Pregnancy genetic testing results
Prenatal Genetic Screening Tests | ACOG
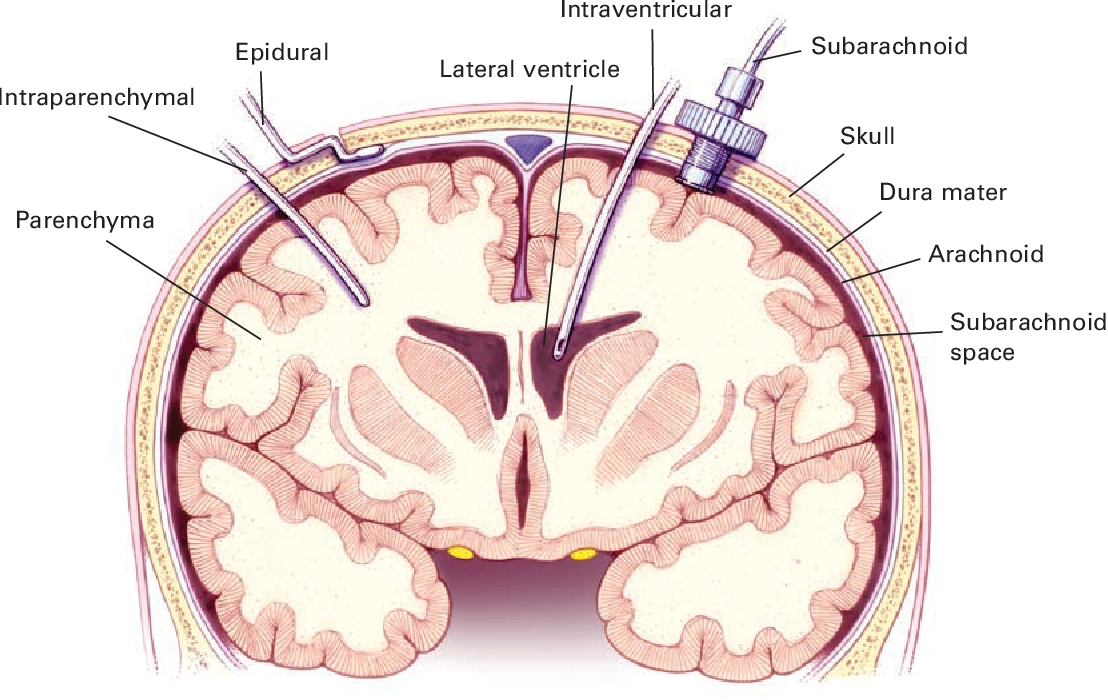
Amniocentesis: A procedure in which amniotic fluid and cells are taken from the uterus for testing. The procedure uses a needle to withdraw fluid and cells from the sac that holds the fetus.
Aneuploidy: Having an abnormal number of chromosomes. Types include trisomy, in which there is an extra chromosome, or monosomy, in which a chromosome is missing. Aneuploidy can affect any chromosome, including the sex chromosomes. Down syndrome (trisomy 21) is a common aneuploidy. Others are Patau syndrome (trisomy 13) and Edwards syndrome (trisomy 18).
Carrier Screening: A test done on a person without signs or symptoms to find out whether he or she carries a gene for a genetic disorder.
Cell-Free DNA: DNA from the placenta that moves freely in a pregnant woman’s blood. Analysis of this DNA can be done as a noninvasive prenatal screening test.
Cells: The smallest units of a structure in the body. Cells are the building blocks for all parts of the body.
Chorionic Villus Sampling (CVS): A procedure in which a small sample of cells is taken from the placenta and tested.
Chromosomes: Structures that are located inside each cell in the body. They contain the genes that determine a person’s physical makeup.
Cystic Fibrosis (CF): An inherited disorder that causes problems with breathing and digestion.
Diagnostic Tests: Tests that look for a disease or cause of a disease.
DNA: The genetic material that is passed down from parent to child. DNA is packaged in structures called chromosomes.
Down Syndrome (Trisomy 21): A genetic disorder that causes abnormal features of the face and body, medical problems such as heart defects, and mental disability. Most cases of Down syndrome are caused by an extra chromosome 21 (trisomy 21).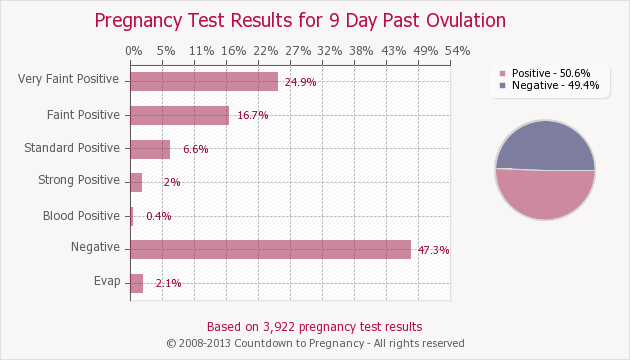
Edwards Syndrome (Trisomy 18): A genetic condition that causes serious problems. It causes a small head, heart defects, and deafness.
Fetus: The stage of human development beyond 8 completed weeks after fertilization.
Genes: Segments of DNA that contain instructions for the development of a person’s physical traits and control of the processes in the body. The gene is the basic unit of heredity and can be passed from parent to child.
Genetic Counselor: A health care professional with special training in genetics who can provide expert advice about genetic disorders and prenatal testing.
Genetic Disorders: Disorders caused by a change in genes or chromosomes.
Inherited Disorders: Disorders caused by a change in a gene that can be passed from parents to children.
Monosomy: A condition in which there is a missing chromosome.
Mutations: Changes in genes that can be passed from parent to child.
