Peeling nipple breastfeeding
Breastfeeding and Nipple Scabs: Treatment, Prevention, and More
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Why do I have nipple scabs?
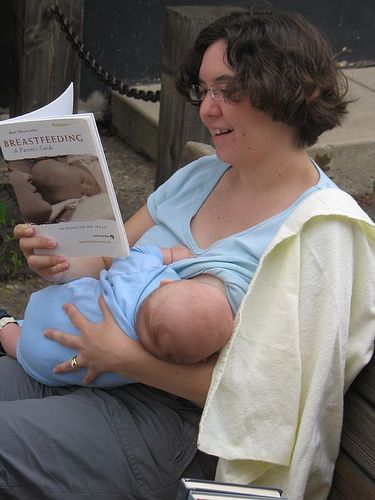
Breastfeeding is one of the leading causes of nipple scabs. Many women are surprised to find that breastfeeding, which seems so natural, is often a painful experience at first.
The good news is that while nipple pain and even cracked, bleeding, and scabbed nipples occur quite commonly, these are usually short-term issues that can be resolved. Even if it’s difficult at first, most women are able to breastfeed their babies.
One of the primary reasons for nipple scabs caused by breastfeeding is simply that the skin of your nipples is very sensitive. They’re not used to the level of abrasion and stimulation that occurs when breastfeeding.
It’s common for women to experience nipple pain during the first few days of breastfeeding, which then decreases as the nipples become accustomed to the process.
However, if a baby is positioned incorrectly, has a poor latch, or has anatomical issues such as a tongue-tie, nipple pain may not go away. These issues can even cause nipples to crack and bleed, which then leads to scab formation.
Yes, you can continue to nurse if you have nipple scabs. If you’ve developed nipple scabs or are experiencing pain with breastfeeding, it’s best to discuss it with your doctor or a lactation consultant immediately. They’ll be able to help troubleshoot and find solutions so your nipples can heal and you can breastfeed painlessly.
Lactation consultants may be available:
- at the hospital where you deliver your baby
- through your baby’s pediatrician’s office
- from local breastfeeding support groups
They can help ensure that your baby is positioned correctly and latching well. They can also assess your baby for what may be affecting their ability to nurse well.
While breastfeeding is one of the most common causes of nipple scabs, there are other reasons someone might develop scabs on their nipples. These include:
These include:
- Sports. Participating in sports such as running, cycling, or surfing can cause nipples to become chafed and scabbed.
- Eczema of the breast. Eczema is a skin condition that may cause nipples to become irritated to the point that they bleed and scab.
- Paget disease. A serious skin condition that causes scabs on the breast, Paget disease usually indicates cancer of the breast.
- Nipple injury. A nipple may be injured during activities, such as vigorous sucking or rubbing during sexual activity.
- Burns. Nipples may burn from exposure to tanning beds or the sun and scabs may form.
Breastfeeding
If you experience nipple pain, cracking, bleeding, or scabbing from breastfeeding, it’s best to consult your doctor or a certified lactation consultant immediately. They can help you determine the cause of your pain and find a solution. Nipple scabs are often caused by improper latching, which results in nipple trauma and injury.
Your lactation consultant may recommend treatments such as:
- pumping for a day or two while your nipples heal
- using a nipple shield
- applying purified lanolin ointment
- rinsing your breasts in saline after nursing
- using warm compresses or cold gel pads to help soothe your nipples
One study of nursing mothers found that applying peppermint essence to the nipples after feeding significantly reduced pain and promoted healing of injured nipples. Another solution to your nipple scabs may be simply changing the position you sit or lie when breastfeeding.
Exercise
If you’re an athlete with nipple scabs, it’s important to wear sports bras and clothing that fits well. Bras and bodysuits that’re too tight or too loose may exacerbate chafing. Fabric should also be breathable and moisture-wicking.
You also may be able to use purified lanolin ointment or powders to help reduce chafing. If your scabs are severe, you may need to take a short break from the activity that’s causing the scabs to allow them to heal.![]()
Rash
If you’re experiencing a rash accompanied by nipple scabs or nipple scabs that don’t have an apparent cause, it’s important to see your doctor. They can help determine why you have nipple scabs and ensure that you receive effective treatment.
Breastfeeding mothers can prevent nipple scabs by seeking help with any breastfeeding issues right away. Working with a certified lactation consultant can help you avoid pain.
To keep nipples moist and free of cracks throughout breastfeeding, it’s important to:
- practice good hand-washing to prevent infection
- keep breasts clean and dry
- apply purified lanolin or expressed breast milk
Shop for lanolin nipple cream.
Women who aren’t breastfeeding can help prevent nipple scabs by:
- avoiding burns from sun or tanning beds
- wearing breathable bras and clothing that fit properly
- keeping breasts clean and dry
- consulting your doctor if you develop a rash or scabs that don’t go away or don’t appear to have a cause
Nipple scabs commonly occur in breastfeeding mothers, especially at the very beginning. Women who aren’t nursing may also develop nipple scabs.
Women who aren’t nursing may also develop nipple scabs.
If you have nipple scabs, it’s important to talk to your doctor to determine the cause and begin the best course of treatment.
Nipple fissures: Causes, symptoms, and treatment
Nipple fissures are painful cracks on the skin of the nipple and areola. Nipple fissures are common during pregnancy and breast-feeding, but may be caused by friction in some athletes.
People who experience nipple fissures should treat them with care, as it is possible for the area to become infected.
Home treatments can provide relief in many cases, though there are times when it is important to see a doctor. Preventing nipple fissures before they happen is the best way to avoid symptoms and complications.
Fast facts on nipple fissure:
- Nipple fissures are common during pregnancy and breast-feeding.
- Knowing what causes them is the best way to prevent them from happening again.
- Antiseptic creams may help prevent infection while the nipples heal.

There are a variety of reasons why nipple fissures occur:
Pregnancy and breast-feeding
Share on PinterestNipple fissures may appear if a woman has problems with breastfeeding.Hormonal changes during pregnancy can cause the breasts to become more full. The extra fullness can stretch the skin and irritate the areola and nipple, which may lead to fissures.
Women who have problems with breast-feeding may also develop nipple fissures. If the baby does not latch on correctly, they may put too much force on the sensitive skin of the nipple and areola. This could cause unnecessary irritation.
Nipple fissures may also be a symptom of thrush, which is a fungal infection.
While nipple fissures are often dry cracks, too much moisture may also be responsible for these symptoms. This may be due to breast-feeding for too long or the nipples being damp for an extended period, either from leakage, wet nursing pads, or too much ointment.
While nipple fissures tend to be prevalent in pregnant and breast-feeding women, the cracks can occur in anyone.
Friction
Too much friction may also irritate the nipple area. For example, long-distance runners might develop what is known as jogger’s nipple or runner’s nipple.
Friction from the cloth of a loose shirt or a poorly fitting bra can rub against the sensitive nipple skin, causing chafing, cracks, and even bleeding. Nipple fissures caused by friction may also occur in surfers and bodyboarders due to the board and seawater rubbing against the nipples while paddling.
Certain fabrics may be more irritating than others, with synthetic fibers, such as nylon, often causing more damage.
Allergic reaction
Nipple fissures may also be due to an allergic reaction to something touching the skin. These allergens can be chemicals or fragrances in products such as:
- laundry detergent
- fabric softener
- shampoo or conditioner
- soap or shower gel
- lotion or moisturizer
- perfume
If irritation and nipple fissures occur after applying a product, it is possible that the person’s skin is sensitive to the chemicals or fragrances in that product. Dermatologists may be able to recommend replacements to prevent the symptoms from coming back.
