Nose bleed and spitting blood
Causes, Prevention and How to Treat
Nationwide Children’s Hospital
Most nosebleeds are a nuisance and stop within 5 to 10 minutes. They usually do not cause enough blood loss to be serious in children who are otherwise healthy. Nosebleeds are common in children because delicate, small blood vessels line the nose and can easily break.
What Causes Nosebleeds
Nosebleeds are most often caused by:
- nose picking or scratching the inside of the nose
- rubbing the nose often
- dry air - Home heating systems may dry the air in your home and also dry the lining of the nose.
- getting hit in the nose or putting an object inside it
- blowing too hard
- colds or allergies
- abnormal tissue (skin) growth inside, such as polyps
Frequent nosebleeds within a few days are usually from the spot where a clot has formed and then comes off.
How to Stop a Nosebleed
Here are a few things you can help your child do to stop a nosebleed. Tell your child to:
- Try to be quiet and calm. Talking, laughing or crying may cause more bleeding.
- Sit up and lean the head forward slightly (Picture 1). Do not lie down, lean back or put their head between their knees.
- Pinch the nostrils tightly closed at the soft part of the nose just below the nasal bone (bone at the top of the nose). For young children, you might need to do this for them.
- Breathe through the mouth.
- Hold the nostrils closed for 5 minutes. Time this with a clock or watch. If the bleeding has not stopped after a full 5 minutes, hold the nostrils closed for 5 more minutes. Call your child’s health care provider if bleeding does not stop after a total of 10 minutes of pinching the nostrils.
- Wet a washcloth or hand towel with cool water. Wring it out and press firmly to the nose and cheeks.

- Do not blow the nose or remove crusts for several hours. If your child needs to blow their nose, remind them to do it very gently. Blowing or wiping the nose may cause the bleeding to start again.
- Spit out any blood that collects in the mouth. Swallowing a large amount of blood may cause your child to have a stomachache or vomit (throw up).
How to Help Prevent Nosebleeds
- Fingernails should be cut short to prevent scratching the inside of the nose.
- Keep fingers and objects out of the nose. Avoid rubbing the nose.
- Teach your child to blow their nose gently.
- Use a cool vaporizer or a humidifier in your child’s bedroom at night, especially during the winter. Be sure to clean the machine once a week.
- Smear a very thin coat of nasal ointment inside each nostril 2 to 3 times a day, especially at bedtime, for 2 weeks during the dry season. Petroleum jelly ointments, such as Vaseline® or Aquaphor® work best.
 This will keep the lining of the nose moist.
This will keep the lining of the nose moist. - For colds or a stuffy nose, use a saline nose spray – 2 sprays to each nostril, 2 or more times a day.
More About Nosebleeds
- If your child takes aspirin, an anticoagulant (anti-clotting) medicine or uses nasal sprays for allergies, be sure to tell the health care provider how often the nosebleeds happen.
Call Your Child’s Health Care Provider If:
- The nosebleed does not stop after 10 minutes of pressure.
- Your child:
- has a nosebleed after an accident or being hit in the face.
- has a clotting disorder, blood in their urine or bruises easily.
- becomes dizzy, pale or has any problems breathing.
Nosebleeds (PDF)
HH-I-84 ©1979, Revised 2021, Nationwide Children’s Hospital
You Might Also Be Interested In
Condition
Nosebleeds (Epistaxis)
Blog
What Is the Right Way to Stop a Nosebleed?
Posterior Nosebleed: Causes and Treatments
What is a posterior nosebleed?
When the tissue at the back of your nose in your nasal cavity is damaged and bleeds, it’s called a posterior nosebleed. Blood may come out of your nostrils, but blood can also leak into your throat. This type of nosebleed can be serious. It may be caused by injuries to your nose, but may also be caused by high blood pressure or other conditions.
Blood may come out of your nostrils, but blood can also leak into your throat. This type of nosebleed can be serious. It may be caused by injuries to your nose, but may also be caused by high blood pressure or other conditions.
You likely have a posterior nosebleed if blood comes out of your nose for more than 20 minutes or the nosebleed happens after you’ve gotten a head, nose, or face injury. Posterior nosebleeds are also more common in children between 2 and 10 years old and adults between 50 and 80 years old.
A nosebleed, also known as epistaxis, can happen for a number of reasons. They’re most common when the blood vessels in the tissue of the inside of your nose, called the mucosa, are damaged and start bleeding, often from scratching, from an object inside your nose rubbing against the tissue, or from an injury to your nose.
When the tissue in the front of your nose or the septum, which divides your two nostrils, is damaged and bleeds, it’s called an anterior nosebleed. In this case, blood usually comes out of the front of your nose. These usually aren’t serious, and they tend to stop bleeding and heal on their own quickly.
