High blood pressure and protein in urine during pregnancy
Preeclampsia - Symptoms and causes
Overview
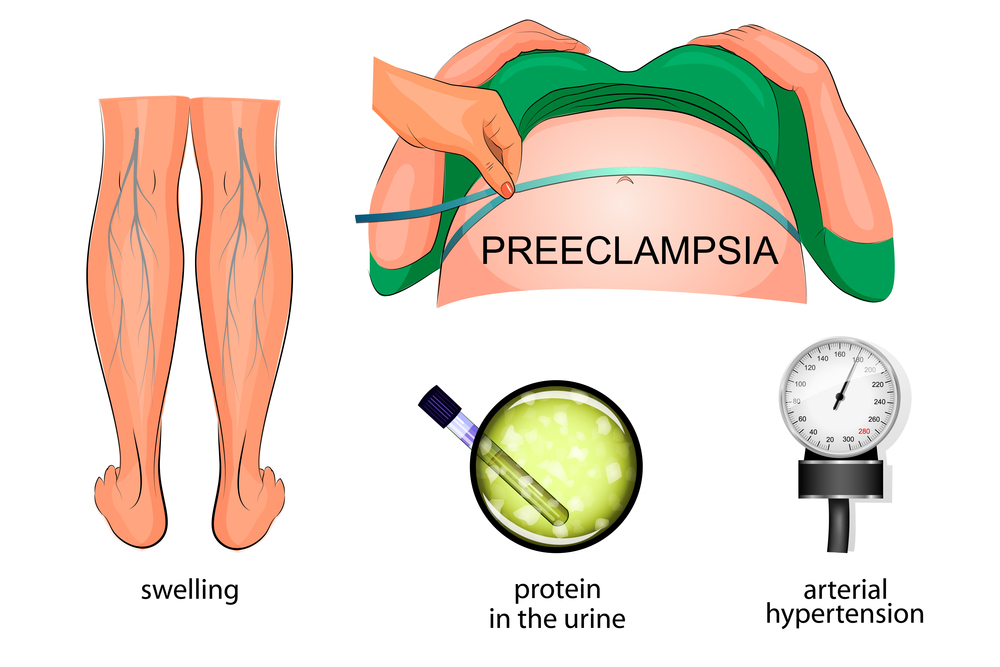
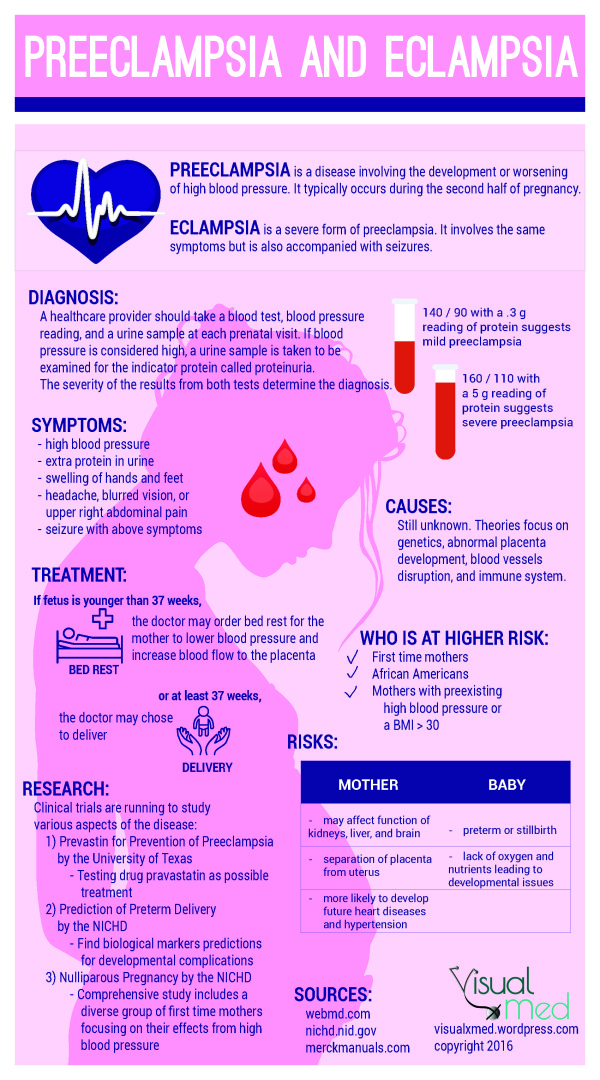
Preeclampsia is a complication of pregnancy. With preeclampsia, you might have high blood pressure, high levels of protein in urine that indicate kidney damage (proteinuria), or other signs of organ damage. Preeclampsia usually begins after 20 weeks of pregnancy in women whose blood pressure had previously been in the standard range.
Left untreated, preeclampsia can lead to serious — even fatal — complications for both the mother and baby.
Early delivery of the baby is often recommended. The timing of delivery depends on how severe the preeclampsia is and how many weeks pregnant you are. Before delivery, preeclampsia treatment includes careful monitoring and medications to lower blood pressure and manage complications.
Preeclampsia may develop after delivery of a baby, a condition known as postpartum preeclampsia.
Products & Services
- Book: Mayo Clinic Guide to a Healthy Pregnancy
Symptoms
The defining feature of preeclampsia is high blood pressure, proteinuria, or other signs of damage to the kidneys or other organs. You may have no noticeable symptoms. The first signs of preeclampsia are often detected during routine prenatal visits with a health care provider.
Along with high blood pressure, preeclampsia signs and symptoms may include:
- Excess protein in urine (proteinuria) or other signs of kidney problems
- Decreased levels of platelets in blood (thrombocytopenia)
- Increased liver enzymes that indicate liver problems
- Severe headaches
- Changes in vision, including temporary loss of vision, blurred vision or light sensitivity
- Shortness of breath, caused by fluid in the lungs
- Pain in the upper belly, usually under the ribs on the right side
- Nausea or vomiting
Weight gain and swelling (edema) are typical during healthy pregnancies. However, sudden weight gain or a sudden appearance of edema — particularly in your face and hands — may be a sign of preeclampsia.
When to see a doctor
Make sure you attend your prenatal visits so that your health care provider can monitor your blood pressure.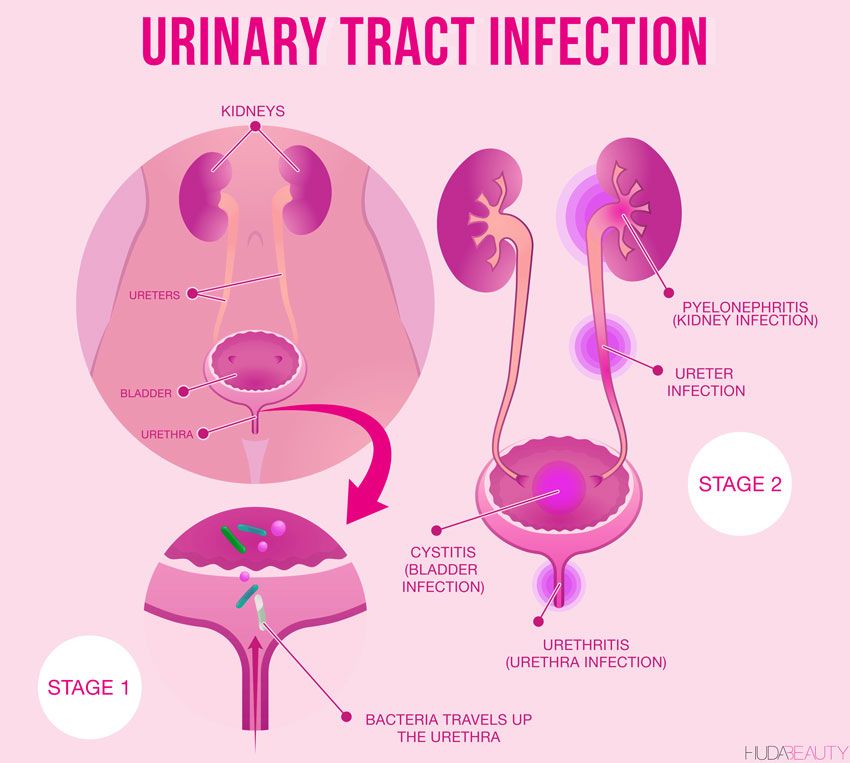 Contact your provider immediately or go to an emergency room if you have severe headaches, blurred vision or other visual disturbances, severe belly pain, or severe shortness of breath.
Contact your provider immediately or go to an emergency room if you have severe headaches, blurred vision or other visual disturbances, severe belly pain, or severe shortness of breath.
Because headaches, nausea, and aches and pains are common pregnancy complaints, it's difficult to know when new symptoms are simply part of being pregnant and when they may indicate a serious problem — especially if it's your first pregnancy. If you're concerned about your symptoms, contact your doctor.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you.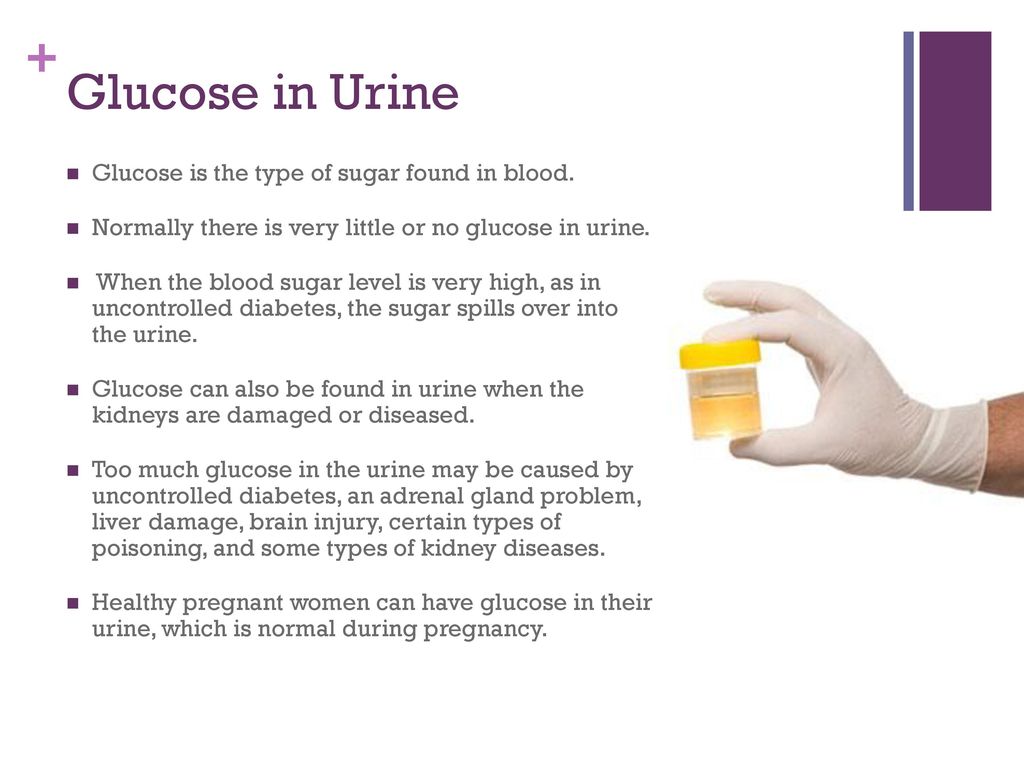 If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
The exact cause of preeclampsia likely involves several factors. Experts believe it begins in the placenta — the organ that nourishes the fetus throughout pregnancy. Early in a pregnancy, new blood vessels develop and evolve to supply oxygen and nutrients to the placenta.
