Uterus and cervix during pregnancy
Anatomy of pregnancy and birth - cervix
Anatomy of pregnancy and birth - cervix | Pregnancy Birth and Baby beginning of content5-minute read
Listen
Where is the cervix?
The cervix plays a critical role throughout a woman’s life, but never more so than during conception, pregnancy and childbirth. The cervix changes during these events, so it’s important to understand the role of this organ and what these changes mean for you and your baby.
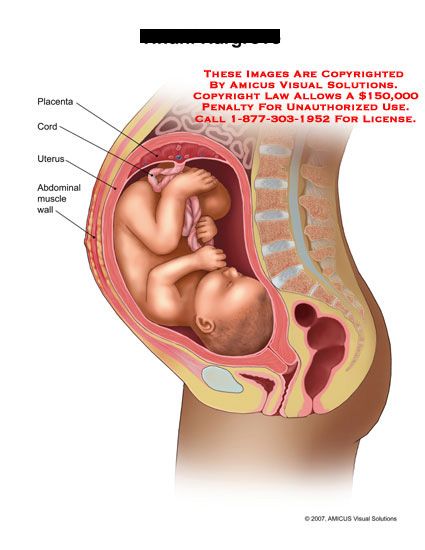
The cervix is the muscular channel or opening that runs between the uterus (also known as the womb) and the vagina. The cervix is located in the pelvis and lies behind the bladder and near the front of the rectum. It is held in its position by tough, flexible ligaments.
Illustration showing the female reproductive system.What does the cervix do in women who are not pregnant?
In women who are not pregnant, the cervix is narrow and firm. Its size, shape and lining undergo subtle changes throughout a woman’s menstrual cycle.
For instance, the cervix has a smooth covering of mucus. When a woman is ovulating, the mucus becomes stretchy and elastic, which helps sperm move and survive following intercourse, and is known as ‘fertile mucus’. When a woman is not ovulating, the mucus takes on a more creamy texture and can be milky or yellow in colour. This change in consistency indicates that sperm are less likely to reach the uterus after intercourse at this time in the menstrual cycle.
The cervix contains a channel, referred to as the 'cervical canal', which also has an important role in women who are not pregnant. Sperm enters the uterus after intercourse and menstrual blood leaves the uterus during menstruation through this channel.
What is the function of the cervix during conception and pregnancy?
The cervix has several important functions during conception.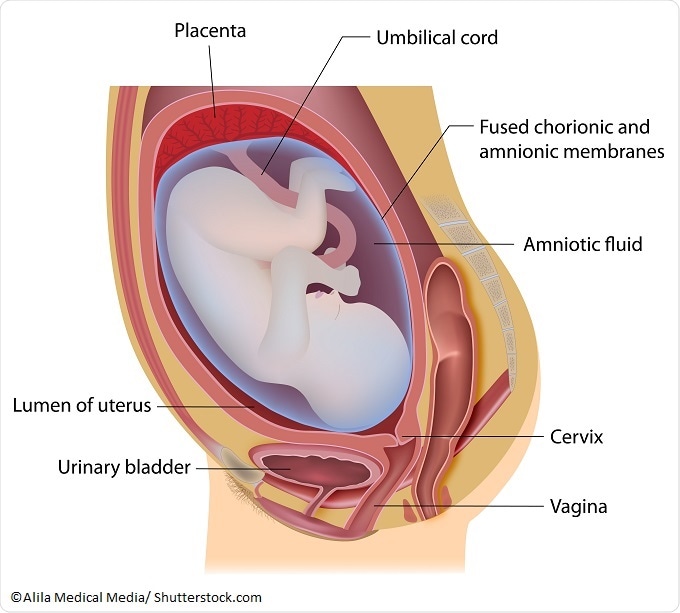 After a woman conceives, the mucus on the surface of the cervix becomes sticky and thick. This stops new sperm and microorganisms, such as bacteria and viruses, from entering the uterus and potentially harming the fetus.
After a woman conceives, the mucus on the surface of the cervix becomes sticky and thick. This stops new sperm and microorganisms, such as bacteria and viruses, from entering the uterus and potentially harming the fetus.
The cervix also plays a crucial role during pregnancy. From conception until just before birth, the cervix protects the growing baby by increasing in size and strength, helping to keep the baby safe and secure in the uterus.
How does the cervix change during labour?
