Shallow hips in babies
Hip Dysplasia | Boston Children's Hospital
Listen
What is hip dysplasia?
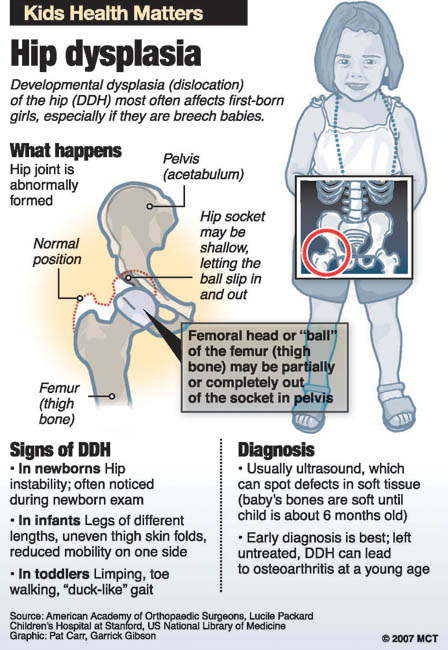
The hip is a ball-and-socket joint. Normally, the ball at the top of the thigh bone fits into the hip socket. Hip dysplasia occurs when the hip joint has not developed properly and the socket (acetabulum) is too shallow. This allows the ball (femoral head) to slip partially or completely out of the joint. Hip dysplasia ranges from a mild abnormality to a complete dislocation of the hip.
Severe cases of hip dysplasia are usually diagnosed during a routine screening within the first few months of a baby’s life. Other times, the problem may only become noticeable as a child grows and becomes more active.
Hip dysplasia is a treatable condition. However, if left untreated, it can cause irreversible damage that will cause pain and loss of function later in life. It is the leading cause of early arthritis of the hip before the age of 60. The severity of the condition and catching it late increase the risk of arthritis. Therefore, monitoring and early intervention are both important to reduce a child’s risk of pain and disability in adulthood.
Who is affected?
Hip dysplasia can affect anyone at any age. Although it is believed to develop around birth, a child with mild dysplasia may not have symptoms for years, or even decades.
- Hip dysplasia in babies is known as infant developmental dysplasia of the hip (DDH).
- When diagnosed in adolescents and young adults, it is sometimes called acetabular dysplasia.
The age at which older kids and young adults with hip dysplasia begin to notice symptoms depend on the severity of the condition and their activity level. Athletes who place a lot of load on their hips by participating in dance, hockey, football, soccer, or track and field may experience symptoms sooner.
Meet Louise
Undiagnosed hip dysplasia caused such severe knee pain, this former track star sometimes had trouble walking after competitions. With surgery behind her, and a degree in medicine in the works, she has returned to the sport she loves.
With surgery behind her, and a degree in medicine in the works, she has returned to the sport she loves.
Read her story
Girls and women are two to four times more likely than boys to have hip dysplasia. It also tends to affect first-born children and those who have a close family member with hip problems. Some people with hip dysplasia are affected in only one hip while others have it in both hips.
In boys, the condition tends to be accompanied by other hip problems. These include acetabular retroversion (when the hip socket grows too far over the head of the femur) or CAM lesions (extra bone growth on the surface of the bone that causes extra friction and joint damage).
Hip dysplasia is sometimes confused with hip impingement, which occurs when extra bone grow on the acetabulum or femoral head. The irregular shape creates friction within the joint and wears down cartilage. Some patients have both conditions, both of which cause hip pain and are easy to confuse. However, they are different issues that require different treatments.
However, they are different issues that require different treatments.
Image
Image
Generally speaking, treating hip dysplasia as early as possible can minimize joint damage and reduce the chance of early onset arthritis.
How we care for hip dysplasia
The Child and Young Adult Hip Preservation Program at Boston Children’s Hospital is at the forefront of research and innovation. We combine specialized expertise in non-surgical and surgical treatments with structured physical therapy to help children, adolescents, and young adults live healthy, active lives.
Our team has treated thousands of children with every level of complexity and severity of hip deformity. Our hip specialists have pioneered minimally invasive procedures as well as open surgical techniques to help treat patients of all ages. We perform more periacetabular osteotomy (PAO) procedures every year than any other hospital in the country and have helped hundreds of athletes return to the activities they love.
We have the experience to treat you or your child. Our goal is the same as yours: to help you get better so you can return to being healthy and pain-free.
Patient resources
Download these fact sheets to learn more about hip dysplasia and treatment options.
- fact sheet: developmental dysplasia of the hip (DDH)
- fact sheet: Pavlik harness
- fact sheet: hip dysplasia in adolescents and young adults
Hip Dysplasia | Hip Dysplasia in Adolescents
What is hip dysplasia in adolescents?
Hip dysplasia occurs when the hip socket (acetabulum) doesn't develop properly and is too shallow to cover the head of the thigh bone (femoral head) completely. Many adolescents and young adults with the condition were born with developmental dysplasia of the hip (DDH). In others, previously healthy hips did not develop properly as their bones and bodies grew.
Meet Alana and Nicole
A year and a half after hip surgery, Nicole still questioned her physical capabilities. That changed when she met Alana, another dancer who’d had the same surgery. This chance meeting became a turning point in both dancers' healing.
That changed when she met Alana, another dancer who’d had the same surgery. This chance meeting became a turning point in both dancers' healing.
Read their story
The condition ranges from a mild abnormality of the hip socket to a complete dislocation of the hip. As children become more active and demand more of their legs, the ill-fitting hip joint becomes unstable. The instability damages cartilage inside the joint that becomes increasingly painful over time.
It is important not to ignore hip pain. Hip dysplasia is a treatable condition but early diagnosis and treatment are critical to preventing irreversible damage.
What are the symptoms of hip dysplasia in adolescents and young adults?
Teens or young adults may develop a limp or have hip pain in the front of the hip or groin. For others, the first sign is knee pain. You might hear a clicking sound in your hip. As the damage progresses, you may find it more and more painful to participate in sports and other activities. Without treatment, the pain will continue to become worse.
Without treatment, the pain will continue to become worse.
What causes hip dysplasia in adolescents and young adults?
Some teens and young adults are born with mild DDH that becomes symptomatic as they grow. However, the hip joint continues to develop throughout the teen years and sometimes does not develop properly, even if you were not born with DDH. Doctors are not sure why this happens but they do know that the condition affects girls two to four times as often as boys. People with a close relative with hip problems are also at higher risk.
Image
Image
How is hip dysplasia diagnosed in adolescents and young adults?
Doctors typically use variety of tests to determine if dysplasia is the source of hip pain in adolescents and young adults.
The first step is a thorough patient history and physical exam. The doctor will check your hip for range of motion. They may order imaging studies such as an x-ray, MRI, or CT scan to confirm the diagnosis. Ultrasound-guided diagnostic injection can help your doctor determine the location of your hip pain with greater precision.
Ultrasound-guided diagnostic injection can help your doctor determine the location of your hip pain with greater precision.
How is hip dysplasia treated in adolescents and young adults?
The goal of treatment is to restore normal hip function and eliminate pain. Your treatment will depend on the severity of your condition.
Non-surgical treatment options for adolescents and young adults
Mild to moderate cases of hip dysplasia are often treated with physical therapy and nonsteroidal anti-inflammatory drugs (NSAIDs). If you continue to be in pain after these treatments, your physician may suggest surgery.
Surgical options for adolescents and young adults
Periacetabular osteotomy (PAO) is the main surgical treatment for adolescents and young adults with hip dysplasia. PAO may serve as a lifelong treatment if performed before serious damage occurs within the joint.
The goals of PAO are to:
- reduce or eliminate pain
- maximize the function of your hip
- enable you to return to sport or other activity
Hip Dysplasia | Hip Dysplasia in Babies
What is hip dysplasia in babies?