In women with preeclampsia, these blood vessels don't seem to develop or work properly.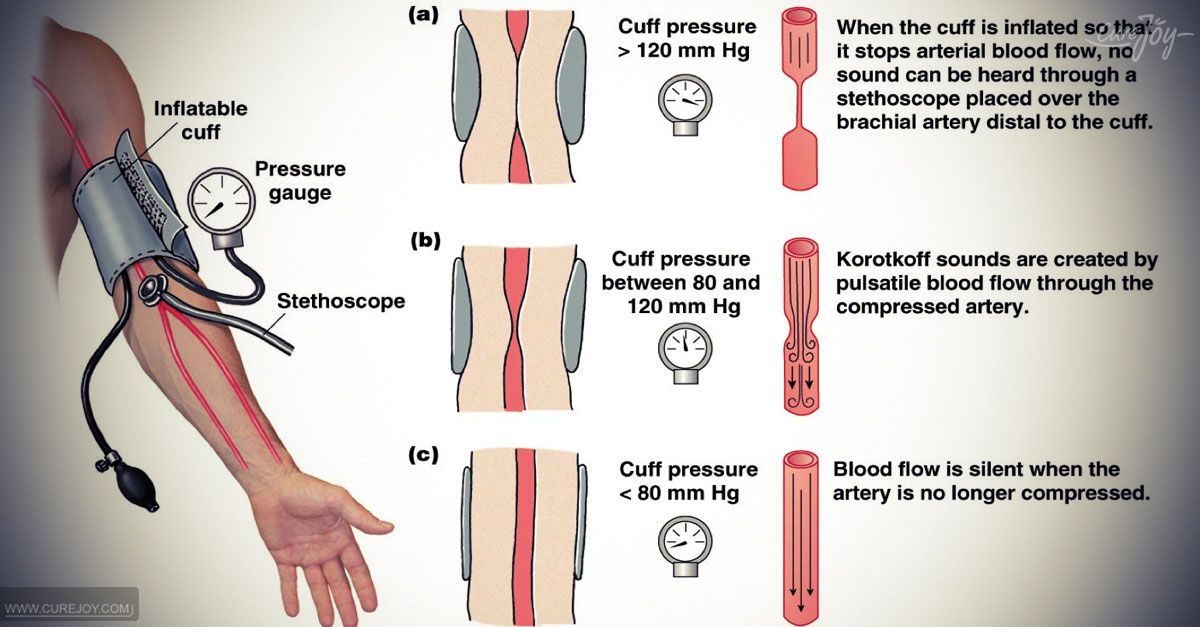 Problems with how well blood circulates in the placenta may lead to the irregular regulation of blood pressure in the mother.
Problems with how well blood circulates in the placenta may lead to the irregular regulation of blood pressure in the mother.
Other high blood pressure disorders during pregnancy
Preeclampsia is one high blood pressure (hypertension) disorder that can occur during pregnancy. Other disorders can happen, too:
- Gestational hypertension is high blood pressure that begins after 20 weeks without problems in the kidneys or other organs. Some women with gestational hypertension may develop preeclampsia.
- Chronic hypertension is high blood pressure that was present before pregnancy or that occurs before 20 weeks of pregnancy. High blood pressure that continues more than three months after a pregnancy also is called chronic hypertension.
- Chronic hypertension with superimposed preeclampsia occurs in women diagnosed with chronic high blood pressure before pregnancy, who then develop worsening high blood pressure and protein in the urine or other health complications during pregnancy.
Risk factors
Conditions that are linked to a higher risk of preeclampsia include:
- Preeclampsia in a previous pregnancy
- Being pregnant with more than one baby
- Chronic high blood pressure (hypertension)
- Type 1 or type 2 diabetes before pregnancy
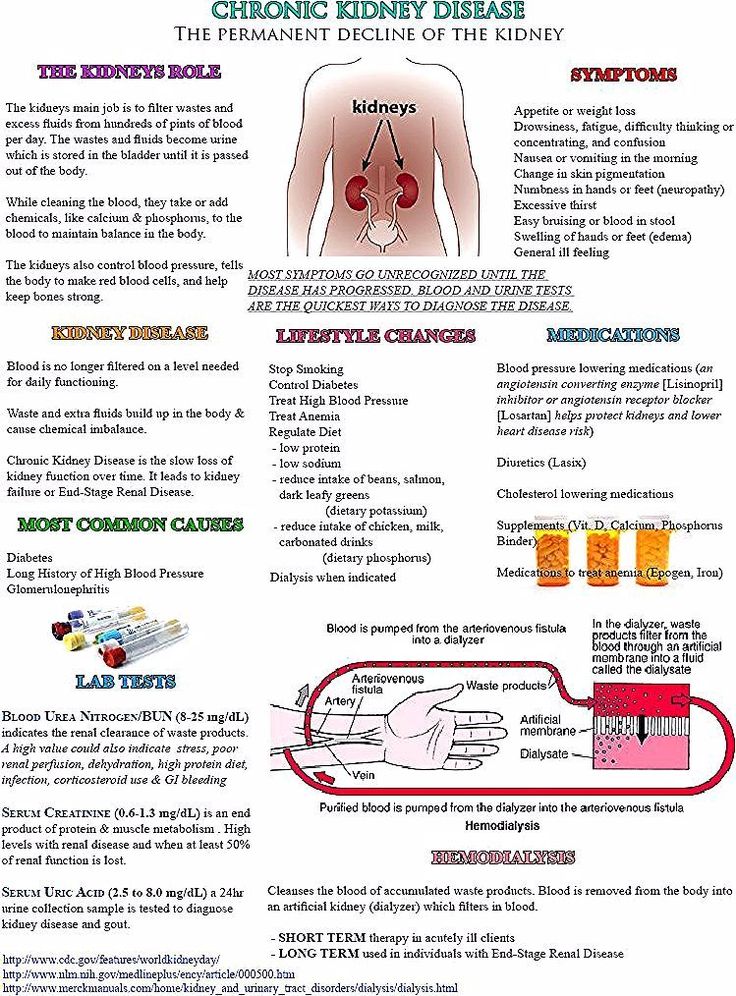
- Kidney disease
- Autoimmune disorders
- Use of in vitro fertilization
Conditions that are associated with a moderate risk of developing preeclampsia include:
- First pregnancy with current partner
- Obesity
- Family history of preeclampsia
- Maternal age of 35 or older
- Complications in a previous pregnancy
- More than 10 years since previous pregnancy
Other risk factors
Several studies have shown a greater risk of preeclampsia among Black women compared with other women. There's also some evidence of an increased risk among indigenous women in North America.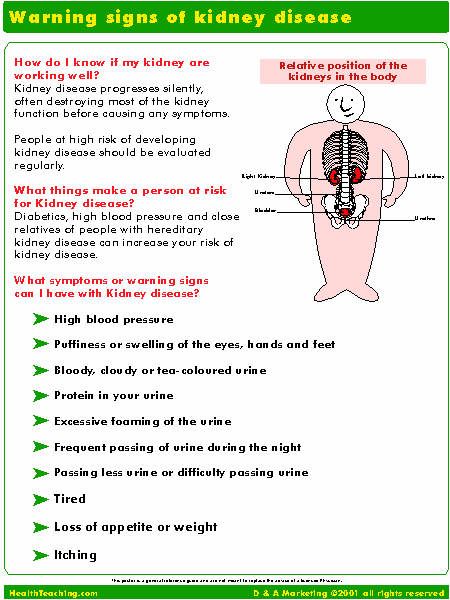
A growing body of evidence suggests that these differences in risk may not necessarily be based on biology. A greater risk may be related to inequities in access to prenatal care and health care in general, as well as social inequities and chronic stressors that affect health and well-being.
Lower income also is associated with a greater risk of preeclampsia likely because of access to health care and social factors affecting health.
For the purposes of making decisions about prevention strategies, a Black woman or a woman with a low income has a moderately increased risk of developing preeclampsia.
Complications
Complications of preeclampsia may include:
- Fetal growth restriction. Preeclampsia affects the arteries carrying blood to the placenta. If the placenta doesn't get enough blood, the baby may receive inadequate blood and oxygen and fewer nutrients. This can lead to slow growth known as fetal growth restriction.
- Preterm birth.
 Preeclampsia may lead to an unplanned preterm birth — delivery before 37 weeks. Also, planned preterm birth is a primary treatment for preeclampsia. A baby born prematurely has increased risk of breathing and feeding difficulties, vision or hearing problems, developmental delays, and cerebral palsy. Treatments before preterm delivery may decrease some risks.
Preeclampsia may lead to an unplanned preterm birth — delivery before 37 weeks. Also, planned preterm birth is a primary treatment for preeclampsia. A baby born prematurely has increased risk of breathing and feeding difficulties, vision or hearing problems, developmental delays, and cerebral palsy. Treatments before preterm delivery may decrease some risks. - Placental abruption. Preeclampsia increases your risk of placental abruption. With this condition, the placenta separates from the inner wall of the uterus before delivery. Severe abruption can cause heavy bleeding, which can be life-threatening for both the mother and baby.
-
HELLP syndrome. HELLP stands for hemolysis (the destruction of red blood cells), elevated liver enzymes and low platelet count.
 This severe form of preeclampsia affects several organ systems. HELLP syndrome is life-threatening to the mother and baby, and it may cause lifelong health problems for the mother.
This severe form of preeclampsia affects several organ systems. HELLP syndrome is life-threatening to the mother and baby, and it may cause lifelong health problems for the mother.Signs and symptoms include nausea and vomiting, headache, upper right belly pain, and a general feeling of illness or being unwell. Sometimes, it develops suddenly, even before high blood pressure is detected. It also may develop without any symptoms.
-
Eclampsia. Eclampsia is the onset of seizures or coma with signs or symptoms of preeclampsia. It is very difficult to predict whether a patient with preeclampsia will develop eclampsia. Eclampsia can happen without any previously observed signs or symptoms of preeclampsia.
Signs and symptoms that may appear before seizures include severe headaches, vision problems, mental confusion or altered behaviors.
 But, there are often no symptoms or warning signs. Eclampsia may occur before, during or after delivery.
But, there are often no symptoms or warning signs. Eclampsia may occur before, during or after delivery. - Other organ damage. Preeclampsia may result in damage to the kidneys, liver, lung, heart, or eyes, and may cause a stroke or other brain injury. The amount of injury to other organs depends on how severe the preeclampsia is.
- Cardiovascular disease. Having preeclampsia may increase your risk of future heart and blood vessel (cardiovascular) disease. The risk is even greater if you've had preeclampsia more than once or you've had a preterm delivery.
Prevention
Medication
The best clinical evidence for prevention of preeclampsia is the use of low-dose aspirin. Your primary care provider may recommend taking an 81-milligram aspirin tablet daily after 12 weeks of pregnancy if you have one high-risk factor for preeclampsia or more than one moderate-risk factor.
It's important that you talk with your provider before taking any medications, vitamins or supplements to make sure it's safe for you.
Lifestyle and healthy choices
Before you become pregnant, especially if you've had preeclampsia before, it's a good idea to be as healthy as you can be. Talk to your provider about managing any conditions that increase the risk of preeclampsia.
By Mayo Clinic Staff
Related
Associated Procedures
News from Mayo Clinic
Products & Services
Symptoms, Causes, Treatments & Prevention
Overview
What is preeclampsia?
Preeclampsia is a serious blood pressure condition that develops during pregnancy. People with preeclampsia often have high blood pressure (hypertension) and high levels of protein in their urine (proteinuria). Preeclampsia typically develops after the 20th week of pregnancy. It can also affect other organs in the body and be dangerous for both the mom and her developing fetus. Because of these risks, preeclampsia needs to be treated by a healthcare provider.
What happens when you have preeclampsia?