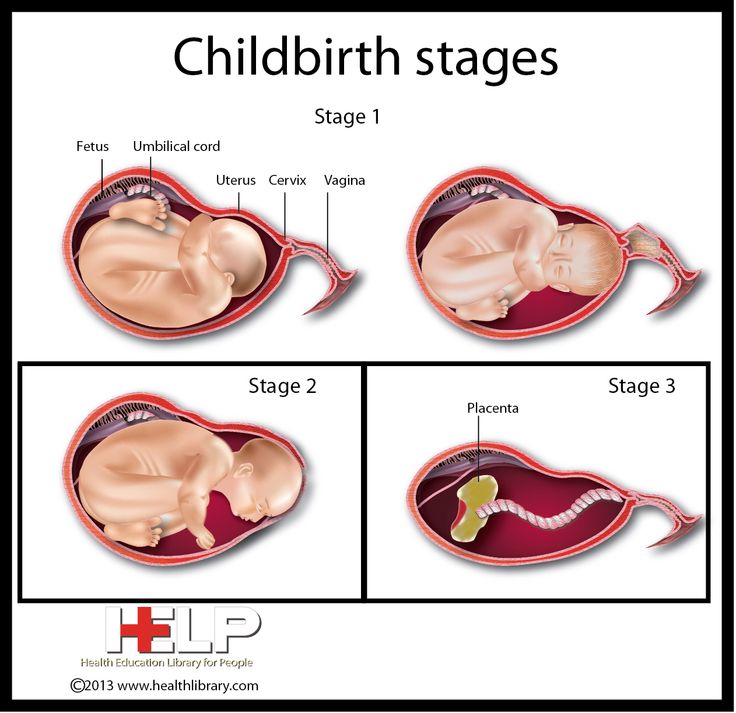
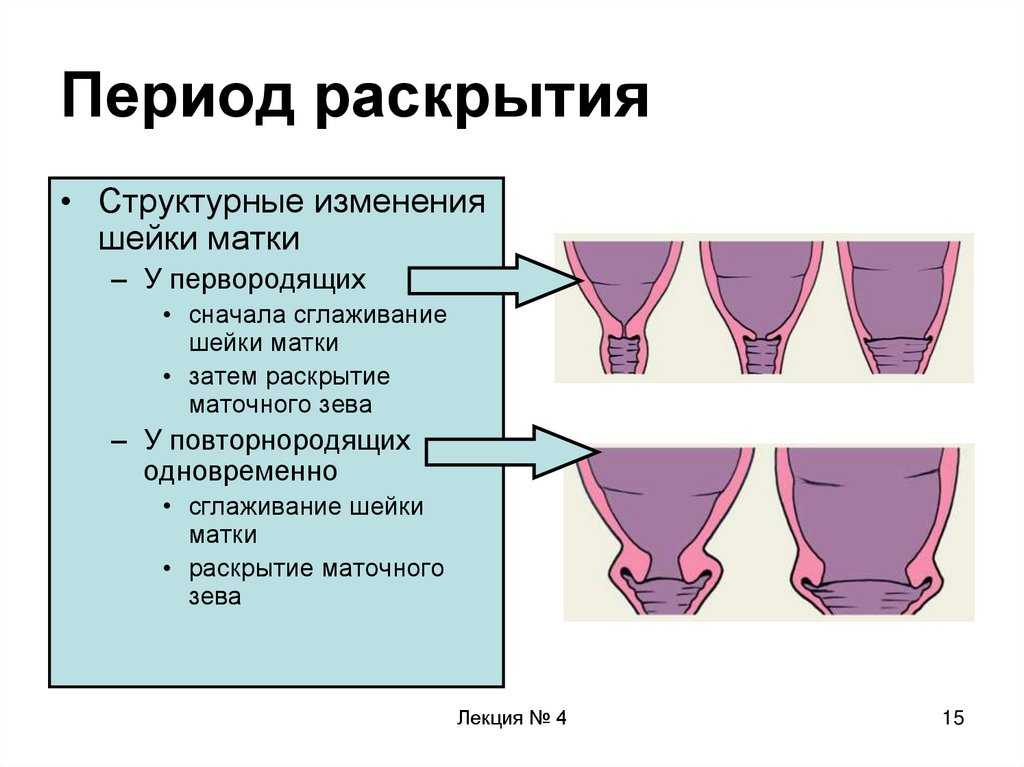
The cervix undergoes dramatic changes during labour in a process known as ‘effacement’ or ‘ripening’. It starts out long and firm, and as labour progresses, it softens, widens and becomes more elastic.
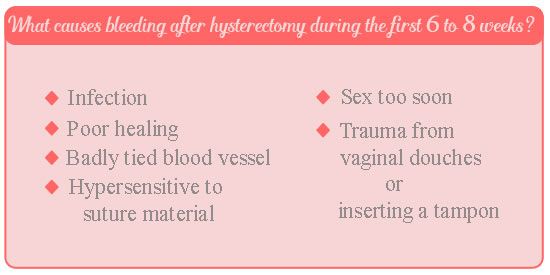
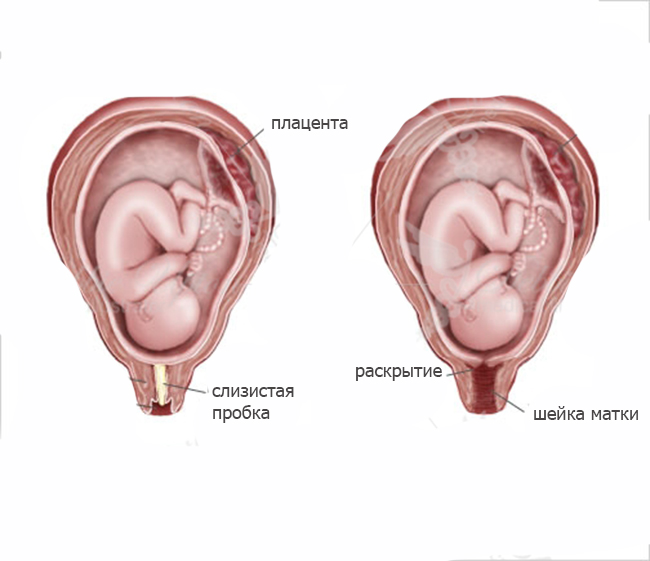
Changes to the cervix are partly triggered by contractions of the muscles of the uterus, which help open the cervix. As the cervix begins to open, you may see a clear, pink, or slightly bloody discharge (sometimes referred to as the 'show'). This is the release of the mucus plug, that sits over the cervical canal during pregnancy.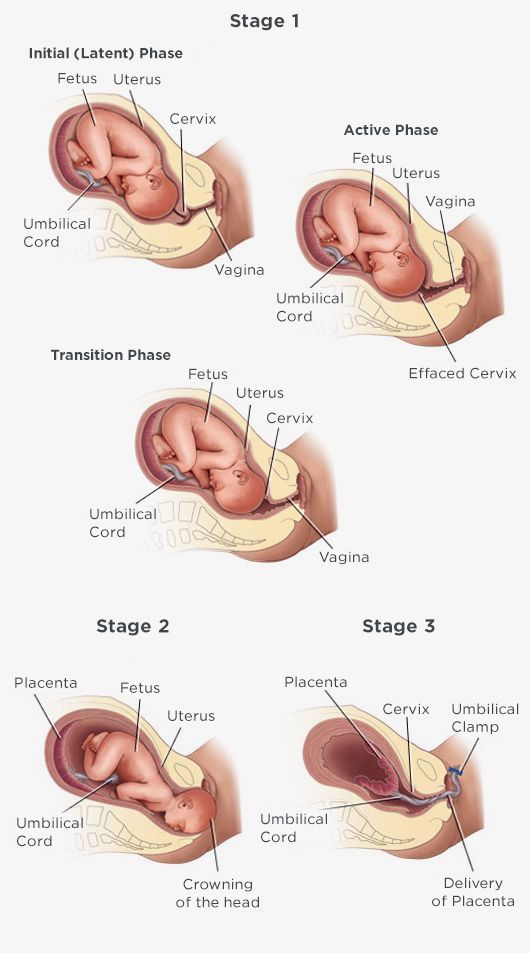
The first stage of labour begins when you feel contractions — your cervix will start to soften and to open. The time it takes for the cervix to open (or dilate) will vary from woman to woman and can range from several hours to days or even weeks. Once the cervix is dilated more than 3cm, and contractions are strong and regular, labour is said to be ‘established’.