Neural Tube Defects (NTDs): Birth defects that result from a problem in development of the brain, spinal cord, or their coverings.
Nuchal Translucency Screening: A test to screen for certain birth defects, such as Down syndrome, Edwards syndrome, or heart defects. The screening uses ultrasound to measure fluid at the back of the fetus’s neck.
Obstetrician: A doctor who cares for women during pregnancy and their labor.
Patau Syndrome (Trisomy 13): A genetic condition that causes serious problems. It involves the heart and brain, cleft lip and palate, and extra fingers and toes.
Placenta: An organ that provides nutrients to and takes waste away from the fetus.
Screening Tests: Tests that look for possible signs of disease in people who do not have signs or symptoms.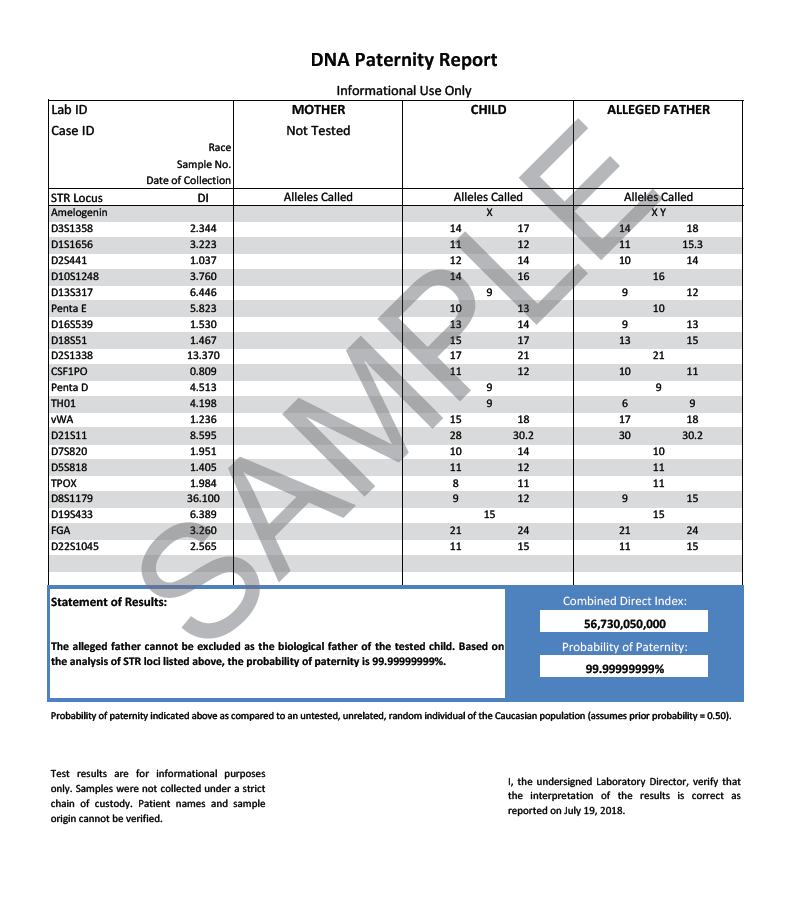
Sex Chromosomes: The chromosomes that determine a person’s sex. In humans, there are two sex chromosomes, X and Y. Females have two X chromosomes and males have an X and a Y chromosome.
Sickle Cell Disease: An inherited disorder in which red blood cells have a crescent shape, which causes chronic anemia and episodes of pain.
Tay–Sachs Disease: An inherited disorder that causes mental disability, blindness, seizures, and death, usually by age 5.
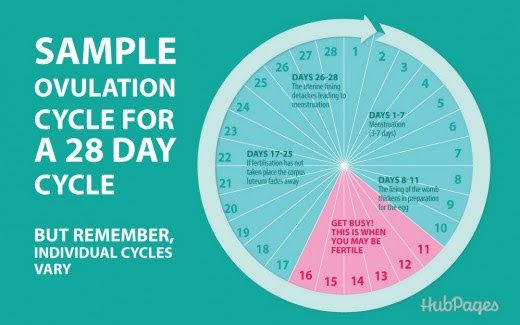
Trimester: A 3-month time in pregnancy. It can be first, second, or third.
Trisomy: A condition in which there is an extra chromosome.
Ultrasound Exams: Tests in which sound waves are used to examine inner parts of the body. During pregnancy, ultrasound can be used to check the fetus.
Pregnancy - NIPS Non Invasive Chromosome Screening
Testing and continuity of care for preconception, pregnancy and pediatric care
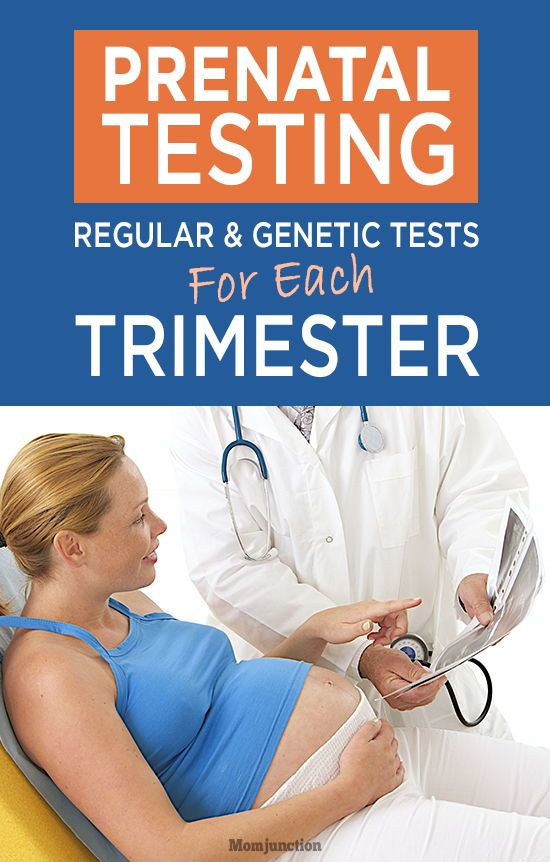
Pregnancy is a dynamic time. Whether you’re looking for carrier screening, routine tests or more advanced diagnostic testing, Labcorp is one of the few laboratories that can deliver pregnancy insights while providing a true continuity of care and support throughout the entire pregnancy period and beyond.