Hip dysplasia in babies, also known as developmental dysplasia of the hip (DDH), occurs when a baby’s hip socket (acetabulum) is too shallow to cover the head of the thighbone (femoral head) to fit properly. DDH ranges in severity. Some babies have a minor looseness in one or both of their hip joints. For other babies, the ball easily comes completely out of the socket.
DDH ranges in severity. Some babies have a minor looseness in one or both of their hip joints. For other babies, the ball easily comes completely out of the socket.
Image
What are the symptoms of hip dysplasia in babies?
Many babies with DDH are diagnosed during their first few months of life.
Common symptoms of DDH in infants may include:
- The leg on the side of the affected hip may appear shorter.
- The folds in the skin of the thigh or buttocks may appear uneven.
- There may be a popping sensation with movement of the hip.
What causes hip dysplasia in babies?
The exact cause is unknown, but doctors believe several factors increase a child’s risk of hip dysplasia:
- a family history of DDH in a parent or other close relative
- gender — girls are two to four times more likely to have the condition
- first-born babies, whose fit in the uterus is tighter than in later babies
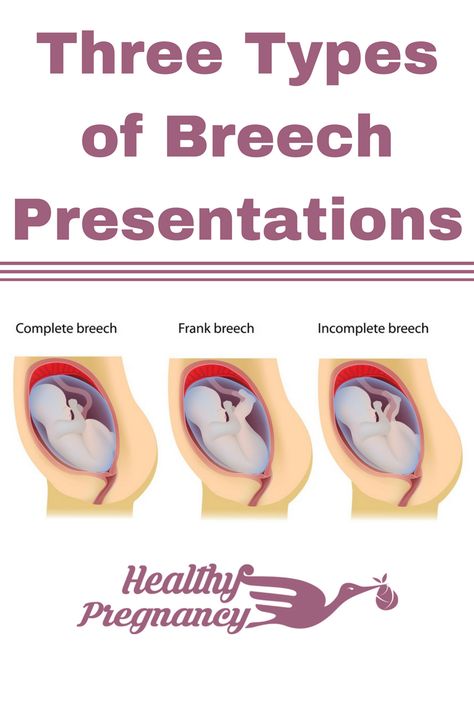
- breech position during pregnancy
- tight swaddling with legs extended
Breech position: Babies whose bottoms are below their heads while their mother is pregnant with them often end up with one or both legs extended in a partially straight position rather than folded in a fetal position. Unfortunately, this position can prevent a developing baby’s hip socket from developing properly.
Unfortunately, this position can prevent a developing baby’s hip socket from developing properly.
Tight swaddling: Wrapping a baby’s legs in a straight position may interfere with healthy development of the joint. If you swaddle your baby, you can wrap their arms and torso snugly, but be sure to leave room for their legs to bend and move.
Angela's story
Angela was 5 when her parents brought her to Boston Children’s Hospital, where she was diagnosed with hip dysplasia in both hips.
How is hip dysplasia diagnosed?
Infants in the U.S. are routinely screened for hip dysplasia. During the exam, the doctor will ask about your child’s history, including their position during pregnancy. They’ll also ask if there is any history of hip problems on either parent’s side.
The doctor will do a physical exam and order diagnostic tests to get detailed images of your child’s hip. Typical tests can include:
- Ultrasound (sonogram): Ultrasound uses high-frequency sound waves to create pictures of the femoral head (ball) and the acetabulum (socket).
 It is the preferred way to diagnose hip dysplasia in babies up to 6 months of age.
It is the preferred way to diagnose hip dysplasia in babies up to 6 months of age. - X-ray: After a child is 6 months old and bone starts to form on the head of the femur, x-rays are more reliable than ultrasounds.
How is hip dysplasia treated?
Your child’s treatment will depend on the severity of their condition. The goal of treatment is to restore normal hip function by correcting the position or structure of the joint.
Non-surgical treatment options
Observation
If your child is 3 months or younger and their hip is reasonably stable, their doctor may observe the acetabulum and femoral head as they develop. There’s a good possibility the joint will form normally on its own as your child grows.
Pavlik harness
If your child’s hip is unstable or sufficiently shallow, their doctor may recommend a Pavlik harness. The Pavlik harness is used on babies up to four months old to hold their hip in place while allowing their legs some movement. The baby usually wears the harness all day and night until their hip is stable and an ultrasound shows their hip is developing normally. Typically, this takes about eight to 12 weeks. Your child’s doctor will tell you how many hours a day your child should wear the harness. Typically, children wear the harness 24 hours a day.
The baby usually wears the harness all day and night until their hip is stable and an ultrasound shows their hip is developing normally. Typically, this takes about eight to 12 weeks. Your child’s doctor will tell you how many hours a day your child should wear the harness. Typically, children wear the harness 24 hours a day.
Image
While your child is wearing the harness, their doctor will frequently examine the hip and use imaging tests to monitor its development. After successful treatment, your child will need to continue to see the doctor regularly for the next few years to monitor the development and growth of their hip joint.
Typically, infants’ hips are successfully treated with the Pavlik harness. But some babies’ hips continue to be partially or completely dislocated. If this is the case, your child’s doctor may recommend another type of brace called an abduction brace. The abduction brace is made of lightweight material that supports your child’s hips and pelvis. If your child’s hip becomes stable with an abduction brace, they will wear the brace for about eight to 12 weeks. If the abduction brace does not stabilize the hip, your child may need surgery.
If your child’s hip becomes stable with an abduction brace, they will wear the brace for about eight to 12 weeks. If the abduction brace does not stabilize the hip, your child may need surgery.
Image
Surgical treatment options for babies
Closed reduction
If your child’s hip continues to be partially or completely dislocated despite the use of the Pavlik harness and bracing, they may need surgery. Under anesthesia, the doctor will insert a very fine needle in the baby’s hip and inject contrast so they can clearly view the ball and the socket. This test is called an arthrogram.
The process of setting the ball back into the socket after the arthrogram is known as a closed reduction. Once the hip is set in place, technicians will put your child in a spica cast. This cast extends from slightly below the armpits to the legs and holds the hip in place. Different casts cover differing amounts of the child’s legs, based on the condition of their hips. Children typically wear a spica cast for three to six months. The cast will be changed from time to time as your baby grows.
Children typically wear a spica cast for three to six months. The cast will be changed from time to time as your baby grows.
Open reduction
If a closed reduction does not work, your child’s doctor may recommend open-reduction surgery. For this, the surgeon makes an incision and repositions the hip so it can grow and function normally. The specifics of the procedure depend on your child’s condition but it may include reshaping the hip socket, redirecting the femoral head, or repairing a dislocation. After the surgery, your child will need to wear a spica cast while they heal.
Follow-up care
Any infant treated surgically for hip dysplasia must be followed periodically by an orthopedist until they have reached physical maturity. At regular visits, their orthopedic doctor will monitor their hip to ensure it develops normally as they grow. Diagnosing and treating any new abnormality early will increase the chance your child will grow up to be active free from hip pain throughout their childhood, the teen years, and adulthood.
Will treatment affect my child’s ability to walk?
Depending on their age during treatment, your child may start walking later than other kids. However, after successful treatment, children typically start walking as well as other kids. By contrast, children with untreated hip dysplasia often start walking later, and many walk with a limp.
Hip Dysplasia | Programs & Services
Departments
Centers
Programs
Hip Dysplasia | Contact Us
Developmental Dysplasia of the Hip (for Parents)
What Is Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip (DDH) is a problem with the way a baby's hip joint forms. Sometimes the condition starts before the baby is born, and sometimes it happens after birth, as the child grows. It can affect one hip or both.
Most infants treated for DDH develop into active, healthy kids and have no hip problems.
What Happens in a Hip With Developmental Dysplasia?
