Bleeding after strep b test
Strep B Test: MedlinePlus Medical Test
What is a group B strep test?
Strep B, also known as group B strep (GBS), is a type of bacteria commonly found in the digestive tract, urinary tract, and genital area. It rarely causes symptoms or problems in adults but can be deadly to newborns.
In women, GBS is mostly found in the vagina and rectum. So a pregnant woman who is infected can pass the bacteria to her baby during labor and delivery. GBS can cause pneumonia, meningitis, and other serious illnesses in a baby. GBS infections are the leading cause of death and disability in newborns.
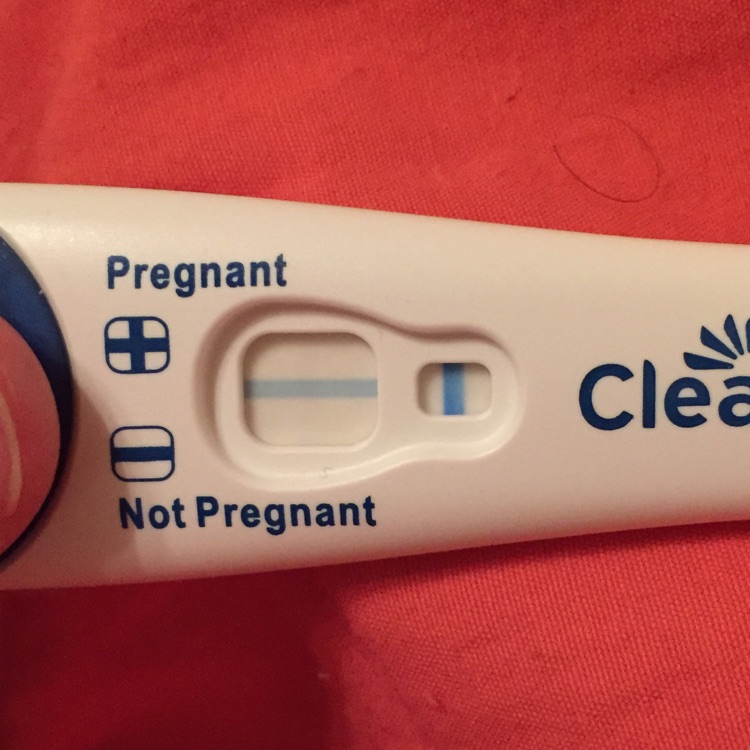
A group B strep test checks for GBS bacteria. If the test shows that a pregnant woman has GBS, she can take antibiotics during labor to protect her baby from infection.
Other names: group B streptococcus, group B beta-hemolytic streptococcus, streptococcus agalactiae, beta-hemolytic strep culture
What is it used for?
A group B strep test is most often used to look for GBS bacteria in pregnant women. Most pregnant women are tested as part of routine prenatal screening. It may also be used to test infants who show signs of infection.
Why do I need a group B strep test?
You may need a strep B test if you are pregnant. The American College of Obstetricians and Gynecologists recommends GBS testing for all pregnant women. Testing is usually done in the 36th or 37th week of pregnancy. If you go into labor earlier than 36 weeks, you may be tested at that time.
A baby may need a group B strep test if he or she has symptoms of infection. These include:
- High fever
- Trouble with feeding
- Trouble breathing
- Lack of energy (hard to wake up)
What happens during a group B strep test?
If you are pregnant, your health care provider may order a swab test or a urine test.
For a swab test, you will lie on your back on an exam table. Your health care provider will use a small cotton swab to take a sample of cells and fluids from your vagina and rectum.
For a urine test, you will most likely be told to use the "clean catch method" to ensure your sample is sterile. It includes the following steps.
- Wash your hands.
- Clean your genital area with a cleansing pad given to you by your provider. To clean, open your labia and wipe from front to back.
- Start to urinate into the toilet.
- Move the collection container under your urine stream.
- Collect at least an ounce or two of urine into the container, which should have markings to indicate the amounts.
- Finish urinating into the toilet.
- Return the sample container as instructed by your health care provider.
If your baby needs testing, a provider may do a blood test or a spinal tap.
For a blood test, a health care professional will use a small needle to take a blood sample from your baby's heel. After the needle is inserted, a small amount of blood will be collected into a test tube or vial. Your baby may feel a little sting when the needle goes in or out.
Your baby may feel a little sting when the needle goes in or out.
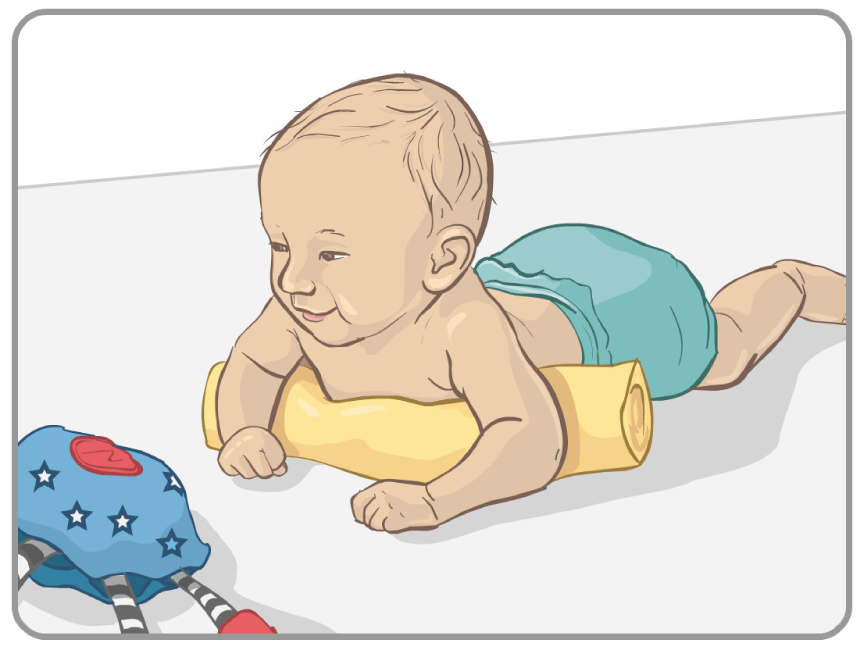
A spinal tap, also known as a lumbar puncture, is a test that collects and looks at spinal fluid, the clear liquid that surrounds the brain and spinal cord. During the procedure:
- A nurse or other health care provider will hold your baby in a curled-up position.