Dermatologists may be able to recommend replacements to prevent the symptoms from coming back.
Depending on the cause, nipple fissures can develop on one or both nipples. Symptoms can vary from person-to-person, but the trademark symptom is cracked, painful skin on the nipple or areola. It may also be accompanied by:
- chapped, dry skin
- open cracks that may ooze or bleed
- redness
- soreness
- crusty or flaky skin
- scabs forming in the area
Share on PinterestStudies suggest that peppermint oil may help to keep treat nipple fissures.
Many people find that keeping the affected nipple and surrounding skin slightly moist with a natural oil or moisturizer is an essential first step to treatment.
A study posted to the Journal of Caring Sciences found that lanolin, peppermint oil, and dexpanthenol creams all had a similar effect on nipple trauma in breast-feeding women. Some people are concerned, however, that the use of any nipple cream may interfere with the natural environment where newborns establish breast-feeding.
It is important to remember that too much moisture may make symptoms worse. Women who are breast-feeding should avoid non-breathable bra pads, as they can hold too much moisture against the nipple.
During pregnancy, the glands surrounding the nipples secrete a natural oil that lubricates and discourages bacteria. When washing this area, women should use only clean water that does not strip away this natural protection.
Breast-feeding women may find relief from bathing their nipples in warm water and applying warm compresses to help soothe any irritation after the baby has fed. Expressing some milk and rubbing it into the nipples before each feeding or pumping may also soothe irritation.
Some people may find similar relief by applying diluted peppermint oil or peppermint water to the affected nipples between feeding.
Breast-feeding women with nipple fissures may also be able to avoid further complications by encouraging the baby to latch onto the breast with a full mouth, alternating breasts at each feed, or using a nipple shell between feeds to allow air to circulate to the nipple.
Using a nipple shield during breast-feeding may keep the nipple too moist, which might make symptoms worse.
Athletes can often help the fissures heal by avoiding loose, rough, or scratchy shirts and covering the nipples with soft gauze or waterproof bandages while active.
If symptoms are left untreated, nipple fissures can lead to more serious complications, such as inflammation or infections. Breast infections may cause abscesses to form, which could require antibiotics, laceration, and drainage.
Nipple thrush is a possible complication in breast-feeding women. Babies with thrush may pass germs from their mouth into the breast milk. The Candida yeast that causes thrush can thrive in the warm, dark environment within the milk ducts, possibly leading to an infection. Many women find that cleaning the nipple in warm water after feeding can help remove the excess milk that may be home to germs.
While most people can treat nipple fissures successfully at home, there are occasions when it is better to see a doctor. A doctor should diagnose symptoms that get worse or do not go away with treatment.
A doctor should diagnose symptoms that get worse or do not go away with treatment.
A doctor should also check out very painful or irritated nipples that make a person’s daily life difficult. Anyone who has signs of infection should visit their doctor for proper treatment. Signs of infection include redness, swelling, warmth, and tenderness in the nipple and surrounding skin.
Women who have developed nipple fissures through breast-feeding may want to talk to a doctor or pediatrician for support. A professional may offer breast-feeding tips or refer the woman to a lactation coach.
There are several ways that a person can reduce the chances of developing nipple fissure:
Sports
Share on PinterestWearing rash guards when surfing and bodyboarding is recommended to avoid chafing.
If nipple fissure is caused by friction during sports, a person could try changing the type of fabric they wear or place waterproof bandages over the nipples to help reduce friction and avoid fissures.
Some runners, surfers, and other athletes may find that applying an anti-chafing balm to their nipples before they exercise can help reduce friction.
Many surfers and bodyboarders simply wear rash guards or wetsuits to avoid irritation.
Tight fitting clothing that helps wick sweat away from the body may help some. Female athletes should be sure to wear a well-fitting sports bra to support the breasts and avoid unnecessary friction.
Breast-feeding
To prevent or reduce the chances of developing nipple fissures, a breast-feeding woman should ensure that she does certain things each time the baby latches on.
While breast-feeding may cause discomfort at first, it is important for both mother and baby to be comfortable during breast-feeding. If the baby has not latched on correctly or if feeding is causing pain, it is best to reposition them. Both mother and child should be relaxed, and the baby should not have to turn their head or body while feeding, as it could pull at the nipple and irritate it further.
Helping the baby latch onto the breast accurately during feeding can also help prevent irritation. The baby should take the entire nipple and part of the areola into their mouth during feeding. Having a full mouth helps keep them from biting down too hard on one part of the nipple, which could irritate the skin.
An allergic reaction
If nipple fissure is caused by an allergic reaction to something, then identifying the irritant and avoiding it however possible may prevent symptoms developing. A person might choose to visit a dermatologist who can carry out some tests to identify potential allergens.
Nipple fissures can be a source of pain and discomfort, but treating them is usually straightforward. Breast-feeding women who have nipple fissures may need to change their feeding habits to continue feeding a baby. In some situations, prevention may be the best option.
Anyone with symptoms that get worse or do not improve should see a doctor to avoid complications.
treatment and prevention of breastfeeding
When breastfeeding, some women develop cracked nipples 1 , accompanied by severe pain. Such cracks can cause the refusal of natural feeding and the transfer of the baby to the mixture, although breast milk is much healthier for the baby. It contains not only nutrients, but also maternal antibodies that provide protection against infections. In addition, with breastfeeding, there is a closer contact between mother and child, which is important for their further relationship and the harmonious development of the baby. Prevention and timely treatment can eliminate nipple cracks, while maintaining breastfeeding.
Crack symptoms
1.2 Nipple cracks are linear lesions that run from the center of the nipple to its edge (areola). They can be single or multiple, of different depths, on one or both mammary glands. Cracks in the female nipples are accompanied by severe pain during breastfeeding or even when touched. The deeper the damage, the stronger the pain. Sometimes a clear liquid or ichor may be secreted. If the cracks are not treated, infectious complications may occur: redness increases, purulent discharge from the wounds appears, and inflammation develops.
The deeper the damage, the stronger the pain. Sometimes a clear liquid or ichor may be secreted. If the cracks are not treated, infectious complications may occur: redness increases, purulent discharge from the wounds appears, and inflammation develops.
In other words, cracked nipples during breastfeeding are a common problem in the very first days of a baby's life.
There are a number of factors that cause cracks 4 :
- Incorrect nipple latch
The baby must latch onto the nipple completely, including the areola. In this case, the load during sucking is distributed evenly, and the milk freely enters the baby's mouth. If the baby only grabs the nipple, no milk is released from the breast, the baby presses and pulls harder on the limited area, which leads to damage to the skin of the nipple. At the same time, milk remains in the breast, stagnation (lactostasis) is formed, which leads to inflammation - mastitis. - Irregular nipple shape
A flat or inverted nipple makes it harder for your baby to latch on properly and increases the risk of abrasions and cracks.
- Incorrect weaning
If you try to take the breast away from the baby while suckling, he instinctively squeezes her gums even tighter, damaging the skin of the nipple. You can take out the breast only when the baby releases it himself. - Sustained suckling
Feeding should not last longer than 30 minutes 3 - there is no milk left in the breast, but the child continues to injure the nipple. If your baby has a firm grip on the nipple, you can insert a clean finger from the side into his mouth to help loosen the grip. - Incorrect pumping
Too much pressure on the nipple by hand or with a breast pump also causes cracks. - Mixed feeding
If a baby is breastfed, then from a bottle, he "loses the settings": it is not immediately possible to "calculate" the force necessary to suck milk out of the breast. Because of this, pressure on the skin of the nipple may be excessive. In addition, the "technique" of sucking at the breast and nipple is different, which is why mixed feeding can sometimes lead to improper nipple latch.
