What to take for acid reflux in pregnancy
Pregnancy Heartburn? 7 Ways to Get Relief
Keywords
Kathryn Walker, MD
Women and Newborn
Learn more about women and newborn services we offer.
Expectant mothers everywhere are aching to know one thing: “How can I get some relief from this awful pregnancy heartburn?”
To help ease your pain, here are some answers to your “burning” questions. (Pardon the pun.)
When you’re growing a human being, you don’t have time for that yucky acid reflux. But your usual go-to methods for treating it may not be safe for your unborn baby. (Remember Pepto Bismol? That’s on the No Fly List for moms-to-be, according to FDA recommendations.)
Instead, here are some of the safest and best ways to get rid of heartburn when you’re pregnant:
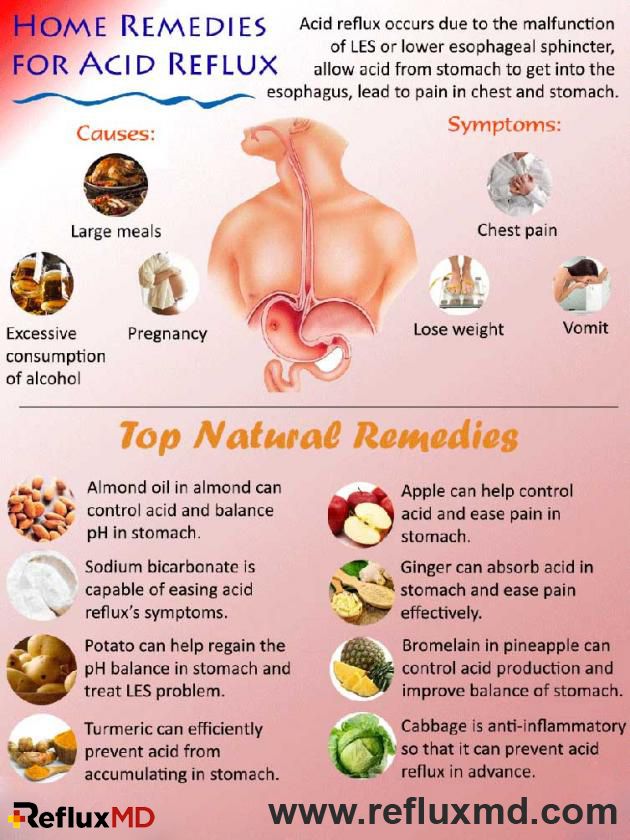
- Dip into some yogurt. Its probiotics and soothing texture make yogurt a great option for extinguishing heartburn – or at least dousing the flames a little.
- Drink milk with honey. According to the American Pregnancy Association, a tablespoon of honey mixed in a glass of warm milk may be just what you need to neutralize heartburn-causing acid.
- Snack on almonds. Munching on a handful of almonds may provide heartburn relief since these nuts have a lower acidity level than others.
- Eat pineapple or papaya.
 For some women, the digestive enzymes in pineapple and papaya have helped ease symptoms. Eating these fruits after your meals can aid digestion and reduce your chances of heartburn.
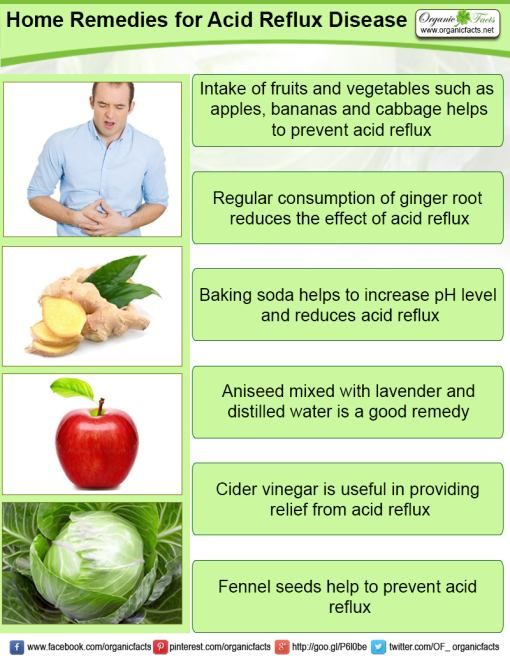
For some women, the digestive enzymes in pineapple and papaya have helped ease symptoms. Eating these fruits after your meals can aid digestion and reduce your chances of heartburn. - Try a little ginger. You probably knew ginger was a good remedy for an upset stomach. Well, that makes it a helpful candidate for fighting off heartburn, too. Among ginger’s many benefits, it can reduce inflammation and prevent stomach acid from traveling up the esophagus.
- Chew sugar-free gum. Another effective method for taming the burn is to chew some sugar-free gum. One study found that chewing sugar-free gum for 30 minutes after a meal can reduce acid reflux.
- Take (doctor-approved) medication. When all else fails, certain medications are considered safe to use for pregnancy heartburn relief. Just make sure you speak to your doctor or OB-GYN first. If your heartburn is severe, they may prescribe special medication to help control it.
While not every tip mentioned above may work to ease your symptoms, you’ve got nine months to try them all and figure out what works.
It’s important to be extremely careful about the medications you take when pregnant.
For heartburn relief, over-the-counter antacids (such as Tums, Mylanta, Rolaids, and Maalox) are all considered safe medications to use during pregnancy.
As always, consult with your provider about any medications you’re taking – even if they’re considered safe. (This is especially true for high-risk pregnancies.)
If you experience any unusual symptoms while taking an over-the-counter medication, call your doctor immediately.
They say prevention is the best medicine, so knowing common heartburn triggers can help you keep the acid at bay.
Of course, pregnancy itself is a major trigger for heartburn. As your growing uterus puts pressure on your stomach, this pushes stomach acid up your throat.
Those lovely hormones are no help either.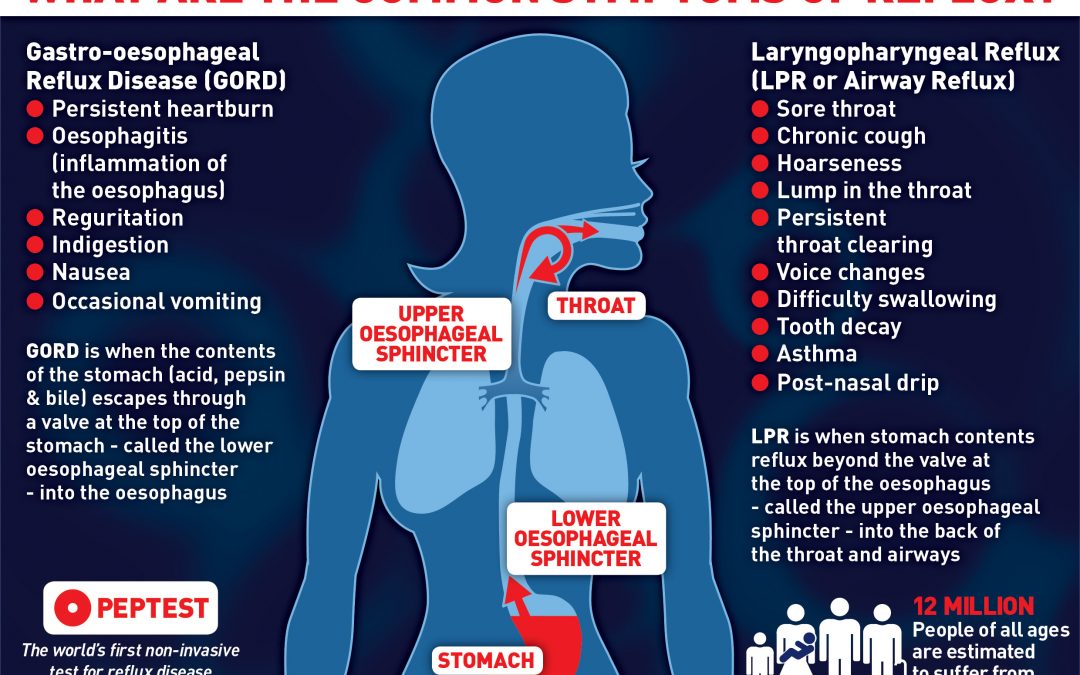 They tend to relax the valve between your stomach and esophagus, which makes it easier for acid to make its way upward.