Established labour is also known as the 'active phase'. This phase continues until the cervix dilates to approximately 7cm, with the contractions being strong, painful and around every 3 or 4 minutes.
This is followed by the ‘transition phase’, when the cervix continues to fully open. There is now less time to rest in between contractions.
First stage of labour is complete when the cervix is fully open (referred to as 'fully dilated'), the baby moves through the pelvis and the mother can begin pushing the baby out. Being fully dilated might not actually be a 10cm opening of the cervix. Rather it is when the doctor or midwife cannot feel any cervix when they perform a vaginal examination.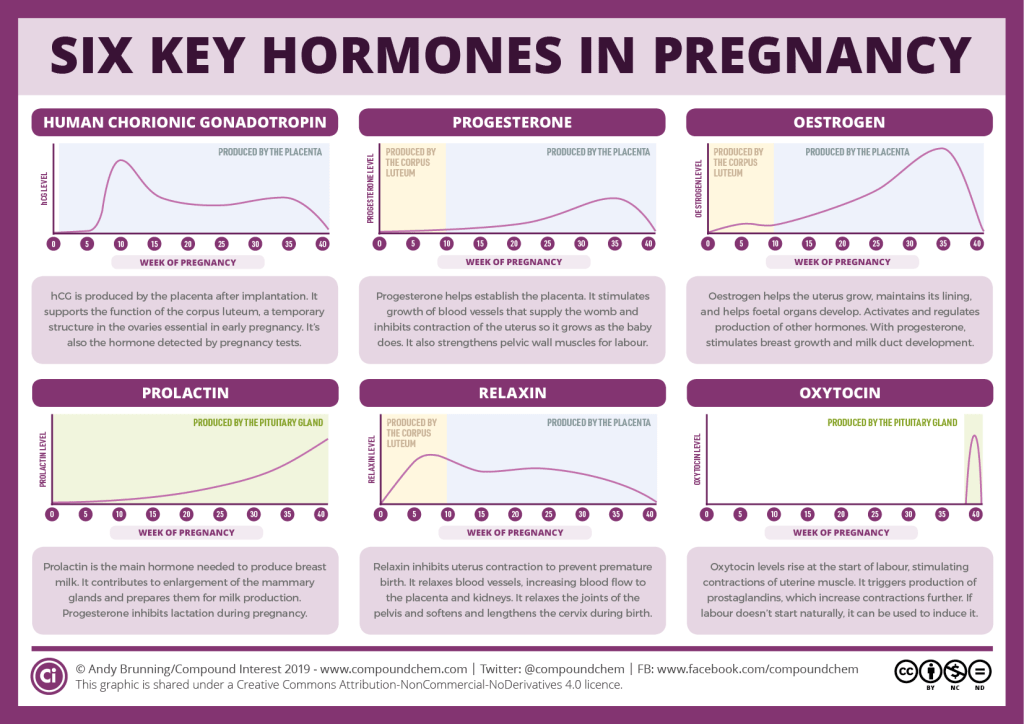
The second stage of labour is when your baby is being born and the third stage is when the placenta is delivered.
What problems can occur with the cervix during pregnancy, labour, or birth?
The cervix is monitored throughout pregnancy, labour and birth to identify any problems. For instance, if the cervix is weak, it might be difficult to keep the baby in the uterus for the whole pregnancy. This can lead to premature labour and birth.
During labour, contractions might not be regular or strong enough to fully open the cervix, which slows labour down. In these situations, the doctor or midwife might intervene by breaking the mother's waters or using a hormone to increase contractions and speed up the dilation of the cervix.
It is important that the mother does not begin pushing the baby out until the cervix is fully dilated. This is because pushing too soon might swell the cervix, which can slow down the birth.
