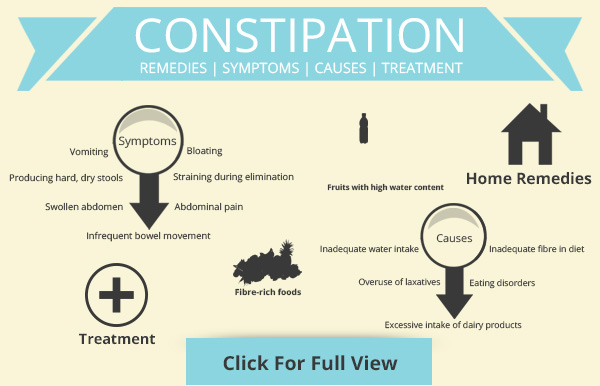
Disadvantages of an epidural
Side effects of an epidural
Epidurals are usually safe, but as with all medical treatments, side effects and complications can sometimes happen.
For more on side effects of epidurals in labour, read about pain relief in labour.
Low blood pressure
It's normal for your blood pressure to fall a little when you have an epidural. Sometimes this can make you feel sick.
Your blood pressure will be closely monitored. If necessary, fluids and medicine can be given through a drip to keep your blood pressure normal.
Loss of bladder control
After having an epidural, you may not be able to feel when your bladder is full because the epidural affects the surrounding nerves.
A catheter may be inserted into your bladder to allow urine to drain away. Your bladder control will return to normal when the epidural wears off.
Itchy skin
This can be a side effect of the pain relief medicines that may be used in your epidural.
Medicine can be given to help the itching, or the medicine in the epidural can be changed.
Feeling sick
Feeling sick (nausea) is less common with epidural medicines than with other pain relief medicines such as morphine and other opiates.
It can be treated with anti-sickness medicines, or by raising your blood pressure if it's low.
Inadequate pain relief
The epidural may not block all your pain. You may be offered an extra, or alternative, pain relief method.
Headache
A severe headache can happen if the bag of fluid that surrounds your spine is accidentally punctured. You may need specific treatment for the headache.
A procedure known as a blood patch may be used to seal the puncture. It involves taking a small sample of your blood and injecting it into the puncture.
When the blood thickens (clots), the hole will be sealed and your headache will stop.
Not all headaches from an epidural require a blood patch. Your anaesthetist will discuss your options with you.
Slow breathing
Occasionally, some medicines used in an epidural can cause slow breathing or drowsiness.
You will be monitored closely to look for this, and it can be treated easily.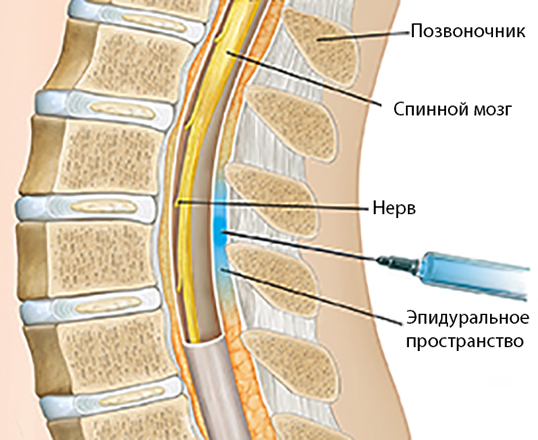
Temporary nerve damage
The needle or epidural tube can damage nerves, but this is uncommon. Nerve damage can cause loss of feeling or movement in parts of your lower body.
The most common symptom is a small, numb area with normal movement and strength. This usually gets better after a few days or weeks, but can sometimes take months.
Infection
An infection can sometimes happen around the skin next to the epidural tube.
It's rare for the infection to spread. Antibiotics may be necessary or, rarely, emergency surgery.
Permanent nerve damage
In rare cases, an epidural can lead to permanent loss of feeling or movement in, for example, 1 or both legs.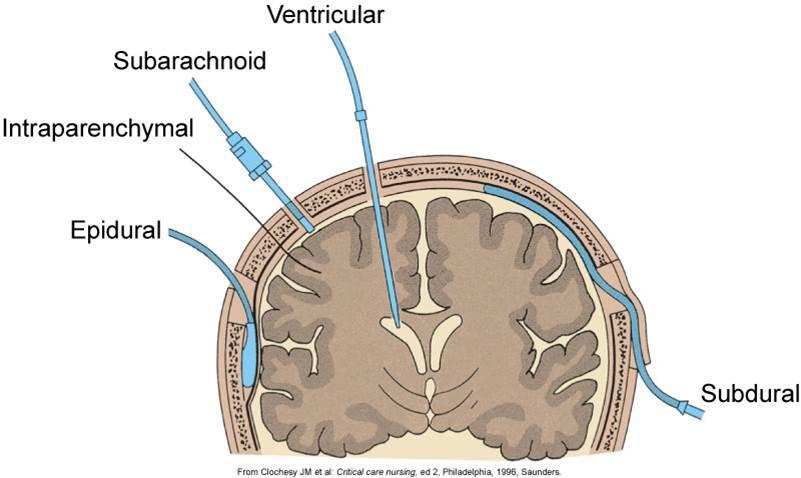
The causes are:
- direct damage to the spinal cord from the epidural needle or catheter
- infection deep in the epidural area or near the spinal cord
- bleeding in the epidural area, causing pressure on the spinal cord
- accidentally injecting the wrong medicine into the epidural catheter
These are rare events, and anaesthetists have extensive training to reduce the chances of these complications.