They tend to relax the valve between your stomach and esophagus, which makes it easier for acid to make its way upward.
While there’s nothing you can do to stop this entirely, there are a few things that can help prevent heartburn from flaring up during pregnancy:
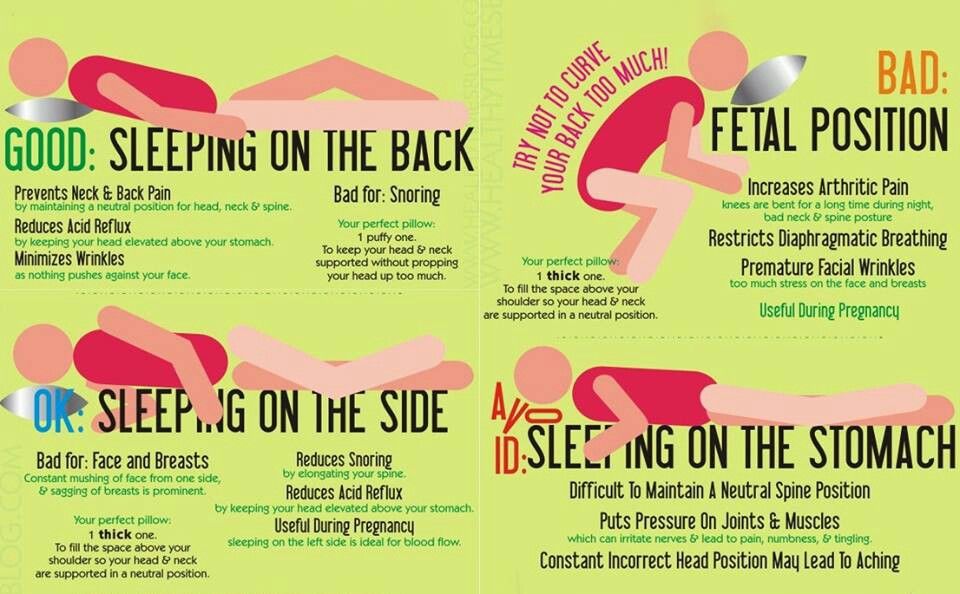
- Avoid lying down after eating. It may be tempting to take a post-meal nap, but if you want to prevent heartburn, don’t lie down after eating. Consider napping in an upright recliner instead.
- Prop yourself up at night. It’s hard enough to sleep well while pregnant without throwing acid reflux on top of everything. To prevent nighttime heartburn, try propping yourself up when you go to sleep to counteract the acid.
- Don’t eat before bedtime. In addition to propping yourself up at night, try not to eat anything within three hours of hitting the sack.
- Skip spicy, acidic, or fried foods. Ask yourself: Are those greasy chips worth being doubled over in pain later? (Probably not.
 ) If you want to avoid the risk, steer clear of any and all rich, fatty foods. Not only will this help prevent heartburn, but making more nutritious choices helps ensure that you your baby is getting the important vitamins and minerals that they need to stay healthy in utero.
) If you want to avoid the risk, steer clear of any and all rich, fatty foods. Not only will this help prevent heartburn, but making more nutritious choices helps ensure that you your baby is getting the important vitamins and minerals that they need to stay healthy in utero. - Eat small meals, but more frequently. Your pregnant tummy doesn’t love to be hit with large amounts of food to digest in one go. Make things easier on your gut by eating several small meals throughout the day instead of three large ones.
- Eat slowly. Wolfing down those small meals will defeat the purpose of spreading them out. Eating quickly increases the risk of acid reflux, so slow down and enjoy your food.
- Wear loose clothing. Tight-fitting clothes are not your stomach’s best friend when you’re trying to prevent heartburn – particularly during pregnancy. Wear clothing that offers support without being restrictive.
- Drink your liquids between meals.
 If you’re the type of person who likes to take a swig of their drink between each bite, it’s time to change course. Drinking liquids during meals can exacerbate heartburn symptoms, so take little sips if you’re thirsty at mealtime.
If you’re the type of person who likes to take a swig of their drink between each bite, it’s time to change course. Drinking liquids during meals can exacerbate heartburn symptoms, so take little sips if you’re thirsty at mealtime.
Someday, scientists may very well invent a miracle medication that promises permanent pregnancy heartburn relief. Unfortunately, that hasn’t happened yet.
So, if you’re wondering how long you can expect to deal with heartburn while you’re pregnant, it will probably be throughout your entire pregnancy. (Now may be a good time to remind yourself that you get a cute little baby out of this when you’re done.)
However, just because there’s no cure, that doesn’t mean you can’t find some relief in the meantime.
If severe pregnancy heartburn is getting in the way of everyday life, it’s time to see a doctor.
Intermountain Healthcare offers individualized and compassionate pregnancy care for women of all ages and health needs.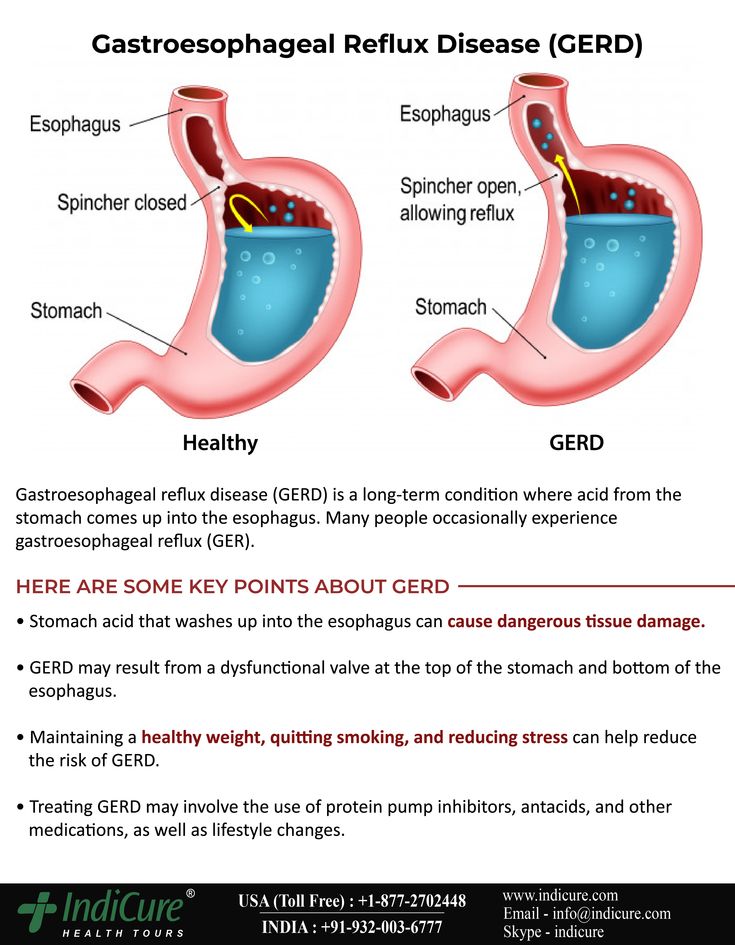
To get the care you need, search for a provider or find an Intermountain Healthcare location near you.
