Formula causes constipation
Newborn Constipation in Formula-Fed Infants: What to Do
The only thing worse than the dreaded poopy diaper? Worrying about why your baby isn’t having one.
If your baby has gone several days without a dirty diaper, you may be ready to tear out your hair trying to figure out what’s wrong.
As you run through all the potential causes, one thing likely to cross your mind is their diet — especially if you’ve recently started them on formula.
Is it true that formula can cause constipation? What should you do if your baby is constipated? When do you need to contact your child’s pediatrician? Let’s take a look.
It’s true: Formula-fed babies are more likely to be constipated than those exclusively on breast milk. Why is this?
Well, breast milk is generally easier for babies to digest and considered a natural laxative.
Formula, on the other hand, is thicker. It has larger proteins that can be harder to digest. This makes gastrointestinal problems — including constipation — more likely.
But keep in mind that this doesn’t mean it’s impossible for a breastfed baby to become constipated or that all babies on formula will be constipated.
Every baby is different. Also, whether formula-fed or breastfed, your baby may show signs of constipation when you introduce solids into their diet.
One other note: Some babies fed exclusively with breast milk don’t poop frequently, but in those cases it’s likely because their bodies are absorbing all the nutrient-filled breast milk they’re eating.
Wondering if your baby is constipated? Signs of constipation include:
- infrequent or less common bowel movements
- hard bowel movements that can appear like pellets, rocks, or hard balls
- blood on the surface of the stool or when wiping
- pain while passing bowel movements — for a baby who can’t communicate with words, this may appear as an arched back, a red face, and crying
- a tight belly
- lack of interest in food
The number of poop-filled diapers a baby will have each day or week can vary greatly.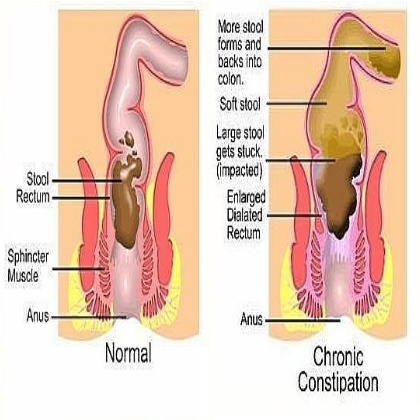 Use your baby’s normal — not your neighbor’s baby or your brother’s baby — as the baseline to help you determine if they’re constipated.
Use your baby’s normal — not your neighbor’s baby or your brother’s baby — as the baseline to help you determine if they’re constipated.
And it’s important to remember that constipation isn’t just about how frequently your infant is pooping, but also about how hard it is for them to do so.
If they poop once every 3 to 4 days, but the poop is soft and seems to pass easily, they may be just fine. On the other hand, if your baby poops every other day but is straining and crying while pooping and the poop is hard, they may be constipated.
If you’ve recently switched to formula after exclusively breastfeeding your baby, you may notice changes in your baby’s poop. It’s not uncommon for it to become harder or change color.
You may also notice an increase in gas, particularly if your baby is transitioning to using a bottle. Every baby is different though, and you may not notice much of a change.
Looking at supermarket formula displays can be enough to set your head spinning.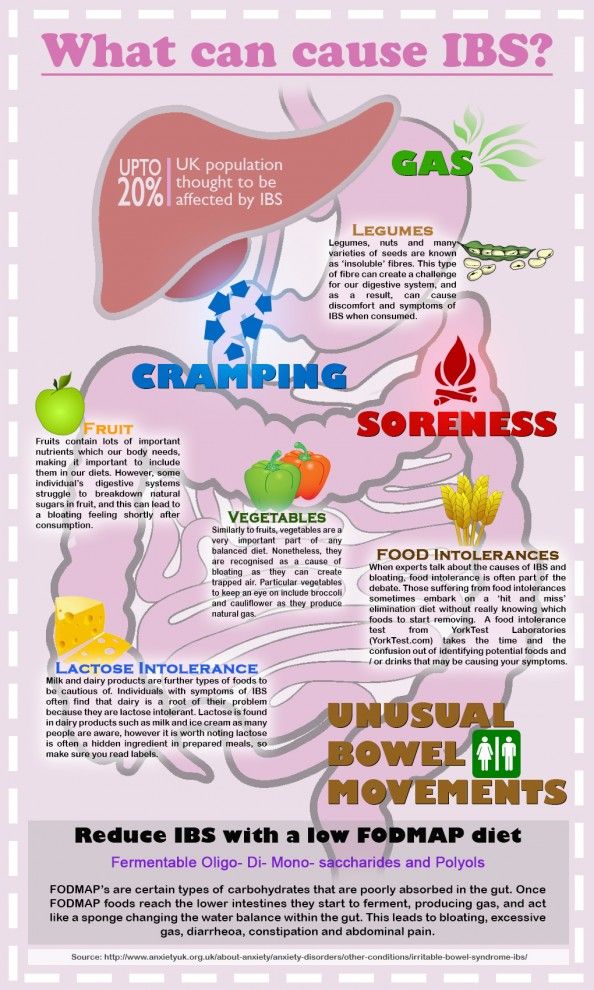
First, there are three different forms of formula you can choose from:
- powders
- concentrates
- ready-to-use
Then, within these forms, they may be:
- milk-based (cow or goat) formulas
- soy-based formulas
- specialty formulas, like organic options
Some formulas advertise themselves as easier to digest.
This can be because they are homogenized, which means they’re processed in a way that breaks down molecules for easier absorption. Or they may be made with ingredients designed to be easier on the digestive system.
Despite this advertisement, there’s no guarantee that any formula will sit well in baby’s stomach. So, how do you choose?
For many parents, the answer lies in asking fellow parents and caregivers about their experiences with formula and researching the ingredients to find one that feels right.
After choosing a formula, you might decide that you’d like to change to another one.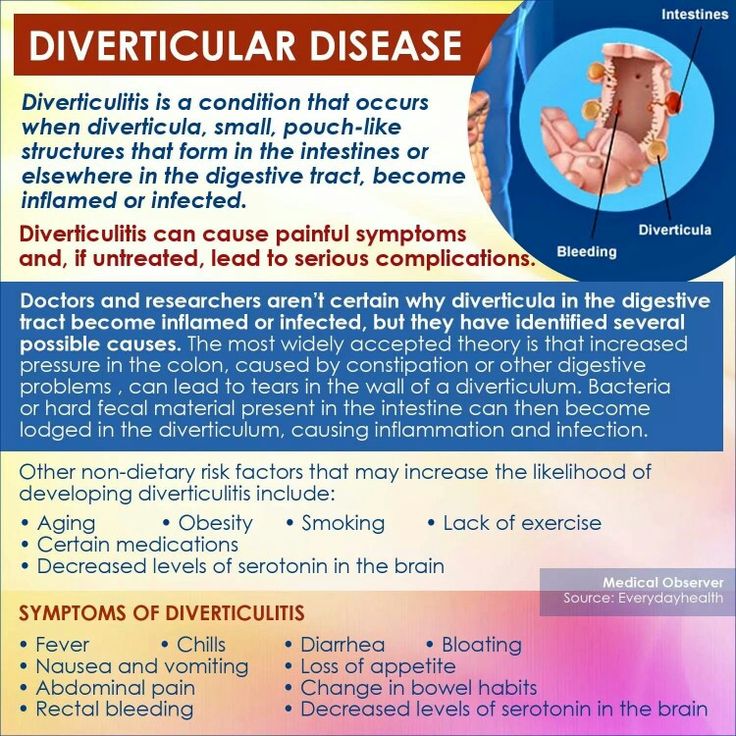 Is this a good idea?
Is this a good idea?
Switching your baby’s formula may make a difference in their poop, since their sensitivity to some of the ingredients in the original formula may have led to their constipation.
However, changing formula styles or brands can also make things worse, especially if you do it too often.
In other words, it’s not a good plan to give your baby one formula for 1 or 2 days, then changing to another formula right away when you see that they’re constipated. Instead, try giving baby a few weeks to adjust to any newly introduced formula.
In some cases, though, changing formulas might be wise. Even so, it’s best to speak with your child’s pediatrician first.