- Excessive hygiene
Frequent use of soap destroys the water-lipid layer that protects the skin. It becomes dry, and cracks may appear from this. It is recommended to use pH-neutral products no more than twice a day. It is important to pay attention to the composition of cosmetics: all components must be safe for the baby. It is strictly forbidden to use alcohol-containing solutions - they greatly dry the skin, destroying the lipid layer. - Deficiency of vitamins and minerals in a woman's body
During pregnancy, a woman's body shares essential nutrients with the fetus, and after childbirth, it often remains in a state of their deficiency. Hypovitaminosis, lack of trace elements lead to a decrease in the elasticity and protective properties of the skin, which, in turn, can cause cracks in the female nipples. - Thrush of the oral mucosa in a child
If a whitish coating appears in the baby's mouth caused by Candida albicans fungi, it means that the skin of the breast comes into contact with them at each feeding: this neighborhood can also provoke cracks in mother's nipples.
- Use of synthetic underwear and liners
Thick, absorbent liners and underwear made of synthetic fabrics make it difficult for the skin to “breathe”, and prolonged contact with a humid environment increases the risk of inflammation and infectious complications.
The main cause of complications is bacteria present on the surface of the skin: staphylococci, streptococci. Under certain conditions, they begin to multiply intensively and cause inflammation. Overheating and high humidity contribute to their reproduction. Such conditions are created when milk leaks, irregular replacement of inserts in a bra 1.3 .
The most common complication caused by cracked nipples is mastitis, an inflammation of the mammary gland. Its characteristic features are redness, swelling, hardening of the chest, often accompanied by an increase in body temperature. A woman experiences acute pain, aggravated by pumping. Impurities of blood and pus appear in milk, so breastfeeding is immediately stopped.
Feeding technique
3In order not to have to get rid of cracked nipples, it is important to start the feeding process right from the start. The newborn is applied to the mother's breast in the first half hour of life for at least 30 minutes, if the mother and baby do not have health problems preventing this. This is an important moment for establishing a psychological connection and stimulating lactation. The woman does not yet have milk, the child manages to get only a little colostrum - a concentrate of useful substances released from the mother's mammary glands after childbirth.
Subsequently, it is recommended to use the free-feeding technique - the baby is breastfed not on time, but on demand. In a newborn it is 10-12 times, by the end of the first month of life - already 7-8 times a day.
The main thing in feeding technique is the correct "grip", so that the nipple and areola completely fill the baby's mouth. To do this, the baby's mouth, when applied to the breast, should be wide open, the lower lip turned outward, and the chin should touch the mother's breast. If the child does not open his mouth wide enough, you need to stroke the cheek or lower lip with a nipple or finger - a sucking reflex will work, providing mouth opening and characteristic lip movements.
If the child does not open his mouth wide enough, you need to stroke the cheek or lower lip with a nipple or finger - a sucking reflex will work, providing mouth opening and characteristic lip movements.
It is advisable to refuse supplementation with water or glucose solution, the use of nipples and bottles. Breast milk contains everything a baby needs, and pacifiers change sucking technique, which can lead to improper nipple latch.
Care must be taken to ensure that the baby suckles adequately at the breast or expresses excess milk to prevent cracking in the mother's nipples, which can provoke lactostasis and the development of mastitis.
Before the birth of a child, 1 :
- Wash chest daily with warm water. In the last trimester, it is better to give up soap, as the areola glands secrete a natural protective lubricant. Soap washes it off, and after childbirth, cracks may appear on the nipples.
- After washing, it is useful to do a light massage of the nipples with cosmetic oil.

- Contrast baths (alternate use of hot and cold water) help to train the contraction and relaxation of the muscles of the nipple area, which will further facilitate breastfeeding.
- It is recommended to rub the breast daily with a rough cloth (terry towel): the less sensitive the skin, the less likely it is to develop cracked nipples from breastfeeding.
After the baby is born, preferably 1.2 :
- Wash breasts with warm water as needed (no soap), then gently pat dry with a paper or textile towel. It is advisable to use soap no more than 1-2 times a day, so as not to overdry the skin and reduce the risk of soap and milk entering the child's body.
- Do not use an alcohol-containing product for nipple care - this greatly dries the skin and destroys its protective lipid layer.
- Use special bra pads made from natural materials that are breathable and absorbent. They need to be changed regularly to avoid prolonged contact with moisture, which often causes cracks in mother's nipples.

- Attach the baby more often to the healthy breast if cracks appear on one breast. This will allow the skin on the second mammary gland to recover.
- Arrange air baths for the chest.
- Use special creams and ointments that soften and moisturize the skin of the nipples, increasing its protective properties. These funds, as a rule, can also be used to treat cracked nipples in nursing mothers. They are applied immediately after feeding, so that before the next application to the breast, the product has time to be absorbed and act. Residues of the cream can remain on the surface of the nipples even after washing, which means that there is a possibility of it getting into the baby's body. For this reason, it is important to carefully choose the drug, giving preference to products with a natural and safe composition.
Timely treatment of nipple cracks is the prevention of infectious complications that require antibiotic therapy and interruption of breastfeeding. 1.2
1.2
Cracked nipples are not a reason to refuse breastfeeding, which is so important for mother and baby. It is necessary to heal the cracks as soon as possible, and when feeding, use silicone pads that reduce pressure on the nipples and the pain caused by it. If cracks appear on one breast, it is worth putting the baby to a healthy one more often to allow the skin on the second mammary gland to recover. It is important to follow the rules of hygiene and arrange air baths for the chest. In addition, it is recommended to use after each feeding special means for healing nipple cracks in the form of an ointment or cream. Timely treatment of nipple cracks is the prevention of infectious complications that require antibiotic therapy and interruption of breastfeeding. 1.2
Treatment of nipple cracks in breastfeeding
Types of nipple cracks, causes and consequences of their occurrence common problems faced by breastfeeding women. They can occur both at the very beginning and in the later period of breastfeeding.
 The main reasons for the appearance of cracks in the nipples during feeding are improper breastfeeding by the child, violation of the sucking mechanism (short frenulum, hypo-, hypertonicity and impaired tongue motility), incorrect, rough weaning of the child from the breast, fungal infection.
The main reasons for the appearance of cracks in the nipples during feeding are improper breastfeeding by the child, violation of the sucking mechanism (short frenulum, hypo-, hypertonicity and impaired tongue motility), incorrect, rough weaning of the child from the breast, fungal infection. Cracks in the nipples are:
- on both or one gland;
- multiple and single;
- deep and superficial.
They can be located both in the very center of the nipple and at its base, even moving to the areola. Deep bleeding wounds serve as a reason for temporary, for the period of treatment of cracks in the nipples, to stop attaching the child to the diseased breast. To prevent milk from stagnating, it must be expressed manually, and then fed to the baby. It is undesirable to use a breast pump in such cases, since the vacuum created by it increases damage and bleeding. With shallow injuries, when blood is not released from the cracks, and there is no scab - "crusts", you can continue to breastfeed the baby, provided that improper attachment and grip are corrected.