- A health care provider will clean your baby's back and inject an anesthetic into the skin, so your baby won't feel pain during the procedure. The provider may put a numbing cream on your baby's back before this injection.
- The provider may also give your baby a sedative and/or pain reliever to help him or her better tolerate the procedure.
- Once the area on the back is completely numb, your provider will insert a thin, hollow needle between two vertebrae in the lower spine. Vertebrae are the small backbones that make up the spine.
- The provider will withdraw a small amount of cerebrospinal fluid for testing.
 This will take about five minutes.
This will take about five minutes.
Will I need to do anything to prepare for the test?
You don't any special preparations for group B strep tests.
Are there any risks to the test?
There is no risk to you from a swab or urine test. Your baby may have slight pain or bruising after a blood test, but that should go away quickly. Your baby will likely feel some pain after a spinal tap, but that shouldn't last too long. There is also a small risk of infection or bleeding after a spinal tap.
What do the results mean?
If you are pregnant and results show you have GBS bacteria, you will be given antibiotics intravenously (directly to your veins) during labor, at least four hours before delivery. This will prevent you from passing the bacteria to your baby. Taking antibiotics earlier in your pregnancy is not effective, because the bacteria can grow back very quickly. It's also more effective to take antibiotics through your vein, rather than by mouth.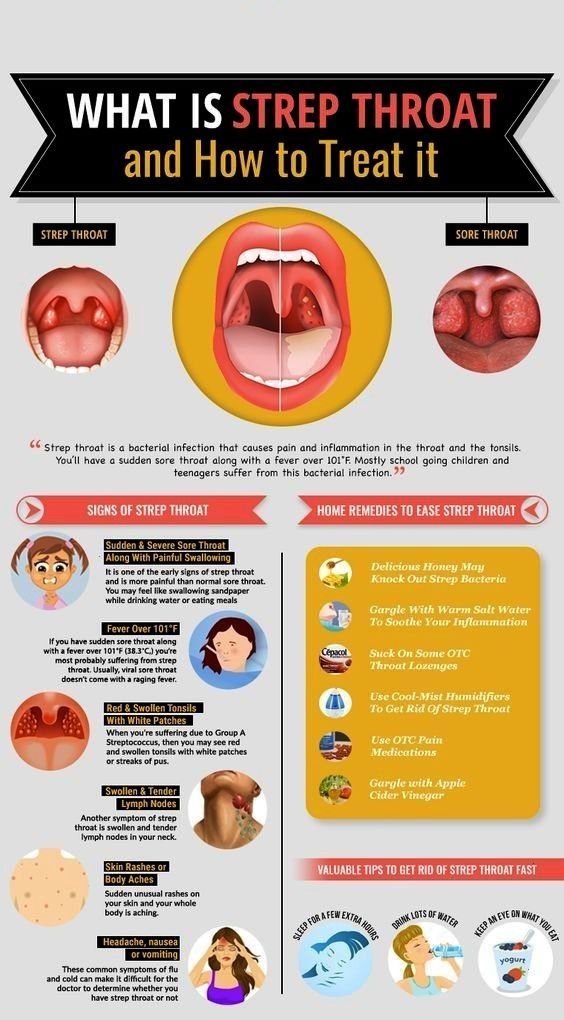
You may not need antibiotics if you are having a planned delivery by Cesarean section (C-section). During a C-section, a baby is delivered through the mother's abdomen rather than vaginally. But you still should be tested during pregnancy because you may go into labor before your scheduled C-section.
If your baby's results show a GBS infection, he or she will be treated with antibiotics. If your provider suspects a GBS infection, he or she may treat your baby before test results are available. This is because GBS can cause serious illness or death.
If you have questions about your results or your baby's results, talk to your health care provider.
Learn more about laboratory tests, reference ranges, and understanding results.
Is there anything else I need to know about a group B strep test?
Strep B is one type of strep bacteria. Other forms of strep cause different types of infections. These include strep A, which causes strep throat, and streptococcus pneumoniae, which causes the most common type of pneumonia. Streptococcus pneumonia bacteria can also cause infections of the ear, sinuses, and bloodstream.
Streptococcus pneumonia bacteria can also cause infections of the ear, sinuses, and bloodstream.
References
- ACOG: The American College of Obstetricians and Gynecologists [Internet]. Washington D.C.: American College of Obstetricians and Gynecologists; c2019. Group B Strep and Pregnancy; 2019 Jul [cited 2019 Nov 15]; [about 3 screens]. Available from: https://www.acog.org/Patients/FAQs/Group-B-Strep-and-Pregnancy
- Centers for Disease Control and Prevention [Internet]. Atlanta: U.S. Department of Health and Human Services; Group B Strep (GBS): Prevention; [cited 2019 Nov 15]; [about 4 screens]. Available from: https://www.cdc.gov/groupbstrep/about/prevention.html
- Centers for Disease Control and Prevention [Internet]. Atlanta: U.S. Department of Health and Human Services; Group B Strep (GBS): Signs and Symptoms; [cited 2019 Nov 15]; [about 4 screens]. Available from: https://www.cdc.gov/groupbstrep/about/symptoms.html
- Centers for Disease Control and Prevention [Internet].