Read more here about complications in labour, and how they are managed.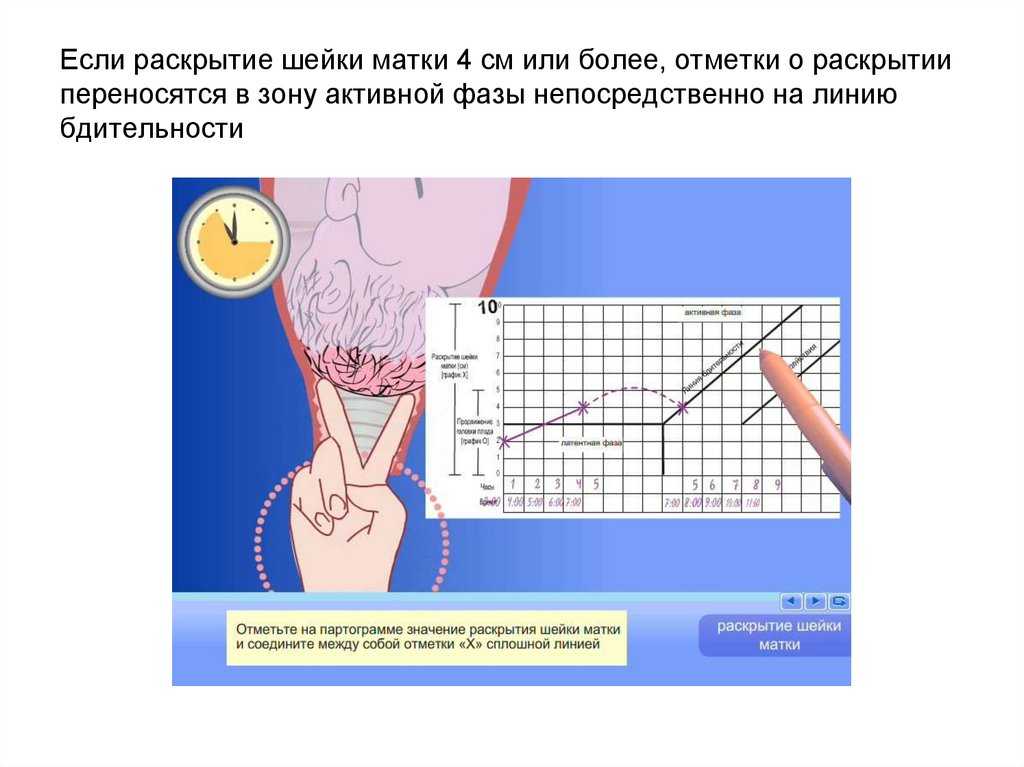
Sources:
MSD Manual (Female internal genital organs), Translational Research in Anatomy (March 2016) (The structure and function of the cervix during pregnancy), Women's Health (Understanding your menstrual cycle fact sheet), Mater Mother's Hospital (Labour and birth information), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), Royal Women's (Stages of labour), King Edward Memorial Hospital (Second stage of labour and birth), SA Health (Induction of labour techniques), Queensland Health (Vaginal examinations in labour)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Anatomy of pregnancy and birth
- Anatomy of pregnancy and birth - abdominal muscles
- Anatomy of pregnancy and birth - pelvis
- Anatomy of pregnancy and birth - perineum and pelvic floor
- Anatomy of pregnancy and birth - uterus
Need more information?
Uterus, cervix & ovaries - fact sheet | Jean Hailes
This fact sheet discusses some of the health conditions that may affect a woman's uterus, cervix and ovaries.
Read more on Jean Hailes for Women's Health website
Placenta previa - Better Health Channel
Placenta previa means the placenta has implanted at the bottom of the uterus, over the cervix or close by.
Read more on Better Health Channel website
Diaphragm - how effective is the diaphragm - Sexual Health Victoria
A diaphragm is a shallow, cup-shape made of silicone inserted inside the cervix. In Australia there is one size diaphragm available sold as Caya®.
Read more on Sexual Health Victoria website
Pap smear tests - MyDr.com.au
Pap smear tests are currently used in Australia as a screening test for cervical cancer. A Pap smear test can detect changes in the cells of the cervix that may develop into cancer.
A Pap smear test can detect changes in the cells of the cervix that may develop into cancer.
Read more on myDr website
Labour & birth: what to expect | Raising Children Network
Early labour signs include a show, waters breaking and pain. During labour, your contractions increase and your cervix dilates, so you can birth your baby.
Read more on raisingchildren.net.au website
Induction of labour
Inducing labour allows women to deliver their baby normally by stimulating labour contractions. There are several medical and surgical techniques which can be used.
Read more on Parenthub website
What happens to your body in childbirth
During childbirth, your body's hormones, ligaments and muscles, as well as the shape of your pelvis, all work together to bring your baby safely into the world.
Read more on Pregnancy, Birth & Baby website
Dilatation and curettage (D&C) - Better Health Channel
A dilatation and curettage (D&C) is an operation performed on women to lightly scrape away the womb lining.
Read more on Better Health Channel website
Asherman Syndrome
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Cervical Screening | Pap Smear | Jean Hailes
All you need to know about cervical screening tests and how they differ from pap smears. Learn why and when you should have one and how they work.
Read more on Jean Hailes for Women's Health website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Control and assessment of the uterus and cervix during pregnancy and labour
Review
. 1998 Sep-Oct;4(5):673-95.
doi: 10.1093/humupd/4.5.673.
R E Garfield 1 , G Saade, C Buhimschi, I Buhimschi, L Shi, S Q Shi, K Chwalisz
Affiliations
Affiliation
- 1 Department of Obstetrics and Gynecology, University of Texas Medical Branch, Galveston 77555-1062, USA.

- PMID: 10027621
- DOI: 10.1093/humupd/4.5.673
Review
R E Garfield et al. Hum Reprod Update. 1998 Sep-Oct.
. 1998 Sep-Oct;4(5):673-95.
doi: 10.1093/humupd/4.5.673.
Authors
R E Garfield 1 , G Saade, C Buhimschi, I Buhimschi, L Shi, S Q Shi, K Chwalisz
Affiliation
- 1 Department of Obstetrics and Gynecology, University of Texas Medical Branch, Galveston 77555-1062, USA.

- PMID: 10027621
- DOI: 10.1093/humupd/4.5.673
Abstract
Preterm labour and resultant preterm birth are the most important problems in perinatology. Countless efforts have failed to establish a single effective treatment of preterm labour, partly because the mechanisms regulating the uterus and cervix during pregnancy are not well understood. New knowledge is needed to inhibit early progression of labour (uterine contractility and cervical ripening), and adequate quantitative tools to evaluate the uterus and cervix during pregnancy are lacking. In this review, we outline studies showing that the uterus (myometrium) and cervix pass through a conditioning step in preparation for labour. This step is not easily identifiable with present methods to assess the uterus or cervix. In the uterus, this seemingly irreversible step consists of changes in the electrical properties to make muscle more excitable and responsive to produce forceful contractions. In the cervix, the step consists of softening of the connective tissue components. Progesterone appears to have a dominant role in controlling both the uterus and cervix, as antiprogestins induce early, preterm conditioning leading to preterm labour. Apparently, nitric oxide (NO) also controls conditioning of the uterus and cervix. In the uterus, NO, in concert with progesterone, inhibits uterine contractility. At term, NO production by the uterus and placenta are decreased and allow labour to progress. In contrast, NO in the cervix increases at the end of pregnancy and it may be the final pathway for stimulating cervical ripening by activation of metalloenzymes. The progress of labour can be assessed non-invasively using electromyographic (EMG) signals from the uterus (the driving force for contractility) recorded from the abdominal surface.