Intermountain Moms Women's Health, Baby Your Baby, Pregnancy, Women and Newborn
Last Updated: 5/21/2021
-
Intermountain Moms
-
Intermountain Moms
Copyright ©2023, Intermountain Health, All rights reserved.
Heartburn, Acid Reflux, and GERD During Pregnancy
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Was this helpful?
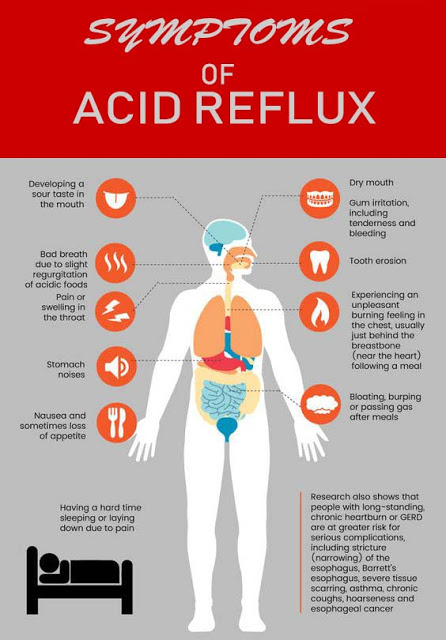
It’s called heartburn, although that burning feeling in your chest has nothing to do with the heart. Uncomfortable and frustrating, it bothers many women, particularly during pregnancy.
Uncomfortable and frustrating, it bothers many women, particularly during pregnancy.
The first question you may have is how to make it stop. You may also wonder if treatments are safe for your baby. Learn what causes heartburn during pregnancy and what you can do about it.
During normal digestion, food travels down the esophagus (the tube between your mouth and stomach), through a muscular valve called the lower esophageal sphincter (LES), and into the stomach.
The LES is part of the doorway between your esophagus and your stomach. It opens to allow food through and closes to stop stomach acids from coming back up.
When you have heartburn, or acid reflux, the LES relaxes enough to allow stomach acid to rise up into the esophagus. This can cause pain and burning in the chest area.
During pregnancy, hormone changes can allow the muscles in the esophagus, including the LES, to relax more frequently. The result is that more acids may seep back up, particularly when you’re lying down or after you’ve eaten a large meal.
In addition, as your fetus grows during the second and third trimesters and your uterus expands to accommodate that growth, your stomach is under more pressure. This can also result in food and acid being pushed back up into your esophagus.
Heartburn is a common occurrence for most people at one time or another, but it doesn’t necessarily mean you’re pregnant. However, if you also experience other symptoms, such as a missed period or nausea, these could be signs that you need to take a pregnancy test.
Pregnancy increases your risk of heartburn or acid reflux. During the first trimester, muscles in your esophagus push food more slowly into the stomach and your stomach takes longer to empty.
This gives your body more time to absorb nutrients for the fetus, but it can also result in heartburn.
During the third trimester, the growth of your baby can push your stomach out of its normal position, which can lead to heartburn.
However, each woman is different. Being pregnant doesn’t necessarily mean you’ll have heartburn. It depends on many factors, including your physiology, diet, daily habits, and your pregnancy.
Being pregnant doesn’t necessarily mean you’ll have heartburn. It depends on many factors, including your physiology, diet, daily habits, and your pregnancy.
Relieving heartburn during pregnancy typically involves some trial and error. Lifestyle habits that can reduce heartburn are often the safest methods for mother and baby. The following tips may help relieve your heartburn:
- Eat smaller meals more frequently and avoid drinking while eating. Drink water in between meals instead.
- Eat slowly and chew every bite thoroughly.
- Avoid eating a few hours before bed.
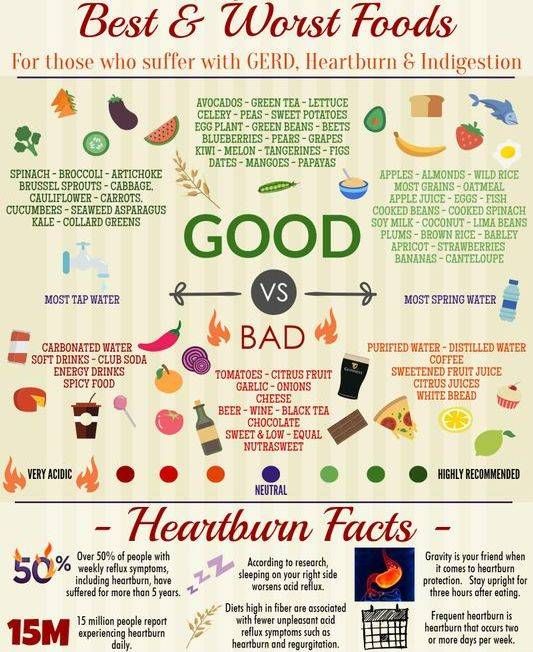
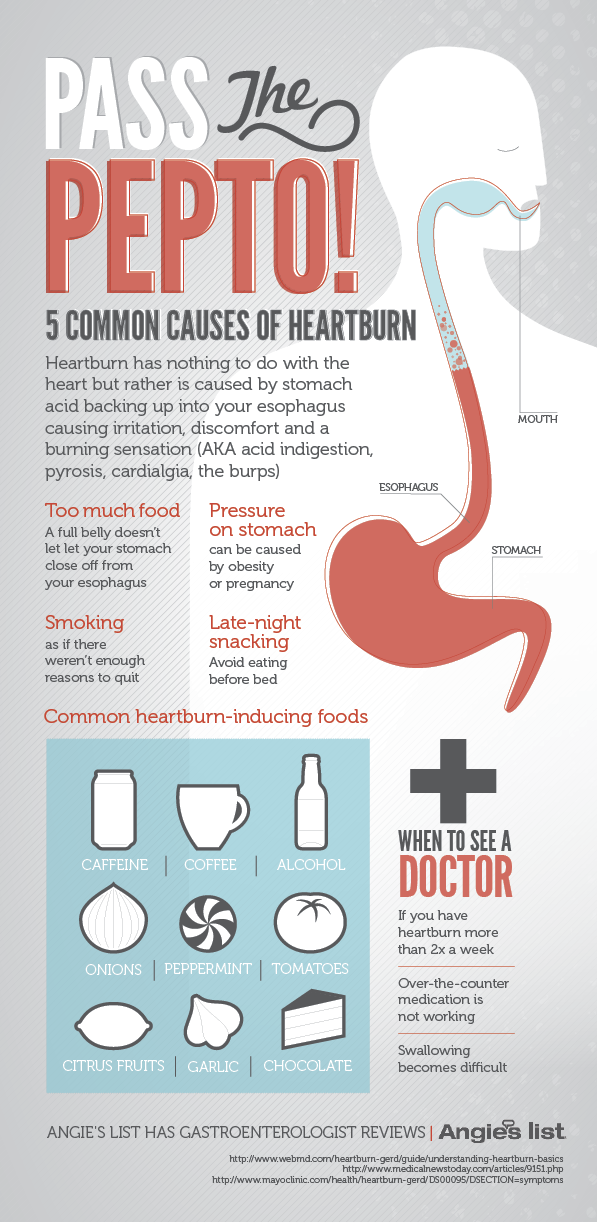
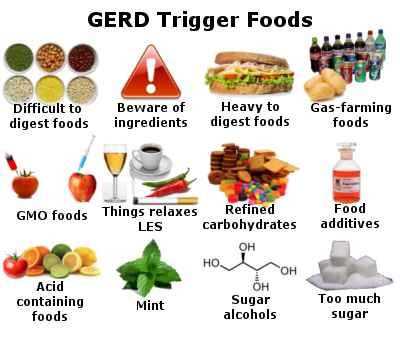
- Avoid foods and beverages that trigger your heartburn. Typical culprits include chocolate, fatty foods, spicy foods, acidic foods like citrus fruits and tomato-based items, carbonated beverages, and caffeine.
