Milk not letting down
What You Should Know About Your Let Down Reflex
Written by WebMD Editorial Contributors
In this Article
- How Does the Let Down Reflex Work?
- What Are Signs of a Good Let Down?
- Complications of the Let Down Reflex
When your baby first latches on to nurse, they don’t actually get much milk at first. Instead, their suckling sends a message to your body to release the milk stored in your breasts. The strength and timing of the let down reflex, also called the milk ejection reflex, varies from mother to mother.
How Does the Let Down Reflex Work?
If milk came out of your breasts instantly when your baby latched on, you’d probably leak constantly. Instead, your breasts store the milk until it’s needed. Most often, your let down reflex is triggered by a particular suckling motion your baby makes to stimulate milk production.
The let down reflex is a physiological response to your baby’s sucking. They stimulate small nerves in the nipple, which causes prolactin and oxytocin to produce milk and let down milk, respectively. The reflex is often accompanied by a tingling sensation in the nipple, but not all women experience that.
If you pay attention to your baby’s nursing patterns, at first their suckling will be faster and shallower to stimulate the release of milk. Once your milk lets down and your baby is drinking, their suckles will be deeper and longer. If they nurse longer and need more milk, they may adjust how they suck to stimulate more milk flow.
Other let down triggers. Since your brain is wired to care for a newborn, other things may trigger the let down reflex. If your baby cries, or if you hear any baby cry, your milk may let down in response. If you go too long without nursing and your breasts get too full, your let down reflex may trigger to relieve the pressure.
Strong emotions may also trigger a let down of milk. If you are feeling intensely stressed, angry, or sad, your body may take that as a sign that you need to nurse your baby or release milk to alleviate pressure.
If your milk is not letting down, you can physically stimulate the nipple to allow let down. Try gently rolling your hand down your breast toward the nipple, then massage gently. It can also help to relax and think about your baby.
What Are Signs of a Good Let Down?
Breastfeeding is wonderful for your baby, but it is often full of doubts and questions. Are you producing enough milk? Are you doing it right? This extends to the let down reflex, too. You may wonder if your let down is strong enough or too strong.
Here are signs of a healthy, functioning let down response:
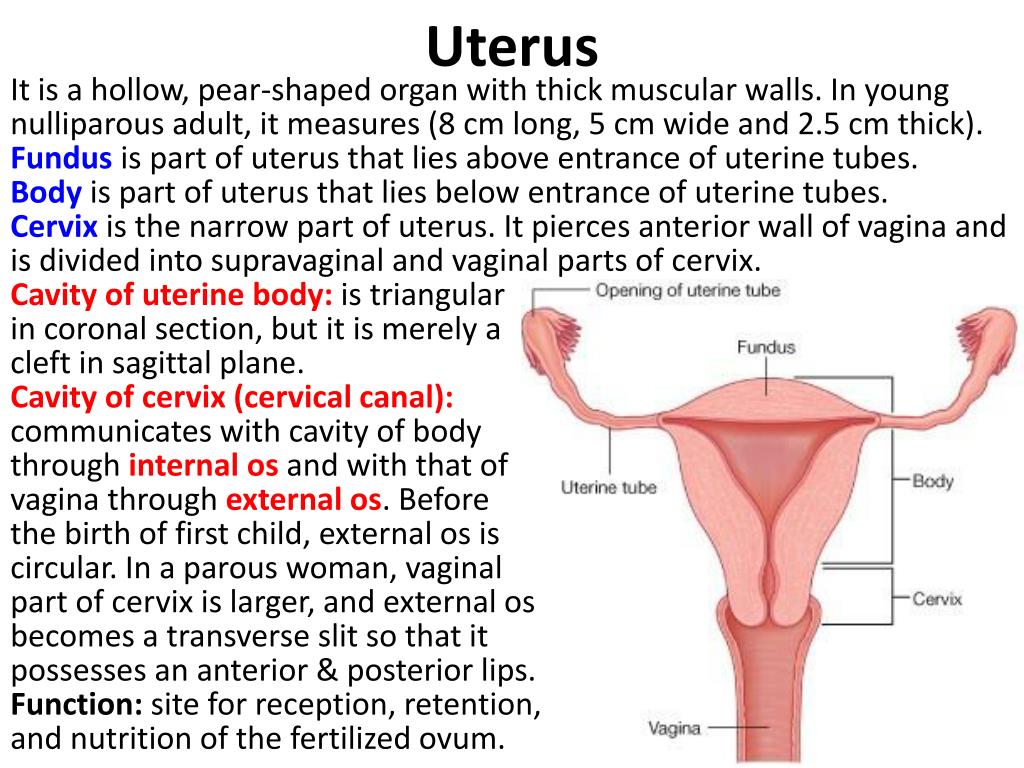
Uterine cramps. You may notice that your uterus cramps during a let down in the days following birth. This is natural and nothing to be concerned about. As with menstrual cramps, for some the cramps are mild and barely noticeable, while for others the contractions can be more painful.
Change in sucking pattern. You may notice a change in your baby’s sucking pattern during a nursing session. Their suckle will go from being short and fast to long and slow once milk lets down. If they need more milk, their sucking may change again to encourage another let down.
Their suckle will go from being short and fast to long and slow once milk lets down. If they need more milk, their sucking may change again to encourage another let down.
Your feelings. Moms often report that they feel very relaxed and even sleepy when their milk lets down. This is a side effect of the oxytocin released during let down. You may also feel suddenly thirsty, which is your body’s way of preparing to replace the milk being removed during a nursing session.
Complications of the Let Down Reflex
Oversupply milk ejection reflex. A powerful let down is often accompanied by an oversupply of milk, sometimes called oversupply milk ejection reflex (O-MER). When your let down happens, you may notice that your baby sputters, coughs, and even chokes on your milk. Your baby may bite down to slow the milk flow. You may leak when not nursing or notice that your baby has more frequent but short feedings if you have an oversupply.
