Infant skin rash types
Baby Rash: Causes, Types, Treatments, Prevention
There are many types of rashes that affect various parts of a baby’s body.
These rashes are typically very treatable. While they may be uncomfortable, they aren’t cause for alarm. Rashes are rarely an emergency.
Sometimes, infant rashes can indicate a more serious illness. We’ll discuss different types of baby rashes, how to treat them, and when to call a doctor.
Babies have very new skin and developing immune systems. Their skin is sensitive and susceptible to many sources of irritation or infection. Causes of rashes in babies include:
- heat
- allergies
- friction
- dampness
- chemicals
- fragrances
- fabrics
Even their own feces can irritate a baby’s skin and cause a rash. Viral and bacterial infections can also cause rashes.
Depending on the cause of the rash, almost any part of your baby’s body can be affected:
- face
- neck
- trunk
- arms
- legs
- hands
- feet
- diaper area
- skin folds
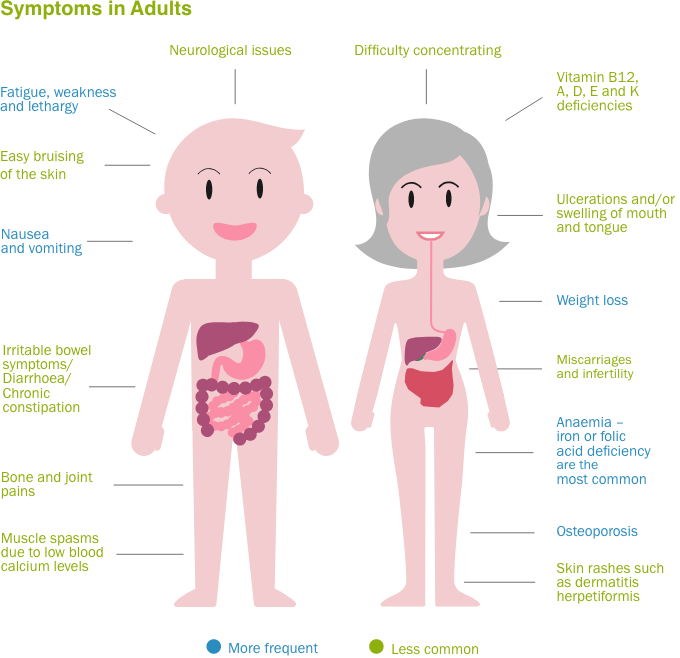
Some of the most common types of infant skin rashes include:
- baby acne, which usually appears on the face
- cradle cap
- diaper rash, which is caused by wetness or the acidity of a baby’s urine and feces
- drool rash, which happens when drool irritates the skin around the mouth or on the chest
- eczema, most commonly found on the face, behind the knees, and on the arms
- fifth disease, which is a “slapped cheek” rash that may be accompanied by fever, fatigue, and sore throat
- hand, foot, and mouth disease
- heat rash, usually found in areas covered by clothes, such as armpits, neck, chest, arms, torso, and legs and is caused by overheating
- hives
- impetigo
- infectious rashes, such as measles, chickenpox, scarlet fever, and roseola
- miliamolluscum contagiosum
- thrush
Seek medical advice for a feverBring your child to a doctor if they’re experiencing a rash with a fever.
![]()
Diaper rash treatment
Diaper rash is one of the most common baby rashes. A diaper holds warmth and moisture close to the skin, and urine and feces may be acidic and very irritating to the skin. The best remedies for diaper rash include:
- frequent diaper changes
- wiping with a soft, wet cloth instead of pre-packaged wipes that contain alcohol and chemicals
- using a barrier cream, typically containing zinc oxide, which shouldn’t be wiped off of the skin with each diaper change or it can cause more irritation
- decreasing acidic foods, such as citrus and tomatoes, in your baby’s diet
- washing your hands before and after diaper changes so the rash doesn’t become infected
Eczema treatment
Eczema is another very common childhood rash. If you have a family history of eczema or sensitive skin, your baby is likely to be more prone to eczema.
It may be caused by allergies or skin sensitivities to food, laundry detergent, types of fabric, or other irritants.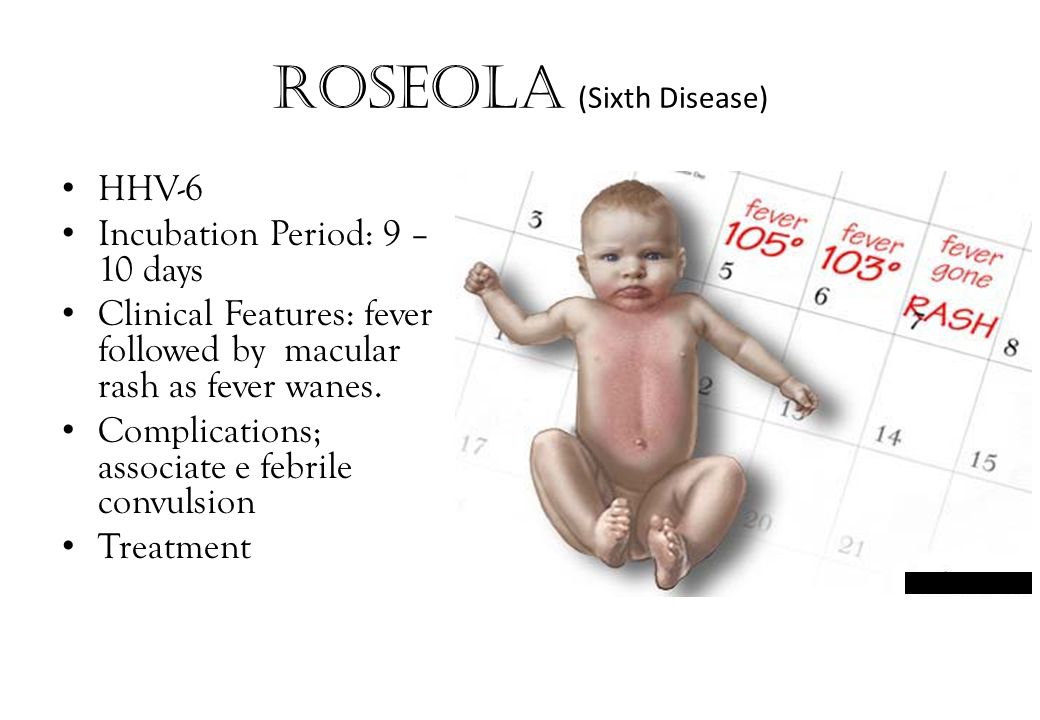 Helpful treatments for eczema include:
Helpful treatments for eczema include:
- keeping the area clean and dry
- over-the-counter creams and ointments
- oatmeal baths
- determining if there’s an allergy and eliminating the allergen
- working with a pediatric dermatologist to identify your baby’s triggers and how to best treat their eczema
Drool rash treatment
Drool rash and general facial rash is very common in babies. They’re developing salivary glands and teething, so it’s not uncommon for them to have drool on their face much of the time. Pacifier use, food particles, teeth growing in, and frequent face-wiping may also irritate the skin.
