Staying pregnant with pcos
Pregnant with PCOS - Here's Everything You Need to Know
For many women with PCOS, getting pregnant is a major step and a reason to celebrate! While the challenges of PCOS persist with pregnancy, there are measures you can take to increase your chances of a normal pregnancy. Especially during pregnancy, it’s essential to stay in close contact with your doctors and PCOS care team. Here are some first points about PCOS and pregnancy you may be interested in learning about, however your doctor and care team will know what will work best for you and your situation, so make sure you note down any questions you may have for the next visit.
Now let’s dive right in:
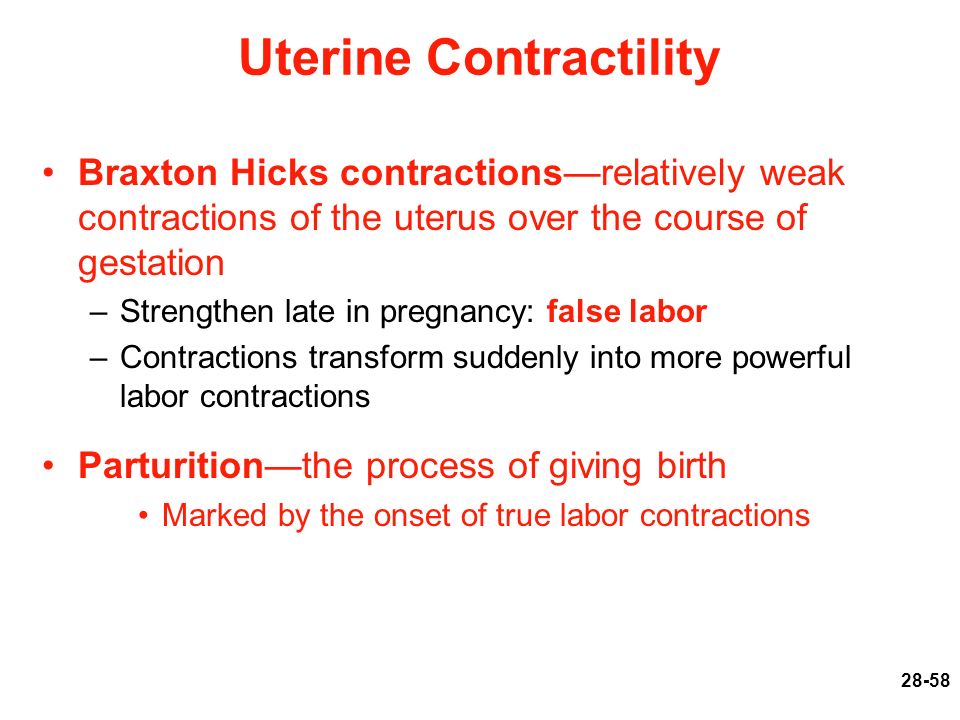
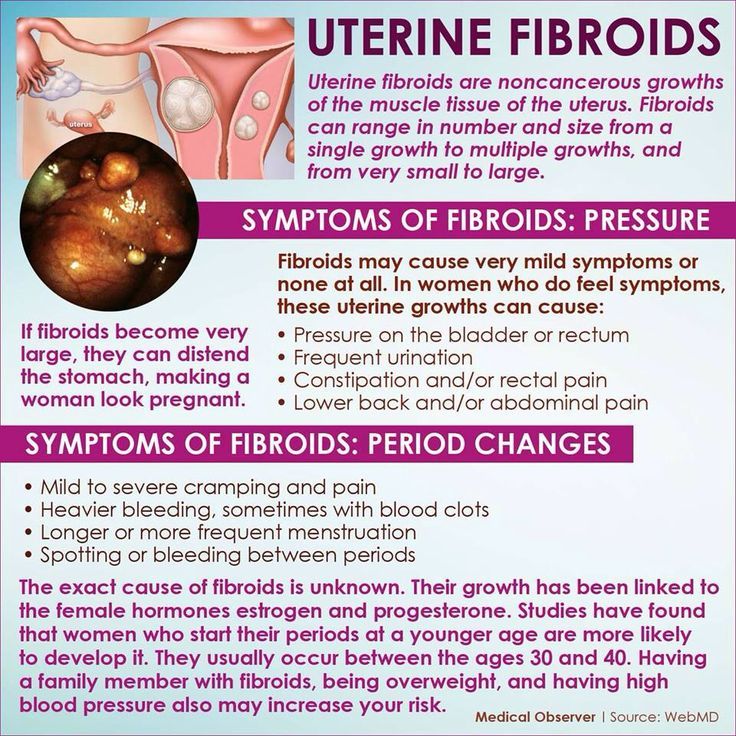
Pregnant women with PCOS need to be more alert than women without PCOS for possible complications. It is well-known that PCOS puts women at higher risk for complications during pregnancy and delivery.1 The two main complications that are associated with PCOS are increased risk for a miscarriage in early pregnancy and gestational diabetes.