Nerve damage can also happen for other reasons during surgery, which are unrelated to the epidural.
Other complications
Other, very rare, complications of an epidural include:
- fits (convulsions)
- severe breathing difficulties
- death
Before deciding to have an epidural, you should discuss the procedure with your anaesthetist.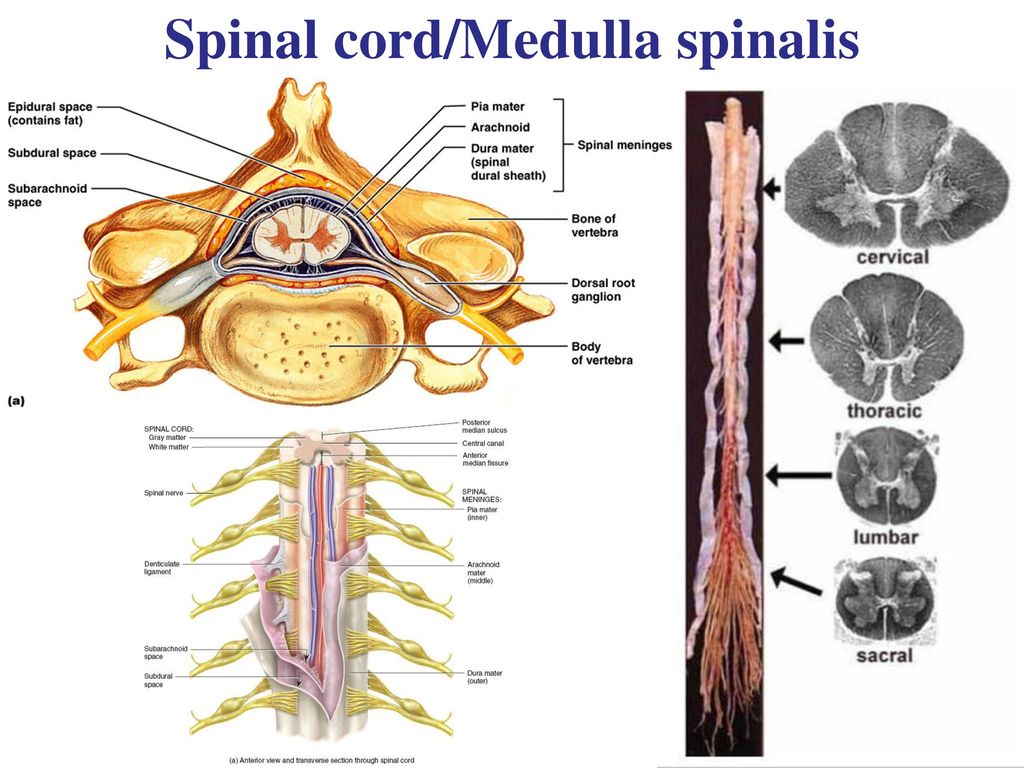
They can provide further information and advice on the risks of developing complications.
Page last reviewed: 01 February 2023
Next review due: 01 February 2026
Should I Get One During Labor?
It’s no secret that delivering a baby can be painful, yet the decision about whether or not to use an epidural is a personal one for you and your family.
An epidural is used to block nerve signals (like the ones responsible for feelings of pain) from the lower part of your spine.
It’s administered through a catheter that is run through a large needle inserted into the epidural space that surrounds your spinal cord. The catheter remains in place during labor and delivery to continue delivering the medication.
Depending on the health of baby and your pregnancy, and the specifics of your labor and delivery, epidural may not be option for you.
You may also change your mind about whether or not to use an epidural in the moment.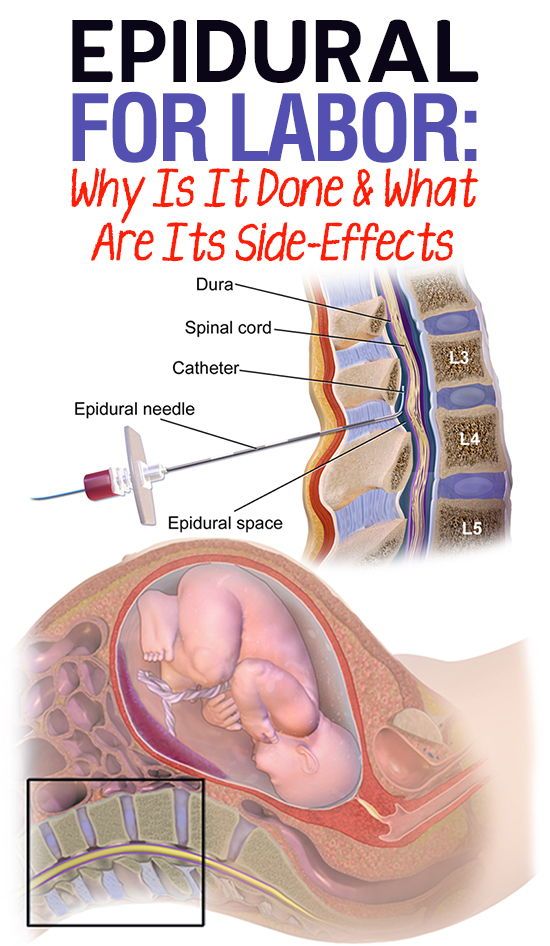 But understanding the pros and cons can help empower you to feel like you’re able to make the best decision for you and your baby.