 Atlanta: U.S. Department of Health and Human Services; Streptococcus Laboratory: Streptococcus pneumoniae; [cited 2019 Nov 15]; [about 3 screens]. Available from: https://www.cdc.gov/streplab/pneumococcus/index.html
Atlanta: U.S. Department of Health and Human Services; Streptococcus Laboratory: Streptococcus pneumoniae; [cited 2019 Nov 15]; [about 3 screens]. Available from: https://www.cdc.gov/streplab/pneumococcus/index.html - Centers for Disease Control and Prevention [Internet]. Atlanta: U.S. Department of Health and Human Services; Travelers' Health: Pneumococcal Disease; [updated 2014 Aug 5; cited 2019 Nov 15]; [about 3 screens]. Available from: https://wwwnc.cdc.gov/travel/diseases/pneumococcal-disease-streptococcus-pneumoniae
- Intermountain Healthcare: Primary Children's Hospital [Internet]. Salt Lake City: Intermountain Healthcare; c2019. Lumbar Puncture in a Newborn; [cited 2019 Nov 15]; [about 4 screens]. Available from: https://intermountainhealthcare.org/ext/Dcmnt?ncid=520190573
- Lab Tests Online [Internet]. Washington D.C.: American Association for Clinical Chemistry; c2001–2019. Blood Culture; [updated 2019 Sep 23; cited 2019 Nov 15]; [about 2 screens]. Available from: https://labtestsonline.
 org/tests/blood-culture
org/tests/blood-culture - Lab Tests Online [Internet]. Washington D.C.: American Association for Clinical Chemistry; c2001–2019. Prenatal Group B Strep (GBS) Screening; [updated 2019 May 6; cited 2019 Nov 15]; [about 2 screens]. Available from: https://labtestsonline.org/tests/prenatal-group-b-strep-gbs-screening
- Lab Tests Online [Internet]. Washington D.C.: American Association for Clinical Chemistry; c2001–2019. Urine Culture; [updated 2019 Sep 18; cited 2019 Nov 15]; [about 2 screens]. Available from: https://labtestsonline.org/tests/urine-culture
- Michigan Medicine: University of Michigan [Internet]. Ann Arbor (MI): Regents of the University of Michigan; c1995–2021. Group B Streptococcal Infections in Newborns[cited 2021 Aug 6]; [about 3 screens]. Available from: https://www.uofmhealth.org/health-library/zp3014spec
- University of Rochester Medical Center [Internet]. Rochester (NY): University of Rochester Medical Center; c2019. Health Encyclopedia: Group B Streptococcus Infection in Babies; [cited 2019 Nov 15]; [about 2 screens].
 Available from: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=P02363
Available from: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=P02363 - University of Rochester Medical Center [Internet]. Rochester (NY): University of Rochester Medical Center; c2019. Health Encyclopedia: Pneumonia; [cited 2019 Nov 15]; [about 2 screens]. Available from: https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=85&contentid=P01321
- WHO Guidelines on Drawing Blood: Best Practices in Phlebotomy [Internet]. Geneva (SUI): World Health Organization; c2010. 6. Paediatric and neonatal blood sampling; [cited 2019 Nov 15]; [about 3 screens]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK138647
Group B strep test | Pregnancy Birth and Baby
Group B strep test | Pregnancy Birth and Baby beginning of content4-minute read
Listen
If you’re pregnant, one of the routine antenatal tests you’ll probably have is for group B streptococcus (also known as ‘group B strep’ or ‘GBS’). This page explains what the test is for, which babies are at risk of infection and how group B strep is treated.
This page explains what the test is for, which babies are at risk of infection and how group B strep is treated.
What is group B strep?
Group B strep is a type of bacteria commonly found in the intestines, rectum, urethra or vagina. Many women have it, and it usually causes no health concerns or symptoms. Some women infected with group B strep get a urinary tract infection, and it increases the risk of a miscarriage only very slightly.
The main concern is passing it on to the baby before or during a vaginal birth. While many babies who get infected stay healthy, a small proportion (about 1 in 200) become very sick within the first few days of life. They get serious infections such as pneumonia and blood poisoning, or meningitis, which is an infection around the brain.
These seriously ill babies are treated with intravenous antibiotics. Most recover with no side-effects, but some don't survive.
Group B strep test
The group B strep test is a routine antenatal test. It involves taking a swab of the inside of the vagina. Your doctor or midwife will do this, or you may be able to do it yourself. The swab is taken at 35 to 37 weeks' pregnancy. Tests done earlier in your pregnancy aren't a good guide to your condition at birth because the bacteria can come and go.
It involves taking a swab of the inside of the vagina. Your doctor or midwife will do this, or you may be able to do it yourself. The swab is taken at 35 to 37 weeks' pregnancy. Tests done earlier in your pregnancy aren't a good guide to your condition at birth because the bacteria can come and go.
Who has the group B strep test?
Some hospital and doctors recommend that every pregnant woman has a group B strep test.
But others ask only some women to have the test if they are at higher-than-average risk because they go into labour early, or their waters break early.
Even if you're planning a caesarean, you can think about having the test in case your waters break early or you go into labour unexpectedly early.
Talk about the risks and benefits of the group B strep test with your midwife or doctor.
Risk factors for infection with group B strep
Babies are more likely to be infected with group B strep if:
- they are born, or your waters break, before 37 weeks
- you give birth more than 18 hours after your waters break
- you have a fever (over 38°C) while in labour
- you've had a previous child with severe group B strep infection
- a urine test during pregnancy detected group B strep
- a swab taken no more than 5 weeks earlier detected group B strep
Preventing group B strep from infecting your baby
If your group B test at 35 to 37 weeks was positive, or if you have the risk factors listed above, your doctor or midwife will probably recommend that you have intravenous antibiotics when your waters break or labour starts.