Reasons to consider changing formulas can include:
- food allergies
- extreme fussiness
- a need for more iron in a baby’s diet, as determined by a doctor (though most infant formulas do contain iron)
- weakness or fatigue
- vomiting (more than just spit-up)
- bloody stools
- diarrhea
Especially if your child is showing signs of allergies or wheat or dairy aversions, changing to a brand with different ingredients may make digestion easier.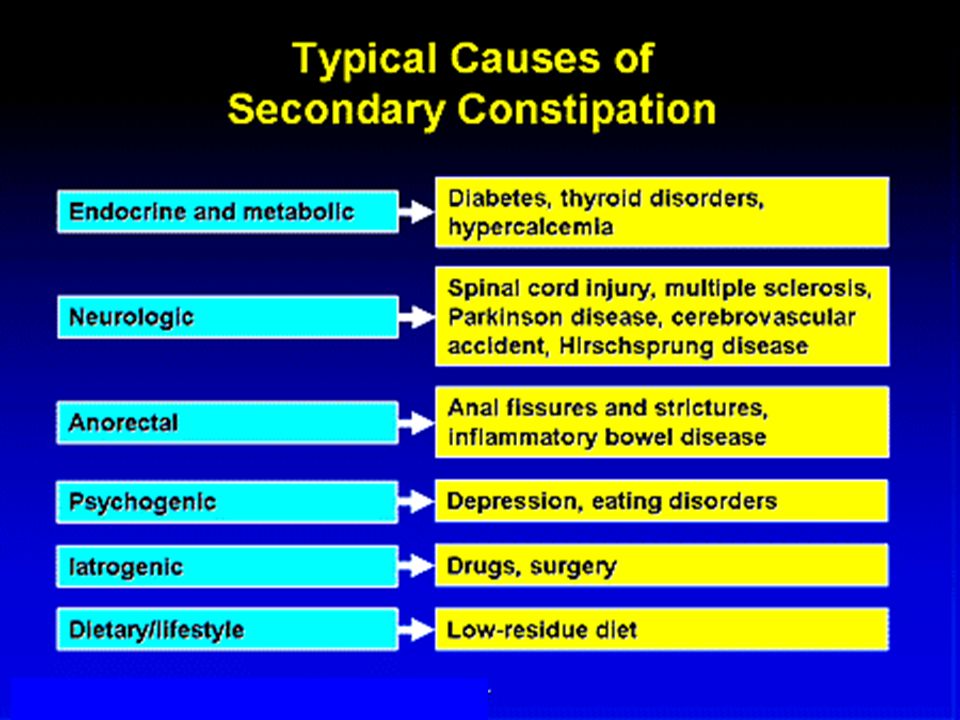
It’s never a good idea to create your own homemade formula, however. Your child’s doctor can help you find an approved formula if your little one needs something special.
For many babies, a simple home remedy or two is all you’ll need to relieve constipation.
For an older baby, you can consider a dietary change.
If your child is over 6 months old, offer them a small amount of 100 percent apple, prune, or pear juice diluted with water. These include sorbitol, a type of sugar. It acts like a laxative and may be able to help with constipation.
Extra water can soften their poop, too. Of course, don’t forget to check with your doctor first for their recommendations on amount and types of liquids.
And if your baby is already eating solids, you may want to consider offering them fiber-filled options like peas and prunes. You may also consider baby cereals with whole wheat or barley instead of rice, since they include more fiber.
For younger babies, you can try the following:
- Bicycle kicks.
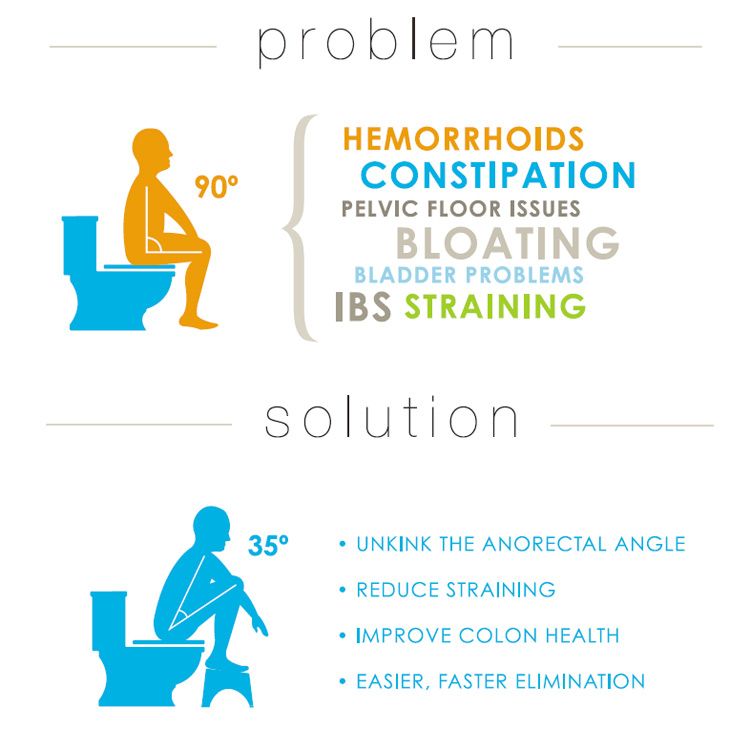
 Gently bend baby’s legs toward their chest or circle their legs in a gentle bicycling motion. (It’s easier to get a poop out in a squat position than lying flat!)
Gently bend baby’s legs toward their chest or circle their legs in a gentle bicycling motion. (It’s easier to get a poop out in a squat position than lying flat!) - Infant massage. Massaging their stomach and having skin-to-skin time may improve your little one’s digestive system.
- Bathing. A warm bath can help your little one’s muscles relax and allow poop to pass.
If these remedies aren’t working, your doctor may suggest other treatments. It’s not recommended to use mineral oil, stimulant laxatives, or enemas to solve constipation in infants, so speak with your pediatrician for safer methods.
Most of the time, infant constipation isn’t a sign of a serious problem, and it can be easily addressed. On very rare occasions, constipation may be a sign of another underlying condition.
Reach out to your baby’s doctor if you notice:
- consistent issues with constipation despite dietary changes to attempt to address it
- vomiting
- weakness
- refusal to eat
- blood in stools
- black stools (after your baby has already passed their meconium, which occurs during the first few days of life)
A constipated baby is one of the few things worse than the smell of a really poopy diaper.
If you’ve recently switched your little one to formula, you may notice that their poops are a little harder and less frequent. You might also notice a change in bowel movements if you’ve introduced solids to your little one’s diet.
If constipation becomes severe or you notice other warning signs of poor health, don’t hesitate to reach out to your baby’s doctor. They can assist you in creating a plan to get your little one feeling better ASAP.
Newborn Constipation in Formula-Fed Infants: What to Do
The only thing worse than the dreaded poopy diaper? Worrying about why your baby isn’t having one.
If your baby has gone several days without a dirty diaper, you may be ready to tear out your hair trying to figure out what’s wrong.
As you run through all the potential causes, one thing likely to cross your mind is their diet — especially if you’ve recently started them on formula.