If this happens, keep a bib or cloth handy to catch your milk when it first lets down so that your baby doesn’t choke. After a moment when the let down slows, you can try latching your baby again. You can also restrict your milk flow by squeezing your areola during breastfeeding.
After a moment when the let down slows, you can try latching your baby again. You can also restrict your milk flow by squeezing your areola during breastfeeding.
Talk to your doctor about safe ways to decrease your oversupply so that your let down is less strong.
Dysphoric milk ejection reflex. In some women, breastfeeding can create a negative physiological response, leading to negative emotions like guilt, anxiety, depression, and sadness. It is usually an isolated response that occurs only when you first let down your milk and into the first few minutes of breastfeeding. This is called dysphoric milk ejection reflex (D-MER) and is different from postpartum depression.
There is still more research needed on the causes and effects of D-MER. Talk to your doctor if you are struggling with negative emotions during breastfeeding.
Weak let down. You may have a weak let down if your baby seems frustrated while nursing. They may not be getting enough milk, or they may not be getting milk as fast as they want it. Using a breast pump can supplement less successful nursing sessions.
Using a breast pump can supplement less successful nursing sessions.
When pumping, look at photos and videos of your baby to try and encourage a let down. And just as you do when breastfeeding, try to relax. Take deep breaths and think about your little one, letting go of any stress.
Let-down Reflex: Too slow? • KellyMom.com
By Kelly Bonyata, BS, IBCLC
- Is my let-down functioning properly?
- Possible causes of slow let-down
- Let-down as a conditioned reflex
- Let-down cues that have proven helpful
- Additional Information (links)
- Relaxation and Visualization Exercises (links)
Is my let-down functioning properly?
It is normal for let-down not to feel as strong as your baby gets older. Some mothers never feel let-down, and some stop feeling the let-down sensation as time goes by. This does not necessarily indicate that let-down is not taking place.
Reliable signs of a healthy, functioning let-down include:
- In the first week or so, mother may notice uterine cramping during letdown.
- Baby changes his sucking pattern from short and choppy (like a pacifier suck) at the beginning of the feeding to more long, drawing, and rhythmic a minute or so into the feeding.
- Mother may have a feeling of calm, relaxation, sleepiness or drowsiness.
- Mother may have a strong sensation of thirst while breastfeeding.
- Baby is swallowing more often. A swallow sounds like a small puff of air coming out the baby’s nose and you can usually see the muscle moving in front of the baby’s ear, giving the baby the appearance of his earlobes subtly wiggling.
Occasionally, mothers will also experience other symptoms during let-down, including itching, nausea, headaches, or negative emotions.
.
Possible causes of slow let-down
It’s quite normal for a mother to have a harder time letting down when pumping than when nursing. The milk may be there, but you may have a hard time letting down and “releasing” the milk. Some mothers also have a let-down which is not functioning properly when baby is nursing.
Many things can be the cause of a slow or inhibited let-down: anxiety, pain, embarrassment, stress, cold, excessive caffeine use, smoking, use of alcohol, or the use of some medications. Mothers who have had breast surgery may have nerve damage that can interfere with let-down. In extreme situations of stress or crisis, the release of extra adrenaline in the mother’s system (the “fight or flight” response) can reduce or block the hormones which affect let-down.
Sometimes a cycle is created, where baby fusses and pulls off because the let-down is slow, which makes mom tense up, which makes the let-down even slower, etc. You can use relaxation techniques and let-down cues to break this cycle.
Let-down as a conditioned reflex
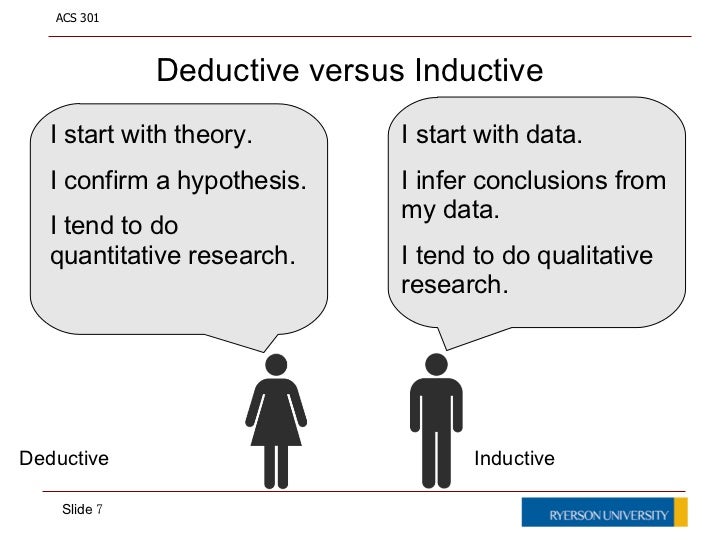
Let-down is partially a conditioned reflex, or one acquired as a result of repeated “training.” The pioneer of research into what he called conditioned reflexes was the Russian neurophysiologist Ivan Pavlov.
A typical experiment of Pavlov’s was as follows: On numerous occasions a bell is rung just before a dog is fed. The dog salivates as usual on receiving its food. Then the bell is rung without any food being presented. The dog salivates in response to the bell ringing.
The dog salivates as usual on receiving its food. Then the bell is rung without any food being presented. The dog salivates in response to the bell ringing.
Let’s put this in terms of nursing. Use a “let-down cue” just before you nurse (for example, deep breathing or drinking a cup of tea). Your milk then lets down in response to baby nursing. Once you have established a conditioned reflex, you will begin to let-down in response to the let-down cue, without baby needing to nurse (or nurse as long).
In Pavlov’s terms:
- the food (nursing) is an unconditioned stimulus
- the salivation (let-down) in response to the food (nursing) is an unconditioned reflex
- the sound of the bell (let-down cue) is the conditioned stimulus
- the salivation (let-down) to the stimulus of the bell (let-down cue) alone is the conditioned reflex.