What causes nipple cracks due to improper feeding technique
When a mother is just learning to breastfeed, pain and cracks indicate a very serious violation - improper breastfeeding. At the same time, feeding becomes painful from the very beginning. A change in the shape of the nipple after sucking is characteristic - it becomes evenly flattened from above and below or beveled on one side. With proper attachment to the breast and sucking technique, the nipple after feeding has an elongated, even cylindrical shape.
If the latch is wrong, sucking is not effective - the baby cannot get all the milk, therefore, it stays at the breast for a very long time, but remains hungry. This can lead to insufficient weight gain for the baby and, as a result, the appointment of an artificial mixture by the pediatrician. Moreover, a baby who is not gaining weight often does not have enough strength to suck out mother's milk, and he has to be fed with expressed milk.
Insufficient release of milk from the mammary glands due to inefficient suckling, replacement of mother's milk with artificial formula, or both, can lead to lactostasis. Which subsequently leads to a decrease in lactation - hypogalactia. This starts the process of completing lactation at its very beginning.
Which subsequently leads to a decrease in lactation - hypogalactia. This starts the process of completing lactation at its very beginning.
From all of the above, it becomes clear how important it is to immediately learn how to properly feed the baby, and when pain and cracks appear on the nipples with breastfeeding, immediately begin to solve this problem.
Nipple thrush
Another cause of cracked nipples during breastfeeding is mycosis (fungal infection). It is less common and can appear at any time, often against the background of a well-established HS. It is characterized by the appearance of acute "shooting" pain from the nipple deep into the mammary gland, even outside of feeding or at the end of it. Other skin manifestations, except for one or more cracks, may not be. If the doctor suspected my mother's nipple mycosis, then he will definitely check the child's oral cavity - it is often combined with thrush in a baby. Accordingly, it is necessary to eliminate the fungal infection at the same time in the mother and child.
Cracks in the nipples in HB serve as a source of infection in the breast tissue. As a result, it becomes inflamed - mastitis. This most serious consequence of cracks requires immediate treatment.
Treatment of cracked nipples
Treatment of cracked nipples in breastfeeding mothers begins with the identification of the factor leading to their damage. In the first month after childbirth, most often, their appearance is associated with improper feeding technique. Therefore, treatment begins with finding out the reasons that prevent proper sucking.
If a short or rigid frenulum of the tongue is found, limiting its mobility or a violation of the tone of the child's tongue, then until these problems are resolved, the baby is transferred to feeding with expressed milk.
In case of incorrect attachment, the doctor begins the treatment of cracks by teaching the mother how to properly position the baby at the breast, how to ensure the baby has a correct grip. He will tell you what his signs are, he will teach you not to take the breast from the baby without trauma. With superficial damage to the nipple, this is enough to make feeding painless and the cracks heal quickly. In the case of deep cracks, the doctor will tell you about the features of caring for the nipples and breasts, and prescribe an effective treatment. If necessary, may recommend to temporarily stop applying the baby to the sore breast and switch to manual pumping.
He will tell you what his signs are, he will teach you not to take the breast from the baby without trauma. With superficial damage to the nipple, this is enough to make feeding painless and the cracks heal quickly. In the case of deep cracks, the doctor will tell you about the features of caring for the nipples and breasts, and prescribe an effective treatment. If necessary, may recommend to temporarily stop applying the baby to the sore breast and switch to manual pumping.
If cracked nipples during breastfeeding appear after a period of successful painless feeding, the doctor may suspect a fungal infection. After identifying characteristic complaints in the mother, the doctor prescribes a course of antifungal drugs that are compatible with breastfeeding. Since this disease is a pair disease - the child is necessarily infected, even if there are no manifestations visible to the eye - then the treatment is prescribed for the baby. Thus, the recurrence of the disease is prevented.
In severe advanced cases, the cracks may extend to the areola. Then the treatment of cracks in the nipple circumference in a nursing mother occurs simultaneously with the treatment of injuries associated with them.
Turning to the breastfeeding center "Laktovita" with a complaint - cracked nipples, you will receive full-fledged consultative and medical assistance. We will carry out diagnostics - find out the cause of the damage, teach you how to eliminate it, and help you quickly fix application errors. If necessary, we will prescribe an effective treatment for cracked nipples. In case of detection of lactostasis or mastitis, the doctors of our Center will immediately provide direct assistance and treatment. If hypogalactia occurs, it will help to increase the amount of milk.
Consultation on breastfeeding issues —
lactostasis, mastitis, nipple cracks, hypogalactia,
including:
All medical services are licensed. The posted price is not an offer.
Paid services with home visits are carried out in Moscow and the Moscow Region up to 30 km from the Moscow Ring Road.
Prices for calling specialists to your home within the Moscow Ring Road are indicated.
Specify the cost of calling a doctor outside the Moscow Ring Road by calling 8 (499) 700-08-80
or WhatsApp
Online consultation services are provided for the entire territory of the Russian Federation and other countries.
Appointment by phone 8 (499) 700-08-80
or WhatsApp
Cracked nipples in nursing mothers, how to cure and prevent them
and for the baby. But there are times when a woman is forced to deprive her baby of breastfeeding, thereby violating the laws of nature and partially destroying the connection with her offspring.
It is not uncommon for mothers to wean their babies because of cracked nipples. According to statistics, almost one in ten women faces the problem. Feeding in this case turns into torture, the chest hurts, and in some situations everything ends with mastitis. Expectant mothers need to know how to deal with the problem, and how to prevent it from occurring.
Feeding in this case turns into torture, the chest hurts, and in some situations everything ends with mastitis. Expectant mothers need to know how to deal with the problem, and how to prevent it from occurring.
Causes of cracked nipples
Several unfortunate circumstances lead to cracked nipples. Very often they act simultaneously, which further exacerbates the problem.
Most often, cracks appear when the baby does not grasp the nipple correctly or the mother behaves incorrectly at the time of feeding. Let's take a closer look at both of these factors.
1. Incomplete latch on the nipple
The sucking reflex in babies begins to form in the womb. Therefore, the process of eating milk from the breast is a reflex, within a few minutes after birth, the newborn is able to grab the nipple and suck out a few drops of milk from there.
But a small newborn baby does not always latch on correctly. If it is not directed, the delicate skin of the nipple may be damaged.
Here are some signs that the baby is suckling incorrectly:
- The mother feels pain during the feeding process
- The child holds only the nipple in his mouth.
- The areola is not captured and remains outside the infant's mouth.
When the breast is not properly latch on, nipple cracks appear very soon, making later breastfeeding difficult or completely impossible.
2. Abnormal cessation of feeding
It happens that babies fall asleep with a nipple in their mouth. It may seem to the mother that the baby has already eaten and is not suckling, she is trying to forcibly take him away from the breast. But at this moment, the muscles contract reflexively, the child does not want to let go of his “bowl of food”. If at this moment the nipple is sharply pulled out, cracks easily form on it.
Therefore, doctors do not recommend taking the nipple from a baby, even a sleeping one, he can eat in his sleep. When the baby is full, the breast itself will fall out of his mouth.
If you need to leave urgently, put your little finger into your mouth lightly. Then the tension of the muscles and jaws weakens, the nipple is easily and safely pulled out.
3. Errors when expressing
Most women do not need to express their milk with the on-demand method of feeding. But there are times when mom needs to be away for a few hours, or even for the whole day. There is a need to express the breast.
During pumping, you need to press on the breast and areola, if you press directly on the nipple, cracks will appear on it.
