C section baby delivery
C-section - Mayo Clinic
Overview
Cesarean delivery (C-section) is used to deliver a baby through surgical incisions made in the abdomen and uterus.
Planning for a C-section might be necessary if there are certain pregnancy complications. Women who have had a C-section might have another C-section. Often, however, the need for a first-time C-section isn' clear until after labor starts.
If you're pregnant, knowing what to expect during and after a C-section can help you prepare.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Obstetricks
Why it's done
Health care providers might recommend a C-section if:
- Labor isn't progressing normally. Labor that isn't progressing (labor dystocia) is one of the most common reasons for a C-section. Issues with labor progression include prolonged first stage (prolonged dilation or opening of the cervix) or prolonged second stage (prolonged time of pushing after complete cervical dilation).
- The baby is in distress. Concern about changes in a baby's heartbeat might make a C-section the safest option.
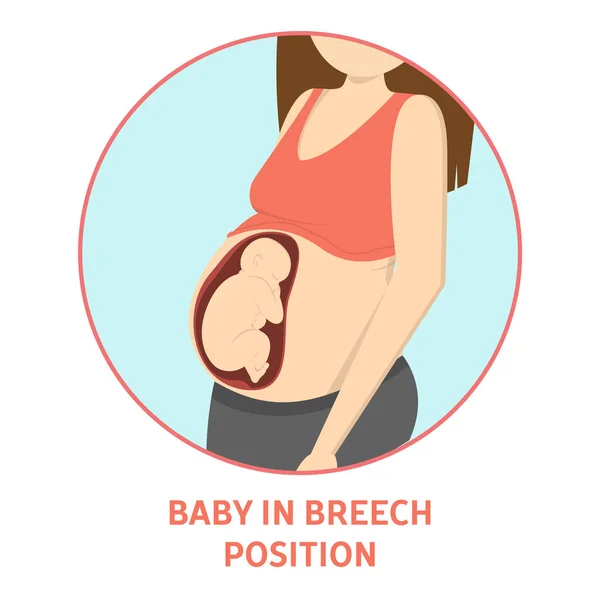
- The baby or babies are in an unusual position. A C-section is the safest way to deliver babies whose feet or buttocks enter the birth canal first (breech) or babies whose sides or shoulders come first (transverse).
- You're carrying more than one baby. A C-section might be needed for women carrying twins, triplets or more. This is especially true if labor starts too early or the babies are not in a head-down position.
- There's a problem with the placenta. If the placenta covers the opening of the cervix (placenta previa), a C-section is recommended for delivery.
- Prolapsed umbilical cord. A C-section might be recommended if a loop of umbilical cord slips through the cervix in front of the baby.
- There's a health concern.
 A C-section might be recommended for women with certain health issues, such as a heart or brain condition.
A C-section might be recommended for women with certain health issues, such as a heart or brain condition. - There's a blockage. A large fibroid blocking the birth canal, a pelvic fracture or a baby who has a condition that can cause the head to be unusually large (severe hydrocephalus) might be reasons for a C-section.
- You've had a previous C-section or other surgery on the uterus. Although it's often possible to have a vaginal birth after a C-section, a health care provider might recommend a repeat C-section.
Some women request C-sections with their first babies. They might want to avoid labor or the possible complications of vaginal birth. Or they might want to plan the time of delivery. However, according to the American College of Obstetricians and Gynecologists, this might not be a good option for women who plan to have several children. The more C-sections a woman has, the greater the risk of problems with future pregnancies.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Risks
Like other types of major surgery, C-sections carry risks.
Risks to babies include:
- Breathing problems. Babies born by scheduled C-section are more likely to develop a breathing issue that causes them to breathe too fast for a few days after birth (transient tachypnea).
- Surgical injury. Although rare, accidental nicks to the baby's skin can occur during surgery.
Risks to mothers include:
- Infection. After a C-section, there might be a risk of developing an infection of the lining of the uterus (endometritis), in the urinary tract or at the site of the incision.
- Blood loss. A C-section might cause heavy bleeding during and after delivery.
- Reactions to anesthesia. Reactions to any type of anesthesia are possible.

- Blood clots. A C-section might increase the risk of developing a blood clot inside a deep vein, especially in the legs or pelvis (deep vein thrombosis). If a blood clot travels to the lungs and blocks blood flow (pulmonary embolism), the damage can be life-threatening.
- Surgical injury. Although rare, surgical injuries to the bladder or bowel can occur during a C-section.