Whether you’re looking for carrier screening, routine tests or more advanced diagnostic testing, Labcorp is one of the few laboratories that can deliver pregnancy insights while providing a true continuity of care and support throughout the entire pregnancy period and beyond.
It’s a fact—getting early and regular prenatal care improves the chances of a healthy pregnancy.
Laboratory testing is a crucial part of your prenatal care and helps your doctor make sure you and your baby are well at this important time.
Carrier Screening
Carrier screening can help determine if you and your partner are at an increased risk of having a baby with a specific inherited disorder, such as cystic fibrosis or spinal muscular atrophy. Early insight can help you better prepare for the future.
Labcorp offers choice in carrier screening, from a comprehensive screen for more than 500 disorders to screening for specific disorders. Your doctor can help you determine which test is right for you.
When should I get screened?
Carrier screening can be performed at any time but is most useful if it is performed before pregnancy or as early as possible during pregnancy.
Learn more about carrier screening tests
Early Pregnancy Health Screening
Routine and regular lab tests are suggested for all women as part of routine prenatal care. These tests can help confirm that you are healthy, as well as provide vital information to help you manage and decrease any risks that your health may pose to your newborn baby. Talk to your doctor about what tests are right for you.
When should I get testing?
Learn more about early pregnancy health screening
NIPS (NIPT) Screening
By detecting small amounts of DNA from the placenta in your bloodstream, a noninvasive prenatal test (NIPS/NIPT) can help identify if there is an increased chance for certain chromosome abnormalities that can affect your baby’s health and development.
 It can also indicate if you are more likely to have a boy, girl or both.
It can also indicate if you are more likely to have a boy, girl or both.Most NIPSs (NIPTs) screen for certain chromosomal abnormalities called trisomies. These include trisomy 21 (Down syndrome), trisomy 18 (Edwards syndrome) and trisomy 13 (Patau syndrome).
When should I get screening?
NIPS (NIPT) can be performed in any of the trimesters during pregnancy but is typically not performed until after nine weeks to ensure there are enough fetal cells to screen.
Learn more about NIPS (NIPT) tests
Prenatal Serum Screening
Prenatal or maternal serum screening tests are another noninvasive option for determining the chance your baby may have a chromosome abnormality that may affect their development. These screening assays can help to detect Down syndrome, trisomy 18 or open neural tube defects, depending on the particular test your doctor uses and how far along you are in your pregnancy.
Similar to NIPS (NIPT), a positive serum screen can be confirmed with a diagnostic test.
 Your doctor can help determine which tests are right for you.
Your doctor can help determine which tests are right for you.When should I get screening?
Prenatal or maternal serum screening is typically performed in the first and second trimesters, and they may be done with sequential blood samples—one collected in the first trimester and another collected in the second trimester.
Learn more about serum screening options
Prenatal & Pediatric Diagnostic
Diagnostic procedures, such as amniocentesis and chorionic villus sampling (CVS), are used to perform tests for chromosomal abnormalities, open neural tube defects and/or specific inherited diseases in an ongoing pregnancy.
We also offer pediatric diagnostic testing to analyze chromosomes in newborns and infants for changes that can explain certain birth defects or developmental delays.
When would testing be considered?
Prenatal diagnostic testing is not a routine test during pregnancy but can be considered or recommended by your physician when clinically indicated, such as in the case of a positive NIPS (NIPT) or prenatal/maternal serum screening result.
 CVS specimens are generally collected at nine weeks or later, and amniotic fluid samples are not recommended to be collected before 15 weeks.
CVS specimens are generally collected at nine weeks or later, and amniotic fluid samples are not recommended to be collected before 15 weeks.
- Carrier Screening
- Early Health Screening
- NIPS (NIPT) Screening
- Serum Screening
- Prenatal & Pediatric Diagnostic
Carrier Screening
Carrier screening can help determine if you and your partner are at an increased risk of having a baby with a specific inherited disorder, such as cystic fibrosis or spinal muscular atrophy. Early insight can help you better prepare for the future.
Labcorp offers choice in carrier screening, from a comprehensive screen for more than 500 disorders to screening for specific disorders. Your doctor can help you determine which test is right for you.
When should I get screened?
Carrier screening can be performed at any time but is most useful if it is performed before pregnancy or as early as possible during pregnancy.
Learn more about carrier screening tests
Early Pregnancy Health Screening
Routine and regular lab tests are suggested for all women as part of routine prenatal care. These tests can help confirm that you are healthy, as well as provide vital information to help you manage and decrease any risks that your health may pose to your newborn baby. Talk to your doctor about what tests are right for you.
When should I get testing?
Learn more about early pregnancy health screening
NIPS (NIPT) Screening
By detecting small amounts of DNA from the placenta in your bloodstream, a noninvasive prenatal test (NIPS/NIPT) can help identify if there is an increased chance for certain chromosome abnormalities that can affect your baby’s health and development. It can also indicate if you are more likely to have a boy, girl or both.