The breast pump also often causes cracks in the nipple when turned on at full force. First, microscopic defects of the epithelium appear, which can later turn into full-fledged cracks.
4. Mistakes of care
Women's breasts during the feeding period should be kept clean, but it is advisable not to overdo it with hygiene. A shower once a day is enough not to expose either yourself or the baby to infection. It is not recommended to constantly wipe the nipples with a soapy or alcohol solution.
It is not recommended to constantly wipe the nipples with a soapy or alcohol solution.
There are glands in the skin that constantly produce a protective lubricant. It makes the epidermis softer, has the properties of a natural antiseptic, helps wounds and minor injuries heal faster. If you constantly wash off this lubricant, the surface of the skin loses its normal natural protection.
Cracked nipples can also appear due to other factors associated with care errors:
- Excessively dry skin on the nipple and areola.
- Uncomfortable synthetic bras that rub against the skin.
- Thrush or candidiasis in the mouth of an infant.
- Allergy or hypersensitivity to detergents, soaps, etc.
- Spontaneous leakage of milk from the breast.
5. Soothers and teats on bottles.
The nipples and pacifiers given by the mother to the child can also cause nipple cracks. Sucking techniques for artificial substitutes and the mother's nipple are slightly different. But with the constant replacement of one for another, the child cannot orient himself. Using the same gripping methods on the nipple as on the shepherdess, the baby can damage it.
But with the constant replacement of one for another, the child cannot orient himself. Using the same gripping methods on the nipple as on the shepherdess, the baby can damage it.
Here is how the different sucking techniques differ:
- The baby does not need to open the mouth wide to latch on to the pacifier, unlike latch on to the mother's nipple with areola.
- When suckling, the baby presses the breast with his tongue, which contributes to a better separation of milk. When consuming food from a bottle, he compresses the papilla with his jaws.
- The pacifier is held by the baby in the area of the hard palate. The nipple during breastfeeding is located in the center of the oral cavity, covered by the tongue.
As you can see, the gripping techniques of a rubber or silicone nipple and a mother's nipple are completely different. With regular use of these aids, the baby begins to confuse them, the mother's breast suffers and nipple cracks form.
What are cracks
It is not difficult to distinguish cracks in the nipples. They resemble a groove or a narrow skin defect that runs from the top of the nipple towards the areola.
Nipple cracks are single and multiple, thin and rather wide, blue-eyed and located in the superficial layers of the skin. They appear on one or both mammary glands. First, the crack is dry, then ichor or blood begins to flow out of it.
The main symptom, which appears even before visible fissures, is pain when the gland is touched and sucked by the child.
When pathogenic microbes or fungus get into the cracks of the nipples, they become inflamed and gradually turn into ulcers.
Should I refuse to breastfeed my baby?
Cracked nipples are not a contraindication for breastfeeding. Even a temporary transfer of a child to artificial mixtures adversely affects lactation, after which it will be very difficult or impossible to resume it at all. Here's what mom should do:
1. In case of small cracks during feeding, it is recommended to use latex or silicone nipple covers. Now on sale there are products from different manufacturers - Avent, Chicco, Conpol, Pigeon, etc. The pads are selected taking into account the size of the areola and nipple.
In case of small cracks during feeding, it is recommended to use latex or silicone nipple covers. Now on sale there are products from different manufacturers - Avent, Chicco, Conpol, Pigeon, etc. The pads are selected taking into account the size of the areola and nipple.
2. With deep cracks in the nipples, the algorithm of actions is slightly different. It is not recommended to feed the baby, overcoming pain. You can express milk and feed the baby through a pipette. At this time, lubricate the nipples with medicinal preparations. It is not advised to use bottles, as the baby gets used to a completely different way of sucking, after which he may refuse to breastfeed.
Breastfeeding has to be stopped only in case of matitis, it is far from possible to return to it after treatment of the pathology.
In case of infection of cracked nipples, it is better to express and boil the milk to avoid infection of the baby.
What methods of treating cracks are dangerous and have no effect
Cracks in the nipples are formed already in the first couple of days after the start of breastfeeding.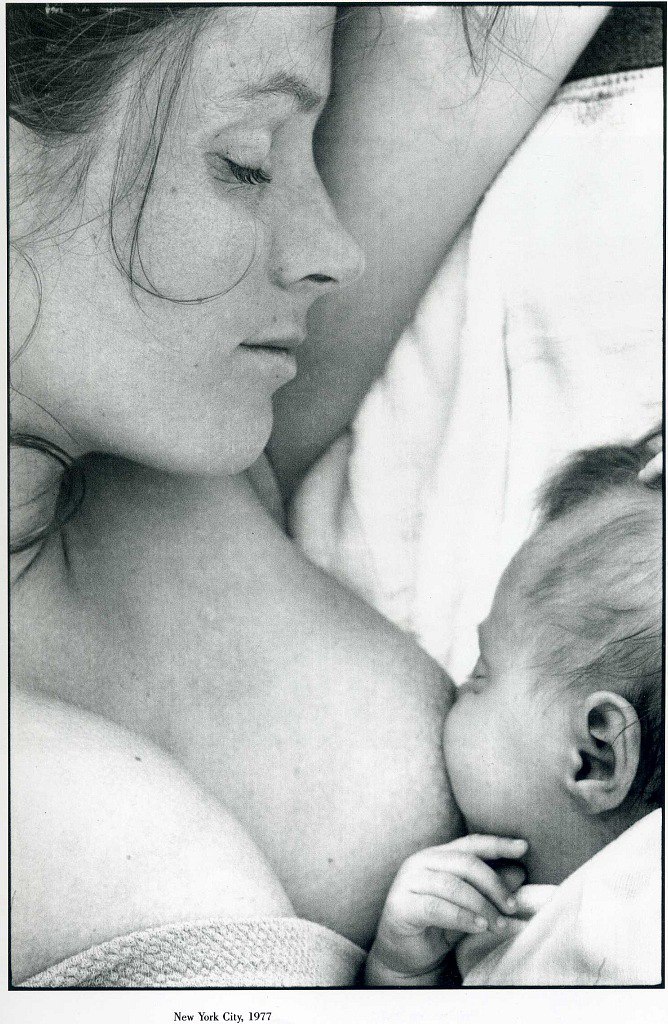 Mothers without experience get scared and take the wrong steps to solve the problem. This leads to complications, breastfeeding becomes impossible.
Mothers without experience get scared and take the wrong steps to solve the problem. This leads to complications, breastfeeding becomes impossible.
Here are some mistakes doctors recommend to avoid:
1. Intensive washing of nipples and breasts with soapy solutions . The alkali that is in the soap irritates the wound, washes away the natural protective lubricant of the skin, disrupts the sebaceous glands, cracked nipples often begin to bleed after that.
2. Use of ointments, lotions with antibacterial ingredients, or oral antibiotics without a prescription . The medicine enters the baby's body and can harm him. With the uncontrolled use of antibacterial drugs, beneficial microflora is destroyed both on the skin and in the intestines of the mother and child. This leads to the activation of pathogenic and conditionally pathogenic flora. Therefore, broad-spectrum antibiotics are prescribed only for a serious bacterial infection.
3. Used as an antiseptic for treating cracked brilliant green or alcohol tinctures with iodine . Alcohol-based solutions provoke a burning sensation, dry the skin. Now there is evidence that brilliant green is unsafe for children and adults, has toxic properties.
