the teeth, since during a coughing fit the tongue protrudes to the limit, its tip bends upward).
Whooping cough is often complicated by bronchitis, otitis media, pneumonia, rectal prolapse, umbilical and inguinal hernias.
After having had whooping cough for a long time (several months), coughing fits may return, especially if the child catches a cold or during physical exertion.
The only reliable prevention against pertussis is vaccination with DTP, a vaccine included in the National Immunization Schedule. Parents' fears about the harmful effects of the vaccine are unfounded. The quality of the DTP vaccine is not inferior in its properties to vaccines produced in other countries.
Memo for parents.
Acute intestinal infections is a large group of diseases that occur with more or less similar symptoms, but can be caused by a huge number of pathogens: bacteria, viruses, protozoa.
In summer, the number of intestinal infections in children inevitably increases. There are several reasons for this.
Firstly, , in summer a large amount of raw vegetables, fruits and berries are consumed, on the unwashed surface of which a huge number of microbes, including potentially dangerous ones, live.
Secondly, , children spend a lot of time outdoors in the summer, and not always even their parents remember that eating with clean hands is a mandatory rule .
The third reason : in the summer, getting into foodstuffs (dairy products, meat, fish, broths), some pathogens multiply at a tremendous speed and quickly reach the amount that successfully breaks through the protective barriers of the gastrointestinal tract.
From the moment the pathogen enters the gastrointestinal tract to the onset of the disease, it can take from several hours to 7 days.
The disease begins with fever, malaise, weakness, lethargy. Appetite is sharply reduced, nausea, vomiting quickly joins. The chair is liquid, frequent with impurities. The consequence of fluid loss is dryness of the mucous membranes and skin, facial features are sharpened, the child loses weight, urinates little. Painful facial expression. If your child has the above signs of illness, call the doctor immediately. Self-treatment not allowed .
Prevention of intestinal infections requires strict adherence to general hygiene measures in the home, when preparing food and while eating.
During the summer, all foodstuffs should be protected from flies. Ready food should be stored in the refrigerator: at a low temperature, even if microbes get into the food, they will not be able to multiply. The disease can also be caused by illegibility when buying products that are eaten without heat treatment - from the hands, outside the markets, where they do not pass sanitary control. When swimming in open water, in no case should water be swallowed. If you eat on the beach, wipe your hands with at least special wet wipes.
And remember that parental example is the best way to teach a child.
Parent Guide .
Tuberculosis is a chronic infectious disease caused by mycobacterium human tuberculosis, affecting mainly the respiratory organs, as well as all organs and systems of the body.
The source of infection for is people with tuberculosis. The most common is the air way of infection. Transmission factors are nasopharyngeal mucus, sputum and dust containing bacteria.
Reproduction of tuberculosis bacteria in the child's body leads to significant functional disorders with symptoms of intoxication: irritability appears or, conversely, lethargy, fatigue, headache, sweating. With a long course of the disease, the child loses weight, the skin becomes pale, and there is a tendency to inflammatory diseases. For children, a reaction from the lymph nodes is typical: they increase in size, become dense. If left untreated, the disease can progress to more severe forms.
For the diagnosis of tuberculosis intoxication, it is important to determine infection using tuberculin tests , and for children from 12 years old - also using fluorography.
It is very important for the prevention of tuberculosis : lead a healthy lifestyle, strictly observe sanitary and hygienic rules: wash hands before eating, do not eat unwashed vegetables and fruits, as well as dairy products that have not passed sanitary control, eat well, play sports, pay attention to changes in health status.
An important point for the prevention of tuberculosis is the annual Mantoux test, which gives a positive result when pathogenic bacteria enter the child's body.
Rash in children. We understand the reasons.
Rash in children. We understand the reasons. 8 812 380 02 38Saint-Petersburg
Make an appointment
Tretyakova Daria Aleksandrovna
Pediatrician
In the life of every parent, suddenly comes a moment, late, or in the life of every parent , some pimples are found. It's a rash. A rash is any change on the skin. It occurs in so many diseases and conditions, some of them very dangerous.
Let's try to figure out what kind of rash, in what cases it appears, what is accompanied and how mom and dad should behave so that it passes faster.
Let's start with the simplest - insect bites. First of all, mosquitoes. As a rule, this rash is surprising in early spring and late autumn, when mosquitoes are not yet remembered or already forgotten. In modern winter conditions, mosquitoes can live indoors (for example, in the basement) almost all year round. Of all family members, the most “tasty” for mosquitoes are small children.
Parents notice skin changes in the morning after the child wakes up. Mosquito bites are characterized by the appearance of pink or reddish spots mainly on open areas of the body: hands, forearms, feet, lower legs, i.e. those parts of the body that are not covered by pajamas, and the presence of elements on the face is mandatory, or, sometimes, on one half of it (in the event that the child slept on his side). Most often, this rash is accompanied by itching, but not very strong. The general condition of the child does not suffer. He behaves as usual - plays, runs, scatters things, watches cartoons and eats with appetite. If the child is not allergic to mosquito bites, then they do not require special treatment. It is enough to turn on the fumigator in the children's room (now there are special, for children), and the problem will be solved by itself. In the case of a severe allergic reaction, accompanied by severe swelling, redness, severe itching, it is necessary to give the child an antiallergic agent (for example, suprastin). You can treat bites with drugs such as "Psilobalm" or "Fenistil-gel", which relieve swelling and irritation.
Another fairly common situation in which a rash occurs is an allergic reaction. Typically, this is a food allergy. There are children with allergies from early childhood. Parents of such children know exactly what kind of food you can give your child and what not. And they know very well how to take care of the skin in this situation. Now I would like to elaborate on the problem of the sudden development of allergies in a previously healthy child. This situation can develop when eating previously unfamiliar foods, exotic fruits, vegetables, seafood. Or in the event that the usual dishes are prepared in a special way, using a large amount of spices and aromatic additives. Or if your child, having lost control, ate a pack of chips, snacked on tangerines, chocolates and washed it all down with a carbonated drink.