But understanding the pros and cons can help empower you to feel like you’re able to make the best decision for you and your baby.
Did you know?
Epidurals are most commonly known for their use during labor, but can also be used during lower body surgical procedures, such as surgery on the pelvis or legs. An epidural is sometimes also used to provide pain relief after a procedure.
Was this helpful?
The following are some of the pros of having an epidural.
Pain relief
Epidural is one of the most effective methods for pain relief during delivery and childbirth, and it has minimal side effects on both mom and baby.
It works quickly and can begin to relieve pain within 10 to 20 minutes. Most women who have an epidural feel little or no pain during labor and delivery.
It allows you to rest
Relief from the pains of labor can help you get more rest. This can be especially beneficial if you have a long labor.
Being able to relax and avoid pain can also provide a more positive birth experience.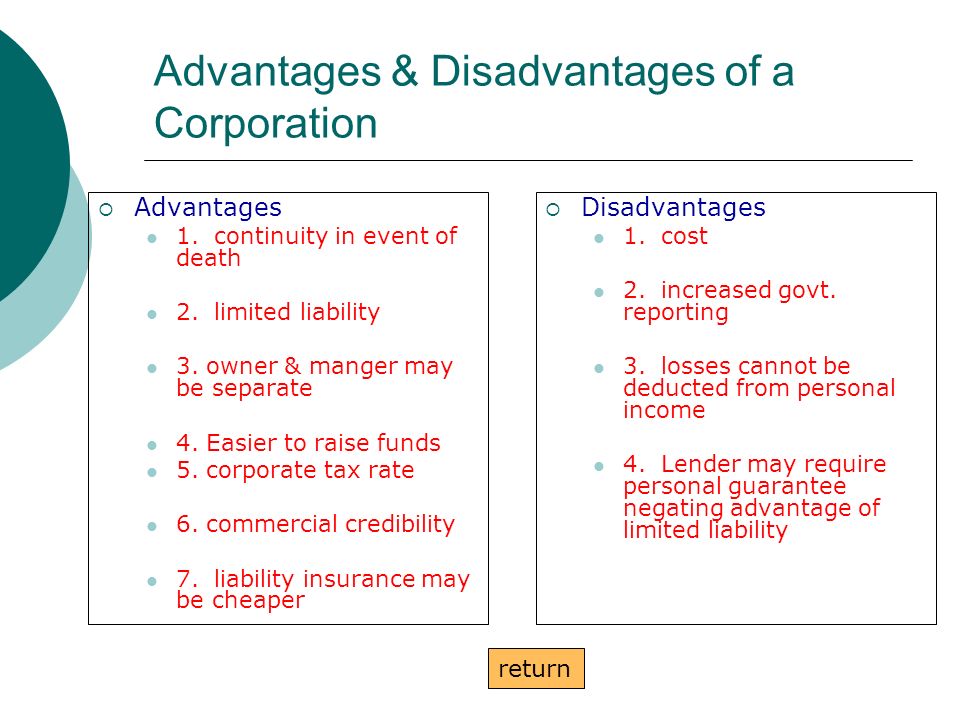
It can help you stay alert
An epidural can help you stay alert so that you can take an active part in the birthing experience. It can also spare you discomfort if forceps or a vacuum are needed to help get your baby out.
If you need to deliver by C-section, an epidural allows you to stay awake during the procedure and provides pain relief during your recovery.
It may help reduce postpartum depression
A 2014 study found some evidence that epidural use may decrease risk for postpartum depression (PPD) in some women. However, results from more recent research have not found evidence to support the claims that epidural use decreases risk for PPD.
Results from another study found a possible connection between decreased incidence of PPD in women who intended to and used an epidural during labor, suggesting that having a pain management plan in place and being able to stick to that plan may help reduce risk for PPD.
It’s important to discuss labor pain management with your doctor or midwife throughout your pregnancy. They can help you come up with a plan that works for you and your goals. They can also help you come up with alternatives in case your original plans need to change during labor.
They can help you come up with a plan that works for you and your goals. They can also help you come up with alternatives in case your original plans need to change during labor.
You can get an epidural anytime during labor
Even if it’s not part of your intended birth plan, it’s good to know that you can get an epidural anytime during labor if the need arises.