4. Use of concentrated alcohol swabs to apply to nipples . With this method of treating cracks, it is difficult to achieve a positive result, it is easy to get a skin burn.
5. Overmoistening of the skin on the chest . This situation occurs with the constant leakage of milk. Therefore, linings must be constantly replaced, otherwise a good environment for the growth of microbes will be created. Ideally, the chest is kept open most of the day or at least at night.
Medication for the treatment of cracked nipples
You can start treating cracked nipples after a medical consultation, this option will be the most successful. Even the most common at first glance means, for example, Bepanten, harm the baby and his mother if used incorrectly.
Topical ointments and creams are considered the main medicines for treating cracked nipples.
Apply drugs to the patient after the end of feeding. Until the next time, the product is absorbed into the skin, for reliability, the nipple can be washed with cold water without soap.
All preparations are divided into several groups, taking into account the active substances that make up their composition. There are also combination products with several active ingredients that have a combined effect.
1. Preparations with dexpanthenol (including Bepanthen)
The substance belongs to vitamins from group B. It is safe, has a wound healing effect and quickly shows its positive effect. Dexpanthenol is an ingredient in many ointments and creams, the most famous and popular drug from this group is Bepanthen ointment.
One of the main advantages of Bepanthen is that there is no need to wash off residues before feeding. The ointment contains only natural ingredients. It consists of wax, a number of vitamins, aromatic oils, distilled water.
It consists of wax, a number of vitamins, aromatic oils, distilled water.
The ointment does not harm the baby's body. In addition, it has a pleasant smell and taste. That is why many doctors recommend treating nipple cracks with Bepanten. It has several analogues with a more affordable price:
- Dexpanthenol
- D-panthenol
- Cream for cracks in the nipples "Elf".
2. Zinc-based products
Such a chemical element as zinc has antiseptic properties, prevents the growth of bacteria and fungi in wounds, and dries the skin.
Apply a thin layer of zinc to the skin of the nipple, rinse off before applying the baby. Here are a number of effective zinc-based preparations:
- Desitin
- Sudocrem
- Zinc ointment
- Zindol.
3. Preparations based on lanolin
The substance lanolin has a structure similar to wax, it is obtained by digestion of sheep's wool. Means, which include lanolin, make the skin soft, provide it with nutrition, create a protective film on top.
Apply a thin layer of ointment with lanolin after the child has eaten. They should not be rubbed into the skin.
Here are lanolin-based preparations that have proven themselves and give excellent results in the treatment of cracked nipples:
- PureLan 100
- Pigeon
- Baby line
- Nipple cream;
- Sanosan
- Lanovit (combination preparation with sea buckthorn oil)
4. Retinol products
Vitamin A or retinol is responsible for the accelerated regeneration of the epidermis and other layers of the skin, mucous membranes, softens the skin. It is recommended to apply retinol-based preparations several times a day so that nipple cracks heal faster. Before feeding the child, the ointment must be washed off with water.
Here are effective preparations with vitamin A recommended by doctors:
5. Ointments and creams with natural oils ), contribute to the regeneration of the epidermis, the healing of cracks in the nipples.
The drugs do not have a direct therapeutic effect, but they can significantly alleviate the symptoms.
Very often such preparations are used when there are contraindications to Bepanthen or other medicines. Here are the most popular products:
- Natura House Cream
- Cream "Mama Comfort";
- Serum "Mama Donna".
6. Products with plant extracts
Ointments and creams based on plant extracts are good at preventing the formation of cracked nipples. Therefore, they are recommended to be used even before childbirth. The components of the preparations strengthen all layers of the skin, after which it becomes more resistant to any damage. They can also speed up the healing of small cracked nipples.
The most popular preparations from this group:
- Cream "9 months"
- Babe Laboratorios
- Vulnuzan
7. Regenerating agents
Regenerating agents are indicated for deep fissures, after treatment of infected wounds.![]() They activate the metabolism in tissues, significantly improve the healing and restoration of the normal structure of the skin. During breastfeeding, they are allowed to be used, but must be washed off before applying the child.
They activate the metabolism in tissues, significantly improve the healing and restoration of the normal structure of the skin. During breastfeeding, they are allowed to be used, but must be washed off before applying the child.
For cracked nipples, it is recommended to use the following drugs from this group:
Non-traditional and folk methods of treatment
Many mothers are afraid to use pharmacy products so as not to harm their child. To get rid of fear, you need to consult a doctor. Although there are folk methods that look quite safe. Some experts have nothing against applying them for small cracked nipples.
- Breast milk . Breast milk contains vitamins, antiseptics, even antibodies and substances that promote regeneration. Our grandmothers also lubricated nipples with this natural remedy for cracked nipples. After applying milk, it is advised to leave the breast open for a while.
- Sea buckthorn oil .
 The natural substance is even included in some pharmaceutical preparations, softens and nourishes the skin, accelerates wound healing, and relieves irritation. Oil should be applied to the nipple after feeding is completed.
The natural substance is even included in some pharmaceutical preparations, softens and nourishes the skin, accelerates wound healing, and relieves irritation. Oil should be applied to the nipple after feeding is completed. - Olive oil . It is recommended to be used for the prevention and treatment of cracked nipples. The oil moisturizes, softens and nourishes the skin.
- Pine Nut Oil . This oil contains vitamin E, a group of B vitamins and other useful substances. It prevents skin damage, softens it, accelerates the healing of nipple cracks.
- Chlorophyllipt . Get the drug from the leaves of eucalyptus. It has antiseptic and anti-inflammatory properties. Therefore, it is recommended to use it for infected cracks and to prevent microbes from entering the wound. Chlorophylipt is applied after feeding the baby, before the next application to the breast, it is washed off with water without soap.
- Cabbage leaves .
 The cabbage leaf is believed to relieve pain, swelling, and inflammation. The technique is very old, proven by many generations. A cabbage leaf should be applied to the chest for several hours, secured with a bra or bandage (but not tight).
The cabbage leaf is believed to relieve pain, swelling, and inflammation. The technique is very old, proven by many generations. A cabbage leaf should be applied to the chest for several hours, secured with a bra or bandage (but not tight). - Aloe juice . The juice from this plant has antiseptic and wound healing properties. You can squeeze the juice onto a gauze pad or apply the pulp from an aloe leaf cut in half to the nipple. Fix it on the nipple with a plaster.
- Zorka preparation . This medicine is sold in veterinary pharmacies and is intended for animals, but it can also be used in humans. The active ingredient of the drug is floralizin, which improves metabolism, metabolism and tissue regeneration, softens the skin and promotes rapid healing of nipple cracks. It is applied after feeding and washed off before the next attachment of the baby to the breast.
It is undesirable to use folk remedies on your own, it is better to consult a doctor first.
Do not treat nipple cracks yourself or rely on the advice of mothers, girlfriends, grandmothers. Even the recommendation of a pharmacist in a pharmacy is not always reliable. Therefore, when the first symptoms appear, you need to contact a specialist.
How to prevent cracked nipples
As you know, prevention always gives better results than subsequent treatment. Cracked nipples are not only a problem for young and inexperienced mothers, even women who have given birth many times face it. Therefore, doctors have developed a number of recommendations that can prevent the problem:
- Do not abruptly take the baby from the breast.
- You can wash your breasts no more than 2 times a day, without the use of cosmetics.
- After a shower, lubricate the nipples well with lanolin cream.
- After feeding, you can apply your own milk to the nipple.
- If milk is secreted from the breast spontaneously outside of feedings, it should be kept open more, when wearing a bra, pads should be changed regularly.