- Stay upright for at least one hour after a meal. A leisurely walk may also encourage digestion.
- Wear comfortable rather than tight-fitting clothing.
- Maintain a healthy weight.

- Use pillows or wedges to elevate your upper body while sleeping.
- Sleep on your left side. Lying on your right side will position your stomach higher than your esophagus, which may lead to heartburn.
- Chew a piece of sugarless gum after meals. The increased saliva may neutralize any acid coming back up into the esophagus.
- Eat yogurt or drink a glass of milk to quell symptoms once they start.
Alternative medicine options include acupuncture and relaxation techniques, such as progressive muscle relaxation, yoga, or guided imagery. Always check with your doctor before trying new treatments.
Over-the-counter antacids such as Tums, Rolaids, and Maalox may help you cope with occasional heartburn symptoms. Those made of calcium carbonate or magnesium are good options.
However, it may be best to avoid magnesium during the last trimester of pregnancy. Magnesium could interfere with contractions during labor.
Most doctors recommend avoiding antacids that contain high levels of sodium. These antacids can lead to a buildup of fluid in the tissues.
These antacids can lead to a buildup of fluid in the tissues.
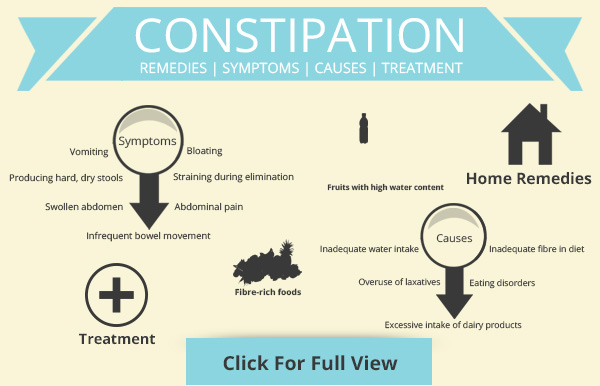
You should also avoid any antacids that list aluminum on the label, as in “aluminum hydroxide” or “aluminum carbonate”. These antacids can lead to constipation.
Finally, stay away from medications like Alka-Seltzer that may contain aspirin.
Ask your doctor for the best option. If you find yourself downing bottles of antacids, your heartburn may have progressed to gastroesophageal acid reflux disease (GERD). In that case, you may need a stronger treatment.
If you have heartburn that often wakes you up at night, returns as soon as your antacid wears off, or creates other symptoms (such as difficulty swallowing, coughing, weight loss, or black stools), you may have a more serious problem that requires attention.
Your doctor may diagnose you with GERD. This means that your heartburn needs to be controlled to protect you from complications such as damage to the esophagus.
Your doctor may prescribe certain acid-reducing medications to reduce your symptoms. Research indicates that medications called h3 blockers, which help block the production of acid, appear to be safe.
Research indicates that medications called h3 blockers, which help block the production of acid, appear to be safe.
Another type of medication, called proton pump inhibitors, is used for people with heartburn that doesn’t respond to other treatments.
If you’re concerned about the effects of medications, be sure to talk to your doctor. Doctors can help you control your symptoms while keeping your unborn child safe.
Acid related diseases in pregnancy | Rassvet Clinic
Heartburn during pregnancy is a very common complaint. It is known that up to 80% of pregnant women experience symptoms characteristic of gastroesophageal reflux disease (GERD) (heartburn, dysphagia, belching, and others), and the frequency of heartburn in the first trimester is 7.2%, in the second - 18.2%, in the third - 40%.
The main factors behind this high prevalence of GERD in pregnancy include hormonal changes such as hyperprogesteronemia (increased levels of the hormone progesterone) and hyperestrogenemia (increased levels of estrogen hormones), as well as increased intra-abdominal pressure due to uterine and fetal growth.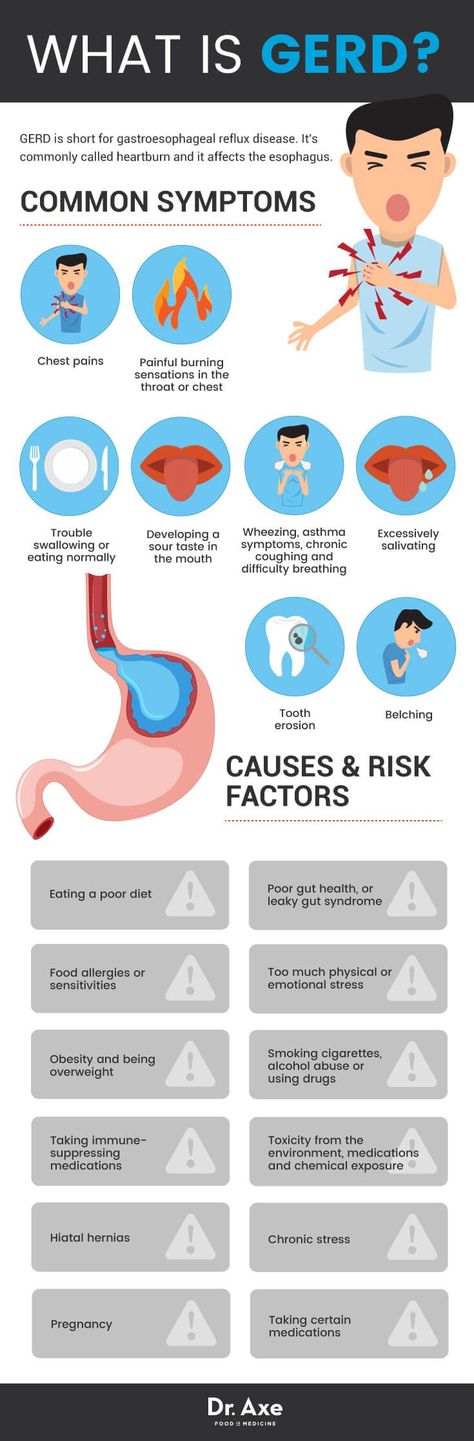
The action of gestational hormones in the first trimester of pregnancy is due to the fact that they, without affecting the basal tone of the lower esophageal sphincter (LES), reduce the increase in pressure of this sphincter in response to a variety of physiological stimuli, including food intake. In the second and third trimesters of pregnancy, progesterone and estrogen reduce the basal tone of the LES to 50% of the initial level, the maximum decrease occurs at 36 weeks of gestation. After a successful delivery, the tone of the LES in women who did not suffer from GERD before pregnancy, as a rule, returns to normal - in connection with this, this condition is called "pregnancy heartburn."
