Let down reflex in breastfeeding
Let-down reflex | Pregnancy Birth and Baby
Let-down reflex | Pregnancy Birth and Baby beginning of content3-minute read
Listen
The let-down reflex is an important part of breastfeeding that starts milk flowing when your baby feeds. Each woman feels it differently, and some may not feel it at all. It can be affected by stress, pain and tiredness but once feeding is established, it requires little or no thought.
What is the let-down reflex?
The let-down reflex is what makes breastmilk flow. When your baby sucks at the breast, tiny nerves are stimulated. This causes two hormones – prolactin and oxytocin – to be released into your bloodstream. Prolactin helps make the milk, while oxytocin causes the breast to push out the milk. Milk is then released or let down through the nipple.
Some women feel the let-down reflex as a tingling sensation in the breasts or a feeling of fullness, although others don’t feel anything in the breast.
Most women notice a change in their baby’s sucking pattern as the milk begins to flow, from small, shallow sucks to stronger, slower sucks.
Some women also notice, while feeding or expressing from one breast, that milk drips from the other.
Your let-down reflex needs to be established and maintained to ensure a good supply of milk. This reflex requires no thought, unless you are having problems with breastfeeding.
When does it occur?
The let-down reflex occurs:
- in response to your baby sucking at the breast
- hearing, seeing or thinking about your baby
- using a breast pump, hand expressing or touching your breasts or nipples
- looking at a picture of your baby
- hearing your baby (or another baby) cry
The let-down reflex generally occurs 2 or 3 times a feed. Most women only feel the first, if at all. This reflex is not always consistent, particularly early on, but after a few weeks of regular breastfeeding or expressing, it becomes an automatic response.
Most women only feel the first, if at all. This reflex is not always consistent, particularly early on, but after a few weeks of regular breastfeeding or expressing, it becomes an automatic response.
The let-down reflex can also occur with other stimulation of the breast, such as by your partner.
Strategies to encourage the reflex
The let-down reflex can be affected by stress, pain and tiredness. There are many things to try if you are experiencing difficulty.
- Ensure that your baby is correctly attached to the breast. A well-attached baby will drain a breast better.
- Feed or express in a familiar and comfortable environment.
- Try different methods to help you to relax: calming music, a warm shower or a warm washer on the breast, some slow deep breathing, or a neck and shoulder massage.
- Gently hand express and massage your breast before commencing the feed.
- Look at and think about your baby.
- If you are away from your baby, try looking at your baby’s photo.

- Always have a glass of water nearby.
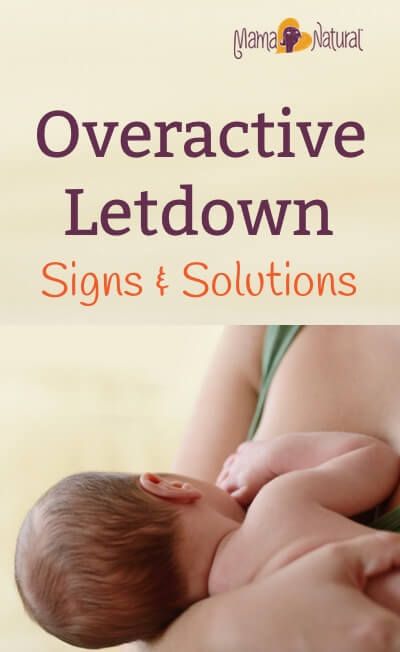
Milk let-down can be quite forceful, particularly at the beginning of a feed. This fast flow of milk can upset your baby, but it might not mean you have oversupply. It can be managed through expressing before a feed, reclining slightly and burping your baby after the first few minutes. If you continue to have problems, seek advice.
How to deal with unexpected let-down
Until you and your baby fine-tune breastfeeding, many sensations and thoughts can trigger your let-down reflex. Leaking breasts can be embarrassing, but should stop once breastfeeding is fully established.
In the meantime you can feed regularly, apply firm pressure to your breasts when you feel the first sensation of let-down, use breast pads and wear clothing that disguises milk stains.
If you need help and advice:
- Pregnancy Birth and Baby on 1800 882 436
- your maternal child health nurse
- a lactation consultant (your maternity hospital might be able to help)
- Australian Breastfeeding Association on 1800 686 268
Sources:
Australian Breastfeeding Association (Breastfeeding - naturally : the Australian Breastfeeding Association's guide to breastfeeding - from birth to weaning), Australian Breastfeeding Association (Let-down reflex)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: April 2021
Back To Top
Related pages
- Breastfeeding your baby
- How to increase breast milk supply
- Oversupply of breastmilk
Need more information?
Breastfeeding challenges - Ngala
Sometimes breastfeeding can be challenging
Read more on Ngala website
Breast refusal and baby biting breast | Raising Children Network
Breast refusal or baby biting breast are common breastfeeding issues. These issues might resolve themselves, or your child and family health nurse can help.
Read more on raisingchildren.net.au website
Breastfeeding - expressing breastmilk - Better Health Channel
Expressing breast milk by hand is a cheap and convenient method.
Read more on Better Health Channel website
Breast feeding your baby - MyDr.com.au
Breast milk has long been known as the ideal food for babies and infants. Major health organisations recommend that women breast feed their babies exclusively until they are 6 months old, and continue breast feeding, along with solids, until they are 12 months old or more. Breast milk has many benefits.
Read more on myDr website
Expressing and storing breast milk
This page includes information about expressing, storing, cleaning equipment, transporting and preparing expressed breastmilk for your baby.
Read more on WA Health website
Expressing breastmilk & storing breastmilk | Raising Children Network
You can express breastmilk by hand, or with a manual or an electric pump. Store expressed breastmilk in special bags or containers in the fridge or freezer.
Store expressed breastmilk in special bags or containers in the fridge or freezer.
Read more on raisingchildren.net.au website
Mastitis, blocked duct & breast abscess | Raising Children Network
If you think you have a blocked milk duct, you can treat it at home to start with. If you think you have mastitis or a breast abscess, see your GP as soon as possible.
Read more on raisingchildren.net.au website
Weaning at 6 Months | Tresillian
Babies start weaning when they begin consuming foods other than breastmilk. For advice on weaning check out Tresillian's tip page.
Read more on Tresillian website
Frequently asked questions about alcohol and pregnancy | FASD Hub
We've answered some common questions about alcohol use during pregnancy and breastfeeding, and about living with fetal alcohol spectrum disorder (FASD).