Drool rash typically resolves on its own in a matter of weeks, but there are some ways to help:
- pat — don’t scrub — your baby’s face to dry
- clean with warm water but avoid using soap on the face
- have your baby wear a drool bib so their shirt doesn’t become soaked
- be gentle when cleaning food off of the face
- avoid fragranced lotions on the face
- minimize pacifier use when possible
Some rashes, such as baby acne, go away by themselves in a matter of weeks or months. You shouldn’t use adult acne medication to treat baby acne.
You shouldn’t use adult acne medication to treat baby acne.
Cradle cap can be treated with topical oil, such as coconut oil, gentle scrubbing with a cradle cap brush, and washing your baby’s head.
Infectious rashes such as thrush, measles, chickenpox, roseola, and scarlet fever should be evaluated by a pediatrician for the best treatment. These rashes are typically accompanied by a fever and other symptoms. They may require antibiotics or antiviral medication, or they may resolve on their own.
Fever
If your baby develops a rash accompanied by a fever or following a fever, it’s best to call your pediatrician. The cause may be infectious and you should have your child evaluated by a doctor.
Learn more about signs of fevers and low temperatures in babies, and what to do.
Rash for a week
If your baby has a rash that persists for more than a week, doesn’t respond to home remedies, or is causing your baby pain or irritation, you should call your doctor.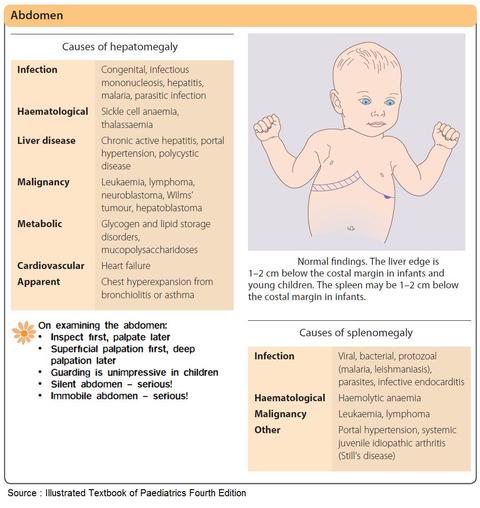
Rash spreads
If your baby develops widespread hives, especially around the mouth, or develops hives accompanied by coughing, vomiting, wheezing, or other respiratory symptoms you should go to the emergency room. This may be a sign of a very serious allergic reaction called anaphylaxis.
Emergency signs
A rash accompanied by a very high fever, a stiff neck, sensitivity to light, neurological changes, or uncontrollable shaking may be caused by meningitis and is considered a medical emergency.
While rashes in babies are very common, there are some steps you can take to help prevent a rash. Preventive steps that some people try include:
- frequent diaper changes
- keeping skin clean and dry
- using irritant-free laundry detergent or detergent specially formulated for babies
- dressing your baby in breathable fabrics, such as cotton
- dressing your baby appropriately for the weather to avoid overheating
- keeping track of any skin reactions to foods so you can avoid trigger foods
- keeping your child up-to-date on vaccinations
- not letting strangers or anyone with symptoms of illness kiss your baby
- using lotions, shampoos, and soaps specifically designed for a baby’s sensitive skin
It can be alarming when your baby develops a rash, especially if they seem to be sick, itchy, or uncomfortable.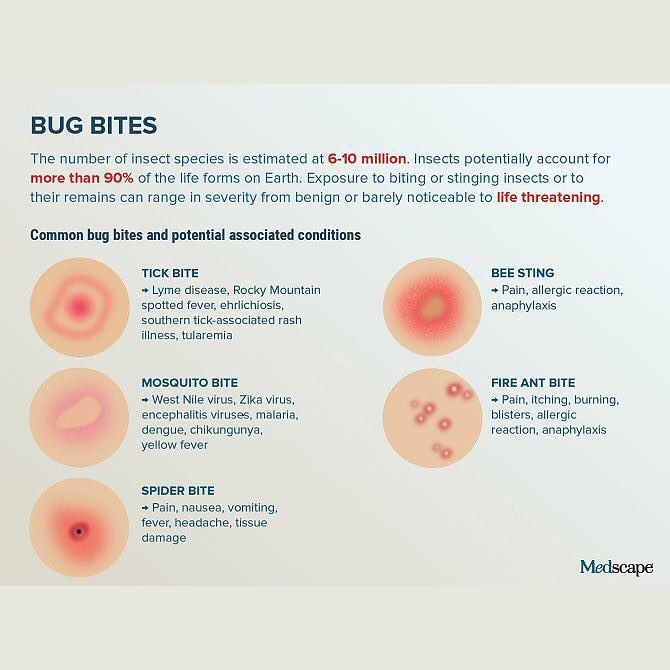 It can also be difficult to determine the cause of the rash.
It can also be difficult to determine the cause of the rash.
The good news is that rashes tend to be very treatable and aren’t usually serious. Many are even preventable and can be managed at home.
If you’re concerned about your child’s rash, or the rash is accompanied by a fever, call your pediatrician. They can help determine what is causing your baby’s rash and how to treat it.
Causes, Types, Treatment, and More
Heat rash is caused by blocked sweat ducts and is characterized by bumps that may be sore or itchy. Cooling the skin and applying lotions can help, but if it persists, speak to your doctor.
If your baby’s on the move or it’s just hot where you are, they’re bound to sweat. This means there’s a chance of them getting a heat rash, especially in warmer weather.
Kids and babies already tend to have higher body temperatures than adults. Add crawling, cruising, running, and climbing to that, and their temperatures climb even higher.
So, if you notice a skin rash when you unbundle your baby, it could be a heat rash, known as miliaria. Below are things you can do and look out for.
Below are things you can do and look out for.
Heat rash happens when sweat ducts in the skin are blocked and sweat gets trapped, creating fluid-filled bumps on the skin.
In most cases, the bumps show up where there’s friction, like where one body part rubs against another, or where tight-fitting clothes rub against the skin.
Did your baby wake up with a rash?
Heat rash can sometimes occur while children are sleeping. If pajamas are bulky, blankets are too heavy, or the fabric doesn’t breathe, these items could be trapping heat and perspiration.
Try these tips:
- Use a light blanket.
- Layer blankets.
- Opt for breathable cotton sleepwear.
If temperatures drop and your baby’s room becomes too cool for comfortable sleeping, it’s better to layer light blankets so you can remove one when the room warms back up.
There are multiple types of heat rash.