-
Increased risks during future pregnancies. Having a C-section increases the risk of complications in a later pregnancy and in other surgeries. The more C-sections, the higher the risks of placenta previa and a condition in which the placenta becomes attached to the wall of the uterus (placenta accreta).
A C-section also increases the risk of the uterus tearing along the scar line (uterine rupture) for women who attempt a vaginal delivery in a later pregnancy.
How you prepare
For a planned C-section, a health care provider might suggest talking with an anesthesiologist if there are medical conditions that might increase the risk of anesthesia complications.
A health care provider might also recommend certain blood tests before a C-section. These tests provide information about blood type and the level of the main component of red blood cells (hemoglobin). The test results can be helpful in case you need a blood transfusion during the C-section.
Even for a planned vaginal birth, it's important to prepare for the unexpected. Discuss the possibility of a C-section with your health care provider well before your due date.
If you don't plan to have more children, you might talk to your health care provider about long-acting reversible birth control or permanent birth control. A permanent birth control procedure might be performed at the time of the C-section.
What you can expect
Before the procedure
Abdominal incisions used during C-sections
Abdominal incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. The abdominal incision is made first. It's either a vertical incision between your navel and pubic hair (left) or, more commonly, a horizontal incision lower on your abdomen (right).
It's either a vertical incision between your navel and pubic hair (left) or, more commonly, a horizontal incision lower on your abdomen (right).
Uterine incisions used during C-sections
Uterine incisions used during C-sections
A C-section includes an abdominal incision and a uterine incision. After the abdominal incision, the health care provider will make an incision in the uterus. Low transverse incisions are the most common (top left).
A C-section can be done in various ways. But most C-sections involve these steps:
- At home. Your health care provider might ask you to shower at home with an antiseptic soap the night before and the morning of your C-section. Don't shave your pubic hair within 24 hours of your C-section. This can increase the risk of a surgical site infection. If your pubic hair needs to be removed, it will be trimmed by the surgical staff just before surgery.
- At the hospital.
 Your abdomen will be cleansed. A thin tube (catheter) will likely be placed into your bladder to collect urine. An intravenous line will be placed in a vein in your hand or arm to provide fluid and drugs, including antibiotics to prevent infection.
Your abdomen will be cleansed. A thin tube (catheter) will likely be placed into your bladder to collect urine. An intravenous line will be placed in a vein in your hand or arm to provide fluid and drugs, including antibiotics to prevent infection. -
Anesthesia. Most C-sections are done under regional anesthesia, which numbs only the lower part of your body. This allows you to be awake during the procedure. Common choices include a spinal block and an epidural block.
Some C-sections might require general anesthesia. With general anesthesia, you won't be awake during the birth.
During the procedure
A doctor makes surgical incisions in the abdomen and the uterus to deliver the baby.
- Abdominal incision. The doctor makes an incision in the abdominal wall. It's usually done horizontally near the pubic hairline. Or the doctor might make a vertical incision from just below the navel to just above the pubic bone.
- Uterine incision. The uterine incision is then made — usually horizontally across the lower part of the uterus (low transverse incision). Other types of uterine incisions might be used depending on the baby's position within the uterus and whether there are complications, such as placenta previa or preterm delivery.
- Delivery. The baby will be delivered through the incisions. The doctor clears the baby's mouth and nose of fluids, then clamps and cuts the umbilical cord. The placenta is then removed from the uterus, and the incisions are closed with sutures.
If you have regional anesthesia, you're likely to be able to hold the baby shortly after delivery.
After the procedure
A C-section usually requires a hospital stay for 2 to 3 days. Your health care provider will discuss pain relief options with you.
Once the anesthesia begins to wear off, you'll be encouraged to drink fluids and walk. This helps prevent constipation and deep vein thrombosis. Your health care team will monitor your incision for signs of infection. The bladder catheter will likely be removed as soon as possible.
Your health care team will monitor your incision for signs of infection. The bladder catheter will likely be removed as soon as possible.
You can start breastfeeding as soon as you're ready, even in the delivery room. Ask your nurse or a lactation consultant to teach you how to position yourself and support your baby so that you're comfortable. Your health care team will select medications for your post-surgical pain with breastfeeding in mind.
When you go home
During the C-section recovery process, discomfort and fatigue are common. To promote healing:
- Take it easy. Rest when possible. Try to keep everything that you and your baby need within reach. For the first few weeks, don't lift more than 25 pounds.
- Use recommended pain relief. To soothe incision soreness, your health care provider might recommend a heating pad and pain medications that are safe for breastfeeding women and their babies. These include ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others).