Read more on FASD Hub Australia website
Breastfeeding challenges - Ngala
Many new mothers experience breastfeeding challenges
Read more on Ngala website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What You Should Know About Your Let Down Reflex
Written by WebMD Editorial Contributors
In this Article
- How Does the Let Down Reflex Work?
- What Are Signs of a Good Let Down?
- Complications of the Let Down Reflex
When your baby first latches on to nurse, they don’t actually get much milk at first. Instead, their suckling sends a message to your body to release the milk stored in your breasts. The strength and timing of the let down reflex, also called the milk ejection reflex, varies from mother to mother.
Instead, their suckling sends a message to your body to release the milk stored in your breasts. The strength and timing of the let down reflex, also called the milk ejection reflex, varies from mother to mother.
How Does the Let Down Reflex Work?
If milk came out of your breasts instantly when your baby latched on, you’d probably leak constantly. Instead, your breasts store the milk until it’s needed. Most often, your let down reflex is triggered by a particular suckling motion your baby makes to stimulate milk production.
The let down reflex is a physiological response to your baby’s sucking. They stimulate small nerves in the nipple, which causes prolactin and oxytocin to produce milk and let down milk, respectively. The reflex is often accompanied by a tingling sensation in the nipple, but not all women experience that.
If you pay attention to your baby’s nursing patterns, at first their suckling will be faster and shallower to stimulate the release of milk. Once your milk lets down and your baby is drinking, their suckles will be deeper and longer. If they nurse longer and need more milk, they may adjust how they suck to stimulate more milk flow.
Once your milk lets down and your baby is drinking, their suckles will be deeper and longer. If they nurse longer and need more milk, they may adjust how they suck to stimulate more milk flow.
Other let down triggers. Since your brain is wired to care for a newborn, other things may trigger the let down reflex. If your baby cries, or if you hear any baby cry, your milk may let down in response. If you go too long without nursing and your breasts get too full, your let down reflex may trigger to relieve the pressure.
Strong emotions may also trigger a let down of milk. If you are feeling intensely stressed, angry, or sad, your body may take that as a sign that you need to nurse your baby or release milk to alleviate pressure.
If your milk is not letting down, you can physically stimulate the nipple to allow let down. Try gently rolling your hand down your breast toward the nipple, then massage gently. It can also help to relax and think about your baby.
What Are Signs of a Good Let Down?
Breastfeeding is wonderful for your baby, but it is often full of doubts and questions. Are you producing enough milk? Are you doing it right? This extends to the let down reflex, too. You may wonder if your let down is strong enough or too strong.
Here are signs of a healthy, functioning let down response:
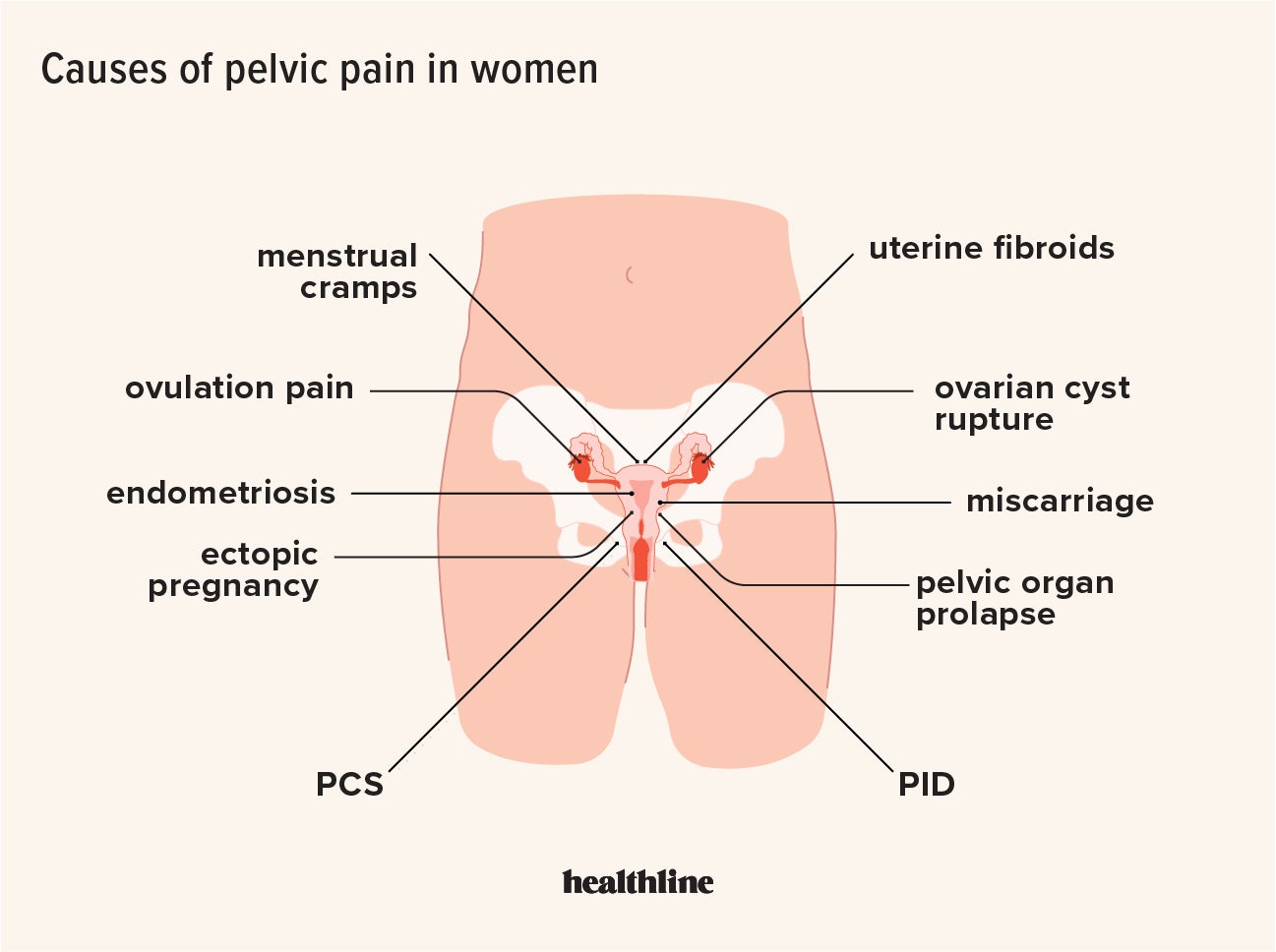
Uterine cramps. You may notice that your uterus cramps during a let down in the days following birth. This is natural and nothing to be concerned about. As with menstrual cramps, for some the cramps are mild and barely noticeable, while for others the contractions can be more painful.