Miliaria crystallina
Miliaria crystallina is the mildest type of heat rash.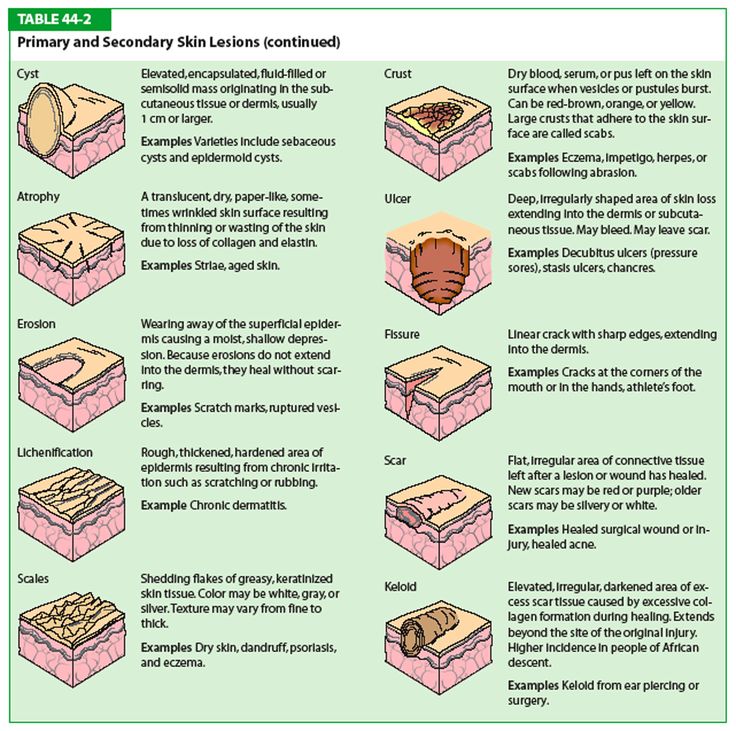 It affects the top layer of skin, which is called the epidermis.
It affects the top layer of skin, which is called the epidermis.
You might see small, clear, blister-like bumps on the surface of your baby’s skin. The bumps aren’t painful. They don’t usually itch, but the lesions can sometimes break open if they’re scratched.
If your baby has a rash, consider putting mittens on their hands to prevent scratching and open wounds.
Miliaria rubra
This red, bumpy rash affects the mid-epidermis, a deeper layer of the outer skin. Miliaria rubra is often called prickly heat because the bumps on the skin can be tender. They can sting or itch, too.
Miliaria rubra is the most common type of heat rash. The rash can cause discomfort and pain. Babies may be irritable while it’s healing.
Sometimes miliaria rubra can develop pustules. This form of the condition is called miliaria pustulosa.
Miliaria profunda
Miliaria profunda affects the deepest layer of skin (the dermis). It’s very rare among babies and toddlers. It occurs when sweat leaks out of the glands, forming fluid-filled pockets under the skin.
The bumps are skin-colored, not clear or red. They’re usually much bigger and tougher than the bumps from other types of heat rash. Although it may look milder, the effects can be more serious.
Symptoms of heat rash include:
- small bumps that may be clear, red, or skin-colored
- redness
- itchiness or a stinging feeling, in some cases
The most commonly affected zones on children’s bodies are:
- neck folds
- elbow and knee creases
- armpits
- inner thighs
Most of the time, heat rash starts clearing up on its own as soon as you cool off your baby. There are several at-home treatments to start healing the rash:
Cool the skin
You can cool the skin by removing extra layers of clothing or by moving to a cooled indoor space. If your baby’s been outside in heat and humidity, remove damp clothing and turn on a fan to dry their skin.
Apply water
- For small rash patches. If the affected area is relatively small — just a patch on the back of the neck or in the creases of the elbows — gently dab a cool, wet cloth on the rash to relieve tenderness and bring down the skin temperature.
- For larger rash areas. You can also give your baby a cool bath for at least 10 minutes, but don’t use soap — it could further irritate the skin. Afterward, let their skin air dry. Supervise your baby at all times during the bath.
Try a steroid cream
It’s important to keep kids from scratching if the rash is itchy. Broken blisters can lead to skin infection.
If it seems that the rash is bothersome to your baby, you can smooth some over-the-counter (OTC) 1 percent hydrocortisone cream onto the bumpy area.
Since steroids can have side effects, discuss their use with your child’s doctor beforehand.
Avoid hydrocortisone ointments that contain petroleum or mineral oil. They can block pores and keep sweat from naturally evaporating.
Use calamine lotion or anhydrous lanolin
If your child has a more severe type of heat rash, calamine lotion can help stop any itching.
Anhydrous lanolin — the kind found in nipple treatments for people who breastfeed — can help keep sweat ducts clear and open.
When to take your baby to a doctor
Heat rash usually clears up on its own within 1 week. If your baby’s skin hasn’t cleared up by then, or if the rash gets worse or looks infected, it may be time to talk with a pediatrician.
As with any rash, if your child develops a fever when the rash appears, it’s also a good idea to check with a doctor. They could prescribe a different steroid cream or advise you on using antihistamines to treat the problem.
Babies are at an increased risk of heat rash due to their higher body temperatures and undeveloped sweat ducts.
Other risk factors for heat rash, in babies or in older children and adults, include:
- sweating
- living in a hot, humid, or tropical climate
- having a fever
- wearing clothing that sticks to the skin
There are multiple steps you can take to help your baby avoid heat rash.
Pause
When you’re at the park or on the playground, check to be sure your child isn’t getting overheated during playtime.
If you notice damp clothing or flushed skin, remove a layer of clothing or move to a shady or air-conditioned space for a while.
Keep them hydrated
Whether you’re playing in cold or warm temperatures, make sure to take frequent breaks for milk or water. When your baby’s hydrated, body temperatures are more likely to stay at healthy levels.
Dress them in layers
If you’re headed out to play in cold weather, dress your baby in clothing made of breathable, moisture-wicking fabric that allows sweat to evaporate from the surface of the skin.
Be cautious about adding too many layers. When kids romp vigorously, layers can trap body heat and sweat. The best practice is to dress your child about as warmly as you’d be in the same temperatures.
Look for proper sleepwear
The Consumer Product Safety Commission recommends that a child’s pajamas (from 9 months to size 14) fit close to the skin and not too loosely.
The American Academy of Pediatrics recommends the use of flame-retardant sleepwear and clothing due to the risk of serious injury from burns.
Keep these recommendations in mind when purchasing sleepwear.
For example, cotton is one natural fiber that allows your child’s body to release heat and sweat. Some cotton items may be pretreated with a special chemical that also makes them flame retardant.
Re-rinse laundry
Detergent or residue from laundering may stay in fabrics and cause skin irritation or contribute to heat rashes. Adjusting your laundry routine a little might help reduce how often heat rashes happen.
Try adding an additional rinse cycle or adjusting your detergent levels. Learn more about laundry detergent rashes.
Heat rash is a skin condition that comes from blocked sweat ducts. The bumps could be clear, red, or skin-colored, depending on how severe the rash is. The bumps might be sore or itchy.
Most of the time, the rash will go away on its own as soon as you cool off your baby’s skin. You can also treat it with cool water, hydrocortisone cream, or calamine lotion.
If the rash doesn’t clear up in a few days, talk with a doctor to be sure your baby’s skin hasn’t become infected. The doctor may prescribe other creams or antihistamines to help with recovery.
The doctor may prescribe other creams or antihistamines to help with recovery.