This step is not easily identifiable with present methods to assess the uterus or cervix. In the uterus, this seemingly irreversible step consists of changes in the electrical properties to make muscle more excitable and responsive to produce forceful contractions. In the cervix, the step consists of softening of the connective tissue components. Progesterone appears to have a dominant role in controlling both the uterus and cervix, as antiprogestins induce early, preterm conditioning leading to preterm labour. Apparently, nitric oxide (NO) also controls conditioning of the uterus and cervix. In the uterus, NO, in concert with progesterone, inhibits uterine contractility. At term, NO production by the uterus and placenta are decreased and allow labour to progress. In contrast, NO in the cervix increases at the end of pregnancy and it may be the final pathway for stimulating cervical ripening by activation of metalloenzymes. The progress of labour can be assessed non-invasively using electromyographic (EMG) signals from the uterus (the driving force for contractility) recorded from the abdominal surface. Uterine EMG bursts detected in this manner characterize uterine contractile events during human and animal pregnancy. A low uterine EMG activity, measured transabdominally throughout most of pregnancy, rises dramatically during labour. EMG activity also increases substantially during preterm labour in humans and rats. This method may be used one day to predict impending preterm labour and identify control steps and treatments. A quantitative method also assesses the cervix, using an optical device which measures collagen fluorescence in the cervix. The collascope estimates cervical collagen content from a fluorescent signal generated when collagen cross-links are illuminated with excitation light of about 340 nm. The system has proved useful in rats and humans at various stages of pregnancy, and indicates that cervical softening occurs progressively in the last one-third of pregnancy. In rats, collascope readings correlate with resistance measurements made in the isolated cervix, which may help to assess cervical function during pregnancy, and indicate control and treatments.
Uterine EMG bursts detected in this manner characterize uterine contractile events during human and animal pregnancy. A low uterine EMG activity, measured transabdominally throughout most of pregnancy, rises dramatically during labour. EMG activity also increases substantially during preterm labour in humans and rats. This method may be used one day to predict impending preterm labour and identify control steps and treatments. A quantitative method also assesses the cervix, using an optical device which measures collagen fluorescence in the cervix. The collascope estimates cervical collagen content from a fluorescent signal generated when collagen cross-links are illuminated with excitation light of about 340 nm. The system has proved useful in rats and humans at various stages of pregnancy, and indicates that cervical softening occurs progressively in the last one-third of pregnancy. In rats, collascope readings correlate with resistance measurements made in the isolated cervix, which may help to assess cervical function during pregnancy, and indicate control and treatments.
Similar articles
-
Methods and devices for the management of term and preterm labor.
Garfield RE, Maul H, Shi L, Maner W, Fittkow C, Olsen G, Saade GR. Garfield RE, et al. Ann N Y Acad Sci. 2001 Sep;943:203-24. doi: 10.1111/j.1749-6632.2001.tb03803.x. Ann N Y Acad Sci. 2001. PMID: 11594541 Review.
-
Changes in expression of the nitric oxide synthase isoforms in rat uterus and cervix during pregnancy and parturition.
Ali M, Buhimschi I, Chwalisz K, Garfield RE. Ali M, et al. Mol Hum Reprod. 1997 Nov;3(11):995-1003. doi: 10.1093/molehr/3.11.995. Mol Hum Reprod. 1997. PMID: 9433927
-
Differential regulation of nitric oxide in the rat uterus and cervix during pregnancy and labour.

Buhimschi I, Ali M, Jain V, Chwalisz K, Garfield RE. Buhimschi I, et al. Hum Reprod. 1996 Aug;11(8):1755-66. doi: 10.1093/oxfordjournals.humrep.a019481. Hum Reprod. 1996. PMID: 8921128
-
Instrumentation for the diagnosis of term and preterm labour.
Garfield RE, Chwalisz K, Shi L, Olson G, Saade GR. Garfield RE, et al. J Perinat Med. 1998;26(6):413-36. doi: 10.1515/jpme.1998.26.6.413. J Perinat Med. 1998. PMID: 10224598 Review.
-
Androgens in pregnancy: roles in parturition.
Makieva S, Saunders PT, Norman JE. Makieva S, et al. Hum Reprod Update. 2014 Jul-Aug;20(4):542-59. doi: 10.1093/humupd/dmu008. Epub 2014 Mar 18. Hum Reprod Update. 2014. PMID: 24643344 Free PMC article.
 Review.
Review.
See all similar articles
Cited by
-
Signaling Pathways Regulating Human Cervical Ripening in Preterm and Term Delivery.
Socha MW, Flis W, Pietrus M, Wartęga M, Stankiewicz M. Socha MW, et al. Cells. 2022 Nov 21;11(22):3690. doi: 10.3390/cells11223690. Cells. 2022. PMID: 36429118 Free PMC article. Review.
-
Impact of Oxidative Stress on Molecular Mechanisms of Cervical Ripening in Pregnant Women.
Socha MW, Flis W, Wartęga M, Stankiewicz M. Socha MW, et al. Int J Mol Sci. 2022 Oct 24;23(21):12780. doi: 10.3390/ijms232112780. Int J Mol Sci. 2022. PMID: 36361572 Free PMC article. Review.
-
Alvarez waves in pregnancy: a comprehensive review.
Russo S, Batista A, Esgalhado F, Palma Dos Reis CR, Serrano F, Vassilenko V, Ortigueira M. Russo S, et al. Biophys Rev. 2021 Jul 8;13(4):563-574. doi: 10.1007/s12551-021-00818-5. eCollection 2021 Aug. Biophys Rev. 2021. PMID: 34471439 Free PMC article. Review.
-
Microvesicles and exosomes released by amnion epithelial cells under oxidative stress cause inflammatory changes in uterine cells†.