Change in sucking pattern. You may notice a change in your baby’s sucking pattern during a nursing session. Their suckle will go from being short and fast to long and slow once milk lets down. If they need more milk, their sucking may change again to encourage another let down.
Your feelings. Moms often report that they feel very relaxed and even sleepy when their milk lets down. This is a side effect of the oxytocin released during let down. You may also feel suddenly thirsty, which is your body’s way of preparing to replace the milk being removed during a nursing session.
Moms often report that they feel very relaxed and even sleepy when their milk lets down. This is a side effect of the oxytocin released during let down. You may also feel suddenly thirsty, which is your body’s way of preparing to replace the milk being removed during a nursing session.
Complications of the Let Down Reflex
Oversupply milk ejection reflex. A powerful let down is often accompanied by an oversupply of milk, sometimes called oversupply milk ejection reflex (O-MER). When your let down happens, you may notice that your baby sputters, coughs, and even chokes on your milk. Your baby may bite down to slow the milk flow. You may leak when not nursing or notice that your baby has more frequent but short feedings if you have an oversupply.
If this happens, keep a bib or cloth handy to catch your milk when it first lets down so that your baby doesn’t choke. After a moment when the let down slows, you can try latching your baby again. You can also restrict your milk flow by squeezing your areola during breastfeeding.
Talk to your doctor about safe ways to decrease your oversupply so that your let down is less strong.
Dysphoric milk ejection reflex. In some women, breastfeeding can create a negative physiological response, leading to negative emotions like guilt, anxiety, depression, and sadness. It is usually an isolated response that occurs only when you first let down your milk and into the first few minutes of breastfeeding. This is called dysphoric milk ejection reflex (D-MER) and is different from postpartum depression.
There is still more research needed on the causes and effects of D-MER. Talk to your doctor if you are struggling with negative emotions during breastfeeding.
Weak let down. You may have a weak let down if your baby seems frustrated while nursing. They may not be getting enough milk, or they may not be getting milk as fast as they want it. Using a breast pump can supplement less successful nursing sessions.
When pumping, look at photos and videos of your baby to try and encourage a let down. And just as you do when breastfeeding, try to relax. Take deep breaths and think about your little one, letting go of any stress.
And just as you do when breastfeeding, try to relax. Take deep breaths and think about your little one, letting go of any stress.
Solutions to six breastfeeding problems in the first week
Are you having difficulty breastfeeding your newborn baby? Read on for expert advice on tackling the main challenges of the first week of breastfeeding.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is not always easy, so if
you are having difficulty, know that you are not alone. A US study found that out of 500 new mothers surveyed, 92% experienced breastfeeding problems by the third day.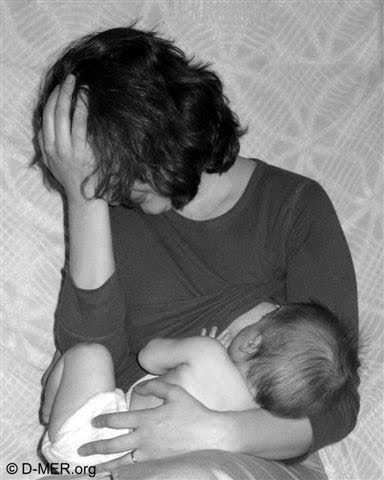 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
Problem #1. Breastfeeding hurts!
Pain during feeding is usually associated with tenderness or inflammation of the nipples, especially when milk "comes" on the second to fourth day after birth. 2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: some mothers' nipples crack, bleed, or blister. This is, of course, very annoying.
Solutions 3
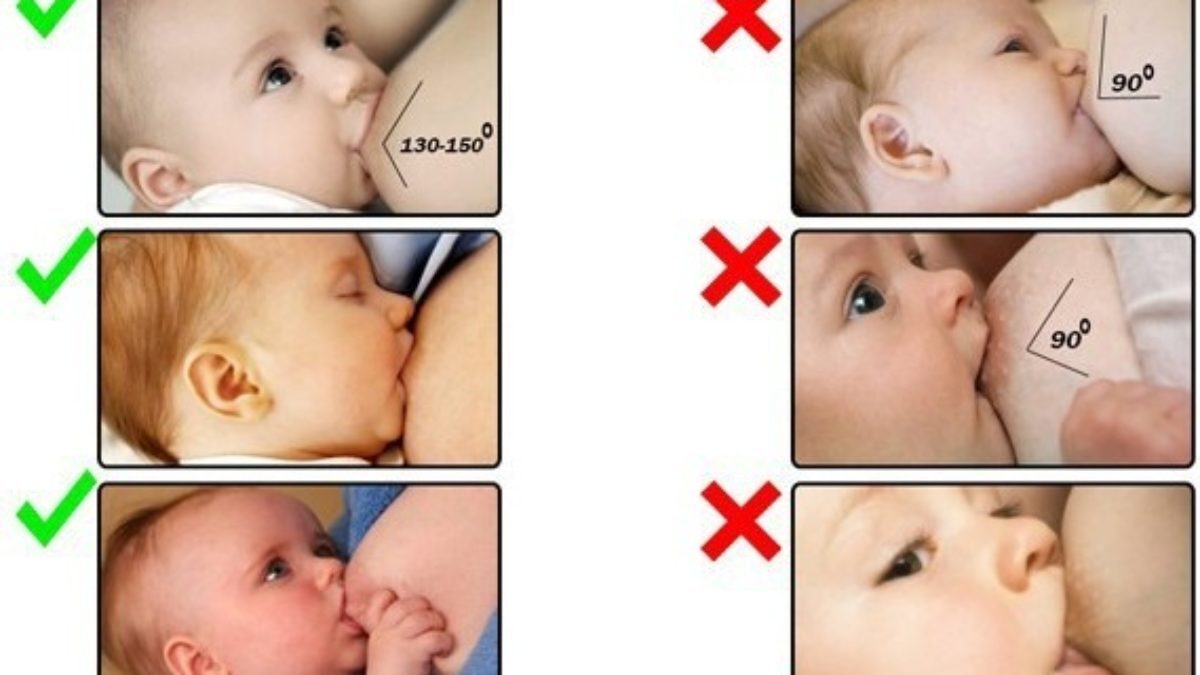
- Check how the baby latch on. An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue.

- Contact a lactation consultant or healthcare professional to make sure your baby's mouth and torso are properly positioned during feeding and there are no other latch-on problems. The doctor may also examine the baby's mouth for physical abnormalities.