Pregnancy heartburn usually does not lead to the development of esophagitis, complications of GERD (strictures, ulcers, bleeding) and does not require serious medical treatment.
If a woman had GERD before pregnancy, the complaints may worsen during pregnancy and require examination and medication.
The diagnosis of GERD during pregnancy is established primarily on the basis of complaints, anamnesis data and objective examination. X-ray examination in pregnant women - due to possible damaging effects on the fetus - is not used, pH-metry and manometry can be used, but the need for its use is doubtful.
Esophagogastroduodenoscopy (EGD) is the method of choice for diagnosing GERD in pregnant women, but it should only be used for strict indications, such as a history of complications of GERD and the ineffectiveness of ongoing drug therapy.
Treatment of GERD in pregnant women should be based on changes in lifestyle and nutrition: exclusion of a horizontal position of the body immediately after meals, sleeping with the head end of the bed elevated (by 15 cm), exclusion of physical activity that increases intra-abdominal pressure (including wearing corsets, tight belts, bandages). The last meal should take place no later than 3 hours before bedtime, you need to eat in small portions, pay special attention to the normalization of the stool.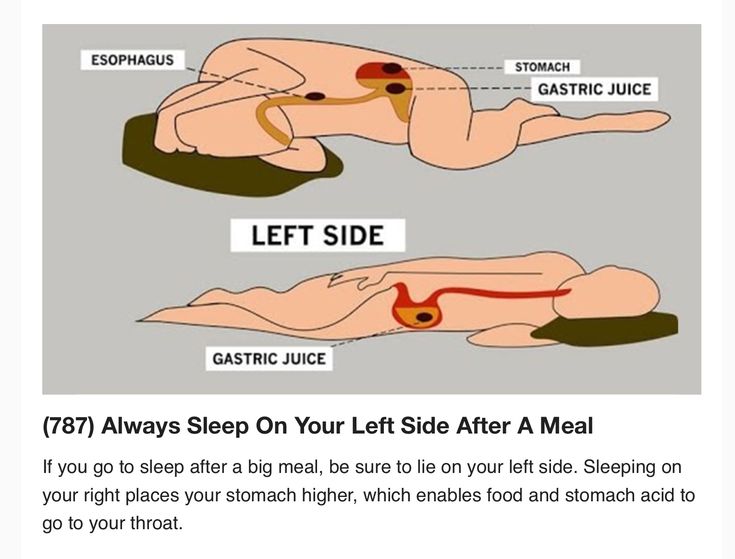
First-line drugs for the treatment of GERD in pregnant women include antacids and alginates. With the ineffectiveness of these drugs, it is permissible to prescribe prokinetics (metoclopramide), blockers of histamine h3 receptors and (according to strict indications) proton pump inhibitors (PPIs).
H2-histamine blockers are the most commonly prescribed group of drugs for pregnant women. They are classified as risk category B by the US Food and Drug Administration (FDA) ( "drugs taken by a limited number of pregnant women without evidence of their effect on the incidence of congenital anomalies or damaging effects on the fetus") . In Russian instructions, only cimetidine and ranitidine are allowed with a caveat: use during pregnancy is possible only if the expected effect of therapy outweighs the potential risk to the fetus. Famotidine and nizatidine in the Russian Federation are contraindicated for pregnant women.
Although most PPIs are also classified by the FDA as risk category B, in Russia there are more stringent restrictions on the use of this group of drugs in pregnant women.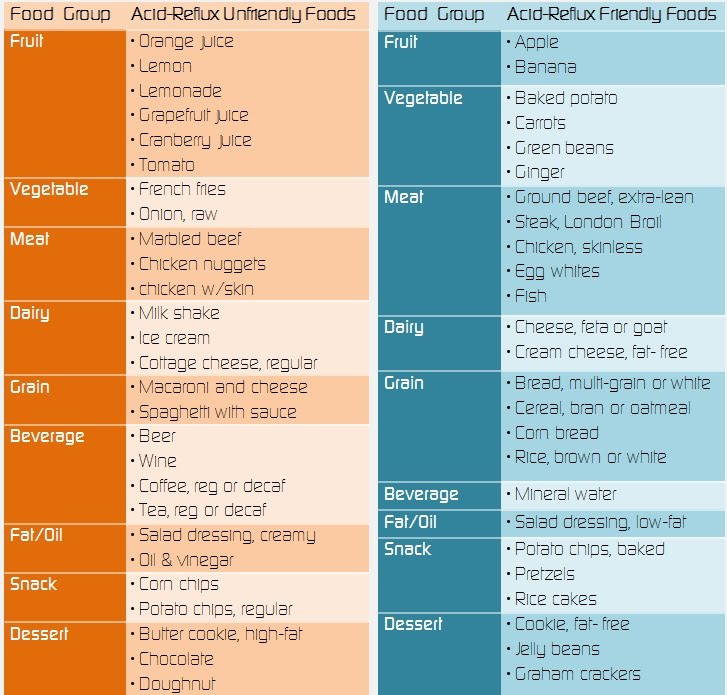 So, lansoprazole is contraindicated in the first trimester, in the second and third trimesters it can be used only if the expected benefit of therapy outweighs the potential risk to the fetus. The use of pantoprazole and esomeprazole is possible only under strict indications, when the benefit to the mother outweighs the potential risk to the fetus. Rabeprazole during pregnancy is contraindicated.
So, lansoprazole is contraindicated in the first trimester, in the second and third trimesters it can be used only if the expected benefit of therapy outweighs the potential risk to the fetus. The use of pantoprazole and esomeprazole is possible only under strict indications, when the benefit to the mother outweighs the potential risk to the fetus. Rabeprazole during pregnancy is contraindicated.
Pregnancy has a beneficial effect on the course of peptic ulcer disease: 75-80% of women experience remission of the disease, and it does not have a noticeable effect on its outcome. However, some patients may experience an exacerbation. This is most often observed in the first trimester of pregnancy (14.8%) and the third trimester (10.2%), as well as 2-4 weeks before the due date or in the early postpartum period. Uncomplicated peptic ulcer does not adversely affect the development of the fetus.