They’re effective for longer surgical procedures
An epidural can provide continuous pain relief during long surgical procedures, such as a C-section delivery, or while recovering from certain procedures.
If you need an epidural for a surgical procedure, you will likely get a larger dose of medication and may temporarily lose all feeling below the waist. Feeling will return once the medication is reduced or stopped.
Here we look at some of the cons of having an epidural.
It can cause low blood pressure
Epidurals can cause a sudden drop in your blood pressure. Your blood pressure is monitored throughout your labor and delivery to ensure adequate blood flow to your baby and throughout your body. If your blood pressure drops, you may need oxygen, fluids, and medication.
If your blood pressure drops, you may need oxygen, fluids, and medication.
You may have some side effects
Some women experience side effects, including shivering, fever, or itchiness. After the removal of the epidural, you may feel nauseous or dizzy, and have back pain and soreness where the needle was inserted.
About around 1 percent of women will experience a severe headache. This is a rare side effect that’s caused by a leakage of spinal fluid. If the headache persists, a blood patch is performed, which involves injecting some of your blood into the epidural space to relieve the headache.
Though very rare, permanent nerve damage is possible if the spinal cord is damaged by the needle or catheter, or by bleeding or infection in the epidural area. Anesthesiologists undergo extensive training and the risk of permanent damage is very low.
It may make pushing more difficult
Some women find pushing more difficult with an epidural. This can increase your chance of needing interventions, such as forceps, medication, or a C-section.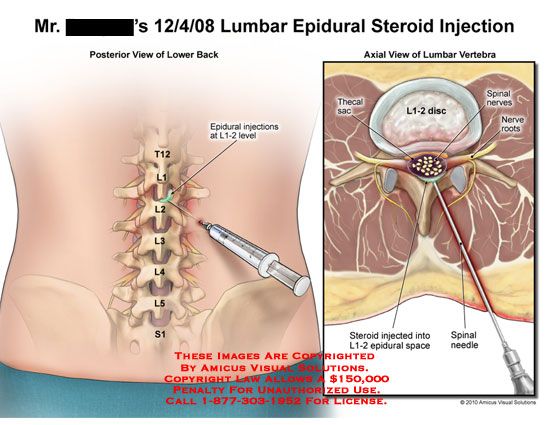
It may increase your risk for a perineal tear
Research shows that perineal tears are more common in women who have epidurals. Other factors that increase your risk for perineal tear include:
- baby with heavier birth weight
- episiotomy
- labor induction
Your lower half may be numb for a while after giving birth
You may experience some numbness in your lower half for a few hours after giving birth. Because of this, you may need to stay in bed until the numbness wears off.
You may have trouble urinating
Having an epidural also increases your chances of needing a urinary catheter to empty your bladder. This is only temporary. The urinary catheter can be removed once your numbness has resolved.
Risk of respiratory distress for your baby
Some evidence suggests that babies whose birth mothers have an epidural are more likely to develop respiratory distress immediately after birth. Though other studies have found no evidence of epidural usage increase risk for respiratory distress in babies.
Talk to your doctor about any concerns you have about the safety of epidural for your baby before you begin labor.
More than 70 percent of women in labor use an epidural, but that doesn’t mean it’s the right choice for everyone. Like with any medical procedures, there are pros and cons to consider.
There are a number of factors that can determine what type of birth might be best for you. Every family is different and it’s impossible to predict how you’ll feel when the time comes. It’s important to keep an open mind and focus on making the experience a positive one, even if it doesn’t go how you originally planned.
Several factors can impact the level of pain you experience during delivery and childbirth. These factors may determine what, if any, medication is recommended:
- physical and mental health
- pain tolerance
- size of the your pelvis
- size of the baby
- the baby’s position
- intensity of contractions
The type of birth that is “better” is not about a specific method. Rather, you’ll want to choose the best method based on your situation and individual needs.
Rather, you’ll want to choose the best method based on your situation and individual needs.
It may be a good idea to come up with two birth plans. One plan can be your optimal plan. A second can serve as your fallback plan in case things don’t go as expected. That can help you feel less caught off guard if plans need to change mid-labor
Epidurals aren’t the only pain management option available during labor. Work with your doctor or midwife to determine which options may be best for you.
Opioids
Also called narcotics, these pain medications are given by injection or intravenously (through an IV). They don’t provide as much pain relief as an epidural, but can make the pain bearable without causing numbness.
Opioids can cause drowsiness, nausea and vomiting, and itching.
Though generally safe, opioids cannot be given right before delivery because they may slow the baby’s breathing and heart rate.
Pudendal block
This is a numbing medicine that is injected into the vagina and the pudendal nerve late in the labor, just before the baby’s head comes out.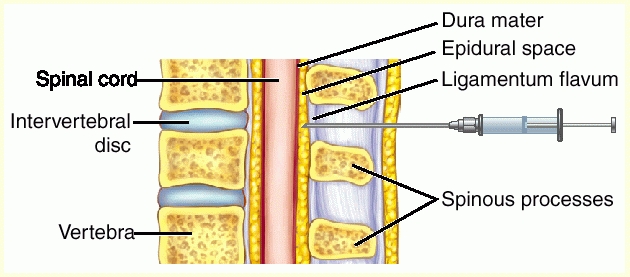 It provides some pain relief while allowing you to remain awake and push. There are no known risks to mother or baby.