An allergic reaction occurs rather quickly. On the skin of the whole body or certain areas (cheeks, buttocks, behind the ears), red spots appear, irregular in shape, prone to fusion and accompanied by severe itching. The general condition of the child may change: he may be lethargic or vice versa, too excited. Sometimes there is vomiting or loose stools. But more often the child feels good, but it itches a lot. How to help the baby in this situation? First of all, it is necessary to exclude from his diet foods that cause an allergic reaction, even if they are very tasty and he loves them very much. Then you need to give the child sorbents - drugs that will remove the allergen from the child's body. These include activated charcoal, smecta, zosterin-ultra, filtrum. It is mandatory to take antiallergic drugs (all the same suprastin or other drugs from this group). "Fenistil-gel" and a moisturizer are applied to the skin. It would be very nice to see a pediatrician or dermatologist.
An allergic reaction can also occur when the skin comes into contact with certain substances, such as washing powder, fabric softener, etc. In this case, the rash appears only on those areas that are in direct contact with the allergen. The tactics of the parents' behavior in this case is similar to the tactics for food allergies. Additionally, the substance that caused the reaction should be removed from the skin - rinse under running water.
Now it is necessary to dwell on a large group of infectious diseases accompanied by a rash.
Chicken pox (chicken pox).
The onset of the rash is usually preceded by mild malaise, and symptoms of mild acute respiratory infections may occur. Then a rash appears. At first it is not much - a few red spots. Every day more and more new spots appear, and the old ones turn first into a papule - a “tubercle” that slightly protrudes above the skin, then into a bubble with transparent contents, and finally, the bubble dries up and a crust forms, which after a while disappears. From the moment the first spot appears until the last crust falls off, about 10-15 days pass, during which the sick child is contagious. The chickenpox rash is spread all over the body, including the scalp and mucous membranes (mouth, eyes, genitals). The appearance of a rash with chickenpox is accompanied by itching, sometimes quite severe. Therefore, you can use suprastin, fenistil gel or psilobalm already known to you.
Rubella.
With rubella, the rash appears almost simultaneously all over the body, but is more pronounced on the face, chest and back. It looks like small pale pink spots, almost the same size. The rash is profuse. Disappears without a trace within 4 days. A characteristic sign of rubella is an increase in the occipital lymph nodes. All this is accompanied by mild symptoms of ARI. There is usually no specific treatment for rubella. But all children at the age of 1 year are recommended to be vaccinated against rubella.
Scarlet fever.
The disease begins acutely with high fever, sore throat when swallowing, tonsillitis. The tongue at the beginning of the disease is densely coated with a white coating, then it becomes bright red, shiny. A rash appears a few hours after the onset of the disease on the trunk, limbs, with thickening in the natural folds of the skin (armpits, inguinal region). Rash pink punctate. At the same time, the area around the mouth remains pale. After the disappearance of the rash at the end of the first - at the beginning of the second week of the disease, peeling appears on the palms and feet. The disease is quite serious, because. leaves behind complications in the form of lesions of the heart and kidneys. It requires the mandatory prescription of antibiotics and a period of dispensary observation with mandatory monitoring of blood and urine tests.
Measles.
Measles rash appears on the 4th-5th day of illness against the background of strongly pronounced signs of acute respiratory infections (cough, runny nose, conjunctivitis, fever) and rashes within 3-4 days. The first elements of the rash appear on the face, upper chest. On the second day, they spread to the trunk, and on the third - to the upper and lower limbs. It looks like small red spots that tend to merge. It is now rare, thanks to the immunization of children at the age of 1 year.
"Sudden exanthema", "roseola" or "sixth disease".
Manifested by high, up to 39C, temperature for 4-5 days with relatively good health. Then the temperature returns to normal, and a pale pink rash appears all over the body. After the rash appears, the child is not contagious. Very often, this rash is mistaken for an allergic reaction to antipyretic drugs.
Meningococcal disease and meningococcal sepsis is a deadly disease.
Manifested by a very high temperature, severe general condition of the child, which worsens every hour, vomiting, impaired consciousness. Against the background of high temperature, the child develops a rash (maybe only a few elements), which does not disappear with pressure. If you see such a picture in a child, you should immediately call an ambulance.
In addition to these diseases, a rash on the body occurs with herpes infection - in the form of vesicles, with infectious mononucleosis - with the appointment of antibiotics from the amoxicillin group, with pseudotuberculosis and yersiniosis - in the form of "socks" and "gloves" and many others.
As a rule, the rash in various infections is quite typical and additional laboratory examination for diagnosis is not required.
In almost all infectious diseases, in addition to a rash, there is a high (or not so) temperature, general malaise, loss of appetite, chills. It may hurt your head, or your throat, or your stomach. Have a runny nose, or cough, or diarrhea.
In addition to infections, the rash occurs in diseases of the blood or blood vessels. In these cases, the appearance of a rash is provoked by injuries, sometimes very minor. The rash looks like large or small hemorrhages (bruises) and requires additional examination for an accurate diagnosis.
In conclusion, I would like to once again draw the attention of parents to the fact that there is no need to try to understand what kind of rash the child has. Call a doctor. And most importantly, do not draw on this rash with fucorcin, iodine or brilliant green. After you satisfy your drawing needs, no doctor will ever guess what was really there.
Request a call from the call center
Thank you, your application has been accepted and is being processed
Thank you for contacting us!
Our specialist will contact you during the day to clarify the details and make an appointment.