In this case, blood usually comes out of the front of your nose. These usually aren’t serious, and they tend to stop bleeding and heal on their own quickly.
Posterior nosebleeds can often have external or environmental causes, including:
- picking or scratching your nose a lot
- blowing your nose too hard or too often
- the skin in your nose becoming more delicate and susceptible to bleeding due to dry, warm weather
- inhaling tobacco smoke, including secondhand smoke
- inhaling chemicals in the workplace, such as gasoline or ammonia
- getting an injury that fractures or breaks parts of your nose or skull
Posterior nosebleeds can result from taking inflammation medications or blood thinners. Some medical conditions can also cause nosebleeds, including:
- a deviated septum, which means that one of your nasal airways is smaller than the other and more likely to bleed
- allergies or the common cold, both of which can cause your nose tissue to become inflamed or make your nasal blood vessels widen and bleed more easily
- disorders that affect your body’s ability to form blood clots or that affect blood vessels, such as hemophilia or high blood pressure
- complication of a recent nose surgery
- tumors in or around your nose
If blood is coming out of the front of your nose, sit up and lean forward to make sure blood doesn’t leak down your throat. Then pinch the front of your nose using your thumb and finger with a clean cloth or tissue to stop the bleeding.
Then pinch the front of your nose using your thumb and finger with a clean cloth or tissue to stop the bleeding.
Keep pinching your nose for 10 to 15 minutes until the bleeding stops and the cut or injury has healed. Putting a bag of ice on top of your nose can help relieve pain or swelling.
If you feel or taste blood dripping down your throat, see your doctor as soon as possible, even if you’re able to stop the nosebleed. If your nose won’t stop bleeding, put gauze or cotton in your nose to control the bleeding.
Don’t lean back or lie down when you have a nosebleed, as the blood can drip down your throat, which can feel uncomfortable.
After you’ve stopped your nosebleed, don’t pick or blow your nose for a few hours or longer to let the injury heal. Don’t smoke, which irritates the nasal passages, and don’t put any foreign objects in your nose, such as cotton swabs.
To prevent nosebleeds, use a humidifier to keep the air around you moist or use a nasal spray to keep the tissue inside your nose from getting too dry.
Nosebleeds aren’t usually serious. But if your nosebleed lasts longer than 20 to 30 minutes, see your doctor to find out what’s causing it.
Your doctor may be able to treat your nosebleed with medications or other tools, including:
- inflatable balloons that deliver saline into your nasal cavity and stop bleeding
- hot water irrigation tools to wash out your nasal cavity and soothe irritation
- chemicals or electric tools, such as probes, that can seal off blood vessels
- medications that are applied to the inside of your nose
- laser beam therapy that seals off blood vessels
- embolization, in which your doctor plugs up blood vessels to stop bleeding
In some cases, your doctor may want to perform surgery to treat a persistent nosebleed, especially if it was caused by an injury or head trauma.
If bleeding or abnormal discharge keeps happening over and over, even if you’ve treated it or tried to prevent nosebleeds, see your doctor to find out if any objects or growths, such as tumors, are causing your nosebleeds to reoccur.
Recurrent nosebleeds: description of the disease, causes, symptoms, cost of treatment in Moscow
array ( [0] => Violation of the work of internal organs and systems with frequent volumetric bleeding; [1] => General exhaustion of the body; [2] => Anemia. )
An otolaryngologist deals with the diagnosis and treatment of the disease.
Disease description
Nosebleeds or epistaxis can often occur regularly. It should not be ignored and considered the norm, since this condition often indicates the presence of certain pathologies that require mandatory treatment. Stopping nosebleeds is usually not difficult, which is why not all patients seek medical help in a timely manner to determine the cause of the problem and its treatment. If there is frequent bleeding from the nose, a visit to the doctor is required.