- Wait to have sex. To prevent infection, wait at least six weeks to have sex and don't put anything in your vagina after your C-section.
- Wait to drive. If you're taking narcotics for pain relief, it might take 1 to 2 weeks before you can comfortably apply brakes and twist to check blind spots.
Check your C-section incision for signs of infection. Pay attention to any symptoms. Contact your health care provider if:
- Your incision is red, swollen or leaking discharge
- You have a fever
- You have heavy bleeding
- You have worsening pain
If you have severe mood swings, loss of appetite, overwhelming fatigue and lack of joy in life shortly after childbirth, you might have postpartum depression. Contact your health care provider if you think you might be depressed, especially if your symptoms don't go away, you have trouble caring for your baby or completing daily tasks, or you have thoughts of harming yourself or your baby.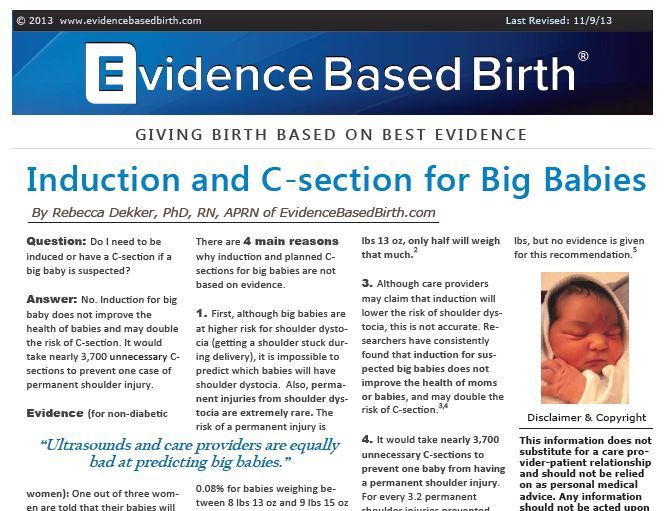
The American College of Obstetricians and Gynecologists recommends that postpartum care be ongoing. Have contact with your health care provider within three weeks after delivery. Within 12 weeks after delivery, see your health care provider for a postpartum evaluation.
During this appointment your health care provider likely will check your mood and emotional well-being, discuss contraception and birth spacing, review information about infant care and feeding, talk about your sleep habits and issues related to fatigue and do a physical exam, including a pap smear if it's due. This might include a check of your abdomen, vagina, cervix and uterus to make sure you're healing well.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
By Mayo Clinic Staff
Related
Products & Services
C-Section (Cesarean Section): Procedure, Risks & Recovery
Overview
What is a C-section?
A C-section, also called a cesarean section or cesarean delivery, is a surgical procedure in which a baby is delivered through incisions in your abdomen and uterus.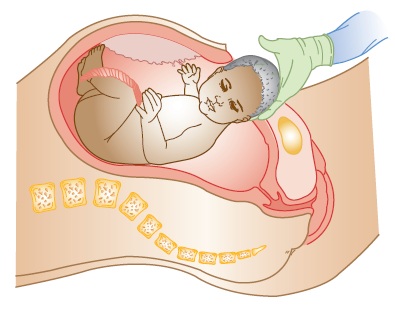 They're performed when a vaginal delivery is not possible or safe, or when the health of you or your baby is at risk.
They're performed when a vaginal delivery is not possible or safe, or when the health of you or your baby is at risk.
When would I need a C-section?
You may need a C-section if you have certain medical conditions or if complications occur during labor in a vaginal delivery. A planned C-section happens when any of the following conditions exist:
- Cephalopelvic disproportion (CPD): CPD is a term that means that your baby's head or body is too large to pass safely through your pelvis, or your pelvis is too small to deliver an average-sized baby.