It provides some pain relief while allowing you to remain awake and push. There are no known risks to mother or baby.
Nitrous oxide
This odorless gas is also commonly known as “laughing gas.” It’s an inhaled analgesic that is administered through a handheld face mask and takes effect within one minute.
Nitrous oxide can be used continuously or as needed during labor. It doesn’t completely eliminate pain and getting relief requires inhaling it approximately 30 seconds before a contraction. Side effects may include:
- dizziness
- drowsiness
- nausea
- vomiting
Natural remedies
There are natural remedies that you can use on their own or in combination with medicine to help ease your labor pain, such as:
- applying heat or cold to the lower back
- massage
- taking warm baths or showers
- finding comfortable positions, such as crouching, standing, or walking
- using a labor ball
Other options for procedures not related to pregnancy
If you’re having a surgical procedure on the lower part of your body, there are alternatives to an epidural. Your doctor can help you determine the best choice based on the procedure you’re having and your needs during recovery.
Your doctor can help you determine the best choice based on the procedure you’re having and your needs during recovery.
These may include:
- a spinal anesthetic, which is a single injection of medication into your spine
- general anesthetic
- nerve block
- opioids
- heat and cold therapy
Epidurals are generally considered safe, but the decision to have one is a personal one. Ultimately, you’ll need to weigh the pros and cons, and decide what’s best for you and your family.
It’s also a good idea to talk to your doctor about the benefits and risks of epidurals, and other pain management options.
Developing a plan can help you feel more prepared for labor. But remember, even the best laid plans can change in the moment. That’s why it’s also a good idea to have a backup plan so that you can be prepared with an alternative birth plan that you’re still comfortable with.
Epidural anesthesia - pros, cons, reviews
Medical anesthesia of childbirth is becoming more and more popular: more and more expectant mothers and their doctors prefer epidural (epidural) anesthesia. According to a number of experts, this is the most modern and safe method for mother and child, which is also widely used due to its high efficiency and convenience. Gynecologists very often refer to multiple positive reviews about epidural anesthesia, and a woman, faced with the well-known fact of labor pain, agrees to avoid pain.
According to a number of experts, this is the most modern and safe method for mother and child, which is also widely used due to its high efficiency and convenience. Gynecologists very often refer to multiple positive reviews about epidural anesthesia, and a woman, faced with the well-known fact of labor pain, agrees to avoid pain.
Indeed, epidurals often receive rave reviews. But in order to make a decision on the use or refusal of pain relief, the expectant mother must have the full range of information about the impact of this type of anesthesia on the birth process, as well as aspects of the psychological interaction between the mother and her baby during childbirth.