Mandatory preventive measure is normal attachment to the breast:
- The baby needs to be in the correct position during feeding - lie on his side, in a half-turned position, with his stomach pressed against his mother's.
- The baby's head should rest on the mother's elbow so that she can move freely.
- The baby needs to latch onto the nipple by himself.
- The entire nipple, along with most of the areola, should be in the baby's mouth. The nose and chin should be firmly pressed against the mother's breast.
How to prevent cracked nipples and treat them normally? It is necessary to adhere to the correct feeding technique, observe hygiene rules and familiarize yourself with ways to prevent this problem before childbirth.
If cracked nipples develop, see a doctor. Most often, experts prescribe Bepanten ointment, its analogues or other means with a similar effect. Breastfeeding is stopped only in extreme cases, because this is the best way to keep the child healthy and strengthen his bond with his mother.
Many women, especially those giving birth for the first time, are afraid to breastfeed and often face various problems. In this article, you will learn how to avoid trouble and provide your baby with quality breast milk.
How to feed your baby properly
Feeding your baby requires a calm, comfortable environment. For the first two weeks, some women will not be allowed to sit for medical reasons, so they can only breastfeed while lying down. This is very convenient, but you should remember about safety: during feeding (especially at night), the mother can fall asleep, and this cannot be allowed, because she can accidentally harm the baby.
Sitting feeding can be done in a chair, in an armchair or on a sofa. It is important that a woman has support behind her back. For women who breastfeed while sitting, a special nursing pillow has been developed, designed to make the process of feeding easier for mommy, to feel comfortable and relaxed.
Using a pillow, you no longer have to strain your arms and back, keeping the baby on the weight, and some babies do not let go of their mother's breast for hours, then falling asleep, then waking up and starting to suck milk again.
Fissure risk group: why does it hurt me to feed? How to relieve pain?
Women with a flat, inverted nipple are more likely to develop cracks. Over time, it will acquire the correct shape, but until then, mommy will experience pain during each feeding.
Silicone nursing pads can be used to reduce pain. These pads are reusable but must be sterilized before each use.
The cap has a convex tip that the child can easily grasp with his small mouth. Starting to suck, the baby draws the mother's nipple into the cavity of the pad and receives milk.
It should be noted that you should not abuse the pads, otherwise the baby will refuse the breast: after all, it is easier for him to suck through the pad, and in order to get milk directly, you need to work hard.
Cracks in the nipples can cause trouble for a woman for about 2 months and, of course, they need to be dealt with. Special nipple creams have a wound-healing effect, which must be applied after each feeding. it is important to understand that any drugs should be prescribed by a mammologist.
it is important to understand that any drugs should be prescribed by a mammologist.
Will there be enough breast milk for full feeding? How to increase milk production?
Expectant mothers worry about whether they will have milk and whether it will be enough to feed the child as many times as he asks.
Such that milk will not appear at all, in principle, should not be - nature will not allow this. There may be little milk or it may disappear due to illness or nervousness, which is why peace of mind and the absence of stress are so important for a nursing woman.
There are several ways to increase lactation (breast milk production).
- The use of walnuts in small quantities, of course, causes the appearance of milk.
- Tea with milk, green tea and in general any liquid should be consumed by a nursing mother in larger volumes than before childbirth. Modern industry, using scientific developments and folk recipes, produces special teas to increase lactation.
 Approximately 30 min. before feeding, you should drink a mug of such hot tea, since it is the hot liquid that will cause the flow of milk.
Approximately 30 min. before feeding, you should drink a mug of such hot tea, since it is the hot liquid that will cause the flow of milk. - Before feeding, you can take a shower: warm water, if it comes into contact with the chest, will contribute to the milk rush.
- To increase lactation, it is useful to carry out night feedings.
Laktostasis: when there is too much milk
Too little milk is bad, too much milk is also not good. When milk is in excess, and the child does not eat the entire portion prepared by the mother's body, milk can overfill the mammary gland or its individual parts and cause such a serious disorder as lactostasis.
Unfortunately, lactostasis occurs in 90% of nursing mothers at least 1-2 times during the breastfeeding period, especially at the very beginning.
- chest lump;
- painful sensations;
- pain from touch.
The woman may feel general severe malaise. In this case, she is worried about: aching joints, chills, hand tremors - a real "flu" condition, accompanied by a high temperature - 38-390.
Causes of lactostasis: improper grip of the nipple by the child, long intervals between feedings (especially the absence of night feeding), the inability of the child to suck out all the milk (weak, premature, lazy baby).
A few words about how to overcome lactostasis
- It is necessary to apply the child to the affected breast as often as possible until the breast becomes soft.
- Expression of milk from a diseased breast - sometimes it can be difficult: the chest is like a stone, but does not give out a drop. In this case, 30 minutes before pumping, you can drink 1 No-shpa tablet, it will help relax the muscles, and it will be easier for the milk to move through the ducts. It is more convenient to express with a breast pump, but sometimes it is also possible to manually express the breast. During pumping, it is necessary to carefully but confidently massage all sectors of the chest, starting from the armpit. All movements should be directed towards the nipple.

- After pumping “to the last drop”, a cold compress should be applied to the chest - directly from the freezer, you can take a bag of semi-finished products or ice cubes. From exposure to cold, the ducts will narrow, and there will be no strong influx of milk.
- High temperature can be brought down by Paracetamol.
If lactostasis is started, it can lead to mastitis, and this is quite a sad story. As a preventive measure for stagnation of milk in the breast, it can be advised to express after each feeding, do not skip nightly feedings, and use special breast oil during lactation.
Breastfeeding is a process colored by bright, incomparable emotions: happiness, affection, tenderness. If you properly prepare for breastfeeding, it will not cause much trouble. We wish you patience, strength and good health.
Cancer of the nipple of the breast is also called Paget's cancer or Paget's disease.
Cancer of the nipple is never symmetrical (on both sides at once), is not associated with breastfeeding, and (usually) does not hurt.
About breast cancer (not nipple cancer) SEE HERE
Nipple changes
Paget's cancer - cancer of the nipple of the breast - is a malignant tumor of the breast that affects the nipple and the pigmented part of the areola (around the nipple).
The nipple initially becomes red, irritated and flaky. Then there is ulceration with slight bleeding. Without treatment, the process destroys the nipple and spreads to the areola.
Click on the photo to enlarge
Photo of nipple cancer: the nipple became flatter, and the skin on it became soft pink, the papillae smoothed out, crusts periodically appear.
All photos on our website are our patients without photoshop!
| ALL SURGERY for breast cancer |
Hormone therapy for postmenopausal disorders
and hormonal contraceptives - increases the risk of breast cancer.
Cancer of the nipple
Paget's cancer of the breast is a rare form of breast cancer. It is always characterized by a primary skin lesion of the nipple and not the areola.
It is always characterized by a primary skin lesion of the nipple and not the areola.
Click on the photo to enlarge
Photo of Paget's cancer: blood crusts on the nipple, leaving stains on the underwear.
The cause of nipple cancer is not known with certainty. One theory is that it occurs as a result of the spread of tumor cells through the ducts of the mammary gland from the primary tumor located in the breast tissue, inside it. And already from the ducts it spreads to the skin. Another theory suggests that it may itself develop in the nipple.
Nipple cancer photo
Photo of a patient with nipple cancer (Paget).