Recurrent nosebleeds can occur at any age due to external and internal causes.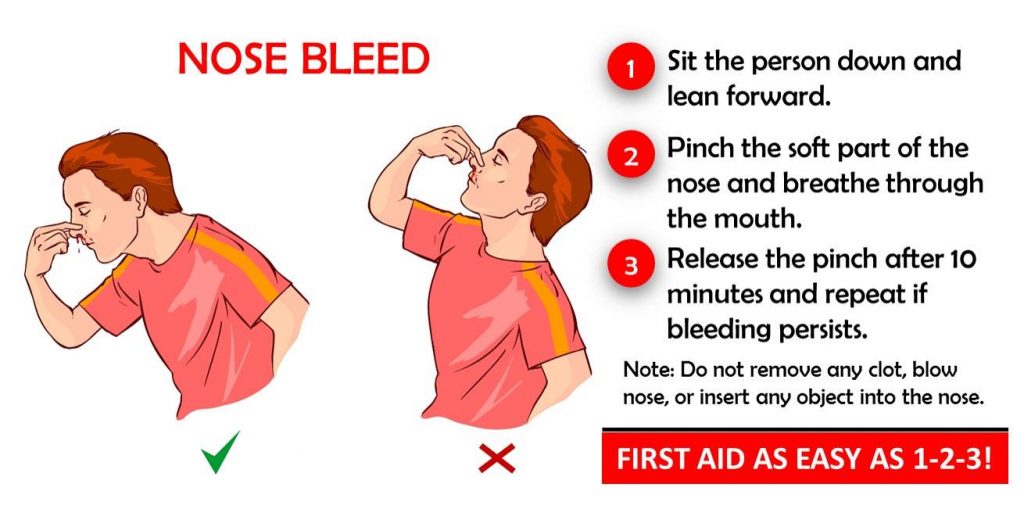 Frequent nosebleeds in adults have a variety of causes.
Frequent nosebleeds in adults have a variety of causes.
It is almost never possible to independently establish the cause of the pathology in a patient. Due to the fact that the nasal mucosa is permeated with a large number of vessels, even a slight damage to it provokes bleeding. For a traumatic reason, it is predominantly single or repeated several times over a short period of time - until the tissues recover. In other cases, with recurrent nosebleeds, medical assistance is indispensable. Nosebleeds for which no cause is known is a serious cause for concern.
Causes of pathology
The causes of nosebleeds, which tend to recur regularly, are divided by doctors into local and general. Local factors that cause bleeding include the following:
- foreign body in the nasal cavity - this phenomenon is more often observed in young children, who, out of interest, can stick a soft or hard object into their nose. It will regularly damage the mucosa and, without timely extraction, will even cause the development of an ulcer on it, which will bleed especially strongly at the slightest violation of the integrity of its surface.
 Frequent bleeding from the nose in a child, be sure to check the nasal cavity for the presence of a foreign body;
Frequent bleeding from the nose in a child, be sure to check the nasal cavity for the presence of a foreign body; - regular mechanical damage to the nasal mucosa is a common cause of frequent nosebleeds in children. Damage can be done with a fingernail or pencil if children have a tendency to pick their nose. After the cause of injury is eliminated, the tissues are restored, and the problem goes away without further treatment;
- larvae of worms - a number of parasites at a certain stage of their development migrate through the body and, penetrating into the nasal cavity, damage the vessels of the mucous membrane. Because of this, moderate to severe bleeding develops. They stop after the parasite leaves the nasal region and resume with the next stage of larval development and migration;
- neoplasms of the nasal cavity - can be a benign or malignant tumor. In children, a benign neoplasm most often occurs. Malignant tumors in most cases are diagnosed in old age in men who are prone to alcohol abuse and smokers;
- Nasal septal defects are congenital disorders that cause bleeding in childhood.
 Without restoring the normal state of the nasal septum, it is almost impossible to eliminate them;
Without restoring the normal state of the nasal septum, it is almost impossible to eliminate them; - chronic ENT diseases, in which there is an overflow of vessels with blood;
- degeneration of the nasal mucosa - frequent bleeding from the nose, while not abundant;
- dryness of the nasal mucosa.
Common causes of recurrent nosebleeds are associated with pathologies of systems and organs in which changes occur in the nasal mucosa, as well as in the walls of blood vessels, which makes them brittle. The most common violations of this nature are:
- congenital excessive vascular fragility;
- severe infectious diseases in which there is a strong increase in temperature. With them, bleeding is repeated several times a day and stops only after the temperature stabilizes;
- vasculitis - inflammation of the walls of blood vessels, which is not of an infectious nature;
- underdevelopment of the vascular walls - a congenital pathology, which most often has a hereditary character;
- deficiency of vitamins C and K - with almost constant bleeding from the nose;
- pulmonary tuberculosis;
- cancer of various parts of the respiratory system;
- significant increase in blood pressure that occurs regularly.
 In this case, when the vessels are as crowded as possible, they burst;
In this case, when the vessels are as crowded as possible, they burst; - various diseases of the circulatory system and blood;
- chronic intoxication of the body - frequent bleeding from the nose, the causes of which are not always easy to establish, can annoy for a very long time.
Whatever causes nosebleeds, it must be treated. Regular blood loss is a serious danger, and it is extremely impossible to leave it unattended. During puberty, against the background of hormonal changes, a temporary decrease in the strength of the vessels of the nasal mucosa may occur and, as a result, the development of frequent bleeding, but even in this case, a doctor's consultation is required. The specialist will help in such a situation to prevent the appearance of anemia and properly support the body until the problem is eliminated.