Is it true that formula can cause constipation? What should you do if your baby is constipated? When do you need to contact your child’s pediatrician? Let’s take a look.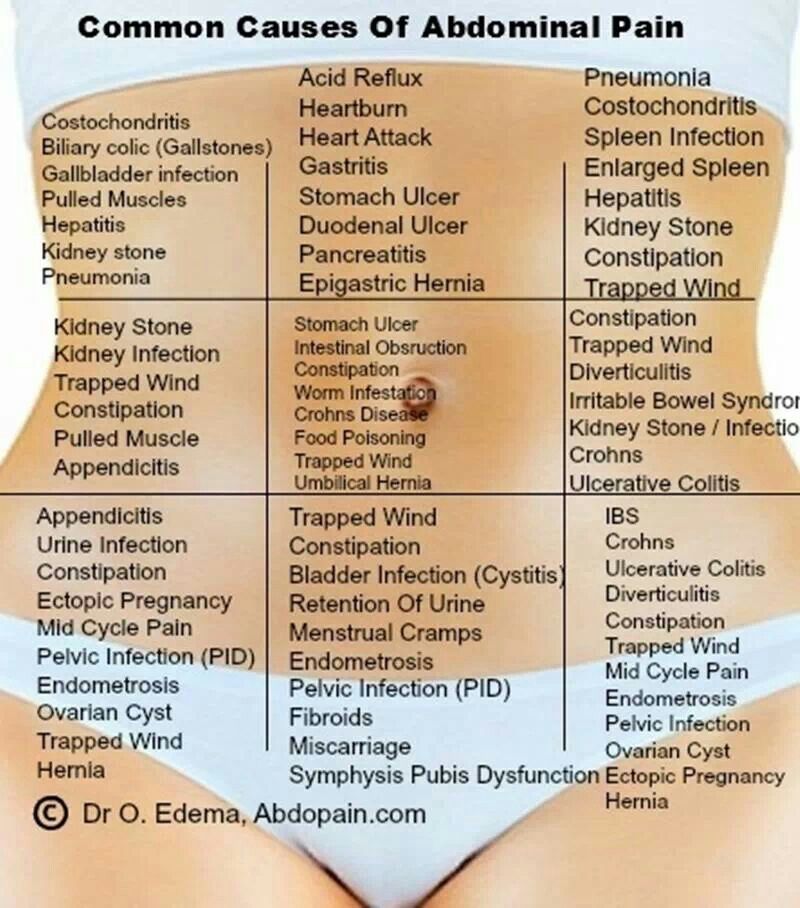
It’s true: Formula-fed babies are more likely to be constipated than those exclusively on breast milk. Why is this?
Well, breast milk is generally easier for babies to digest and considered a natural laxative.
Formula, on the other hand, is thicker. It has larger proteins that can be harder to digest. This makes gastrointestinal problems — including constipation — more likely.
But keep in mind that this doesn’t mean it’s impossible for a breastfed baby to become constipated or that all babies on formula will be constipated.
Every baby is different. Also, whether formula-fed or breastfed, your baby may show signs of constipation when you introduce solids into their diet.
One other note: Some babies fed exclusively with breast milk don’t poop frequently, but in those cases it’s likely because their bodies are absorbing all the nutrient-filled breast milk they’re eating.
Wondering if your baby is constipated? Signs of constipation include:
- infrequent or less common bowel movements
- hard bowel movements that can appear like pellets, rocks, or hard balls
- blood on the surface of the stool or when wiping
- pain while passing bowel movements — for a baby who can’t communicate with words, this may appear as an arched back, a red face, and crying
- a tight belly
- lack of interest in food
The number of poop-filled diapers a baby will have each day or week can vary greatly.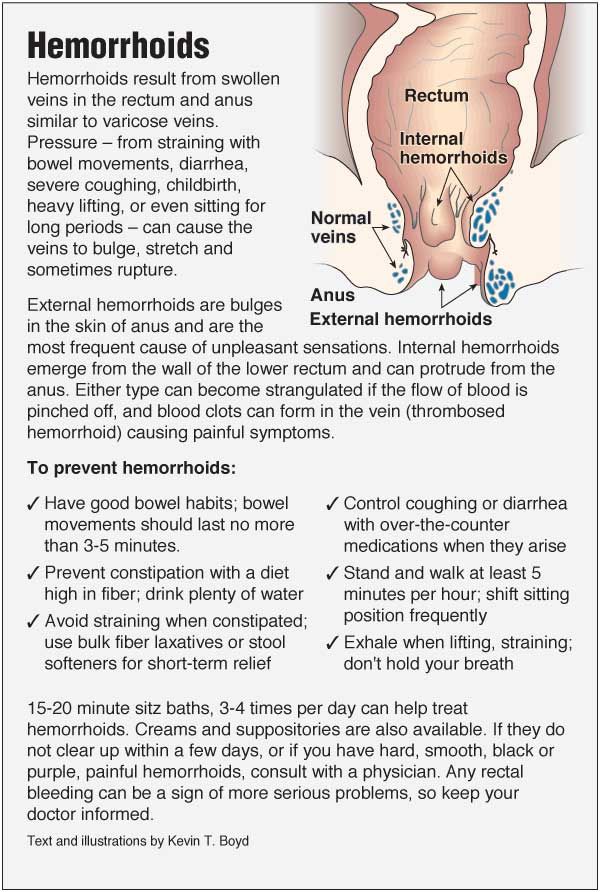 Use your baby’s normal — not your neighbor’s baby or your brother’s baby — as the baseline to help you determine if they’re constipated.
Use your baby’s normal — not your neighbor’s baby or your brother’s baby — as the baseline to help you determine if they’re constipated.
And it’s important to remember that constipation isn’t just about how frequently your infant is pooping, but also about how hard it is for them to do so.
If they poop once every 3 to 4 days, but the poop is soft and seems to pass easily, they may be just fine. On the other hand, if your baby poops every other day but is straining and crying while pooping and the poop is hard, they may be constipated.
If you’ve recently switched to formula after exclusively breastfeeding your baby, you may notice changes in your baby’s poop. It’s not uncommon for it to become harder or change color.
You may also notice an increase in gas, particularly if your baby is transitioning to using a bottle. Every baby is different though, and you may not notice much of a change.
Looking at supermarket formula displays can be enough to set your head spinning.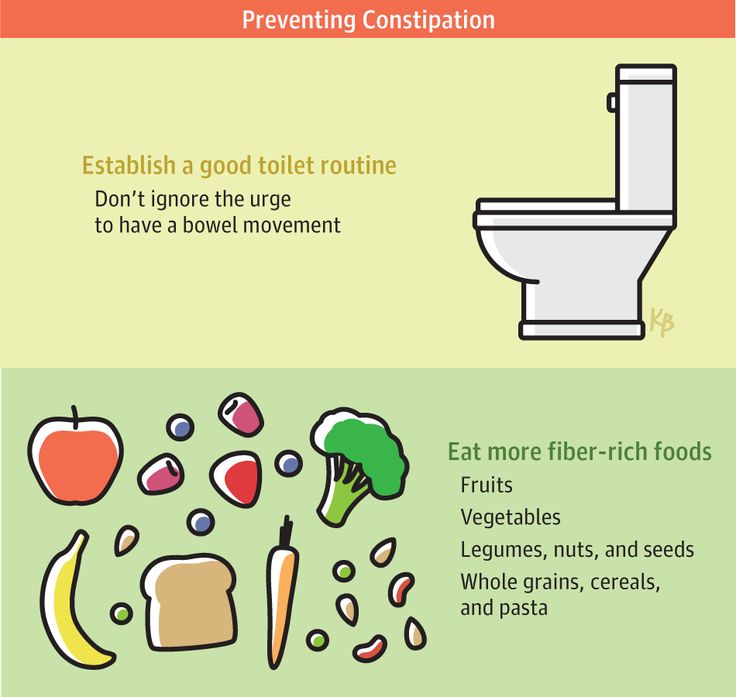
First, there are three different forms of formula you can choose from:
- powders
- concentrates
- ready-to-use
Then, within these forms, they may be:
- milk-based (cow or goat) formulas
- soy-based formulas
- specialty formulas, like organic options
Some formulas advertise themselves as easier to digest.
This can be because they are homogenized, which means they’re processed in a way that breaks down molecules for easier absorption. Or they may be made with ingredients designed to be easier on the digestive system.
Despite this advertisement, there’s no guarantee that any formula will sit well in baby’s stomach. So, how do you choose?
For many parents, the answer lies in asking fellow parents and caregivers about their experiences with formula and researching the ingredients to find one that feels right.
After choosing a formula, you might decide that you’d like to change to another one. Is this a good idea?
Is this a good idea?
Switching your baby’s formula may make a difference in their poop, since their sensitivity to some of the ingredients in the original formula may have led to their constipation.
However, changing formula styles or brands can also make things worse, especially if you do it too often.
In other words, it’s not a good plan to give your baby one formula for 1 or 2 days, then changing to another formula right away when you see that they’re constipated. Instead, try giving baby a few weeks to adjust to any newly introduced formula.
In some cases, though, changing formulas might be wise. Even so, it’s best to speak with your child’s pediatrician first.