Often this is penicillin, but alternatives are available if you are allergic to penicillin. The antibiotics pass through the placenta and into the baby. This greatly reduces your baby's chances of becoming ill.
There's no need for antibiotics before a planned caesarean because the baby will not pass through the vagina. You can't pass the bacteria to your baby through the placenta.
After the birth
If you had antibiotics during labour, your baby will be monitored for the first couple of days for signs of infection. The chance of your baby being infected is low.
Late-onset group B strep
There is a very small group of babies that develop group B strep infection weeks or months after birth (called ‘late onset group B strep'). They become seriously ill quite quickly, with fevers and vomiting and difficulty feeding. Unfortunately, the group B strep test and use of antibiotics doesn’t prevent a baby developing late-onset group B strep infection.
If your child's condition deteriorates quickly, call triple zero (000) and ask for an ambulance, or go to the nearest hospital emergency department.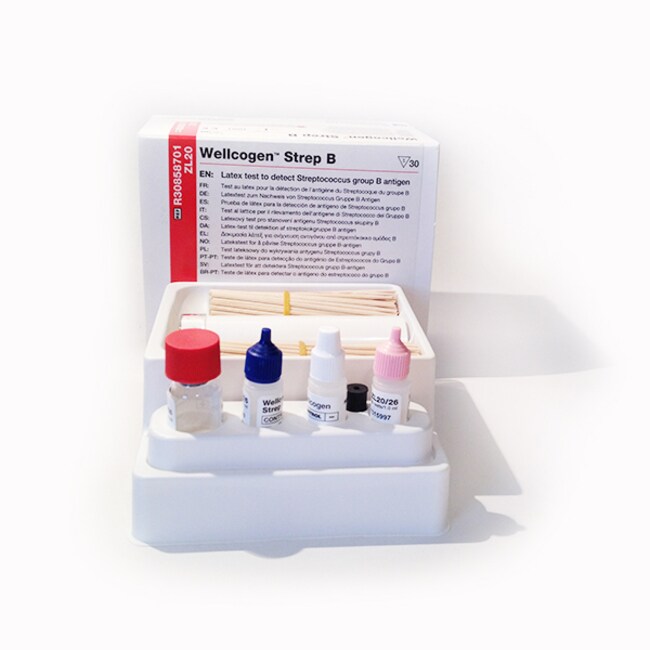
When to seek help
If you want more information about group B strep, or if you have any concerns about your baby, call Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse, or talk to your midwife or doctor.
Sources:
RANZCOG (Group B Streptococcus), RANZCOG (Maternal Group B Streptococcus in pregnancy), Cochrane Database of Systematic Reviews (Vaginal chlorhexidine during labour to prevent early-onset neonatal group B streptococcal infection), Cochrane Database of Systematic Reviews (Intrapartum antibiotics for known maternal Group B streptococcal colonization), Department of Health (Pregnancy Care Guidelines, Group B streptococcus)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2020
Back To Top
Related pages
- Pregnancy checkups, screenings and scans
Need more information?
Group B Streptococcus
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Pregnancy screening Group B Streptococcus (GBS) - Maternal, child and family health
The Pregnancy screening for Group B Streptococcus (GBS) consumer brochure provides information to all pregnant women on screening and recommended treatment for GBS.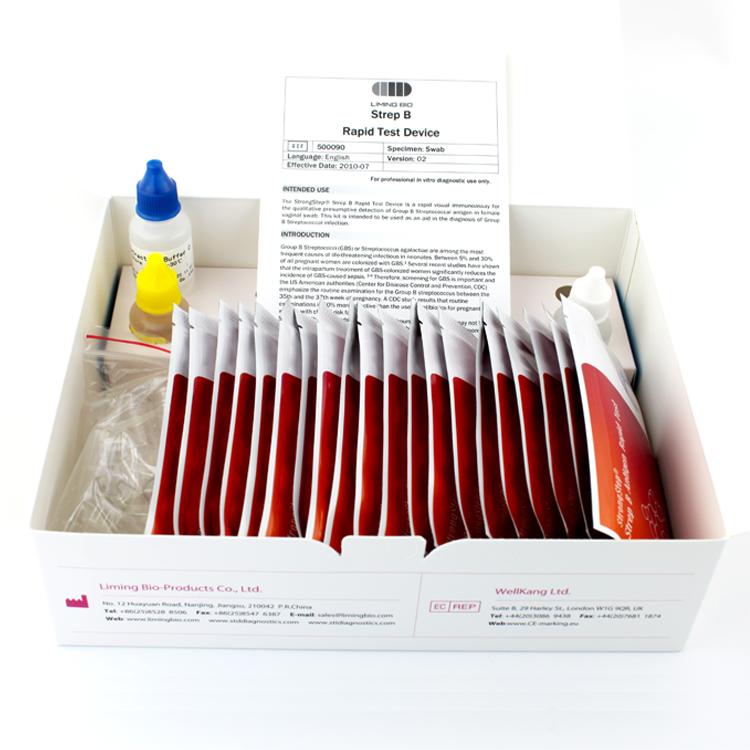
Read more on NSW Health website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.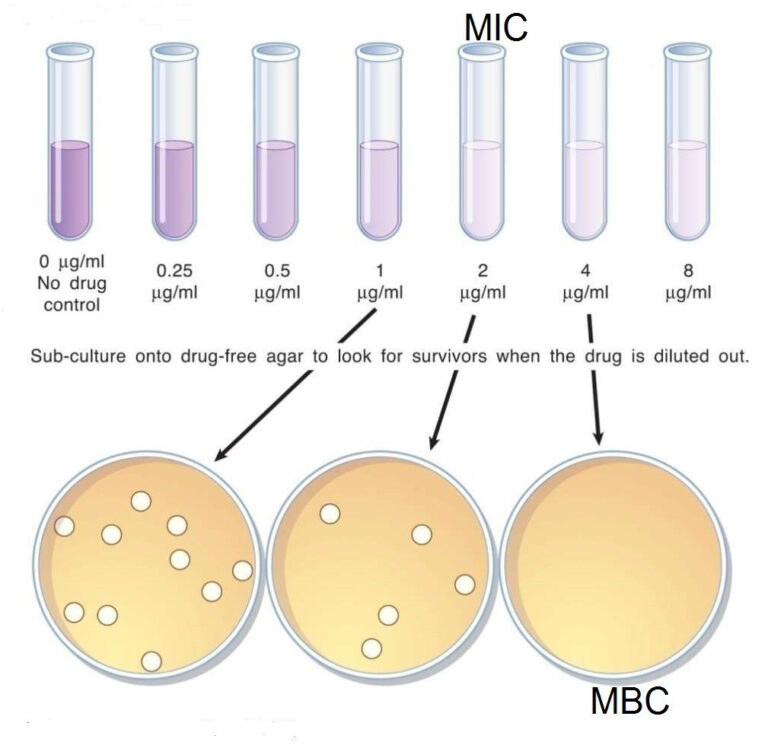
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.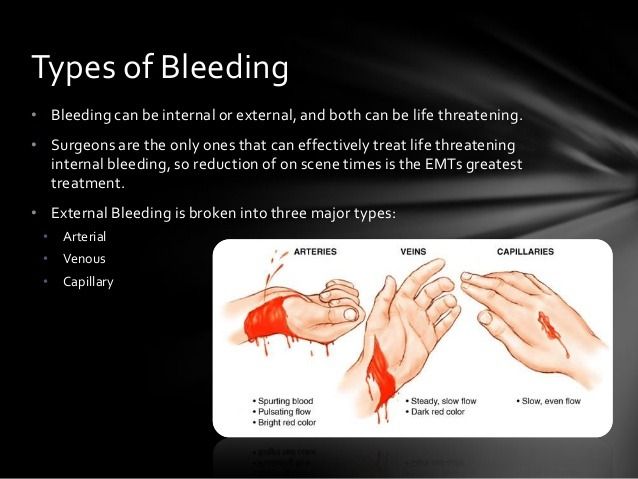
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Blood test for streptococcus in the laboratory