When there is blood from the nose, the causes in an adult and in a child of the appearance of a problem are in many ways similar. This also determines similar treatment.
This also determines similar treatment.
Diagnostics
To determine the violation, the doctor, in addition to questioning the patient about his condition, conducts an examination, which determines the following: is there bleeding from the posterior parts of the nasal cavity, damage to the mucosa and neoplasms in the front of the nose. To obtain maximum information, rhinoscopy, endoscopic examination of the nasal cavity, and pharyngoscopy are prescribed. Frequent nosebleeds require a full examination. The causes of frequent nosebleeds need to be established precisely. Without this, therapy will not be more effective.
To obtain information about blood parameters, its general analysis is performed, supplemented by studies to determine clotting indicators and iron levels (to determine the degree of anemia). This will allow you to understand why nosebleeds often come.
Prevention of nosebleeds
To reduce the risk of developing recurrent nosebleeds, preventive measures aimed at reducing the likelihood of external causes of the problem, as well as part of the internal ones, help. The main recommendations for preventing the problem are as follows:
The main recommendations for preventing the problem are as follows:
- use of humidifiers if the air is excessively dry;
- the use of antipyretics when the temperature rises to more than 38 about ;
- timely removal of benign neoplasms of the nasal cavity;
- smoking cessation, since nicotine smoke contributes to the development of mucosal atrophy;
- refusal of alcohol, especially strong - it leads to a sharp expansion of blood vessels, which may cause their rupture;
- explaining to children from early childhood the danger of picking their nose and sticking foreign objects into it;
- regular monitoring of blood pressure in the presence of hypertension;
- prevention of contact with irritants and aggressive chemicals on the mucous membrane.
Prevention cannot completely protect against the occurrence of a violation. Because of this, if there is often blood from the nose, the reasons must be determined without fail.
Performed by
Mazlakova Rita Arbievna
Otorhinolaryngologist
Consult this doctor
possible by phone
+74952233088
All fields marked with "*" are required
By clicking on the "Make an appointment" button, you agree to the processing of personal data.
Thank you! Your application has been accepted.
Our manager will contact you in 5 minutes.
Pulmonary bleeding. What is pulmonary hemorrhage?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests.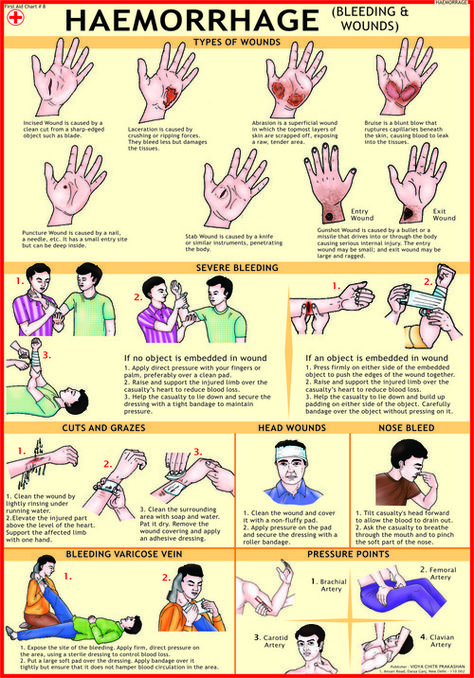 For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor.
Pulmonary bleeding is a dangerous complication of various diseases of the respiratory system, accompanied by the outflow of blood from the bronchial or pulmonary vessels and its release through the airways. Pulmonary bleeding is manifested by coughing with the release of liquid scarlet blood or clots, weakness, dizziness, hypotension, fainting. With a diagnostic purpose in case of pulmonary bleeding, X-ray of the lungs, tomography, bronchoscopy, bronchography, angiopulmonography, selective angiography of the bronchial arteries is performed. Stopping pulmonary hemorrhage may include conservative hemostatic therapy, endoscopic hemostasis, endovascular embolization of bronchial arteries. In the future, to eliminate the source of pulmonary bleeding, surgical treatment is indicated, taking into account etiological and pathogenetic factors.
ICD-10
R04. 8 R04.2
8 R04.2
- Causes of pulmonary hemorrhage
- Pathogenesis
- Classification
- Symptoms of pulmonary haemorrhage
- Diagnostics
- Treatment of pulmonary hemorrhage
- Forecast
- Treatment prices
General
Pulmonary bleeding is one of the most dangerous conditions that complicate the course of a wide range of diseases of the broncho-pulmonary and cardiovascular systems, diseases of the blood system and hemostasis. Therefore, the problem of providing emergency care for pulmonary hemorrhage is relevant for specialists in the field of pulmonology, phthisiology, oncology, cardiology, hematology, and rheumatology. Delay in carrying out emergency hemostatic measures can cause rapid death of patients. Depending on the severity of blood loss and the condition that caused it, mortality from pulmonary hemorrhage varies from 5-15% to 60-80%. Among patients with pulmonary hemorrhage, persons of mature age (50-55 years) with aggravated somatic pathology predominate.