Rashes in infants | Rassvet Clinic
Babies are generous with various rashes. According to the "good" tradition, most of them are considered allergic with all the consequences - a strict diet for a nursing mother, transfer to artificial feeding, prescription of therapeutic mixtures, etc. In fact, true allergic rashes in infants are not so common. Allergic diseases affecting the skin in infants include: atopic dermatitis, acute urticaria and angioedema. Acute urticaria is extremely rare in infants - this is an acute allergic reaction in the form of peculiar rashes like blisters (as with a nettle burn, hence the name), which suddenly appear on the skin and just as suddenly disappear without leaving any trace, usually do not exist on the skin for longer than a day and are accompanied by severe itching, which manifests itself in the general anxiety of the child. The most common causes are dietary proteins (such as cow's milk), viral infections, insect bites, and drugs (such as antibiotics). In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
In severe cases, it may be accompanied by swelling and redness of the soft tissues of the face, neck, larynx, arms, legs, genitals or abdominal cavity - Quincke's edema, which requires immediate medical attention.
Let's look at what is most often undeservedly called an allergy:
Toxic erythema newborns - a transient benign rash, the exact cause of the appearance is unknown (possibly due to skin irritation by environmental factors).
Appears at birth or in the first 24-48 hours of life. Localization - face, trunk, limbs, except for the palms and soles. Disappears on its own within 5-7 days, sometimes 3 weeks. Does not require treatment.
Neonatal acne (acne infancy, neonatal pustulosis) is caused by androgen stimulation of the baby's sebaceous glands.
Peak rash falls on the 3rd week of life. It is localized more often on the face, sometimes spreads to the scalp, less often to the collar zone. They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
They resolve spontaneously. The skin needs cleansing and moisturizing, in some cases, the application of
treatment creams may be required.
Sweating rash , which occurs in poorly "ventilated" areas as a result of blockage of the sweat glands. May occur at any age.
Localization - skin folds, buttocks and back surface of the body, sometimes the face (after sleep). Depending on the depth of the lesion, it happens - crystal prickly heat, prickly heat, deep prickly heat (superficial).
The duration of the rash is from several hours to several days.
Treatment - cool water baths, air baths, prevention of overheating. Lotions containing calamine and creams with corticosteroids and antibiotics may be used to treat some cases of red and deep prickly heat.
Seborrheic dermatitis is a skin disorder that develops in areas rich in sebum. The exact cause is unknown (a certain role is assigned to the skin saprophyte - the Malassezia fungus, which grows well and multiplies in the sebaceous secretion).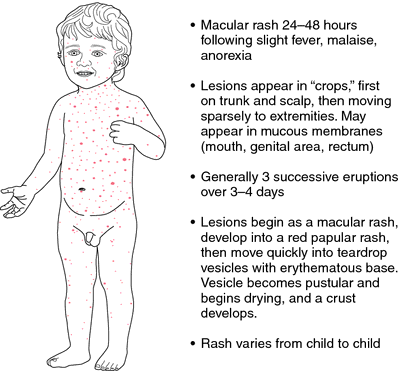
It can be foci or widespread, dermatitis with bran-like scales, which can form a crust (“bonnet”, gneiss) on the scalp.
Favorite localization - scalp, face, folds (!).
May begin at 1-2 weeks of age or later, resolve spontaneously within weeks or months.
Treatment consists of softening the crusts with oil or cream and then removing them, moisturizing the skin and, in some cases, applying antifungal and anti-inflammatory creams.
Simple contact dermatitis is a non-specific skin injury due to prolonged or repeated exposure to a variety of substances - saliva, fruit juices, foaming bath products, detergents (their residues on the walls of the bath), etc. In infants, saliva is often causes dermatitis in the area of contact with the nipple and in the folds of the neck.
Usually, removal of the damaging agent and short-term use of anti-inflammatory creams will quickly lead to recovery, but some children are so sensitive that it is almost impossible to identify the causative factor.
Diaper dermatitis (contact dermatitis prototype) is a skin lesion that occurs under the influence of physical (overheating), chemical, enzymatic (contact with sweat, urine and feces) and microbial factors. Localization - the area of the diaper or diaper fit.
Treatment is carried out using the abbreviation ABCDE (air, barrier, cleansing, diaper, education) - air, barrier, cleansing, diaper and parent education. Frequent diaper changes, washing the skin and drying it thoroughly help. Dermatitis is effectively prevented by the application to clean skin of products that completely cover it (Vaseline, zinc paste). In stubborn cases, medicated creams containing corticosteroids, antibiotics, or antifungals may be recommended.
And now a few words about AD:
Atopic dermatitis is a chronic allergic inflammation of the skin, genetically determined, associated with the loss of the skin barrier and, therefore, accompanied by dryness, itching and various rashes. In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
In a third (!) of cases, it is combined with food allergies (the most common "culprits" are cow's milk, chicken eggs, wheat, fish, soy, nuts).
Starts more often not earlier than 3 months of life.
The most common localization up to 2-3 years is the face (cheeks, forehead, chin), convex parts of the limbs (extensor surfaces) and trunk, never in babies in folds (!).
Exacerbations are provoked by various factors - stress, dry air, sweat, food (histamine liberators), infections, contact with tobacco smoke, animal hair, rough fabrics, detergent residues on clothes, etc.
Treated with careful skin care and using anti-inflammatory creams.
There are also:
Pseudo-allergic reactions are reactions that look similar to allergic reactions (for example, various rashes), but are not such, due to the non-immune mechanism of their development.
The reason is an increased content of histamine (tyramine, serotonin) in foods, or the ability of foods to increase the release of these substances in the body, or their increased absorption, due to the pathology of the gastrointestinal tract (fermentopathy, inflammation in the intestinal wall, etc. ). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
). ). Such products include chocolate, cocoa, strawberries, citrus fruits, honey, sauerkraut, marinades and spices, seafood, fish, caviar, pork, mushrooms, cheeses, nuts, smoked meats, preservatives, dyes and flavor enhancers.
Treatment includes dietary advice, skin care, and in some cases, antihistamines and anti-inflammatory creams.
Clinical manifestations of atopic dermatitis, simple contact dermatitis in highly sensitive children and the manifestation of pseudo-allergic reactions are very similar to each other, so the main task remains to create a "skin barrier" by constantly moisturizing the skin with the help of emollients, stopping exacerbation with anti-inflammatory creams and eliminating exacerbation-provoking factors .
And the last:
Skin infections - herpesvirus, staphylococcal pemphigus, candidiasis also occurs in infants, do not forget about them. It is worth contacting a doctor immediately if the child is lethargic, has a fever, refuses to breast or bottle, skin rashes are accompanied by pus or are covered with purulent crusts, there are blisters or a group of bubbles, erosion (violation of the integrity of the skin), severe swelling and redness of the skin.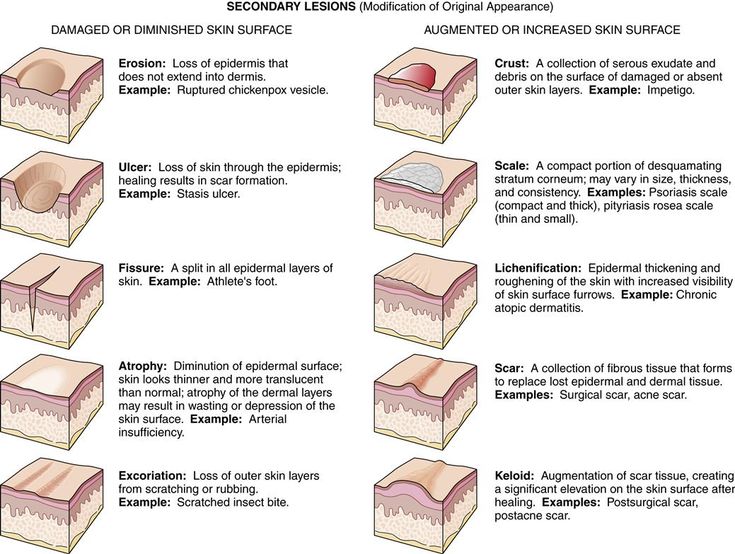
Author:
Eroshkina Maria Sergeevna
pediatrician
Rashes in newborns | clinic blog Nashe Vremya
The rash is localized on the face, head, in the oral and nasal cavities, as well as any part of the body. When combing, abrasions and erosion occur, a secondary infection may join.