Pavlov also found that:
- It is much easier to form a conditioned reflex if the unconditioned stimulus follows the conditioned one (i.
 e. the food follows the bell)
e. the food follows the bell) - It is easier to form a conditioned reflex if the conditioned stimulus (bell) occurs very close in time to the unconditioned stimulus (food)
- The intensity of the stimuli is important – a dog salivates more if trained on larger pieces of food; and it also salivates more in response to a louder bell
Transferring this to nursing and let-down, we can surmise that:
- Your let-down cue should be used directly before and just as you begin nursing.
- Intensity makes a difference: Using a couple of different nursing cues at the beginning of nursing (for example, sitting down, getting a drink of water, and doing some deep breathing) should work better than just sitting down to nurse.
While you’re having problems with let-down, it may be helpful to try to nurse in as close to the same setting and same circumstances every time, or have at least one thing that you do that’s the same every time you nurse (deep breathing, visualization, the same drink in the same cup, etc.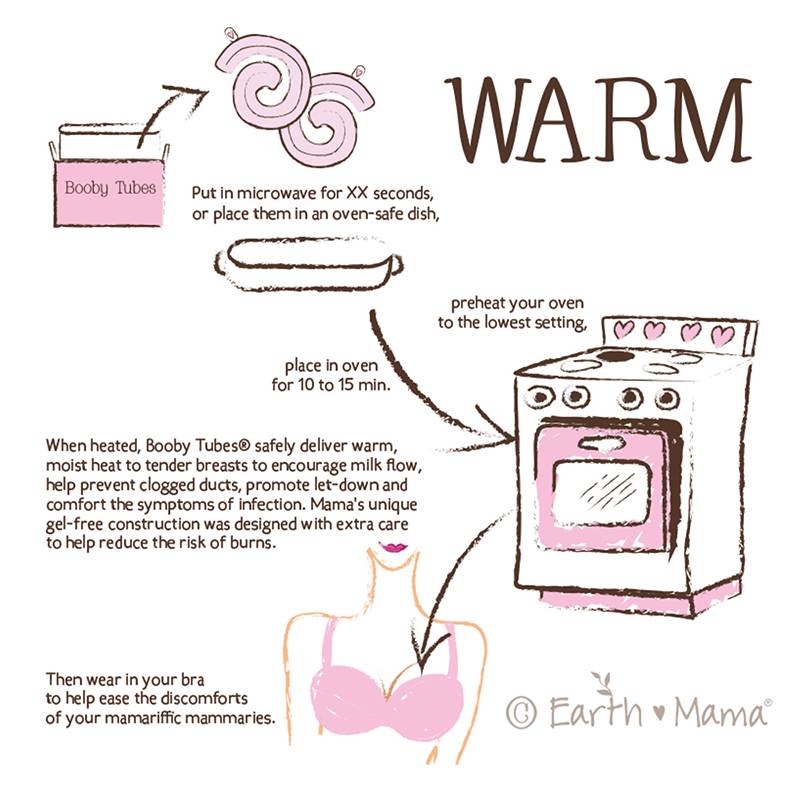 ). If you begin routinely using a few of these let-down cues, your let-down should kick right back in.
). If you begin routinely using a few of these let-down cues, your let-down should kick right back in.
Let-down cues that have proven helpful
Use all of your senses to facilitate let-down. Concentrate on the sight, sound, smell and feel of your baby. Have a certain beverage that you drink (the sense of taste) at the beginning of every nursing session, have a certain song that you listen to, etc.
Directly before nursing:
- Take a warm shower or bath prior to nursing.
- If you are in any pain, consider taking some Advil or Tylenol about 30 minutes before you expect to nurse. Pain can cause stress and inhibit let-down.
- Choose a calm, less distracting setting for nursing.
- Turn on some music that you enjoy.
- Undress baby to his diaper and yourself from the waist up to increase skin-to-skin contact.
- Get something to drink, like a glass of water or a cup of tea.
- Sit in a comfortable chair with arm support and good back support or better, nurse while lying down.

- Get in a warm bath with baby and nurse there.
- Before putting baby to breast, massage your breasts and do some nipple rolls and gentle tugging. Moist heat on the breasts should be helpful, too. See “Assisting the Milk Ejection Reflex” in this information on the Marmet technique of manual expression.
- Reverse pressure softening helps let-down for some moms.
During nursing:
- Deep breathe or use other relaxation techniques at the beginning of a feeding, like the techniques that are taught for childbirth
- Singing or humming can also speed let-down.
- Use visualization. Take several deep breaths and close your eyes as you begin. Try to visualize and “feel” what the let-down response feels like for you (if you normally feel anything). Some women imagine their milk flowing or use images of waterfalls. Some women concentrate on looking at baby’s soft little hand moving at mom’s breast, with fingers curled under.
 Some women use visualizations such as being on the beach or any other relaxing place. Use all five senses; imagine the sights, smells such as the salt air, sensations such as the feel of the sand under you or the warmth of the sun on your skin, imagine tastes and what you might hear too. An excellent book on visualization techniques is Mind Over Labor by Carl Jones.
Some women use visualizations such as being on the beach or any other relaxing place. Use all five senses; imagine the sights, smells such as the salt air, sensations such as the feel of the sand under you or the warmth of the sun on your skin, imagine tastes and what you might hear too. An excellent book on visualization techniques is Mind Over Labor by Carl Jones. - The opposite can also be helpful: watch TV, talk on the phone, read a book, etc. – whatever will relax you and get your mind off it.
- Place a heating pad on your shoulders and back. Get someone else to massage your back and shoulders before and while you nurse.
- Switch nurse: move baby back and forth frequently between breasts until let-down occurs
- Continue to massage and use breast compression as you nurse.
Additional suggestions if you’re pumping while separated from baby:
- Look at a picture of your baby (nursing, if possible).