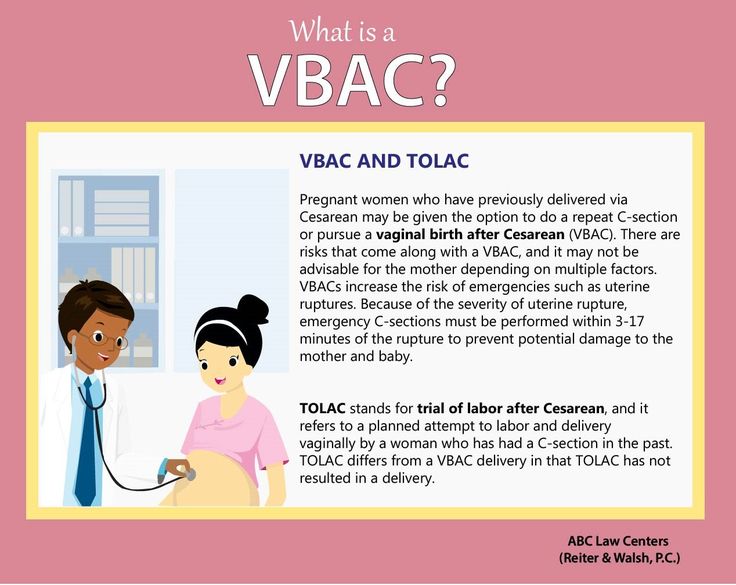
- Previous C-section: Although it’s possible to have a vaginal birth after a previous C-section, it’s not an option for everyone. Factors that can affect this include type of uterine incision used in the previous C-section and the risk of uterine rupture.
- Expecting multiples: Although twins can often be delivered vaginally, two or more babies might require a C-section.
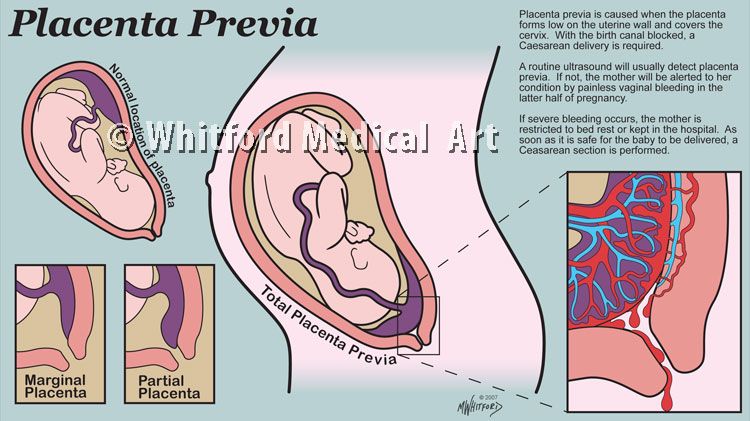
- Placenta previa: In this condition, the placenta is attached too low in your uterus and blocks your baby's exit through your cervix.
- Transverse lie: The baby is in a horizontal, or sideways, position in your uterus.
- Breech presentation: In a breech presentation, your baby's feet- or bottom-first in your uterus. Some providers may attempt to turn your baby, but a C-section will be necessary if that's unsuccessful.
- Health conditions: Conditions like heart disease could worsen with labor during a vaginal birth. A C-section is necessary if you have genital herpes at the time of delivery.
- Obstruction: A large uterine fibroid, a pelvic fracture or you're expecting a baby with certain congenital anomalies may also be reasons for a C-section.
An unplanned C-section delivery might be necessary if any of the following conditions arise during your labor:
- Labor isn't progressing: Also called prolonged labor, this means your cervix dilates and stops, doesn't efface (or thin) or your baby stops moving down the birth canal.

- Umbilical cord compression: The umbilical cord is looped around your baby's neck or body or caught between your baby's head and your pelvis.
- Umbilical cord prolapse: The umbilical cord comes out of your cervix before your baby does.
- Placental abruption: The placenta separates from the wall of your uterus before your baby is born.
- Fetal distress: Your baby might develop problems that cause an irregular heart rate during labor. Your obstetrician might decide that the baby can no longer tolerate labor and that a C-section is necessary.
How common are C-sections?
According to the Centers for Disease Control (CDC), C-sections account for about 30% of all deliveries in the United States.
Procedure Details
What can I expect before a C-section?
If you have a planned C-section, the following procedures will take place:
- You'll sign consent forms for the procedure.

- The anesthesiologist will discuss options for anesthesia. Most often, it's an epidural (or spinal block) that numbs you from your breasts down to your feet.
- The hair in the area around the incision will be clipped or shaved.
- A catheter will be inserted to keep your bladder empty.
- You will have heart and blood pressure monitors applied.
- You'll get an IV in your hand or arm to give you medicine and fluid.
- You'll discuss the procedure and what to expect with your obstetrician (if you haven't already).
If you need an emergency C-section, your obstetrician delivers your baby quickly because either the health of you or your baby is at risk. However, there's typically not much time to prepare, and you may need general anesthesia because it works faster.
What actually happens during a C-section?
The first step in a C-section procedure is preparing you for anesthesia. Most planned C-sections use an epidural, so you are awake for the delivery. However, in some cases, you're asleep under general anesthesia.
However, in some cases, you're asleep under general anesthesia.