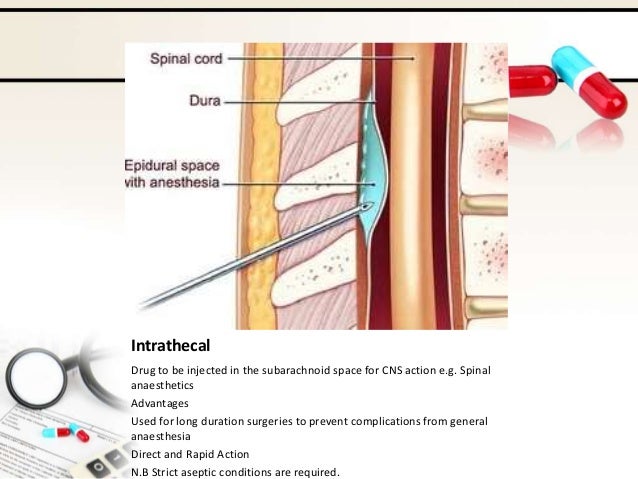
The name of the method is due to the method of administration of the anesthetic drug: the anesthetic is injected directly into the space surrounding the dura mater of the spinal cord (from Latin peri - "around", epi - "above", dura mater - "dura mater"). In essence, the anesthetic blocks the impulses that the lower body sends to the pain centers of the brain (analgesia) or generally all signals, including motor impulses (anesthesia).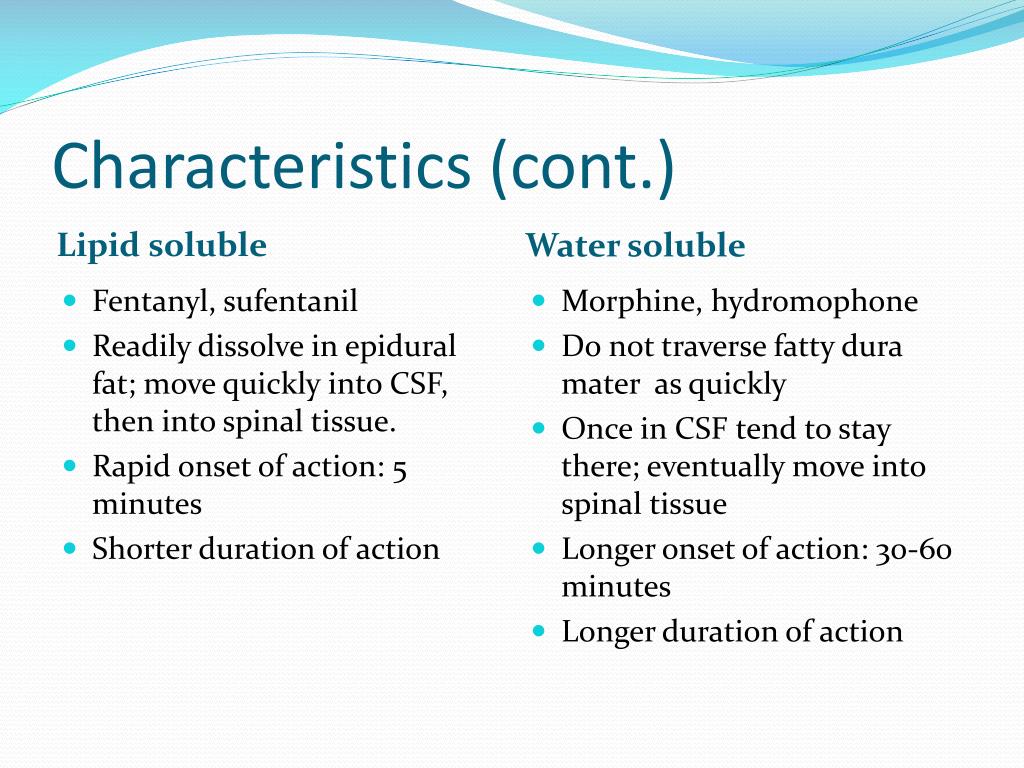 To perform epidural (epidural) anesthesia, the anesthesiologist performs a puncture at a height of 3 or 4 vertebrae of the lumbar spine, introducing a special flexible catheter through a needle with a stylet. It is through the catheter that every half an hour an anesthetic drug will be supplied to the woman's body. After anesthesia, the lower part of the body of the woman in labor remains insensitive and motionless; after analgesia, the woman does not feel pain, but retains the ability to move (sit, stand, roll over).
To perform epidural (epidural) anesthesia, the anesthesiologist performs a puncture at a height of 3 or 4 vertebrae of the lumbar spine, introducing a special flexible catheter through a needle with a stylet. It is through the catheter that every half an hour an anesthetic drug will be supplied to the woman's body. After anesthesia, the lower part of the body of the woman in labor remains insensitive and motionless; after analgesia, the woman does not feel pain, but retains the ability to move (sit, stand, roll over).
The advantages of epidural anesthesia include the following features of this method of anesthesia:
- the woman remains fully conscious, does not feel labor pain, her kidneys and uterus are well supplied with blood;
- the anesthetic does not act directly on the fetus without entering the child's blood;
- the influence of the anesthetic does not harm the woman more often.
It would seem that a panacea has been found.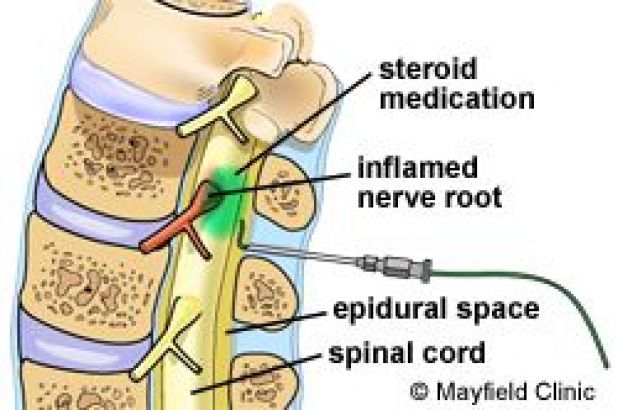 Many women are so afraid of labor pain that the temptation to agree to pain relief after numerous positive reviews about epidural anesthesia is very high. This is practically a guarantee of easy and painless childbirth!
Many women are so afraid of labor pain that the temptation to agree to pain relief after numerous positive reviews about epidural anesthesia is very high. This is practically a guarantee of easy and painless childbirth!
However, despite all the obvious advantages of epidural anesthesia, we must not forget about the impact that any anesthesia has on the most important area of the birth process - the interaction between mother and baby. Epidural anesthesia can be a real salvation if there are violations of labor activity, which is accompanied by severe pain (not at all characteristic of normal physiological childbirth). But at the same time, this pain relief can become an obstacle to deep interaction between mother and child, if used in advance, only because of the fear of possible pain.