Click on the photo to enlarge
Scabs on the nipple
In this patient (pictured above), at an early stage, the cancer manifested itself as itching, crusting, and ineffectiveness of treatment by a dermatologist. During the examination (mammography, MRI) a second tumor was found in the thickness of the gland.
It should be noted that with cancer, crusts always appear on only one nipple. If the same crusts appear on both nipples at the same time, this is definitely not cancer.
In this patient, blood crusts appeared on the nipple and soaked in the shower, the nipple itself was somewhat retracted. During the examination, a tumor was found in the thickness of the mammary gland, from which a cord from the ducts infiltrated by the tumor is determined to the nipple. A biopsy from the nipple also showed cancer.
Nipple cancer symptoms
Paget's cancer is almost always initially confused with dermatitis or mechanical abrasion, trauma to the nipple - because it manifests itself with non-specific signs.
Oncology nipple
| Click on the photo to enlarge |
If you zoom in on the photo, you can see the signs of Paget's cancer on the nipple of the left breast. Visible preoperative markings. Below is a photo of her after the operation.
Visible preoperative markings. Below is a photo of her after the operation.
Wet nipple
In the patient, whose photo above, the first manifestation of Paget's cancer was weeping of the nipple, which for a long time dermatologists mistook for eczema.
Signs of nipple cancer
Early detection of nipple cancer provides self-examination:
- Initially there is a scale or scales on the skin of the nipple - often goes unnoticed
- The skin of the nipple (and areola) becomes hard and/or the ichor begins to separate from it through cracks or sores - often confused with eczema
- Unpleasant burning, itching or tingling sensation in the nipple area. No severe pain
- Redness of the skin on the nipple, which is replaced by weeping with light or bloody discharge, leaving scanty stains on the linen
- Nipple flattening or curvature to the side
- Breast seal
- Thickening of the entire breast skin around the areola
Without treatment for Paget's cancer, the nipple is completely destroyed. Instead, one areola remains with crusts instead of the nipple.
Instead, one areola remains with crusts instead of the nipple.
Areola cancer
If Paget's cancer is left untreated, it spreads to the areola. There is no independent disease "Cancer of the areola".
Paget's cancer of the breast
Paget's cancer itself refers to non-invasive skin cancer of the nipple of the breast. It does not metastasize either to the lymph nodes or to other organs, unlike invasive cancers.
A cytological examination of secretions or skin scrapings of the nipple is performed to confirm the diagnosis. Anesthesia is not required for this.
Therefore, it is impossible to die from it - of course, with the right treatment and if Paget's cancer was not combined with another tumor of the mammary gland - more aggressive.
All doctors of our Center trained and studied with the best foreign specialists, and our work is organized according to the most modern quality criteria.
Breast nipple cancer
Breast nipple cancer is a rare independent disease. Most often, it is combined with non-invasive duct cancer or invasive breast cancer located in its thickness. Therefore, if Paget's cancer is suspected or already detected, a full-fledged study is necessary, as in breast cancer: mammography (or MRI) and ultrasound examination of the mammary glands (with regional lymph nodes).
Most often, it is combined with non-invasive duct cancer or invasive breast cancer located in its thickness. Therefore, if Paget's cancer is suspected or already detected, a full-fledged study is necessary, as in breast cancer: mammography (or MRI) and ultrasound examination of the mammary glands (with regional lymph nodes).
Most patients with breast cancer have no known risk factors for cancer.
Detailed examination algorithm for breast cancer SEE HERE
Paget's disease of the nipple
Paget's disease of the nipple
Photo of the patient before and after surgery (before discharge) to remove the tumor of the left breast, excision of the nipple (Paget's cancer) and its reconstruction from the skin cut over the areola during a vertical breast lift. You can see that the recreated nipple is slightly lighter than its areola.
Paget's treatment
Paget's cancer treatment - surgical - removal of the nipple and (if necessary) areola within healthy tissue, with breast ducts. After the operation, the resection margins of the removed nipple are examined - it is not a matter of the surgical resection margin being “clean” or “negative”. If a “positive” or “dirty” edge is detected, a repeated, wider excision is performed. A mastectomy operation with or without one-stage prosthetics is possible.
After the operation, the resection margins of the removed nipple are examined - it is not a matter of the surgical resection margin being “clean” or “negative”. If a “positive” or “dirty” edge is detected, a repeated, wider excision is performed. A mastectomy operation with or without one-stage prosthetics is possible.
After breast-sparing surgery, a course of radiotherapy is prescribed.
Paget's cancer treatment
In cases where Paget's cancer is combined with a breast tumor (most often it happens), the operation to remove the nipple is combined with the removal of the breast tumor and biopsy of the sentinel nodes. At the same time, it is the second tumor that determines the treatment strategy, as it is more aggressive.
Paget's cancer photo
Paget's nipple
Photo before surgery with preoperative markings. Cancer manifests itself as redness at the top of the nipple. and flattening it in this place. It is planned to remove the nipple with its simultaneous reconstruction from the skin of the areola.
Photo of a patient with Paget's cancer before surgery and after nipple removal and reconstruction (operated by Chizh I.A.).
Breast Paget
Signs and symptoms almost always occur in only one breast.
Skin changes on the nipple may come and go. There may be a temporary positive effect of treatment, creating the illusion of recovery. Because of this, most often, several months pass from the appearance of the first symptoms to the correct diagnosis.
Pageta photo
Same patient. Photo of the result of the operation to remove the nipple and its simultaneous restoration from the skin of the areola in case of Paget's cancer. Chizh I.A. operated on. In the future, the areola can be tattooed to achieve a greater resemblance to the opposite mammary gland.
Paget's cancer of the breast
Cancer of the areola of the nipple
Photo after surgery for Paget's cancer - removal of the nipple and its simultaneous reconstruction from the skin of the areola of the nipple. Chizh I.A. operated on.
Chizh I.A. operated on.
Paget's cancer
In case of Paget's cancer and removal of the nipple, its immediate recovery is possible during oncoplastic surgery due to the traditionally removed skin (during breast lift).
Photos before and after surgery for cancer of the nipple of the left breast. The removed nipple was reconstructed from the skin of the breast, it is lighter than the right one. If you make his tattoo to match the areola and nipple of the right gland, it will be completely unnoticeable. Chizh I.A. operated on.
Paget's nipple cancer
Loss of a nipple is a heavy loss for any woman. We are aware of this and we always strive to offer an option to restore it immediately, simultaneously with removal.
Photo of the patient before and 3 weeks after surgery to remove nipple cancer and a second malignant tumor in the left breast. An oncoplastic resection "under a lift" was performed with one-stage nipple restoration. After the completion of the entire treatment, it is planned to tattoo the reconstructed nipple and areola to match the nipple and areola of the right gland. Chizh I.A. operated on.
Chizh I.A. operated on.
Skin cancer of the nipple
It is often necessary to remove the nipple during oncological operations. This happens when the tumor is located centrally, when it grows into the skin of the areola, or when the tumor is located directly in the nipple, for example, in Paget's cancer.
Paget's disease of the mammary gland
In such cases, the nipple can be restored delayed (see HERE for more on this) and at the same time.
Paget's breast
Paget's cancer of the nipple of the left breast - the patient came to us a year ago, but instead of the proposed operation, she decided to self-medicate. I came when the tumor completely destroyed the nipple and moved to the areola. There is an unwritten rule in surgery: "Don't do stupid operations on fools." Therefore, we simply removed her areola with juice without reconstruction. Reconstruction is additional work and additional risks. In obviously problematic patients, it is better to prevent them.