- Try listening to a tape recording of your baby fussing before nursing and/or feeding sounds.
 Use a portable tape player with headphones if needed. Or just visualize what he sounds like when he’s ready to nurse.
Use a portable tape player with headphones if needed. Or just visualize what he sounds like when he’s ready to nurse. - Put a sleeper or t-shirt or blanket that baby has worn in a ziplock bag. Open it up when ready to pump – smell and touch it.
- One study has shown that the moms of hospitalized babies who listened to guided relaxation or soothing music while pumping had an increased pumping output. When mom listened to a recording that included both music and guided relaxation while pumping, in addition to looking at photos of her baby, pumping output was increased even more. In this study, the interventions led to moms producing 2-3 times their normal pumping output. Milk fat content also increased for these moms in the early days of the study. (Reference: Keith DR, Weaver BS, Vogel RL. The effect of music-based listening interventions on the volume, fat content, and caloric content of breast milk-produced by mothers of premature and critically ill infants. Adv Neonatal Care.
 2012 Apr;12(2):112-9.)
2012 Apr;12(2):112-9.)
Additional Information
- Marmet technique of manual expression by Chele Marmet. Scroll down to “Assisting the Milk Ejection Reflex”
- Fennel is sometimes used to help elicit let-down
Relaxation and Visualization Exercises
- Relaxation Techniques for pumping, by Diane O’Brien Juve, from the Working Cow website
- Elicitation of the Relaxation Response from the Mind Body Medical Institute
- Progressive muscular relaxation script from the Centre for Clinical Interventions (Australia)
- Relaxation and desensitization scripts by David Ross, College of Lake County
Why the cow does not give milk after calving - Tips and features
The moment has come when the cow gave birth to a calf. Like a person, she does not produce milk for the first week after childbirth, but colostrum. Without colostrum, the calf will not survive, and it is not suitable for the human body. But you can’t stop milking a cow; milking begins immediately after childbirth. The uterus is milked, as usual, three times a day, but very carefully so that the udder does not hurt. If this is not done, the cattle will not give much milk. Continue reading →
The uterus is milked, as usual, three times a day, but very carefully so that the udder does not hurt. If this is not done, the cattle will not give much milk. Continue reading →
Milk quantity at first calving
A cow giving birth for the first time cannot give much milk, although this depends on her future milk production. A small amount of milk in 1 period after childbirth is due to the laws of nature: the female produces as much milk as the calf needs, and not a gram more.
In the first days, a cub does not need much food, a heifer can only have 3-4 liters. colostrum. But over time, the calf will need more food. Despite the fact that a cow giving birth for the first time gives one and a half times less milk than an adult, she will fully provide the newborn with food. With the growth of the calf, they are transferred to feed, and lactation is declining.
From the first days of calving, the owner must imitate the lack of food for the cub and milk the cattle 3 times a day. This makes it possible to stock up on colostrum, which has a huge amount of immunoglobulins. The largest milk yields are obtained from those individuals that calved 3 times.
This makes it possible to stock up on colostrum, which has a huge amount of immunoglobulins. The largest milk yields are obtained from those individuals that calved 3 times.
Can a cow give birth if the udder does not fill up?
It happens that the mammary glands of a female do not fill up during calving, but swell. This happens due to hormonal changes, and each organism is different. Therefore, the approaching birth can not always be recognized by the swollen udder. In adult cows, the udder can be poured just before or during calving. Due to hormonal failure, the udder may not swell or fill at all. This is the worst option. Colostrum is released after childbirth in several stages. The production of milk is helped by hormones that the heifer receives with the rest of the mucus, licking the cub. Therefore, it is not necessary to immediately take the newborn from the mother.
Physiological reasons why a cow does not produce milk after giving birth
Sometimes, after calving, the uterus does not produce milk for no apparent reason. This can be explained by some kind of illness, postpartum pathology, "wild" instincts. This is more common in young individuals giving birth for the first time. The heifer "pulls in" the nipples and does not want to be milked. The same thing can happen when a stranger milks her. In this case, it is necessary that a calf be near the cow during the milking period.
This can be explained by some kind of illness, postpartum pathology, "wild" instincts. This is more common in young individuals giving birth for the first time. The heifer "pulls in" the nipples and does not want to be milked. The same thing can happen when a stranger milks her. In this case, it is necessary that a calf be near the cow during the milking period.
There may be a more serious reason for not wanting to produce milk. This is chronic thirst. The point here is not that the owners do not allow the cattle to drink, but that the diet lacks fresh grass, vegetables, ground grains and dietary supplements. Then the animal drinks a lot of water to support itself. With such meager nutrition, even a well-milked cow per day can give out only up to 4 liters. milk. Of course, this amount of food is enough only for a calf.
Also, a heifer does not give milk if she has had mastitis before. Adhesions form in the nipples and milk is difficult to pass. On the first day of calving, the colostrum is very thick and does not pass through the nipple canal.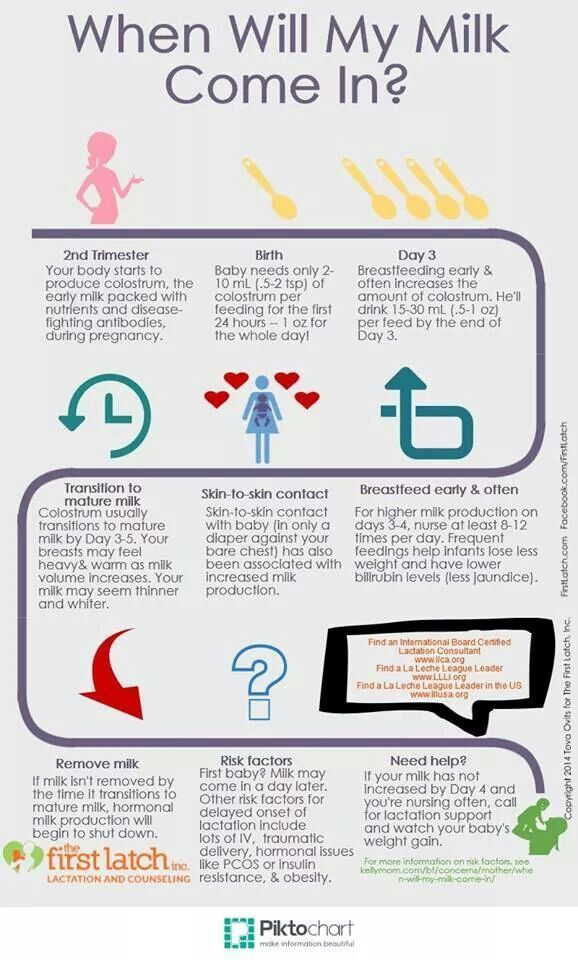 There is no need to despair, only a cub can suck it. If he can’t cope, then it’s worth teaching the heifer to feed other people’s calves. It may be that the uterus also drives away her child, this is because a strong swelling of the mammary glands causes pain from touch.