Your abdomen will be cleaned with an antiseptic, and you might have an oxygen mask placed over your mouth and nose to increase oxygen to your baby. Next, your provider places a sterile drape around the incision site and over your legs and chest. Finally, your providers raise a sterile curtain or drape between your head and your lower body.
The obstetrician will then make an incision through your skin and into the wall of your abdomen. They might use either a vertical or transverse incision. A horizontal incision is also called a bikini incision.
Next, your provider cuts a 3- to 4-inch incision into the wall of your uterus. This incision can also be transverse or vertical. Finally, the obstetrician removes your baby through the incisions. The umbilical cord is cut, the placenta is removed and the incisions are closed with stitches and staples.
Emergency C-sections follow the same steps; however, the speed at which your baby is removed is different. During a planned C-section, the delivery takes about 10 to 15 minutes. Your provider removes your baby in only a few minutes in an emergency C-section.
During a planned C-section, the delivery takes about 10 to 15 minutes. Your provider removes your baby in only a few minutes in an emergency C-section.
If you're awake for your C-section surgery, you will be able to see and hold your baby shortly after it's born.
What does a C-section feel like?
You'll be under anesthesia, which should prevent you from feeling any pain. Most people report feeling a tug or pull when their baby is removed from their abdomen.
Are C-sections safe?
Vaginal births are usually preferred, but in some cases, a C-section is the only safe option. For example, a C-section is the safer option when your baby is breech or you have placenta previa (placenta covers part of the cervix). A C-section carries risks and benefits, which should be discussed with your pregnancy care provider.
How long does a C-section surgery take?
The typical C-section takes about 45 minutes from start to finish. After your provider delivers your baby, they'll stitch your uterus and close the incision in your abdomen. Different types of emergencies can arise during a delivery. In some cases, the delivery will happen very quickly, with your baby being delivered in as little as 15 minutes. This is an emergency C-section.
Different types of emergencies can arise during a delivery. In some cases, the delivery will happen very quickly, with your baby being delivered in as little as 15 minutes. This is an emergency C-section.
What happens after a C-section?
Like vaginal births, your obstetrician will deliver the placenta after your baby is born. Next, your provider will stitch your uterus and stitch or staple your abdominal muscles. Stitches should dissolve, but staples are removed at the hospital about one week later. Your abdomen will be sore for several days or weeks. In some cases, your provider may prescribe stronger pain medication.
You can expect to limit your activities, take it easy and rely on family and friends once you go home. A typical C-section surgery requires at least two to three days in the hospital.
Risks / Benefits
What are the benefits of a C-section?
The advantages of a C-section depend on your pregnancy. In most cases, the biggest benefit of a C-section is that it's safer for both you and your baby. When a vaginal birth is risky or could hurt your baby, most providers will turn to a C-section to minimize risks. Sometimes C-sections are unplanned. For example, if your baby's heart rate drops to an unsafe level, an emergency C-section is safer than letting your baby's heart rate decline further.
When a vaginal birth is risky or could hurt your baby, most providers will turn to a C-section to minimize risks. Sometimes C-sections are unplanned. For example, if your baby's heart rate drops to an unsafe level, an emergency C-section is safer than letting your baby's heart rate decline further.
What are the risks involved in a C-section?
Like any surgery, a C-section involves some risks. The risks of complications are slightly higher with C-sections than with vaginal delivery. These might include:
- Infection.
- Loss of blood (hemorrhage).
- A blood clot that may break off and enter your bloodstream (embolism).
- Injury to the bowel or bladder.
- A cut that might weaken the uterine wall.
- Abnormalities of the placenta in future pregnancies.
- Risks from general anesthesia.
- Fetal injury.
Other disadvantages of having a C-section are:
- Recovering from a C-section may be more difficult than a vaginal delivery.

- C-sections are more likely to cause chronic pelvic pain.
- You're more likely to have a C-section in future pregnancies.
- Your baby may have trouble breastfeeding.
- Your baby may be at greater risk for breathing problems.
Recovery and Outlook
How long does a C-section recovery take?
Once the anesthesia wears off, you’ll begin to feel the pain from the incisions. You might also experience gas pains and have trouble taking deep breaths. Make sure an adult is there to help you get up from bed the first several days following C-section surgery. Most people stay in the hospital between two and three days.
A full recovery can take between four and six weeks. Ask your healthcare provider what you can expect during recovery. Most providers recommend avoiding steps, lifting, exercise and other strenuous activities for several weeks. Ask your friends or partner for help with errands, cooking and cleaning so you can rest and recover. Your provider may put restrictions on driving until you're able to turn your body and apply pressure to the pedals with ease.