Reasons to consider changing formulas can include:
- food allergies
- extreme fussiness
- a need for more iron in a baby’s diet, as determined by a doctor (though most infant formulas do contain iron)
- weakness or fatigue
- vomiting (more than just spit-up)
- bloody stools
- diarrhea
Especially if your child is showing signs of allergies or wheat or dairy aversions, changing to a brand with different ingredients may make digestion easier.
It’s never a good idea to create your own homemade formula, however. Your child’s doctor can help you find an approved formula if your little one needs something special.
For many babies, a simple home remedy or two is all you’ll need to relieve constipation.
For an older baby, you can consider a dietary change.
If your child is over 6 months old, offer them a small amount of 100 percent apple, prune, or pear juice diluted with water. These include sorbitol, a type of sugar. It acts like a laxative and may be able to help with constipation.
Extra water can soften their poop, too. Of course, don’t forget to check with your doctor first for their recommendations on amount and types of liquids.
And if your baby is already eating solids, you may want to consider offering them fiber-filled options like peas and prunes. You may also consider baby cereals with whole wheat or barley instead of rice, since they include more fiber.
For younger babies, you can try the following:
- Bicycle kicks.
 Gently bend baby’s legs toward their chest or circle their legs in a gentle bicycling motion. (It’s easier to get a poop out in a squat position than lying flat!)
Gently bend baby’s legs toward their chest or circle their legs in a gentle bicycling motion. (It’s easier to get a poop out in a squat position than lying flat!) - Infant massage. Massaging their stomach and having skin-to-skin time may improve your little one’s digestive system.
- Bathing. A warm bath can help your little one’s muscles relax and allow poop to pass.
If these remedies aren’t working, your doctor may suggest other treatments. It’s not recommended to use mineral oil, stimulant laxatives, or enemas to solve constipation in infants, so speak with your pediatrician for safer methods.
Most of the time, infant constipation isn’t a sign of a serious problem, and it can be easily addressed. On very rare occasions, constipation may be a sign of another underlying condition.
Reach out to your baby’s doctor if you notice:
- consistent issues with constipation despite dietary changes to attempt to address it
- vomiting
- weakness
- refusal to eat
- blood in stools
- black stools (after your baby has already passed their meconium, which occurs during the first few days of life)
A constipated baby is one of the few things worse than the smell of a really poopy diaper.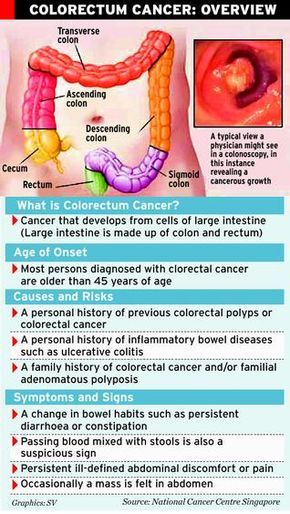
If you’ve recently switched your little one to formula, you may notice that their poops are a little harder and less frequent. You might also notice a change in bowel movements if you’ve introduced solids to your little one’s diet.
If constipation becomes severe or you notice other warning signs of poor health, don’t hesitate to reach out to your baby’s doctor. They can assist you in creating a plan to get your little one feeling better ASAP.
Constipation in children. Prevention. Diet therapy
home
Articles
Health
Sabitova Vasily Ilyasovna Gastroenterologist
06/21/2019
Constipation is widespread among both adults and children (5-30% depending on the diagnostic criteria). Symptoms become chronic in more than 30% of patients, not only cause discomfort and pain to the child himself, but also disrupt the quality of life of his family.
CONSTIPATION - a condition manifested by an increase in the intervals between bowel movements (compared to the individual norm) or systematically slow, difficult and / or insufficient bowel movements. Constipation also includes stools with “gruel”, but after defecation was absent for up to 3 days.
Constipation also includes stools with “gruel”, but after defecation was absent for up to 3 days.
Constipation can be related to functional or organic causes (abnormalities, inflammation). In children, 90-95% of constipation is functional. The peak incidence of functional constipation falls on 2-4 years, when they begin to accustom the child to the potty / toilet.
Main causes of functional constipation
- Pain
- Fever
- Dehydration
- Wrong diet of a nursing mother
- Insufficient drinking regime of a child with artificial feeding
- Insufficient drinking regimen of a breast-fed child with the introduction of complementary foods
- Early transition of the child to artificial feeding
- Fast transition of the baby from one mixture to another (less than 7 days)
- Irrational nutrition of the child (for a long time the child receives food with a large amount of proteins, fats and insufficient dietary fiber, abuse of drinks containing a large amount of astringents - tea, coffee, cocoa)
- Excessive use of baby hygiene products or the development of an allergic reaction of the skin of the perianal area
- Consequences of perinatal injuries of the nervous system
- Rickets, vitamin D deficiency
- Anemia
- Impaired thyroid function (deficiency - hypothyroidism)
- Food allergy, especially cow's milk protein allergy
- Forced potty training, period of adaptation to new conditions (nursery, kindergarten)
- Physical inactivity - a sedentary lifestyle
- Mental trauma or stress
- Systematic suppression of the urge to empty the bowels, associated, for example, with the beginning of attending a kindergarten, school, etc.
- Taking certain drugs
- Constipation in family members
Frequency of defecation in children of different ages
| Age | Number of bowel movements per week | Number of bowel movements per day |
| 0 – 3 months breastfeeding artificial feeding | 5 - 40 5 - 20 | 2.9 2.0 |
| 6 - 12 months | 5 - 28 | 1.8 |
| 1 - 3 years | 4-21 | 1.4 |
| 4 years and older | 3 - 14 | 1.0 |
In addition to the frequency of the chair, you should pay attention to its nature. For a more objective assessment, the “Bristol fecal shape scale” is convenient, since it is the shape of the feces, and not the frequency of the stool, that is more consistent with the time of intestinal transit.
Bristol stool chart
In accordance with this scale, 3 and 4 form of feces is regarded as normal, and 1 and 2 indicate delayed transit (constipation). Quite often, in practice, there are situations when a child has a bowel movement frequency within the normal range, but the stool is dense, fragmented, in a meager amount. These signs indicate incomplete emptying of the bowels and are considered as manifestations of constipation.
The consistency of the stool in newborns and infants should be mushy. From 6 months to 1.5 - 2 years, feces can be both formalized and mushy. From the age of two, the chair must be decorated.
Signs and symptoms of constipation
- abdominal pain, often bursting, aching, sometimes colicky
- bloating
- change in the shape and consistency of the stool
- excessive flatulence
- unpleasant smell of flatus and stool
- may have pain during bowel movements
- straining during bowel movements
- there may be blood in the stool - on the surface of the feces or in the form of traces on a napkin (indicates an anal fissure)
If you do not eliminate constipation and do not establish bowel movements, then there is a risk of coprostasis (formation of fecal stones) and fecal intoxication:
- loss of appetite
- lack of energy
- general malaise
- depression, irritability
- nausea, vomiting
- skin symptoms - dryness, rash, peeling
- fecal incontinence, stool spotting
- urinary retention and incontinence due to pressure from a crowded bowel on the bladder
- bleeding from fissures, hemorrhoids
The treatment of constipation involves the following goals:
1. Normalization of stool consistency (soft, painless stools)
Normalization of stool consistency (soft, painless stools)
2. Regularity of bowel movements (prevention of re-accumulation of feces)
The treatment of constipation is a sequential, complex, individual process and consists of several stages:
- child and parent education
- correction of nutrition and drinking regimen
- elimination of existing coprostasis with the help of medications
- maintenance therapy
It is necessary to exclude factors that provoke and contribute to constipation (normalization of motor and nutritional regimen, discontinuation of medications that can cause constipation, identification of a food allergen, exclusion or confirmation of neuromuscular disease, celiac disease, etc.).
Lifestyle normalization includes:
- development of a conditioned reflex
- active lifestyle
- gymnastics
- light abdominal massage training
- for small children - laying out on the stomach, bending the legs to the stomach.