Most NIPSs (NIPTs) screen for certain chromosomal abnormalities called trisomies. These include trisomy 21 (Down syndrome), trisomy 18 (Edwards syndrome) and trisomy 13 (Patau syndrome).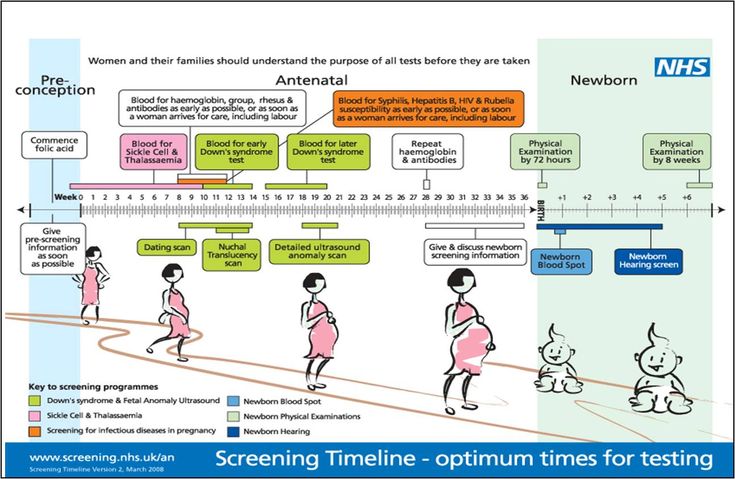
When should I get screening?
NIPS (NIPT) can be performed in any of the trimesters during pregnancy but is typically not performed until after nine weeks to ensure there are enough fetal cells to screen.
Learn more about NIPS (NIPT) tests
Prenatal Serum Screening
Prenatal or maternal serum screening tests are another noninvasive option for determining the chance your baby may have a chromosome abnormality that may affect their development. These screening assays can help to detect Down syndrome, trisomy 18 or open neural tube defects, depending on the particular test your doctor uses and how far along you are in your pregnancy.
Similar to NIPS (NIPT), a positive serum screen can be confirmed with a diagnostic test. Your doctor can help determine which tests are right for you.
When should I get screening?
Prenatal or maternal serum screening is typically performed in the first and second trimesters, and they may be done with sequential blood samples—one collected in the first trimester and another collected in the second trimester.
Learn more about serum screening options
Prenatal & Pediatric Diagnostic
Diagnostic procedures, such as amniocentesis and chorionic villus sampling (CVS), are used to perform tests for chromosomal abnormalities, open neural tube defects and/or specific inherited diseases in an ongoing pregnancy.
We also offer pediatric diagnostic testing to analyze chromosomes in newborns and infants for changes that can explain certain birth defects or developmental delays.
When would testing be considered?
Prenatal diagnostic testing is not a routine test during pregnancy but can be considered or recommended by your physician when clinically indicated, such as in the case of a positive NIPS (NIPT) or prenatal/maternal serum screening result. CVS specimens are generally collected at nine weeks or later, and amniotic fluid samples are not recommended to be collected before 15 weeks.
Ovia® Pregnancy App
Download Ovia® Pregnancy to see how big your baby is, track your weekly milestones and access a library of pregnancy features and tools.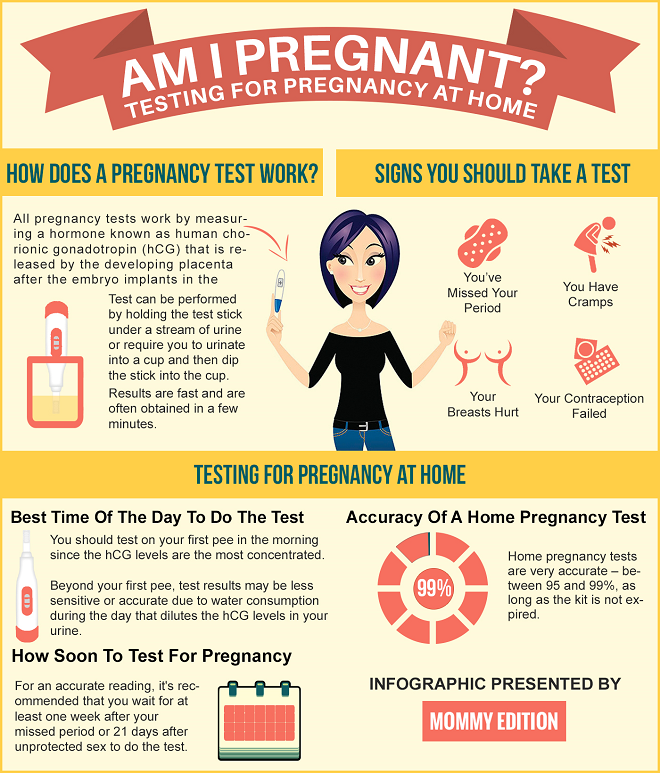
Learn more »
Labcorp OnDemandPurchase the same tests trusted by doctors, directly from Labcorp.
Get Started »
Genetic Counseling
Genetics is complicated. Navigating the world of genetics doesn’t have to be.
Learn More »
Reference:
- US Preventive Services Task Force. Screening for Gestational Diabetes: US Preventive Services Task Force recommendation statement. JAMA. 2021;326(6):531-538. DOI:10.1001/jama.2021.11922.
what does genetic analysis show during pregnancy and where to do it in Moscow?