Treatment of peptic ulcer in pregnant women includes adherence to generally accepted "regime" measures and diet; taking in the usual therapeutic doses of non-absorbable antacids (1 sachet 3 times a day 1 hour after meals and adsorbents 1 sachet 3 times a day 1 hour after meals).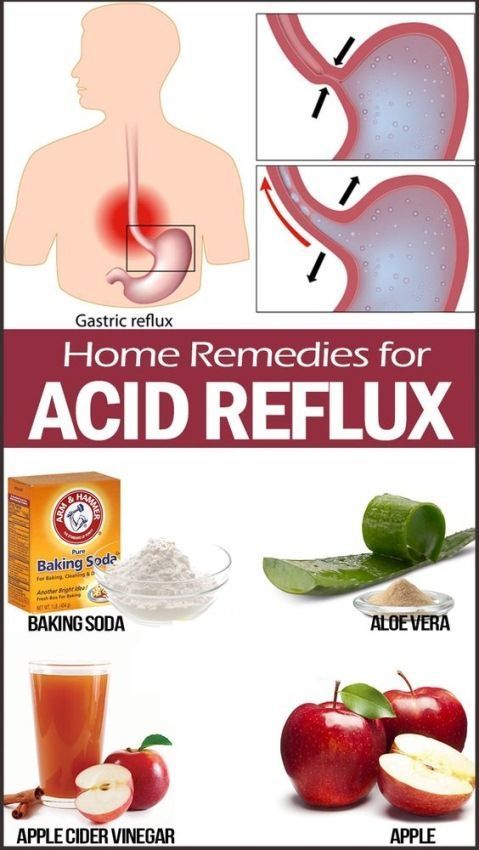 If there is no effect, h3-blockers are prescribed (ranitidine 150/300 mg once a night), in case of their insufficient effectiveness, as well as with the development of complications, we can take PPIs (omeprazole 20-40 mg, lansoprazole 30-60 mg, pantoprazole 40 mg). mg in the morning before the first meal). Bismuth preparations are contraindicated for pregnant women. Eradication therapy for H. pylori infection in pregnant women is not carried out.
If there is no effect, h3-blockers are prescribed (ranitidine 150/300 mg once a night), in case of their insufficient effectiveness, as well as with the development of complications, we can take PPIs (omeprazole 20-40 mg, lansoprazole 30-60 mg, pantoprazole 40 mg). mg in the morning before the first meal). Bismuth preparations are contraindicated for pregnant women. Eradication therapy for H. pylori infection in pregnant women is not carried out.
Author:
Kaibysheva Valeria Olegovna
Gastroenterologist Ph.D.
Treatment and prevention of gastroesophageal reflux disease
Treatment and prevention of gastroesophageal reflux disease (GERD)
Gastroesophageal reflux disease (GERD) undesirable as GERD usually responds well to treatment.
GERD is treated gradually. The doctor will help you choose the right course of treatment. If the disease is mild, it will be enough for the patient to follow a certain diet, give up certain activities, and sometimes take over-the-counter medications.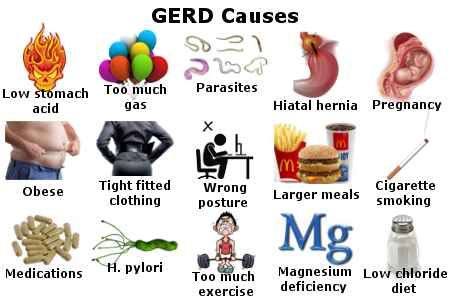
In cases where symptoms are more persistent (daily heartburn, symptoms that come on at night), prescription medication may be required. Surgery is a reasonable alternative to permanent medication, especially if the disease is acquired at an early age.
Surgery is also recommended if medication does not help. However, today there is a new generation of drugs that can effectively control gastroesophageal reflux.
If symptoms are still uncomfortable after taking strong drugs, GERD is most likely not the cause. Most gastroenterologists and surgeons do not recommend surgery in such cases, since the symptoms still continue to disturb after it.
Lifestyle changes
Gastroesophageal reflux treatment begins with lifestyle changes. First you need to understand what affects the occurrence of symptoms.
If you have symptoms of GERD, use the following tips:
- Avoid foods and drinks that stimulate the lower esophageal sphincter to relax, such as foods flavored with mint, chocolate, and alcohol.
- Lose weight if you are overweight. Being overweight and obese contributes to GERD because being overweight increases pressure on the stomach and lower esophageal sphincter, causing acidic stomach acid to reflux into the esophagus and irritate the esophageal mucosa.
- Do not lie down for at least two or three hours after eating. After eating it is good to take a walk. This not only prevents the onset of GERD symptoms, but also burns extra calories.
- Avoid foods that trigger GERD symptoms. Do not eat fatty or fried foods, creamy sauces, mayonnaise or ice cream. Other foods that may exacerbate symptoms include coffee, tea, sodas, tomatoes, and citrus fruits.
- Stop smoking. Smoking disrupts the digestive system and, according to some studies, relaxes the lower esophageal sphincter. Smoking also reduces the amount of bicarbonate in saliva and reduces its ability to protect the esophagus from stomach acid.
 Some types of nicotine replacement therapy (nicotine patch, nicotine gum) can cause indigestion, stomach pain, and vomiting. Talk to your doctor about possible side effects of these products before use.
Some types of nicotine replacement therapy (nicotine patch, nicotine gum) can cause indigestion, stomach pain, and vomiting. Talk to your doctor about possible side effects of these products before use.
- Avoid clothing that puts pressure on your belly, such as tight belts, tight jeans, and elastic waistbands, which put pressure on your stomach and lower esophageal sphincter.
- Raise the head of the bed 15-20 cm or use a wedge-shaped pillow to force acid into the stomach by gravity.
- Don't bend over after eating. If you need to pick something up from the floor, it's better to squat on half-bent knees and try not to bend at the waist. Do not engage in sports and physical labor after eating.
- Check your medications. Some medications can make symptoms worse. These drugs include theophylline, calcium channel blockers, alpha and beta blockers, anticholinergics that may be present in drugs used to treat Parkinson's disease, asthma, and some over-the-counter cold and cough medicines.
 If you think a drug you are taking is affecting your symptoms, talk to your doctor about alternatives. Do not interrupt the prescribed treatment without consulting a doctor.
If you think a drug you are taking is affecting your symptoms, talk to your doctor about alternatives. Do not interrupt the prescribed treatment without consulting a doctor.
Medication for gastroesophageal reflux
Your doctor may prescribe medication for GERD. Because GERD is often a chronic condition, you will need to take medication for the rest of your life. In some cases, long-term treatment is not required.
Be patient, it takes time to find the right drug and dosage. If the symptoms do not go away even after taking the drugs, or if they reappear immediately after completing the course, consult your doctor. If GERD symptoms appear during pregnancy, contact your obstetrician before starting medication.
The following is information about drugs that are commonly prescribed to treat GERD:
Over-the-counter antacids
These drugs help with mild and rare symptoms. Their action is to neutralize the acidic gastric juice. Antacids are usually fast-acting and can be taken as needed. Because they do not last long, they do not prevent heartburn and are less effective for symptoms that often occur.
Antacids are usually fast-acting and can be taken as needed. Because they do not last long, they do not prevent heartburn and are less effective for symptoms that often occur.