You can expect cramping and bleeding for up to six weeks, as well as some discomfort around the incision. Taking over-the-counter pain relievers such as acetaminophen or ibuprofen for pain may help. Avoid sex for at least six weeks or until your healthcare provider gives you the OK.
You will also have a vaginal discharge after the surgery due to the shedding of your uterine lining. The discharge, called lochia, will be red at first and then gradually change to yellow. Be sure to call your healthcare provider if you experience heavy bleeding or a foul odor from the vaginal discharge. Use sanitary pads, not tampons, until you're completely done bleeding.
Can I have a baby vaginally after a C-section?
The majority of people who had a C-section can consider a vaginal delivery in future pregnancies. If you meet the following criteria, your chances of vaginal birth after cesarean (VBAC) are significantly increased:
- Your provider used a low transverse incision.

- Your pelvis is not too small to accommodate an average-sized baby.
- You're not expecting multiples.
- Your first C-section was only performed because your baby was breech.
When to Call the Doctor
When should I see my healthcare provider?
If you have an infection at your C-section incision, contact your healthcare provider. Watch for signs of infection such as:
- Red or swollen incision.
- Pus or leaking discharge from the incision.
- Fever or worsening pain.
Other signs of a problem include heavy bleeding or severe pelvic pain and cramping.
Additional Details
What is more painful: a C-section or natural birth?
The level of pain you experience during childbirth is unique. For example, if you opt for an unmedicated vaginal birth, you can expect more pain than someone who had an epidural before a vaginal birth. During a C-section delivery, you won't feel much pain. However, recovering from a C-section may be more painful and take longer than recovering from a natural birth. There isn't a right or wrong answer as to what is more painful because every birth is different.
There isn't a right or wrong answer as to what is more painful because every birth is different.
How many C-sections can you have?
The number of C-sections you can have is unique to your medical history and pregnancy. An exact number hasn't been agreed on. The surgery may be slightly more complicated each time due to prior incisions or scarring.
A note from Cleveland Clinic
C-sections are often necessary for the health of you and your baby. If you know you're having a C-section, your obstetrician can walk you through the procedure and discuss the recovery process with you in advance. In the cases where a C-section is unexpected, you may end up feeling upset that your birth plan didn't go as expected. Just know that most providers prefer a vaginal delivery and that the decision to proceed with a C-section was made for you or your baby's wellbeing. The best thing you can do after a C-section delivery is rest and allow others to help you recover.
Birth beds Partura
In stock
Price on request
Price includes standard equipment without footrests and other accessories
Order
Partura is a new approach to childbirth - a combination of comfort, flexibility and safety.
In modern medical practice, special attention is paid to both safety and satisfaction of the needs of the patient. The new birthing bed from Schmitz meets these requirements. Attractive design and maximum comfort for the expectant mother and the most favorable working conditions for the obstetric team.
Partura birthing beds are designed in such a way that the mother-to-be has maximum freedom of movement during the first stage of labor and during the delivery of the fetus. With the manual control of the Partura birthing bed, you can adjust it infinitely. The woman in labor can adjust the profile of the Partura table according to her own needs.
The pleasantly upholstered surface of the Partura table is large enough to allow the partner to actively support the mother-to-be. The leg section can be used as a midwife seat.
The soft, smooth cover and cushions of the Partura table are easy to clean and disinfect. If necessary, the Partura table can be adapted for urgent surgical intervention in two or three steps. New generation Partura birthing beds for easy and safe delivery.
- The main section of the generic bed includes ischial, support and leg sections, on casters, central lock.
- Butt section has a 150mm radius cutout.
- Mattress - two-piece for seat and leg sections; made of highly elastic foam rubber; water repellent and non-slip.
- Shell and frame made of powder-coated sheet steel.
- Two-piece white cover, washable up to 95°C.
- Main and foot section separated. The foot section can be slid under the main section in four fixed positions.
- Leatherette covered back support attaches to the head or leg side.

- Finish color can be selected from the color list.
- Two Goepel type footrests, 18/10 stainless steel, leatherette-coated one-piece foam padding, height adjustable.
- Two swivel joints for attaching leg supports.
- Two handles, 18/10 stainless steel, leatherette-coated foam pad; attached to the side of the table.
- Transfusion stand with 4 hooks, 18/10 stainless steel. Can be installed in the head or next to the handles, height adjustable.
- Back support next to the butt section cutout; semi-circular foam lining with leatherette coating.