Shahin HI, Radnaa E, Tantengco OAG, Kechichian T, Kammala AK, Sheller-Miller S, Taylor BD, Menon R. Shahin HI, et al. Biol Reprod. 2021 Aug 3;105(2):464-480. doi: 10.1093/biolre/ioab088. Biol Reprod. 2021. PMID: 33962471 Free PMC article.
-
Neurosteroid involvement in threatened preterm labour.
Turkmen S, Bäckström T, Kangas Flodin Y, Bixo M.
 Turkmen S, et al. Endocrinol Diabetes Metab. 2020 Dec 10;4(2):e00216. doi: 10.1002/edm2.216. eCollection 2021 Apr. Endocrinol Diabetes Metab. 2020. PMID: 33855217 Free PMC article.
Turkmen S, et al. Endocrinol Diabetes Metab. 2020 Dec 10;4(2):e00216. doi: 10.1002/edm2.216. eCollection 2021 Apr. Endocrinol Diabetes Metab. 2020. PMID: 33855217 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned. And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina.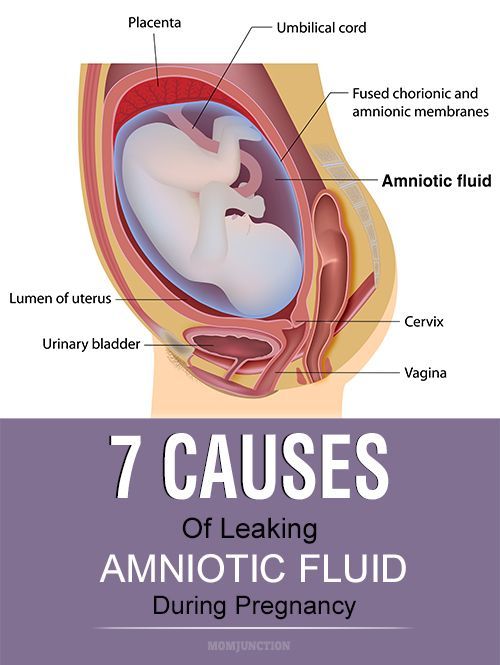 On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft. During pregnancy, the cervical glands expand and become more branched.
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium.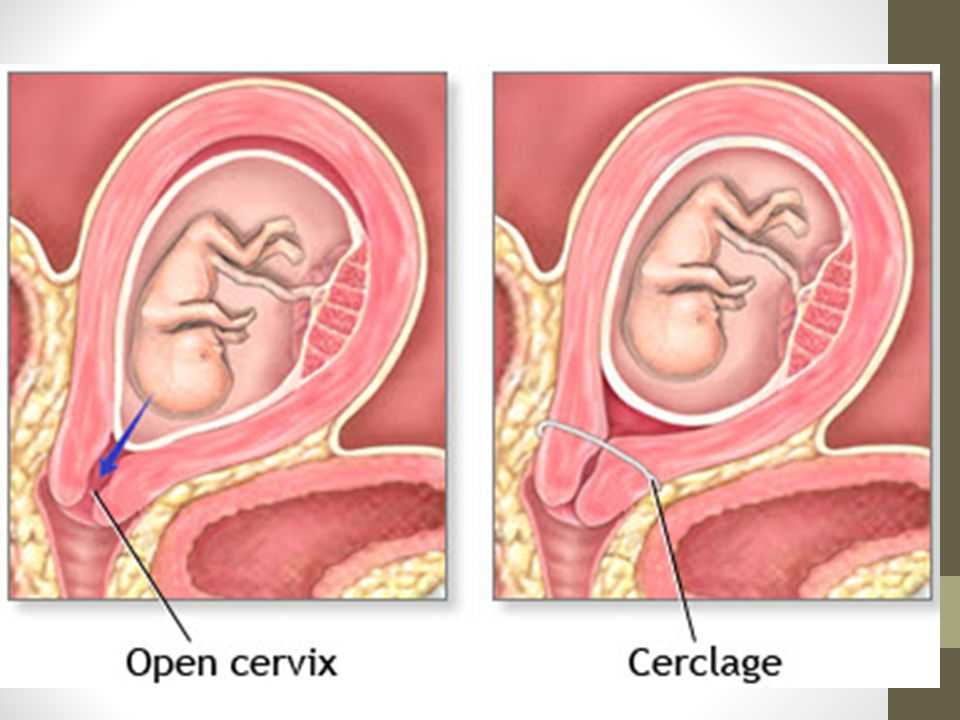 The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal.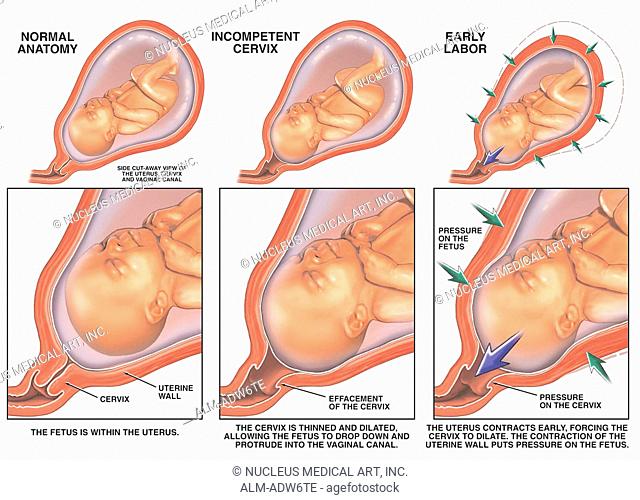 During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle.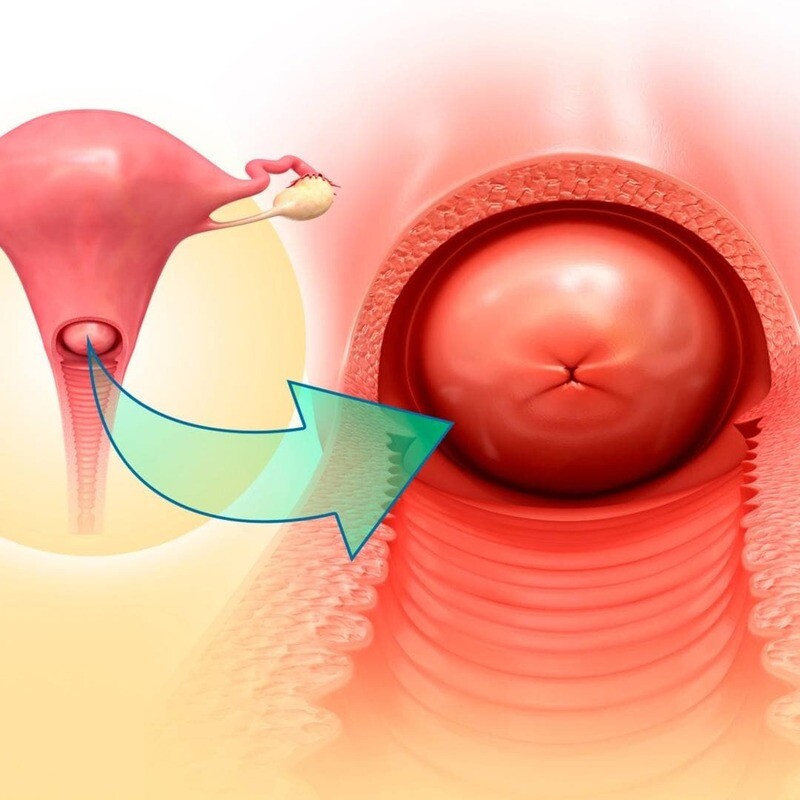 They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection. Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.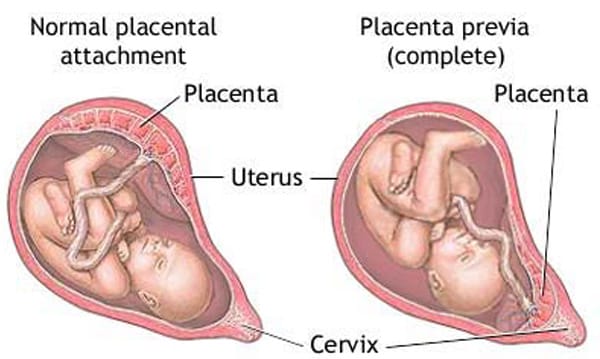
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners. The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable;
- is an injury to the cervix.
 The main cause of such injuries is, of course, childbirth and abortion;
The main cause of such injuries is, of course, childbirth and abortion; - hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select the clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you check the cost of services by phone / with the managers of the clinic
Clinical Hospital IDKMother and Child Clinic Enthusiastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children)Molecular genetics laboratoryGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsAdult ultrasound examinations
01.
Specialist consultations (adults)
02.
Consultations of specialists (children's)
03.
Laboratory of molecular genetics
04.
Adult Telemedicine
08.
Therapeutic Research
09.
Adult Ultrasound
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
Short cervix during pregnancy. What is a short cervix during pregnancy?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
A short cervix during pregnancy is a pathological condition in which the length of the organ is less than the minimum for a certain gestational age. In most cases, it is asymptomatic, detected by ultrasound screening. The appearance of clinical symptoms in the form of vaginal discharge and pain in the lower abdomen indicates a high risk of abortion. To make a diagnosis, the examination data on the chair are supplemented by the results of cervicometry and, if necessary, by the determination of the hormonal background. The treatment is combined with the use of tocolytics, hormone therapy, the installation of an obstetric pessary or suturing of the cervical canal.