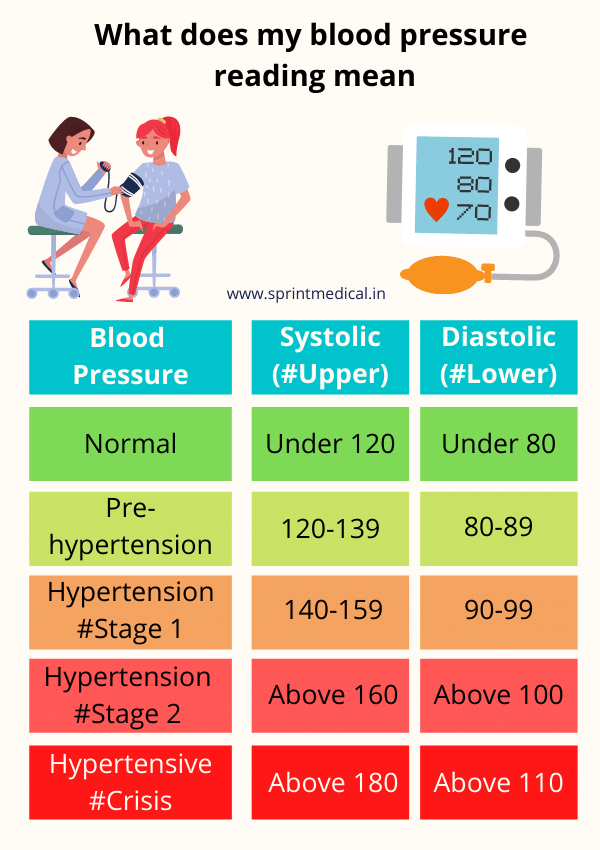
When you have preeclampsia, your blood pressure is elevated (higher than 140/90 mmHg), and you may have high levels of protein in your urine. Preeclampsia puts stress on your heart and other organs and can cause serious complications. It can also affect the blood supply to your placenta, impair liver and kidney function or cause fluid to build up in your lungs. The protein in your urine is a sign of kidney dysfunction.
Preeclampsia puts stress on your heart and other organs and can cause serious complications. It can also affect the blood supply to your placenta, impair liver and kidney function or cause fluid to build up in your lungs. The protein in your urine is a sign of kidney dysfunction.
How common is preeclampsia?
Preeclampsia is a condition unique to pregnancy that complicates up to 8% of all deliveries worldwide. In the United States, it's the cause of about 15% of premature deliveries (delivery before 37 weeks of pregnancy).
Who gets preeclampsia?
Preeclampsia may be more common in first-time mothers. Healthcare providers are not entirely sure why some people develop preeclampsia. Some factors that may put you at a higher risk are:
- History of high blood pressure, kidney disease or diabetes.
- Expecting multiples.
- Family history of preeclampsia.
- Autoimmune conditions like lupus.
- Obesity.
Symptoms and Causes
What are the symptoms?
Many people with preeclampsia do not have any symptoms.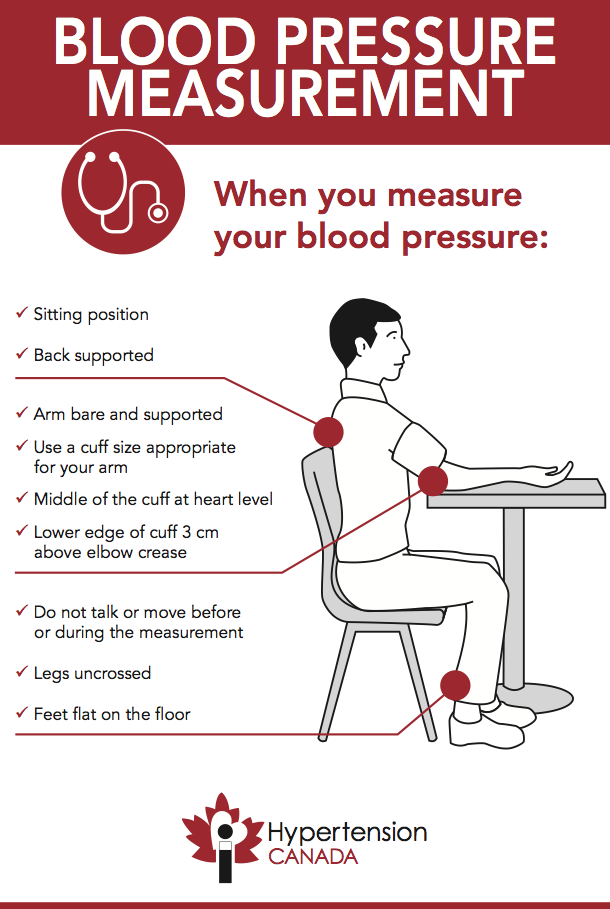 For those that do, some of the first signs of preeclampsia are high blood pressure, protein in the urine and retaining water (this can cause weight gain and swelling).
For those that do, some of the first signs of preeclampsia are high blood pressure, protein in the urine and retaining water (this can cause weight gain and swelling).
Other signs of preeclampsia include:
- Headaches.
- Blurry vision or light sensitivity.
- Dark spots appearing in your vision.
- Right side abdominal pain.
- Swelling in your hands and face (edema).
- Shortness of breath.
It's essential to share all of your pregnancy symptoms with your healthcare provider. Many people are unaware they have preeclampsia until their blood pressure and urine are checked at a prenatal appointment.
Severe preeclampsia may include symptoms like:
- Hypertensive emergency (blood pressure is 160/110 mmHg or higher).
- Decreased kidney or liver function.
- Fluid in the lungs.
- Low blood platelet levels (thrombocytopenia).
- Decreased urine production
If your preeclampsia is severe, you may be admitted to the hospital for closer observation or need to deliver your baby as soon as possible. Your healthcare provider may give you medications for high blood pressure or to help the fetus's lungs develop before delivery.
Your healthcare provider may give you medications for high blood pressure or to help the fetus's lungs develop before delivery.
What causes preeclampsia?
No one is entirely sure. Preeclampsia is believed to come from a problem with the health of the placenta (the organ that develops in the uterus during pregnancy and is responsible for providing oxygen and nutrients to the fetus). The blood supply to the placenta might be decreased in preeclampsia, and this can lead to problems with both you and the fetus.
Does stress cause preeclampsia?
While stress may impact blood pressure, stress is not one of the direct causes of preeclampsia. While some stress is unavoidable during pregnancy, avoiding high-stress situations or learning to manage your stress is a good idea.
What week of pregnancy does preeclampsia start?
Preeclampsia typically occurs after 20 weeks of pregnancy, but it can come earlier. Most preeclampsia occurs at or near term (37 weeks gestation). Preeclampsia can also come after delivery (postpartum preeclampsia), which usually occurs between the first few days to one week after delivery. In rare cases, it begins weeks after delivery.
Preeclampsia can also come after delivery (postpartum preeclampsia), which usually occurs between the first few days to one week after delivery. In rare cases, it begins weeks after delivery.
Will preeclampsia affect my baby?
Preeclampsia can cause preterm delivery (your baby needing delivered early). Premature babies are at increased risk for health complications like low birth weight and respiratory issues.
Diagnosis and Tests
How is it diagnosed?
Preeclampsia is often diagnosed during routine prenatal appointments when your healthcare provider checks your weight gain, blood pressure and urine.
If preeclampsia is suspected, your healthcare provider may:
- Order additional blood tests to check kidney and liver functions.
- Suggest a 24-hour urine collection to watch for proteinuria.
- Perform an ultrasound and other fetal monitoring to look at the size of the fetus and assess the amniotic fluid volume.
Preeclampsia can be categorized as mild or severe. You may be diagnosed with mild preeclampsia if you have high blood pressure plus high levels of protein in your urine.
You may be diagnosed with mild preeclampsia if you have high blood pressure plus high levels of protein in your urine.
You are diagnosed with severe preeclampsia if you have symptoms of mild preeclampsia plus:
- Signs of kidney or liver damage (seen in blood work).
- Low platelet count
- Fluid in your lungs.
- Headaches and dizziness.
- Visual impairment or seeing spots.
Management and Treatment
How is preeclampsia treated?
Your healthcare provider will advise you on the best way to treat preeclampsia. Treatment generally depends on how severe your preeclampsia is and how far along you are in pregnancy.
If you're close to full term (37 weeks pregnant or greater), your baby will probably be delivered early. You can still have a vaginal delivery, but sometimes a Cesarean delivery (C-section) is recommended. Your healthcare provider may give you medication to help the fetus's lungs develop and manage your blood pressure until the baby can be delivered.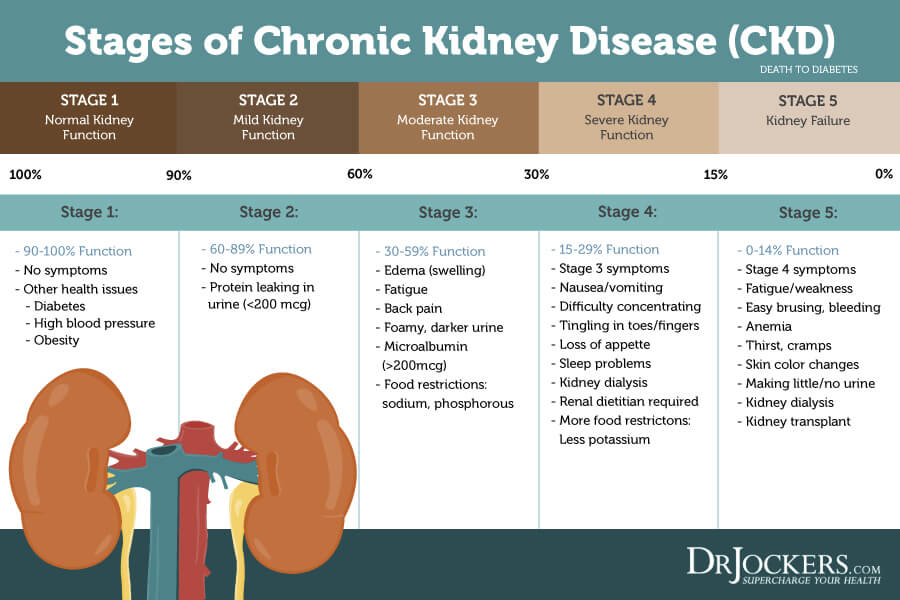 Sometimes it is safer to deliver the baby early than to risk prolonging the pregnancy.
Sometimes it is safer to deliver the baby early than to risk prolonging the pregnancy.
When preeclampsia develops earlier in pregnancy, you'll be monitored closely in an effort to prolong the pregnancy and allow for the fetus to grow and develop. You'll have more prenatal appointments, including ultrasounds, urine tests and blood draws. You may be asked to check your blood pressure at home. If you are diagnosed with severe preeclampsia, you could remain in the hospital until you deliver your baby.
If the preeclampsia worsens or becomes more severe, your baby will need to be delivered.
During labor and following delivery, people with preeclampsia are often given magnesium intravenously (directly into the vein) to prevent the development of eclampsia (seizures from preeclampsia).
Is there a cure for preeclampsia?
No, there isn't a cure for preeclampsia. Preeclampsia can only be cured with delivery. Your healthcare provider will still want to monitor you for several weeks after delivery to make sure your symptoms go away.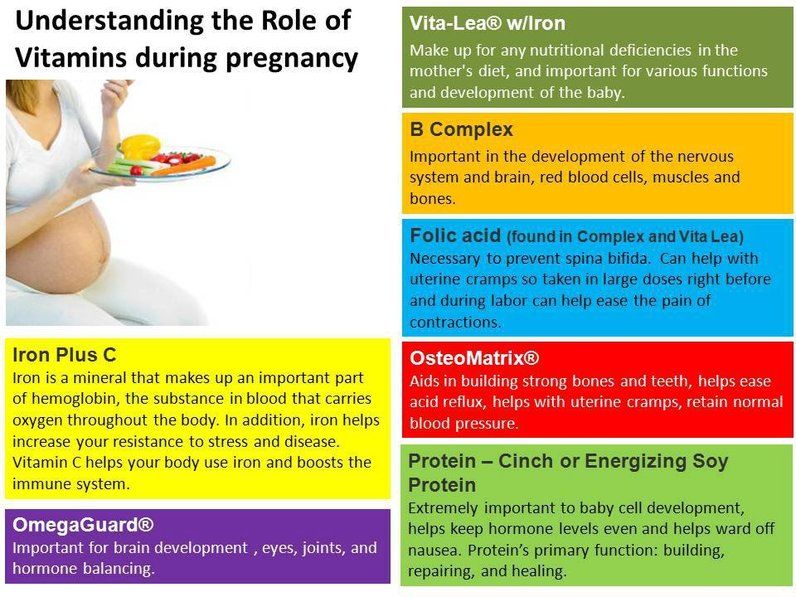
Prevention
How can I reduce my risk of getting preeclampsia?