The perception of pain is purely individual and depends primarily on the psychological mood of the woman and her ability to relax. Indeed, the real cause of labor pain is muscle tension that interferes with the normal physiological changes that occur in a woman's body during childbirth. If a woman feels fear of childbirth, anxiety and anxiety, muscle tension increases. A vicious circle appears: fear causes muscle tension, tension causes pain, pain causes fear. To get rid of pain, you need to learn how to relax. Actually, epidural anesthesia solves the same problem - it relaxes the muscles. But this is far from the only and not the most harmless way to get rid of stress. Relaxation of your body is achieved through a relaxed state of your mind. That is why during childbirth, a sense of calm, self-confidence, trust in others, and a comfortable environment are very important for a woman.
If a woman feels fear of childbirth, anxiety and anxiety, muscle tension increases. A vicious circle appears: fear causes muscle tension, tension causes pain, pain causes fear. To get rid of pain, you need to learn how to relax. Actually, epidural anesthesia solves the same problem - it relaxes the muscles. But this is far from the only and not the most harmless way to get rid of stress. Relaxation of your body is achieved through a relaxed state of your mind. That is why during childbirth, a sense of calm, self-confidence, trust in others, and a comfortable environment are very important for a woman.
Nature has taken care to supply the woman with the painkillers she needs for childbirth. Among the hormones that regulate labor activity, a woman's body secretes a large amount of hormones of joy and pleasure - endorphins, which can reduce unpleasant physical sensations and create a special psycho-emotional state, somewhat reminiscent of a state of mild intoxication. These hormones have a beneficial effect on the course of childbirth, help a woman relax, relieve pain, and give a feeling of emotional uplift. However, the mechanism for the production of these hormones is very fragile, it directly depends on the general emotional state of the woman during childbirth. Feelings of anxiety, anxiety, fear can suppress the production of endorphins, and then the strength of this natural pain-relieving mechanism is significantly reduced.
However, the mechanism for the production of these hormones is very fragile, it directly depends on the general emotional state of the woman during childbirth. Feelings of anxiety, anxiety, fear can suppress the production of endorphins, and then the strength of this natural pain-relieving mechanism is significantly reduced.
When a woman is not internally ready for childbirth, does not know how to control her body, does not know how to relax, it seems to her that the easiest thing is to just take it and switch off from unpleasant sensations. But at the same time, she disconnects from her child, who needs empathy and support at this moment. Now his birth will not bring her any inconvenience. What will the child feel? He will most likely be very lonely. The world in which he lived for nine months, so tender and loving, understanding and sensitive to any movement, this world in an instant turned into a cold and indifferent, not feeling and not understanding the signals of the child. Mom seems to have stopped "hearing" her baby.
Mom seems to have stopped "hearing" her baby.
But birth is not only and not so much a physiological process, it is a joint spiritual experience of two people – mother and baby. Not only the successful birth of a child depends on how well they understand each other, but also his further relationship with his mother, loved ones, and the whole world. A woman whose body is devoid of sensitivity ceases to feel the child along with pain, cannot help him in the birth, does not empathize with his feelings. The greatest feeling of maternal love is amazing because only a mother is able to subtly feel her baby, as if he is part of her. If voluntarily or involuntarily violate this relationship, childbirth becomes unnatural. While easing the physical inconveniences of childbirth, think about possible emotional experiences, regret about the missed opportunity to give birth to your child naturally.
The use of anesthesia turns a woman from a mother into a patient, and the miracle of the birth of a person into an act of extracting a fetus from the body of a woman in labor. Even when the child is born, the woman still has some time to recover from anesthesia. Natural childbirth allows a woman to fully communicate with the baby from the first seconds of his birth. This moment is very important for a person, this is the first experience of his communication with the world. What awaits the little man at the moment of birth? Warm, loving motherly hands or a set of medical manipulations performed by a doctor?
Even when the child is born, the woman still has some time to recover from anesthesia. Natural childbirth allows a woman to fully communicate with the baby from the first seconds of his birth. This moment is very important for a person, this is the first experience of his communication with the world. What awaits the little man at the moment of birth? Warm, loving motherly hands or a set of medical manipulations performed by a doctor?
Many women who have deprived themselves of the opportunity to feel how their child was born, very much regret this. Together with pain sensitivity, they lost the greatest joy of empathy, that indescribable feeling of delight from meeting their child, which happens only after natural childbirth. A woman whose birth was anesthetized often wonders why the baby does not evoke love feelings in her. Without experiencing the maximum stress of not only physical, but also mental strength, it is impossible to fully experience the happiness of meeting with the baby. This isolation from the child in childbirth interferes with their further deep emotional contact. Mom easily stops breastfeeding the child, easily entrusts him to grandmothers or nannies, does not feel his emotional needs. This happens when anesthesia has been applied for no serious reason.
This isolation from the child in childbirth interferes with their further deep emotional contact. Mom easily stops breastfeeding the child, easily entrusts him to grandmothers or nannies, does not feel his emotional needs. This happens when anesthesia has been applied for no serious reason.