Every expectant mother wants to be 100% sure that her baby will be born healthy. But until recently, it was possible to verify this only with the help of risky research methods, which were prescribed only for vital indications. Now there is a safe way to detect genetic abnormalities in the fetus - a non-invasive DNA test. What does it show and how is it carried out? We understand the topic and answer questions.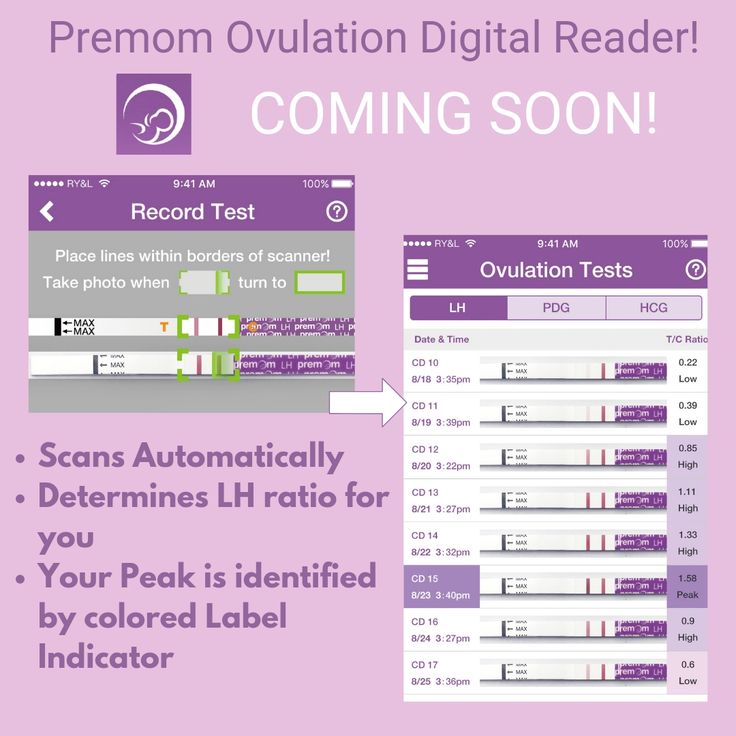
During pregnancy, most genetic defects in the fetus can be diagnosed with a DNA test, and are often performed for this purpose.
Here are the main purposes of a DNA test for pregnant women:
Diagnosis of chromosomal abnormalities:
- Down syndrome (additional chromosome in the twenty-first pair) occurs in about one in a thousand newborns [1]. With the increase in the age of the expectant mother, the risk of giving birth to a baby with an anomaly increases. Children with Down syndrome are often born with heart defects, epilepsy, their physical development lags behind the norm, and all have more or less severe mental retardation.
- Edwards syndrome occurs due to the presence of an extra chromosome in the eighteenth pair. This is a rare anomaly: it occurs in about one in 7,000 cases [2]. Newborns with Edwards syndrome have numerous malformations: 90-95% of them die in the first months.
- Patau syndrome is trisomy of the thirteenth pair.
 This anomaly is even rarer, affecting approximately one in 14,000 newborns[3]. Like Edwards syndrome, this type of hereditary pathology is manifested by multiple gross malformations; life expectancy of patients rarely exceeds a year.
This anomaly is even rarer, affecting approximately one in 14,000 newborns[3]. Like Edwards syndrome, this type of hereditary pathology is manifested by multiple gross malformations; life expectancy of patients rarely exceeds a year.
Important
Ultrasound screening is performed for early diagnosis of Down, Edwards and Patau syndromes. Some features of the development of the fetus allow us to suggest chromosomal abnormalities: an increased width of the collar zone, a shortened nasal bone, and others. But in the first trimester, ultrasound signs cannot be considered as reliable evidence of disorders, and later, when the screening results become more convincing, time may be lost. Meanwhile, research among 18 955 women showed that the most accurate test for the presence of chromosomal abnormalities is DNA analysis during pregnancy (in the first trimester) [4].
- Anomalies in the number of sex chromosomes .
 These include Klinefelter syndrome, Shereshevsky-Turner syndrome and many other abnormalities associated with a decrease or increase in the normal number of X and Y chromosomes. Such genetic defects are often accompanied by underdevelopment of the gonads (sex glands), infertility, various changes in appearance, often mental retardation.
These include Klinefelter syndrome, Shereshevsky-Turner syndrome and many other abnormalities associated with a decrease or increase in the normal number of X and Y chromosomes. Such genetic defects are often accompanied by underdevelopment of the gonads (sex glands), infertility, various changes in appearance, often mental retardation.
Diagnosis of congenital pathologies of the nervous system . For example, a DNA test early in pregnancy can detect Rett syndrome (a severe neuropsychiatric disorder that does not become apparent until several months after birth), infantile epileptic encephalopathy, and other CNS disorders.
Identification of hereditary forms of craniosynostosis (premature fusion of the bones of the skull) - Pfeiffer, Aper, Cruzon, Müncke syndromes.
Many other genetic diseases poorly diagnosed by traditional screening can be detected by DNA testing during pregnancy.
Determination of the sex of the unborn baby .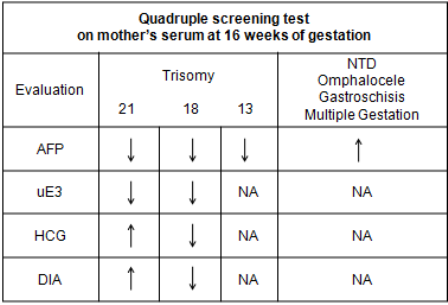 Yes, you can see it on the screen of the ultrasound machine already during the second screening. But sometimes you need to get a 100% accurate result as early as possible. This is necessary primarily for the timely diagnosis of hereditary anomalies associated with sex. For example, hemophilia and Klinefelter's syndrome occur only in boys, while Turner's syndrome affects only girls. The reliability of sex determination by prenatal DNA testing at seven to nine weeks of gestation is 95%, from 12 weeks onwards it reaches 99% [5].
Yes, you can see it on the screen of the ultrasound machine already during the second screening. But sometimes you need to get a 100% accurate result as early as possible. This is necessary primarily for the timely diagnosis of hereditary anomalies associated with sex. For example, hemophilia and Klinefelter's syndrome occur only in boys, while Turner's syndrome affects only girls. The reliability of sex determination by prenatal DNA testing at seven to nine weeks of gestation is 95%, from 12 weeks onwards it reaches 99% [5].