Pulmonary bleeding
Causes of pulmonary hemorrhage
The frequent occurrence of hemoptysis and pulmonary hemorrhage is determined by the polyetiology of these conditions. The first place in the structure of causes of pulmonary hemorrhage belongs to pulmonary tuberculosis (over 60% of cases). A significant role in the etiology of pulmonary bleeding is given to non-specific and purulent-destructive diseases - bronchitis, chronic pneumonia, bronchiectasis, pneumosclerosis, abscess and gangrene of the lung.
Often the causes of pulmonary bleeding are bronchial adenoma, malignant tumors of the lungs and bronchi, parasitic and fungal infections (ascariasis, echinococcosis, schistosomiasis, actinomycosis of the lungs), pneumoconiosis (silicosis, silicosis). Pulmonary bleeding may be due to inadequate local hemostasis after endoscopic or transthoracic biopsy, surgery on the lungs and bronchi. Foreign bodies of the bronchi, chest injuries (fractured ribs, etc. ) can lead to pulmonary bleeding.
) can lead to pulmonary bleeding.
In addition to respiratory diseases, hemoptysis and pulmonary bleeding can occur with diseases of the heart and blood vessels: pulmonary embolism, mitral stenosis, aortic aneurysm, arterial hypertension, atherosclerotic cardiosclerosis, myocardial infarction. Relatively rare causes of pulmonary bleeding include pulmonary endometriosis, Wegener's granulomatosis, systemic capillaritis (Goodpasture's syndrome), hereditary telangiectasia of the skin and mucous membranes (Rendu-Osler syndrome), hemorrhagic diathesis, etc. Pulmonary bleeding may be due to a violation of blood clotting with prolonged and poorly controlled anticoagulant therapy.
Factors provoking pulmonary bleeding can be physical or emotional stress, infections, insolation, hemodynamic disorders, pulmonary hypertension, menstruation (in women), etc.
Pathogenesis
The morphological basis for pulmonary hemorrhage is thinned and aneurysmally dilated branches of the pulmonary artery or bronchial arteries, as well as pulmonary veins. Rupture or erosion of altered vessels may be accompanied by pulmonary hemorrhage of varying severity. At the same time, the magnitude of pulmonary bleeding largely determines the caliber of the damaged vessel, and the severity of the disorders occurring in the body determines the rate and intensity of blood loss.
Rupture or erosion of altered vessels may be accompanied by pulmonary hemorrhage of varying severity. At the same time, the magnitude of pulmonary bleeding largely determines the caliber of the damaged vessel, and the severity of the disorders occurring in the body determines the rate and intensity of blood loss.
Developing in further disorders are associated with obstruction of the airways by outflowing blood and the actual amount of blood loss. Getting into the bronchi even in small quantities, the blood causes the development of obstructive atelectasis and aspiration pneumonia. In turn, this leads to a decrease in the volume of functioning lung tissue, gas exchange disorders, a progressive increase in respiratory failure, and hypoxemia.
Hypovolemia and anemia accompanying acute and chronic (with recurrent pulmonary bleeding) blood loss lead to a general disruption of homeostasis. This is primarily expressed in the activation of fibrinolytic and anticoagulant mechanisms, which causes an increase in the tendency to hypocoagulation, an increase in the permeability of the vascular walls. The cumulative result of such changes determines the pathological readiness of the body for the resumption of pulmonary hemorrhage at any time.
The cumulative result of such changes determines the pathological readiness of the body for the resumption of pulmonary hemorrhage at any time.
Classification
In the clinical aspect, it is important to distinguish between pulmonary hemorrhage and another, less dangerous, but more common condition - hemoptysis. Hemoptysis differs in volume and rate of blood release from the airways. In some cases, hemoptysis precedes massive pulmonary hemorrhage, and therefore also requires a complete clinical and radiological examination and urgent measures to stop it. Usually, hemoptysis is understood as coughing up sputum with streaks or an admixture of blood; while the amount of blood released does not exceed 50 ml per day. An increase in the volume of coughed up blood is regarded as pulmonary bleeding.