Most antacids contain calcium carbonate (Maalox) or magnesium hydroxide. Sodium bicarbonate, or baking soda, helps with heartburn and indigestion. It should be mixed with at least 120 ml of water and taken one to two hours after meals so as not to overload a full stomach. Talk to your doctor about the need for this treatment. Do not use this method for more than two weeks and use it only in extreme cases, since soda can lead to metabolic disorders (pH) and the formation of erosions in the esophagus and stomach. Before using it on children under 12 years of age, consult a doctor.
Another type of antacid contains alginate or alginic acid (eg Gaviscon). The advantage of such an antacid is that it does not allow fluid to seep back into the esophagus.
Antacids can interfere with the body's ability to absorb other drugs, so if you are taking other drugs, check with your doctor before taking antacids.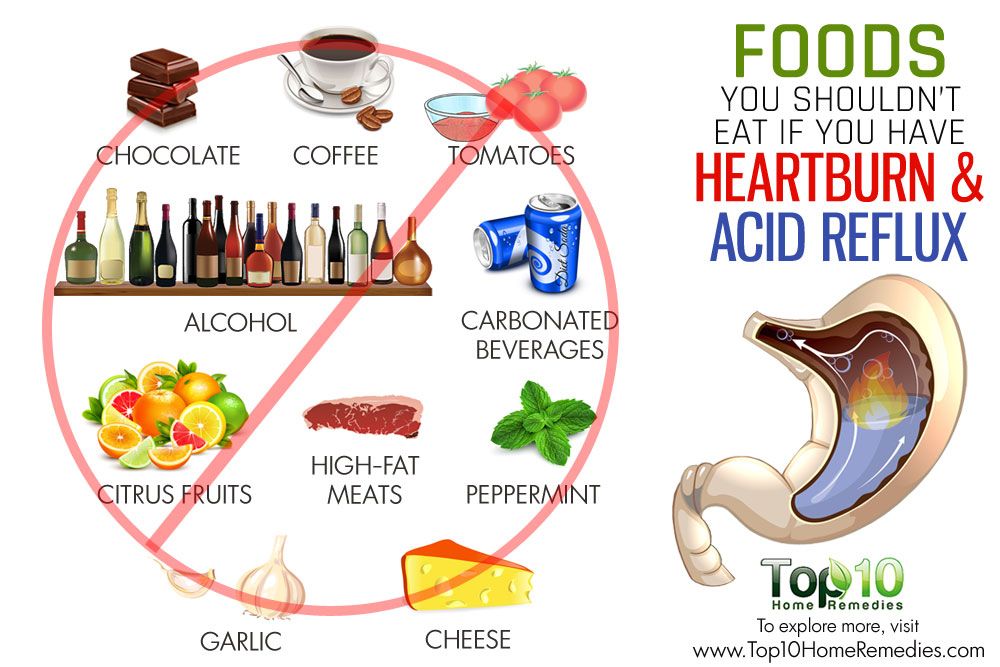
Ideally, you should take antacids at least 2-4 hours after taking other drugs to minimize the chance of them not being absorbed. People with high blood pressure should avoid taking high sodium antacids (Gaviscon).
Finally, antacids are not a reliable treatment for erosive esophagitis, a disease that must be treated with other drugs.
Hydrochloric Acid Suppressants
These drugs reduce the amount of acid produced by the stomach and are available with or without a prescription. Usually, the same drugs are dispensed on prescription, but in a larger dosage. They may help those who are not helped by antacids. Most patients get better if they take drugs that suppress the production of hydrochloric acid and make lifestyle changes.
The mechanism of action distinguishes between two groups of such drugs:
-Blocks H 2 -gistamine reticators
-Proton pump inhibitors
Most likely, the doctor recommends taking the drug for several weeks in a standard dose, and then if it is not possible to achieve the desired effect, prescribe a drug with a higher dosage.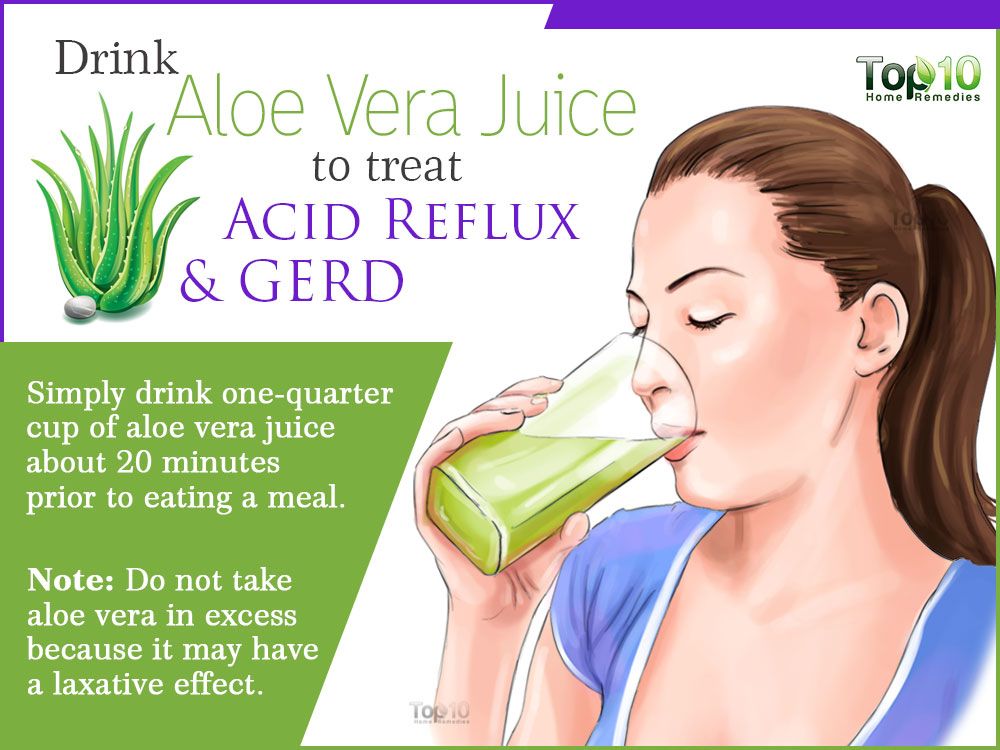
Traditional h3 blockers include:
- nizatidine (Axid AR Axid AR)
- famotidine (Pepcid AS Pepcid AC)
- cimetidine (Tagamet HB Tagamet HB)
- ranitidine 75 (Zantac 75)
Pepcid Complete is a combination of famotidine, calcium carbonate and magnesium hydroxide found in antacids.
Conventional proton pump inhibitors include:
- lansoprazole (Prevacid)
- omeprazole (Prilosec, Prilosec)
- rabeprazole (AcipHex, AcipHex, Pariet)
- pantoprazole (Protonix Protonix, Nolpaza Nolpaza)
- esomeprazole (Nexium) , Nexium)
- omeprazole + sodium bicarbonate ("Zegeride" Zegerid)
- dexlansoprazole ("Dexilant" Dexilant)
Proton pump inhibitors (PPI) also reduce acidity, but are more powerful than h3- blockers. Proton pump inhibitors are most commonly prescribed to treat heartburn and acid reflux.