Women with PCOS are three times more likely to experience a miscarriage in the first trimester of pregnancy than women without PCOS.2 Some women with PCOS may already have diabetes prior to pregnancy and many are vulnerable to gestational diabetes. The rate of C-section deliveries is also higher in women with PCOS.
However, the risk for some pregnancy complications can be prevented by maintaining a healthy weight and limiting the amount of weight gain before and during pregnancy.
Pregnancy Complications in Women with PCOSA meta-analysis in 2006 found that PCOS can increase the risk of gestational diabetes, pregnancy-induced hypertension (PIH), preeclampsia, and preterm birth.4 This may also be connected to the fact that women with PCOS will most likely have other pre-existing medical conditions, such as hyperandrogenemia, hyperinsulinemia, and obesity.
Miscarriage or Early Pregnancy LossSeveral studies show an increase in the chance for miscarriage in women with PCOS, but other researchers attribute the increase to other factors such as obesity, increased age, and use of fertility treatments. 5,6
5,6
In addition, women treated with ovulation-inducing medications may have a higher risk of spontaneous miscarriage compared with normally ovulating women.7 Metformin can be used to reduce miscarriage risk in pregnant women with PCOS. It is classified as a Category B drug, which means that it does not cause fetal abnormalities in animal studies. Make sure to check your treatment plan and all the medications and supplements you are taking with your doctor and care team.
Gestational DiabetesGestational diabetes mellitus (GDM) is an increase in the mother’s blood sugar levels during pregnancy, which typically resolves after the birth of the baby.8 However, there is a good chance that you will develop it again in future pregnancies. This type of diabetes usually occurs during the last half of pregnancy. Gestational diabetes is different from diabetes mellitus as the latter is more severe and does not go away after pregnancy.
In healthy women, blood insulin levels typically increase up to three times during pregnancy. The increase is about sevenfold in women with PCOS. Increased blood sugar in the mother can cause fetal anomalies and even miscarriage.
Infants of mothers with GDM are often larger than other babies, resulting in the need for cesarean delivery. Taking metformin before and after a pregnancy reduces the rate of GDM to 7 percent.
PreeclampsiaPre-eclampsia is described as a dangerous rise in blood pressure during pregnancy, accompanied by swelling of the legs and the presence of protein in the urine. When left untreated it can turn into eclampsia, causing kidney and liver damage, seizures, and in rare cases, even death. Maintaining normal blood pressure is the most important preventive measure you can take. If you notice any change in your well-being during pregnancy, make sure to check in with your doctor and care team.
Pregnancy-Related High Blood Pressure (Gestational Hypertension)This type of hypertension usually develops about halfway through the pregnancy. Unlike pre-eclampsia and eclampsia, there are no proteins excreted in the urine. Blood pressure often normalizes two to three months after delivery.
Unlike pre-eclampsia and eclampsia, there are no proteins excreted in the urine. Blood pressure often normalizes two to three months after delivery.
Lowering your high blood pressure, losing at least 10 percent of your weight if you are overweight or obese, and regular exercise can reduce your risk of developing gestational hypertension.
Preterm BirthThe rate of preterm delivery is increased in women with PCOS, particularly those with high androgen levels in the blood.9 The rate is higher by 67% for multiple pregnancies. Causes of preterm delivery are preterm labor, incompetent cervix, and hypertensive complications, among others.
Cesarean DeliveryThe risk for pregnancy and neonatal complications are high in women with PCOS, which often leads to cesarean or C-section delivery. In an observational study involving 9,068 women with PCOS, 27.7% of PCOS births were delivered by cesarean section compared with 23. 7% of controls.10 Birth through C-section has its own risks for both the mother and the baby.
7% of controls.10 Birth through C-section has its own risks for both the mother and the baby.
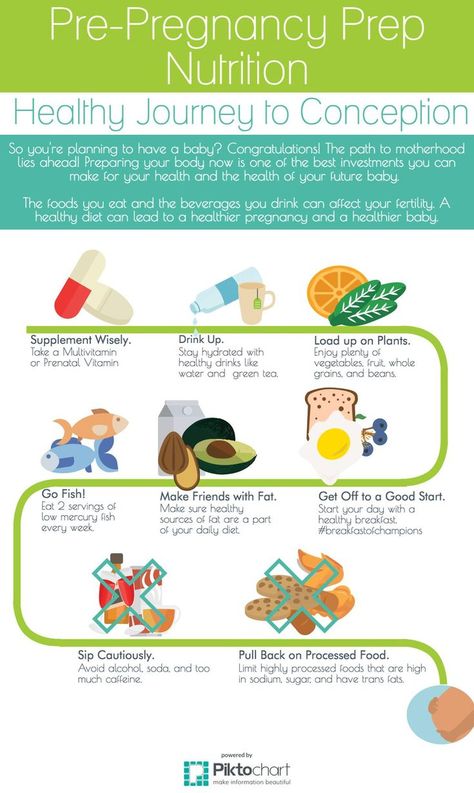
Before becoming pregnant it’s important to prepare your body and keep it in a healthy condition. It may be difficult to take extra steps to improve your health, but it will greatly benefit the outcome of your pregnancy and your child’s well-being.
Recent findings suggest that following a healthy lifestyle reduces pregnancy-related complications in PCOS.11 It is advisable to stop drinking alcoholic beverages and, of course, to stop smoking if you are planning to conceive.
When you are pregnant, make sure to work closely with your doctors and PCOS care team, presumably, your obstetrician or fertility specialist, endocrinologist, and dietitian. Your healthcare providers will guide your medical care before, during and after your pregnancy journey. Check in with them any time you feel changes in your well-being, or have any questions or concerns, as they know you and your situation best.
Sources:
- Kjerulff LE, Sanchez-Ramos L, Duffy D. Pregnancy outcomes in women with polycystic ovary syndrome: a meta-analysis. Am J Obstet Gynecol 2011;204:558.e1-6.
- Jakubowicz, D. J., Iuorno, M. J., Jakubowicz, S., Roberts, K. A., & Nestler, J. E. (2002). Effects of metformin on early pregnancy loss in polycystic ovary syndrome. Journal of Clinical Endocrinology and Metabolism, 87(2), 524–529.
- Sivalingam VN, Myers J, Nicholas S, Balen AH, Crosbie EJ. Metformin in reproductive health, pregnancy and gynaecological cancer: established and emerging indications. Hum Reprod Update. 2014;20:853–68.)
- Boomsma CM, Eijkemans MJC, Huges EG, et al. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum Reprod Update 2006;12:673-83. for the European society of human reproduction and embryology(Eshre). Hum Reprod. 2018;33(9):1586-1601. doi:10.1093/humrep/dey242
- Joham AE, Boyle JA, Ranasinha S, Zoungas S, Teede HJ.
 Contraception use and pregnancy outcome in women with polycystic ovary syndrome: data from the Australian Longitudinal Study on Women’s Health. Hum Reprod. 2014;29(4):802-8.
Contraception use and pregnancy outcome in women with polycystic ovary syndrome: data from the Australian Longitudinal Study on Women’s Health. Hum Reprod. 2014;29(4):802-8. - Hudecova M, Olovsson JH, Poromaa IS. Long-term follow-up of patients with polycystic ovary syndrome: reproductive outcome and ovarian reserve. Hum Reprod. 2009;24(5):1176-83.
- Schindler AE. REVIEW – Pregnancy failure after spontaneous conception or ovulation induction: endocrine causes and treatment. Published online December 31, 2004. Accessed June 23, 2020. https://tspace.library.utoronto.ca/handle/1807/7415
- WHO recommendation on the diagnosis of gestational diabetes in pregnancy | RHL. Accessed June 23, 2020. https://extranet.who.int/rhl/topics/preconception-pregnancy-childbirth-and-postpartum-care/antenatal-care/who-recommendation-diagnosis-gestational-diabetes-pregnancy-0
- Joham AE, Palomba S and Hart R. Polycystic ovary syndrome, obesity, and pregnancy. Semin Reprod Med 2016 34(2): 93–101.
- Rees DA, Jenkins-Jones S, Morgan CL. Contemporary Reproductive Outcomes for Patients With Polycystic Ovary Syndrome: A Retrospective Observational Study. J Clin Endocrinol Metab. 2016;101(4):1664-1672. doi:10.1210/jc.2015-2682
- Bahri Khomami M, Moran LJ, Kenny L, et al. Lifestyle and pregnancy complications in polycystic ovary syndrome: The SCOPE cohort study. Clin Endocrinol. 2019;90(6):814-821. doi:10.1111/cen.13954
Polycystic ovarian syndrome (PCOS) and pregnancy – symptoms and treatments
Polycystic ovarian syndrome (PCOS) and pregnancy – symptoms and treatments | Pregnancy Birth and Baby beginning of content7-minute read
Listen
What is PCOS?
Polycystic ovarian syndrome, or PCOS, is a common condition.
People with PCOS can have:
- higher than normal levels of androgens (male-type hormones)
- problems with ovulation (the release of eggs from the ovaries)
- multiple cysts on the ovaries
This can affect your menstrual cycle, fertility and appearance.
If you have PCOS you may struggle to become pregnant and may be at higher risk of developing some pregnancy complications.
Illustration showing a normal ovary and a polycystic ovary.What are the symptoms of PCOS?
There are many signs and symptoms that are associated with PCOS. These can include:
- irregular menstrual periods
- cysts on the ovaries
- infertility
- weight gain
- acne
- depression
- excessive face and body hair
- thinning or balding head hair
- insulin resistance (where your cells don't respond to insulin and your blood sugar levels rise)
Some of these symptoms (such as acne, excess face and body hair, and scalp hair loss) are due to increased levels of the hormones called androgens. These hormones are found in all females, but those with PCOS have slightly higher amounts.
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.
How is PCOS diagnosed?
It often takes a while to get a PCOS diagnosis. This is because the condition can mimic other problems. Sometimes, people only find out that they have PCOS when they have tests to find out why they are having trouble getting pregnant.
If you think you might have PCOS, see your doctor. Early diagnosis means that your symptoms can be treated early.
At your appointment, your doctor will:
- ask about your symptoms
- ask for your medical history
- examine you
Your doctor may also recommend blood tests and an ultrasound scan to look for any cysts in the ovaries.
In general, to be diagnosed with PCOS, you need to have 2 out of 3 of the following;
- irregular periods, or no periods
- symptoms due to increased levels of androgen hormones, or a blood test showing you have increased levels of androgen hormones
- an ultrasound scan showing multiple cysts on your ovary or ovaries
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
Will PCOS affect my fertility?
If you have PCOS, you might struggle to get pregnant.
Fortunately, with lifestyle changes or infertility treatment, most people with PCOS can become pregnant. Talk to your doctor or fertility specialist for individual advice for your situation.
Can PCOS increase my risk of complications during pregnancy?
Having PCOS can increase your risk of some complications during pregnancy, such as:
- high blood pressure
- gestational diabetes
- premature birth
If you have PCOS, you are also at increased risk of having a baby larger than expected for their gestational age. This comes with a higher risk of needing a caesarean delivery.
Babies born to people with PCOS have a higher chance of being admitted to a newborn intensive care unit.
Pregnant women with PCOS may have a higher risk of miscarriage and stillbirth. However, more research is needed in this area.
If you have PCOS and are pregnant, it is important you talk with your doctor. The risk of these complications can be reduced by monitoring your PCOS symptoms and taking extra care during your pregnancy.
The risk of these complications can be reduced by monitoring your PCOS symptoms and taking extra care during your pregnancy.
What steps can I take to look after my health?
You can make lifestyle changes to manage your PCOS and look after your health. These include:
- maintaining a healthy weight
- eating healthily
- exercising
- managing stress
- getting enough sleep
These lifestyle changes can reduce the symptoms of PCOS and improve your chance of falling pregnant.
If you are overweight, a 5% to 10% loss in weight can increase your fertility.
Speak to your doctor for guidance on how to make effective lifestyle changes.
How is PCOS treated?
Treatment for PCOS depends on each person. Speak to your doctor about the best treatment for you.
If you are trying to fall pregnant, your PCOS treatment will focus on:
- restoring regular ovulation
- weight loss
- improving your general health and wellbeing
If you have made lifestyle changes and are still struggling to fall pregnant, your doctor may order fertility tests. They may also prescribe fertility medicines to help you ovulate. In some cases, they may recommend surgery.
They may also prescribe fertility medicines to help you ovulate. In some cases, they may recommend surgery.
Another possibility is in vitro fertilisation (IVF), which offers the best chance of conception. However, this can be expensive and is usually only considered when all other options have been unsuccessful.
If you are not trying to fall pregnant, your PCOS treatment will focus on:
- reducing your symptoms
- reducing your risk of long-term health issues, including heart disease and type 2 diabetes
Speak to your doctor. They can help you manage your PCOS symptoms by providing:
- weight loss management strategies
- treatment for sleeping problems
- acne treatment
- medicines, including hormonal contraception (birth control) to manage irregular menstruation
Dealing with infertility and PCOS symptoms can be difficult. You may experience feelings of depression and anxiety. Your doctor can refer you to a counsellor or psychologist for your mental health.
Resources and support
Visit the Jean Hailes website for more information on PCOS and its complications.
Hormones Australia also supplies information on PCOS, including questions to ask your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Australian Family Physician (Polycystic ovary system), Jean Hailes (PCOS), Royal Australian College of General Practitioners (Polycystic ovary system - clinical guidelines), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Long-term consequences of PCOS - statement)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Need more information?
Polycystic Ovary Syndrome (PCOS) | Your Fertility
PCOS can be associated with a range of symptoms including irregular periods and difficulties getting pregnant
Read more on Your Fertility website
Fact sheets | Your Fertility
Polycystic ovary syndrome (PCOS) is the most common hormonal condition affecting women in their reproductive years
Read more on Your Fertility website
What is PCOS?
Polycystic ovary syndrome (PCOS) is the most common hormonal condition affecting women in their reproductive years.
Read more on Your Fertility website
Polycystic ovarian syndrome (PCOS) - Better Health Channel
Polycystic ovarian syndrome is a hormonal condition associated with irregular menstrual cycles, excess hair growth, acne, reduced fertility, and increased risk of diabetes and mood changes.
Read more on Better Health Channel website
Polycystic ovary syndrome (PCOS) | Dietitians Australia
PCOS is a common hormonal condition of the ovaries that can cause problems such as an irregular menstrual cycle, weight gain, impaired fertility and poor mental health. Diet and lifestyle changes are the first steps to manage PCOS, and an Accredited Practising Dietitian specialising in PCOS is the most qualified professional to help.
Read more on Dietitians Australia website
Fertility explained | VARTA
Fertility is the ability to conceive a child. Most of us take our fertility for granted but the process of reproduction is complex, so some people may experience difficulties when trying for a baby. There are a range of factors that can affect fertility. Taking care of your preconception health by modifying your lifestyle can improve your chance of a pregnancy and the health of your future child. Medical conditions such as polycystic ovary syndrome (PCOS) and endometriosis can reduce fertility, however it may just take longer to get pregnant. In some cases, medical procedures can be used to preserve fertility. Fertility preservation (freezing of gametes for later use) is used by people who are not ready to have a baby during their most fertile years or for those facing medical treatment that might impair their fertility. Understanding reproduction It is useful to understand how eggs and sperm are normally formed, and how conception occurs to understand the causes of infertility and how they are targeted in fertility treatment. The hormones which control the production of sperm and eggs are called gonadotrophins.
Most of us take our fertility for granted but the process of reproduction is complex, so some people may experience difficulties when trying for a baby. There are a range of factors that can affect fertility. Taking care of your preconception health by modifying your lifestyle can improve your chance of a pregnancy and the health of your future child. Medical conditions such as polycystic ovary syndrome (PCOS) and endometriosis can reduce fertility, however it may just take longer to get pregnant. In some cases, medical procedures can be used to preserve fertility. Fertility preservation (freezing of gametes for later use) is used by people who are not ready to have a baby during their most fertile years or for those facing medical treatment that might impair their fertility. Understanding reproduction It is useful to understand how eggs and sperm are normally formed, and how conception occurs to understand the causes of infertility and how they are targeted in fertility treatment. The hormones which control the production of sperm and eggs are called gonadotrophins. There are two types of gonadotrophins: follicle-stimulating hormone (FSH) and luteinising hormone (LH). In men, they stimulate the testicles to produce sperm and testosterone. In women, they act on the ovaries where the eggs develop. The female sex hormones, oestrogen and progesterone, are produced by the ovaries when eggs mature and are released (ovulation). For women, the production of sex hormones and the release of an egg is known as the menstrual cycle. It is counted from the first day of the period until the day before the start of the next period. In an average cycle of 28 days, ovulation happens on day 14. However, cycle length varies between women, and it is important to note that ovulation occurs earlier in women with shorter cycles and later in women with longer cycles. Sperm are produced at the rate of about 300 million per day. They take some 80 days to mature. Each sperm has a head, which contains the genetic material, and a tail, which propels it up through the vagina, uterus, and fallopian tubes where the egg is fertilised.
There are two types of gonadotrophins: follicle-stimulating hormone (FSH) and luteinising hormone (LH). In men, they stimulate the testicles to produce sperm and testosterone. In women, they act on the ovaries where the eggs develop. The female sex hormones, oestrogen and progesterone, are produced by the ovaries when eggs mature and are released (ovulation). For women, the production of sex hormones and the release of an egg is known as the menstrual cycle. It is counted from the first day of the period until the day before the start of the next period. In an average cycle of 28 days, ovulation happens on day 14. However, cycle length varies between women, and it is important to note that ovulation occurs earlier in women with shorter cycles and later in women with longer cycles. Sperm are produced at the rate of about 300 million per day. They take some 80 days to mature. Each sperm has a head, which contains the genetic material, and a tail, which propels it up through the vagina, uterus, and fallopian tubes where the egg is fertilised. Conception occurs when an egg and a sperm come together. At ovulation, an egg is released from the ovary into the fallopian tube. If sperm is present at that time, the egg can be fertilised. The fertilised egg then starts to divide and becomes an embryo. After ovulation, the ovary produces progesterone which prepares the lining of the uterus - the endometrium - for the growing embryo. A few days after implantation, the embryo starts to produce human chorionic gonadotrophins (HCG) - the hormone that gives a positive pregnancy test reading. If an embryo does not form or attach to the endometrium (implantation), the level of progesterone drops and the next period starts.
Read more on Victorian Assisted Reproductive Treatment Authority website
Good fertility health
Your age and your health can affect your chances of falling pregnant. Maintaining a healthy lifestyle may help you improve your fertility.
Read more on Pregnancy, Birth & Baby website
All about Polycystic Ovary Syndrome (PCOS) | Jean Hailes
Read about causes, signs and symptoms of PCOS, as well as diagnosis and treatments available to help. Jean Hailes is Australia's leader in women's health.
Read more on Jean Hailes for Women's Health website
Ovulation and fertility - Better Health Channel
The female body shows several signs of ovulation and you may experience some or all of these signs.
Read more on Better Health Channel website
Planning to have a baby | VARTA
Planning ahead If you are thinking about having a baby in future, there are some things you can do to improve your chances. Preconception is the period leading up to getting pregnant. This is a great time for both men and women to focus on ways to improve their health, and increase the chance of pregnancy and having a healthy baby. The earlier you start the conversations about having a baby, the better. Here are some things you and your partner (if any) should start thinking about now: the number of children you would like to have the age at which you would like to have your first and last child improving your health before you try booking a preconception health check with your GP. Your Fertility has practical ideas for how you can improve your preconception health including checklists for men and women. Improving fertility Age is the most important factor affecting a woman’s chance of conceiving. Female fertility starts to decline around age 30 and after age 35 the monthly chance of conceiving decreases more rapidly. Age can also affect a man’s fertility and the chance of having a healthy baby. Certain lifestyle factors for both men and women also affect the ability to conceive, the health of the pregnancy, and the health of the future baby.
A healthy weight, a nutritious diet and regular exercise can significantly boost fertility, as can quitting smoking, stopping drug use and curbing heavy drinking. When you are ready to try for a baby, it is important to know when conception is most likely to happen. In an average cycle of 28 days, ovulation happens on day 14. However, cycle length varies between women, and it is important to note that ovulation occurs earlier in women with shorter cycles and later in women with longer cycles. However, pregnancy is only possible during the five days before ovulation through to the day of ovulation. These six days are the ‘fertile window’ in a woman’s cycle, and reflect the lifespan of sperm (five days) and the lifespan of the egg (24 hours). Your Fertility’s ovulation calculator can help you work out the fertile window. Medical conditions and fertility PCOS Polycystic ovary syndrome (PCOS) is a common hormonal condition affecting up to one in five women of childbearing age. The condition affects two hormones, insulin and testosterone (male-like hormones), which may be produced in higher levels and can impact on fertility.
Women with PCOS are prone to irregular menstrual cycles due to absent or infrequent ovulation. While the majority of women with PCOS become pregnant without fertility treatment, they often take longer to fall pregnant and are more likely to need treatment (ovulation induction or IVF) than women without PCOS. Despite this, studies show little difference between the number of children born to women with PCOS than to those without. Conception may sometimes occur as a result of lifestyle modification or after receiving medication to assist with ovulation (ovulation induction) and advice regarding the timing of sex. The most successful way to treat PCOS is by making healthy lifestyle changes. Eating a healthy diet and exercising regularly is the best way to reduce symptoms and increase fertility. If you have difficulty conceiving, your GP may refer you to a specialist clinician. Monash Centre for Health Research and Implementation (MCHRI) has a list of questions that may be helpful. You can find more information and resources about PCOS at Your Fertility, Jean Hailes for Women’s Health and MCHRI.
Endometriosis Endometriosis is a condition in which endometrium, the tissue that normally lines the womb (uterus), grows outside the uterus. Endometriosis may cause fibrous scar tissue to form on the uterus. It can also affect the ovaries, fallopian tubes and the bowel. Endometriosis may cause very painful periods and reduce fertility or cause infertility. You can find out more about endometriosis at Jean Hailes for Women’s Health and the Better Health Channel.
Read more on Victorian Assisted Reproductive Treatment Authority website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Polycystic ovary syndrome
Kuznetsova Ekaterina Viktorovna
Reproductologist, Gynecologist
Novosibirsk Center for Reproductive Medicine
The criteria for the diagnosis of PCOS are:
- absence of ovulation (anovulation),
- hyperandrogenism,
- the presence of polycystic (multifollicular ovaries) with an increase in the volume of the ovaries according to ultrasound.
The diagnosis can be made if two of these three manifestations are present.
As a rule, the examination of a woman begins with an ultrasound examination of the pelvic organs. Often, if the conclusion indicates the presence of "multifollicular ovaries" (MFO), on this basis, the diagnosis of PCOS is erroneously established. The term "multifollicular ovaries" is simply a description of the ultrasound picture, which reflects the presence of a large number of antral follicles in the ovaries.
Such a conclusion, of course, is one of the criteria for PCOS, but, I remind you that not one symptom, but two, is required for a diagnosis. The presence of MFN by ultrasound performed at the beginning of the menstrual cycle does not make it possible to judge from the presence or absence of ovulation in a woman's menstrual cycles. The detection of a large number of follicles in the ovaries and by ultrasound is the norm for young women! With preserved ovulation, the absence of menstrual irregularities, this treatment does not require and does not prevent pregnancy!
To diagnose anovulation, it is necessary to perform ultrasonic folliculometry (FM), preferably within 2-3 menstrual cycles. Moreover, when performing FM, you need to decide on the period until which it makes sense to wait for the appearance of the dominant follicle. This is where mistakes often happen. The fact is that most women have a menstrual cycle of 28-30 days, while ovulation occurs on days 14-16 of the cycle.
But, if this is the case for the majority, should it be so for everyone? No. The normal length of a menstrual cycle is 21 to 42 days. This means that with a 21 day cycle, ovulation occurs on days 7–8 of the cycle, but with a 42 day cycle? On the 20th day? No. With a cycle duration of 42 days, ovulation should occur on days 26-30 of the cycle. Thus, when folliculometry is stopped on the 14th-16th day of the cycle due to the absence of a dominant follicle, an erroneous conclusion is made about anovulation. Although, with a regular, but long (32–42 days) menstrual cycle, ovulatory function can be preserved. Such a delusion is very dangerous, because it entails the start of stimulation therapy in women who are planning a pregnancy, although, in fact, they do not need it. Conversely, women who are not currently planning a pregnancy get the wrong impression that there is no need for contraception, which leads to unwanted pregnancies and, as a result, to abortion.
The next symptom of PCOS is hyperandrogenism, which is an increase in the content of male hormones (androgens). This is a sufficient general statement. Characteristic of PCOS is an increase in testosterone, which is produced in excess in the ovaries. This can lead to appearances such as excessive hair growth on the skin of the abdomen, thighs and even the face (this is called hirsutism), as well as increased activity of the skin sebaceous glands, which is manifested by oily skin and a tendency to acne. But testosterone is not the only androgen in the body.
In addition, other male hormones are present in the body: androstenedione, DEHA, 17-OH progesterone, etc., which are produced mainly by the adrenal glands. Their determination is necessary during the examination in case of suspicion of PCOS, the presence of manifestations of hyperandrogenism, anovulation, but is not a sign of PCOS, since they are produced not in the ovary, but in the adrenal glands. So the determination of DHEA is necessary to exclude formations of the adrenal glands that produce hormones (hormone-producing tumors), the determination of 17-OH progesterone is performed to diagnose such a congenital disease as VDKN (formerly called adrenogenital syndrome - AGS), which can also lead to cycle disorders and anovulation, but, however, is not synonymous with PCOS and requires different treatment. With HCHD, there is at least a three-fold increase in the level of 17-OH progesterone, while a slight increase of 1-2 ng / ml or nmol / ml is neither a sign of HCHD nor PCOS, and, as a rule, is asymptomatic and does not require treatment.
Often, hormonal disorders in PCOS are accompanied by impaired insulin function (insulin resistance) and/or its excessive production (hyperinsulinemia). This leads to the fact that PCOS is accompanied by a complex of symptoms called metabolic syndrome (MS) and is manifested by obesity, hypertension, high cholesterol, and impaired glucose uptake. This manifestation of PCOS is dangerous with very serious consequences: if left untreated, type 2 diabetes mellitus, coronary heart disease, etc. develop over time, which is the main cause of death along with cancer. Insulin resistance, of course, requires medical correction with special drugs, but a woman herself can help the drugs work more efficiently. How? Weight loss, proper nutrition and regular physical activity. Agree, it is available to everyone.
It's time to move on to treating PCOS.
Speaking about the treatment of this disease, it is important to answer the question: is a woman planning a pregnancy at the moment or not? So, if pregnancy is not planned in the near future, then combined oral contraceptives (COCs) are the best suited to normalize the cycle, prevent and treat endometrial hyperplasia, dysfunctional bleeding, and cosmetic problems. These drugs are quite effective, inexpensive and easy to take, which allows you to solve these problems.
On the topic "COC - to drink or not to drink?" many copies have been broken, but there is still no tool more effective, safer and easier to use. Like any other drug, COCs have both contraindications and side effects, so these drugs should be prescribed by a doctor who has experience working with them, after identifying possible contraindications to taking, for example, a tendency to thrombosis. There are a lot of drugs from this group on the market now, and their tolerance can be quite different. But I am convinced that among the existing variety it is possible to choose the right drug, it just does not always happen the first time, even if the appointment is made by a very experienced doctor. Unfortunately, in the medical literature, there is no unequivocal answer to the question of how long it is safe to take COCs. Based on my own experience, I can say that on average this is up to 5 years. I emphasize that this is an average value - in each individual case, this issue should be resolved individually.
If a woman diagnosed with PCOS is planning a pregnancy, she needs to contact a reproductive specialist in a specialized clinic. Since for the onset of pregnancy it is necessary not only to make the menstrual cycle regular, but to establish the ovulatory function of the ovary, since without the release of the egg from the ovary, that is, ovulation, pregnancy is impossible. In such cases, ovulation induction (stimulation of ovulation, stimulation of ovarian function) is carried out using special preparations.
It is good if ovulation stimulation is carried out by a reproductive specialist who knows ultrasound and can independently monitor the growth of follicles and prescribe appropriate drugs. Before using ovulation induction, it is necessary to perform a study of the patency of the fallopian tubes and a diagnosis of the state of the sperm in the husband/partner (spermogram, MAP test, strict morphology according to the Kruger criteria) and other examinations that are mandatory when planning a pregnancy. Since, unfortunately, the lack of ovulation may not be the only reason for the lack of a desired pregnancy.
Often, a replacement for ovulation stimulation is the appointment of progesterone preparations from days 16 to 25 of the cycle. However, this is not at all the case. The appointment of these drugs will help to even out the cycle, make it 28 days, may be an alternative to COCs for the prevention and treatment of endometrial hyperplasia, but will not help the onset of pregnancy. On the contrary, it's more likely to get in the way. The fact is that under the influence of these drugs, changes occur in the endometrium that are characteristic of the second phase of the cycle, that is, after ovulation has occurred, which allows you to get a menstrual-like reaction, but their effect does not extend to the ovary, does not allow you to establish ovulation. But, in the event that ovulation suddenly decides to occur (this happens, including with PCOS once a year or once every several years), then taking these drugs can desynchronize the development of the embryo and the preparation of the endometrium, and this is one of the necessary conditions for pregnancy .
Previously, to normalize the cycle and restore ovulation, the method of cauterization of the ovaries (“notches”, resection of the ovaries) was used, which was performed during laparoscopy. For a long time, this was almost the only means of restoring the functioning of the ovaries in the absence of special drugs, the wide availability of ultrasound and qualified reproductologists. But now this method is not the method of choice, since among its consequences there is often premature ovarian exhaustion, that is, the irreversible disappearance of the follicular apparatus.
These are very difficult situations when young women begin menopausal manifestations, and there are no own eggs left, and pregnancy planning becomes possible only with the use of donor oocytes. In addition, I want to note that ovarian biopsy during laparoscopy is also not a modern criterion for the diagnosis of PCOS and you will not find indications of its need in any modern manual on operative gynecology. Since, unfortunately, even a slight damage to the ovarian tissue can lead to irreversible consequences.
In conclusion, I want to say that although PCOS is a common pathology that leads to serious consequences, in the modern world there are many means to cope with it and realize the reproductive function. Take care of your health, contact qualified specialists and be happy!
Make an appointment
to the doctor - Kuznetsova Ekaterina Viktorovna
Novosibirsk Center for Reproductive Medicine
Polycystic ovary syndrome (PCOS) is one of the most mysterious diseases in the practice of a gynecologist-reproductologist. There are several classifications and various criteria for this diagnosis.
Types and causes of polycystic ovaries
In 2012, an expert group report on this pathology was presented to the entire medical community, on the basis of which four types of disorders were identified in patients with PCOS.
The first type was characterized by a combination of an increased level of androgens in the blood (hyperandrogenism) and a violation of ovulation processes. The second type, respectively, had a combination with ultrasound signs of polycystic ovaries. The third type is the absence or decrease in the frequency of ovulation in combination with ultrasound changes in the ovaries. The fourth type was a combination of all previously described types. Based on the data obtained, any of the above combinations of PCOS signs can be a confirmation of this diagnosis.
Among the causes of PCOS, there is a violation of the regulation of maturation of follicles, as well as a change in the enzyme systems involved in the biosynthesis of ovarian androgens (male hormones in the female body), which can lead to an imbalance between the process of division and reverse development of cells (apoptosis) of ovarian tissue. In addition, the role of genetic factors that can disrupt the regulation of cytochrome P450c17, a key enzyme in the biosynthesis of ovarian and adrenal androgens, is not denied. It is important to note that PCOS often develops against the background of neuroendocrine syndromes, obesity, hyperprolactinemia, congenital dysfunction of the adrenal cortex, Cushing's disease. Such women often report menstrual irregularities, overweight, increased blood insulin levels, impaired glucose tolerance, and type 2 diabetes.
Pregnancy with polycystic ovaries
It is believed that about 70% of patients with infertility caused by impaired egg maturation have some form of PCOS. Achieving pregnancy through the IVF program or ovulation stimulation as part of artificial insemination in such a contingent of patients are the most effective methods of treating this disease.
Commonly used drugs included in the ovarian stimulation protocol are clomiphene citrate, as well as gonadotropins, hormonal drugs that promote the maturation of eggs and the restoration of ovulation, as well as the onset of pregnancy.
Clomiphene citrate is most effective in patients under 30 years of age, the duration of menstrual irregularities in which does not exceed about 5 years with a short duration of infertility. When using this drug in 50% of cases, it is possible to achieve ovulation (the release of an egg from the ovary), but pregnancy occurs in only less than 25% of women.
Patients with PCOS who are over 30 years of age, overweight, markedly increased ovarian volume, decreased estrogen levels in the blood, have low sensitivity to clomiphene citrate. In such cases, the prescription of medications that affect insulin resistance, weight loss, and therefore improve the response to hormonal stimulation of ovarian function, comes to the rescue in such cases before the IVF program. An example of this is the drug metformin. According to some researchers, this makes it possible to increase the effectiveness of the ovulation stimulation protocol by up to 10-15%.
Complications of the IVF program for polycystic
The key to the correct implementation of hormonal treatment in patients with PCOS is to assess the risk of complications in the IVF program. The most common of which is ovarian hyperstimulation syndrome (OHSS). It should be noted that in patients with PCOS, the risk of developing OHSS reaches 10-12%, while in the general population of women it does not exceed 3%. It is more common in those who have many follicles and increased ovarian volume, as well as more than 20 maturing oocytes during stimulation. To help overcome this complication of assisted reproductive technologies, patients with PCOS come with the use of small doses of gonadotropins (hormonal drugs to stimulate ovarian function), the use of "soft protocols", the mandatory determination of anti-Müllerian hormone in the blood serum, which characterizes the ovarian reserve. In severe cases, an alternative tactic for reproductologists is the abolition of embryo transfer and their cryopreservation with the possibility of completing the IVF program only after 1-2 menstrual cycles.
In addition to developing OHSS, these women remain at risk of multiple pregnancies, especially in programs with intrauterine insemination. With the development of a large number of follicles in such women, this procedure is proposed to be abandoned, and an ovarian puncture should be performed as part of the IVF program with a complete collection of eggs for in vitro fertilization.