For people with risk factors, there are some steps that can be taken prior to and during pregnancy to lower the chance of developing preeclampsia. These steps can include:
- Losing weight if you have overweight/obesity (prior to pregnancy-related weight gain).
- Controlling your blood pressure and blood sugar (if you had high blood pressure or diabetes prior to pregnancy).
- Maintaining a regular exercise routine.
- Getting enough sleep.
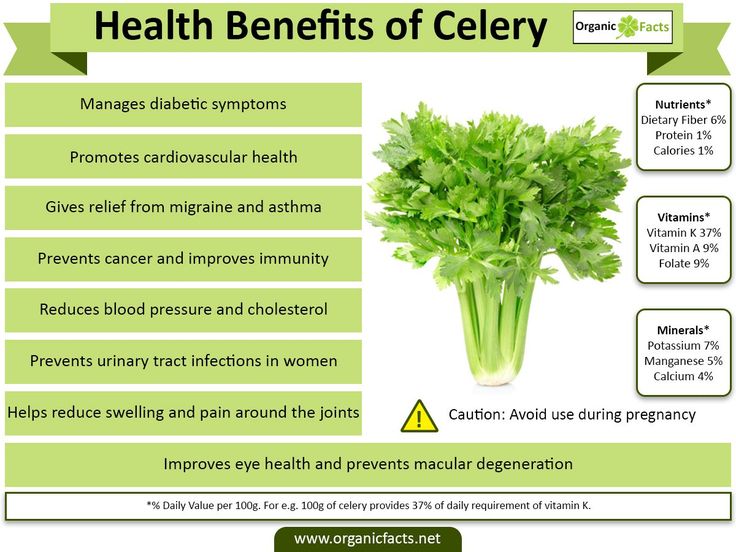
- Eating healthy foods that are low in salt and avoiding caffeine.
Can you prevent preeclampsia?
Taking a baby aspirin daily has been demonstrated to decrease your risk of developing preeclampsia by approximately 15%. If you have risk factors for preeclampsia, your healthcare provider may recommend starting aspirin in early pregnancy (by 12 weeks gestation).
Outlook / Prognosis
What are the most common complications of preeclampsia?
If left untreated, preeclampsia can be potentially fatal to both you and the fetus.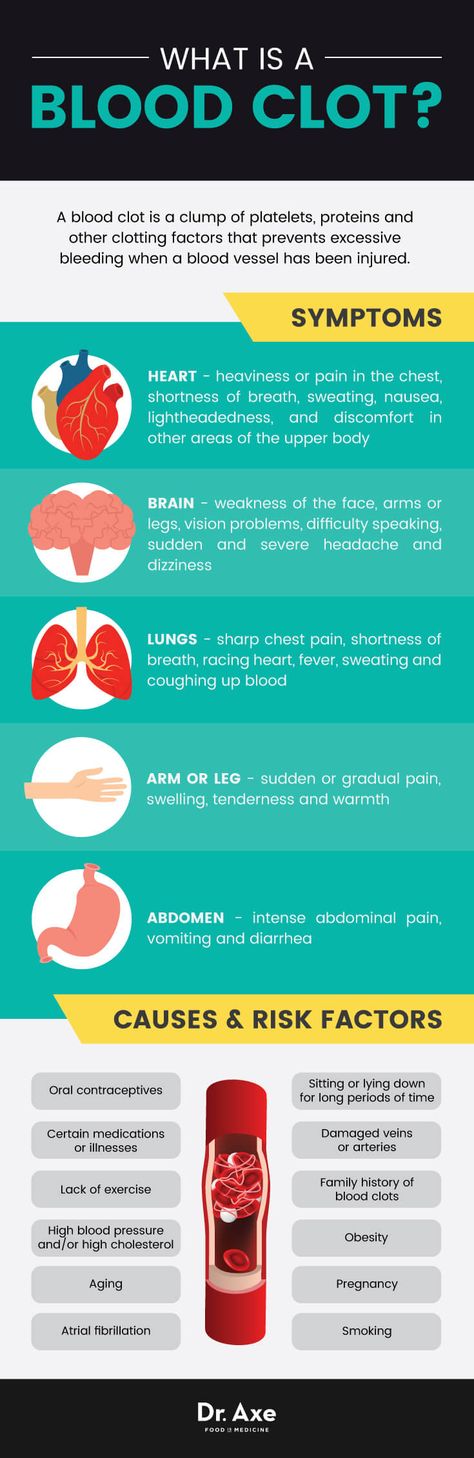
Before delivery, the most common complications are preterm birth, low birth weight or placental abruption.
Preeclampsia can cause HELLP syndrome (hemolysis, elevated liver enzymes and low platelet count). This happens when preeclampsia damages your liver and red blood cells and interferes with blood clotting. Other signs of HELLP syndrome are blurry vision, chest pain, headaches and nosebleeds.
After you've delivered your baby, you may be at an increased risk for:
- Kidney disease.
- Heart attack.
- Stroke.
- Developing preeclampsia in future pregnancies.
Does preeclampsia go away after delivery?
Preeclampsia typically goes away within days to weeks following delivery. Sometimes, your blood pressure can remain high for a few weeks after delivery, requiring treatment with medication. Your healthcare provider will work with you after your pregnancy to manage your blood pressure. People with preeclampsia — particularly those who develop the condition early in pregnancy — are at greater risk for high blood pressure (hypertension) and heart disease later in life.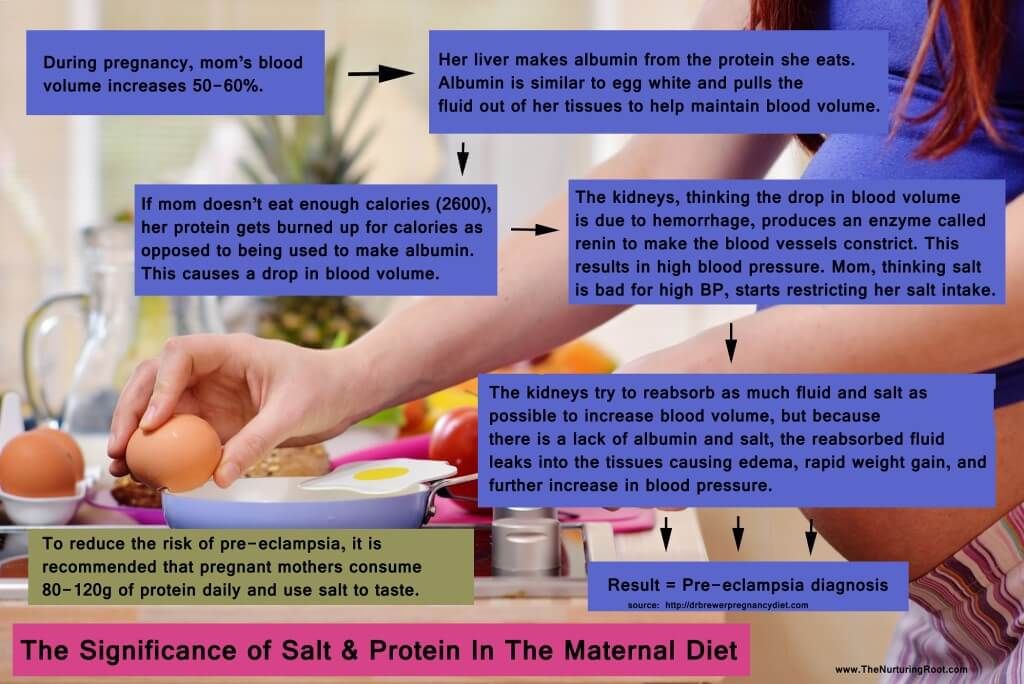 Knowing this information, those individuals can work with their primary care provider to take steps to reduce these risks.
Knowing this information, those individuals can work with their primary care provider to take steps to reduce these risks.
Living With
When should I see my healthcare provider?
Preeclampsia can be a fatal condition during pregnancy. If you're being treated for this condition, make sure to see your healthcare provider for all of your appointments and blood or urine tests. Contact your obstetrician if you have any concerns or questions about your symptoms.
Go to the nearest hospital if you're pregnant and experience the following:
- Symptoms of a seizure-like twitching or convulsing.
- Shortness of breath.
- Sharp pain in your abdomen (specifically the right side).
- Blurry vision.
- Severe headache that won't go away.
- Dark spots in your vision that don't go away.
What questions should I ask my doctor?
If your healthcare provider has diagnosed you with preeclampsia, it's normal to have concerns.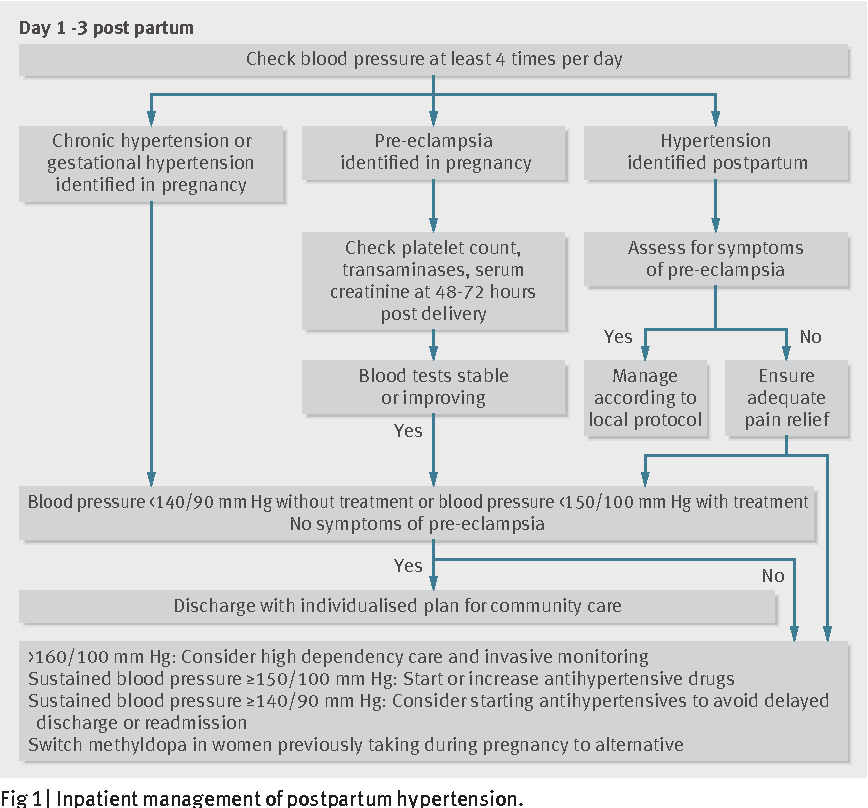 Some common questions to ask your healthcare provider are:
Some common questions to ask your healthcare provider are:
- Do I need to take medication?
- Do I need to restrict my activities?
- What changes should I make to my diet?
- How often will you need to monitor my health during pregnancy?
- Will I need to deliver my baby early?
- How can I best manage preeclampsia?
Frequently Asked Questions
What's the difference between preeclampsia and eclampsia?