Serogroup B streptococci (GBS) have long been known to cause mastitis in cattle and small cattle and have been named Streptococcus agalactiae . Previously, until 1937 inclusive, this microorganism was considered as a commensal of the human body. Since the 60s, this species, as a human pathogen, has occasionally begun to be isolated in a variety of nosological forms of infection: endocarditis, pyelonephritis, meningitis, pneumonia, abscess, peritonitis, generic sepsis, neonatal sepsis, pharyngitis, etc. Within 1970s–1980s GBS is becoming one of the most common causative agents of purulent-septic infections in newborns and mothers in the United States and Western Europe. In the early 90s, the first publications about the role of this type of streptococcus in the pathology of pregnancy and pyoinflammatory diseases of newborns also appeared in our country. To date, official registration of diseases caused by this microorganism in the Russian Federation has not been carried out.
Within 1970s–1980s GBS is becoming one of the most common causative agents of purulent-septic infections in newborns and mothers in the United States and Western Europe. In the early 90s, the first publications about the role of this type of streptococcus in the pathology of pregnancy and pyoinflammatory diseases of newborns also appeared in our country. To date, official registration of diseases caused by this microorganism in the Russian Federation has not been carried out.
Streptococci of this species, according to the modern nomenclature according to the Bergay determinant, are included in the genus Streptococcus family Sreptococcaeae species S.agalactiae . The modern classification of streptococci is based on the division into serological groups according to the Lensfield classification. S.agalactiae are assigned to serogroup B and are its only representatives. GBS is a heterogeneous population consisting of a number of serotypes and their combinations. Currently, 9 serotypes have been identified, designated by Roman numerals: I, II, III, IV, V, VI, VII, VIII. Type I is divided into subtypes Ia and Ib.
Currently, 9 serotypes have been identified, designated by Roman numerals: I, II, III, IV, V, VI, VII, VIII. Type I is divided into subtypes Ia and Ib.
The habitat of the pathogen is the human body, large and small cattle, the possibility of its transmission from animals to humans and vice versa has not been proven. The localization of GBS in humans is the gastrointestinal tract (colon), vagina, urethra, sometimes the microorganism can colonize the pharynx. Pathogenicity factors: the ability to adhere and invade, resistance to phagocytosis, hemolysin, hyaluronidase, peptidase (impairs the chemotaxis of polymorphonuclear leukocytes to the site of GBS infection).