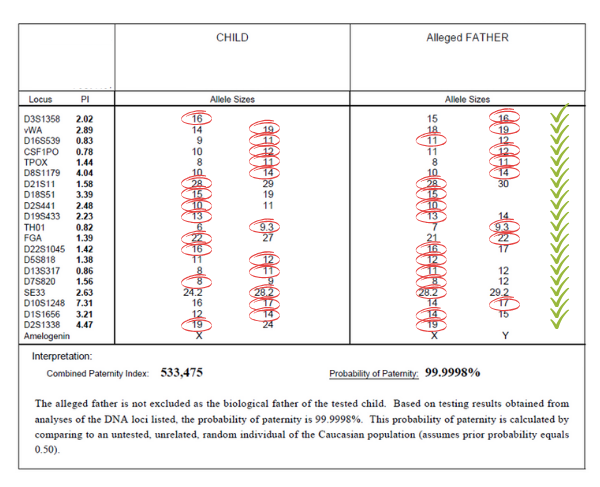
Establishment of paternity . The need for this study arises for various reasons. For example, it may be required if the future father refuses to admit his involvement in the conception. In controversial cases, the results of the examination can serve as evidence in court.
Indications and contraindications for testing
It is natural for any expectant mother to worry about the health of her baby, so the mere desire of a pregnant woman is enough to perform a non-invasive genetic test.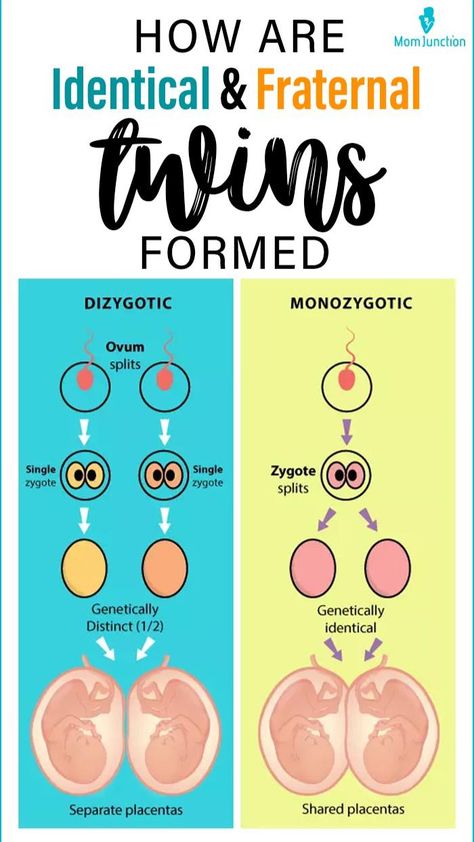 This cannot be said about invasive research methods that carry a risk to the fetus and therefore are not carried out without strict indications. But there are situations when genetic analysis is simply necessary for pregnant women. Such a study is highly desirable if:
This cannot be said about invasive research methods that carry a risk to the fetus and therefore are not carried out without strict indications. But there are situations when genetic analysis is simply necessary for pregnant women. Such a study is highly desirable if:
- Routine screening showed that there is a high risk of giving birth to a child with anomalies. According to the results of ultrasound, it is impossible to draw a conclusion about the presence of Down syndrome and other hereditary pathologies in the fetus, one can only suspect this for a number of reasons. To clarify the diagnosis, the pregnant woman is sent for DNA analysis. Previously, it was possible to confirm or refute malformations only through traumatic and risky methods - amniocentesis, cordocentesis and others. Not so long ago, a safe alternative appeared - a non-invasive prenatal genetic test.
- Expectant mother over 35 years old. With age, the likelihood of having a child with Down syndrome increases.
 Other chromosomal abnormalities are less dependent on this indicator, but some association can also be traced.
Other chromosomal abnormalities are less dependent on this indicator, but some association can also be traced. - The woman has a history of miscarriages or miscarriages. A common cause of miscarriage lies precisely in the genetic defects of the fetus. If the last pregnancy ended unsuccessfully, it makes sense to make sure that everything is in order this time.
- In the family of the future mother or father, there were cases of the appearance of children with hereditary pathologies. Until the results of the study are available, a recurrence of such a situation cannot be completely ruled out.
- One of the future parents suffered from alcohol or drug addiction. Even if the problem is in the past, the risk to the child's health still exists.
- In the first weeks of pregnancy, a woman suffered from an acute infectious disease (the most dangerous of them is rubella) or experienced the effects of other teratogenic factors (which can lead to abnormalities in the development of the fetus).
 The latter include radiation exposure, taking certain medications (for example, tetracycline antibiotics), drinking alcohol, poisoning with salts of heavy metals.
The latter include radiation exposure, taking certain medications (for example, tetracycline antibiotics), drinking alcohol, poisoning with salts of heavy metals.
There are cases when it is not possible to carry out genetic testing of pregnant women. The main contraindication to invasive tests is the threat of miscarriage. Also, studies are not performed for acute infections, inflammatory gynecological diseases, myoma. A non-invasive test for genetic abnormalities is not done for multiple pregnancies (triplets or more), since in this case it is difficult to determine the DNA of each fetus and the data may be inaccurate. The analysis is not performed in surrogate mothers and women who conceived by fertilization with a donor egg (with the exception of certain types of testing). It is impossible to obtain reliable test data if a blood transfusion or bone marrow transplantation was performed shortly before pregnancy.
How testing is done
There are many types of genetic tests performed during pregnancy, but all of them can be divided into two groups depending on the method of sampling. From this point of view, invasive and non-invasive methods are distinguished. The former are associated with the penetration of the future mother and fetus into the body, the latter do not imply such an intervention.