Eclampsia is severe preeclampsia that causes seizures. It's considered a complication of preeclampsia, but it can happen without signs of preeclampsia. In rare cases, it can lead to coma, stroke or death.
What is postpartum preeclampsia?
Postpartum preeclampsia is when you develop preeclampsia after your baby is born. It typically happens within two days of giving birth but can also develop several weeks later. The signs of postpartum preeclampsia are similar to preeclampsia and include swelling in your limbs and extremities, headaches, seeing spots, stomach pains and nausea.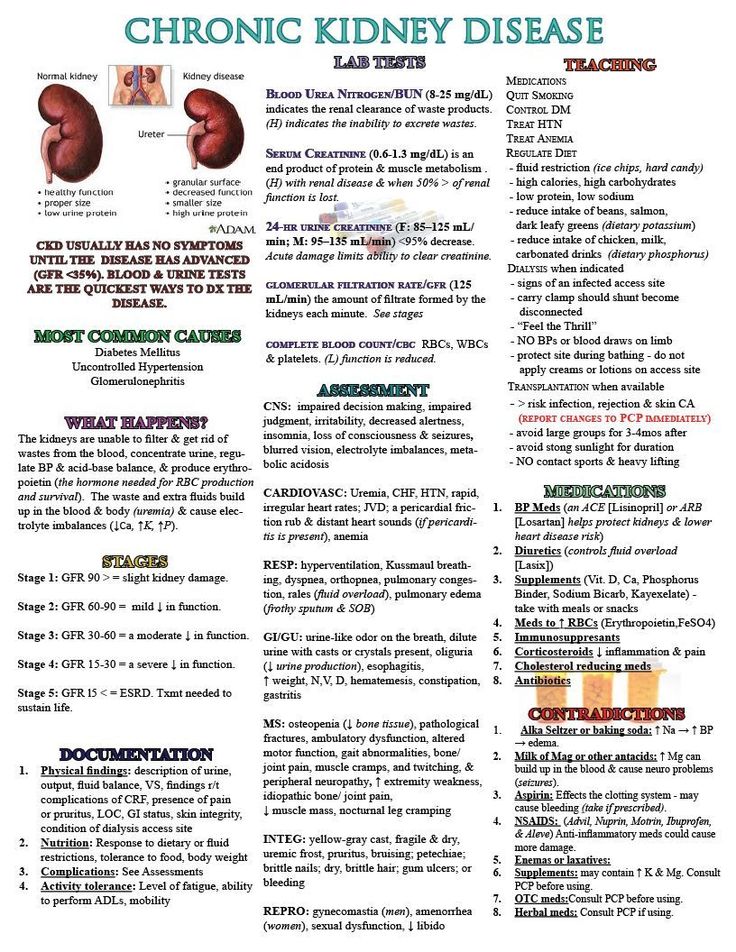 It's a serious condition that can cause seizures, stroke and organ damage.
It's a serious condition that can cause seizures, stroke and organ damage.
A note from Cleveland Clinic
Preeclampsia is a serious condition that you may not be aware you even have. It's important to go to all your prenatal appointments and be open about all the symptoms you feel during pregnancy. When preeclampsia is caught early, it can be treated and managed to keep both you and the fetus safe and healthy. Most people with preeclampsia go on to have healthy babies.
Hypertension in pregnancy
High blood pressure during pregnancy
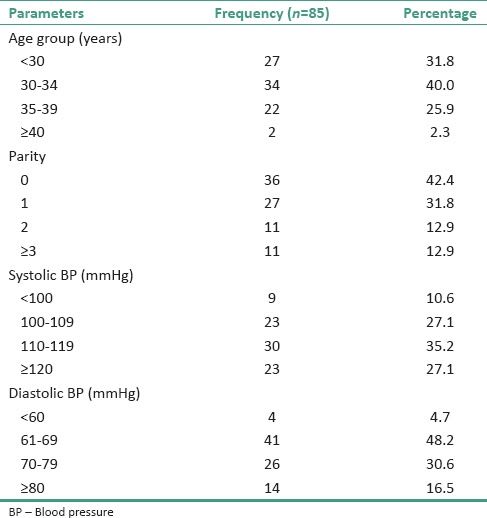
Changes in blood pressure (BP) in women during pregnancy are observed quite often, which can adversely affect the mother and fetus. Blood pressure is one of the most important indicators of the functioning of the circulatory system in the body. During pregnancy, all organs and systems of the mother work with increased stress, especially the cardiovascular system. Therefore, it is necessary to regularly measure blood pressure to prevent the development of severe complications. At the beginning of pregnancy, blood pressure, as a rule, decreases slightly, which is associated with the action of hormones. In later pregnancy, as the fetus grows and blood flow increases to feed it, blood pressure may increase relative to pre-pregnancy physiological values. Hypertension is said to occur when a pregnant woman's blood pressure exceeds 140/9.0 mmHg However, in women with low blood pressure before pregnancy, arterial hypertension may be at blood pressure levels that are usually considered normal. Therefore, it is important to know your normal blood pressure.
At the beginning of pregnancy, blood pressure, as a rule, decreases slightly, which is associated with the action of hormones. In later pregnancy, as the fetus grows and blood flow increases to feed it, blood pressure may increase relative to pre-pregnancy physiological values. Hypertension is said to occur when a pregnant woman's blood pressure exceeds 140/9.0 mmHg However, in women with low blood pressure before pregnancy, arterial hypertension may be at blood pressure levels that are usually considered normal. Therefore, it is important to know your normal blood pressure.
Why is high blood pressure dangerous during pregnancy?
High blood pressure during pregnancy poses a great danger to the mother and fetus. Against this background, vasoconstriction occurs and the blood supply to all vital organs, including the placenta, is disrupted. Due to the lack of essential nutrients and oxygen, the process of growth and development of the fetus slows down. There is a serious danger of placental abruption, which is accompanied by bleeding and threatens the life of the mother and fetus. High blood pressure during pregnancy can lead to the development of a dangerous pregnancy complication - preeclampsia. Edema, large weight gain, and the presence of protein in the urine can also be a manifestation of preeclampsia. Very dangerous symptoms of preeclampsia are: headache, blurred vision ("flies", "veil" before the eyes), pain in the upper abdomen. Deterioration of the general condition may be accompanied by dizziness, tinnitus, nausea, vomiting. Pre-eclampsia can provoke a formidable complication - eclampsia. In this condition, the pregnant woman loses consciousness and convulsions occur.
High blood pressure during pregnancy can lead to the development of a dangerous pregnancy complication - preeclampsia. Edema, large weight gain, and the presence of protein in the urine can also be a manifestation of preeclampsia. Very dangerous symptoms of preeclampsia are: headache, blurred vision ("flies", "veil" before the eyes), pain in the upper abdomen. Deterioration of the general condition may be accompanied by dizziness, tinnitus, nausea, vomiting. Pre-eclampsia can provoke a formidable complication - eclampsia. In this condition, the pregnant woman loses consciousness and convulsions occur.
Register for pregnancy at the antenatal clinic as early as possible!
A very important feature of arterial hypertension during pregnancy is that often even with high blood pressure numbers, the patient feels normal. High blood pressure is detected by chance, at the next appearance in the antenatal clinic. The absence of clinical manifestations of elevated blood pressure does not exclude the development of dangerous complications.
In order to detect unwanted deviations during pregnancy in time and prevent the development of complications in the mother and fetus, pregnant women need to regularly monitor their blood pressure. It is very important to register for pregnancy in a antenatal clinic in a timely manner. The doctor will promptly detect changes in blood pressure and prescribe the optimal therapy to maintain blood pressure in the normal range. If a woman had high blood pressure before pregnancy, and she is taking medications, it is necessary to adjust the treatment and individually select the drugs that can be taken during pregnancy. To prevent high blood pressure, a pregnant woman should eat a healthy and balanced diet, observe a drinking regimen, and monitor weight gain. The correct recommendations on these issues will also be given by the doctor of the antenatal clinic. A pregnant woman must follow the recommendations and not violate the prescribed therapy.
What to do if a pregnant woman has high blood pressure?
If a pregnant woman regularly monitors blood pressure on her own and notes even a slight increase with good health, she should visit the doctor of the antenatal clinic as soon as possible (before the scheduled next visit). Self-administration of drugs in this case is strictly prohibited. Before visiting a doctor, you can reduce blood pressure by taking a mild sedative based on motherwort or valerian.
Self-administration of drugs in this case is strictly prohibited. Before visiting a doctor, you can reduce blood pressure by taking a mild sedative based on motherwort or valerian.
If necessary, you can consult with an obstetrician-gynecologist of the remote medical advisory panel of the Ambulance and Emergency Medical Care Station. A.S. Puchkov, Moscow by phone: (495) 620-42-44.
When is it necessary to call an ambulance?
If blood pressure rises suddenly, you feel unwell, urgent hospitalization is necessary, and it is advisable for the patient to immediately call an ambulance team. Such signs as: headache, feeling of flashing dots or "flies", a veil before the eyes, pain in the upper abdomen, nausea, vomiting, agitation or depression, along with this - an increase in blood pressure should alert. There may be a high convulsive readiness, which is manifested by twitching of the muscles of the face, neck, upper limbs, loss of consciousness, convulsions are possible.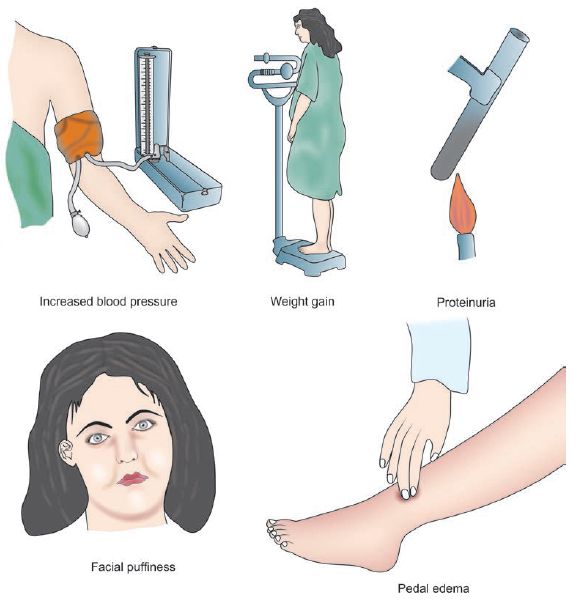
What to do before the ambulance arrives?
First of all, go to bed, if possible, eliminate all unwanted irritants (turn off all sources of noise, close the curtains), do not leave the pregnant woman alone, as convulsions may occur and help will be needed. Give it a position with a raised head end. It is possible to take pressure-lowering drugs prescribed by a doctor. If a woman has not previously taken antihypertensive drugs, then drugs should not be taken on the advice of others.
If an attack of convulsions occurs, the pregnant woman should be laid on a flat surface, turn her head to the side (to prevent aspiration of vomit), protect from damage (cover with a blanket), do not hold physically. After an attack, clean the oral cavity with a napkin from vomit, blood and mucus. Wait for the ambulance to arrive!
The ambulance will arrive quickly and provide the necessary assistance. Hospitalization in this condition is mandatory.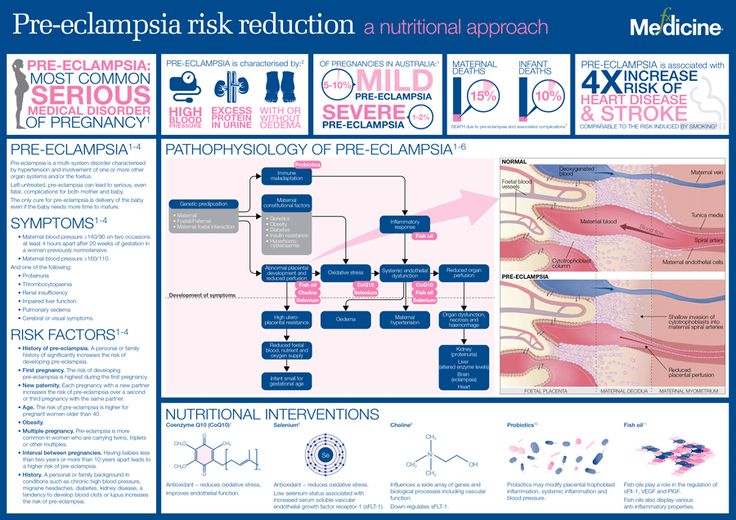 Only in a hospital is it possible to fully monitor the condition of the mother and child, complete therapy and determine the delivery plan.