Education is the first step in the treatment of functional constipation. It must be remembered that episodes of fecal smearing and encopresis (fecal incontinence) are not arbitrary and should not be blamed on the child, who may already be frightened and disoriented. In some cases, when the intra-family situation is difficult, the help of a family psychologist may be needed.
It is important to understand that the treatment of functional constipation can be lengthy, based on trust, partnership and requires patience. Modern laxatives that are legal in children will not make the intestines “lazy”, will not cause “addiction”, they enter the bloodstream in minimal amounts or are not absorbed at all and are safe for long-term use.
Correction of the behavior of a child with constipation is based on the development of a routine of visiting the toilet, in order to achieve regular defecation. Defecation should be every time at the same time. The urge to defecate is based on the gastrocecal reflex, which manifests itself in the morning 1 hour after eating. A child with constipation needs to spend 3-10 minutes in the toilet (depending on age). It is necessary to plant the child on a potty or offer to visit the toilet after each meal.
A child with constipation needs to spend 3-10 minutes in the toilet (depending on age). It is necessary to plant the child on a potty or offer to visit the toilet after each meal.
A prerequisite for effective defecation is to provide a good support for the legs (a low bench on which the child can put his feet), which helps to increase intra-abdominal pressure.
If the defecation is not successful, the child should never be punished and vice versa. The daily frequency of bowel movements can be noted in a diary, which can be analyzed at a scheduled visit to the doctor.
Treatment of constipation should begin with lifestyle changes, which include dietary modification, drinking regimen and physical activity.
Calculation of fluid volume for healthy children
Children under the age of 1 year should drink at least 100 ml of water per day.
For healthy children weighing 10 to 20 kg the water requirement is calculated using the formula:
100 ml (volume of water for children under 1 year old) + 50 ml per kg for body weight over 10 kg.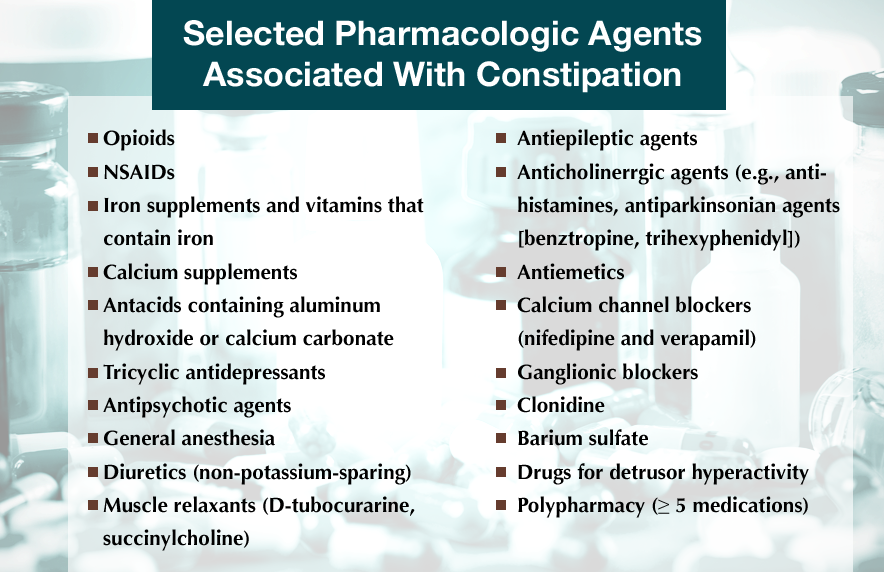
For example, with a mass of 12 kg: 100 ml + 2 x 50 ml = 200 ml.
A child weighing 20 kg should drink water: 100 ml + 50 x 10 = 600 ml
For children weighing over 20 kg the following formula is suggested for calculation:
600 ml (volume of water for a child weighing 20 kg) + 20 ml for each kg over 20 kg.
For children over 3-5 years old you can use the calculation of the amount of water: 30ml / kg of weight
Principles of diet therapy for constipation:
- satisfaction of physical needs for nutrients and energy
- exclusion of excessive consumption of proteins and fats, which can inhibit intestinal motility
- enrichment of the diet with dietary fiber
- normalization of intestinal microflora with pro- and prebiotics
If the child is breastfed, then the mother's nutrition is corrected (restriction of products that promote gas formation). With artificial feeding, special mixtures are shown. For constipation associated with an allergy to cow's milk protein, therapeutic mixtures are prescribed if the child is bottle-fed. If the child is breastfed, cow's milk and products based on it are completely excluded from the mother's diet.
For constipation associated with an allergy to cow's milk protein, therapeutic mixtures are prescribed if the child is bottle-fed. If the child is breastfed, cow's milk and products based on it are completely excluded from the mother's diet.
After the introduction of “thick” complementary foods, boiled water is necessary for all children, regardless of the type of feeding.
For older children, it is recommended to eat foods rich in vegetable fibers. It is not recommended to “smear food”, puree, “snacks”, “eating on the go”. Food should be crumbly, meat / poultry / fish - “piece”. A “bulk” breakfast is required to stimulate the “gastrocecal reflex”.
The main source of coarse-fiber vegetable fiber, containing a large amount of dietary fiber, is cereal bran, rye bread, as well as a number of vegetables and fruits. According to the principles of evidence-based medicine, a statistically significant increase in stool frequency and improvement in its consistency was demonstrated with the use of fiber compared with placebo.
Bran, as the main source of vegetable fiber, is recommended to be added to the second and third courses, after pouring boiling water over it and settling for 20 minutes. Bran can also be used in between meals, drinking plenty of fluids. For school-age children, the total amount of fluid when taking bran should be at least 1.5-2 liters per day, otherwise they mainly act as sorbents, absorbing fluid from the intestines, thereby increasing constipation. The dose is selected individually, it is recommended to start with 1 teaspoon 2-3 times a day, with a gradual increase to 40 g per day. When the effect is achieved, the dose is reduced and limited to one dose.
The American Academy of Pediatrics (2009) recommends a fiber intake of 0.5 g/kg/day (maximum 35 g/day) for all children. Fiber intake below the minimum recommended value has been shown to be a risk factor for chronic constipation in children.
However, long-term intake of a large amount of plant fibers due to fermentation by intestinal microflora is naturally accompanied by bloating and flatulence.
Children with constipation are shown to take cool liquids on an empty stomach (drinking and mineral water, juice, compotes, kvass), to enhance the laxative effect, it is possible to add honey, xylitol or sorbitol. It is very beneficial for bowel function to increase the intake of juices containing sorbitol/sorbitol, such as juice from plums, pears, apricots, peaches and apples,
With “sluggish” bowel function (hypomotor constipation), cool mineral water of medium and high mineralization is used, such as Essentuki 17, Batalinskaya, Arzni, Donat Magnesium, etc.; with spastic constipation (hypermotor constipation, stool form more often type 1) - warm and low mineralization (Essentuki 4). Calculation of mineral water - 3-5 ml / kg per day.
It is necessary to limit milk in its pure form and in dishes, as flatulence may occur with the appearance or intensification of abdominal pain. It is better to replace whole milk with sour-milk products - kefir, acidophilus, yogurt, yogurt, etc.
The diet of children with constipation includes dishes rich in vegetable fiber - salads from fresh vegetables, greens 2-3 times a day, baked apples, stewed vegetables, diluted vegetable and fruit juices with pulp. Food is cooked mostly unground, steamed or boiled in water.
It is preferable to take raw vegetables and fruits (in the absence of contraindications). Especially recommended are tomatoes, zucchini, pumpkin, carrots, beets, lettuce, cauliflower, apples. Dried fruits (prunes, dried apricots, figs) are given in soaked form and as part of cooked dishes. White cabbage, young green beans, green peas are allowed with good tolerance. Parsley, dill, celery are good to add to various dishes and salads.