For childbirth in a squatting position. - Two control panels, left and right of the main section.
- Motorized unlimited adjustment:
- Main section height adjustment
- Base section adjustment
- Butt section adjustment
- Surface slope (in case of shock)
- Foot section height adjustment (in connection with the main section)
- Built-in emergency power supply in case of momentary power failure.

| First stage of childbirth. The Partura table is in the lower position (64 cm) for rest or movement. The low height of the Partura table makes it possible to rise from the table and lie down on it. | The second stage of labor in an upright position with a partner. A woman can lean on her partner. | ||
| Childbirth in the classical position. | Childbirth in a squatting position, optimization of the birth axis, the perineum is relaxed. | ||
| Childbirth in a squatting position with a partner. When the fetal head appears, the man can slightly lift the woman. | The first stage of labor and / or an intermediate stage in the knee-elbow position in case of attempts with the passage of the cervix remaining in the same position or in case of intrauterine asphyxia. | ||
| Surgical delivery, forceps delivery or vacuum extraction, manual breech delivery, postpartum perineal treatment, manual removal of the placenta. | Childbirth in the knee-elbow position for multiparous women, if it is necessary to relax the perineum or when giving birth to especially large children. | ||
| Caesarean section in the delivery room. |
| The second stage of labor in an upright position is a comfortable sitting position. A cutout in the mattress eliminates pressure on the perineum. In the case of breech presentation of the fetus, manual squeezing is possible. | |
| The situation in case of shock is a prolapse of the sex cord or a large loss of blood. | After childbirth in the knee-elbow position. After the fetus is released, the woman does not need to roll over. | ||
| Childbirth in the Trendelenburg position in case of pathological childbirth, surgical intervention or manual squeezing. | Raise your legs to relax. |
| Main section height adjustment | 645–925 mm |
| Foot section height adjustment | 460–925 mm |
| Delivery table dimensions including backrest | 2330 × 1015 mm |
| Mattress length on back support | 890 mm |
| Mattress length at butt section | 350 mm |
| Mattress length on foot section | 695 mm |
| Mattress thickness | 80 mm |
| Angle of inclination of the table surface | 0–12° |
| Back section adjustment angle | 0–78° |
| Seat section adjustment angle | 0–27° |
| Weight | 280 kg |
| Supply voltage | 230 V, 50 Hz, 0. 36 kW 36 kW |
Upholstery color selection
SCHMITZ PARTURA gynecological delivery bed
The Partura delivery bed from the well-known manufacturer Schmitz will create all the necessary conditions for a comfortable delivery and other gynecological and obstetric procedures. The Partura birthing bed fully meets all the requirements and quality parameters, is distinguished by a safe and reliable design that will be as comfortable as possible for a pregnant woman and obstetricians.
Benefits of the Partura delivery bed
- Extended use. The peculiarity of the Partura birthing bed is that it expands the possibilities of operation, providing complete freedom of movement for the expectant mother, not only during childbirth, but also after the birth of the fetus. The high ergonomics of the manual control system helps to adjust the birthing bed. In addition, the woman herself can also change the profile of the table according to individual requirements.
- Comfortable conditions for everyone. The Partura Birthing Bed has a large comfortable surface to accommodate a partner (if required). Thanks to the thoughtful design, soft padding and ergonomic leg section that can be used as an additional seat for an obstetrician, childbirth will be comfortable for the woman in labor, her partner and doctors.
- Ergonomic upholstery and surface of the delivery bed. Accessories are easy to clean and disinfect, the upholstery materials make it as quick and effortless as possible.
- Ability to adapt to any circumstances. The gynecological delivery chair has a flexible design that can be easily adapted to any type of delivery, depending on the circumstances and the wishes of the woman or doctor. Another advantage of the delivery bed is the ability to adapt the table for emergency surgery.
- Wide choice of colors. Partura birthing bed will become an indispensable part of the interior and furnishing design thanks to the choice of any color and its shade.