Only in a hospital is it possible to fully monitor the condition of the mother and child, complete therapy and determine the delivery plan.
We wish you health and happy motherhood!
Chief Specialist
in Obstetrics and Gynecology Arkhipova N.L.
Protein in the urine during pregnancy 1st, 2nd, 3rd trimester: normal, increased, decreased
Content:
- Symptoms of increased protein during pregnancy
- Causes of increased protein in the urine of a pregnant woman
- The norm of protein in the urine during pregnancy
- What to do if the protein in the urine is increased?
- How to pass the analysis correctly?
- Diet adjustment
- Special diet for pregnant women in trimesters
- Physical activity
- Medical treatment
- Why you need to control protein during pregnancy
- How often should I pass urine during pregnancy?
- Prevention of proteinuria
- Q&A
Urinalysis is one of the most important procedures that allows timely detection of the patient's dangerous condition: detection of infections, determination of glucose, calcium, leukocyte levels. Research is also being done to monitor protein in the urine during pregnancy. The deviation of the albumin indicator indicates a deterioration in the patient's health. This pathology in medicine is called proteinuria and can cause premature birth or miscarriage.
Research is also being done to monitor protein in the urine during pregnancy. The deviation of the albumin indicator indicates a deterioration in the patient's health. This pathology in medicine is called proteinuria and can cause premature birth or miscarriage.
Symptoms of high protein during pregnancy
Proteins play an important part in the processes of saturating the cells of the fetus with nutrients, they also help improve hormone production. The level of albumin affects the function of repairing damaged tissues (regeneration process).
The amount of albumin is determined by the general condition of the pregnant woman, which depends on a number of provoking factors. With an increased concentration of protein in the urine, the diagnosis of "proteinuria" is made, which indicates the presence of kidney pathology. Preeclampsia may indicate a primary kidney lesion or a secondary one, which may be the result of various diseases or abnormalities.
Women often complain of back pain accompanied by fever. This condition can be caused by strong pressure on the kidneys from the uterus, the spine. In addition to changes in the level of albumin in the urine, a patient with an abnormal course of pregnancy may show the following symptoms:
This condition can be caused by strong pressure on the kidneys from the uterus, the spine. In addition to changes in the level of albumin in the urine, a patient with an abnormal course of pregnancy may show the following symptoms:
- change in the smell of discharge;
- discoloration of urine;
- toxicosis;
- edema;
- headaches;
- pain in the back and lower back;
- high blood pressure;
- chills;
- loss of appetite;
- blood in urine;
- increased level of fatigue;
- persistent drowsiness;
- severe joint pain due to protein loss;
- numbness of limbs;
- decreased muscle tone;
- involuntary muscle contractions.
Symptoms of proteinuria are directly related to the loss of protein in urine:
- Lack of albumin reduces osmotic pressure, which leads to edema, hypotension and hypovolemia.
- Deficiency of antithrobin leads to a violation of the functions of blood coagulation, which contributes to the formation of blood clots.
- Deficiency of high density lipoproteins in the body during pregnancy contributes to the appearance of atherogenesis.
- The lack of immunoglobulins leads to a decrease in immunity.
- Bleeding tendencies are increased by lack of procoagulants.
- Deficiency of the protein that binds vitamin D causes hypocalcemia and muscle weakness.
There are cases when the presence of an elevated level of albumin in a patient does not manifest itself by any signs. In this case, the disease is asymptomatic. To avoid negative consequences that can harm the health of the patient and the fetus, the doctor prescribes additional diagnostics. It happens that the results of the tests do not reveal the presence of proteinuria in the patient. This is usually due to the presence of vaginal discharge in the urine or physiological causes.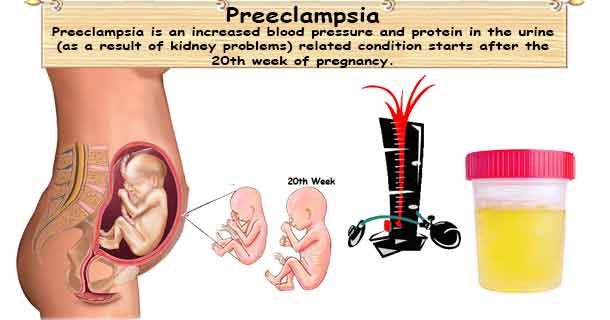
Causes of increased protein in the urine of a pregnant woman
Detection of increased protein in the urine of a pregnant woman is a reason for conducting a comprehensive examination to determine the causes. There are a number of reasons for the increased level of proteins in the urine of pregnant women, which are divided into physiological and pathological.
Causes contributing to the appearance of physiological albumin:
- Strong physical activity during pregnancy is not recommended by a gynecologist, as they lead to increased body fatigue. Overwork is one of the reasons for the appearance of protein in urine.
- Stressful situations can provoke an increased protein.
- Due to the intake of protein-containing foods.
- Long exposure to the street during the cold season can lead to hypothermia, which will adversely affect albumin.
- Protein can also increase due to dehydration. The cause is insufficient fluid intake or increased sweating.

- During pregnancy, the female body begins to rebuild, putting pressure on the kidneys, which can cause the formation of physiological albumin.
Physiological proteinuria does not require medical intervention. However, the signs of pathological proteinuria found in patient indicate the presence of serious health problems: oncology, infectious diseases (including tuberculosis), inflammatory processes, urolithiasis, kidney pathology, and diabetes.
A number of signs of severe preeclampsia:
- an increase in the level of protein in the urine up to 5 grams or more;
- severe deterioration of vision;
- decrease in urine volume (diuresis) to 400 ml. per day;
- increased blood pressure;
- the appearance of edema;
- the appearance of a bluish tint to the mucous membranes and skin.
Urine protein content above 3 g/l. due to a number of reasons:
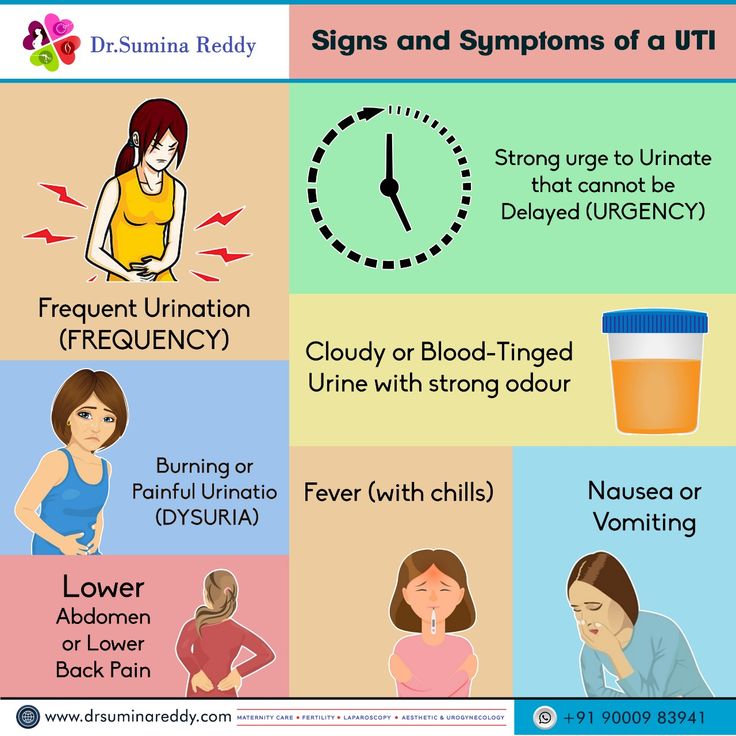
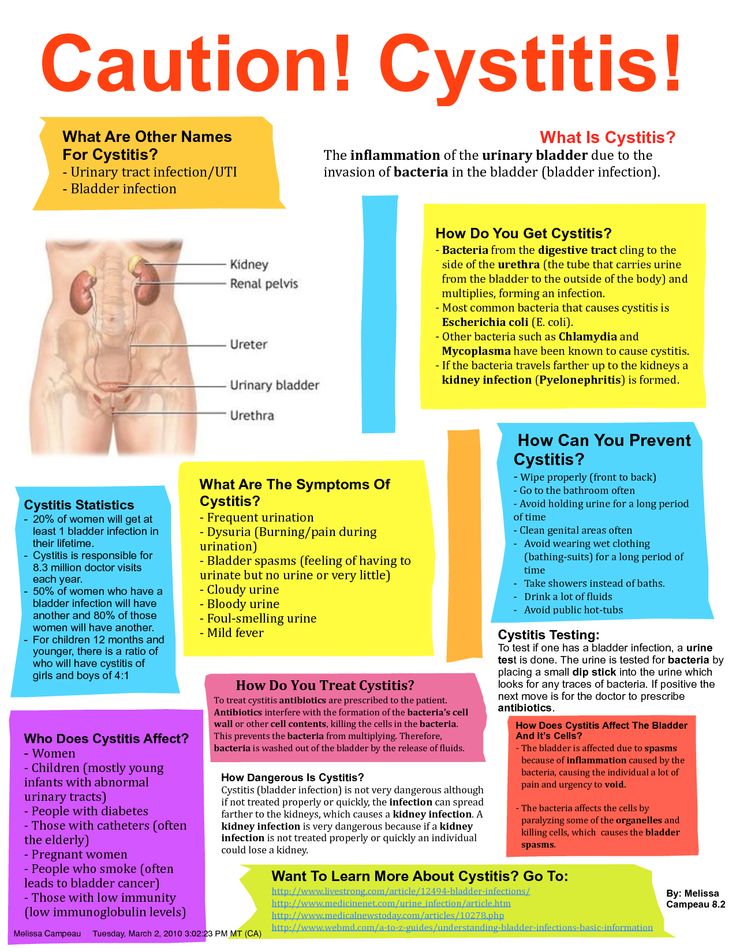
- The occurrence of pyelonephritis in the patient.
 This disease consists in inflammatory processes in the kidneys and the formation of bacteria in the urinary tract.
This disease consists in inflammatory processes in the kidneys and the formation of bacteria in the urinary tract. - Kidney disease associated with infection of the glomeruli. The causative agent of the disease is streptococcus, staphylococcus aureus.
- Presence of a renal cyst. The development of the disease in pregnant women occurs due to alcohol consumption, smoking or X-ray exposure.
- Presence of stones in the bladder or kidneys due to impaired fluid balance. Hereditary factor or stress is also the cause of the presence of the disease.
- With complications of pregnancy. As a rule, preeclampsia is detected in the 3rd trimester of pregnancy. During this period, the female body does not cope well with the functions of saturating the fetus with oxygen and providing the necessary nutrients.
Important to know! Women with impaired hormonal and metabolic functions (diabetes mellitus, hypertension, overweight) are at risk for the development of proteinuria.
Increased protein in the urine of pregnant women may appear in the presence of diseases that do not affect the urinary system:
- Diagnosis of heart failure - the heart muscle does not cope well with the process of pumping blood, which leads to insufficient blood supply to organs and tissues.
- Problems with the thyroid gland.
- Pathological diseases of the central nervous system.
- Injuries and burns.
- Infections of the urinary system.