The hip joint is a ball and socket joint. The top part of the thighbone (the ball part of the hip) sits inside a socket that's part of the pelvic bone. The ball moves around in different directions, but always stays inside the socket. This lets us move our hips front, back, and side to side. It also supports our body weight for walking and running.
In DDH, the hip does not form well. The ball part of the joint may be completely, or partly, out of the socket. Sometimes the ball part may slide in and out of the socket. Often, the socket is shallow. If this is not fixed, the hip joint will not grow well. This can lead to pain with walking and hip arthritis at a young age.
What Are the Signs & Symptoms of Developmental Dysplasia of the Hip?
Developmental dysplasia of the hip doesn't cause pain in babies, so can be hard to notice. Doctors check the hips of all newborns and babies during well-child exams to look for signs of DDH.
Parents could notice:
- The baby's hips make a popping or clicking that is heard or felt.
- The baby's legs are not the same length.
- One hip or leg doesn't move the same as the other side.
- The skin folds under the buttocks or on the thighs don't line up.
- The child has a limp when starting to walk.
Babies with any of these signs should see a doctor to have their hips checked. Finding and treating DDH early usually means there's a better chance for a baby's hips to develop normally.
What Is Hip Laxity?
Many babies are born with hips that feel loose when moved around. This is called neonatal hip laxity. It happens because the bands of tissue that connect one bone to another, called ligaments, are extra stretchy. Neonatal hip laxity usually gets better on its own by 4–6 weeks of age and is not considered true DDH.
A baby's whose hip ligaments are still loose after 6 weeks might need treatment. So follow-up doctor visits for babies with hip laxity are important.
So follow-up doctor visits for babies with hip laxity are important.
Who Gets Developmental Dysplasia of the Hip?
Any baby can have DDH. But there's a higher chance of being born with it in babies who:
- are girls
- are first-born
- were breech babies (in the womb buttocks-down instead of head-down), especially during the third trimester of pregnancy
- have a family member with the condition, such as parent or sibling
Rarely, a baby isn't born with DDH, but develops it after birth. To prevent DDH in babies who aren't born with it, don't swaddle a newborn's hips or legs tightly together. Always make sure a baby's legs have plenty of wiggle room.
How Is Developmental Dysplasia of the Hip Diagnosed?
Doctors find most cases of DDH during well-child exams. If a baby has signs of DDH or has a higher risk for it, the doctor will order tests.
Two tests help doctors check for DDH:
- An ultrasound uses sound waves to make pictures of the baby's hip joint.
 This works best with babies under 6 months of age. That's because most of a baby's hip joint is still soft cartilage, which won't show up on an X-ray.
This works best with babies under 6 months of age. That's because most of a baby's hip joint is still soft cartilage, which won't show up on an X-ray. - An X-ray works best in babies older than 4–6 months. At that age, their bones have formed enough to see them on an X-ray.
How Is Developmental Dysplasia of the Hip Treated?
A pediatric orthopedic surgeon (a specialist in children's bone conditions) cares for babies and kids with DDH. The goal of care is to get the ball of the hip in the socket and keep it there, so the joint can grow normally.
The orthopedic surgeon chooses the treatment based on the child's age. Options include:
- bracing
- a closed reduction and casting
- an open reduction (surgery) and casting
A brace or cast will hold the hip in place and will be on both sides, even if only one hip is affected.
Bracing
Treatment for babies younger than 6 months old usually is a brace. The brace used most often is a Pavlik harness. It has a shoulder harness that attaches to foot stirrups. It puts the baby's legs into a position that guides the ball of the hip joint into the socket.
The brace used most often is a Pavlik harness. It has a shoulder harness that attaches to foot stirrups. It puts the baby's legs into a position that guides the ball of the hip joint into the socket.
Treatment with the Pavlik harness often lasts about 6–12 weeks. While wearing the harness, the baby has a checkup every 1–3 weeks with hip ultrasounds and exams. During the visit, the medical team can adjust the harness if needed.
The harness (brace) usually works well to keep the hips in position. Most babies won't need other treatment.
Rarely, the harness isn't able to keep the ball of the hip in the socket. Then, doctors might do either:
- a closed reduction (manually moving the ball back into the socket) and casting
- an open reduction (surgery) and casting
Closed Reduction and Casting
A child might need a closed reduction if:
- The harness was not successful at keeping the ball of the hip in the socket.

- A baby starts care after age 6 months.
For a closed reduction, the baby gets medicine (general anesthesia) to sleep through the procedure and not feel pain. The surgeon:
- Injects contrast dye into the joint to see the cartilagepart of the ball.
- Moves the baby's thighbone so that the ball of the joint goes back into place in the socket.
- Puts on a hip spica cast to hold the hip in place. The baby wears the cast for 2–4 months.
Sometimes, the orthopedic surgeon also loosens the tight muscle in the groin during the closed reduction.
Open Reduction (Surgery) and Casting
A child might need surgery (an open reduction) if:
- The closed reduction was not successful at keeping the ball of the hip in the socket.
- The child is older than 18 months when starting treatment.
During an open reduction, the child is asleep under anesthesia. The surgeon:
- Makes a cut through the skin.

- Moves muscles out of the way to see the hip joint directly.
- Puts the ball back into place.
- Closes the surgical cut with stitches placed under the skin. These won't need to be removed.
- Puts on a hip spica cast to hold the hip in place. The child wears the cast for 6–12 weeks.
Sometimes, the orthopedic surgeon also does a surgery on the pelvic bone to deepen a very shallow hip socket, especially for a child older than 18 months.
What Else Should I Know?
Kids will have regular checkups with their orthopedic specialist until they're 16–18 years old and done growing. These help make sure the hip develops well.
Hip Dysplasia ~【Treatment】
Hip dysplasia is a congenital disorder in the structure of the hip joint due to abnormal development of the joint. The disease occurs when the joint has not formed normally, and therefore does not work properly. With excessive mobility or stress on the joint due to the immaturity of its structure, dislocation can occur. Most often, the disease occurs in newborn girls, usually on the left side. To prevent the negative consequences of pathology, it is necessary to start treatment on time.
Most often, the disease occurs in newborn girls, usually on the left side. To prevent the negative consequences of pathology, it is necessary to start treatment on time.
Vidkriti Zgornuti
Classification
Pathologies of the hip joints are classified according to the degree of underdevelopment.
Hip dysplasia is divided into the following types:
- Acetabular - the acetabulum is affected, as a result, leg mobility worsens, pain and crunch in the thigh are observed.
- Femur - the articulation of the neck and head of the femur to the bone is disturbed, it is difficult for the patient to move the leg, turn it, changes in gait occur.
- Rotational - the anatomy of articular and bone tissues is disturbed in the horizontal plane. If the axes do not coincide, the limb turns inward.
The disease proceeds in several stages, among which:
- I — immaturity of articular tissues, which often affects newborns weighing up to 3 kg.
 The cause of the violation is the underdevelopment of the placenta, genetic predisposition, negative external factors during pregnancy.
The cause of the violation is the underdevelopment of the placenta, genetic predisposition, negative external factors during pregnancy. - II - predislocation, in which the femur is highly mobile, located in the cavity, but can slip out of it under intense impact.
- III - subluxation. There is a displacement of the head, but without falling out of the acetabular recess. The bone is highly mobile; a characteristic click is observed during movement.
- IV - dislocation. The femoral head comes out of the cavity, which requires mandatory reduction.
If treatment is not started on time, connective and adipose tissue will form in the joint cavity. Such compaction leads to complete immobility of the joint.
Vidkriti Zgornuti
Etiology and pathogenesis
The hip joint is formed in the womb. If a pregnant woman has any disorders in the body, this is also reflected in the development of the structure of the hip joint. One of the main causes of the disease is genetic predisposition. If the blood relatives of the baby have already encountered violations, then the risk of developing the disease in him increases 10 times.