A rash in a baby does not appear on its own, most often it is a sign of pathological processes in the body, although sometimes it is also a consequence of physiological conditions. Usually accompanied by additional symptoms - fever, sleep disturbance and appetite, joint and muscle pain, nausea, vomiting, weakness.
The rash may look different. First, primary elements are formed:
- pustules - small vesicles with purulent contents
- papules - raised firm nodules
- bullae blisters raised above the skin
- vesicles - small vesicles up to 5 mm containing exudate
- maculae - flat red spots
- plaques vesicles fused together
- petechiae - subcutaneous hemorrhages caused by capillary injury
- hemorrhages - subcutaneous hemorrhages caused by high permeability of vessel walls
After a while, secondary elements may form on the affected areas:
- hyperpigmentation or depigmentation skin discoloration
- desquamation - scaling of dying epidermis
- erosions - superficial lesions arising from the opening of a vesicle or abscess
- abrasions - violations of the integrity of the skin when scratching
- crusts - formations in place of burst pustules and vesicles
- lichenification thickening of the skin with enhancement of its pattern
Most rashes are harmless and go away either on their own or with minor interventions.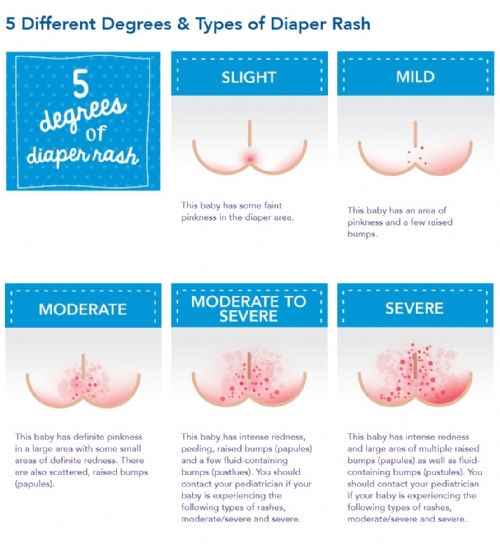 A baby is born with thin and sensitive skin, which tends to react sharply to any stimuli. Because of this, acne, peeling, redness appear. Despite the fact that usually skin manifestations are physiological and disappear on their own, some of them still require a mandatory examination and follow-up by a doctor.
A baby is born with thin and sensitive skin, which tends to react sharply to any stimuli. Because of this, acne, peeling, redness appear. Despite the fact that usually skin manifestations are physiological and disappear on their own, some of them still require a mandatory examination and follow-up by a doctor.
Reasons for the appearance of
The causes of skin changes and lesions are physiological conditions, various diseases, allergic reactions and physical irritants.
Physiological states
At birth, the baby is covered with primordial lubrication, which protects the skin from pathogenic microorganisms. In the hospital, it is not completely removed so that the skin adapts to the environment. But later, external conditions begin to act on it, causing various reactions that pass over time and are not dangerous for the baby.
A few minutes after childbirth, the color of the skin changes - it becomes bright pink or reddish. This is due to the fact that the air pressure is lower than the pressure of the aquatic environment in which the newborn has been for a long time, blood begins to flow to the skin, changing its color.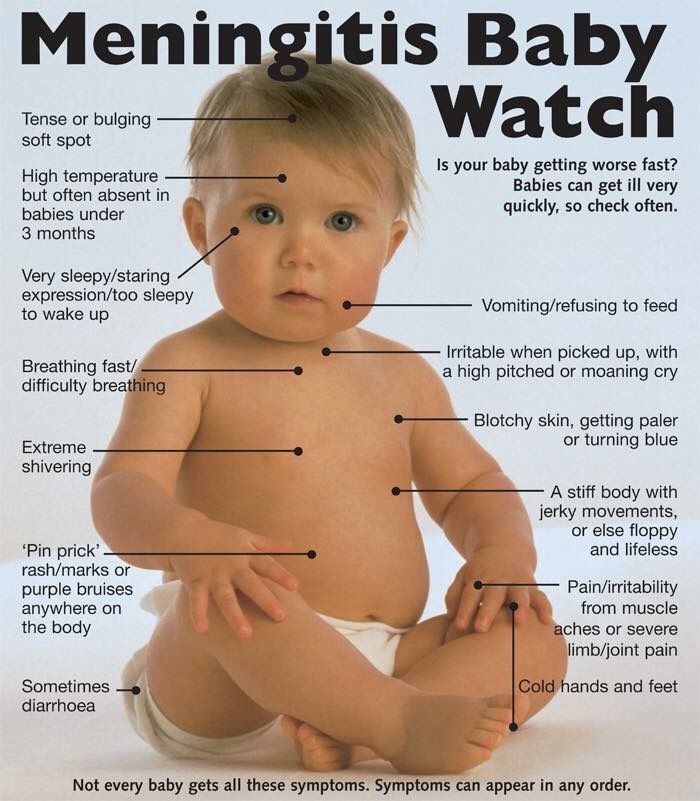 When the vessels return to normal, it will become the usual pink color. This takes about 2 weeks, premature babies a little more - up to 3 weeks.
When the vessels return to normal, it will become the usual pink color. This takes about 2 weeks, premature babies a little more - up to 3 weeks.
At first, the baby's skin may look like marble due to pink-purple spots. This is how the vessels react to cold, so marbling is usually noticeable when dressing or swaddling until the child is protected by clothes. If the marble spots are uniform and disappear when the baby is warmed, then there is no cause for concern. However, if something worries you, it is better to consult a doctor for advice so as not to miss heart or lung diseases, when marbling is a symptom of oxygen starvation.
On days 2-3, the baby's skin begins to peel off due to the transition to a dry environment after the womb. The degree of peeling is different, in post-term children it is more pronounced. It goes away in a few days. If cracks occur during peeling, you need to use special tools - emollients. However, if the skin bursts and is very desquamated, you need to see a doctor to exclude ichthyosis, hyperkeratosis and other pathologies.
Babies can develop seborrheic dermatitis, which forms in areas with strong sebum production. Appears as yellow scales on the head and behind the ears, less often in the axillary and inguinal folds. The second name for seborrheic dermatitis is "milk crusts". Usually pass without treatment, do not cause itching and do not cause discomfort, although it does not look aesthetically pleasing. To speed up the healing process, you can use baby oil and comb out the scales with a soft baby comb. Sometimes antifungal and anti-inflammatory creams may be needed.