The norm of protein in the urine during pregnancy
| 1st trimester (weeks 1-13) | 2 trimester (14-26 weeks) | 3rd trimester (27-42 weeks) | |
| Permissible norm of protein in urine, g/l | does not exceed 0.033 | does not exceed 0.04 | does not exceed 0.05 |
For pregnant women, the maximum allowable limits of the norm indicator are reduced:
- protein in the urine during pregnancy 1 trimester should not exceed 0.
 002 g / l;
002 g / l; - protein in the urine during pregnancy 2nd semester should not be higher than 0.1 g / l;
- the level of protein in pregnant women in the 3rd semester should not exceed 0.033 g / l.
An indicator of 0.033 g/l is the norm for protein in the urine of pregnant women.
There are several degrees of high protein in urine:
| Grade | Amount of protein, g/l |
| Moderate increase in albumin | no more than 0.3 |
| Easy level | no more than 1 |
| Moderate | no more than 3 |
| Heavy | over 3 |
With a high level of protein indicators, the patient undergoes additional diagnostics with subsequent treatment of the pathology. If during the examination signs of preeclampsia with symptoms of severe proteinuria are detected, the doctor sends the patient to inpatient treatment.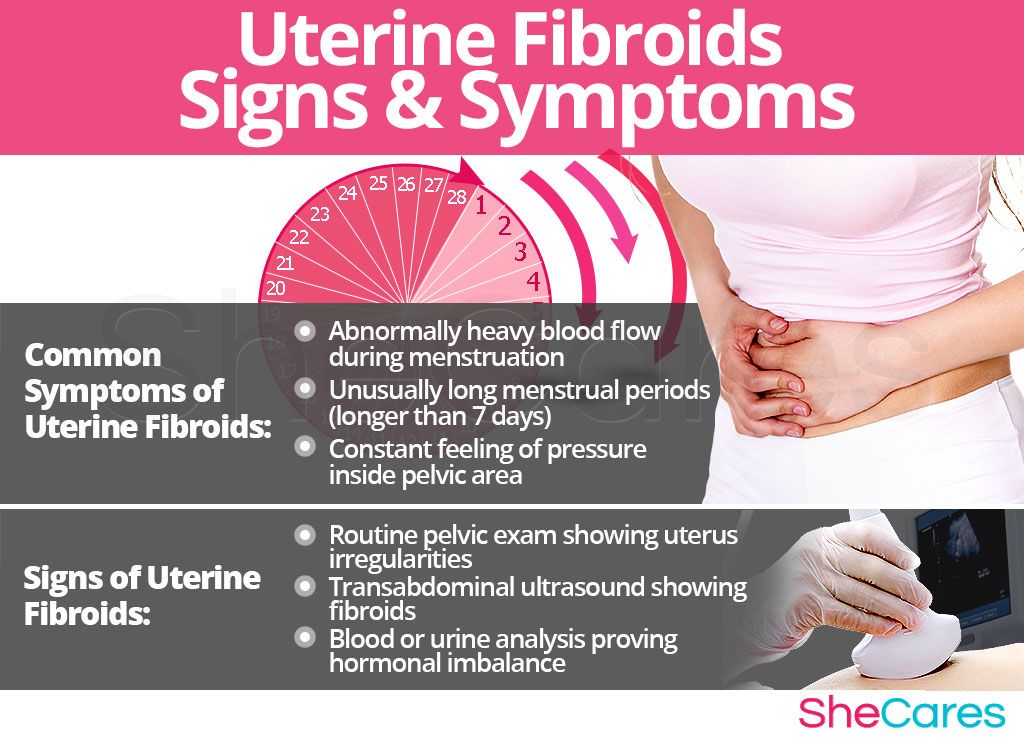 In the hospital, the woman is undergoing enhanced therapy. In the absence of results, the doctor may decide to deliver by caesarean section.
In the hospital, the woman is undergoing enhanced therapy. In the absence of results, the doctor may decide to deliver by caesarean section.
Signs of severe preeclampsia include:
- urinary protein excretion of more than 5 g/day;
- sudden increase in blood pressure;
- severe pain in the back of the head;
- the appearance of severe edema;
- decrease in daily urine output to critical values.
What to do if the protein in the urine is high?
The presence of protein in the urine during pregnancy in the 1st trimester (up to 20 weeks) indicates pathological processes in the kidneys, which manifested themselves even before conception. With a high degree of protein concentration in urine in the second and third trimester, there is a risk of preeclampsia, accompanied by increased pressure and the appearance of swelling of the body.
The doctor makes a decision on the treatment of a patient with an elevated level of protein in the urine on the basis of:
- a complete history taken;
- survey of a pregnant woman;
- results of examination of the patient by a therapist;
- results of daily and general urine analysis;
- results of the conducted studies of the general blood test;
- results of a biochemical blood test;
- ultrasound results;
- results of immunological studies (if necessary).
A protein not exceeding 0.14 g/l and the absence of alarm symptoms do not indicate a disorder in the patient, but require increased medical attention. In such situations, the doctor prescribes a second test for the patient.
How to pass the test correctly?
For an accurate result, you must follow a few rules:
- a special sterile container should be used for urine, which can be purchased at a pharmacy;
- washing the genitals with warm water and soap in the direction from the urethra to the perineum is an important procedure before collecting the analysis;
- the sample must be delivered to the laboratory no later than 120 minutes after urine collection.
Sometimes, in order to more accurately assess the performance of the patient's kidneys, the doctor writes out a referral for a daily urine test.
Based on the results of the analysis, the doctor determines a treatment method aimed at reducing the level of protein in the urine.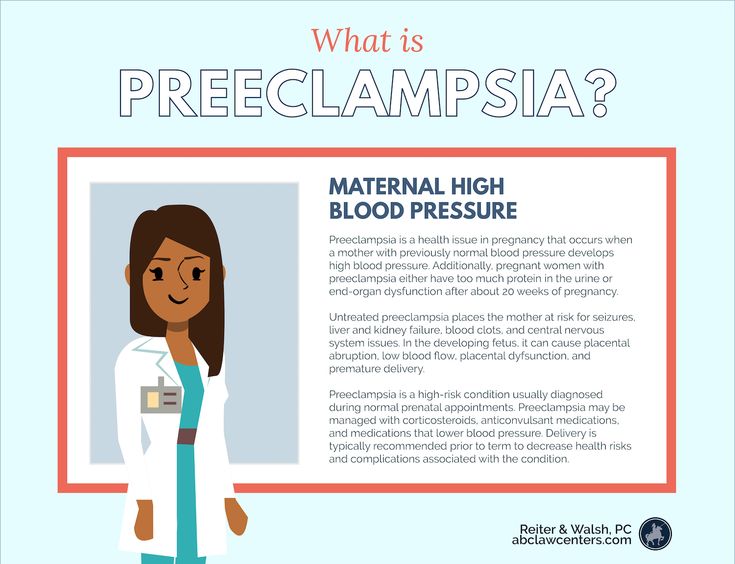
Diet adjustment
This method of protein reduction is most likely to help in the first trimester. Protein in urine can be the result of malnutrition. 5 days before the re-test, it is necessary to abandon the large consumption of foods containing protein (meat, legumes, dairy). Smoked meats, salty, fried, pickled foods are excluded from the diet. In the presence of severe toxicosis, warm food should be consumed.
Lean meats (chicken, turkey), fish are allowed. Be sure to eat fruits and vegetables.
It is recommended to eat small meals five times a day. Proper and balanced nutrition helps to reduce the additional burden on the kidneys.
Special diet for pregnant women by trimesters
wholemeal bread, fruits, juices, fish. It is not recommended to eat fast food, coffee, carbonated and alcoholic drinks. Conservation should also be abandoned.
In the 2nd trimester a pregnant woman needs calcium, vitamins A, C, E, D.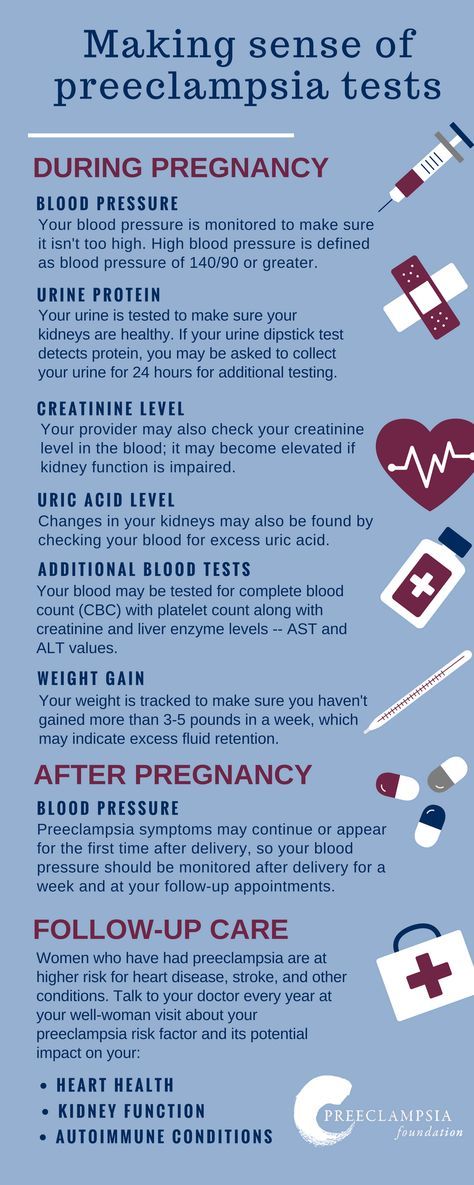 Magnesium, fluorine, iron and potassium are also required. The list of recommended products includes: dairy products, bran bread, fish, cereals, greens, fruits and vegetables. It is worth abandoning conservation, buns, coffee, mushrooms, spicy dishes, alcoholic beverages.
Magnesium, fluorine, iron and potassium are also required. The list of recommended products includes: dairy products, bran bread, fish, cereals, greens, fruits and vegetables. It is worth abandoning conservation, buns, coffee, mushrooms, spicy dishes, alcoholic beverages.
In the 3rd trimester there is a need for vegetable fats, vitamins E and D, retinol and calcium. Fruits, vegetables, various nuts will be useful. It is recommended to eat vegetable soups, cereals and dairy products. You should refrain from salty, fried foods. It is forbidden to drink alcohol. It is undesirable to drink carbonated drinks and coffee.
The recommended products can be used to create a varied, balanced daily menu that contributes to the proper development of the fetus.
Physical activity
The doctor selects a set of physical activity based on the duration of pregnancy. Regular walks, going to the pool, doing special exercises, going to yoga help improve blood flow.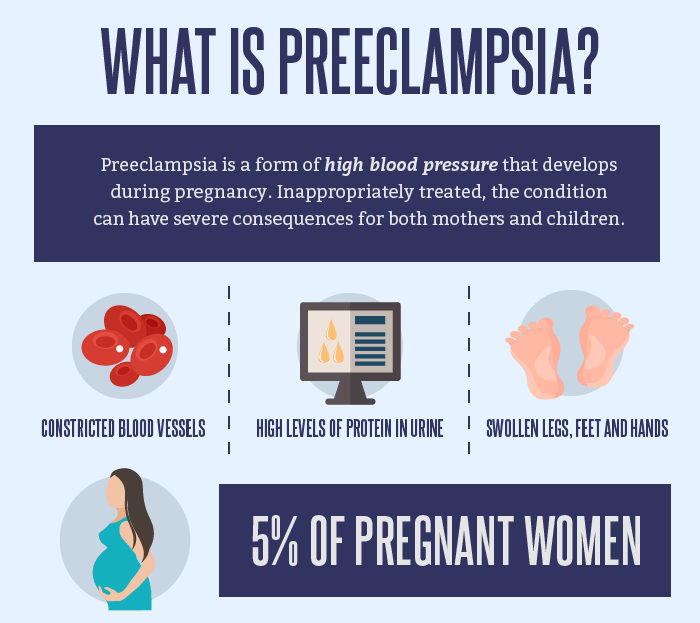 Sometimes, physical activity can lower protein levels in the urine without prescribing medication.