There is no need to despair, only a cub can suck it. If he can’t cope, then it’s worth teaching the heifer to feed other people’s calves. It may be that the uterus also drives away her child, this is because a strong swelling of the mammary glands causes pain from touch.
The next reason for the lack of milk yield is an unsuitable milking machine. First, the animal may have irregularly shaped nipples. Secondly, the apparatus may be damaged and cause pain to the cow.
Pathologies of milk production after childbirth
There are the following complications after childbirth that lead to lactation disorders:
- abnormal metabolism;
- mastitis;
- hormonal failure;
- brucellosis;
- infections.
There may be little milk after childbirth, even if the food is too dry.
Mastitis
May resolve with severe or mild symptoms. Often the owner notices the disease when the cow has already given birth, and the nipples remain hard and there is no milk. No one does tests on the animal, so the disease is not noticed at the initial stage. But after calving, one must be careful and not neglect the analysis of colostrum from each nipple. On large farms, such studies are always done after each calving, and private traders often neglect them. Only after the results of the analysis, the calf is allowed to suckle the uterus.
No one does tests on the animal, so the disease is not noticed at the initial stage. But after calving, one must be careful and not neglect the analysis of colostrum from each nipple. On large farms, such studies are always done after each calving, and private traders often neglect them. Only after the results of the analysis, the calf is allowed to suckle the uterus.
Incorrect production of hormones
Cattle of any age may have a lack of prolactin, the hormone that produces milk. The production of prolactin depends on the hormone oxytocin. If a person does not have enough of this hormone, he develops symptoms of a mental disorder. The cow, on the other hand, becomes irritable, but often farmers do not pay attention to this, attributing it to the bad “character” of the individual. If there is not enough prolactin in the body, there may not be milk after calving. In this case, injections of oxytocin can help.
Brucellosis
This is the most unpleasant cause of lack of lactation. The onset of the disease is difficult to recognize, the symptoms are invisible, the disease develops slowly. Therefore, it is necessary to do tests from time to time. At the last stage, the female has miscarriages. Pregnancy lasts 9 months, and miscarriage occurs just at 8-9 months. It is urgent to check the cattle for brucellosis if the cow has calved ahead of time and there is no milk. This is not normal calving, the necessary hormones are not produced, and the animal can become seriously ill.
The onset of the disease is difficult to recognize, the symptoms are invisible, the disease develops slowly. Therefore, it is necessary to do tests from time to time. At the last stage, the female has miscarriages. Pregnancy lasts 9 months, and miscarriage occurs just at 8-9 months. It is urgent to check the cattle for brucellosis if the cow has calved ahead of time and there is no milk. This is not normal calving, the necessary hormones are not produced, and the animal can become seriously ill.
Infections
If, after analysis, a cow is found to have an infection (eg Staphylococcus aureus) and inflammation of the mammary glands, antibiotics are prescribed, and udder massage is often performed.
What to do with pathologies of lactation after calving?
Be sure to submit materials for analysis and determine why there is no milk. If the birth went well and on time, there are no mastitis and other visible diseases, then maybe this is a hormone malfunction. In this case, it is worth pricking the hormone oxytocin, which will cause lactation. Too dry or unbalanced nutrition disrupts the metabolism in the body. It will not be possible to quickly fix it, you can only stimulate the pumping of milk.
In this case, it is worth pricking the hormone oxytocin, which will cause lactation. Too dry or unbalanced nutrition disrupts the metabolism in the body. It will not be possible to quickly fix it, you can only stimulate the pumping of milk.
It is worth remembering that the main function of oxytocin is to stimulate uterine contractions during childbirth. An inexperienced person will find it easier to inject intramuscularly or under the skin. If injected subcutaneously, then give a double dose. The consequences of an overdose after oxytocin have not been recorded. With an intramuscular injection, the dose for cattle is 30-60 IU. They do it once. Oxytocin is also administered if the heifer has very weak contractions. The drug helps the release of the placenta after childbirth.
A cow with mastitis is not so easy to cure. A newborn calf is not given colostrum from a sick mother. He is fed milk from another heifer, and the sick one is given a course of antibiotics. Antibiotics can be local and general. If this is a local treatment, then the diseased nipples are smeared with an antibacterial ointment. It is absolutely impossible to give such an udder to a cub.
If this is a local treatment, then the diseased nipples are smeared with an antibacterial ointment. It is absolutely impossible to give such an udder to a cub.
When several teats or the entire udder are damaged by mastitis, it is best to treat the entire body with intramuscular antibiotics. It is necessary to milk low-quality colostrum every 2 hours, and pour it out.
Most calves die in premature births. Calf body samples must be taken to the laboratory for analysis.
If the placenta does not come out completely during normal delivery, this may be a symptom of early brucellosis.
What do veterinarians advise?