These drugs block the secretion of acid from the cells of the gastric mucosa and significantly reduce the amount of stomach acid.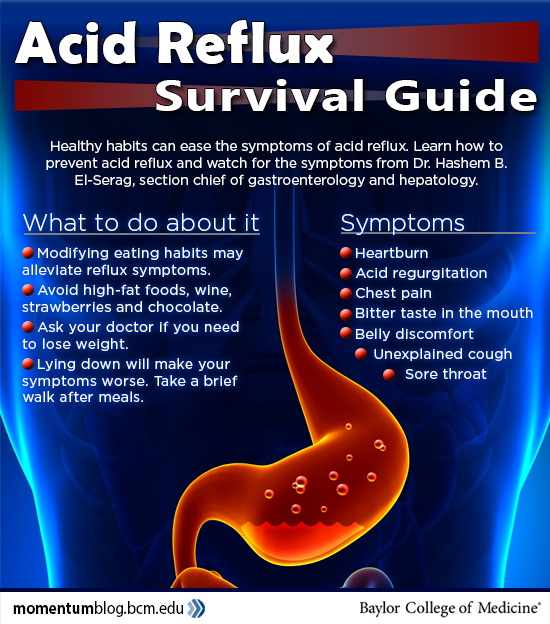 They don't work as fast as antacids, but they can relieve reflux symptoms for hours.
They don't work as fast as antacids, but they can relieve reflux symptoms for hours.
PPIs are also used to treat inflammation of the esophagus (esophagitis) and erosions of the esophagus. Studies have shown that the majority of patients with esophagitis who took these drugs recovered after 6-8 weeks. It is likely that your doctor will re-evaluate your health after 8 weeks of taking proton pump inhibitors and, according to the results, reduce the dosage or stop treatment. If symptoms do not return within three months, you will only need to take medication occasionally. People with liver disease should consult their doctor before taking these drugs.
Prokinetics
Prokinetics, e.g. They also increase the contractions of the esophagus and stomach to some extent, so that the stomach is emptied more quickly. These drugs may be used as an adjunctive treatment for people with GERD.
GERD surgery
Surgery is an alternative to conservative treatment of GERD. Surgery is most commonly performed on young patients (because they would otherwise require long-term treatment) with typical GERD symptoms (heartburn and belching) who are helped by medication but are looking for an alternative to daily medication.
Surgery is most commonly performed on young patients (because they would otherwise require long-term treatment) with typical GERD symptoms (heartburn and belching) who are helped by medication but are looking for an alternative to daily medication.
Patients with atypical symptoms or patients who are not responding to medical treatment should undergo surgery only when there is no doubt about the diagnosis of GERD and the relationship between symptoms and reflux is confirmed by research results.
Fundoplication is used in most cases. During this operation, the upper part of the stomach is wrapped around the lower esophageal sphincter, which increases its tone. These days, minimally invasive (laparoscopic) techniques are commonly used instead of traditional "open" surgery. One of the benefits of a fundoplication is that the hiatal hernia can also be repaired during the operation.
Surgery is not always effective and some patients still need to take medication after surgery.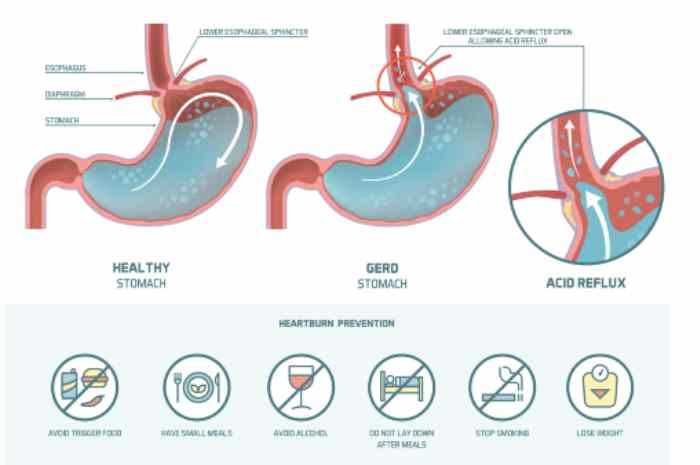 The results of this surgery are usually positive, but complications can still occur, such as difficulty swallowing, bloating and gas, difficult recovery after surgery, and diarrhea that occurs due to damage to the nerve endings that are adjacent to the stomach and intestines.
The results of this surgery are usually positive, but complications can still occur, such as difficulty swallowing, bloating and gas, difficult recovery after surgery, and diarrhea that occurs due to damage to the nerve endings that are adjacent to the stomach and intestines.
Prevention of GERD
First of all, you need to pay attention to lifestyle and avoid situations that can trigger the onset of the disease.
Remember that GERD happens when stomach acid backs up into the esophagus, which connects the throat to the stomach.
To keep the lower esophageal sphincter functioning properly, follow these guidelines:
Avoid bending over and other physical exercises that increase pressure on the abdominal cavity. Don't exercise on a full stomach.
Do not wear clothes that are tight around the waist, such as elastic waistbands and belts, which can increase pressure on the stomach.
Do not lie down in the field of food. If you lie on your back after a large meal, it will be easier for the contents of the stomach to pass into the esophagus. For a similar reason, don't eat before bed. The head of the bed should rise 15-20cm so that gravity keeps the acid in the stomach where it should be while you sleep.
If you lie on your back after a large meal, it will be easier for the contents of the stomach to pass into the esophagus. For a similar reason, don't eat before bed. The head of the bed should rise 15-20cm so that gravity keeps the acid in the stomach where it should be while you sleep.
Do not overeat. Due to the fact that there is a large amount of food in the stomach, pressure on the lower esophageal sphincter increases, as a result of which it opens.
To keep your lower esophageal sphincter and esophagus functioning properly, follow these tips:
Quit smoking and avoid products containing tobacco. Smoking relaxes the lower esophageal sphincter, reduces the amount of acid-neutralizing saliva in the mouth and throat, and damages the esophagus.
Avoid foods that aggravate symptoms, such as tomato sauces, mints, citrus fruits, onions, coffee, fried foods, and carbonated drinks.
Do not drink alcoholic beverages. Alcohol causes the lower esophageal sphincter to relax, and the esophagus may begin to contract unevenly, causing acid to reflux into the esophagus and cause heartburn.
Alcohol causes the lower esophageal sphincter to relax, and the esophagus may begin to contract unevenly, causing acid to reflux into the esophagus and cause heartburn.
Check your medications. Some medications can make symptoms worse. Do not interrupt the prescribed treatment without consulting your doctor. Drugs that have this effect include asthma and emphysema drugs (such as theophylline), anticholinergics for Parkinson's disease and asthma, sometimes found in over-the-counter drugs, some calcium channel blockers, alpha blockers, and beta-blockers to treat heart disease or high blood pressure, some drugs that affect the nervous system, iron supplements.
While some drugs exacerbate GERD symptoms, others can cause drug-induced esophagitis, a condition that causes the same symptoms as GERD but is not due to reflux. Drug esophagitis happens when a pill is swallowed but does not reach the stomach because it sticks to the wall of the esophagus. Because of this, the mucous membrane of the esophagus is corroded, chest pain, esophageal ulcers and pain during swallowing occur.