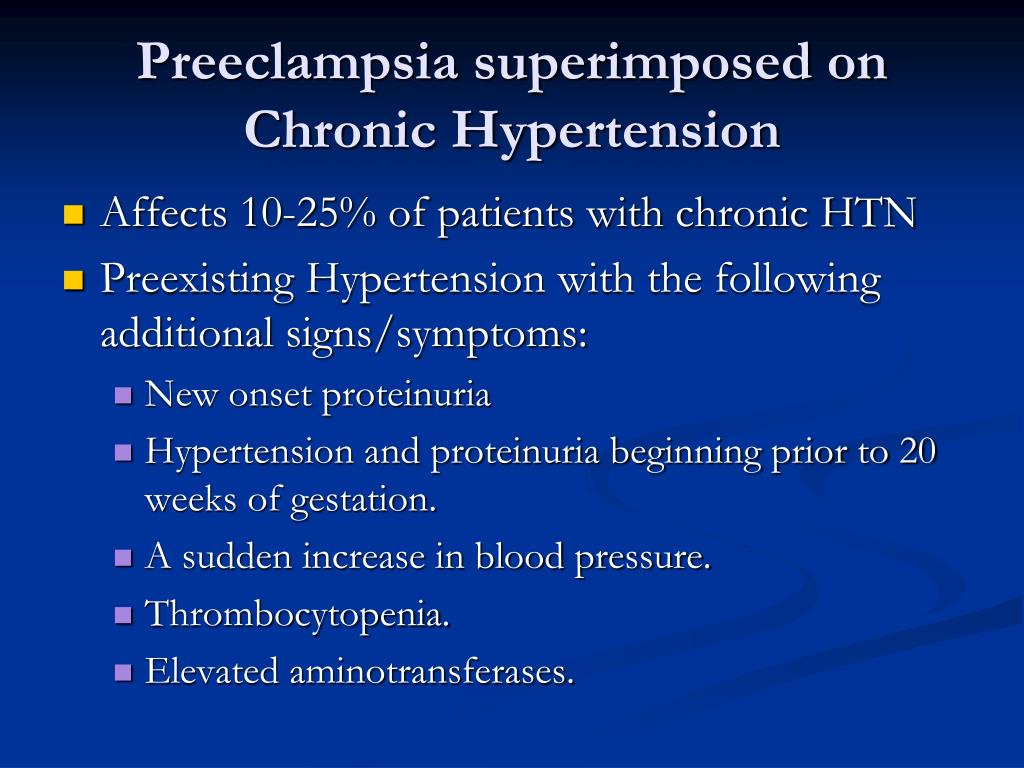
GBS can cause severe infections in people. The most sensitive to them are newborns, pregnant women, diabetics, chronic patients, children with dystrophy, the elderly, people with reduced immunity. Spontaneous abortions, preterm labor, chorioamnionitis, pyelonephritis, urinary tract infections, endocarditis, sepsis, as well as complications after caesarean section, meningitis, mastitis and endometritis in puerperas can be associated with GBS. In neonates, GBS mainly causes sepsis, meningitis, and pneumonia. Transmission of the pathogen to the newborn can occur intranatally and postnatally. According to foreign sources, in recent years there has been a relative increase in the number of diseases caused by GBS in the elderly against the background of a slight decrease in the incidence among newborns. The observed phenomenon is associated, on the one hand, with the active prevention of this infection in maternity hospitals, and, on the other hand, with an increase in the number of elderly patients with reduced immunity. In the latter, GBS usually causes infection of the skin and bones, sepsis without a clear source of its origin, urosepsis, pneumonia, and peritonitis. Often these infections occur repeatedly in such patients.
In neonates, GBS mainly causes sepsis, meningitis, and pneumonia. Transmission of the pathogen to the newborn can occur intranatally and postnatally. According to foreign sources, in recent years there has been a relative increase in the number of diseases caused by GBS in the elderly against the background of a slight decrease in the incidence among newborns. The observed phenomenon is associated, on the one hand, with the active prevention of this infection in maternity hospitals, and, on the other hand, with an increase in the number of elderly patients with reduced immunity. In the latter, GBS usually causes infection of the skin and bones, sepsis without a clear source of its origin, urosepsis, pneumonia, and peritonitis. Often these infections occur repeatedly in such patients.
An important role in the development of GBS infections in newborns is played by factors predisposing to the disease, the so-called “risk factors”, which can be conditionally divided into two groups:
- associated with the peculiarities of childbirth or colonization of mothers with GBS;
- directly related to newborns.
The first group includes the presence of GBS on the mucous membrane of the cervix in pregnant women, the massiveness of colonization (isolation of the pathogen simultaneously from several examined loci), cases of GBS infections in children in anamnesis in parturient women, premature birth, a long anhydrous period, fever during childbirth, chorioamnionitis , bacteriuria due to GBS.
The second group includes the fact and massive colonization of newborns with GBS, prematurity and low birth weight, birth by caesarean section, intrauterine instrumental examination of the fetus, lasting more than 12 hours.
Penicillin is still the most effective and widely used drug for the treatment of infections caused by streptococci. Along with serogroup A streptococci, GBS retain their sensitivity to this antibiotic, although GBS strains in a small number of cases are resistant to penicillin G. In addition to penicillin, streptococci have been found to be highly sensitive to ampicillin, erythromycin, clindamycin, lincomycin, oxacillin and meroponem. The first three generations of cephalosprins, with the exception of cefoxitin and moxalactam, have a wider spectrum of activity than penicillin. The high sensitivity of GBS to a number of relatively new drugs with a wide spectrum of activity was also noted: thienamycin, mezlocillin, azlocillin and piperacillin. GBS strains have been found to be frequently resistant to aminoglycoses, nalidixic acid, tetracycline, chloramphenicol, bacitracin, trimethoprim, and metromnidazole. Nevertheless, the combined use of aminoglycosides with penicillin or ampicillin in experimental studies on laboratory animals revealed a synergistic effect of such combinations. In recent years, foreign literature reports on the isolation of GBS strains resistant to beta-lactam antibiotics. The nature of this phenomenon is associated with the appearance in the cells of microorganisms of the genes responsible for the synthesis of penicillin-binding proteins (PBPs). According to a number of foreign researchers, the number of GBS strains resistant to erythromycin can range from 5.