It often happens that even a veterinarian cannot understand why a seemingly healthy cow does not give milk. The doctor can make recommendations if there are already clear signs. Usually they do everything the same as in the treatment of mastitis.
When it is clear that a cow is not milking due to edema, she is given a natural diuretic. A decoction of dill or bearberry does not overload the kidneys and liver, and acts gently. But it takes a long time to drink the decoction. A decoction of dill is made from seeds, they have a greater diuretic effect.
A decoction of dill or bearberry does not overload the kidneys and liver, and acts gently. But it takes a long time to drink the decoction. A decoction of dill is made from seeds, they have a greater diuretic effect.
The udder massage is also used at this time. The anterior lobes prominate in the direction of the abdomen, the posterior lobes - from the nipples to the tail. Movements should be from the bottom up, they must be done carefully so as not to cause pain in the animal.
In the last month of pregnancy, the cow is not given concentrates to eat, so that there is no severe swelling. With mastitis, the nipples are treated with Perkutan, a spray for external use. It is also used to disinfect minor wounds and scratches on the udder. In food, milk is used only from healthy shares, to which no medicine has been applied. With Staphylococcus aureus, all milk is milked and poured out; in no case should it be given to a calf.
If the owner of cattle has never encountered such problems, then in order not to harm the animal, it is better to call a veterinarian.
Conclusion
If the first calving cow does not have milk, but looks absolutely healthy, then first of all she is given an injection of oxytocin. Edema is removed with topical medications, proper nutrition and massages. In the event that all manipulations have not led to a result, the help of a veterinarian is required to make an accurate diagnosis.
Breastfeeding in the first month: what to expect
Not sure how to establish lactation and increase milk production? If you need help, support, or just want to know what to expect, read our first month breastfeeding advice
Share this information
The first weeks of breastfeeding are a very stressful period. If at times you feel like you can't handle it, know that you are not alone. Feeding your baby all day long is completely natural and helps produce breast milk, but can be quite tiring at times. Be patient, think about yourself and remember: after the first month, when milk production stabilizes, it will become easier.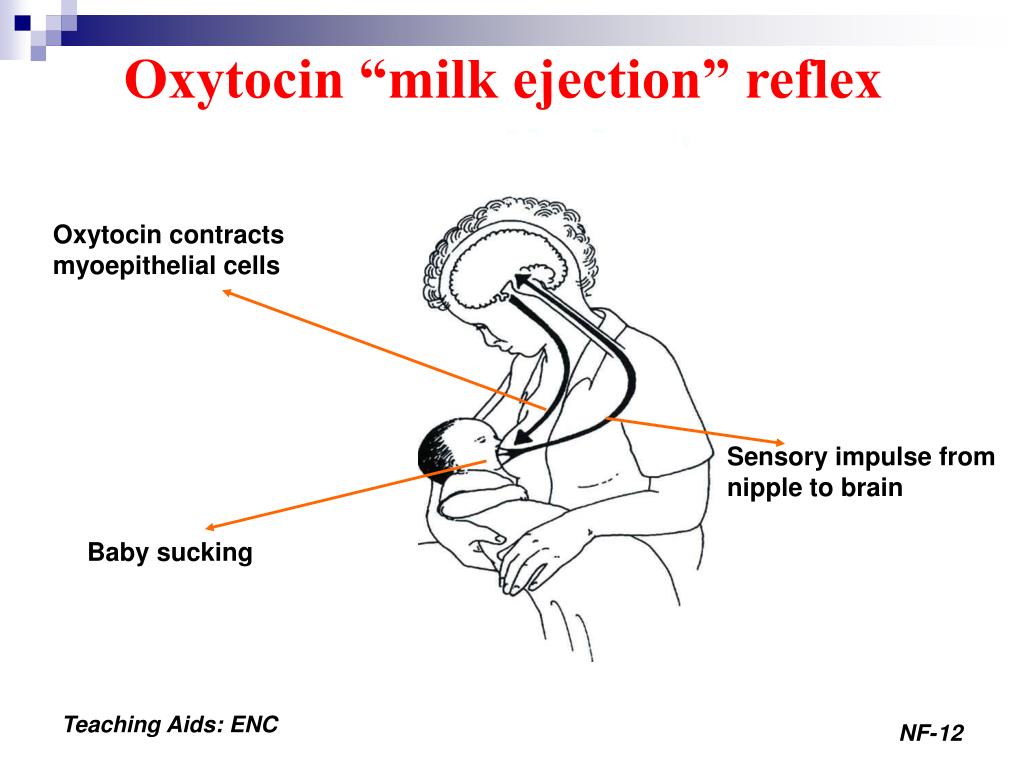
How often should a baby be breastfed?
Babies are born with a small stomach that grows rapidly with increasing milk production: in the first week it is no larger than an apricot, and after two weeks it is already the size of a large chicken egg. 1.2 Let the child eat as much as he wants and when he wants. This will help him quickly regain the weight lost after birth and grow and develop further.
“Be prepared to feed every two to three hours throughout the day. At night, the intervals between feedings can be longer: three to four or even five hours, says Cathy Garbin, a recognized international expert on breastfeeding. Some eat quickly and are satiated in 15 minutes, while others take an entire hour to feed. Do not compare your breastfeeding regimen with that of other mothers - it is very likely that there will be nothing in common between them.
At each feed, give your baby a full meal from one breast and then offer a second one, but don't worry if the baby doesn't take it. When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
When the baby is full, he lets go of his chest and at the same time looks relaxed and satisfied - so much so that he can immediately fall asleep. The next time you feed, start on the other breast. You can monitor the order of the mammary glands during feeding using a special application.
Why does the child always ask for a breast?
The first month is usually the hardest time to breastfeed. But do not think that because the baby is constantly hungry and asks for a breast almost every 45 minutes, then you do not have enough milk.