Depending on the amount of blood released when coughing, there are small pulmonary bleeding (50-100 ml per day), medium (100-500 ml per day), heavy or severe pulmonary bleeding (over 500 ml of blood per day).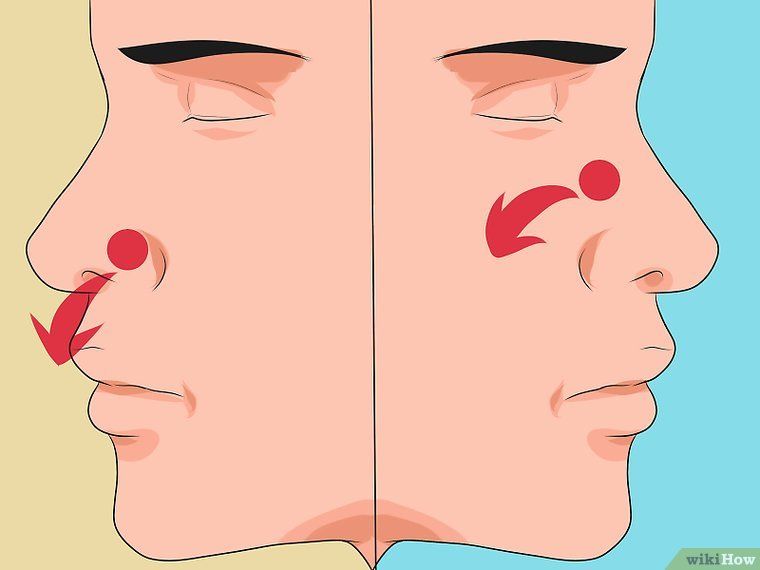 Especially dangerous are "lightning" heavy bleeding that occurs simultaneously or within a short period of time. As a rule, they lead to acute asphyxia and death.
Especially dangerous are "lightning" heavy bleeding that occurs simultaneously or within a short period of time. As a rule, they lead to acute asphyxia and death.
Unlike hemothorax, pulmonary bleeding refers to external bleeding. Mixed pulmonary-pleural bleeding also occurs.
Symptoms of pulmonary hemorrhage
The clinic of pulmonary hemorrhage consists of a symptom complex due to general blood loss, external bleeding and pulmonary heart failure. The onset of pulmonary bleeding is preceded by the appearance of a strong persistent cough, initially dry, and then with the separation of mucous sputum and scarlet blood or coughing up blood clots. Sometimes shortly before pulmonary bleeding in the throat there is a sensation of gurgling or tickling, a burning sensation in the chest on the side of the lesion. In the initial period of pulmonary hemorrhage, the separated blood has a bright red color, later it becomes darker, rusty brown. When the bronchus is obstructed by a blood clot, pulmonary bleeding may stop on its own.
When the bronchus is obstructed by a blood clot, pulmonary bleeding may stop on its own.
The general condition is determined by the severity of blood loss. Patients with pulmonary hemorrhage are characterized by a frightened appearance, weakness, pallor of the skin of the face, cold sticky sweat, acrocyanosis, decreased blood pressure, tachycardia, dizziness, noise in the ears and head, shortness of breath. With abundant pulmonary bleeding, visual impairment (amaurosis), fainting, sometimes vomiting and convulsions, asphyxia may occur. On the 2-3rd day after pulmonary bleeding, a picture of aspiration pneumonia may develop.
Diagnostics
To establish the cause of pulmonary bleeding, a diagnostic consultation is often required with the participation of specialists in pulmonology, phthisiatricians, thoracic surgeons, oncologists, radiologists, vascular surgeons, cardiologists, otolaryngologists, rheumatologists, and hematologists. On auscultatory examination, moist medium bubbling rales in the lungs and gurgling rales in the sternum are determined. With aspiration of blood, there is a shortening of percussion sound, pleural friction noise, weakening of breathing and voice trembling.
On auscultatory examination, moist medium bubbling rales in the lungs and gurgling rales in the sternum are determined. With aspiration of blood, there is a shortening of percussion sound, pleural friction noise, weakening of breathing and voice trembling.
The source of bleeding can presumably be determined by the color of the blood. Isolation of scarlet, foamy blood, as a rule, indicates pulmonary hemorrhage; blood dark red, coffee color - for gastrointestinal bleeding. Sometimes the clinic of hemoptysis can simulate nosebleeds, therefore, for the purpose of differential diagnosis, it is important to consult an otolaryngologist and rhinoscopy. In doubtful cases, in order to exclude bleeding from the gastrointestinal tract, endoscopy may be required.
To confirm the source of bleeding in the lungs, an X-ray examination is performed: polypositional radiography of the lungs, linear and computed tomography, MRI of the lungs. If necessary, they resort to an in-depth x-ray examination: bronchography, bronchial arteriography, angiopulmonography.
The leading method of instrumental diagnosis in pulmonary bleeding is bronchoscopy. Endoscopic examination allows visualization of the source of bleeding in the bronchial tree, aspiration of lavage water, forceps and scarification biopsy from the area of pathological changes.