- Try other feeding positions. Reclining, cross cradle, underarm, or lying positions can relieve pressure on the most painful areas of your breasts.
- Gently wipe soaked nipples with water-soaked cotton swabs after each feed to remove milk residues that can cause infection.
- Air dry nipples or blot with a clean, soft muslin or flannel cloth to prevent bacterial growth in a humid environment. Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly.
- Soften your nipples. An ultra-pure lanolin treatment will help relieve inflammation and dry skin. You can also apply a few drops of your own breast milk to your nipples.
 In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing.
In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing. - Protect your nipples. Nipple shields* protect the sore area from rubbing against clothing.
- Be patient. The inflammation usually resolves after a few days as your body adjusts to breastfeeding and your baby learns to suckle.
- Seek medical attention, if pain during feeding does not go away after a few days. Constant inflammation of the nipples may indicate an infection that requires prompt treatment.
Problem #2. Baby doesn't latch on properly
Some newborns do not latch on properly right away. Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.
Solutions
- Contact a lactation consultant or healthcare professional who can help identify the cause of the problem and suggest solutions.
- Flat or inverted nipples must be pulled out. Nipple formers* fit comfortably in the bra and apply gentle pressure to the nipples to help them come out for easier feeding.
- Try different positions and ways to support your newborn. The baby needs to feel supported. He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. 4
- When feeding, try to find the optimal position. Instead of putting your baby on and off, stressing both of you, try to position him in a way that is easy and comfortable for him.
 Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional.
Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional. - Use nursing pads. If your baby is having difficulty latch-on, a lactation consultant or healthcare professional may suggest trying nursing pads*. A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
Problem #3. Not enough breast milk
You will produce little breast milk at the very beginning, as the hormonal changes that trigger milk production occur slowly and do not end until the second or fourth day after birth. 2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
Solutions
- Contact a Lactation Consultant or your healthcare provider who can determine if you have problems with milk production. The sooner you do this, the better.
- Feed your baby on demand, not on a schedule. In the first week after birth, your baby will ask to breastfeed every two to three hours (or more often!), both day and night. Such frequent feeding helps to establish the production of breast milk.
- Take care of yourself. It's not always easy with a newborn, but try to rest whenever you can, eat right, and accept any help around the house or with older children that your loved ones can give you to fully focus on breastfeeding.

- Try expressing milk. If a baby is feeding frequently but not gaining any weight, a lactation consultant or doctor may recommend pumping to increase breast milk production. If milk is not coming out at all, you can try the Medela Symphony Dual Electric Clinical Breast Pump**. It features an Initiate program that mimics a baby's natural sucking rhythm for the first few days.
Problem #4. Breast full and heavy
Your breasts will become fuller and heavier as milk comes in.
If the baby suckles well and often, this should not cause any problems. However, in some women, the breasts become so full that they become hard and painful. This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on.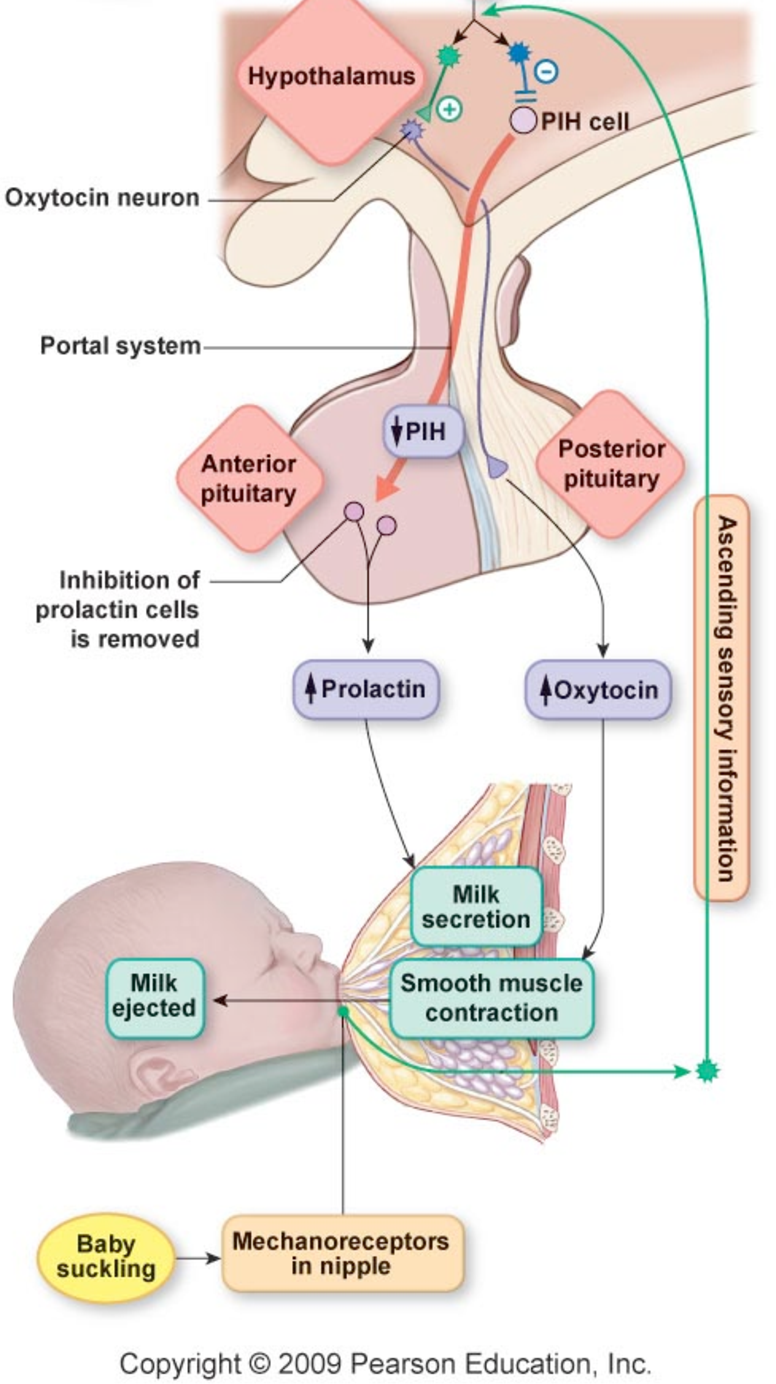 5
5
Solutions
- Feed your baby often. Try to breastfeed at least 8-12 times a day. This is the main way to alleviate this condition. For more tips and tricks, see the article on Breast Swelling. 6.7
- Call your healthcare provider, if symptoms persist for more than 48 hours, you have a fever, or your baby is unable to breastfeed due to swelling.