In most cases, it is asymptomatic, detected by ultrasound screening. The appearance of clinical symptoms in the form of vaginal discharge and pain in the lower abdomen indicates a high risk of abortion. To make a diagnosis, the examination data on the chair are supplemented by the results of cervicometry and, if necessary, by the determination of the hormonal background. The treatment is combined with the use of tocolytics, hormone therapy, the installation of an obstetric pessary or suturing of the cervical canal.
- Causes of a short cervix during pregnancy
- Pathogenesis
- Symptoms of a short cervix during pregnancy
- Complications
- Diagnostics
- Treatment of a short cervix during pregnancy
- Prognosis and prevention
- Prices for treatment
General
A shortened cervix is one of the most common causes of miscarriage. According to experts in the field of obstetrics and gynecology, from 15 to 42% of late spontaneous abortions and premature births are provoked by this pathology. Signs of a short neck are detected in almost every 10th pregnant woman. The diagnosis is usually established at 15-20 weeks of gestation. An organ length of less than 3 cm at the 20th week of gestation is considered critical for continuing pregnancy. A direct indication for surgical correction of the disorder is the shortening of the neck to 2.0 cm or less by the end of the second trimester. Pathology is more often determined in multiparous women, which is associated with possible trauma in past births.
Signs of a short neck are detected in almost every 10th pregnant woman. The diagnosis is usually established at 15-20 weeks of gestation. An organ length of less than 3 cm at the 20th week of gestation is considered critical for continuing pregnancy. A direct indication for surgical correction of the disorder is the shortening of the neck to 2.0 cm or less by the end of the second trimester. Pathology is more often determined in multiparous women, which is associated with possible trauma in past births.
Short cervix during pregnancy
Causes of a short cervix during pregnancy
A clinically significant shortening of the isthmic-cervical zone occurs in the presence of pathological changes in the tissues of the cervix, its hypersensitivity to the action of regulatory hormones or an increase in their concentration, pressure of the growing fetus and its membranes on the lower uterine segment. The immediate causes of the formation of a shortened neck are:
- Anatomical defects and mechanical damage.
 Initially, a short neck occurs with genital infantilism, congenital anomalies in the development of the uterus or cervical canal. Deformation with a decrease in the length of the organ is possible due to trauma received in previous births or during invasive manipulations (diagnostic curettage, abortion).
Initially, a short neck occurs with genital infantilism, congenital anomalies in the development of the uterus or cervical canal. Deformation with a decrease in the length of the organ is possible due to trauma received in previous births or during invasive manipulations (diagnostic curettage, abortion). - Hormonal disorders. The condition of the cervix is affected by hormones produced by the ovaries and placenta during pregnancy. Most often, its shortening is observed with increased secretion of androgens. The occurrence of pathology is also facilitated by connective tissue dysplasia, caused by an increase in the level of relaxin as the birth approaches.