In peripheral blood with pulmonary bleeding, hypochromic anemia, poikilocytosis, anisocytosis, and a decrease in hematocrit are detected. In order to assess the severity of changes in the coagulation and anticoagulation systems of the blood, the coagulogram and the number of platelets are examined. In sputum tests (microscopic, PCR, for acid-resistant mycobacteria), atypical cells, Mycobacterium tuberculosis, indicating the etiology of pulmonary hemorrhage, can be determined.
Treatment of pulmonary hemorrhage
In the treatment of pulmonary hemorrhage, conservative methods, local hemostasis, palliative and radical surgical interventions are used. Therapeutic measures are used for pulmonary bleeding of small and medium volume. The patient is assigned to rest, given a semi-sitting position, venous tourniquets are applied to the limbs. Tracheal aspiration is performed to remove blood from the lumen of the trachea. Asphyxia requires emergency intubation, blood suction and mechanical ventilation.
Therapeutic measures are used for pulmonary bleeding of small and medium volume. The patient is assigned to rest, given a semi-sitting position, venous tourniquets are applied to the limbs. Tracheal aspiration is performed to remove blood from the lumen of the trachea. Asphyxia requires emergency intubation, blood suction and mechanical ventilation.
Drug therapy includes the introduction of hemostatic drugs (aminocaproic acid, calcium chloride, vikasol, sodium etamsylate, etc.), antihypertensive drugs (azamethonium bromide, hexamethonium benzosulfonate, trimethaphan camsylate). In order to combat posthemorrhagic anemia, a replacement transfusion of erythrocyte mass is performed; to eliminate hypovolemia, native plasma, rheopolyglucin, dextran, or gelatin solution are injected.
If conservative measures are ineffective, they resort to instrumental stopping of pulmonary bleeding using local endoscopic hemostasis. Therapeutic bronchoscopy should be performed in the operating room, ready to proceed to an emergency thoracotomy.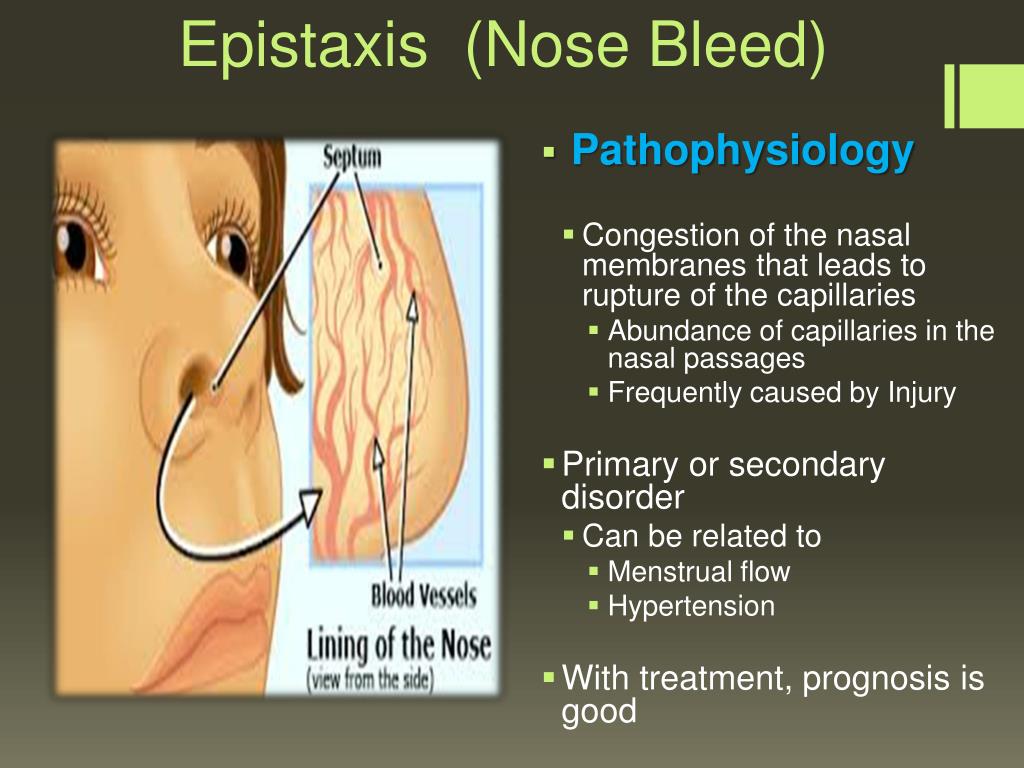 For endoscopic hemostasis, local applications with adrenaline, etamsylate, hydrogen peroxide solution can be used; installation of a hemostatic sponge, electrocoagulation of the vessel at the site of blood outflow, short-term occlusion with an inflatable balloon of the Fogarty type or temporary obturation of the bronchus with a foam rubber seal. In some cases, endovascular embolization of bronchial arteries, performed under x-ray control, is effective.