Problem #5. Milk is leaking
Breast leakage is very common in the early days of breastfeeding when milk production begins. Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Solutions
- Protect clothes from stains will help disposable or reusable bra pads to be used day and night.

- Don't waste precious drops! Breast milk collection pads* fit inside the bra and allow you to collect any leaking milk. This is a very useful thing when there is too much milk and the pads are not absorbing well, or when one breast is leaking while you are feeding the other. If you want to save the collected milk, use only the milk collected at the feeding. Place it in a sterile container and refrigerate immediately if you are not supplementing with it right away. Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.
Problem #6. There seems to be too much milk
Sometimes when milk comes in, too much is produced! In the first few weeks there may be an overabundance of milk, but usually everything returns to normal soon. 7 Up to this point, the breasts may be heavy and sore almost all the time, even immediately after a feed, and a lot of milk may leak. A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
Solutions
- Express some milk by hand at the beginning of each feed to ease the force of the flush.
- Try to feed while leaning back: this will help your baby control the flow of milk. The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you.
- Be kind and patient. Let your baby rest and absorb milk both during and after feeding. Don't move your baby too much or too fast, as this can make him nauseous. As the baby grows, he will learn to better cope with the rush of milk, which is likely to weaken anyway.
- Use the towel or swaddle to soak up spilled milk if the baby can't handle the flush, and place the breast milk collection pad on the other breast to catch any spilled milk.
- Contact a lactation consultant or doctor if problems persist after a few weeks . He will examine you and may suggest one-sided feedings or hourly breast changes (“breast duty”) to reduce your milk supply.
Related materials: Difficulties in breastfeeding in the next few weeks and problems with breastfeeding after the first month
Literature
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Child's Life and Type of Feeding at 2 Months". Pediatrix (Pediatrics). 2013:e865–e875.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. . ABM Clinical Protocol# 4: Mastitis , Revised MARCH 2014. Breastfeed : 5): 5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
7 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement.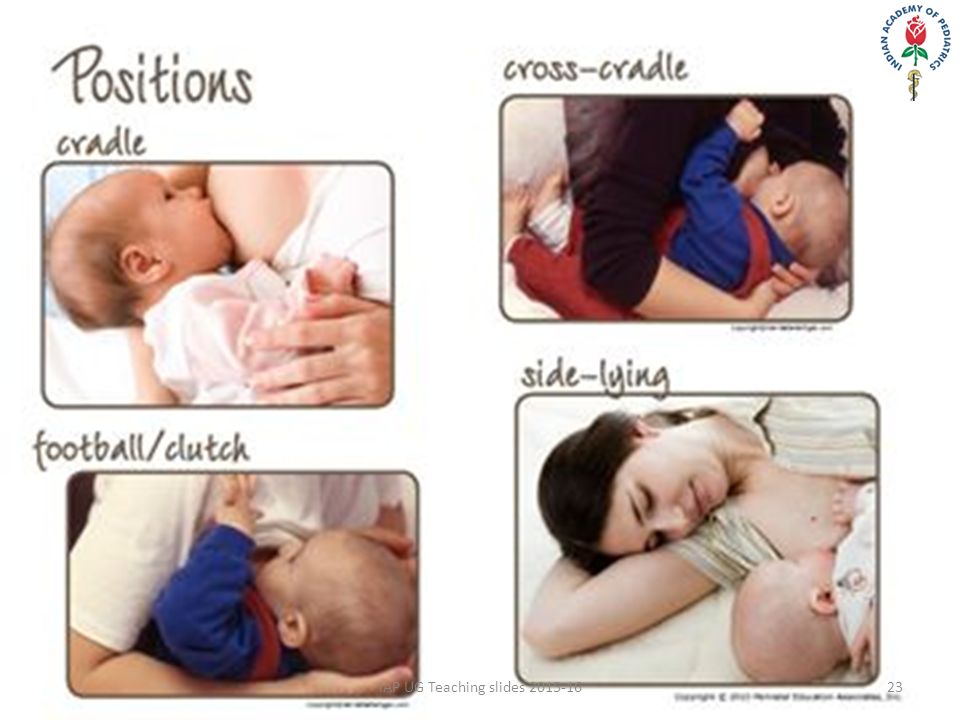 Breastfeed Med . 2009;4(2):111-113. - Protocol Committee of the Academy of Breastfeeding Medicine, "AVM Clinical Protocol No. 20: Engorgement, Revision 2016". Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
Breastfeed Med . 2009;4(2):111-113. - Protocol Committee of the Academy of Breastfeeding Medicine, "AVM Clinical Protocol No. 20: Engorgement, Revision 2016". Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
Read instructions before use. Consult a specialist about possible contraindications.
*RU No. FSZ 2010/07352 dated 07/19/10
** RA No. FCZ 2010/06525 dated 17/03/2021
breastfeeding GBUZ GBUZ VFD Kopeisk
9000 9000
Breastal fed
2 it is natural, useful, convenient and cheap. Nobody has come up with anything better than breast milk for a baby. And no formula, even the most expensive and enriched with vitamins, will replace mother's milk, because laboratories cannot synthesize or isolate most of the important components that are contained in breast milk from cow's milk. For example, protective cells of maternal immunity.
Breastfeeding is also good for the mother herself. Long-term breastfeeding is a proven prevention of breast cancer, ovarian cancer, and the development of diabetes.
Long-term breastfeeding is a proven prevention of breast cancer, ovarian cancer, and the development of diabetes.
And one more thing. Any woman can breastfeed, regardless of breast size, the baby was born on time or not, and other factors. True milk deficiency occurs in less than 2-3 percent of cases.
Advice for breastfeeding mothers
There are many difficulties that a breastfeeding mother may face. Here are some important tips for breastfeeding moms from a lactation consultant Anastasia Kulikova .
- It is important to ensure that the baby is properly attached to the breast. Otherwise, he will not completely empty the breast, this may lead to a decrease in milk production, and may also injure the nipples. Please note that the newborn should capture not only the nipple, but also the areola, and its main part is from below, that is, the attachment should not be symmetrical. Mom's posture should be comfortable and relaxed.

- Night feedings are very important for successful breastfeeding, namely between 3 and 6 am. It is at this time that the brain releases large amounts of prolactin, the hormone responsible for milk production.
- Drink plenty of fluids - 2-3 liters per day. It is also very important for a sufficient amount of milk. At night, put a bottle of water near you so as not to run to the kitchen.