From this point of view, invasive and non-invasive methods are distinguished. The former are associated with the penetration of the future mother and fetus into the body, the latter do not imply such an intervention.
Invasive tests
All studies in this group carry a certain risk of spontaneous abortion, so they are resorted to only in extreme cases - if the likelihood of genetic abnormalities in the fetus is high enough.
Chorionic villus biopsy is the earliest invasive test and is performed at 10-14 weeks. The material for analysis is the tissue cells of the chorion - the future placenta. The fence is carried out by puncturing the abdominal wall and uterus with a long needle. The procedure is performed under ultrasound guidance. The accuracy of diagnosing genetic abnormalities by this method is 99% [6]. The same study performed at a later date is called placentocentesis.
Amniocentesis - analysis of fetal DNA contained in amniotic fluid cells. It is used in the second trimester of pregnancy. Using a syringe with a needle, the fetal bladder is punctured through the abdominal wall and a small amount of amniotic fluid (about 30 ml) is taken. The results of the study need to wait two to three weeks. The accuracy of the method also reaches 99%.
It is used in the second trimester of pregnancy. Using a syringe with a needle, the fetal bladder is punctured through the abdominal wall and a small amount of amniotic fluid (about 30 ml) is taken. The results of the study need to wait two to three weeks. The accuracy of the method also reaches 99%.
Cordocentesis is an analysis of cord blood, which is also taken through the abdominal wall. The procedure is also performed in the II trimester. With the help of cordocentesis, genetic diseases, infections and other intrauterine pathologies can be determined.
Non-invasive genetic test
The technique is relatively new for Russia, and such testing is not yet carried out in all medical centers. This is due to the insufficient equipment of the laboratories of state institutions, and the rather high cost of the study (because it cannot be used everywhere, like screening).
In contrast to all the methods described above, non-invasive testing for fetal genetic abnormalities can be said to be safe. To take a biomaterial, you do not need to resort to a puncture and other traumatic interventions that can lead to complications. For analysis, only the blood of a pregnant woman is needed, which is taken from a vein in the usual way. No special preparation is required for the study.
To take a biomaterial, you do not need to resort to a puncture and other traumatic interventions that can lead to complications. For analysis, only the blood of a pregnant woman is needed, which is taken from a vein in the usual way. No special preparation is required for the study.
The test is carried out using high-tech medical equipment. The blood taken from a woman in a centrifuge is divided into erythrocyte mass, a layer of leukocytes and plasma. DNA from the last two fractions is "deciphered" by sequencing, separating the genomes of the mother and fetus. The resulting material is analyzed for the risk of chromosomal and other pathologies. The method of analysis depends on the type of testing. The entire research process takes an average of two weeks.
The informativeness of tests differs depending on their type. Almost all such analyzes are able to determine the presence or absence of Down syndrome, Edwards and Patau, sex chromosome anomalies, the sex of the unborn child. Some methods are suitable for studying the genetic risks of pregnancy after IVF (including with a donor egg). The reliability of the results of non-invasive testing reaches 99%.
Some methods are suitable for studying the genetic risks of pregnancy after IVF (including with a donor egg). The reliability of the results of non-invasive testing reaches 99%.
In addition to safety and high accuracy, the study has another weight advantage - the ability to perform DNA analysis in early pregnancy. It is done starting at nine to ten weeks, when fetal DNA begins to be detected in the mother's blood. No screening method or invasive test is performed at such times. Early diagnosis of pathologies is crucial in maintaining pregnancy, and the confidence that the unborn child is healthy allows you to expect his birth with joy and without fear.
Thanks to the latest technology in medicine, it has become possible to determine the risk of hereditary diseases in the fetus without resorting to invasive research methods. Genetic analysis of the blood of pregnant women is accurate and safe, and besides, it is the earliest of all possible ways to detect intrauterine pathologies.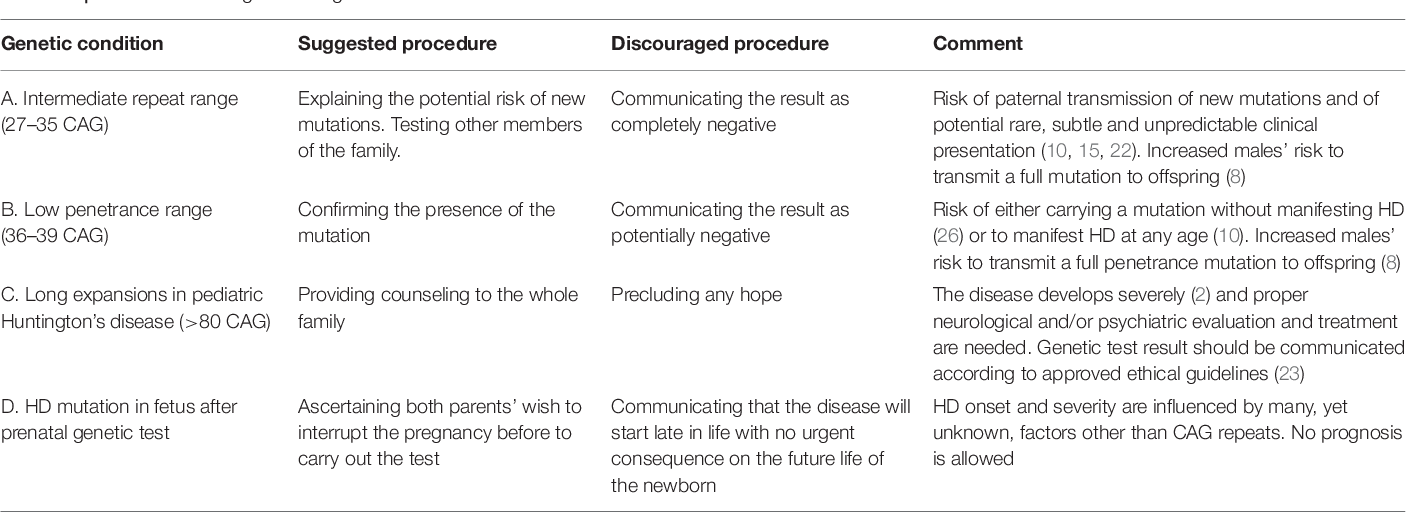 This testing has two drawbacks: firstly, it is paid, and secondly, it is carried out so far only in a few clinics.