For endoscopic hemostasis, local applications with adrenaline, etamsylate, hydrogen peroxide solution can be used; installation of a hemostatic sponge, electrocoagulation of the vessel at the site of blood outflow, short-term occlusion with an inflatable balloon of the Fogarty type or temporary obturation of the bronchus with a foam rubber seal. In some cases, endovascular embolization of bronchial arteries, performed under x-ray control, is effective.
In most cases, these methods allow you to temporarily stop pulmonary bleeding and avoid emergency surgery. The final and reliable hemostasis is possible only with the surgical elimination of the source of bleeding.
Palliative interventions for pulmonary hemorrhage may include operative collapse therapy for pulmonary tuberculosis (thoracoplasty, extrapleural filling), ligation of the pulmonary artery, or a combination of this surgical technique with pneumotomy. Palliative interventions are resorted to only in forced situations, when a radical operation is impossible for some reason.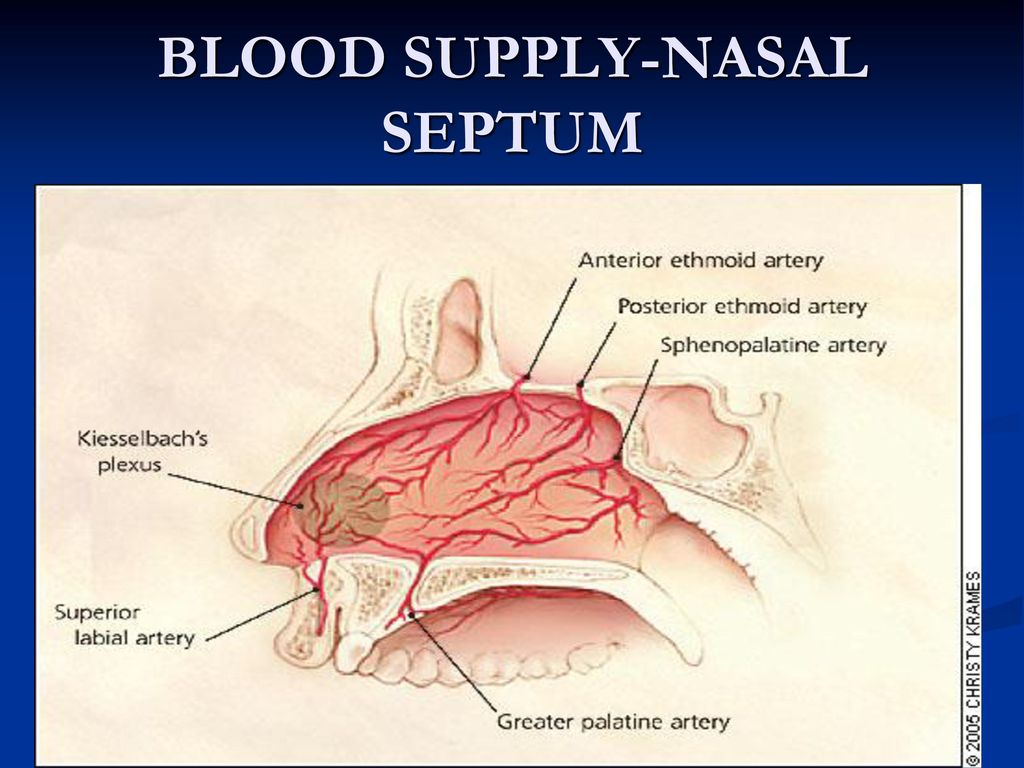
Radical operations for pulmonary bleeding involve the removal of all pathologically altered areas of the lung. They can consist in partial resection of the lung within healthy tissues (marginal resection, segmentectomy, lobectomy, bilobectomy) or removal of the entire lung (pneumonectomy).
Forecast
Even a single and spontaneously stopped pulmonary bleeding is always potentially dangerous in terms of resumption. Abundant pulmonary bleeding threatens the life of the patient. In severe cases, death occurs as a result of asphyxia caused by blockage of the airways by blood clots and simultaneous spastic contraction of the bronchi. The percentage of postoperative complications and mortality in operations performed at the height of pulmonary bleeding is more than 10 times higher than in elective operations.
You can share your medical history, what helped you in the treatment of pulmonary hemorrhage.
References
- Clinical guidelines for the treatment of patients with pulmonary hemorrhage / Association of Thoracic Surgeons of Russia.