- Pressure on the isthmic-cervical region. The probability of stretching the lower uterine segment and the internal cervical os with its decrease increases from the 2nd trimester of pregnancy, when faster growth of the fetus begins. Risk factors are multiple pregnancies and polyhydramnios, in which the pressure on the cervix from inside the uterus is higher.
Pathogenesis
The mechanism of pathological disorders in the shortening of the cervix is associated with changes occurring in its tissues during pregnancy and an increase in pressure in the uterine cavity. Normally, after conception, the cervical canal closes, its mucosa becomes edematous and cyanotic due to accelerated blood supply, and the size of the cervix gradually increases, reaching a maximum value of 3.5-4.5 cm at 28 weeks. By the end of pregnancy, the cervix gradually shortens, opens and smoothes. In the presence of congenital or acquired anatomical defects, dyshormonal influences, the closing function of the cervical canal is impaired. As a result, under the pressure of the fetus, the internal and then the external uterine os are stretched, the neck becomes shorter. However, at the same time, it usually does not soften and does not reach the degree of maturity necessary for childbirth.
Symptoms of a short cervix during pregnancy
Pathology in more than 80% of cases is latent, diagnosed during routine ultrasound screening in the second trimester of pregnancy. The presence of a short neck may be indicated by the appearance of watery or bloody vaginal discharge, slight pulling pains in the lower abdomen, which become cramping as the disorder progresses. However, such disorders are typical for severe violations of the closure function of the cervix, occur with a high risk of premature termination of pregnancy, which increases the importance of routine examinations.
Complications
The most serious consequence of a short and deformed cervix is the increasing isthmic-cervical insufficiency. In the presence of such a pathology, the risk of spontaneous miscarriage and premature onset of labor increases. The failure of the cervical canal contributes to the upward spread of genital infections with the development of endometritis, chorioamnionitis, and other inflammatory processes. If a woman with a short neck carries a pregnancy, she may experience rapid labor with ruptures of the vagina and perineum, intranatal trauma to the child.
Diagnostics
In connection with the almost asymptomatic course of the disorder and the absence of its visible external signs, instrumental methods play a leading role in making the correct diagnosis, allowing you to accurately determine the size, condition and shape of the cervix. The most informative in the diagnostic plan are such studies of a pregnant woman as:
- Gynecological examination. The method is more indicative in multiparous patients with the expansion of the cervical canal along the entire length. An increase in the diameter of the external pharynx is clearly visible during examination of the neck in the mirrors. With a significant shortening, he passes the finger of an obstetrician-gynecologist, the fetal membranes can protrude through it. Palpation provides only indicative data on the possible size of the organ.
- Cervicometry. Transvaginal ultrasound determination of the length of the cervix, the diameter of its internal and external pharynx, the state of the cervical canal is the gold standard for diagnosing the disorder.
As a screening method, the method is indicated for all pregnant women with a period of 18-22 weeks. With a burdened obstetric history, cervical ultrasound is performed in the 1st trimester. Unscheduled sonography is performed if organ shortening is suspected.
- Determination of the level of hormones. If the anatomical prerequisites for the development of pathology are not identified, laboratory tests are indicated to assess the concentration of hormones. With a functional shortening of the neck, an increase in the concentration of androgens, a decrease in the content of progesterone, may be noted. A small number of pregnant women with a short cervix have increased levels of relaxin, but data from this analysis are rarely used.
The short neck is differentiated from other pathological conditions that have characteristic signs of early termination of pregnancy - detachment of a normally located placenta, its presentation or infarction, leakage of amniotic fluid, etc. In doubtful cases, consultations of related specialists are prescribed - endocrinologist, infectious disease specialist, immunologist.
Treatment of short cervix during pregnancy
Medical tactics after the detection of pathology depends on the gestational age, the degree of shortening of the organ, the presence or absence of a threat of termination of pregnancy, the burden of the obstetric history with habitual miscarriages or premature births. All patients are recommended to limit physical and emotional stress, sufficient rest and night sleep. For best results, pharmaceuticals are usually combined with minor invasive techniques. Pregnant women with this disorder are shown:
- Medical therapy. To reduce pressure on the lower segment of the uterus, in addition to wearing a bandage, patients are prescribed antispasmodics and tocolytics that reduce the tone of the uterine muscles. In the presence of hormonal disorders, it is possible to use drugs that regulate the secretion of hormones.
To correct emotional disorders, herbal remedies with a sedative effect are used.
- Installation of an obstetric ring (pessary). During the manipulation, a special device is put on the cervix, which keeps it closed. The method of non-surgical prophylaxis is effective with a slight shortening of the organ in 2-3 trimesters. The pessary allows you to compensate for the pressure of the fetus on the cervical region and prolong the pregnancy. The device is selected individually, taking into account the size of the body.
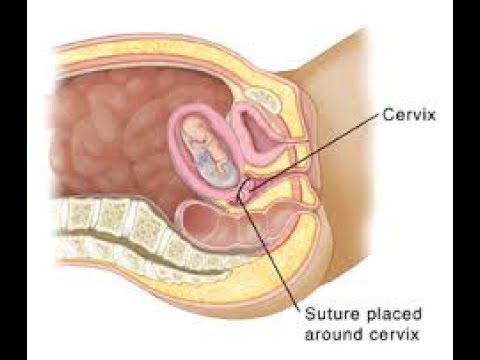
- Cervical cerclage. Surgical intervention for suturing the uterine neck is performed at 14-25 weeks of pregnancy. During the operation, circular purse-string or U-shaped sutures are placed around the cervical canal to prevent its expansion. Stitches are removed after the amniotic fluid breaks, the onset of labor, the onset of bleeding, or upon reaching the 38-week gestational age.
Prognosis and prevention
The prognosis of pregnancy with a shortened cervix depends on the time of detection of pathology and an adequate choice of pregnancy management tactics.