- Do not be nervous, try to get enough sleep and be sure that you will be able to feed your baby for a long time. The calmness of the mother, her good emotional state is the key to successful breastfeeding of the newborn.
- If you have problems that you cannot solve yourself: you cannot establish proper attachment, you feel that there is not enough milk and nothing helps to increase lactation, or vice versa, you are experiencing milk stagnation, seek the help of a breastfeeding consultant . There are such specialists in some antenatal clinics, there are also special services that work on a paid basis.

How to start breastfeeding
It is important that the newborn is put to the breast immediately after birth, in the delivery room. In most maternity hospitals, the joint stay of mother and child is practiced today, which is also very important for the successful establishment of breastfeeding. In the first 1-3 days, colostrum is produced - it is very small, just a few drops, but enough for a newborn. Then comes the milk.
While in the hospital, breastfeed your baby more often to stimulate milk production. Remember, you need to feed the baby on demand, and not by the hour, as was customary in the past. This is the key to successful and long-term breastfeeding.
In the first month when lactation is established, discard bottles and nipples. Sucking from a bottle is much easier for a newborn, so there is a risk of rejection of the breast.
According to WHO recommendations, newborns should also not be supplemented with water. It is enough in mother's milk. And supplementation can lead to a decrease in milk production, as the baby will eat less of it.
And supplementation can lead to a decrease in milk production, as the baby will eat less of it.
Until what age can a child be fed
The World Health Organization recommends breastfeeding up to two years of age.
- In fact, there is no unequivocally correct answer to this question, - says Anna Levadnaya , pediatrician, PhD, author of the blog about pediatrics on Instagram @doctor_annamama. - I am convinced that you need to feed as long as both the baby and the mother enjoy it. If there are no objective reasons for stopping breastfeeding, up to a year, mother's milk must be present in the baby's diet. It is optimal to keep it up to a year and a half.
There is an opinion that after a year milk no longer brings much benefit to the child, but this is not so.
- Studies show that even after the first year of life in breast milk there is a high amount of protein, the concentration of immunoglobulins, lysozyme and lactoferrin, which help to form immunity, Anna Levadnaya notes. - Long-term breastfeeding reduces the risk of atherosclerosis in adulthood, diabetes and obesity, and many other diseases. Long-term breastfeeding helps the correct formation of the maxillofacial skeleton, the likelihood that the child will not have the correct bite is much lower. And some studies suggest that babies who breastfeed for a long time have higher IQs.
- Long-term breastfeeding reduces the risk of atherosclerosis in adulthood, diabetes and obesity, and many other diseases. Long-term breastfeeding helps the correct formation of the maxillofacial skeleton, the likelihood that the child will not have the correct bite is much lower. And some studies suggest that babies who breastfeed for a long time have higher IQs.
The benefits of breastfeeding
The benefits of breastfeeding cannot be overestimated. It is not only a source of valuable nutrients. During feeding, a strong emotional bond is formed between the newborn and mother. Scientists have conducted many studies on the benefits of breast milk. Here's what they say.
- Breast milk contributes to the maturation of the child's immune system, reduces the risk of cancer.
- Children on breastfeeding have a lower risk of atopic dermatitis, they are less likely to get otitis media, they need to remove the pharyngeal tonsils less often, they have better vision.

- Breastfed babies are less likely to experience constipation, diarrhea and intestinal infections, as well as food allergies (when breastfed for 6 months or more). Adults who were breastfed as children are less likely to develop Crohn's disease (severe inflammation of the intestines), ulcerative colitis (inflammation of the colon), and appendicitis.
- Breast milk contains less protein and salts, so there is less stress on the baby's immature kidneys. Less common are urinary tract infections.
- Improves the growth of nervous tissue - this is facilitated by cholesterol and other fats of breast milk.
- Breast sucking improves jaw muscle development. And if you feed your baby for more than a year, this reduces the risk of malocclusion. In addition, the gradual changes in the taste of breast milk with age prepare the baby for a variety of solid foods.
- Breastfed babies develop less respiratory tract infections and are much milder, less likely to develop bronchial asthma, pneumonia, and influenza.

What breast milk should look like
Don't look online for a picture of the "correct" color of breast milk. This is such a unique product that adapts to the needs of the child depending on his age and condition, which can change its composition, fat content and color even during the day. For example, in summer, when a child has a great need to drink, the milk becomes more liquid, the color is more transparent.
But usually with established lactation, the foremilk - the one that the baby receives at the beginning of feeding, is more liquid, it is rich in carbohydrates, its color is less saturated, white-bluish. Back milk, which the baby receives at the end of feeding, is rich in fats, the color is more saturated, yellowish.
If you express milk using a breast pump, you will first see a homogeneous liquid in the bottle. But after standing for quite a bit, it will separate just into these two layers: the top one - the “cream” layer - will be fatter, but smaller in volume.
How to know if a child is hungry
In fact, a child can ask for a breast not only because he is hungry. It helps the newborn to calm down, feel safe, sucking reduces the pain that the baby may experience due to colic. However, there are signs by which you can understand that the child really wants to eat.
- The child is anxious.
- He turns his head from side to side, opens his mouth, as if looking for a nipple, starts doing this especially actively if you pass his hand over his cheek.
- Starts fiddling, groaning, sticking out his tongue.
- Looks for breasts when you pick him up.
- Cries, does not calm down with motion sickness and other actions.
Remember, it is recommended to breastfeed on demand, but at least once every 3 hours during the day and 5 hours at night. Within 1-2 months, lactation gradually improves, milk is released during feeding, and the breast gets used to working in a certain rhythm of feeding.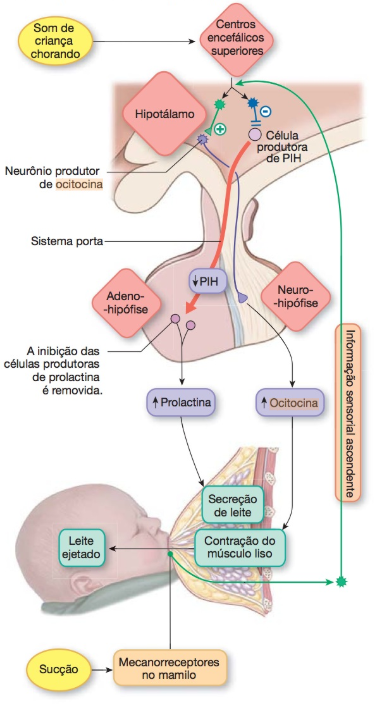
Why breast milk is expressed
It is important to remember that when lactation is established, pumping is not necessary. Advice to a nursing mother: do not listen to grandmothers who are convinced that if you do not express milk after each feeding, then it will disappear. This is wrong.