The first three generations of cephalosprins, with the exception of cefoxitin and moxalactam, have a wider spectrum of activity than penicillin. The high sensitivity of GBS to a number of relatively new drugs with a wide spectrum of activity was also noted: thienamycin, mezlocillin, azlocillin and piperacillin. GBS strains have been found to be frequently resistant to aminoglycoses, nalidixic acid, tetracycline, chloramphenicol, bacitracin, trimethoprim, and metromnidazole. Nevertheless, the combined use of aminoglycosides with penicillin or ampicillin in experimental studies on laboratory animals revealed a synergistic effect of such combinations. In recent years, foreign literature reports on the isolation of GBS strains resistant to beta-lactam antibiotics. The nature of this phenomenon is associated with the appearance in the cells of microorganisms of the genes responsible for the synthesis of penicillin-binding proteins (PBPs). According to a number of foreign researchers, the number of GBS strains resistant to erythromycin can range from 5. 9up to 32.0% and the number of strains resistant to clindamycin from 6.9 to 14.3%. The use of therapeutic bacteriophages for the prevention and treatment of GBS infection is currently impossible due to the lack of active specific bacteriophages.
9up to 32.0% and the number of strains resistant to clindamycin from 6.9 to 14.3%. The use of therapeutic bacteriophages for the prevention and treatment of GBS infection is currently impossible due to the lack of active specific bacteriophages.
Indications for examination. Birth of a child with a history of GBS infection in a woman in labor, GBS bacteriuria during this pregnancy, threatened preterm labor, fever during labor (≥ 38°C), waterless period lasting more than 18 hours.
Material for research. Blood, CSF, sputum, fetal fluid, joint fluid, tissue fragments, oropharyngeal swabs, vaginal swabs/scrapes, rectal swabs.
Etiological diagnosis includes isolation of the pathogen and identification of its DNA.
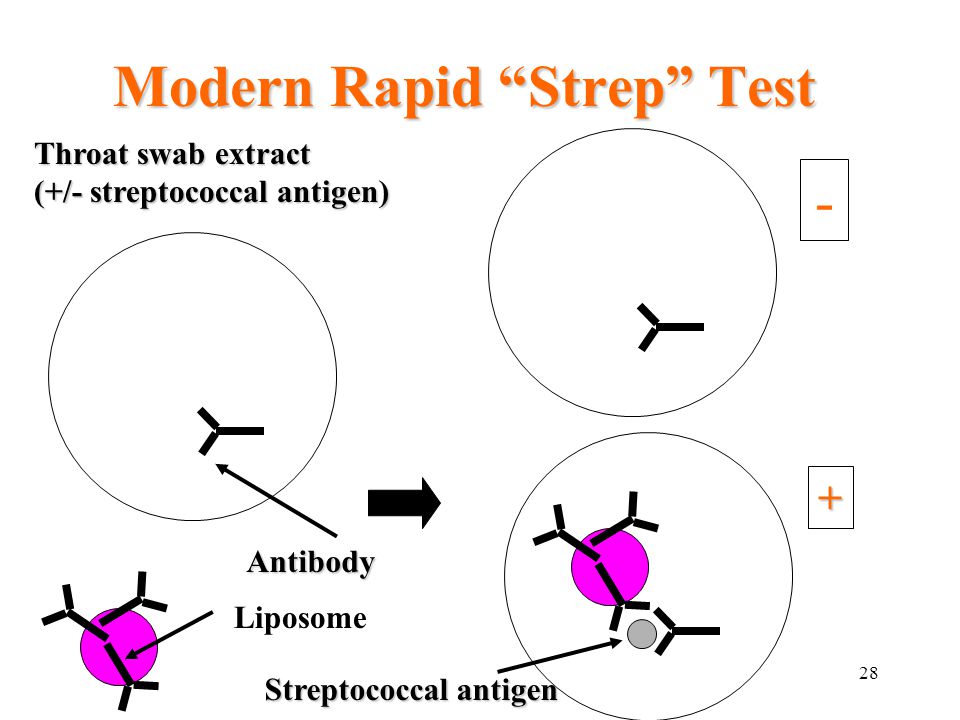
Comparative characteristics of laboratory diagnostic methods. Isolation of the pathogen in the diagnosis of GBS infections is the "gold standard" and is an important step in a series of diagnostic measures.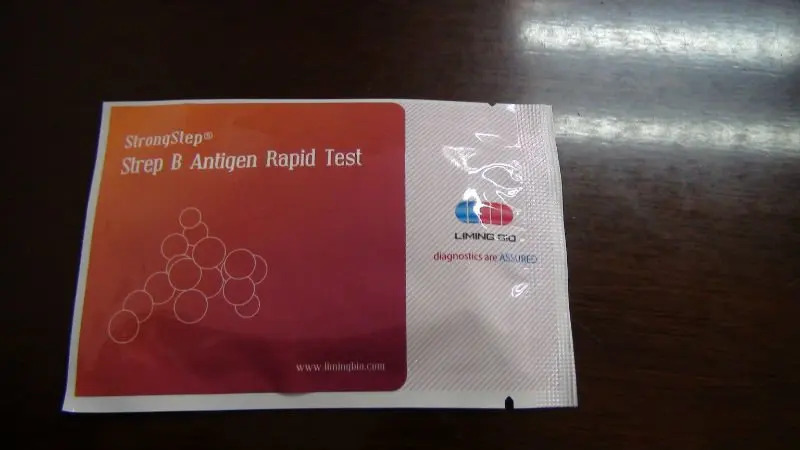 A standard culture is used using, for example, 5% blood agar. Timely isolation of the pathogen with the determination of sensitivity to antibiotics largely determines the effectiveness of the treatment and prevention of this disease.
A standard culture is used using, for example, 5% blood agar. Timely isolation of the pathogen with the determination of sensitivity to antibiotics largely determines the effectiveness of the treatment and prevention of this disease.
If an infection is suspected, a variety of biological material is examined. In the case of determining the carriage of GBS in pregnant women, smears from the mucous membrane of the vagina and rectum are examined for 35–37 weeks. pregnancy. If it is not possible to inoculate immediately, transport media may be used. The time needed to isolate and identify GBS is usually 4 to 5 days.