Delivery bed set Partura
The table shows the main components of the Partura delivery bed 140.100:
| Main bed section (composition of the section) |
|
| Ischial section | cut-out radius 150 mm. |
| Delivery bed mattress | 2 parts for seat and leg section; material: high elastic foam rubber; water repellent and non-slip. |
| Birthing bed upholstery and frame | in powder coated sheet steel. |
| Back support | near butt section cutout; semi-circular foam lining with leatherette coating. |
| Motorized unlimited adjustment |
|
| Back support | leatherette coated head or leg side. |
| Integrated emergency power supply | in case of momentary power failure. |
| Transfer stand | with 4 hooks, material - stainless steel 18/10. Can be installed in the head or next to the handles, height adjustable. |
| Two footrests | Goepel style, 18/10 stainless steel, leatherette-coated one-piece foam liner, height adjustable. |
| Two control panels | to the left and right of the main section. |
| Main and foot sections | separate |
| Two handles | 18/10 stainless steel, leatherette coated foam lining; attached to the side of the table. |
| Two rotating joints | for attaching leg supports |
| Leg section | suggests the possibility of placing under the main one in four fixed positions. |
| Finish color | Optional. |
| White case | two-piece, wash up to 95 °C. |
Specifications of the PARTURA delivery bed
The table shows the parameters and main specifications of the bed:
| Main section height adjustment | 645–925 mm |
| Foot section height adjustment | 460–925 mm |
| Delivery table dimensions including backrest | 2330 × 1015 mm |
| Mattress length on back support | 890 mm |
| Mattress length on butt section | 350 mm |
| Mattress length on leg section | 695 mm |
| Mattress thickness | 80 mm |
| Table top angle | 0–12° |
| Back section adjustment angle | 0–78° |
| Seat section adjustment angle | 0–27° |
| Weight | 280 kg |
| Supply voltage | 230 V, 50 Hz, 0. |
Partura delivery bed positions
| 1st stage of labor. Birthing bed Partura is in the lower position (64 cm) for rest or movement. The low height makes it possible for a woman to rise from the table and lie down on it. | 2nd stage of labor in an upright position (partner expected). A woman in labor has the opportunity to lean on her partner during childbirth. | ||
| Classic position for childbirth. | Squatting position, optimization of the birth axis, relaxed perineum. | ||
| Squatting position (partner expected). When a fetal head appears, a man can help a woman by lifting her up a little. | The first stage of labor and/or the intermediate stage in the knee-elbow position in case of attempts with the passage of the cervix remaining in the same position or in case of intrauterine asphyxia. | ||
| Delivery position (suggesting surgery), forceps delivery or vacuum extraction, manual breech delivery, postpartum perineal debridement, manual removal of the placenta. | Knee-elbow position for childbirth of multiparous women, if it is necessary to relax the perineum, also when giving birth to large children. | ||
| Position for caesarean section in the delivery room. | 2nd stage of labor in an upright position - comfortable sitting position. A cutout in the mattress eliminates pressure on the perineum. In the case of breech presentation of the fetus, manual squeezing is possible. | ||
| Position in case of shock - genital cord prolapse or significant blood loss. | Knee-elbow position for the period after childbirth. After the fetus is released, the woman does not need to roll over. | ||
| Trendelenburg birthing bed position for pathological deliveries, surgery or manual squeezing. | A position where the legs are raised to relax. |
Maternity bed color options
The RAL color chart includes more than 40 shades and their combinations. You can opt for muted pastels, vibrant hues or original color combinations.
Protective colors
Left to right:
- gray white RAL 9002,
- pure white RAL 9010,
- alabaster gray RAL 0007500*,
- light gray RAL 7035,
- anthracite gray RAL 7016,
- intense black RAL 9005,
- white aluminum RAL 9006,
- gray aluminum RAL 9007,
- RAL yellow 1009050*,
- signal yellow RAL 1003,
- yellow-orange RAL 0506060*,
- ivory RAL 1015,
- sand beige RAL 0607030*,
- copper brown RAL 8004,
- antique pink RAL 3014,
- RAL lilac 3108010*,
- green RAL 1808010*,
- green - herringbone RAL 1703020*,
- lemon green RAL 1206050*,
- leaf green RAL 1206050*,
- blue RAL 5018,
- white-blue RAL 2408015*,
- light blue RAL 2606030*,
- sapphire blue RAL 5003.

* RAL 9 halftones are marked with an asterisk0005
Upholstery colors
Left to right:
- mint green 80,
- marsh green 81,
- Caribbean blue 82,
- atlantic blue 83,
- parchment beige 85,
- golden yellow 86,
- tobacco brown 87,
- granite gray 89,
- platinum gray 90,
- titanium gray 91,
- intense red 92,
- natural brown 93,
- silver gray 55,
- ocean 52,
- black 57.
Accessories for delivery bed
| Picture of | Art. No. | Designation | Options |
| 104.681 | Tray |
|
 She can just sit down, leaning back.
She can just sit down, leaning back. 

 36 kW
36 kW 
 She can just sit down, leaning back.
She can just sit down, leaning back.