- The arrival of milk is carried out according to the so-called "principle of direct feedback": the more milk left, the more it will come, - says Anna Levadnaya. - The child himself regulates the amount he needs. If a woman expresses milk after each feeding, she will be trapped: more milk will come, but the child does not need such an amount, it will stagnate in the chest, which threatens the development of lactostasis and mastitis.
However, there are times when it is necessary to express milk. If your baby was born prematurely and is in intensive care, then the mother should start expressing milk as soon as possible after birth. This will help preserve the milk until the newborn can suckle on his own. In the meantime, the expressed milk will be valuable food for him. Premature babies, as a rule, are fed through a tube, as they are still very weak, they do not have a sucking reflex.
In the meantime, the expressed milk will be valuable food for him. Premature babies, as a rule, are fed through a tube, as they are still very weak, they do not have a sucking reflex.
Another occasion when it is necessary to express milk is when you feel that there is less or not enough milk. You need to pump after each feeding, including at night. In this case, breastfeeding specialists can help you.
If you have to be separated from your baby, you also need to express milk so that dad or someone else in the family can feed the baby. Also, pumping is necessary for lactostasis and mastitis in order to cope with milk stagnation.
What can be done while breastfeeding
How many unreasonable prohibitions today for a nursing mother. In fact, the list of what not to do while breastfeeding is very small. We will dispel myths and tell you what a woman can do while breastfeeding.
- No hypoallergenic diet required. We have long been of the opinion that a nursing mother should follow a special diet so that the child does not have diathesis.
 Meanwhile, in other countries, women eat what they want and how much they want, and the concept of “nursing mother’s diet” simply does not exist. But, despite the widespread practice of diets in pregnant and lactating women, the incidence of allergies continues to grow, and studies have shown that restrictions do not affect its manifestation in any way. Therefore, a nursing mother should eat varied, eat her favorite vegetables, fruits. It is necessary to exclude this or that product from the diet only with a proven food allergy to it.
Meanwhile, in other countries, women eat what they want and how much they want, and the concept of “nursing mother’s diet” simply does not exist. But, despite the widespread practice of diets in pregnant and lactating women, the incidence of allergies continues to grow, and studies have shown that restrictions do not affect its manifestation in any way. Therefore, a nursing mother should eat varied, eat her favorite vegetables, fruits. It is necessary to exclude this or that product from the diet only with a proven food allergy to it. - You can drink coffee, many women love it. But the amount should be limited to 2 cups per day.
- You can play sports. This does not affect the production and quality of milk. But consider important nuances. It is worth returning to full-fledged training not earlier than the child is 6 months old. It is better to give preference to moderate physical activity. During too intense activities, lactic acid accumulates in milk, the child may not like its taste.
 When playing sports, a lot of fluid is lost, so you need to drink more water to avoid dehydration.
When playing sports, a lot of fluid is lost, so you need to drink more water to avoid dehydration. - Can be dyed and curled.
- You can visit the sauna, observing all hygiene measures.
- You can do, if necessary, x-rays, fluorography, treat teeth using anesthesia (it is selected by the doctor, taking into account the fact that you are breastfeeding).
- You can visit beauty salons and get simple facial and body treatments, including massages that do not affect the chest area.
- You can drink alcohol in moderation. Yes, don't be surprised. Sometimes you can afford to have a glass of wine and relax a bit. But remember a few important points. Alcohol penetrates into breast milk, and its maximum concentration in it is reached after 60-90 minutes if you eat, and after 30-60 minutes if you drink on an empty stomach. And the rate of elimination of alcohol from the body depends on the weight of the woman (in full it will happen faster), the amount of alcohol consumed, its strength.
 A glass of wine or a glass of beer is excreted on average in 2-3 hours, strong alcohol - in 13 hours. Therefore, if you want to drink a glass of dry white wine, do it immediately after feeding your baby so that the next alcohol will be out of the body. Or express milk 1-2 feedings ahead if you plan to drink more. But in any case, cut out alcohol until your baby is 3 months old.
A glass of wine or a glass of beer is excreted on average in 2-3 hours, strong alcohol - in 13 hours. Therefore, if you want to drink a glass of dry white wine, do it immediately after feeding your baby so that the next alcohol will be out of the body. Or express milk 1-2 feedings ahead if you plan to drink more. But in any case, cut out alcohol until your baby is 3 months old.
What not to do while breastfeeding
- A breastfeeding mother should not smoke. Continuous smoking reduces the level of prolactin, the hormone responsible for the production of sufficient milk. In a child, it can cause nausea, vomiting, colic, problems with stools, and irritability.
- You can not drink alcohol in large quantities, in a state of intoxication to feed a child.
- You can not do complex cosmetic procedures involving injections, the introduction of various drugs. For example, mesotherapy of the face and scalp, apparatus treatment, photo and laser hair removal, and others, their impact on the body of the mother and child during this period has not been studied.

What to do if the mother falls ill
Unfortunately, mothers get sick during breastfeeding. And often women unreasonably stop breastfeeding because of this. In fact, it is possible and necessary to feed a baby with SARS (perhaps, mothers get sick most often with them). Together with milk, the child will receive the necessary antibodies. And a woman can bring down a high temperature with drugs based on paracetamol or ibuprofen, they are allowed when breastfeeding.
But even more serious illnesses that require medication, including antibiotics, are no reason to stop breastfeeding. First, there are many drugs allowed during this period. And secondly, despite the fact that the instructions for the medicine often say that it can be taken only if the benefit to the woman outweighs the risks to the child, this does not mean at all that the remedy is dangerous and should not be taken.
- The fact is that studies on the safety of drugs during breastfeeding are very expensive, and manufacturers usually do not conduct them, - says Anna Levadnaya. - It is easier for them to write that the drug is not recommended for breastfeeding, for fear of liability. But such studies were carried out by other independent organizations, for example, the World Health Organization, the American Academy of Pediatrics. And in most cases, the drug is allowed during feeding. Or you can choose a safe analogue.
- It is easier for them to write that the drug is not recommended for breastfeeding, for fear of liability. But such studies were carried out by other independent organizations, for example, the World Health Organization, the American Academy of Pediatrics. And in most cases, the drug is allowed during feeding. Or you can choose a safe analogue.
Moreover, this information is publicly available and you can check the compatibility of the drug and breastfeeding yourself.
- There are several sites for this, the simplest is the Spanish site. All data here is based on scientific publications and medical research.