This testing has two drawbacks: firstly, it is paid, and secondly, it is carried out so far only in a few clinics.
Frequently asked questions about biochemical screening of pregnant women
Which tests are performed on pregnant women?
Currently, two main types of tests are recommended for pregnant women in St. Petersburg:
- analysis for PAPP-A and beta-hCG in the period of 9-13 weeks
- analysis for AFP and hCG.
Should I do a “triple test”?
Some private laboratories use the so-called "triple test", using kits that, in addition to AFP and hCG, have added the determination of the concentration of another hormone - unconjugated estriol. According to modern data, its assessment for clarifying the risks of fetal chromosomal pathology has too little weight and is highly dependent on many other factors of the woman's condition, which is not significant for calculating risks for fetal chromosomal pathology. If the results of the “double” test reveal an increased risk for you, it is better to contact a geneticist and understand the situation, taking into account a professional clinical assessment of the test results.
If the results of the “double” test reveal an increased risk for you, it is better to contact a geneticist and understand the situation, taking into account a professional clinical assessment of the test results.
How important is it to accurately indicate the weight of a pregnant woman when taking blood for “fetal proteins”?
Each woman's weight must be recorded on the examination referral. In the absence of such information, the risk can be calculated "according to the average" weight of pregnant women in this period - 60 kg.
All women are different - there are pregnant women weighing 45 and 145 kg. For a more accurate assessment of the results, an amendment is introduced in accordance with the "weight category". But absolute accuracy is not required here - individual grams will not change the calculations. An individual approach is important. Therefore, we always measure a woman's weight before taking tests.
I took a blood test for fetal proteins, as the doctor prescribed them immediately after taking them, now I'm worried, so I had a hearty breakfast in the morning. Will this affect the outcome of the study? Can I retake blood on an empty stomach?
Don't worry! Unlike most "adult" tests that are sensitive to food intake, the measurement of the amount of any proteins entering the mother's blood from the fetus is not dependent on the time of the meal. The most important thing here is to know exactly the gestational age established by ultrasound. It makes no sense to retake the analysis. And it is very important for pregnant women to eat breakfast and continue to eat more often during the day than usual.
In clinics where an individual approach to the examination of pregnant women is possible, and of course, in our Center for Fetal Medicine, blood for screening tests can be donated throughout the working day.
Which test is better - PAPP-A and beta-hCG or AFP and hCG?
At present, the first one has the absolute advantage. It has been proven that it is more specific for assessing risks for chromosomal pathology, including Down syndrome. Its important advantage is that it is carried out in the first trimester, you can donate blood from the age of 9weeks of pregnancy (determined by the size of the fetus on ultrasound). The most optimal terms for this analysis are 9-12 weeks. A study period of up to almost 14 (13 weeks 6 days) is allowed, but the reliability of the risk assessment will be lower.
If you have completed a full first trimester test, performed an ultrasound and received a conclusion from a geneticist that the fetus is at low risk for chromosomal abnormalities, testing for AFP and hCG is not worth it.
In special cases, after the first screening, a test for AFP and hCG is prescribed as an additional test on the recommendation of a geneticist.
If you missed the first screening test, then, of course, you need to donate blood at least for the second one within 15-18 weeks.
I would like to emphasize that, on the recommendation of international experts in prenatal diagnosis, analysis for PAPP-A and beta-hCG in a period of 9-12 weeks is recommended for all pregnant women at any age.
I went through the IVF procedure and used a donor cell, since my cells do not mature at 46 years old. Now 12 weeks. How do I correctly pass a biochemical test?
You urgently need to donate blood for PAPP-A and beta-hCG and perform an ultrasound. From your age, the IVF procedure itself does not change the amount of proteins. And the risk "by proteins" will be assessed depending on certain concentrations.
But the computer program calculates the "combined" risks - by proteins, by ultrasound and by the age of the woman, more precisely, by the "age of the egg." Accordingly, for this analysis, the age of the egg donor must be indicated in the calculation referral. If you do not know it exactly, you can calculate by low age risk, since all donors have age restrictions for participating in the IVF program. If you have already been calculated according to your age, don't worry, we can reassess the risks taking into account real data and issue you a Medical Genetic Conclusion based on the results of prenatal studies.
Doctors of the Center for Fetal Medicine are one of the leading specialists in prenatal diagnostics, candidates of medical sciences, doctors of the highest categories with a narrow specialization and extensive experience in prenatal medicine.
All ultrasound examinations in the center are carried out according to the international standards FMF (Fetal Medicine Foundation) and ISUOG (International Society for Ultrasound in Obstetrics and Gynecology).
Ultrasound doctors have international certificates from the Fetal Medicine Foundation (Fundamental Medicine Foundation, UK), which are are confirmed annually.
We take care of the most complex cases and, if necessary, it is possible to consult with specialists from King's College Hospital, King's College Hospital (London, UK).
The pride of our Centers - modern and high-tech medical equipment from General Electric: expert-class ultrasonic devices Voluson E8 / E10
The capabilities of these devices allow us to talk about a new level of information content.