Sometimes, physical activity can lower protein levels in the urine without prescribing medication.
Medical treatment
In the second and third semesters of pregnancy it is important to lead a healthy lifestyle, but albumin in the urine may be associated with developing diseases. With a comprehensive examination and installation of the cause, the doctor prescribes treatment with anti-inflammatory, antimicrobial, as well as sedatives and painkillers. They also prescribe medications aimed at normalizing pressure. Often a doctor prescribes a course of antibiotics.
Why you need to control protein during pregnancy
It is important to control the level of albumin, since the absence or untimely treatment of the appearance of protein in the urine can lead to serious complications of pregnancy:
- The appearance of arrhythmia and shortness of breath.
- The appearance of persistent bouts of vomiting.
- Occurrence of swelling of the internal organs.
 There is also swelling of the hands, feet, face.
There is also swelling of the hands, feet, face. - The occurrence of high blood pressure.
- Occurrence of renal failure.
- The emergence of a threat of termination of pregnancy due to premature aging of the placenta.
- Occurrence of acute fetal oxygen starvation (hypoxia).
With the increase in symptoms, there is a risk of pregnancy complications and a multisystem pathological condition that occurs in the second half of pregnancy (preeclassia) of the patient. Blood pressure rises, convulsions appear, leading to loss of consciousness or coma. And hypertension can cause intracerebral hemorrhage.
The presence of bacterial infections in the urinary system can not only cause blood poisoning, but also infect the baby even before birth.
Any abnormalities detected in the analysis of urine during pregnancy require additional diagnosis and subsequent treatment.
How often should I pass urine during pregnancy?
OAM contributes to the timely detection of disorders in the functioning of body systems and the exclusion of various complications during pregnancy. This type of laboratory research is the most frequently prescribed. In an uncomplicated pregnancy, OAM is prescribed at least three times: at the first visit to the gynecologist, in the second and third trimesters. In fact, patients need to be tested at every scheduled visit to a gynecologist.
This type of laboratory research is the most frequently prescribed. In an uncomplicated pregnancy, OAM is prescribed at least three times: at the first visit to the gynecologist, in the second and third trimesters. In fact, patients need to be tested at every scheduled visit to a gynecologist.
During pregnancy, the female body is rebuilt:
- the cardiovascular system is under heavy stress;
- increases the digestive and urinary systems;
- the composition, volume of blood changes;
- the metabolism is rebuilt.
The work of the kidneys is to remove metabolic products not only from the mother, but also from the fetus.
To rule out possible complications, women undergo this study about 12 times during the entire period of pregnancy. This frequency of studies is aimed at determining the presence of asymptomatic pathologies. For example, in the absence of complaints about the well-being of a patient, bacteria can be detected in the urine.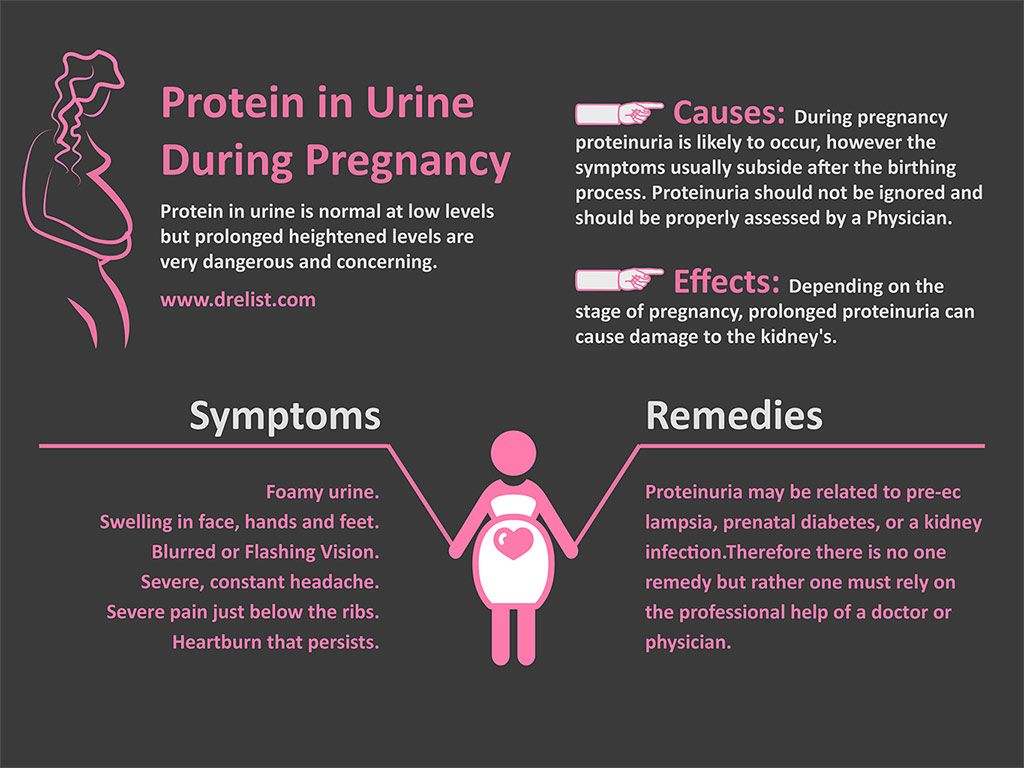 In such cases, the doctor writes out a referral for a bacteriological urine culture test for microflora. Based on the results obtained, the doctor prescribes the correct treatment and prevention of the disease.
In such cases, the doctor writes out a referral for a bacteriological urine culture test for microflora. Based on the results obtained, the doctor prescribes the correct treatment and prevention of the disease.
Prevention of proteinuria
There is no universal scheme for the treatment and prevention of proteinuria. All procedures are prescribed depending on the causes of the failure of the female body. You can prevent the possible occurrence of complications during the planning of conception. It is required to get rid of bad habits, normalize nutrition, lifestyle. It is important to have a complete medical examination. If latent infections are detected, a woman should undergo a course of treatment prescribed by her doctor.
You should visit a gynecologist, it is not recommended to ignore referrals for tests. A woman should not only monitor her own weight and blood pressure, but also follow all the doctor's instructions.
Preventive measures aimed at preventing an increase in the level of protein in the urine during pregnancy come down to a healthy lifestyle, timely delivery of the necessary tests, as well as compliance with all prescriptions of the attending physician.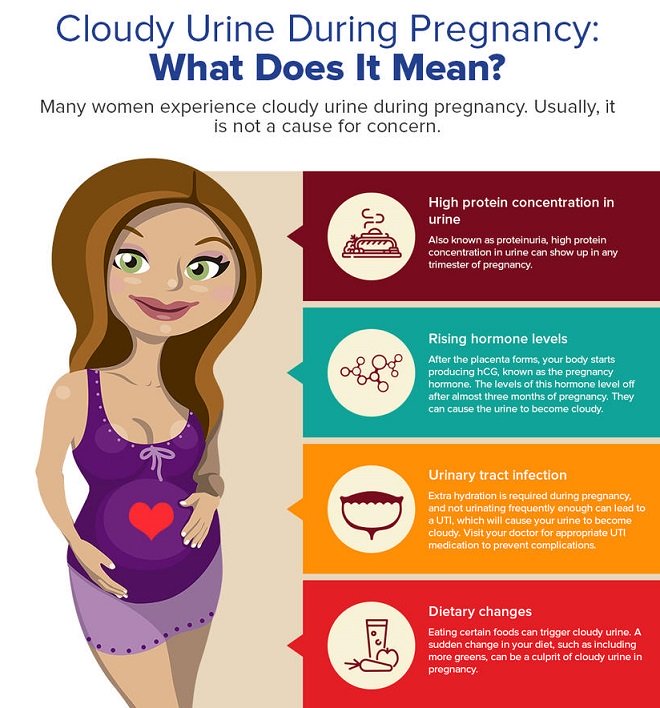
Q&A
✅ How to collect material for protein analysis during pregnancy?
Unfortunately, many women observe the rules of genital hygiene when collecting urine. The results of the study will show the presence of protein if secretions enter the container during urine collection. Urine for general analysis should be collected in the morning. During urination, a certain amount of liquid descends into the toilet bowl, the rest of the urine is collected in a container.
It is important to wash thoroughly with soap before the procedure. To collect urine, special jars are used, which can be purchased at a pharmacy. The use of baby food jars is not recommended. The analysis is recommended to be submitted within 2 hours after its collection. Do not collect urine in advance, this will lead to a distortion of the results of the study.
✅ Can albumin concentration in urine affect its color and smell?
Some diseases of the patient can lead to a change in the color and smell of urine.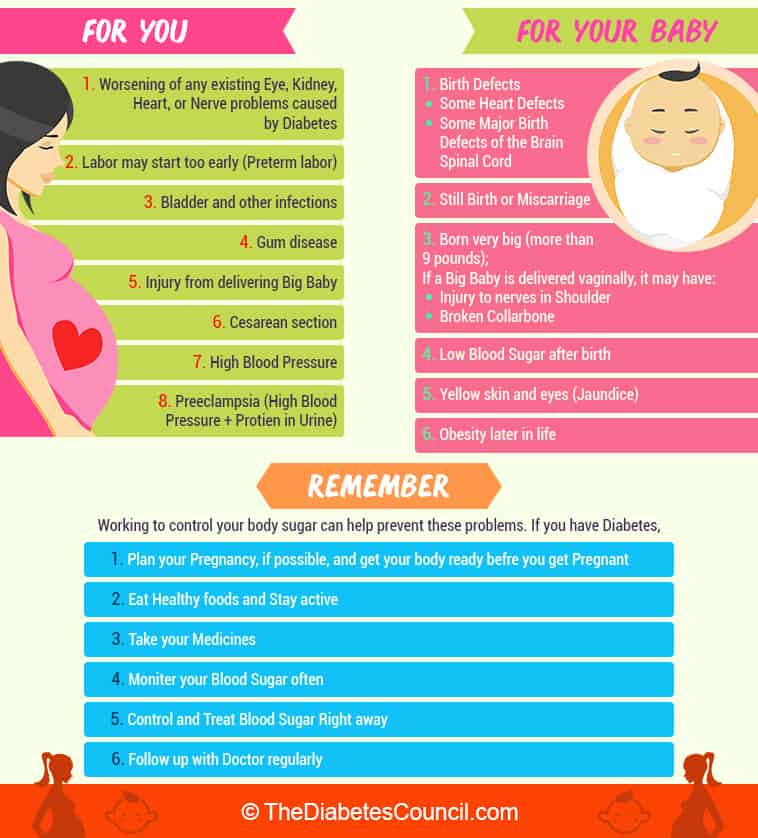 Sometimes it can take on a blue tint. However, elevated protein levels make the urine cloudy and frothy.
Sometimes it can take on a blue tint. However, elevated protein levels make the urine cloudy and frothy.
✅ Is it possible to self-diagnose proteinuria and how to do it at home?
Proteinuria can be self-diagnosed at home. Pharmacies sell special test strips at an affordable price, designed to determine albumin in urine. The cost of the product depends on the number of tests in the package and the manufacturer. The test strips are in a special sealed tube.
Express analysis is carried out as follows: a strip must be placed in the urine for a few seconds. The resulting shade on the strip should be compared with the scale indicated on the product packaging.
Test strips are used not only for self-monitoring of protein levels in urine during pregnancy, but also in medical institutions for express analysis. The accuracy of the results is quite high, provided that the manufacturer's instructions and storage conditions are observed. Important! The test can indicate the presence of albumin in the urine, and the causes and diagnosis are determined by the gynecologist.