In the first month, the baby needs to eat frequently to start and stimulate the mother's milk production. It lays the foundation for a stable milk supply in the future. 3
In addition, we must not forget that the child needs almost constant contact with the mother. The bright light and noise of the surrounding world at first frighten the baby, and only by clinging to his mother, he can calm down.
Sarah, mother of three from the UK, confirms: “Crying is not always a sign of hunger. Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body."
Sometimes my kids just wanted me to be around and begged for breasts to calm them down. Use a sling. Place the cradle next to the bed. Don't look at the clock. Take advantage of every opportunity to relax. Forget about cleaning. Let those around you take care of you. And not three days, but six weeks at least! Hug your baby, enjoy the comfort - and trust your body."
Do I need to feed my baby on a schedule?
Your baby is still too young for a strict daily routine, so
forget about breastfeeding schedules and focus on his needs.
“Volumes have been written about how to feed a baby on a schedule, but babies don't read or understand books,” Cathy says. - All children are different. Some people can eat on a schedule, but most can't. Most often, over time, the child develops his own schedule.
Some mothers report that their babies are fine with scheduled feedings, but they are probably just the few babies who would eat every four hours anyway. Adults rarely eat and drink the same foods at the same time of day - so why do we expect this from toddlers?
Offer your baby the breast at the first sign of hunger.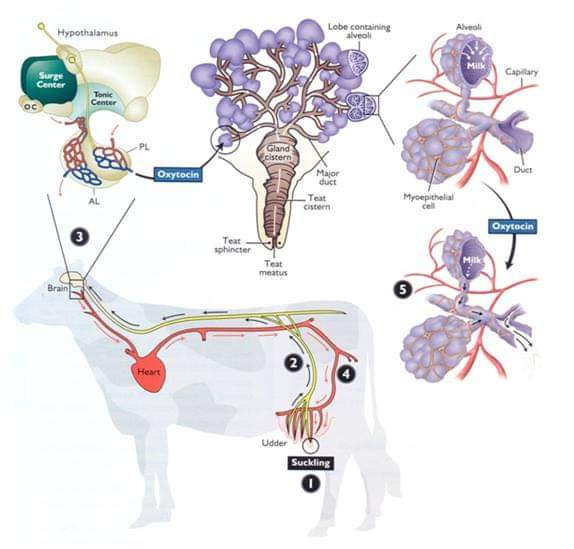 Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. 4
Crying is already the last stage, so be attentive to early signs: the baby licks his lips, opens his mouth, sucks his fist, turns his head with his mouth open - looking for the breast. 4
What is a "milk flush"?
At the beginning of each feeding, a hungry baby actively suckles the nipple,
thereby stimulating the milk flow reflex - the movement of milk through the milk ducts. 5
“Nipple stimulation triggers the release of the hormone oxytocin,” explains Cathy. “Oxytocin circulates throughout the body and causes the muscles around the milk-producing glands to contract and the milk ducts to dilate. This stimulates the flow of milk.
If the flushing reflex fails, milk will not come out. This is a hormonal response, and under stress it may not work at all or work poorly. Therefore, it is so important that you feel comfortable and calm when feeding.
“Studies show that each mother has a different rhythm of hot flashes during one feed,” Kathy continues, “Oxytocin is a short-acting hormone, it breaks down in just 30-40 seconds after formation. Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended.
Milk begins to flow, the baby eats, the effect of oxytocin ends, but then a new rush of milk occurs, the baby continues to suckle the breast, and this process is repeated cyclically. That is why, during feeding, the child periodically stops and rests - this is how nature intended.
The flow of milk may be accompanied by a strong sensation of movement or tingling in the chest, although 21% of mothers, according to surveys, do not feel anything at all. 5 Cathy explains: “Many women only feel the first rush of milk. If you do not feel hot flashes, do not worry: since the child eats normally, most likely, you simply do not understand that they are.
How do you know if a baby is getting enough milk?
Since it is impossible to track how much milk a baby eats while breastfeeding, mothers sometimes worry that the baby is malnourished. Trust your child and your body.
After a rush of milk, the baby usually begins to suckle more slowly. Some mothers clearly hear how the baby swallows, others do not notice it. But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
But one way or another, the child himself will show when he is full - just watch carefully. Many babies make two or three approaches to the breast at one feeding. 6
“When a child has had enough, it is noticeable almost immediately: a kind of “milk intoxication” sets in. The baby is relaxed and makes it clear with his whole body that he is completely full, says Katie, “Diapers are another great way to assess whether the baby is getting enough milk. During this period, a breastfed baby should have at least five wet diapers a day and at least two portions of soft yellow stool, and often more.”
From one month until weaning at six months of age, a baby's stool (if exclusively breastfed) should look the same every day: yellow, grainy, loose, and watery.
When is the child's birth weight restored?
Most newborns lose weight in the first few days of life. This is normal and should not be cause for concern. As a rule, weight is reduced by 5-7%, although some may lose up to 10%. One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. 7.8
One way or another, by 10–14 days, almost all newborns regain their birth weight. In the first three to four months, the minimum expected weight gain is an average of 150 grams per week. But one week the child may gain weight faster, and the next slower, so it is necessary that the attending physician monitor the health and growth of the baby constantly. 7.8
At the slightest doubt or signs of dehydration, such as
dark urine, no stool for more than 24 hours, retraction of the fontanel (soft spot on the head), yellowing of the skin, drowsiness, lethargy, lack of appetite (ability to four to six hours without feeding), you should immediately consult a doctor. 7
What is "cluster feeding"?