One of the main causes of the disease is genetic predisposition. If the blood relatives of the baby have already encountered violations, then the risk of developing the disease in him increases 10 times.
Other causes of hip dysplasia:
- unfavorable ecology;
- use of hormonal drugs;
- baby's reaction to maternal hormones during pregnancy;
- breech birth, when the baby is born with legs instead of head;
- tight uterus that makes it difficult for the fetus to move;
- baby swaddling tight etc.
Vidkriti Zgornuti
In adults, hip dysplasia appears against the background of hormonal disorders and overload, as well as in the presence of chronic arthritis and arthrosis, bone growths near the articular cavity.
In a normal hip joint, the tip (head) of the hip bone fits snugly into the hip socket. A child with DTS has a shallow hip joint. As a result, the femoral head can slip out and protrude. A dislocation occurs. One limb becomes shorter than the other, and the patient develops lameness.
A dislocation occurs. One limb becomes shorter than the other, and the patient develops lameness.
Vidkriti Zgornuti
Symptoms and signs of DTS
Hip dysplasia may not cause symptoms until the person is a teenager or young adult. This makes timely diagnosis difficult. But still there are symptoms by which it is possible to determine the onset of the disease early.
Symptoms of hip dysplasia:
- limitation of movement;
- lameness, change in gait;
- crunching in the joints, stiffness;
- spinal instability;
- paroxysmal, prolonged pain in the pelvis, knee, thigh, radiating to the lower part of the body.
Vidkriti Zgornuti
Girls suffer from hip dysplasia more often than boys. In boys, this disease is usually accompanied by other hip problems. These include retroversion of the acetabulum, when the hip socket grows too far above the head of the femur, and other diseases.
Hip dysplasia is sometimes confused with hip impact, which occurs when extra bone grows on the acetabulum or head of the femur. The wrong shape causes friction in the joint and wears out the cartilage. Some patients have both conditions that cause hip pain and it is easy to confuse the two. However, these are different problems that require different treatments.
Vidkriti Zgornuti
Features of hip dysplasia in children
Only 2-3% of children are diagnosed with hip dysplasia after birth. In girls, pathology occurs 6 times more often. Therefore, already in the first hours of a child's life, a pediatric orthopedist-traumatologist without fail examines. The doctor must make sure that everything is in order with the newborn. And if any abnormalities in the hip joint are suddenly found, it is necessary to start treatment as soon as possible. But most often, hip dysplasia in infants does not have pronounced signs. The first symptoms appear only after a year. Therefore, often the doctor makes a diagnosis for almost one-year-old children.
Therefore, often the doctor makes a diagnosis for almost one-year-old children.
Symptoms of hip dysplasia, which indicate the possibility of the presence of pathology in newborns:
- Different sizes of folds on the skin.
The symptom is well manifested in children up to 3 months. Inguinal, popliteal and gluteal folds have different depths and shapes, the level of location is different. If their number is greater, subluxation or dislocation is possible. But not always, since the symptom can also occur in healthy children. - Hip shortening.
Sign of dislocation, occurs in a severe case. To detect a symptom, you need to put the baby on his back and bend his legs. If one knee is lower or higher than the other, a congenital dislocation is suspected. - Violation of hip abduction.
The sign is observed in babies up to 3 weeks. To determine the pathology, the child is laid on his back, the legs are spread apart. The presence of dislocation can be said if the angle of abduction is up to 50%.
The presence of dislocation can be said if the angle of abduction is up to 50%. - Marx-Ortolani symptom.
Informative test, also called "slipping symptom". The doctor lays the child on his back and slowly spreads his legs. For hip dysplasia, a push is characteristic when the head is reduced. If you let go of the leg, it will return to its original position on its own and at some point jerk sharply - a dislocation will occur. In a healthy baby, the limbs almost completely touch the surface during abduction. The sign is informative in a child up to 2 months.
The first signs of hip dysplasia in a child after a year appear when he begins to walk. The baby incorrectly leans on the feet, lameness is noted. With bilateral dysplasia, the gait resembles a "duck". At an early age, the disease can go away on its own. Pathology affects mainly the left thigh. At risk are first-borns, breech presentation of the fetus, toxicosis in the mother.
Vidkriti Zgornuti
Complications and consequences of hip dysplasia
In the absence of treatment or incorrect therapy, hip dysplasia worsens and leads to the following complications:
- muscular atrophy;
- chronic pain in the back and limbs;
- misalignment of the lower body;
- dysplastic coxarthrosis;
- gait deformities;
- impaired mobility of the back;
- neoarthrosis;
- curvature of the spine;
- lameness of varying severity and forms.

Vidkriti Zgornuti
Over time, a new, defective articulation may develop along with leg shortening and muscle atrophy. Such a joint performs some of the functions of the hip joint, but not all.
Vidkriti Zgornuti
Diagnosis of hip dysplasia
A preliminary diagnosis is sometimes made in the first hours after birth. The doctor necessarily examines the newborn to make sure that the baby is all right. Palpation and examination of the baby is carried out after feeding in a calm environment. To confirm the diagnosis, an additional study is prescribed, which includes the following procedures:
- Ultrasound - to determine the cause and localization of disorders;
- radiography - for adults and children older than one year;
- CT, MRI - to assess the state of the bone and ligament apparatus.
Diagnosis of hip dysplasia is carried out by the ratio of clinical manifestations and changes on ultrasound, x-rays. Since the skeletal system is not formed in young children, a special marking method is used for decoding. On pictures taken in the frontal projection, conditional lines are drawn to obtain the acetabular angle. Based on the data, the presence of violations is determined.
Since the skeletal system is not formed in young children, a special marking method is used for decoding. On pictures taken in the frontal projection, conditional lines are drawn to obtain the acetabular angle. Based on the data, the presence of violations is determined.
Vidkriti Zgornuti
Treatment of hip dysplasia
If DTS is diagnosed in early infancy, the problem can usually be corrected with a soft brace. Pathology can damage the cartilage lining the joint, as well as the soft cartilage (upper lip) that borders the articular part of the hip joint. This is called a tear in the upper lip of the thigh.
School-aged children and teenagers may need surgery to move the bones into the correct position for smooth joint movement.
Treatment for hip dysplasia involves reducing pain and protecting the hip joint from further damage. The doctor will select methods of treating hip dysplasia in accordance with the specific needs of the patient.
Conservative therapies include:
- Wide swaddling - fixing the baby's legs in a divorced state. The method allows to stop the progression of the pathology and eliminate the symptoms.
- Orthopedic structures - wearing Vilensky, Volkov splints, Freik pillows, Pavlik stirrups and other devices for fixing the legs. For children up to 4 months. constructions made of elastic materials that do not cause discomfort are used.
- Therapeutic children's massage - is prescribed from 10-15 sessions, then a break is made for a month. In total, 2-3 courses are shown. Massage is done daily and exclusively by specialists. The method is contraindicated in case of heart disease, elevated temperature, hernias. At home, you can gently massage the feet and lower back, pinch and rub the baby's body in the position on the stomach.
- exercise therapy for children - gymnastics is performed 2-3 times a day.
 Good efficiency was shown by the exercise of imitation of cycling and “patties”. Therapeutic exercise allows you to stabilize the structures of the joint and restore motor function. Exercises are selected only by a doctor. The course of treatment is 2 weeks.
Good efficiency was shown by the exercise of imitation of cycling and “patties”. Therapeutic exercise allows you to stabilize the structures of the joint and restore motor function. Exercises are selected only by a doctor. The course of treatment is 2 weeks. - Physiotherapy for children - electrophoresis with iodine, phosphorus, calcium, ozokerite compresses, UV therapy, a warm bath are prescribed. Procedures improve blood circulation, accelerate recovery, nourish tissues, strengthen and properly shape the joint.