Despite the fact that there is no Russian version of the site, it is not difficult to use it. Here are some tips for breastfeeding moms on how to do this. First determine the Latin name of the drug or active substance. On the site, select English, enter the name of the desired medicine in the search bar. A rectangle of green, yellow, orange or red color with a description will be highlighted. Green means very low risk, which means the drug is safe for the baby. Red - the risk is very high, which means that the drug cannot be used, you need to choose an analogue. But the final decision whether to take this or the drug during breastfeeding or the abolition of breastfeeding, you still need to work with your doctor.
Green means very low risk, which means the drug is safe for the baby. Red - the risk is very high, which means that the drug cannot be used, you need to choose an analogue. But the final decision whether to take this or the drug during breastfeeding or the abolition of breastfeeding, you still need to work with your doctor.
Feeding after caesarean section
Women whose babies are born by caesarean section often worry that they will not be able to breastfeed their baby. Of course it isn't. There are some difficulties that a mother may face, but they are all surmountable. Milk after a cesarean may come a little later than after a natural birth. To speed up this process, take the baby to you from the nursery as soon as you can take care of him yourself, breastfeed more often.
If for some reason it is not possible to stay together with the baby in the maternity hospital after the operation, then the mother needs to express milk in order to maintain lactation, start doing this as soon as possible after the birth. True, in this case, the baby, who will receive the mixture at the maternity hospital, may refuse the breast at home: sucking from it requires much more effort than from a bottle. Do not despair! Try not to use nipples and bottles, offer breasts more often, and you can feed with expressed milk from a spoon or pipette.
True, in this case, the baby, who will receive the mixture at the maternity hospital, may refuse the breast at home: sucking from it requires much more effort than from a bottle. Do not despair! Try not to use nipples and bottles, offer breasts more often, and you can feed with expressed milk from a spoon or pipette.
Feeding premature babies
Breast milk is very important for premature babies. The baby receives the necessary nutrients, protection from infections. Breast milk is easier to digest, which is very important for the still immature digestive system of the baby.
Unfortunately, often children born prematurely can be in intensive care, sometimes for quite a long time. They cannot suckle on their own, they are fed through a tube. In this case, in order to save breast milk, the mother needs to start expressing as soon as possible after childbirth and continue to do this until the baby gets stronger and can not eat on her own. “If a premature baby is discharged from the hospital with a normal weight for his age, then the mother can only feed the baby with breast milk,” says Anna Levadnaya.
- If the baby is underweight, breast milk fortifiers should be used. These are special supplements that give a premature baby extra calories, vitamins, macro- and microelements. They are available in the form of a powder or a ready-made mixture. Add to expressed milk just before feeding.
There are two points of view, in many ways different.
The first is followed by many pediatricians and, in particular, the famous Dr. Komarovsky: the baby should be weaned when he is one year old, and do it quickly, decisively and irrevocably . Doctors assure: by this age the child has already received everything that is needed from mother's milk, and is able to eat coarser food, since teeth are already growing. Not delaying feeding is also good for the mother, in terms of social needs: for example, going to work.
Radical completion methods are proposed. For example, for a few days to leave the baby with his grandmother.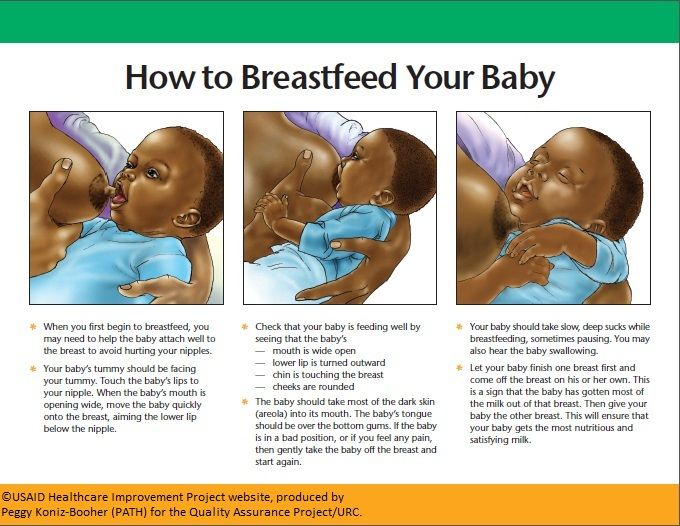 Of course, the child will cry and look for his mother, but he will have to be firm. Mom, meanwhile, takes lactation suppressant pills and pumps. If you do everything right, the stress will be minimal and quickly forgotten. Weaning should be postponed if the baby is sick, teething, or there is a change of scenery (moving, going on vacation, etc.). But the time of year doesn't matter here. Previously, pediatricians really dissuaded from completing breastfeeding in the summer to protect the baby from intestinal infections and disorders. Now this is not relevant: it is enough to follow the usual rules of hygiene.
Of course, the child will cry and look for his mother, but he will have to be firm. Mom, meanwhile, takes lactation suppressant pills and pumps. If you do everything right, the stress will be minimal and quickly forgotten. Weaning should be postponed if the baby is sick, teething, or there is a change of scenery (moving, going on vacation, etc.). But the time of year doesn't matter here. Previously, pediatricians really dissuaded from completing breastfeeding in the summer to protect the baby from intestinal infections and disorders. Now this is not relevant: it is enough to follow the usual rules of hygiene.
Lactation consultants and perinatal psychologists (yes, there are some) are strongly opposed to such an early termination, and especially disagree with doctoral methods, considering them ruthless. Like, for a child, separation from his mother is a catastrophe and betrayal, such injuries do not go away without a trace.
Breastfeeding should be completed by 2-3 years of age, gradually and gently, the authors of the popular BF blog advise. The breast is not only food for the baby, but also contact with the mother, calm falling asleep, confidence that everything is fine.
The breast is not only food for the baby, but also contact with the mother, calm falling asleep, confidence that everything is fine.
The scheme is as follows: from the age of 6 months, small restrictions on feeding are introduced, for example, on the street, at a party - only at home. Then the number of applications during the day is gradually reduced. How? Minimize everything that reminds of mother's milk: do not change clothes in front of the child, choose clothes that make it difficult to access the breast. Distract with something interesting or tasty. Next, we teach the baby to calm down and fall asleep without a breast. First during the day and then at night. Rituals will help here: before going to bed, read a fairy tale, sing a song, stroke ... Night feedings are removed the very last and also gradually, until the attachments become symbolic. This completion of the GW may take several weeks or even months, but it is worth it. And you can “round off” in a day or two, if the child himself is ready and simply outgrew the need for sucking.