Identification of a specific DNA fragment S.agalactiae by PCR is carried out in the study of various biological material. Scrapings of epithelial cells from the side walls of the vagina, perianal smears at 34–36 weeks of gestation are examined to detect colonization of the vagina and/or rectum by S.agalactiae; blood, CSF of a newborn - for the diagnosis of septic conditions; swabs from the oropharynx - in newborns with clinical symptoms of pneumonia to confirm the diagnosis.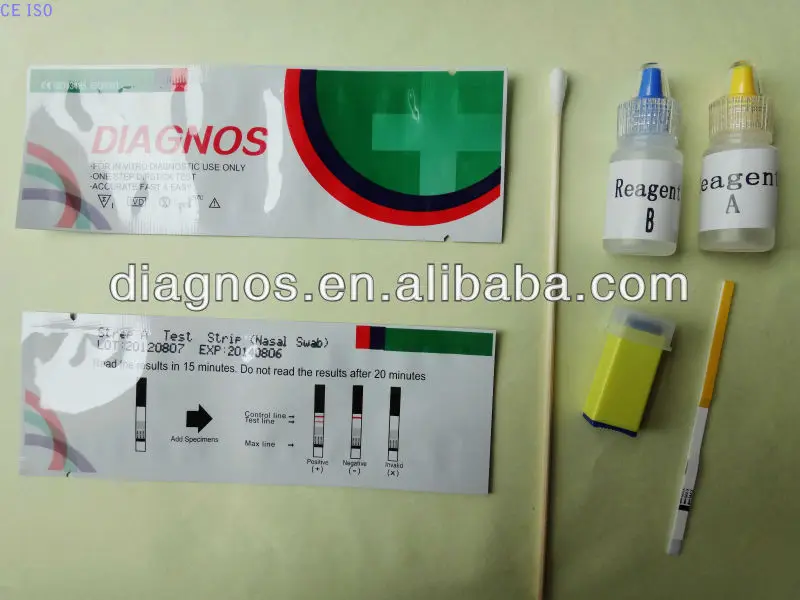 The advantage of this study is that it allows testing within a few hours and thereby accelerates clinical decision-making on the prevention and treatment of the disease. The diagnostic sensitivity of the study is 81%, the diagnostic specificity is 97.6%. Detection of S.agalactiae DNA by PCR can be performed in a qualitative and quantitative format. The quantitative format of the test allows the study to be used to assess the degree of GBS colonization of a selected locus. However, the detection of a specific DNA fragment S.agalactiae by PCR does not allow the detection of viable microorganisms and, accordingly, their sensitivity to antibiotics.
The advantage of this study is that it allows testing within a few hours and thereby accelerates clinical decision-making on the prevention and treatment of the disease. The diagnostic sensitivity of the study is 81%, the diagnostic specificity is 97.6%. Detection of S.agalactiae DNA by PCR can be performed in a qualitative and quantitative format. The quantitative format of the test allows the study to be used to assess the degree of GBS colonization of a selected locus. However, the detection of a specific DNA fragment S.agalactiae by PCR does not allow the detection of viable microorganisms and, accordingly, their sensitivity to antibiotics.
Article "Streptococcus B - danger during pregnancy"
Clinic of Gynecology and Oncogynecology
Moscow, st. Shchepkina, 35
Moscow, Spiridonievsky per., 5/1
Moscow, st. Pravdy, 15 building 1
Write to WhatsApp
Streptococcus B (Strept. Agalactiae) is a bacteria that is very often found in the vagina and/or lower intestines of women. They do not pose any danger to a non-pregnant woman, because. these bacteria may be part of the normal flora. In addition, even if this disease is treated, it may appear again after a few days.
Agalactiae) is a bacteria that is very often found in the vagina and/or lower intestines of women. They do not pose any danger to a non-pregnant woman, because. these bacteria may be part of the normal flora. In addition, even if this disease is treated, it may appear again after a few days.
It is also quite common during pregnancy - about 10% of pregnant women are thought to carry Streptococcus B.
The problem is that these bacteria can cause serious illness in newborns. It does not help the situation and the fact that the risk of disease in newborns is very small. Although streptococcus B is transmitted from every second mother to a child at birth, only 1% of infected babies will develop a neonatal infection.
Thus, we are talking about a banal and often occurring microbe, which, some time after the treatment of its carrier, will return again, which makes the treatment useless and dangerous. This microbe is very often transmitted to newborns, without bringing the latter any harm, not counting 1% of babies.
Taking into account these features of the disease, the scientific community recommends the following recommendations:
Systematic diagnosis of Streptococcus B is recommended at the end of pregnancy, between 34 and 38 weeks amenorrhea;
Treatment of asymptomatic disease in women in early and mid-pregnancy is not justified. This means that you should not treat Streptococcus B during pregnancy, except for the presence of infectious signs or a dangerous condition of the patient (rupture of the amniotic membranes).
But in case of a positive test result during childbirth, it is necessary to carry out antibiotic prophylaxis. It is carried out with antibiotics of the penicillin series (penicillin or amoxicillin).
Rate
Average: 3.95 (20 ratings)
Clinic of Gynecology and Oncogynecology
Moscow, st. Shchepkina, 35
Moscow, Spiridonievsky per. , 5/1
, 5/1
Moscow, st. Pravdy, 15 building 1
Write to WhatsApp
Doctors and staff
IMPORTANT QUESTIONS ABOUT PREGNANCY | About vitamins, nutrition, shoes, etc...
October 20
All videos
Clinic of Gynecology and Oncogynecology
Dear Vladimir Borisovich! Thank you from the bottom of my heart. You are truly a doctor from God with a capital letter. Thanks to your professionalism, kindness, tact, charm and talent, I believed in the success of the upcoming operation immediately at the first meeting at your appointment, you explained everything so intelligibly and convincingly that there was complete confidence in success. The operation you have done is fantastic! The very next day it was possible to sit, get up and groom, and on the third day I was discharged home.