- Closed reduction - the procedure is performed under anesthesia. Six months later, it is necessary to apply a plaster (coxite) bandage to fix the limbs in a divorced position. Then massage, physiotherapy, exercise therapy are prescribed.
Mud therapy is widely used, which warms up the joints, heals and reduces the manifestation of symptoms.
Vidkriti Zgornuti
Hip dysplasia: surgeries
In many cases, doctors reconstruct the hip joint with the following surgeries:
- arthroscopy, a minimally invasive procedure to repair a torn upper lip, the layer of cartilage around the hip joint;
- periacetabular osteotomy - movement of the femur into the hip socket;
- total hip replacement - reconstruction of the hip joint with an artificial joint.
Surgical therapy for hip dysplasia does not provide a 100% cure rate. There is a risk of incomplete recovery of hip joint functions, as well as postoperative complications, especially at the age of 30 years.
Vidkriti Zgornuti
Control of cure
After treatment, the child remains for 3-5 years at the dispensary until the end of growth. To monitor the changes and the correct development of HBS, ultrasound or radiography is performed 2 times a year. It is recommended to visit special orthopedic groups in kindergartens.
Adults should also visit a doctor to monitor the effectiveness of treatment. Therapy is considered successful if it was possible to eliminate the violations, to avoid the progression and complications of the pathology. With early diagnosis of the disease, 98% of children recover completely.
Vidkriti Zgornuti
Prevention of hip dysplasia
Most cases of hip dysplasia cannot be prevented. To reduce the risk of illness after childbirth, you must:
To reduce the risk of illness after childbirth, you must:
- avoid tight swaddling when hips and legs are tied together;
- regularly visit a pediatrician for examination, especially in the first 6 months of a child's life, because this way the pediatrician can detect pathology in time;
- choose special clothes for newborns with dysplasia that will keep the baby's legs apart, which promotes healthy development of the hip joints.
It is important for children to lead an active lifestyle and exercise. Teach your child to exercise from an early age.
Vidkriti Zgornuti
Tips and tricks
To avoid developing hip dysplasia in your baby, follow these simple tips:
- get an ultrasound scan during pregnancy at the right time;
- do not swaddle the baby too tight, wear sliders from birth;
- choose shoes with a hard heel;
- do not let a baby with foot problems jump in jumpers;
- Give your child vitamin D3 to prevent rickets.

It is important that children are examined by an orthopedic doctor every 3 months. This will help detect violations at an early stage.
Vidkriti Zgornuti
Q&A
Is it possible to do X-ray of the hip joints of a baby?
Hip dysplasia in a newborn is a congenital dislocation of the hip. The first diagnosis is carried out by a neonatologist immediately after birth by the maximum divorce of the legs. Also, dysplasia in newborns may appear later. The best way to diagnose bone pathologies is X-ray diagnostics. However, x-rays are not recommended for children aged 0 to 4 months.
Is it possible to play sports with hip dysplasia?
Hip dysplasia occurs when the baby has not yet developed a hip joint or has dislocated the femoral head at the time of birth. Accompanied by lameness and load on the spinal column. Conservative treatment includes therapeutic massage, exercise therapy for children. You can go swimming. But axial loads are not recommended.
You can go swimming. But axial loads are not recommended.
What is hip subluxation?
Hip dislocation - displacement of the femoral head relative to the socket, which is accompanied by damage to the joint capsule. With subluxation of the hip joint, displacement occurs in the region of the cavity without damaging the capsule. According to the degree of congenital underdevelopment of the hip joint, hip dysplasia is divided into three forms: acetabular, rotational, pathology of the upper thigh. To exclude pathologies, it is necessary to diagnose it at an early stage, which is possible with the help of radiography.
Vidkriti Zgornuti
The article is for informational purposes only. Please remember: self-medication can harm your health.
Vidkriti Zgornuti
The author of the article:
Sakhan Ruslan Vasilyevich
Orthopedist-traumatologist, pediatric orthopedic-traumatologist
Expert in the direction:
Kopeikin Igor Ivanovich
Orthopedist-traumatologist of the first category, pediatric orthopedic-traumatologist
Which doctor treats hip dysplasia?
DTS in adults is treated by an orthopedic traumatologist, in children by a pediatric orthopedic traumatologist. Our highly qualified specialists will examine with modern equipment and make an accurate diagnosis. You can get a detailed consultation and undergo a comprehensive effective treatment of hip dysplasia at the MEDICOM clinic.
Our highly qualified specialists will examine with modern equipment and make an accurate diagnosis. You can get a detailed consultation and undergo a comprehensive effective treatment of hip dysplasia at the MEDICOM clinic.
show more
Certificates
Reviews
23.02.2021 12:06
Sergey
I myself experienced joint replacement, now I feel just fine.
02/01/2021 17:33
Valeria Sidorova
Good service, excellent specialists. Thank you!
15.01.2021 12:39
Egor Petrov
Thank you, the information is really correct, there are more and more people with dysplasia every year.
28.12.2020 09:11
Voronina Katerina
My mother was operated on two times, if all the symptoms were described, unfortunately, I was only happy to change the snow, but not again.
11/19/2020 10:00
Olga Sergiivna
Supervisory service, miracle fahivtsy, thank you for those who work.
04.11.2020 15:51
Artur
Everything is written correctly, but you can describe more prophylactically in detail. How can dysplasia be saved, or zupiniti.
25.09.2020 20:06
Inessa Gladchenko
Until the age of 20 she was engaged in sports dancing, then a decree, another decree. I tried to stay in shape as much as possible. At the age of 40, pains in the thigh appeared, at first she managed with physiotherapy, then she could no longer live without painkillers. Today I'm getting ready for surgery. Sports do not always save.
Show 3 more
Total 7 reviews
leave feedback
symptoms and treatments at EMC
-
Diagnosis and treatment of eczema according to international protocols
-
Dermatologists with experience and long-term internships in leading clinics in Israel and Western Europe
-
Opportunity to obtain a second opinion from the world's leading experts in the treatment of eczema
-
We help even in the most difficult cases
Treatment of eczema
In each case, for the correct selection of therapy, preliminary diagnosis is necessary, which may include immunological, allergological, biochemical methods and microbiological examination. If necessary, consultations of narrow specialists (therapist, endocrinologist, gastroenterologist, psychotherapist, etc.) are held.
If necessary, consultations of narrow specialists (therapist, endocrinologist, gastroenterologist, psychotherapist, etc.) are held.
Comprehensive personalized treatment is prescribed taking into account the characteristics and degree of skin lesions and always includes the use of antihistamines.
When prescribing therapy, the doctor also takes into account the gender and age of the patient, medical history, the results of previous treatment, and individual intolerance to drugs. The key factors are the stage and prevalence of the disease.
What is eczema?
Eczema is a chronic inflammatory skin disease characterized by itching, redness and rashes in the form of small fluid-filled vesicles. Rashes resemble air bubbles that form when water boils. Hence the name of the disease (from the Greek eczeo - boil).
Eczema is not transmitted from person to person. This is a genetically determined disease. Eczema is quite common, it is diagnosed in about 30-40% of patients who visit a dermatologist.
What does eczema look like and on what parts of the body does it appear
Weeping and itchy skin on the face and hands
Rashes on the skin in the form of vesicles and bumps, accompanied by redness, may be manifestations of true eczema. Subsequently, the bubbles open with the release of serous fluid, in their place shallow point erosions (ulcers) form. The released liquid dries up with the formation of a soft crust.
The appearance of repeated rashes in the area of the pathological focus leads to the simultaneous localization of vesicles, sores, and crusts on the skin. All rashes are accompanied by severe itching, which causes significant discomfort to the patient and reduces the quality of life. Sometimes nighttime itching causes insomnia.