When a baby asks for a breast very often for several hours, this is called cluster feeding. 6 The peak often occurs in the evening between 18:00 and 22:00, when many babies are especially restless and need close contact with their mother. Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Most often, mothers complain about this in the period from two to nine weeks after childbirth. This is perfectly normal and common behavior as long as the baby is otherwise healthy, eating well, gaining weight normally, and appears content throughout the day. 9
Cluster feeding can be caused by a sharp jump in the development of the body - during this period the baby especially needs love, comfort and a sense of security. The growing brain of a child is so excited that it can be difficult for him to turn off, or it just scares the baby. 9 If a child is overworked, it is often difficult for him or her to calm down on his own and adult assistance is needed. And breastfeeding is the best way to calm the baby, because breast milk is not only food, but also pain reliever and a source of happiness hormones. 10
“No one told me about cluster feeding, so for the first 10 days I just went crazy with worry - I was sure that my milk was not enough for the baby,” recalls Camille, a mother from Australia, “It was a very difficult period . I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all.
I was advised to pump and supplement until I finally contacted the Australian Breastfeeding Association. There they explained to me what was happening: it turned out that it was not about milk at all.
Remember, this is temporary. Try to prepare dinner for yourself in the afternoon, when the baby is fast asleep, so that in the evening, when he begins to often breastfeed, you have the opportunity to quickly warm up the food and have a snack. If you are not alone, arrange to carry and rock the baby in turns so that you have the opportunity to rest. If you have no one to turn to for help and you feel that your strength is leaving you, put the baby in the crib and rest for a few minutes, and then pick it up again.
Ask your partner, family and friends to help you with household chores, cooking and caring for older children if you have any. If possible, hire an au pair. Get as much rest as possible, eat well and drink plenty of water.
“My daughter slept a lot during the day, but from 23:00 to 5:00 the cluster feeding period began, which was very tiring,” recalls Jenal, a mother from the USA, “My husband tried his best to make life easier for me - washed, cleaned, cooked, changed diapers, let me sleep at every opportunity and never tired of assuring me that we were doing well.
If you are concerned about the frequency of breastfeeding, it is worth contacting a specialist. “Check with a lactation consultant or doctor to see if this is indicative of any problems,” recommends Cathy. “Resist the temptation to supplement your baby with formula (unless recommended by your doctor) until you find the cause. It may not be a matter of limited milk production at all - it may be that the child is inefficiently sucking it.
When will breastfeeding become easier?
This early stage is very special and does not last long. Although sometimes it seems that there will be no end to it, rest assured: it will get easier soon! By the end of the first month, breast milk production will stabilize, and the baby will become stronger and learn to suckle better. 2.3 Any problems with latch on by this time will most likely be resolved, and the body will be producing milk more efficiently, so inflammation and leakage of milk will begin to pass.
“The first four to six weeks are the hardest, but then things start to get better,” Cathy assures. It just needs to be experienced!”
It just needs to be experienced!”
The longer breastfeeding continues, the more benefits it brings, from saving on formula and improving sleep quality 11-13 to boosting your baby's immune system 14 and reducing your risk of certain cancers. 15
“When you feel like you're pushing yourself, try to go from feed to feed and day to day,” says Hannah, a UK mom. “I was sure I wouldn’t make it to eight weeks. And now I have been breastfeeding for almost 17 weeks, and I dare say it is very easy.”
Read the resource Breastfeeding Beyond the First Month: What to Expect
Literature
1 Naveed M et al. An autopsy study of relationship between perinatal stomach capacity and birth weight. Indian J Gastroenterol .1992;11(4):156-158. - Navid M. et al., Association between prenatal gastric volume and birth weight. Autopsy. Indian J Gastroenterol. 1992;11(4):156-158.
2 Neville MC et al. Studies in human lactation: milk volumes in lactating women during the onset of lactation and full lactation AM J CLINL NUTR . 1988; 48 (6): 1375-1386. - Neville M.S. and co -author, "Research of female lactation in lactating women at the beginning and at the peak of lactation." Am F Klin Nutr. 1988;48(6):1375-1386.
3 Kent JC et al. Principles for maintaining or increasing breast milk production. J Obstet , Gynecol , & Neonatal Nurs . 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
4 Australian Breastfeeding Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
- Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
5 Kent JC et al. Response of breasts to different stimulation patterns of an electric breast pump. J Human Lact . 2003;19(2):179-186. - Kent J.S. et al., Breast Response to Different Types of Electric Breast Pump Stimulation. J Human Lact (Journal of the International Association of Lactation Consultants). 2003;19(2):179-186.
6) Kent JC et al . Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3): e 387-395. - Kent J.S. et al., "Amount and frequency of breastfeeding and fat content of breast milk during the day." Pediatrix (Pediatrics). 2006;117(3):e387-95.
7 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
8 World Health Organization. [Internet]. Child growth standards; 2018 [cited 2018 Feb] - World Health Organization. [Internet]. Child Growth Standards 2018 [cited February 2018].
9 Australian Breastfeeding Association . [ Internet ]. Cluster feeding and fussing babies ; - Australian Breastfeeding Association [Internet], Cluster Feeding and Screaming Babies; December 2017 [cited February 2018].
10 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206.- Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
Infant . 2013;9(6):201-206.- Moberg K, Prime DK, "Oxytocin effects on mother and child during breastfeeding". Infant. 2013;9(6):201-206.
11 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet; 2011 Jan 20 [cited 2017 Feb] - Department of Health and Human Services [Internet], "Breastfeeding Facts from the Chief Medical Officer", Jan 20, 2011 [cited Feb 2017]
12 Kendall-Tackett K et al. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. clinical lactation. 2011;1;2(2):22-26. - Kendall-Tuckett, K. et al., "Influence of feeding pattern on sleep duration, maternal well-being and the development of postpartum depression." Clinical Lactation. 2011;2(2):22-26.
13 Brown A, Harries V. Infant sleep and night feeding patterns during later infancy: Association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
Breast Med . 2015;10(5):246-252. - Brown A., Harris W., "Night feedings and infant sleep in the first year of life and their association with feeding frequency, daytime supplementation, and infant weight." Brest Med (Breastfeeding Medicine). 2015;10(5):246-252.
14 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl immunology. 2013;2(4). - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
15 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev . 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies.