Fetal position oblique
Causes, Risks, Avoiding a Cesarean, and More
Your baby is growing and moving every day. As you advance through pregnancy, your little one will shift positions in an effort to get ready for their grand debut.
And while most babies will settle into the head-down position before birth, others get turned around and end up in some unusual lies.
If your doctor mentions an oblique lie, you might be wondering what that means and how it may change your plans for childbirth.
Like other fetal positions, an oblique lie presents some challenges. That’s why it’s important to work closely with your doctor as you near your due date.
Here’s what you need to know if your baby is in an oblique lie, what you can do to help your baby change directions, and what may happen if they decide to stay put.
Before we dive into the specifics of an oblique lie, it’s important to describe, in general, what we’re talking about when we say “fetal lie.”
When a doctor or midwife describes the lie of your baby, they’re technically describing the relationship between your long axis and the baby’s long axis. In other words, the baby’s position in your belly.
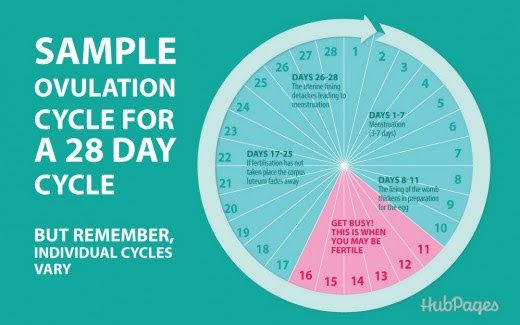
Fetal positions change throughout pregnancy, and it’s normal for your baby to present in a lot of different “lies.” But, as you get closer to your due date, the goal is to have the baby in a head-down position in preparation for birth. This often happens between weeks 32 and 36.
If your little one is presenting in an oblique lie, which often results in a shoulder or arm presentation, their head and feet will rest on your pelvis.
More specifically, Thomas Ruiz, MD, an OB-GYN at MemorialCare Orange Coast Medical Center, says an oblique lie is when the baby’s head is just to the side of the pelvic inlet.
To understand how close this position is to a traditional vertex presentation, Ruiz says if the baby’s head changes position slightly, centers itself over the inlet, and then drops into the pelvis, you get a head-down position.
However, oblique lies can just as easily become transverse if the head moves away from the pelvis.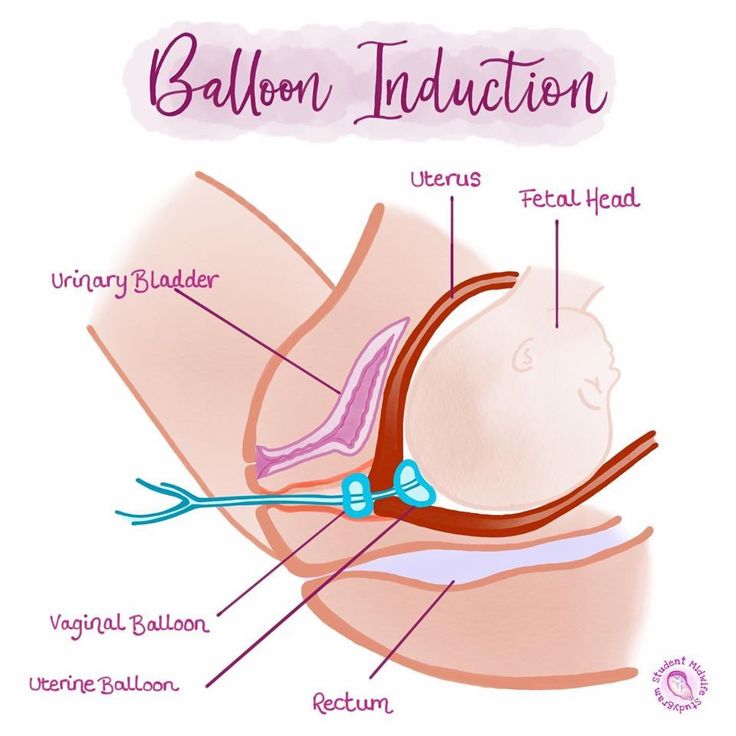
Some of the more common causes of an oblique lie, according to Jamie Lipeles, DO, founder of Marina OB-GYN, include:
- an abnormally shaped uterus
- baby is too large for the pelvis
- presence of fibroids in the uterus
- excessive amniotic fluid
When a pregnancy isn’t textbook (and when is it ever?), we all want to know and understand the potential risks for baby. If your little one has decided to hang out in an oblique lie, there are some risks if they don’t get turned around before you go into labor.
The most threatening risk of an oblique lie, says Lipeles, is that this presentation doesn’t allow the head to obstruct the outlet where the baby is supposed to be delivered through.
“If you go into labor and the amniotic sac ruptures, there is nothing at the outlet to prevent the umbilical cord exiting the uterus through the cervix,” he explains. This is called cord prolapse, which is a surgical emergency and can be life threatening or result in permanent neurological damage to the baby’s brain.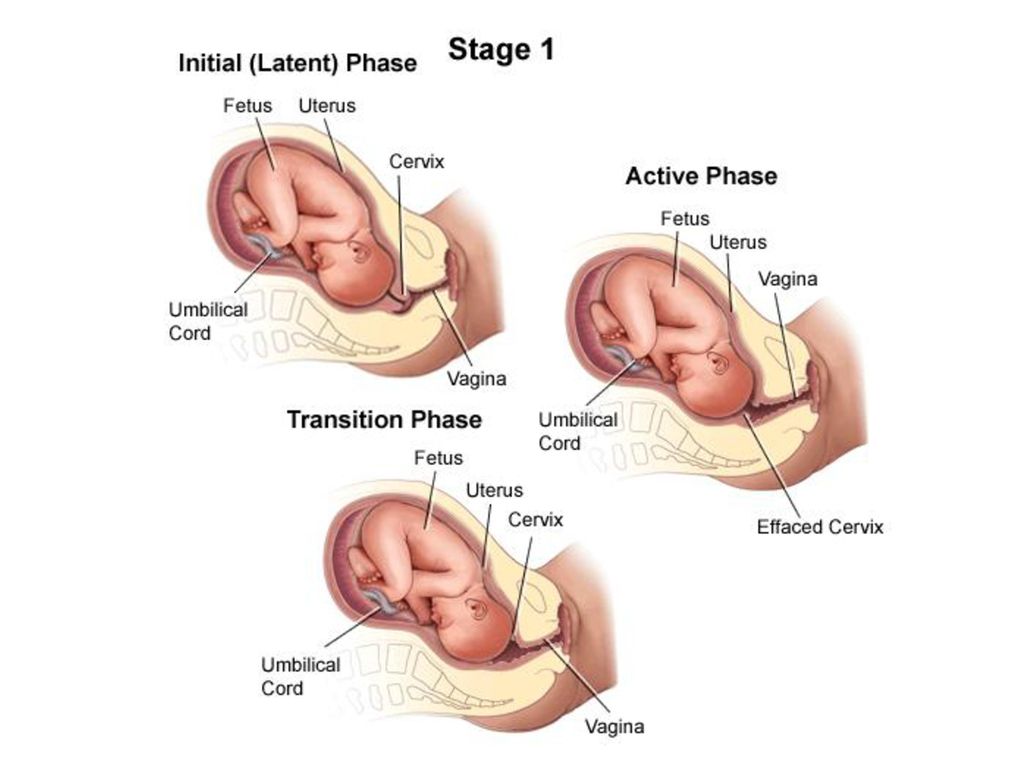
Additionally, if the baby can’t fit through the pelvis and remains in an oblique lie, Lipeles says the doctor must perform an immediate caesarean delivery.
Now that you understand the predicament your little bean is in, it’s time to tackle the mechanics of how to get them headed in the right direction.
The solutions for an oblique lie are often similar to the ones used for a transverse lie. And the best part? There are several exercises that work.
Here are a few that Lipeles recommends:
- doing yoga poses such as downward dog
- sitting on a birthing ball and rolling your hips with an open leg stance (aka pelvic rocking)
- floating in a swimming pool to attempt to get the baby to move into a better position
- remaining in a squatting position to “open the pelvis” to give way to the baby changing their position
One 2019 study found that pelvic rocking on a stability or birthing ball while pregnant contributed to correcting the fetal lie and, more specifically, the oblique lie, in women at or more than 29 weeks pregnant.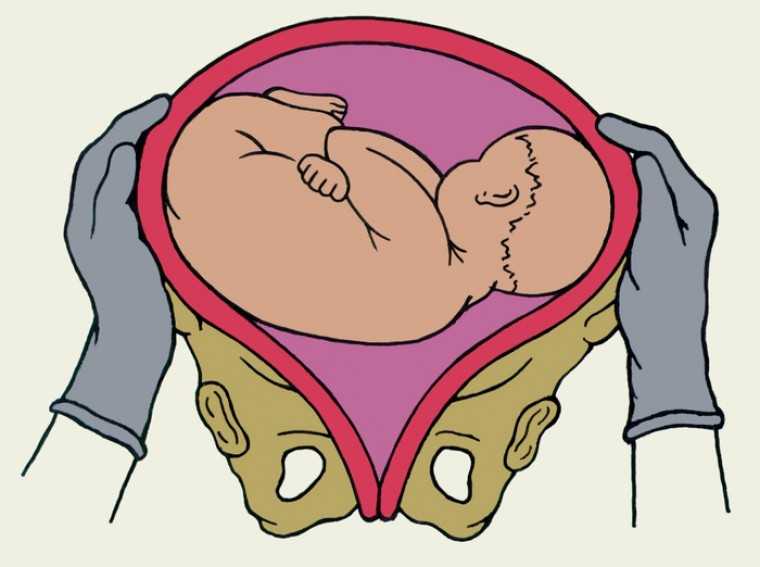 More than 49 percent of women in the intervention group indicated a longitudinal lie compared to 29.8 percent of those in the control group.
More than 49 percent of women in the intervention group indicated a longitudinal lie compared to 29.8 percent of those in the control group.
While all of those interventions can work, Lipeles says in his 14 years of practice, there’s one activity he finds the most effective with both an oblique lie and breech position that you can do at home.
He instructs his patients to take whatever frozen fruits or vegetables (or any other item) they have in the freezer and place them in a thin cloth and leave them on their belly in the area that the baby’s head is positioned.
“The unborn baby is sensitive to changes in temperature, and thus these frozen items near their head are uncomfortable, and will encourage them to move their head away from the cold item, which often leads to the baby moving into a more desirable position,” he explains.
Doctor-involved interventions are also a possibility. Because the head is so close to the pelvic inlet, Ruiz says these lies often respond to manual manipulation or external cephalic version.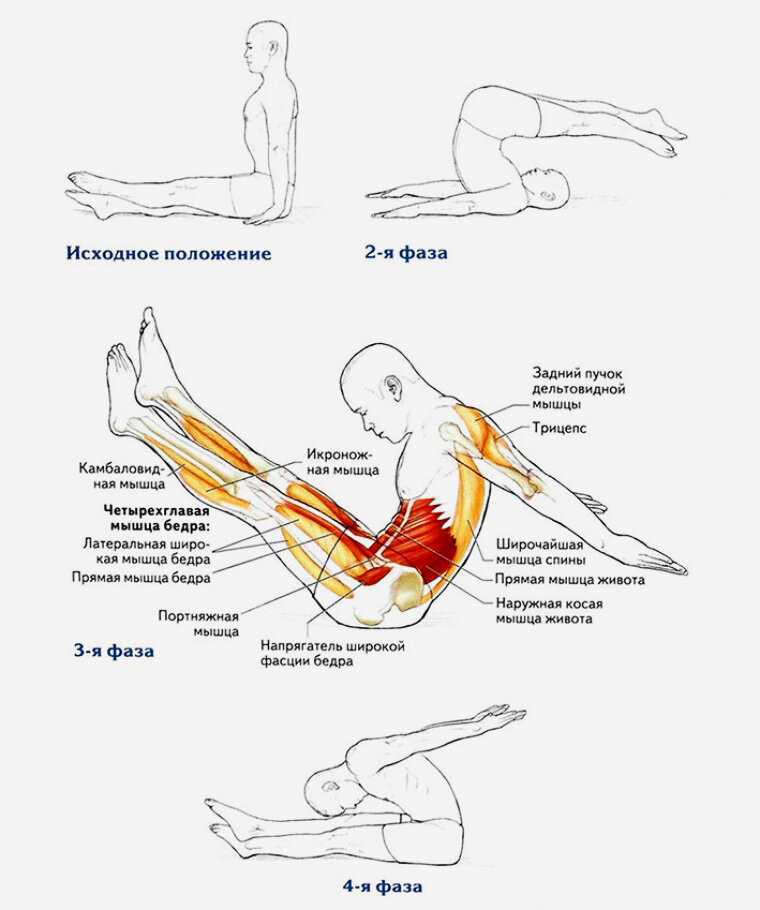
To do this procedure, your doctor, with the help of an ultrasound, will manually guide the head into the pelvis. “If there’s adequate space within the pelvis, the head will usually drop down into a normal position,” he says.
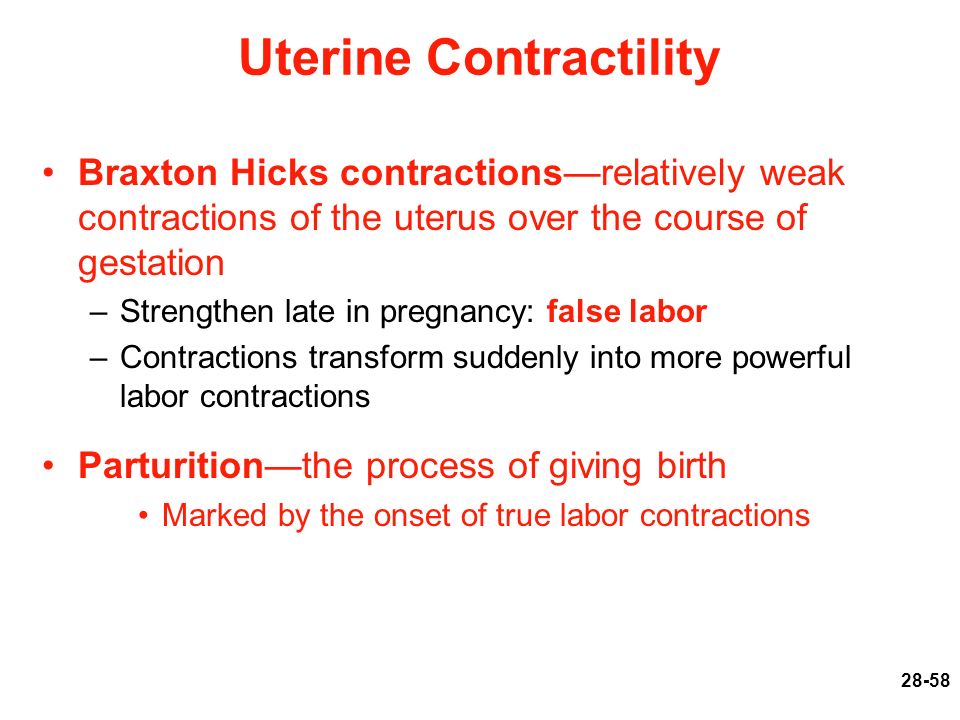
Since uterine contractions can also force the baby’s head into the pelvis, Ruiz says at 39 weeks, a doctor can use external version cephalic techniques to push the baby’s head down into the pelvis and then start an induction.
“This usually works and can lead to a vaginal delivery, if you’ve had more than one pregnancy,” he says. But if this is your first pregnancy, Ruiz says the maneuver is more difficult, and not as successful, because the uterus and abdomen are more firm.
And finally, Kecia Gaither, MD, an OB-GYN and director of perinatal services at NYC Health + Hospitals, says there are some alternative methods like acupuncture and Spinning Babies classes. “Acupuncture, which has been utilized for fetal movement for years, relaxes the mother’s musculature, allowing the baby to turn head-first into the pelvis,” she says.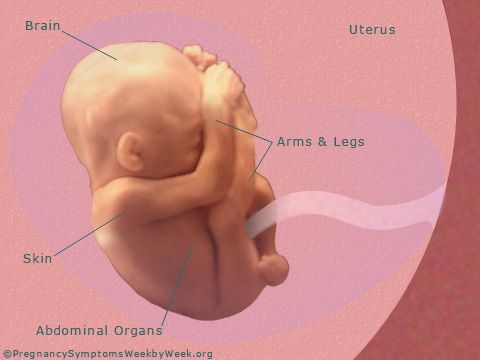
The classes Gaither is referring to are called “Spinning Babies,” which she says employ certain yoga positions to relax mom and encourage fetal movement into a head-first position.
If you’re nearing your due date, regular labor can also push the baby’s head down into the pelvis. “If this happens, you will get a chance at a vaginal delivery,” says Ruiz. Of course, if the head moves laterally, Ruiz says the baby will move into a transverse lie, and you’ll end up with a cesarean section.
In a normal shaped uterus, the forces of uterine contractions will force the baby’s head in the pelvis. Fortunately, the forces of uterine contractions can force the baby’s head into the pelvis.
But if the contractions don’t push the baby’s head into the pelvis, and you’re going into labor while still in an oblique lie, your doctor will most likely need to perform an expedited C-section.
Your baby will move into various positions before your due date. As you near the end of your pregnancy, your doctor will keep a close eye on the fetal position and recommend interventions if the baby is in an oblique lie.
Like other fetal positions, an oblique lie may require a cesarean delivery if the baby doesn’t move into a head-down position before you go into labor.
Causes, Risks, Avoiding a Cesarean, and More
Your baby is growing and moving every day. As you advance through pregnancy, your little one will shift positions in an effort to get ready for their grand debut.
And while most babies will settle into the head-down position before birth, others get turned around and end up in some unusual lies.
If your doctor mentions an oblique lie, you might be wondering what that means and how it may change your plans for childbirth.
Like other fetal positions, an oblique lie presents some challenges. That’s why it’s important to work closely with your doctor as you near your due date.
Here’s what you need to know if your baby is in an oblique lie, what you can do to help your baby change directions, and what may happen if they decide to stay put.
Before we dive into the specifics of an oblique lie, it’s important to describe, in general, what we’re talking about when we say “fetal lie.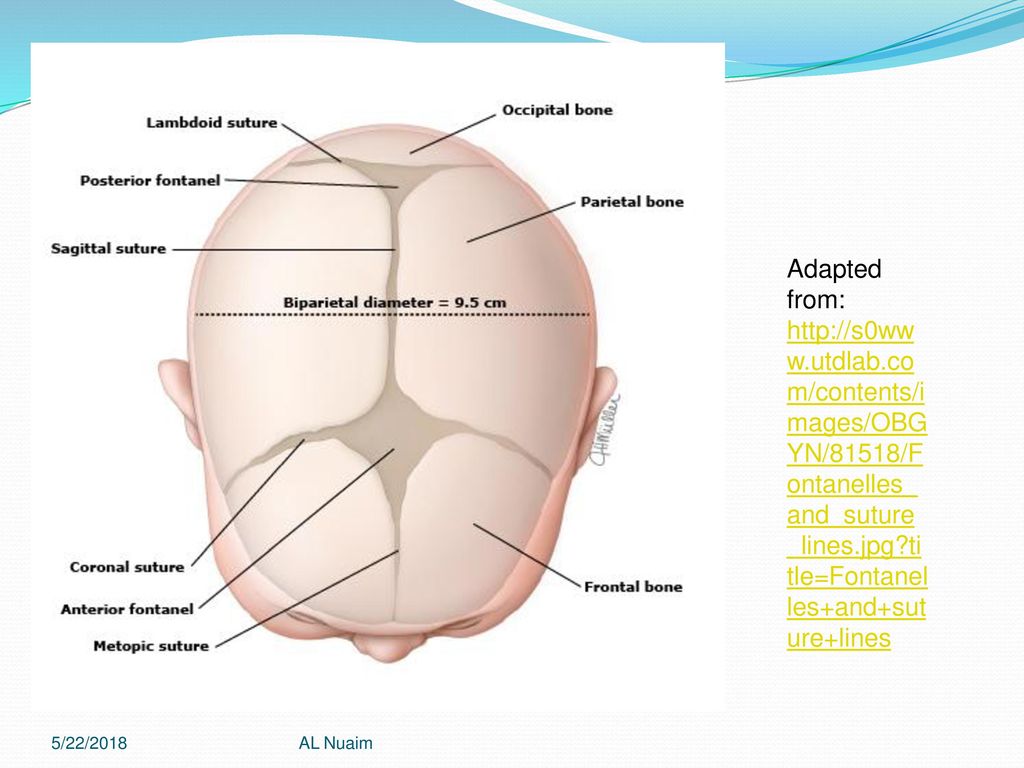 ”
”
When a doctor or midwife describes the lie of your baby, they’re technically describing the relationship between your long axis and the baby’s long axis. In other words, the baby’s position in your belly.
Fetal positions change throughout pregnancy, and it’s normal for your baby to present in a lot of different “lies.” But, as you get closer to your due date, the goal is to have the baby in a head-down position in preparation for birth. This often happens between weeks 32 and 36.
If your little one is presenting in an oblique lie, which often results in a shoulder or arm presentation, their head and feet will rest on your pelvis.
More specifically, Thomas Ruiz, MD, an OB-GYN at MemorialCare Orange Coast Medical Center, says an oblique lie is when the baby’s head is just to the side of the pelvic inlet.
To understand how close this position is to a traditional vertex presentation, Ruiz says if the baby’s head changes position slightly, centers itself over the inlet, and then drops into the pelvis, you get a head-down position.
However, oblique lies can just as easily become transverse if the head moves away from the pelvis.
Some of the more common causes of an oblique lie, according to Jamie Lipeles, DO, founder of Marina OB-GYN, include:
- an abnormally shaped uterus
- baby is too large for the pelvis
- presence of fibroids in the uterus
- excessive amniotic fluid
When a pregnancy isn’t textbook (and when is it ever?), we all want to know and understand the potential risks for baby. If your little one has decided to hang out in an oblique lie, there are some risks if they don’t get turned around before you go into labor.
The most threatening risk of an oblique lie, says Lipeles, is that this presentation doesn’t allow the head to obstruct the outlet where the baby is supposed to be delivered through.
“If you go into labor and the amniotic sac ruptures, there is nothing at the outlet to prevent the umbilical cord exiting the uterus through the cervix,” he explains.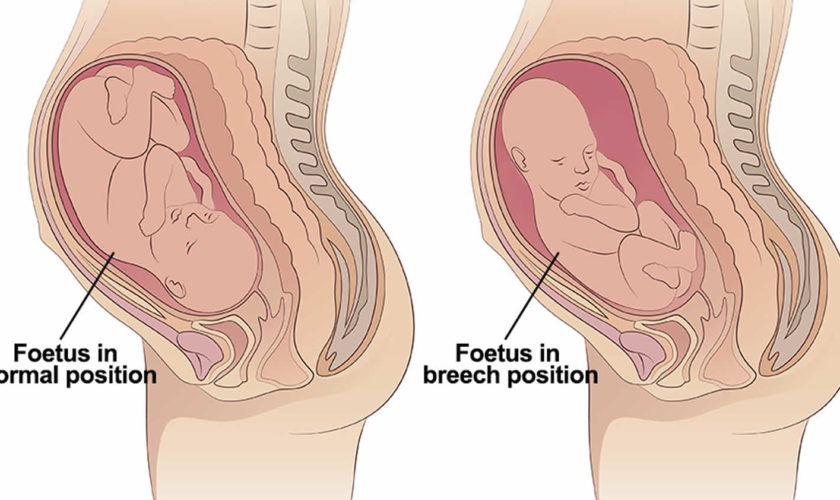 This is called cord prolapse, which is a surgical emergency and can be life threatening or result in permanent neurological damage to the baby’s brain.
This is called cord prolapse, which is a surgical emergency and can be life threatening or result in permanent neurological damage to the baby’s brain.
Additionally, if the baby can’t fit through the pelvis and remains in an oblique lie, Lipeles says the doctor must perform an immediate caesarean delivery.
Now that you understand the predicament your little bean is in, it’s time to tackle the mechanics of how to get them headed in the right direction.
The solutions for an oblique lie are often similar to the ones used for a transverse lie. And the best part? There are several exercises that work.
Here are a few that Lipeles recommends:
- doing yoga poses such as downward dog
- sitting on a birthing ball and rolling your hips with an open leg stance (aka pelvic rocking)
- floating in a swimming pool to attempt to get the baby to move into a better position
- remaining in a squatting position to “open the pelvis” to give way to the baby changing their position
One 2019 study found that pelvic rocking on a stability or birthing ball while pregnant contributed to correcting the fetal lie and, more specifically, the oblique lie, in women at or more than 29 weeks pregnant.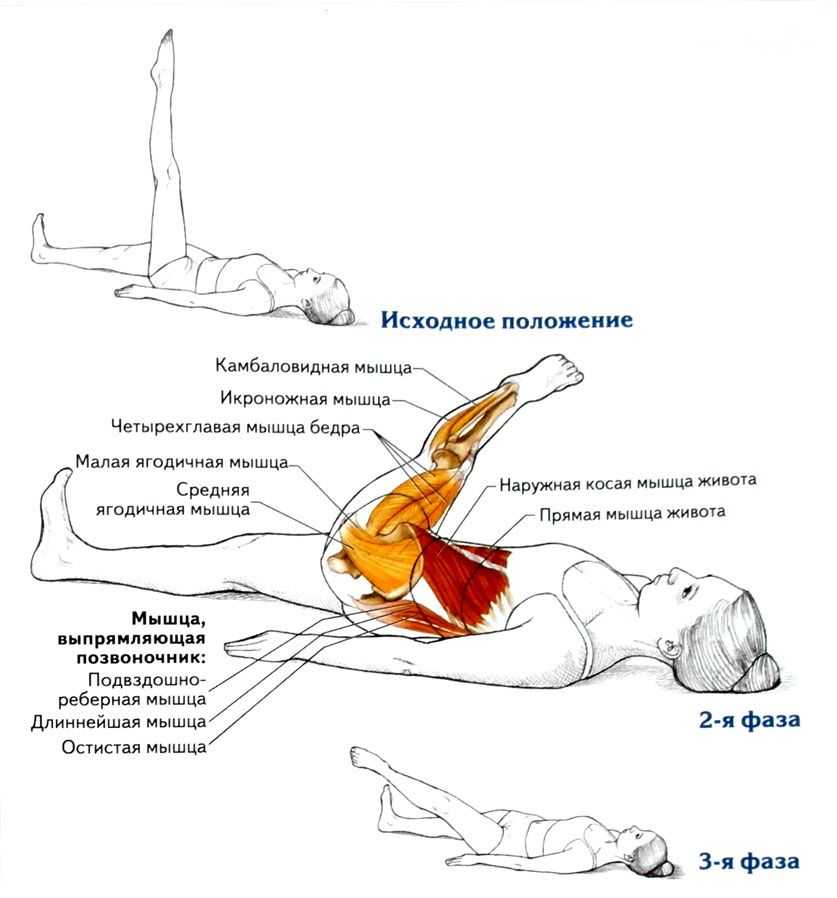 More than 49 percent of women in the intervention group indicated a longitudinal lie compared to 29.8 percent of those in the control group.
More than 49 percent of women in the intervention group indicated a longitudinal lie compared to 29.8 percent of those in the control group.
While all of those interventions can work, Lipeles says in his 14 years of practice, there’s one activity he finds the most effective with both an oblique lie and breech position that you can do at home.
He instructs his patients to take whatever frozen fruits or vegetables (or any other item) they have in the freezer and place them in a thin cloth and leave them on their belly in the area that the baby’s head is positioned.
“The unborn baby is sensitive to changes in temperature, and thus these frozen items near their head are uncomfortable, and will encourage them to move their head away from the cold item, which often leads to the baby moving into a more desirable position,” he explains.
Doctor-involved interventions are also a possibility. Because the head is so close to the pelvic inlet, Ruiz says these lies often respond to manual manipulation or external cephalic version.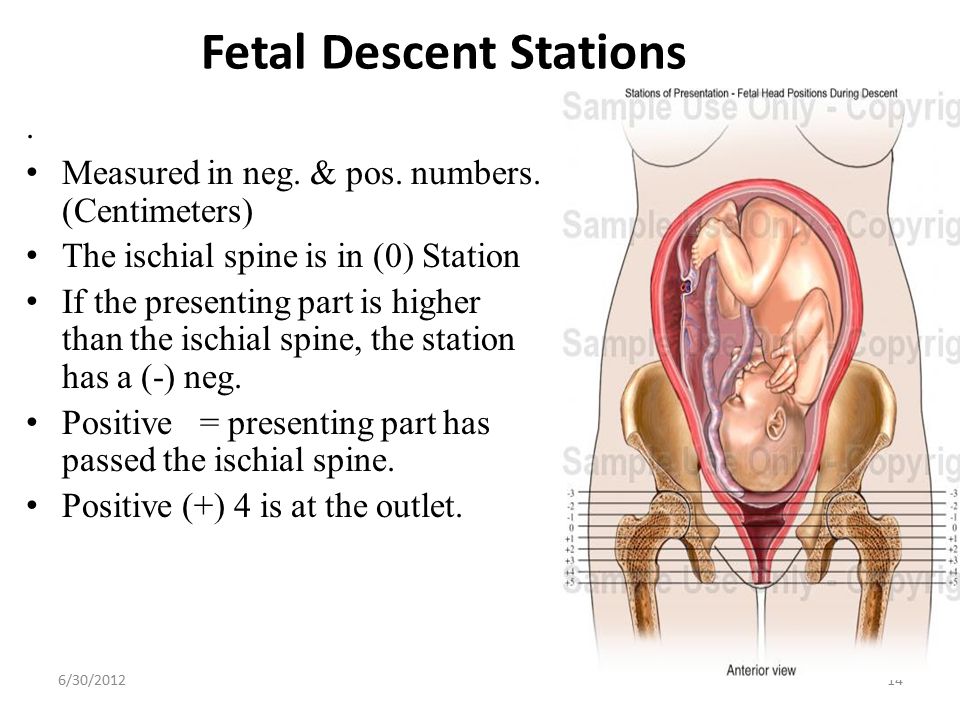
To do this procedure, your doctor, with the help of an ultrasound, will manually guide the head into the pelvis. “If there’s adequate space within the pelvis, the head will usually drop down into a normal position,” he says.
Since uterine contractions can also force the baby’s head into the pelvis, Ruiz says at 39 weeks, a doctor can use external version cephalic techniques to push the baby’s head down into the pelvis and then start an induction.
“This usually works and can lead to a vaginal delivery, if you’ve had more than one pregnancy,” he says. But if this is your first pregnancy, Ruiz says the maneuver is more difficult, and not as successful, because the uterus and abdomen are more firm.
And finally, Kecia Gaither, MD, an OB-GYN and director of perinatal services at NYC Health + Hospitals, says there are some alternative methods like acupuncture and Spinning Babies classes. “Acupuncture, which has been utilized for fetal movement for years, relaxes the mother’s musculature, allowing the baby to turn head-first into the pelvis,” she says.
The classes Gaither is referring to are called “Spinning Babies,” which she says employ certain yoga positions to relax mom and encourage fetal movement into a head-first position.
If you’re nearing your due date, regular labor can also push the baby’s head down into the pelvis. “If this happens, you will get a chance at a vaginal delivery,” says Ruiz. Of course, if the head moves laterally, Ruiz says the baby will move into a transverse lie, and you’ll end up with a cesarean section.
In a normal shaped uterus, the forces of uterine contractions will force the baby’s head in the pelvis. Fortunately, the forces of uterine contractions can force the baby’s head into the pelvis.
But if the contractions don’t push the baby’s head into the pelvis, and you’re going into labor while still in an oblique lie, your doctor will most likely need to perform an expedited C-section.
Your baby will move into various positions before your due date. As you near the end of your pregnancy, your doctor will keep a close eye on the fetal position and recommend interventions if the baby is in an oblique lie.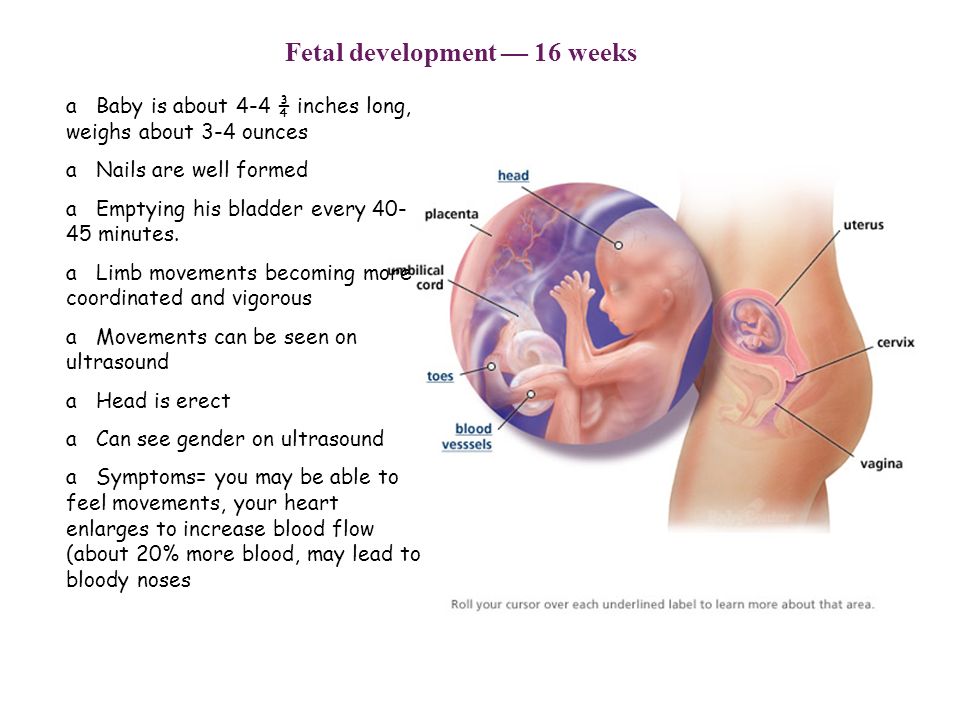
Like other fetal positions, an oblique lie may require a cesarean delivery if the baby doesn’t move into a head-down position before you go into labor.
Pathological position of the fetus - causes, symptoms of the disease, diagnosis and methods of treatment
I confirm More
- INVITRO
- Library
- Directory of diseases
- Pathological...
Pregnancy
Low water
Polyhydramnios
Caesarean section
7110 March 23
Pathological position of the fetus: causes, symptoms, diagnosis and treatment.
Definition
During pregnancy, the fetus can change its position in the uterus many times, as long as there is enough room for it to move. In a normal pregnancy, by the 22-24th week, the fetus is set head down, until about the 32-34th week, its position remains unstable, but then the fetus is fixed.
The position of the fetus is the ratio of its axis passing through the head and buttocks to the longitudinal axis of the uterus.
If the axes of the fetus and uterus coincide, this is called the longitudinal position of the fetus, if the fetus lies across the uterus - the transverse position. In addition, an oblique position is distinguished - the middle between the longitudinal and transverse.
When the fetus is located longitudinally in the uterus, it can be turned towards the entrance to the small pelvis with the head or pelvic end (buttocks, legs). This is the presentation - head or pelvic. In the transverse position, the presenting part is not defined.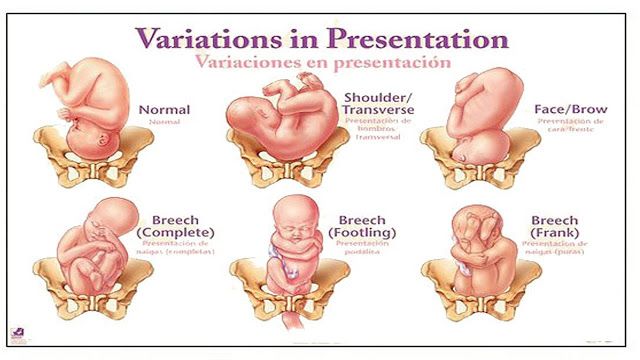
In 95-97% of cases, the presenting part is the head. Breech presentation, when the buttocks or legs of the fetus are above the entrance to the small pelvis, and its head is at the bottom of the uterus, is determined in 3-5% of cases. Oblique and transverse positions (the so-called incorrect positions of the fetus) are detected in 0.3-0.7% of full-term pregnancies, but 10 times more often in multiple births (starting from 4 births) than in primiparas. With a gestation period of less than 32 weeks, while the fetus has enough space to move, the incorrect position of the fetus in the uterus is observed 6 times more often than with a full-term pregnancy.
Pathological positions include breech presentation, transverse, oblique and unstable position of the fetus.
Causes of the pathological position of the fetus
The exact causes of the pathological position of the fetus are not well understood. Factors that contribute to the occurrence of breech presentation, transverse and oblique positions can be divided into maternal, fetal and placental.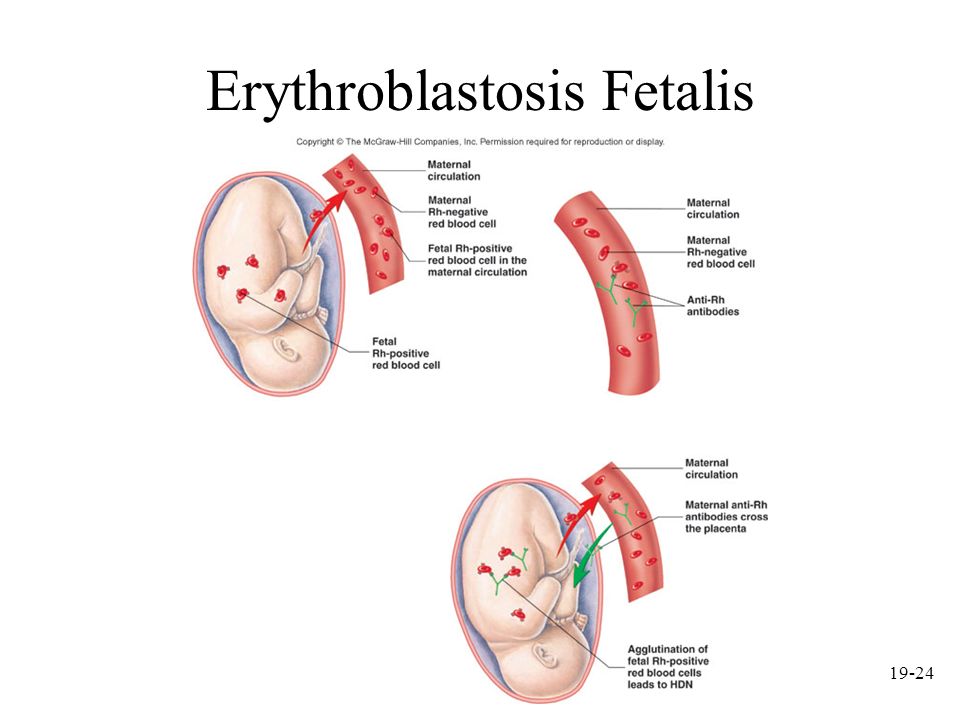
Maternal causes include:
- anomalies in the development of the uterus (bicornuate, saddle uterus, uterine septum),
- uterine tumors,
- narrow pregnant pelvis,
- pelvic tumors,
- decrease or increase in uterine tone,
- a large number of births in a woman,
- scar on the uterus after caesarean section.
Fetal causes:
- prematurity,
- multiple pregnancy,
- intrauterine growth retardation,
- congenital fetal anomalies (anencephaly, hydrocephalus),
- abnormal fetal articulation (relation of limbs to head and torso),
- features of the vestibular apparatus of the fetus.
Placental causes:
- placenta previa,
- oligohydramnios or polyhydramnios,
- short cord.
Classification of the pathological position of the fetus
Breech presentation is divided into breech (80-90%) and foot (10-15%).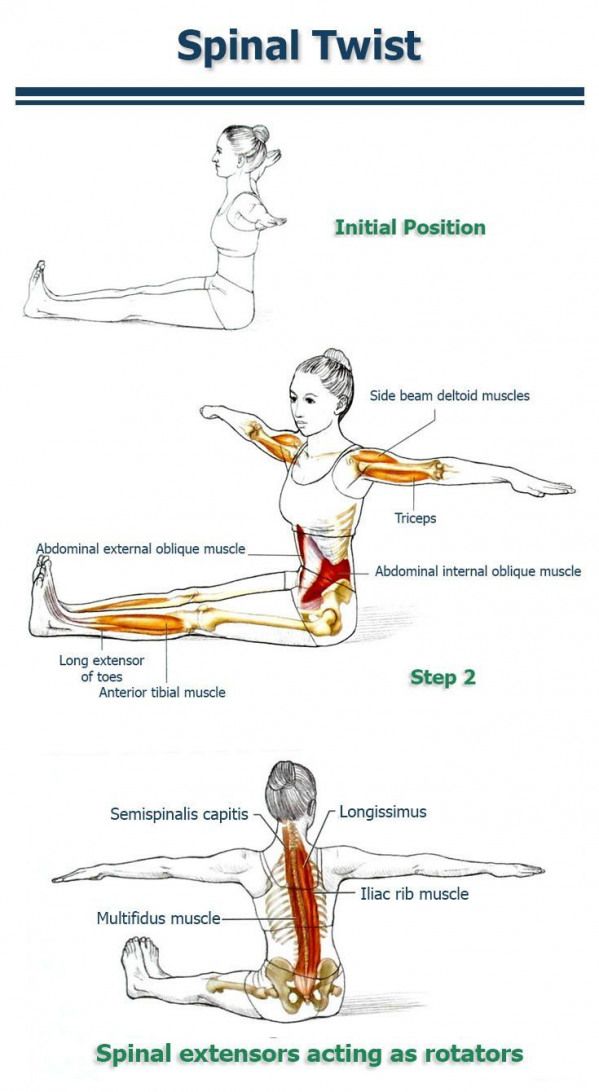 Breech presentation is pure (63-68%) and mixed (20-23%), and foot presentation is complete, incomplete (more common than complete) and knee (rare).
Breech presentation is pure (63-68%) and mixed (20-23%), and foot presentation is complete, incomplete (more common than complete) and knee (rare).
In a purely breech presentation, the buttocks are facing the entrance to the pelvis, and the legs are extended along the body, i.e., bent at the hip and extended at the knee joints, feet are located in the area of the chin and face. With a mixed breech presentation, the buttocks are facing the entrance to the pelvis along with the legs, bent at the hip and knee joints, somewhat unbent at the ankle joints, that is, the fetus is in the “squatting” position.
In full foot presentation, the fetus is turned towards the entrance to the pelvis with both legs slightly extended at the hip and bent at the knee joints; knee joints, located above; in the case of a knee presentation, the legs are unbent at the hip joints and bent at the knee, and the knees are presented to the entrance to the pelvis.
Incorrect include transverse and oblique positions, as well as the unstable position of the fetus.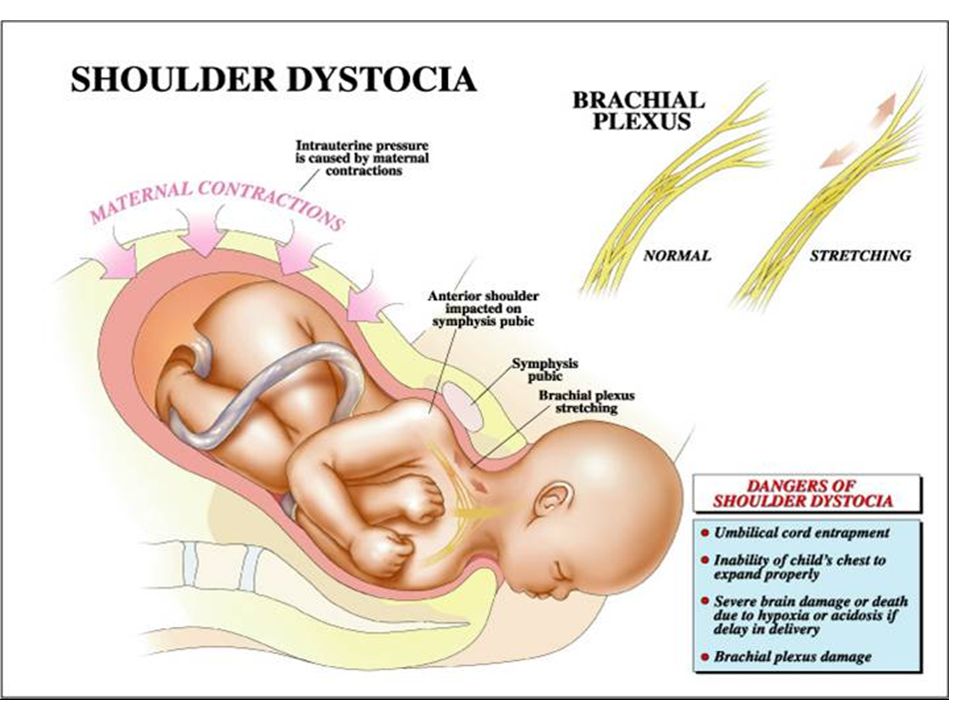
Transverse is the position of the fetus, in which the axis of its trunk intersects the axis of the uterus at a right angle, and large parts of the fetus are located above the iliac crests. An oblique is a position in which the axis of the fetal body intersects the axis of the uterus at an acute angle, and the underlying large part of the fetus is located in one of the iliac cavities of the large pelvis. The oblique position is considered a transitional state, because at the end of the gestation period and during childbirth, it turns into a longitudinal or transverse position.
The oblique position is usually unstable, temporary, which is why it is often called unstable.
Also, in case of incorrect positions, the position of the fetus is determined by the head: if the head is located to the left of the midline of the pregnant woman's body, this is the first position, if to the right, the second.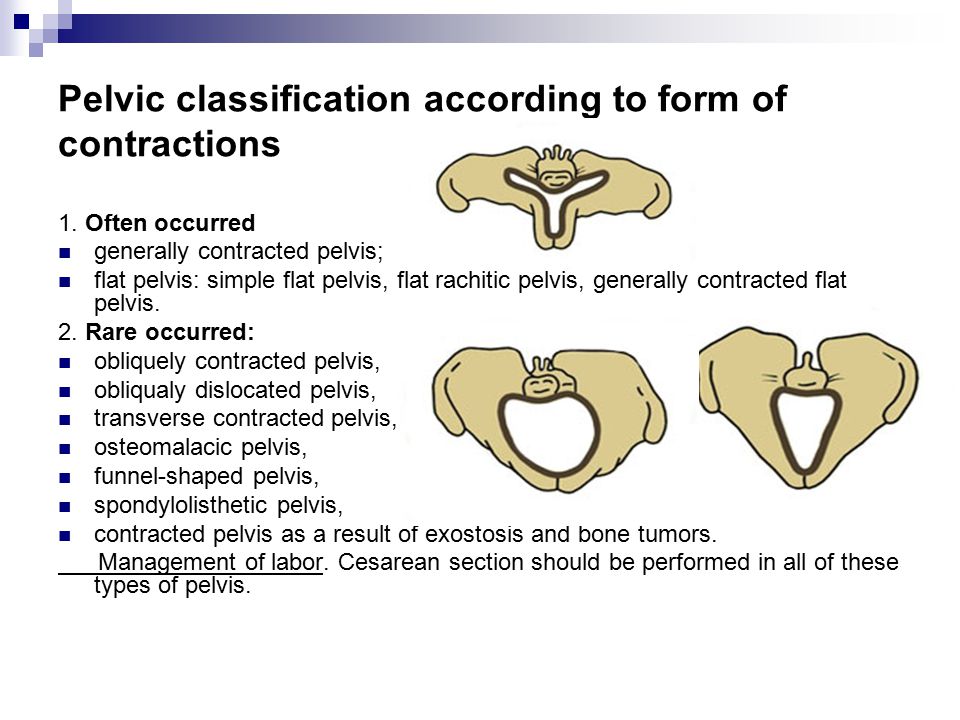 The view is determined by the back: if it is facing anteriorly - front view, backwards - rear. The location of the back of the fetus in relation to the bottom of the uterus and the entrance to the small pelvis matters.
The view is determined by the back: if it is facing anteriorly - front view, backwards - rear. The location of the back of the fetus in relation to the bottom of the uterus and the entrance to the small pelvis matters.
Symptoms of abnormal fetal position
Usually, with a pathological position of the fetus, the pregnant woman does not have specific complaints, however, she may be disturbed by discomfort in the hypochondria, and in the case of a mixed breech or foot presentation of the fetus, a woman may feel the fetus move mainly in the lower abdomen.
Diagnosis of abnormal fetal position
Diagnosis of abnormal fetal position is usually made at 32-34 weeks of gestation. A preliminary diagnosis is established on a gynecological examination. With breech presentation, there is a high standing of the fundus of the uterus. The gynecologist determines this indicator at each visit, starting from the 20th week of pregnancy - it reflects the height to which the widest, domed part of the uterus (its bottom) has risen relative to the pubis.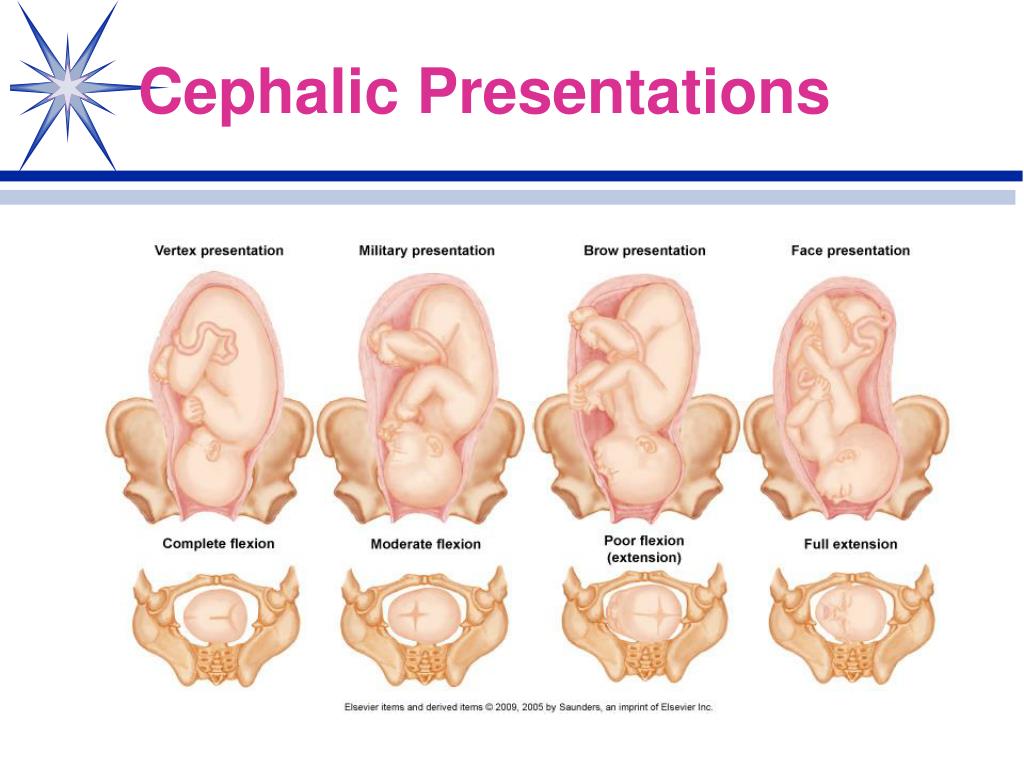 This indicator indirectly indicates whether the pregnancy is proceeding normally. In breech presentation, the pelvic end of the fetus is located high above the entrance to the pelvis, which causes a high standing of the uterine fundus. The head of the fetus is located in the bottom of the uterus, the buttocks are above the entrance to the pelvis, the doctor can determine this by palpation. The fetal heartbeat is heard at or above the umbilicus.
This indicator indirectly indicates whether the pregnancy is proceeding normally. In breech presentation, the pelvic end of the fetus is located high above the entrance to the pelvis, which causes a high standing of the uterine fundus. The head of the fetus is located in the bottom of the uterus, the buttocks are above the entrance to the pelvis, the doctor can determine this by palpation. The fetal heartbeat is heard at or above the umbilicus.
The transverse and oblique position of the fetus can also be suspected by the doctor during the examination. In the transverse position, the belly of the pregnant woman acquires a transverse-oval shape, the bottom of the uterus is lower than in the longitudinal position, there is no large presenting part - the head or pelvic end, and small parts of the fetus, for example, a handle or shoulder, are presented at the entrance to the small pelvis. The fetal heartbeat is best heard in the navel.
In an oblique position, the abdomen visually acquires an oblique-oval shape, the abdominal circumference is greater than normal, the fundus of the uterus is low.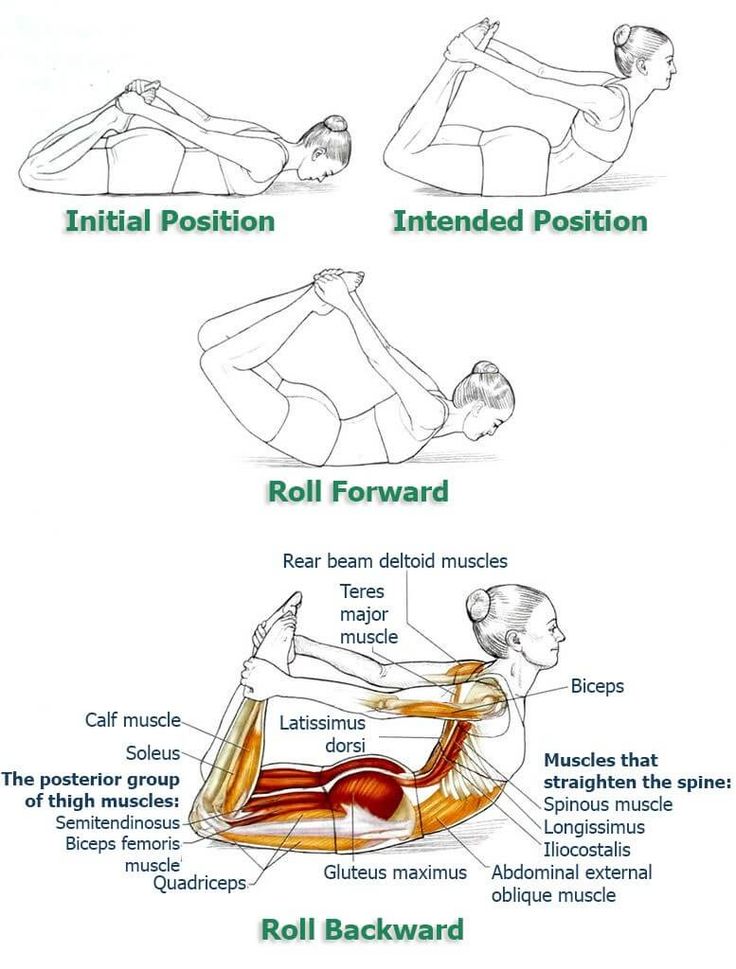 The large presenting part is located below the level of the iliac crest, in one of the iliac fossae of the large pelvis, the fetal heartbeat, as in the transverse position, is better heard in the navel.
The large presenting part is located below the level of the iliac crest, in one of the iliac fossae of the large pelvis, the fetal heartbeat, as in the transverse position, is better heard in the navel.
If the doctor suspects an abnormal position of the fetus, an ultrasound examination is mandatory. When performing ultrasound, reasons that could lead to an incorrect position of the fetus are excluded: severe fetal malformations or an abnormal location of the placenta.
Screening ultrasound of the 3rd trimester of pregnancy (30-34 weeks) with Doppler evaluation of blood flow parameters
Ultrasound examination for functional assessment of intrauterine development of the fetus, its estimated height and weight, as well as blood circulation.
RUB 3,890 Sign up
Which doctors to contact
As in a normal pregnancy, the doctor - obstetrician-gynecologist.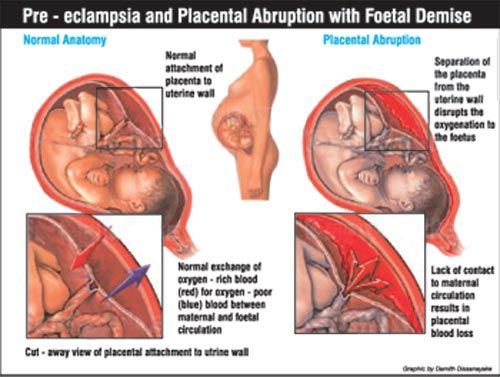
Treatment of abnormal fetal position
Until a certain time, breech presentation requires expectant observation, since the fetus can turn in the right direction on its own. In some cases, doctors may recommend that a pregnant woman perform a set of exercises that help change the breech presentation to the head.
In breech presentation, to reduce the likelihood of a caesarean section and in the absence of contraindications for natural childbirth, the patient may be advised to externally rotate the fetus on the head. Indications and contraindications are determined by the doctor. This procedure is performed by an obstetrician-gynecologist in an obstetric hospital, at a period of ≥36 weeks of gestation in primiparas and ≥37 weeks of gestation in multiparous.
The efficiency of cephalic rotation ranges from 30 to 80%, and in 5% of cases spontaneous reverse rotation of the fetus is observed.
Depending on the situation and the health of the woman and the fetus, the doctor recommends a natural birth or a caesarean section.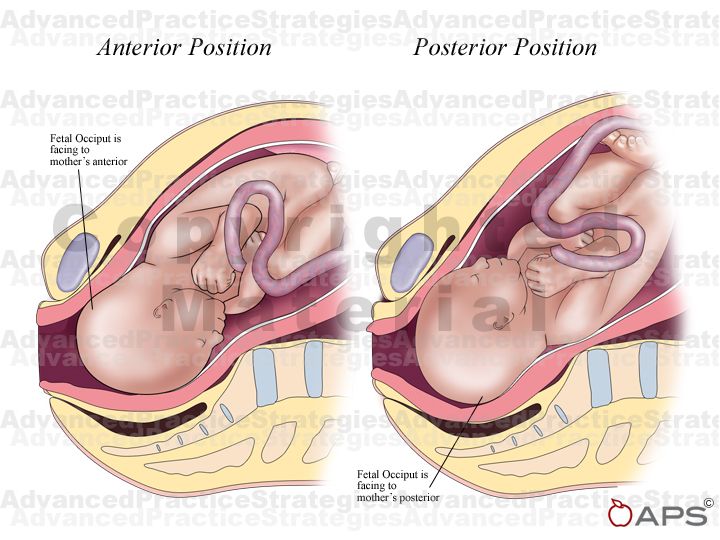
In case of abnormal position of the fetus up to 36 weeks of pregnancy in the absence of contraindications (a scar on the uterus, threatening premature birth, uterine fibroids, placenta previa and low location, somatic pathology of the pregnant woman, etc.), corrective exercises are recommended. The transverse and oblique positions of the fetus are an absolute indication for a caesarean section, it is dangerous to give birth naturally in these cases.
Complications
Breech presentations have higher perinatal morbidity and mortality than cephalic presentations. This is due to a number of reasons: prematurity, hypoxia, birth trauma, damage to the abdominal cavity and spinal cord, abnormalities in the development of the fetus, etc. Perinatal losses in breech presentation with various methods of delivery are 3–5 times higher than with cephalic presentation.
Childbirth with abnormal fetal positions is accompanied by a number of life-threatening complications for the mother and fetus: early outflow of water, prolapse of small parts of the fetus, rupture of the uterus, bleeding from the genital tract with abnormalities in the location of the placenta.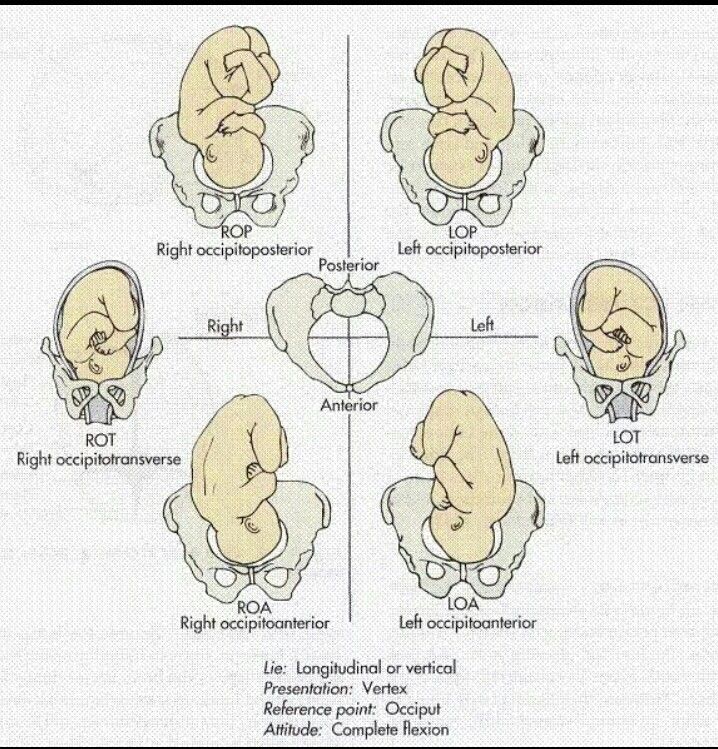
With an unstable or transverse position of the fetus, perinatal mortality reaches 24%.
Prolapse of the umbilical cord loops occurs 20 times more often than in the longitudinal position and head presentation of the fetus. Maternal mortality associated with ascending infection with premature outflow of water, bleeding with an abnormal location of the placenta, complications of surgical aids and uterine rupture, reaches 10%.
Prevention of abnormal fetal position
Currently, there are no effective methods for preventing fetal malposition.
Sources:
- Clinical guidelines "breech presentation of the fetus". Developed by: Russian Society of Obstetricians and Gynecologists. – 2020.
- Pathological childbirth (narrow pelvis, incorrect position of the fetus, anomalies of the contractile activity of the uterus): textbook / O.E. Baryaeva, V.V. Florensov, M.Yu. Akhmetov. FGBOU VO IGMU of the Ministry of Health of Russia, Department of Obstetrics and Gynecology with a course in gynecology of children and adolescents.
 - Irkutsk: IGMU. – 2020. – 88 from
- Irkutsk: IGMU. – 2020. – 88 from
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
-
Huntington's disease
2803 09 April
-
Winivarter-Buerger's disease
2800 08 April
-
Gestational diabetes mellitus
2797 07 April
Show more
Diabetes mellitus
Pregnancy
Edema
Hypertension
Proteinuria
Convulsions
Eclampsia
Preeclampsia
Preeclampsia
Preeclampsia: causes, symptoms, diagnosis and treatment.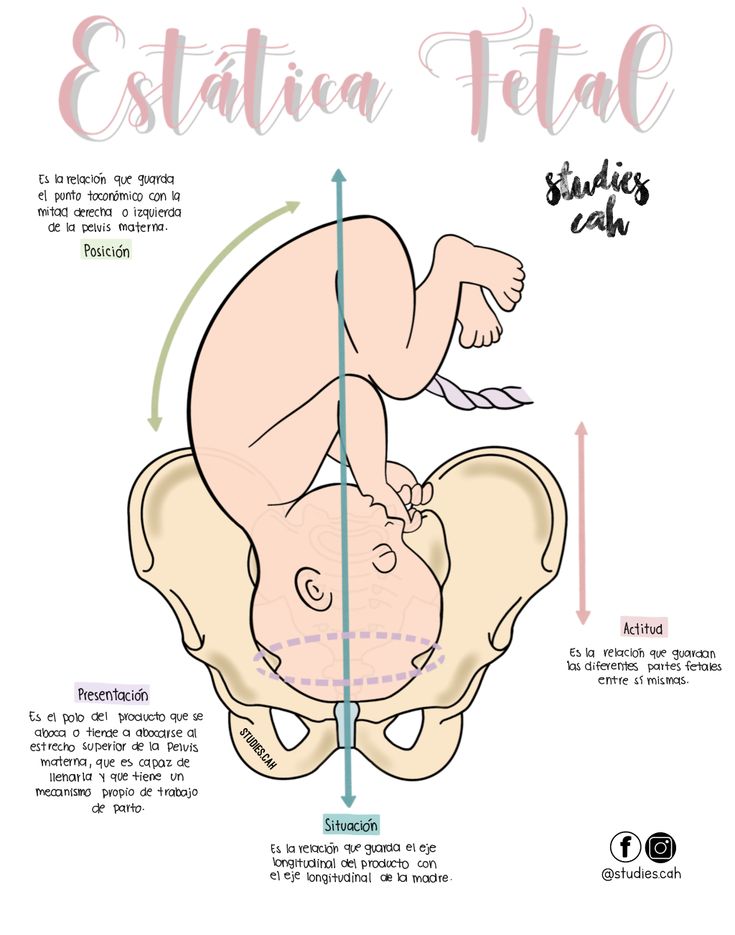
More
Pregnancy
HCG
Fertilized egg
Miscarriage
Tumor
Mole
Mole: causes, symptoms, diagnosis and treatment.
More
Arthritis
Encephalitis
Pregnancy
Rash
Meningitis
Lymphadenopathy
Rubella (German measles, Rubella, Measles)
Rubella: causes, symptoms, diagnosis and treatment.
More
Vomiting
Nausea
Preeclampsia
Pregnancy
Dehydration
Dehydration
Toxicosis of pregnancy
Toxicosis of pregnancy is considered a complication of pregnancy and manifests itself mainly in its first half.
More
Diabetes mellitus
Thyrotoxicosis
Bulimia
Pregnancy
Obesity
Increased hunger
The feeling of hunger is an expression of the body's need for nutrients.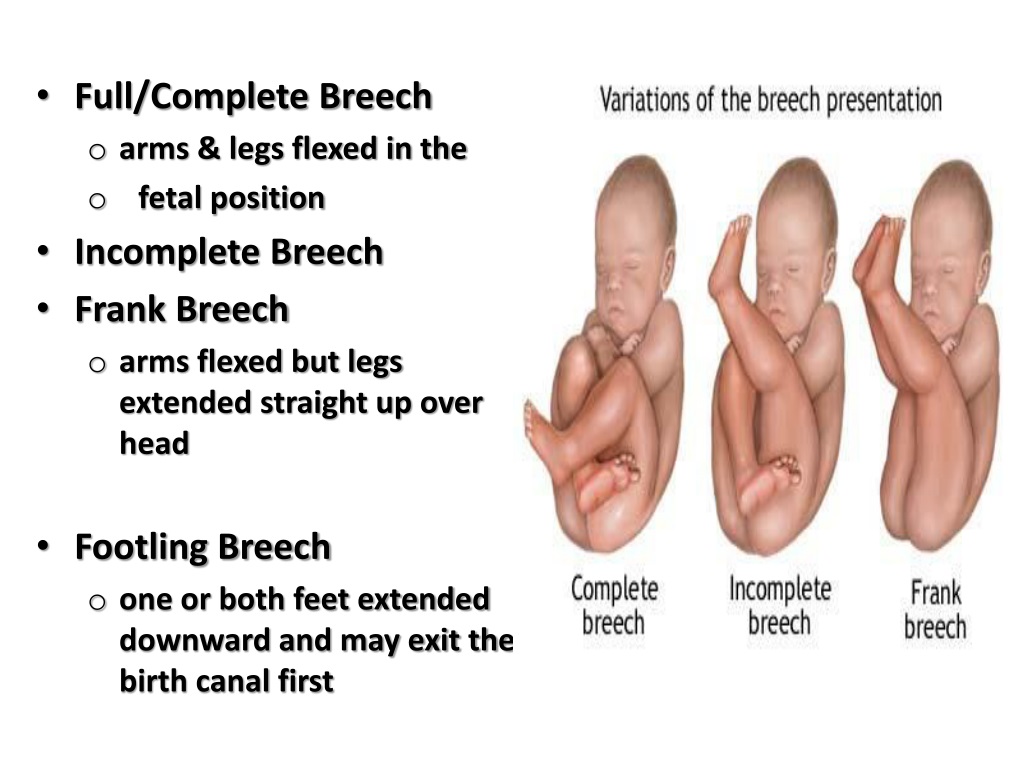
More
Nothing found
Try changing your query or select a doctor or service from the list.
Doctor not found
Try changing your query or select doctor from the list
Medical office not found
Try changing your request or select medical office from list
Therapist Traumatologist-orthopedist Endocrinologist Urologist Gynecologist Ultrasound doctor Cardiologist Pediatrician
Nothing found
Please try editing your query
Thank you!
You have successfully made an appointment
Detailed information has been sent to your e-mail
Subscribe to our newsletters
Enter e-mail
I consent to processing of personal data
Subscribe
Transverse position of the fetus.
 What is the transverse position of the fetus?
What is the transverse position of the fetus? IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Transverse position of the fetus - an incorrect location of the fetus in the uterus, in which its longitudinal axis intersects with the axis of the uterus at an angle of 90 °; while large parts of the fetus (buttocks, head) are located above the line of the crests of the iliac bones of the pelvis. The transverse position of the fetus is determined using an external obstetric and vaginal examination, ultrasound. Pregnancy with a transverse position of the fetus can proceed uncomplicated, however, premature birth is possible, which can pose a threat to the life of the mother and fetus. The optimal tactic in the transverse position of the fetus is operative delivery.
- Causes of transverse fetal position
- Diagnosis of the transverse position of the fetus
- Fetal transverse risks
- Tactics of conducting labor in the transverse position of the fetus
- Prices for treatment
General
The transverse position of the fetus occurs in 0.5-0.7% of pregnancies, and in primiparous women 10 times less than in multiparous women. The danger of the transverse position of the fetus lies in the likelihood of developing severe complications during childbirth if timely obstetric care is not provided: early outflow of water, loss of parts of the fetus, rupture of the uterus, the occurrence of a neglected transverse position of the fetus, death of the fetus and mother.
Variants of malposition of the fetus also include an oblique position, characterized by the intersection of the axis of the fetus and uterus at an acute angle and the placement of one of the large parts of the fetus (head or pelvic end) below the line connecting the iliac crests.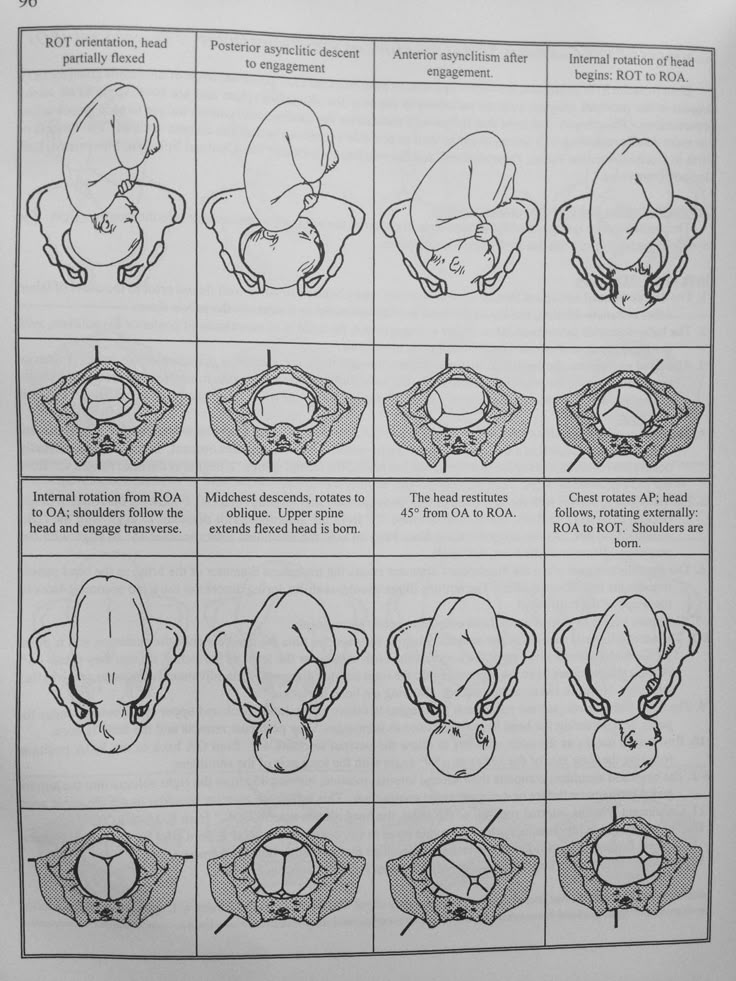 The oblique position of the fetus is considered transitional - during childbirth, it can turn into a longitudinal or transverse position.
The oblique position of the fetus is considered transitional - during childbirth, it can turn into a longitudinal or transverse position.
The position in the transverse position of the fetus is determined by the head: 1st position - when the head is located on the left, 2nd position - the head is determined on the right. The type of position depends on the turn of the back: the back facing the anterior wall of the uterus is regarded as an anterior view, towards the back - a rear view. With the transverse position of the fetus, it is also important to consider the ratio of the back of the fetus to the fundus of the uterus.
Transverse position of the fetus
Causes of the transverse position of the fetus
The intrauterine transverse position of the fetus may be due to various factors. These, first of all, include conditions that ensure excessive fetal mobility: polyhydramnios, flabbiness of the muscles of the abdominal wall, fetal hypotrophy, etc.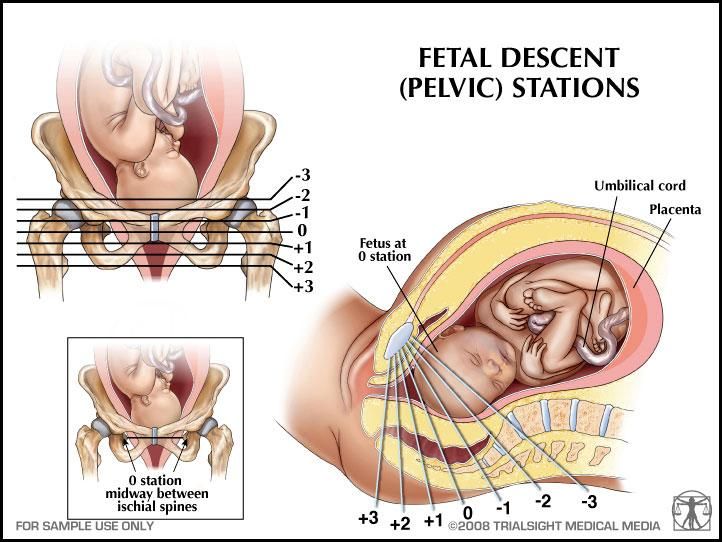 , increased tone of the uterus, the threat of spontaneous abortion, anomalies in the structure of the uterus (saddle or bicornuate uterus), uterine fibroids, etc.
, increased tone of the uterus, the threat of spontaneous abortion, anomalies in the structure of the uterus (saddle or bicornuate uterus), uterine fibroids, etc.
The transverse position of the fetus in some cases is the result of anatomical reasons that prevent the insertion of the head into the small pelvis, in particular, placenta previa, tumors of the lower segment of the uterus or pelvic bones, narrow pelvis. The transverse position can be facilitated by such fetal developmental anomalies as anencephaly and hydrocephalus.
Diagnosis of the transverse position of the fetus
An incorrect (oblique or transverse) position of the fetus is established during an obstetric examination of a pregnant woman, palpation of the abdomen and vaginal examination. With the transverse position of the fetus, the abdomen acquires a transversely stretched (obliquely stretched) irregular shape. Due to transverse stretching, the uterus has a spherical, and not elongated-oval shape. Attention is drawn to the excess of the norm of the circumference of the abdomen in comparison with the gestational age and the insufficient height of the fundus of the uterus.
Attention is drawn to the excess of the norm of the circumference of the abdomen in comparison with the gestational age and the insufficient height of the fundus of the uterus.
In the process of palpation, the presenting part of the fetus is not determined; the head can be felt to the right or left of the median axis of the body of the pregnant woman, and large parts (head or pelvic end) - in the lateral sections of the uterus. With the transverse position of the fetus, the heartbeat is better heard in the navel. Difficulties in determining the position and position of the fetus may arise in situations of multiple pregnancy, polyhydramnios, uterine hypertonicity. Obstetric ultrasound reliably confirms the transverse position of the fetus.
A gynecological examination performed during pregnancy and the initial period of childbirth with a intact fetal bladder is not very informative. Its implementation only confirms the absence of the presenting part of the fetus at the entrance to the small pelvis.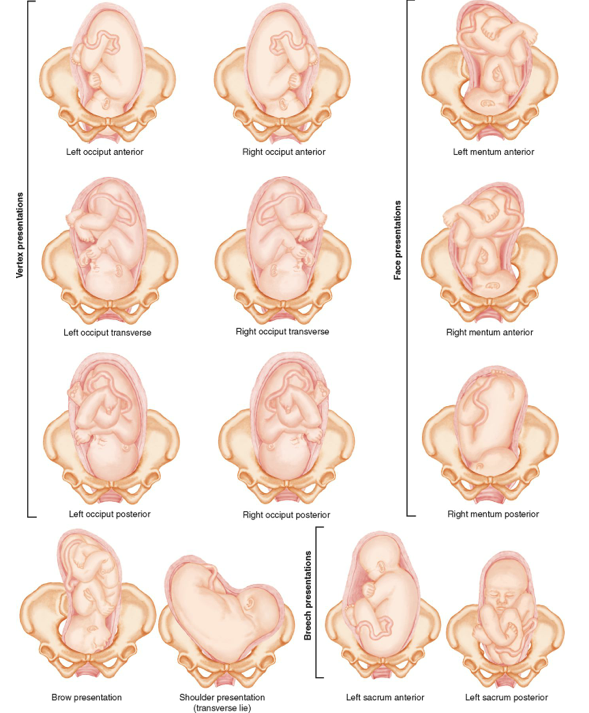 After the discharge of water and the opening of the uterine pharynx by 4-5 cm, with the transverse position of the fetus, the shoulder, shoulder blade, ribs, axilla, spinous processes of the vertebrae, sometimes the elbow or hand of the handle can be determined. In the event that the fetal handle falls out of the genital slit, there is no doubt that the fetus has a transverse position.
After the discharge of water and the opening of the uterine pharynx by 4-5 cm, with the transverse position of the fetus, the shoulder, shoulder blade, ribs, axilla, spinous processes of the vertebrae, sometimes the elbow or hand of the handle can be determined. In the event that the fetal handle falls out of the genital slit, there is no doubt that the fetus has a transverse position.
Risks of transverse fetal position
The presence of the transverse position of the fetus, as a rule, does not violate the general course of pregnancy. However, most often in the transverse position of the fetus, premature rupture of amniotic fluid and the development of premature birth occur. If the transverse position of the fetus is accompanied by placenta previa, massive bleeding is possible.
The rapid discharge of water often leads to a sharp restriction of fetal mobility, driving the shoulder into the pelvic inlet, falling out of the fetus parts (handles, umbilical cord) and the development of the so-called neglected transverse position of the fetus.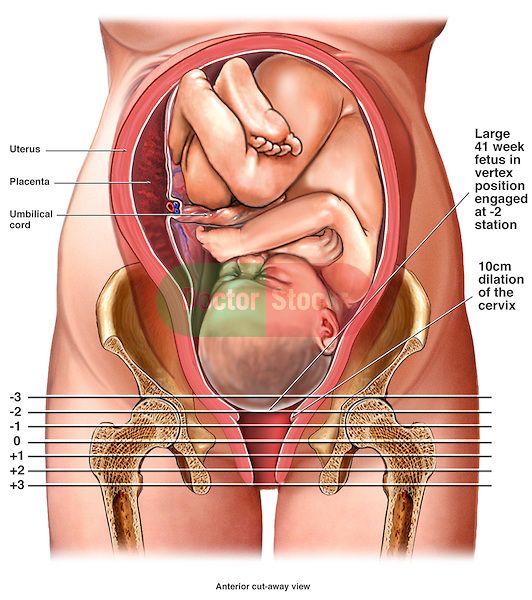
When parts of the fetus fall out, ascending infection can occur with the development of chorioamnionitis, diffuse peritonitis, and sepsis. A long anhydrous interval lasting 12 or more hours leads to acute hypoxia or fetal asphyxia. The neglected transverse position of the fetus against the background of increasing labor activity threatens to rupture the uterus.
In rare cases, with the transverse position of the fetus during childbirth, self-torsion in the head or pelvic presentation or the birth of a baby with a double body can occur. Such an outcome of childbirth is an exception and is possible in case of strong contractions, deep prematurity of the fetus, or with a dead fetus.
Tactics of conducting labor in the transverse position of the fetus
For up to 34-35 weeks of gestation, the oblique or transverse position of the fetus is considered unstable, since it can independently change to a longitudinal one.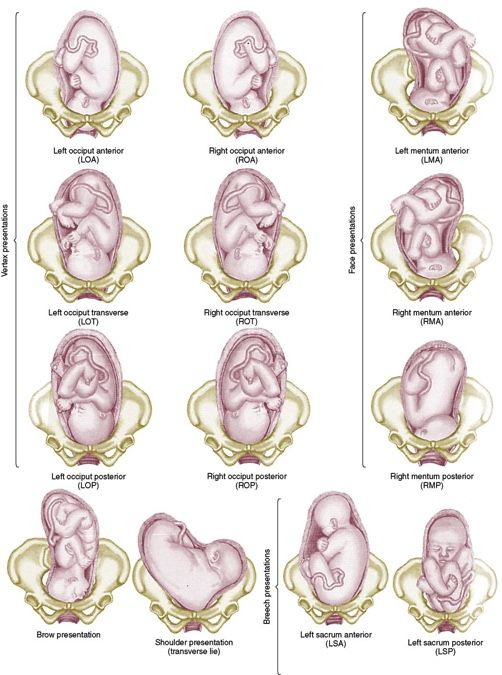 When diagnosing the transverse position of the fetus, a complete gynecological examination of the pregnant woman is required to identify the causes of the anomaly, the choice of tactics for further management of pregnancy and the method of delivery.
When diagnosing the transverse position of the fetus, a complete gynecological examination of the pregnant woman is required to identify the causes of the anomaly, the choice of tactics for further management of pregnancy and the method of delivery.
At a period of 30-34 weeks of pregnancy, corrective gymnastics may be prescribed, which contributes to the reversal of the fetus in the head presentation. Special sets of exercises are indicated in the absence of signs of a threatened abortion, a scar on the uterus, fibroids, spotting, decompensated heart defects in a pregnant woman, etc., and are carried out under the supervision of an obstetrician-gynecologist observing the woman. Also, in the transverse position of the fetus, a pregnant woman is recommended to lie on her side for more time, corresponding to the position being determined.
After 35-36 weeks of gestation, the fetus takes a stable position, therefore, while maintaining the transverse position, the pregnant woman is hospitalized in the maternity hospital to determine the tactics of delivery.
The technique of external rotation to the head - changes in the transverse position of the fetus using external techniques is currently practically not used. This is due to the low efficiency of the rotation, since, with unresolved causes, the fetus often again assumes a transverse position. In some cases, external rotation can result in serious consequences: placental abruption, uterine rupture, fetal hypoxia.
The optimal method of delivery of patients with a transverse position of the fetus is a planned caesarean section. Absolute indications for operative delivery are post-term pregnancy, the presence of placenta previa, premature discharge of amniotic fluid, scars on the uterus, and the development of fetal hypoxia. When the transverse position of the fetus is started with the prolapse of its handle or umbilical cord, the reduction of the fallen parts is unacceptable.
In the case of full disclosure of the cervix, determined by the live fetus and its mobility, it is possible to turn the fetus on the leg and its subsequent extraction.