If after reading the article you still have questions or you do not understand how to apply the recommendations in your particular case, we invite you and your child to be examined by a pediatric gastroenterologist at the DDC. For the convenience of parents, you can make an appointment with a pediatric gastroenterologist at the Children's Diagnostic Center on a weekday and on Saturdays.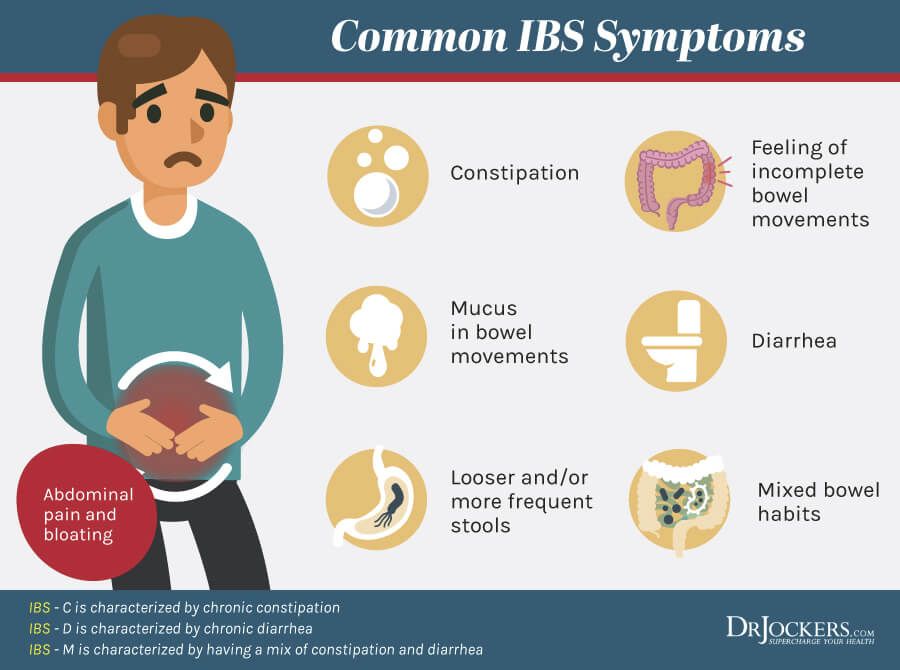
We will be happy to help!
Who gets a tan, who gets a blow!
If a child has a fever, what should I do?
Back to list
Natural approach to constipation
The information in this blog has not been verified by your country's public health authority and is not intended as a diagnosis, treatment or medical advice. Read more
Constipation - irregular stools or difficult bowel movements - is a common problem affecting 20% of people. With constipation, the bowel is emptied less than three times a week. A condition is considered chronic if it persists for two weeks or longer.
Constipation is very common but should not be ignored. In each case, the cause of the constipation must be determined, especially if the symptoms persist after a few weeks. It is important to consult a doctor to make sure that constipation is not caused by some serious medical condition.
The main causes of constipation:
Sedentary lifestyle Constipation can be caused by lack of physical activity, resulting in disruption of normal intestinal motility.
Nutrition is a diet low in fiber - one that is low in legumes, vegetables and fruits. Eating a large amount of fiber helps to normalize the beneficial intestinal microflora and establish regular stools.
Constipation can be caused by processed foods - fried foods, cakes, sweets, pastries, pasta and bread. Cheese also often causes constipation. If you suspect a particular food or foods are causing your bowel problems, start keeping a food journal to find out the cause of your constipation.
Dehydration , often due to insufficient water intake or excessive drinking of coffee and tea, can interfere with bowel movements. Certain medications can also cause dehydration, such as blood pressure diuretics.
Certain medications are known to cause constipation - allergy medications (diphenhydramine, loratadine, fexofenadine, etc.) and opiate drugs (hydrocodone, oxycodone, morphine, etc.) for chronic pain.
calcium and iron supplements can also contribute to constipation. Calcium in a daily dose of more than 1000 mg per day can cause constipation if you do not take enough magnesium with it. Similarly, constipation can be triggered by iron supplements, which are often taken for iron deficiency anemia (must be diagnosed by a doctor). However, taking iron with vitamin C may help iron absorption and prevent constipation.
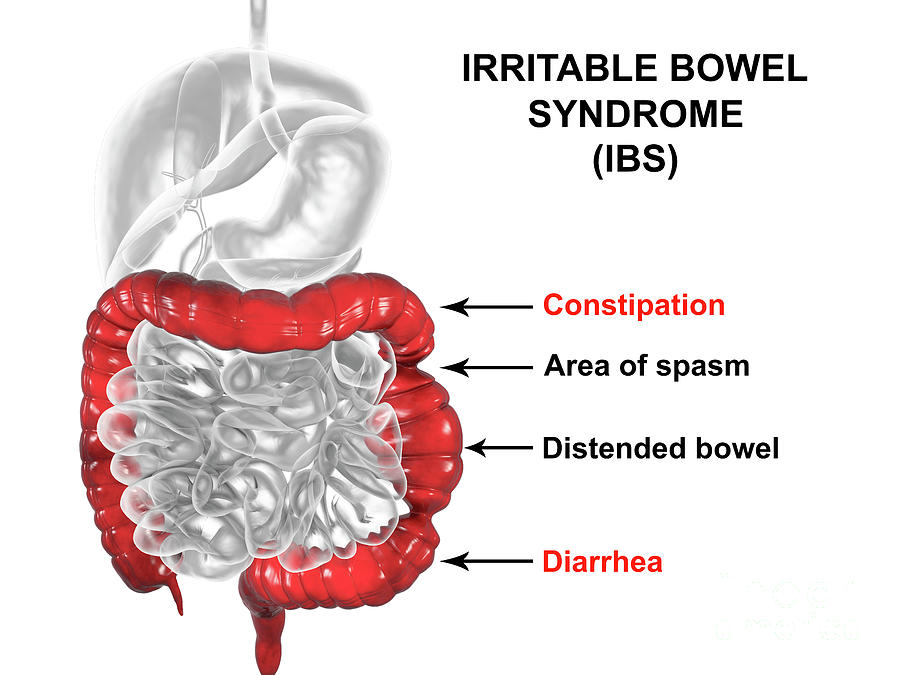
Irritable Bowel Syndrome (IBS) - IBS sometimes presents with diarrhea, but often with constipation. In some patients with IBS, constipation alternates with diarrhea. For those with predominantly constipated IBS, doctors often prescribe medication if diet and lifestyle changes are not enough.
Small Intestine Bacterial Overgrowth (SIBO) - According to some reports, an overgrowth of methane gas producing bacteria may increase the risk of constipation due to methane gas slowing intestinal transit time.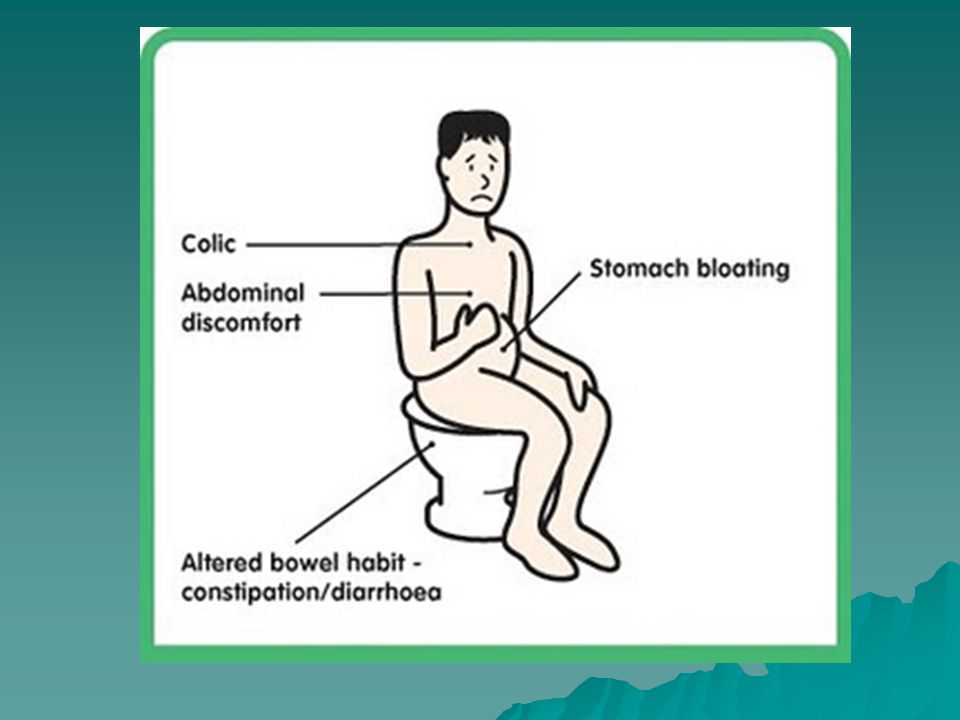
Hypothyroidism is a hypofunction of the thyroid gland, which affects up to 10% of the world's inhabitants. With this disease, the transit of food through the gastrointestinal tract slows down, which leads to constipation.
Frequent use of antibiotics - Disruption of the gut microbiome can be caused by antibiotics. In some cases, this causes diarrhea. In this case, the beneficial microflora is disturbed, which can lead to chronic constipation or SIBO, as mentioned above.
Stress - each of us reacts to stress in our own way. For some, stress can lead to constipation. To maintain mental and physical health, it is important to find a healthy way to reduce internal stress. As I said before, constipation comes from holding back in the literal sense of the word. Therefore, stress reduction, biofeedback and the restoration of a normal regime of work and rest will help to establish regular stools.
Chronic diseases such as Parkinson's disease, colon cancer, spinal cord injury, and sometimes even stroke can lead to chronic constipation.
Complications of chronic constipation:
- Pain during defecation
- Increased risk of diverticulosis (small pockets in the colon) and eventually diverticulitis (pocket infection)
- Blood in stool
- Development of hemorrhoids
- Leaky bowel (More)
- Increased exposure to intestinal toxins and bacterial growth in the intestines
- Difficulty urinating (due to pressure of stool on urethra)
Have you been tested for colon cancer?
Most doctors recommend that people over 50 get tested for colon cancer. This can be done with a colonoscopy, sigmoidoscopy, or a stool test to look for blood or DNA from cancer cells.
Those with a family history of colon cancer may need to be screened at age 40 or even earlier. Consult your doctor and review medical advice based on your age and family risk factors.
Prescription drugs:
If no underlying or reversible cause of constipation is identified, doctors often prescribe docusate sodium (Colace), polyethylene glycol (PEG or Miralax), lactulose (enulose), or sorbitol.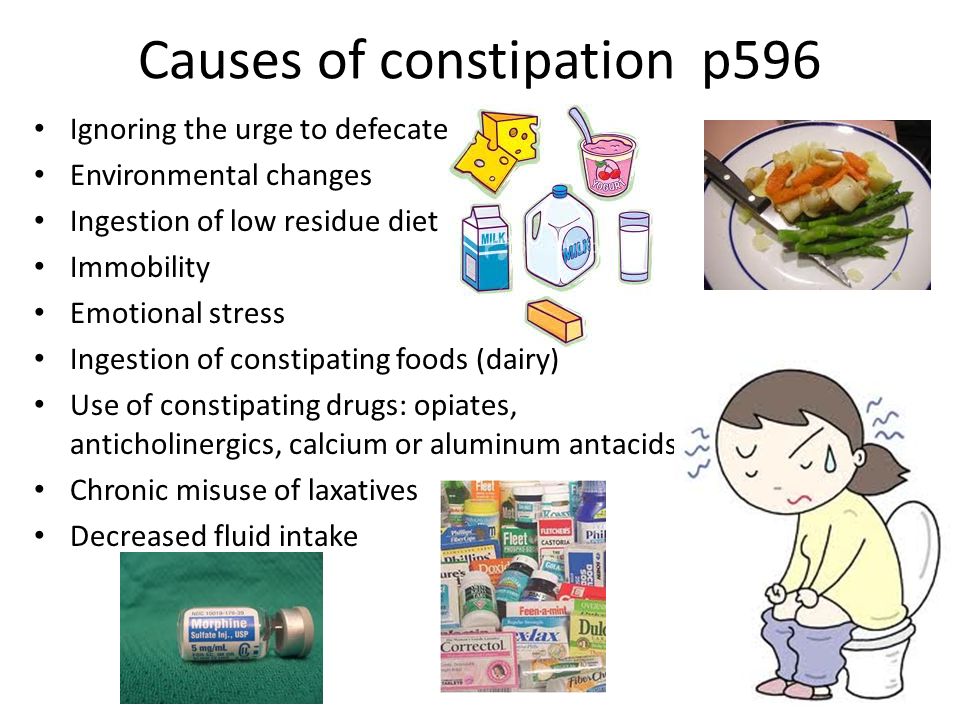
Other drugs for chronic constipation include linaclotide (Linzess, Constella), plecanatide (Trulance), and lubiprostone (Amitiza).
When constipation is caused by an opiate drug (constipation is a common side effect for this class of drugs), pharmaceutical companies have developed drugs (methylnaltrexone) to address this side effect.
Natural
Many people want to avoid prescription drugs because of the side effects they cause. Listed below are natural approaches to constipation that are preferred by many patients who want to relieve the symptoms of constipation and help the body establish regular bowel movements. The decisive factors underlying normal bowel function are diet and lifestyle. They are always worth starting with. However, sometimes this is not enough.
Physical education - to stimulate regular bowel movements, it is important to lead as active a lifestyle as possible. Doctors recommend that most people get at least 150 minutes of moderate physical activity a week.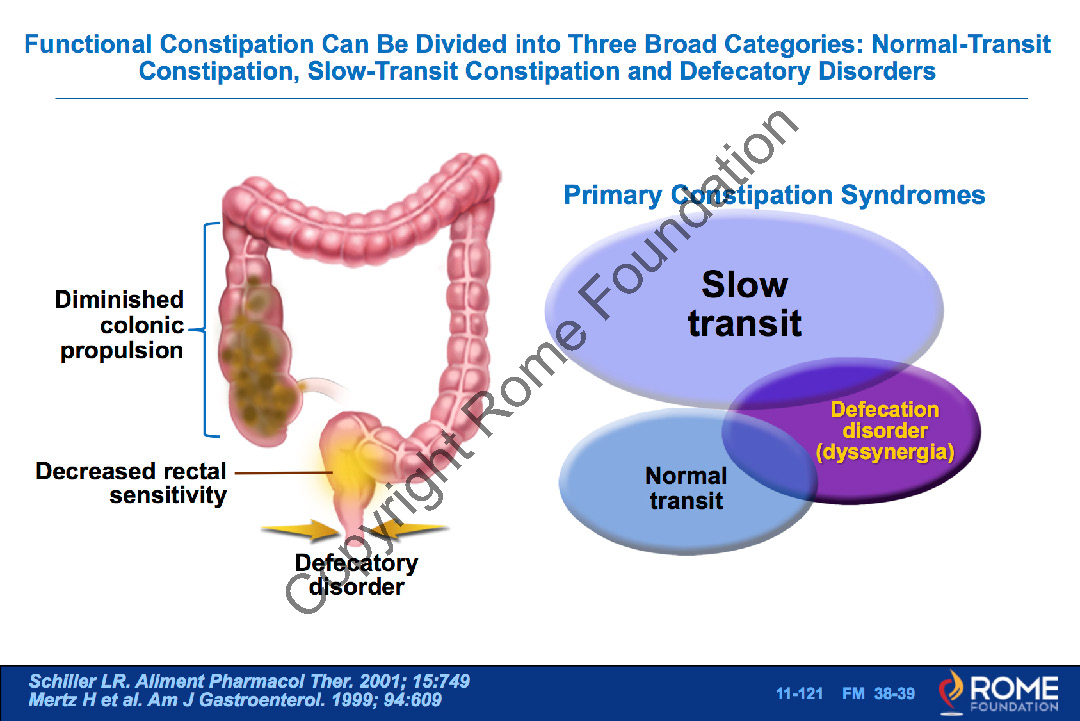 It contributes to normal functioning and regular bowel movements. A simple daily half-hour walk can be very beneficial for health. Some people find yoga helpful.
It contributes to normal functioning and regular bowel movements. A simple daily half-hour walk can be very beneficial for health. Some people find yoga helpful.
A lot of fiber in the diet is very important. Doctors advise eating at least 25 grams of fiber per day, for this you need to eat 5-9portions of fruits and vegetables. For example, one avocado has 13 grams of fiber, an average apple has 4 grams, and a banana has 3 grams. Berries are not only high in fiber, but they also help protect the body from colon cancer, according to a 2016 study published in Molecules. Chia seeds are also a good food - just one teaspoon of chia seeds contains almost 6 grams of fiber. A glass of black beans has as much as 15 grams of fiber.
Herbal products will help normalize stool frequency. Plant-based foods have a number of other health benefits, including increased absorption of vitamins A, K, and E, as well as vitamin C and other antioxidant-rich phytonutrients.
A 2015 study found that fiber is effective for mild to moderate constipation and for constipation caused by IBS. A diet high in plant foods is associated with a reduced risk of colon cancer and has a beneficial effect on beneficial gut microflora. A 2012 study published in the World Journal of Gastroenterology found that fiber helps increase stool frequency in adults.
A diet high in plant foods is associated with a reduced risk of colon cancer and has a beneficial effect on beneficial gut microflora. A 2012 study published in the World Journal of Gastroenterology found that fiber helps increase stool frequency in adults.
Products with probiotics - probiotics are beneficial bacteria. They can be very effective in restoring the balance of the gut microbiome, especially if the balance has been disturbed by antibiotics or chronic use of acid-reducing drugs.
Repopulation of healthy bacteria (such as lactobacilli, bifidobacteria) and other important and beneficial micro-organisms is important for overall health and constipation. A 2017 study published in Advances in Nutrition showed a downward trend in these vital bacteria in chronic constipation.
Eating sour-milk and fermented foods and drinks such as sauerkraut, miso soup, tempeh, yogurt, and kombucha can also be helpful in restoring this natural balance. A 2016 study in Iran found that constipated pregnant women improved with daily consumption of yogurt. Many also take probiotic supplements. We will talk about them a little later.
The best nutritional supplements for constipation
Magnesium - Magnesium is a ubiquitous trace mineral that is involved in over 350 biochemical reactions throughout the body. Magnesium deficiency is one of the most common nutritional deficiencies and can manifest as headaches, palpitations, muscle cramps, and even constipation.
Magnesium supplements can therefore be an effective remedy for those who suffer from constipation. If a laxative effect is observed while taking magnesium, the dosage of magnesium should be reduced. Patients with advanced kidney disease should consult their physician. A 2017 study published in Magnesium Research assessed the condition of patients undergoing open-heart surgery. Magnesium helped prevent not only constipation, but also arrhythmia, especially atrial fibrillation.
A study published in 2014 in Clinical Gastroenterology and Hepatology involved French women suffering from constipation. The researchers found that with daily intake of magnesium-rich mineral water, the symptoms of constipation were significantly reduced.
Vitamin C - Commonly found in citrus fruits and peppers. Vitamin C intake is important for the prevention of scurvy. Vitamin C helps with constipation.
Psyllium Husk - Psyllium husk can be very effective for chronic constipation. It can also help control blood sugar in diabetics. A 2018 study published in Complementary Therapies in Medicine found that constipated patients with type 2 diabetes not only lost weight, but also improved glucose control when taking psyllium husk. And a 2016 study published in Appetite found that taking psyllium husks contributed to feelings of fullness, which allowed subjects to not feel hungry between meals.
Prebiotics - Prebiotics are nutrients and/or foods consumed by beneficial gut bacteria. Introducing prebiotics such as inulin into the diet can provide a complete nutrition of beneficial intestinal bacteria, helping to restore a harmonious balance in the gastrointestinal tract.
Prebiotics include foods such as apples, asparagus, banana, barley, chicory root, dandelion greens, flaxseed, and garlic. Learn more about prebiotics.
A 2019 study demonstrated the benefit of optimizing prebiotic intake for the treatment of constipation. A similar 2017 study published in the American Journal of Medical Sciences found that a prebiotic, alone and in combination with probiotics, can help improve stool frequency and reduce symptoms of tension and bloating.
Probiotics - Over the years, many of my patients have noticed that their constipation is relieved when taking a probiotic. The authors of a 2017 study published in the Archives of Gerontology and Geriatrics compared a probiotic supplement with a placebo tablet and found that probiotics improved constipation in 10-40% of patients.
Another 2017 study of constipated Asian children found that probiotics helped increase bowel frequency. A 2018 study also demonstrated the effectiveness of probiotics in treating constipation in patients with Parkinson's disease.
Medicinal plants for constipation
Cascara sagrada (buckthorn ) - buckthorn is a medicinal plant that has been used for centuries as a remedy for chronic constipation. The name of the plant is translated as "sacred bark". This plant was an important healing agent among the indigenous peoples. Scientists have discovered that the active component of the plant is anthraquinone. It is this substance that has beneficial properties for the intestines.
Triphala - Triphala is often used as a remedy for constipation, but I have not been able to find any studies to support it specifically for constipation. What I did find, however, was research showing a positive effect of triphala on the gut microbiome, which may explain its effectiveness in treating constipation.
Aloe - Aloe cactus has been used for centuries for a variety of purposes in Asia and Mexico. There are many reports of its effectiveness in the treatment of chronic constipation. Studies proving the benefits of aloe were conducted back in 1974 (and the most recent - in 2008). Aloe can be taken as a juice or supplement.
Senna has been used for thousands of years. The effectiveness of senna was clearly demonstrated in a 2017 study of constipated children. Another 2018 study found that senna was not only effective, but also safe. It can be taken as a tea or dietary supplement.
Rhubarb - The Chinese have been using rhubarb for almost 3,000 years for medicinal purposes, particularly as a laxative. Modern science supports the ancient methods of using this plant. A 2018 study found that rhubarb may be helpful for people who become constipated while in the hospital. Rhubarb can be eaten raw or taken as a dietary supplement.
Others:
An ancient Ayurvedic medicine, a glass of warm milk with melted ghee, can be helpful. I recommend adding ghee to coffee or tea - such a drink is called armor-piercing coffee or tea.
Licorice Root Powder can also be helpful if mixed with warm water.
Prunes and prune juice is a well-known folk remedy for constipation, which is considered by many to be effective. A 2011 study found that prunes were more effective than psyllium for constipation.
You can also stimulate intestinal motility by regularly drinking a cup of warm herbal tea, such as black tea, chamomile tea, green tea, ginger tea, mint tea or senna extract.
Sources :
- Paré P, Fedorak RN. Systematic review of stimulant and nonstimulant laxatives for the treatment of functional constipation. Can J Gastroenterol Hepatol. 2014;28(10):549-57.
- Molecules. 2016 Jan 30;21(2):169. doi: 10.3390/molecules21020169.
- Aliment Pharmacol Ther. 2015 Jun;41(12):1256-70. doi: 10.1111/apt.13167. Epub 2015 Apr 22.
- Cancer Causes Control. 1997 Jul;8(4):575-90.
- World J Gastroenterol. 2012 Dec 28;18(48):7378-83. doi: 10.
3748/wjg.v18.i48.7378.
- Dimidi E, Christodoulides S, Scott SM, Whelan K. Mechanisms of Action of Probiotics and the Gastrointestinal Microbiota on Gut Motility and Constipation. Ad Nutr. 2017;8(3):484-494. Published 2017 May 5. doi:10.3945/an.116.014407
- Iran Red Crescent Med J. 2016 Oct 1;18(11):e39870. doi: 10.5812/ircmj.39870. eCollection 2016 Nov.
- Clinical Gastroenterology and Hepatology. 2014 Aug;12(8):1280-7. doi: 10.1016/j.cgh.2013.12.005. Epub 2013 Dec 14.
- Complementary Therapies in Medicine. 2018 Oct;40:1-7. doi: 10.1016/j.ctim.2018.07.004. Epub 2018 Jul 10.
- Appetite. 2016 Oct 1;105:27-36. doi: 10.1016/j.appet.2016.04.041. Epub 2016 May 7.
- Ohkusa T, Koido S, Nishikawa Y, Sato N. Gut Microbiota and Chronic Constipation: A Review and Update. Front Med (Lausanne). 2019;6:19. Published 2019 Feb 12. doi:10.3389/fmed.2019.00019
- Am J Med Sci. 2017 Mar;353(3):282-292. doi: 10.1016/j.amjms.2016.09.014.