Eruptions are characterized by symmetry, the absence of clear boundaries near the affected area.
The rash tends to spread to the chest, trunk, abdomen and back.
Scaly layer on the border of the scalp
Seborrheic eczema often develops on the scalp. In the initial stages, it manifests itself as single yellowish nodules, the number of which increases rapidly. The nodules turn into spots with the formation of whitish scales on the surface.
In the initial stages, it manifests itself as single yellowish nodules, the number of which increases rapidly. The nodules turn into spots with the formation of whitish scales on the surface.
Due to the fusion of foci of rashes on the border of the hair, a “seborrheic crown” is often formed - a scaly ring, along the edges of which there are areas of hyperemic skin. Without treatment, this form of scalp eczema spreads to the behind the ear and neck.
Some doctors consider seborrheic eczema to be just a variation of true seborrhea with minor differences in the course of the pathological process.
Round rashes on the skin of the hands
Itchy rashes on the hands can indicate many different diseases. Eczema is one of them, in 80% of cases true eczema is localized on the hands.
Rashes at the initial stage have rounded outlines, with the development of the disease, the contours lose their correctness. A similar nature of rashes on the hands is also characteristic of mycotic eczema.
Microbial eczema on the hands is rare and is characterized by the formation of purulent crusts on the surface.
Rashes with clear edges on the legs
Due to the increased frequency of skin trauma and chronic venous insufficiency, post-traumatic and microbial eczema most often appear on the legs. In 75% of cases, they occur in women. Rashes are often located next to varicose veins, have a rounded shape and clear boundaries.
Often, microbial eczema is manifested by many separate rounded foci up to 3 cm in size. Due to the similarity with a scattering of coins, this form of eczema is called coin-shaped.
Symmetrical scaly rashes on the body
Symmetrical rashes are characteristic of true eczema. In most cases, it primarily appears on the limbs, but sometimes the foci initially form on the trunk.
In the early stages, lesions are typical and consist of fluid-filled vesicles. With a long course, in place of weeping foci, areas of compacted skin appear with increased skin pattern. In chronic eczema, the lesions become covered with flaky skin during healing, eczema becomes dry.
In chronic eczema, the lesions become covered with flaky skin during healing, eczema becomes dry.
Fine-grained eruptions on the palms and soles
Eczema may affect the skin of the palms and soles. In these cases, due to the structural features of the skin, foci of eczema appear as small whitish bumps. The bumps come together to form blisters that can open. After opening, large sores remain on the palms and feet, releasing serous fluid.
Callus-like rashes on the palms
Callus-like rashes on the palms, appearing in places uncharacteristic of corns, may indicate tylotic eczema. Bubbles form, but may not open due to the structure of the skin.
Tylotic eczema usually accompanies true eczema, therefore, when corn-like rashes appear, it is recommended to pay attention to other parts of the body.
Multiple vesicles in the axillary region with a hair in the center
A rash with a hair in the center is a sign of sycosis - a special lesion of the hair follicles. Eruptions of this kind, located outside the scalp, are called sycosiform eczema. Eczema is also indicated by the itching that accompanies the rash. In addition to the axillary region, this type of eczema can be localized on the chin, upper lip and pubic area.
Eruptions of this kind, located outside the scalp, are called sycosiform eczema. Eczema is also indicated by the itching that accompanies the rash. In addition to the axillary region, this type of eczema can be localized on the chin, upper lip and pubic area.
Indurations on the skin of the hands and on the body
Induration of the skin may indicate the transition of eczema into a chronic form. Additionally, a decrease in weeping and the appearance of large areas of thickened, scaly skin indicate the chronicity of the disease.
Areas of depigmentation after peeling on the skin
Usually appear during the recovery phase. At the site of the rash, the skin is lighter. Most often, such light spots disappear on their own within a month.
Areas of depigmentation appear after most types of eczema, but more often after true and microbial.
Multiple bumps on the face and hands without weeping and crusts
Sometimes with true eczema, the vesicles do not open, but appear only as multiple bumps and papules. This is how pruriginous eczema manifests itself - one of the varieties of true eczema. Pruriginous eczema is localized on the extensor surfaces of the hands and on the face.
This is how pruriginous eczema manifests itself - one of the varieties of true eczema. Pruriginous eczema is localized on the extensor surfaces of the hands and on the face.
Itchy areas of redness on the skin of the legs and arms
A hyperemic and itchy area of the skin with many rashes indicates true or microbial eczema. The most pronounced pruritus in eczema is manifested at the stages of active formation of fresh papules and vesicles. Itching is aggravated by the addition of bacterial flora.
With varicose and post-traumatic eczema, these symptoms are observed in most cases on the legs. In occupational eczema, itching and flushing are typical signs. The severity of symptoms increases after repeated contact with the provoking agent. After the provoking factor is eliminated, the symptoms disappear.
Suppuration and itching around the wounds on the legs and arms
Hyperemia of the skin and the formation of purulent crusts indicate microbial eczema. Most often they appear on areas of the skin that are most susceptible to injury.
Most often they appear on areas of the skin that are most susceptible to injury.
When the pus dries out, rough crusts form, which fall off, exposing the skin that continues to become wet.
Types of eczema
Understanding the types of eczema is essential for correct treatment.
True or idiopathic eczema.
Characterized by a classic course, rashes go through all six stages.
Stages of true eczema:
First stage . It is characterized by wide foci of hyperemia with a red-blue tint and blurred edges without clear boundaries.
Second stage - papules. Soft nodular connections appear, merging into small foci. In places, swelling and plaques appear.
The third stage is vasculotic. The nodules gradually turn into bubbles.
Fourth stage . The accumulation of subcutaneous exudate causes the opening of papules and the release of serous fluid. Point foci of maceration with depressions (wells) appear on the skin. At this stage, the development of the disease reaches its peak.
Point foci of maceration with depressions (wells) appear on the skin. At this stage, the development of the disease reaches its peak.
The fifth stage is crusty. The secreted serous fluid begins to dry out, the forming crusts are layered on top of each other.
The sixth stage is squamous. Dried whitish scales separate on their own, the skin is restored. In places of the rash, pink or whitish spots may remain.
It is serous wells that are the main distinguishing feature of true eczema. Foci of inflammation are often located in a symmetrical order. The first symptoms appear on the face and hands, then the disease spreads to other parts of the body. Severe itching and soreness joins in places where ulcers form.
Without treatment, the process quickly flows into the chronic stage, when even during the period of remission, the foci of rashes are excessively compacted, a pronounced linear pattern appears on the skin.
Chronic eczema
The acute stage of true eczema can quickly turn into a chronic one. It is characterized by compaction and coarsening of endogenous foci. New rashes actively appear, followed by infiltration and the formation of serous wells. Itching increases many times and does not stop even at night, so patients with chronic eczema often suffer from insomnia. After getting rid of the symptoms in the affected areas, pigmentation is disturbed, dry skin appears.
It is characterized by compaction and coarsening of endogenous foci. New rashes actively appear, followed by infiltration and the formation of serous wells. Itching increases many times and does not stop even at night, so patients with chronic eczema often suffer from insomnia. After getting rid of the symptoms in the affected areas, pigmentation is disturbed, dry skin appears.
Exacerbations are more common in winter.
Microbial eczema
Caused by infectious or fungal agents. It occurs at the stage of opening papules with true eczema or with chronic ulcerative-vegetative pyoderma, in places of fistulas, wounds, etc.
Pathogenic foci have clear pink borders. In addition to papules and weeping erosions, from which fluid is released, there is a layering of purulent crusts. The size of the affected areas increases rapidly. Often, separate pustules with scaly areas form near the foci.
Depending on the source of the disease, microbial eczema is divided into nummular and varicose.
Coin-shaped eczema
The name is due to the appearance of red spots that resemble coins in shape. Education may not take place for a long time (from a month to several years). In most cases, symptoms begin to appear on the inner thigh and outer side of the hands.
In addition to blisters of a red-pink, sometimes bluish tint, there is a strong itching and burning, weeping is noted after the opening of the rash.
Varicose eczema
Primarily develops on the legs. Accompanied by moderate itching, increased dryness of the skin, scaly formations in the localization of dilated venous vessels. The disease greatly affects the condition of the skin - edematous, hyperemic foci with a burgundy-violet tint appear. Specific dark spots appear on the skin.
Small blisters also form on the skin, which break open with the release of fluid and the formation of ulcers. The weeping stage passes into the drying stage after about two weeks. Outgrowths are formed by the type of crusts. Pathological foci thicken and darken, up to brown. There is pain when pressed.
Outgrowths are formed by the type of crusts. Pathological foci thicken and darken, up to brown. There is pain when pressed.
The inflammatory process is accompanied by severe itching. The patient combs the foci of inflammation, as a result of which abrasions and cracks form on the skin, there is a risk of secondary infection.
Seborrheic eczema
The trigger of this type of eczema is the weakening of local immunity, dysfunction of the sebaceous glands, malnutrition of the scalp. Most patients have a history of congenital allergic reactions.
Each person has the fungus Pityrosporum ovale as part of the hairy epithelial layer. In case of failures in the protective function, it can penetrate deeper, in response, local immunity reacts in the form of an allergic reaction. The inflammatory process begins in the form of local edema. Normally, it stops after the treatment of the fungus, but with seborrheic eczema, the inflammatory process is more pronounced and lasts a long time.
A feature of seborrheic eczema is excessive activity of the sebaceous glands in the lesions. There is a gluing of thinned skin scales and the formation of yellow fatty flakes.
Localization of rashes:
-
trunk: umbilical region, chest, around the halo of the mammary glands, in the folds of the axillary and inguinal zones;
-
head: nasolabial fold, ears and behind the ears, eyebrows, chin, eyelashes, scalp.
Dry eczema
In the initial stages, patches form with blurred pink edges, later the contours turn red. Sharp papules appear, merging into large plaques.
Blisters do not form, but skin breaks down. The upper thin and dry layer peels off, forming small and deep cracks. Without treatment, the disease progresses and becomes acute with weeping, the formation of dense crusts and severe redness. In this case, the patient may not experience pain.
The disease worsens in dry and cold seasons.
Allergic eczema
Is the result of the body's hypersensitivity to external or internal stimuli. More often develops in patients with a weak immune response.
The main factor is contact with foreign compounds that cause excessive production of histamine.
Any manifestation of the disease causes excitation of the nervous system, so the patient experiences irritation, may suffer from insomnia and severe headaches.
Symptoms:
-
rash accompanied by itching,
-
dryness and flaking of the skin,
-
Crusts form at the site of opening blisters,
-
reddening of the skin, burning sensation,
-
thickening of the skin in the eyes of the lesion.
Allergic eczema is divided into dry and weeping. The first type is characterized by dry, flaky skin. The trigger may be direct contact with the allergen or the presence of internal diseases.
The first type is characterized by dry, flaky skin. The trigger may be direct contact with the allergen or the presence of internal diseases.
The second type is more often localized on the hands and occurs due to direct contact with the chemical. At the same time, the skin swells strongly, red foci appear with small papules, which, after opening, turn into painful ulcers.
Eruptions in this type of eczema can appear on any part of the body.
Dyshidrotic eczema
Dyshidrosis affects the sweat glands of the feet (in 20% of cases) and hands (80%), has a chronic course with seasonal exacerbations. Serous vesicles form on the affected areas.
The hallmark of dyshidrosis is the development of vesicles. The rashes are covered with a dense membrane. Purulent discharge appears only when a secondary infection is attached. Under normal conditions, the formations contain a clear liquid.
All stages are accompanied by gradually increasing itching. The lesions are swollen and flaky. Vesicles open themselves, or in the process of combing or damage, small wounds and cracks appear in their place. The skin pattern becomes more distinct.
The lesions are swollen and flaky. Vesicles open themselves, or in the process of combing or damage, small wounds and cracks appear in their place. The skin pattern becomes more distinct.
In this type of eczema, itching appears before skin symptoms, rashes form later, first on the lateral areas of the fingers, then on the palms and feet.
Weeping eczema
This species is characterized by several phases. The first phase: pink spots of various shapes and sizes appear on the skin, swelling, as well as papules or vesicles. Due to the constant release of subcutaneous exudate, weeping zones are formed.
Opening, formations are covered with crusts with active exfoliation. A feature of this type is that the rash is at different stages of development. In one zone, new and already opened rashes can be located, and rejection of dead cells is also observed. Severe itching causes insomnia and neuroses.
When the process is chronic, the skin in the affected areas thickens and scars, a blue-red tint appears. During the period of remission, the skin in the lesions constantly peels off.
During the period of remission, the skin in the lesions constantly peels off.
Symptoms
Symptoms of eczema may vary depending on the type of disease, but there are common symptoms:
-
regular fever in occupational eczema;
-
the appearance of a focus of inflammation and redness, thickening of the skin;
-
appearance of rash;
-
increased sensitivity of the skin, the appearance of itching, which reduces the quality of life of the patient;
-
the appearance of painful cracks, wounds, erosion at the site of the rash, the formation of serous or hemorrhagic crusts;
-
increased dryness of the skin, loss of elasticity during remission.
Eczema has very specific manifestations even with a small area of rash. In adults, it usually affects large areas of the body, most commonly on the arms, shoulders, face, feet, and lower legs. Eczema can also occur against the background of swelling and redness of the skin.
In adults, it usually affects large areas of the body, most commonly on the arms, shoulders, face, feet, and lower legs. Eczema can also occur against the background of swelling and redness of the skin.
Eczema is difficult to treat, frequent relapses are possible, but thanks to modern protocols, doctors are increasingly able to achieve stable remissions. It is important to consult a doctor in a timely manner.
Eczema on the face
City air, climate, improper care can have a negative effect on the skin. If you notice itchy, swollen reddish spots on your face with rashes in the form of bubbles that burst, forming crusts, and the crusts then merge into a large weeping spot, urgently make an appointment with a dermatologist. This is especially true, given that eczema is accompanied by severe burning and itching.
The disease is characterized by symmetry, if rashes appear on one side of the face, they will appear on the other. Eczema can affect the mouth and eyes. The skin on the eyelids thickens and coarsens, itching and peeling appear. Lamellar scales form on the lips, which then turn into bleeding painful cracks.
The skin on the eyelids thickens and coarsens, itching and peeling appear. Lamellar scales form on the lips, which then turn into bleeding painful cracks.
True, seborrheic and occupational eczema appears on the face. The symptoms are largely similar. Separate areas on the face swell and turn red, then small itchy vesicles appear, filled with a clear or cloudy liquid. Cracks form on the skin, it begins to peel off.
True eczema is distinguished by symmetrical rashes, seborrheic eczema appears on the scalp, and professional eczema occurs in places of direct contact with the irritant.
Eczema on the legs
Often, eczema on the legs appears as a result of an allergic reaction and the presence of vascular pathology of the lower extremities (varicose eczema). Psycho-emotional state and reduced immunity can also be triggers.
Most often, microbial eczema appears on the legs. It is localized in places of burns, postoperative sutures, fungal infection, varicose veins. Eczema occurs against the background of an already existing inflammatory process.
Eczema occurs against the background of an already existing inflammatory process.
Main symptoms of eczema on the legs:
-
swelling of the legs;
-
the appearance of a characteristic crust;
-
sore and dry skin;
-
the appearance of bubbles, cracks and pigmentation in places of localization.
Possible sleep disturbances and headache.
Self-treatment of eczema is unacceptable. It can lead to the development of complications and complicate the treatment process.
Eczema on the hands
According to the intensity of the development of the disease on the hands, acute and chronic eczema can be distinguished.
Depending on triggers:
-
microbial (affects areas around wounds, abrasions, boils),
-
professional,
-
dyshidrotic (affects palms, nails), horny (may appear in the form of calluses).

There is a childhood eczema that appears as a severe rash on the hands and may go away with age.
There are 4 stages of the disease:
-
Erythematous - swelling and redness of the focus.
-
Papulovesicular - the appearance of rashes.
-
Moist - opening of the bubbles.
-
Cortical - formation of crusts.
When the disease passes into the chronic stage, the skin becomes rough, pigmentation, peeling, dryness appear.
Causes of the disease
Hereditary factor is the main cause of eczema . If there are cases of eczema in close relatives, the patient is at times more likely to develop this disease.
One of the provoking factors is immune disorders. The immune system begins to produce immunoglobulins to its own skin cells, which leads to the appearance of areas of inflammation. Violation of intercellular immunity is confirmed by an imbalance of glycoproteins: laboratory values of IgG and IgE are above normal, IgM is in short supply.
Violation of intercellular immunity is confirmed by an imbalance of glycoproteins: laboratory values of IgG and IgE are above normal, IgM is in short supply.
There is a connection between exacerbations of eczema and stress.
It has been scientifically proven that eating habits and gastrointestinal disturbances can also influence the development of eczema.
How to treat eczema
Weeping eczema
Weeping eczema character for all types of eczema. After the diagnosis, the dermatologist will create a personalized treatment plan, including:
- Drug treatment:
a) general;
b) local.
-
Physiotherapy.
-
Dieting.
The goal of treatment is to diagnose and eliminate the cause of the disease.
Dry eczema
Dry eczema is manifested by excessive dryness of the skin. Features are:
Features are:
-
chronic course;
-
seasonal exacerbations;
-
localization on any part of the skin, but most often on the limbs.
Dry eczema on the hands is often a sign of liver or gastrointestinal disease. It can also appear due to frequent stress. But the main factor is genetic predisposition.
In treatment, adherence to therapy is extremely important, all activities prescribed as part of the treatment plan must be fully implemented. Treatment should not be interrupted at the first sign of improvement.
A good effect in the early stages of eczema is shown by corticosteroids in the form of an ointment. But they are not recommended for long-term use. To eliminate the symptoms in the future, emollients are used.
The attending dermatologist can recommend consultations of specialized specialists: endocrinologist, gastroenterologist, etc. A multidisciplinary approach improves the results of therapy.
A multidisciplinary approach improves the results of therapy.
Treatment of eczema with medicines
The development of eczema is associated with increased sensitivity of the body to a number of irritants. Therefore, treatment should be systemic with the appointment of hormonal ointments, antihistamines, antibiotics. The doctor's task is to select the most effective drugs in each case.
Sorbents and antihistamines
Antihistamines help to get rid of itching and inflammation.
Antibacterial therapy
Antibiotics with tetracycline should be used with caution in children under 10 years of age. Laboratory diagnostics helps the doctor determine the safest drug.
Anti-itch and sedatives
-
moisturizers;
-
oral substances;
-
intravenous corticosteroids.
Among sedatives, Novopassit, Persen, Valemidin are more commonly prescribed.
Hormonal preparations
Therapeutic regimens include hydrocortisone. Hormonal preparations are recommended in the form of ointments, tablets, lotions. These drugs are not recommended for use for more than 2 weeks due to possible complications.
Corticosteroid-based creams are effective for weeping eczema because they dry out the skin. Ointments have a healing effect and eliminate rough crusts. When localized in the scalp, emulsions and lotions with a light texture are used.
Antiseptic and anti-inflammatory drugs
Antiseptic drugs are used to exclude additional complications and disorders:
Features of the treatment of eczema on the hands
For local treatment of eczema, ointments (pastes and creams) with corticosteroids, hormones with a pronounced anti-inflammatory effect, are used. They can reduce the inflammatory response and accelerate the process of skin regeneration.
Corticosteroid ointments have side effects: thinning of the skin, increased risk of bacterial and fungal infections, etc. Therefore, they should only be prescribed by the attending physician.
There are non-hormonal preparations that are also effective in treating eczema. These are topical calcineurin inhibitors - tacrolimus ointment (Protopic) and pimecrolimus cream. They reduce inflammation and itching. The dosage and duration of administration should also be determined only by the attending physician.
In severe eczema, extensive foci of inflammation and the absence of the effect of local therapy, systemic treatment is prescribed in the form of immunosuppressants - medicines that suppress the immune system.
In case of severe course of the disease, as well as in case of erythroderma, cytostatics are prescribed.
Antibiotics and antifungals are used to treat microbial and fungal eczema.
Features of the treatment of eczema on the legs
Eczema on the legs often develops as a result of an allergic reaction or severe vascular pathology (varicose eczema). Additional provoking factors may be weakened immunity and prolonged psycho-emotional stress.
Additional provoking factors may be weakened immunity and prolonged psycho-emotional stress.
Most often, microbial eczema develops on the legs. The main localization in places of burns, postoperative sutures, fungal infection, varicose veins. Eczema develops against the background of an already existing inflammatory process.
Main symptoms of eczema on the legs:
Sleep disturbances and headache may occur.
If you see a doctor in time, the prognosis for the treatment of eczema on the legs is favorable.
What is the treatment for eczema
The essence of the treatment of eczema is:
-
exclusion of contact with irritants,
-
proper nutrition,
-
itching,
-
local treatment with ointments and creams,
-
General treatment with tablets and injections.

The treatment of eczema in children is no different from that in adults. Often, the treatment plan includes physiotherapeutic methods that allow you to act directly on the damaged areas.
Dermatologists, through a combination of different methods, develop the best treatment for each patient.
Treatment of eczema in children
To determine the tactics of treatment, it is necessary to establish the type of eczema, the cause of its occurrence and differentiate it from other dermatological diseases (herpes rash, diathesis, allergic reactions, urticaria, lichen, etc.).
Diagnosis includes:
-
complete blood count;
-
skin scraping for examination under a microscope;
-
allergy tests for atopic eczema to identify the source of the allergy;
-
histological examination - for the diagnosis of autoimmune diseases.

Treatment is selected taking into account the results of examinations, the age and characteristics of the health status of a small patient.
Comprehensive therapeutic treatment includes:
-
Individual diet
-
Sedatives (for the regulation of sleep)
-
Antihistamines (for itching and burning)
-
Anti-inflammatory drugs (to relieve swelling of the skin and improve general condition)
-
Multivitamins
-
Antibiotics or antivirals
May be used as an alternative to some medications to speed up recovery processes physiotherapy .
Mandatory antiseptic treatment of wounds and abrasions to exclude secondary infections.
It is especially important to properly care for the child's skin and follow all the recommendations of a dermatologist who will select individual care products.
Prevention of eczema
Personal hygiene is important, frequent overheating, accompanied by increased sweating, is unacceptable. A balanced diet should include a dairy-vegetarian diet with a low amount of carbohydrates and spices.
Prevention of eczema in adults
Overwork and stress can be triggers for the development of eczema, so it is important to maintain a balance between work and personal life, take time for good sleep and rest, play sports.
Use gloves when working around the house to prevent harsh detergents from coming into contact with your skin. Clean your hands thoroughly and use protective moisturizers.
For oily skin and genetic predisposition to eczema:
-
it is recommended to exclude fatty, sweet, fried and spicy foods from the diet.
-
it is not recommended to visit the bath and sauna.
-
it is not advisable to visit countries with high humidity or too hot climate.