For physiological reasons, various rashes can occur - toxic erythema, neonatal acne, milia. This is normal, because the delicate skin of the baby adapts to new living conditions. A rash in a baby appears due to an increased content of hormones, activation of the sebaceous glands and blockage of the follicles.
Physical influences (overheating, cold, friction)
Baby's skin is sensitive not only to the natural environment, but also to various mechanical influences and irritants. For example, overheating can cause prickly heat, contact with saliva can cause contact dermatitis, and a diaper can cause diaper dermatitis.
For example, overheating can cause prickly heat, contact with saliva can cause contact dermatitis, and a diaper can cause diaper dermatitis.
Infections
Infections that can cause rashes are viral, bacterial, or fungal. In this case, other symptoms are usually present - fever, intoxication, pain. See a doctor as soon as possible if the baby refuses to eat, the rash is accompanied by high fever, pus, severe swelling or redness of the skin. Hemorrhages in the form of red-blue blots, which do not disappear when pressed (test with a glass), require special attention.
Allergy
A rash in newborns can also appear upon contact with an allergen. Allergy can be food, contact, drug, cold, etc. Its symptoms are manifested by rashes, itching, urticaria, Quincke's edema, runny nose, cough, bronchospasm and intestinal disorders (diarrhea, constipation, flatulence, colic). Anaphylaxis is life-threatening and requires an immediate emergency call.
Also, a rash in newborns is caused by autoimmune diseases, vascular and other pathologies of the body, but this happens extremely rarely.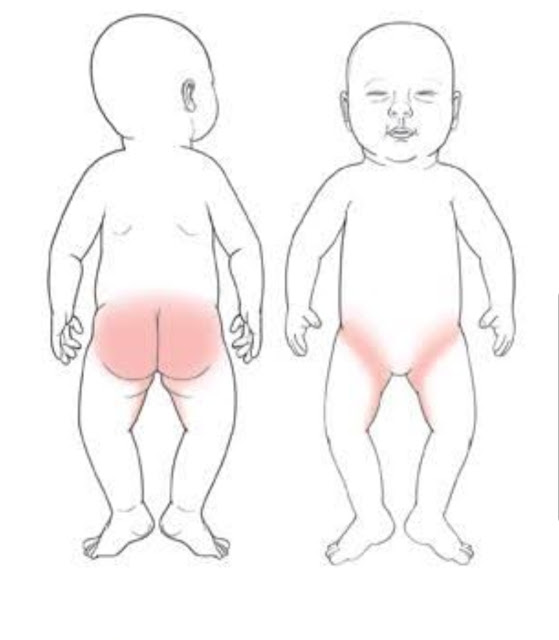
Types of rashes
Types of rash in newborns depend on its cause and are divided into physiological and pathological , and the latter - into infectious, allergic and mechanical .
Physiological
Neonatal acne (neonatal pustulosis)
In the 3rd week of life, 20% of newborns may develop teenage acne. They occur under the influence of hormones and look like pustules with a red border. The rash on the body of the baby is usually localized on the face, sometimes spreads to the scalp, less often to the collar zone. It is not dangerous and goes away on its own in 1-3 months.
With neonatal acne, the skin needs to be properly cleansed and moisturized, and may sometimes require the use of medicated creams. It is absolutely impossible to squeeze pimples and cauterize with alcohol-containing solutions. If the rash in the baby is abundant and leads to secondary infection, you should definitely see a doctor. Acne can drag on for a month or more, then it is considered infantile.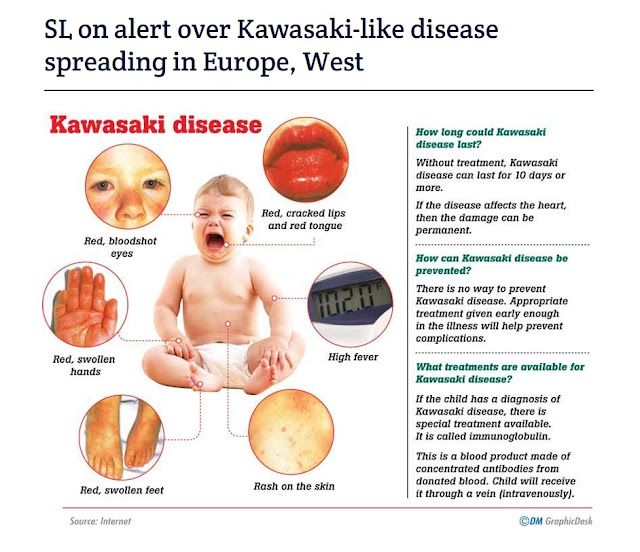 If more than six months do not pass, the risk of developing acne in adolescence increases.
If more than six months do not pass, the risk of developing acne in adolescence increases.
Milia
50% of babies develop small yellow or white nodules 1-2 mm in size, called milia or milia. These are cysts of the sebaceous glands that do not require removal. They spread to the face, head, chest and disappear in about a month.
Toxic erythema
This is a benign rash in a newborn child, resulting from the influence of the external environment on delicate skin. Develops by 2-3 days of life in 70% of babies in the form of small red rashes on the face, limbs, trunk. First, small dots appear, which later merge into spots with a 1-2 mm tubercle in the center. Toxic erythema is not dangerous and disappears within a week, sometimes 2-3 weeks. If something worries you, it is better to consult a doctor to rule out infections.
Pathological
Viral eruptions
Chickenpox
It starts with a few blisters and spreads throughout the body, including the scalp and mucous membranes. First, red spots appear, and then turn into bubbles. Then they burst and form crusts that cause itching and bother the baby. The rashes last 5-10 days.
First, red spots appear, and then turn into bubbles. Then they burst and form crusts that cause itching and bother the baby. The rashes last 5-10 days.
Measles
A highly contagious disease characterized by a small raspberry-red rash that first appears in the mouth, then spreads to the whole body. Affected skin becomes rough, later scaly patches remain for 1–2 weeks. Develops against the background of high temperature.
Rubella
Small pink-red spots appear on the head, and then all over the body, which last 2-4 days, and then disappear. Other symptoms are sore throat, nasal congestion, high fever.
Herpes
A rash in newborns occurs in the form of blisters on the lips and in the oral cavity, which disappears in 1-2 weeks.
Infectious mononucleosis
With infectious mononucleosis, densely spaced pink spots of about 10–15 mm appear. Other symptoms are high fever, swollen lymph nodes, sore throat.
Roseola
First, the temperature rises, after its normalization, small light pink dots appear. It goes away on its own and does not require treatment.
Coxsackie syndrome
Bubble rashes appear on the palms, feet and in the oral cavity. Additional symptoms are fever, vomiting.
Erythema infectiosum (fifth disease)
This is a common viral infection among newborns, which is manifested by a red rash on the cheeks and is accompanied by fever. It resolves on its own in a few days and does not require treatment.
Molluscum contagiosum
Appears as a cluster of white-pink bubbles with curdled contents inside. It is usually localized on the face, neck, eyelids, trunk and extremities.