If there are such reasons, and anesthesia is indispensable, do not forget how much depends on your attention to the child's experiences. Your warm thoughts about him, the ability to empathize, the desire to support your baby at such an important moment will help to overcome all the negative aspects of epidural anesthesia, and then nothing will prevent you from establishing a deep connection with your baby. It is unreasonable to reject modern scientific achievements, but it is even more unreasonable to reject ourselves. Do not forget that the most effective painkiller is love.
Give birth with pleasure!
D. Streltsova, S. Abramova
Epidural analgesia and anesthesia during childbirth
ArticlesPublication date:
Epidural analgesia is a regional pain relief method that relieves pain only in a specific area of the body.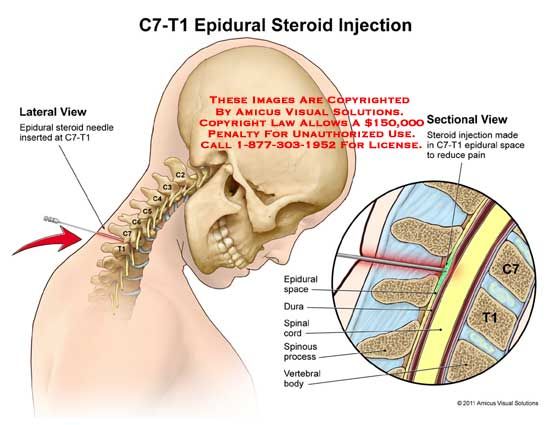 This procedure is performed by an anesthesiologist. The essence of the method is the blockade of the nerve roots of the spinal cord at the level of the lumbar region and the loss of sensitivity in the blocked area (the area of the uterus). To do this, a catheter is placed in the space next to between the lumbar vertebrae, into which an anesthetic medicine (local anesthetic) is injected. At the same time, the pain during contractions is significantly weakened or disappears. Childbirth is much more comfortable, and the woman in labor is resting.
This procedure is performed by an anesthesiologist. The essence of the method is the blockade of the nerve roots of the spinal cord at the level of the lumbar region and the loss of sensitivity in the blocked area (the area of the uterus). To do this, a catheter is placed in the space next to between the lumbar vertebrae, into which an anesthetic medicine (local anesthetic) is injected. At the same time, the pain during contractions is significantly weakened or disappears. Childbirth is much more comfortable, and the woman in labor is resting.
Pros and cons of epidural analgesia in childbirth
Pain relief in labor with epidural analgesia has a number of advantages over other methods :
- Participation of the patient in the birth act. The patient has the opportunity to interact with medical staff, control the course of childbirth, and after the birth of the baby, she can hug him and attach him to the breast, which makes the first meeting unforgettable.
- Epidural analgesia has no negative effect on the course of labor and on the condition of the child in childbirth.
- The method is controlled, the duration and depth of anesthesia can be adjusted
- Administering epidural analgesia in labor allows the patient to move
- During epidural analgesia, uterine contractions normalize, cervical dilatation occurs faster
- Rapid transition from labor pain relief to caesarean section pain relief. If an emergency caesarean delivery is necessary during childbirth, a highly concentrated local anesthetic is injected into the epidural catheter, complete anesthesia is achieved, and the operation can be started immediately
Epidural anesthesia also has some disadvantages:
- With an increase in the intensity of contractions and the need to increase the dosage of pain medication, a side effect is possible, expressed in a decrease in sensitivity and the ability to move the legs.
 This is temporary and will go away after a few hours of pain relief.
This is temporary and will go away after a few hours of pain relief. - Epidurals require the patient to be in a horizontal position in bed, therefore, vertical and tub births are excluded
- During anesthesia, sometimes the patient is unable to urinate on her own, which requires emptying the bladder with a catheter. After the anesthesia is over, it goes away.
- Chills can also be a side effect, which occurs due to a violation of thermoregulation in the area of anesthesia. As a rule, a comfortable temperature is maintained in the maternity box, which allows you to cope with this.
Contraindications for epidural anesthesia during childbirth
- Informed refusal of the patient
- Downward coagulation disorder
- Intolerance to local anesthetics.
- Purulent lesion of the skin at the puncture site
- Diseases of the cardiovascular system (rhythm disturbances, heart defects, the presence of artificial valves, pacemakers).
 In this situation, the possibility of epidural analgesia is assessed individually and agreed with the cardiac surgeon.
In this situation, the possibility of epidural analgesia is assessed individually and agreed with the cardiac surgeon. - Liver failure
- Demyelinating diseases of the nervous system and peripheral neuropathy
- Tattoo at the puncture site.
If there are contraindications to epidural analgesia, then there is always the possibility of alternative labor pain relief.
Consequences and complications after epidural anesthesia during childbirth
Any method may have complications that may be associated with the characteristics of the patient's body, violation of the technique of the procedure
- Due to involuntary movement of the patient, anatomical features (scoliosis, herniated discs) or inadvertent violation of the technique of the procedure, back pain, sensory disturbances due to trauma to the nerve roots, as well as headache
- Difficulty urinating may be longer (an individual feature of the patient's body, expressed in increased sensitivity to painkillers)
- Blood pressure may decrease if the mother drinks little fluid and is dehydrated.