Bacterial eruptions
Scarlet fever
With scarlet fever, numerous red dots appear in the folds of the skin, on the abdomen and on the sides of the body, accompanied by itching and flaking. A distinctive feature is that there are no rashes in the nasolabial triangle. Passes in 3-7 days. Additional symptoms are severe sore throat, crimson tongue.
Passes in 3-7 days. Additional symptoms are severe sore throat, crimson tongue.
Meningitis
Terrible disease, accompanied by a rash in the form of hemorrhages caused by rupture of capillaries, which do not go away and do not turn pale when pressed. Additional symptoms are headache, vomiting, pain in the extremities, stiff neck. The disease develops rapidly and can be deadly. If you suspect meningitis, you need to urgently call an ambulance.
Impetigo (streptoderma)
Accompanied by large blisters with purulent contents. Treatment is with topical or systemic antibiotics.
Fungal eruptions
Caused by contact with a fungal infection, they are divided into keratomycosis (damage to the stratum corneum of the epidermis) and dermatophytosis (damage to the skin, hair and nails). Usually appear as red rings on any part of the body. Transmitted from sick animals and people.
Rashes caused by parasites
Scabies
It manifests itself in the form of pairwise located points between the fingers, in the inguinal folds, on the knees and elbows.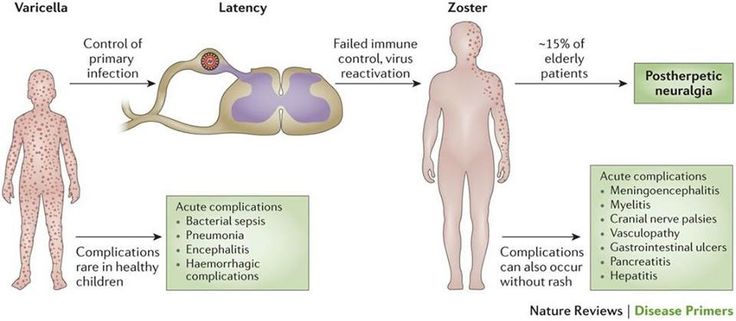 Accompanied by severe itching and disturb the baby. The reason is the scabies mite. Special creams are usually prescribed, and all family members should be treated.
Accompanied by severe itching and disturb the baby. The reason is the scabies mite. Special creams are usually prescribed, and all family members should be treated.
Allergic rashes
Urticaria
This is an acute allergic reaction in which raised red blisters quickly appear, similar to a nettle burn. It develops suddenly upon contact with an allergen, accompanied by severe itching. It has an acute and chronic character. Occurs with the use of food proteins, viral infections, insect bites and the use of drugs. In severe cases, it is accompanied by Quincke's edema, which requires an ambulance call.
Atopic dermatitis
This is a genetically determined disease associated with a defect in the skin barrier. It is important to note that allergy is not the cause of its occurrence, but rather a consequence. Only in 30% of cases, atopic dermatitis is combined with food allergies. The rash in the baby is localized on the face, buttocks, torso, extensor surfaces of the limbs. It is manifested by redness and peeling, accompanied by itching. Exacerbation is provoked by various triggers - stress, infections, sweat, histamine liberator products, tobacco smoke, animal hair.
It is manifested by redness and peeling, accompanied by itching. Exacerbation is provoked by various triggers - stress, infections, sweat, histamine liberator products, tobacco smoke, animal hair.
For treatment, special creams are used that restore the barrier function - emollients. They need to be used daily, plentifully lubricating the skin. In severe cases, hormonal ointments are prescribed.
Pseudoallergic
A pseudo-allergic reaction looks like an allergic reaction, but in fact it is not, since its development does not have an immune mechanism. The reasons are an increased content of histamine in foods, the ability of foods to stimulate its release from mast cells, increased absorption of histamine due to gastrointestinal pathologies. Histamine liberators include strawberries, chocolate, cocoa, citrus fruits, cheeses, preservatives, colorants and flavor enhancers. In a breastfed newborn, they arise due to the use of these products by the mother. Treatment consists of a tolerable dose, skin care, and sometimes antihistamines.
Mechanical eruptions
Prickly heat
Appears in the form of small red spots when overheated. It may also look like nodules or vesicles, appears in the folds of the skin, on the face, head, trunk, limbs. The occurrence of prickly heat contributes to an increase in body temperature, overheating due to too warm clothes, the use of things made of dense fabric. Lasts from several hours to several days, air baths speed up the healing process.
To prevent prickly heat, do not wrap the baby while walking, dress according to the principle - plus one layer of clothing relative to an adult. During wakefulness, periodically undress the baby for air baths. If prickly heat has already appeared, choose looser clothes, bathe without soap and protect from overheating.
Contact dermatitis
This is skin damage due to prolonged exposure to various irritants - saliva, fruit and vegetable juices, detergents. In newborns, saliva often causes dermatitis near the mouth and on the neck. Passes when the irritant is eliminated, anti-inflammatory creams are sometimes prescribed.
Passes when the irritant is eliminated, anti-inflammatory creams are sometimes prescribed.
Diaper dermatitis
Prototype contact dermatitis, only appears under a diaper. The cause is both overheating and contact with urine, sweat and feces. A rash in a baby occurs on the thighs, abdomen, buttocks in the form of red spots, bumps and peeling.
Treatment is carried out according to the abbreviation ABCDE (air, barrier, cleansing, diaper, education) - air, barrier, cleansing, diaper, education. With diaper dermatitis, you need to change diapers every 2-3 hours, arrange air baths when changing clothes, dry the skin thoroughly after bathing, and also lubricate with diaper cream. Sometimes local hormonal agents are used.
How to tell a rash from an allergy
An allergic reaction develops when an allergen enters the body. The immune system rushes to the defense, while blood vessels dilate, the skin turns red and inflamed, rashes appear, and edema may develop.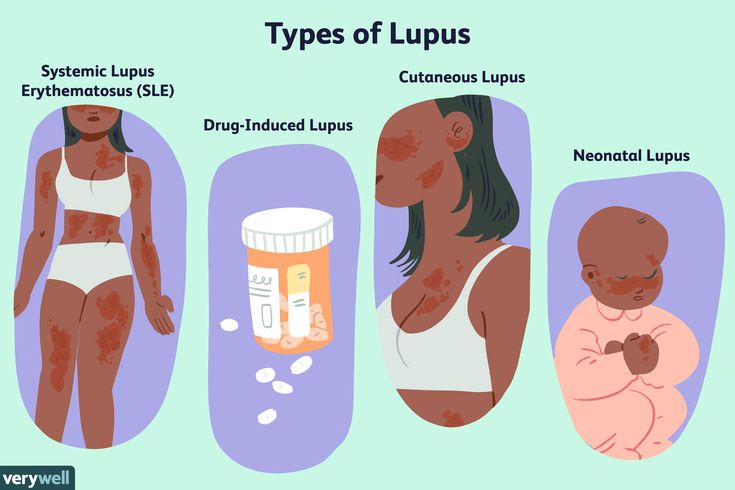 If there was no contact with the allergen, then the rash is most likely not allergic.
If there was no contact with the allergen, then the rash is most likely not allergic.
It is also worth distinguishing an allergic rash in an infant from an infectious one. With an allergy, it occurs suddenly, with an infection in stages - first it is localized in one place, and then it appears in another, it has clear boundaries of lesions. An infectious rash is contagious, so if one of the family members has it, then it is not an allergy. Viral or bacterial infections are often accompanied by fever, allergies are not. With an allergic rash, there is almost always severe itching, swelling, rhinitis, conjunctivitis may appear.
But still, it is very difficult to establish the cause on your own, so you should consult a doctor for the correct diagnosis and treatment. The doctor may prescribe tests to confirm a particular disease.
What to do if a child has a rash
A rash in a newborn baby can be of different etiologies, in some cases it goes away on its own, and in some it requires treatment. It is especially dangerous to miss formidable diseases such as meningitis or scarlet fever. Since eruptions often occur in greased molds, it is easy to make a mistake.
It is especially dangerous to miss formidable diseases such as meningitis or scarlet fever. Since eruptions often occur in greased molds, it is easy to make a mistake.
If simple methods like air baths, using breathable fabrics, frequent diaper changes, using emollients do not help, and even more so if the condition of the newborn worsens - the temperature rises, breathing is difficult, swelling has developed, the baby refuses to eat, urgently seek medical help .
When to see a doctor
In fact, it is better to show any rashes to the doctor. And do it in person, not by photo or video call. The doctor needs not only to examine the rash live, but also to feel, conduct certain tests, and also independently assess the condition of the child. If you find yourself in such a situation, you can contact our specialists.
Pediatricians of the Nashe Vremya clinic work in accordance with the principles of evidence-based medicine. They treat children with great care, carefully and carefully treat babies and are tactful with parents. Here they will not prescribe unnecessary tests, they will not make non-existent diagnoses, they will answer all questions, reassure and prescribe the correct treatment in case it is necessary.
Here they will not prescribe unnecessary tests, they will not make non-existent diagnoses, they will answer all questions, reassure and prescribe the correct treatment in case it is necessary.
If you want the baby to be examined at home, contact our field service. The pediatrician will arrive on the day of the call, after the examination he will give the necessary recommendations and will observe the baby until he is fully recovered.
We have specialists with extensive experience, as well as great love for their profession and little patients.
Prevention
To prevent rashes, the following measures should be taken:
- take care of the baby's hygiene and wash hands before touching the baby
- monitor the cleanliness of the room, humidify and ventilate in time
- use loose, breathable clothing for the newborn
- avoid overheating and hypothermia of the child
- change diapers more often and take air baths
- limit the amount of contact other people have with the baby
- buy quality toys and baby care products
- if possible, invite a doctor to the house, and not come to the clinic yourself
- avoid contact with allergens
- keep baby safe from insects
And the most important thing is to vaccinate both the child and others in a timely manner, especially if the child cannot be vaccinated due to age.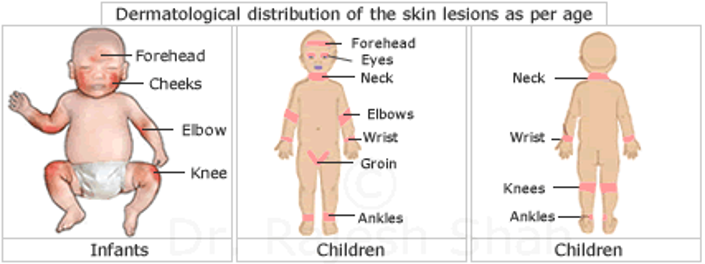 For example, adults should be vaccinated against influenza or covid.
For example, adults should be vaccinated against influenza or covid.
Methods of treatment
Treatment depends on the cause that caused the damage to the skin. First you need to see a doctor for an accurate diagnosis. Further, depending on the disease, antihistamines, hormonal ointments, emollients, antibiotics, antifungals can be prescribed.
And sometimes a rash in a newborn baby does not need to be treated at all, but just wait. But additional measures may be required - air baths, a comfortable indoor climate, breathable clothing, quality diapers.
Tips for parents
A rash in a baby is not an independent disease or its cause, it is always a symptom. Therefore, it is very important to determine what caused the rash in the baby - allergies, infections, insect bites or mechanical damage.
If the rash is accompanied by fever, the child is lethargic - urgently see a doctor, if hemorrhages appear - immediately call an ambulance! If the rash occurs against the background of the complete health of the child, see the pediatrician in a planned manner.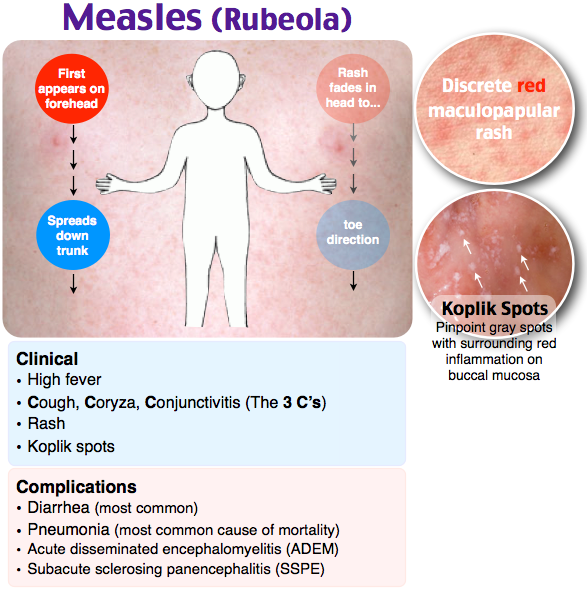
Terminals
The rash can manifest itself in the form of various elements - from small dots to large blisters and hemorrhages. Types of rash in newborns, as well as their causes, can be completely different:
- physiological - neonatal acne, milia, toxic erythema
- pathological - viral, bacterial, fungal, allergic
- mechanical - prickly heat, contact dermatitis, diaper dermatitis
Therefore, it is important to understand what exactly caused this or that rash in an infant.
Most often, a rash on the body of a baby goes away on its own and does not need treatment, for example, a hormonal rash in a newborn. However, you need to be careful not to miss a serious illness.
It is difficult for parents to figure out the reasons themselves, so it is better to entrust this to a doctor. If the rash is not dangerous, calmly wait until it passes, and if it is the cause of some kind of disease, establish it in time and start treatment.
Sources
1. Kudryavtseva A.V., Atopic dermatitis and food allergy: features of patient management in Russia and other countries (Europe, USA and Japan), School of atopic dermatitis as the basis for successful treatment of children, 2018.
2. Kudryavtseva A.V., Urticaria in children: pathogenetic mechanisms and possibilities of modern therapy, 2017.
3. Revyakina V.A., Urticaria in pediatric practice, 2007.
4. Clinical guidelines: Atopic dermatitis, 2020.
5. Pozdnyakova O.N., Reshetnikova T.B., Bychkov S.G., The structure of the incidence of dermatoses in newborns and infants with a burdened somatic history, 2019.
6. Bokova T.A., Diaper (diaper) dermatitis in a newborn: modern approaches to prevention and treatment, 2019.
7. Gorlanov I.A., Leina L.M., Milyavskaya I.R., Skin of newborns: differential diagnosis of pathological conditions, features of care, 2018.
8. Diagnosis and treatment of seborrheic dermatitis, Gary W Clark et al.