Symptoms of dead fetus in first trimester
Early Pregnancy Loss - familydoctor.org
What is early pregnancy loss?
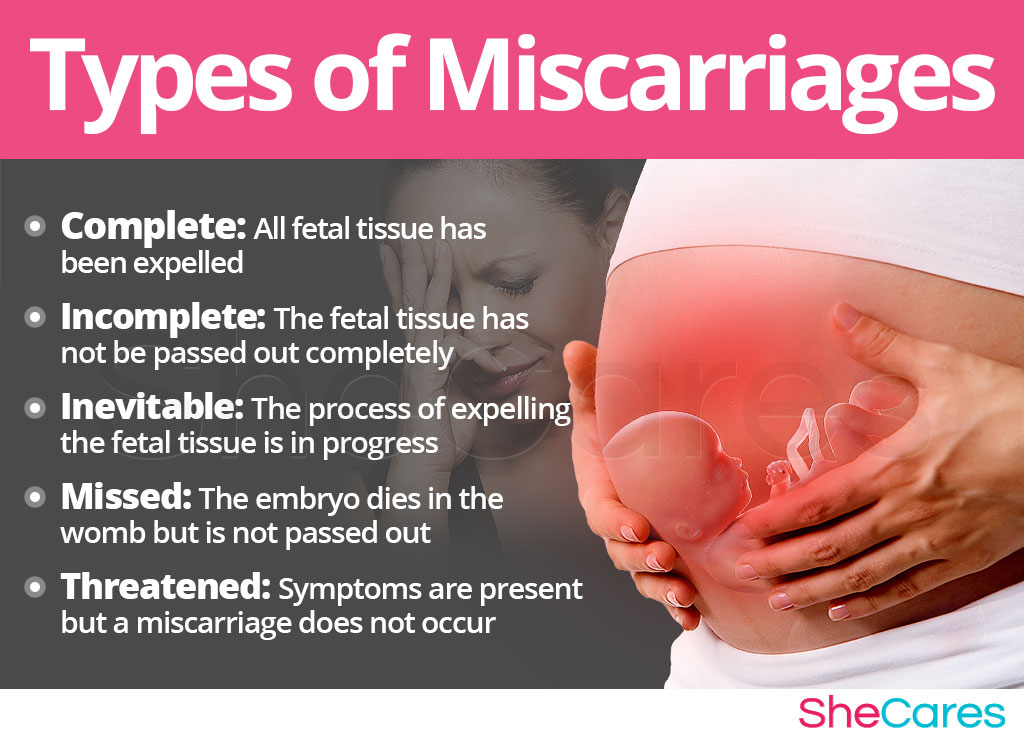
An early pregnancy loss is known as a miscarriage. This represents any pregnancy that ends on its own in the first 20 weeks of gestation. Experts estimate that 10% to 20% of known pregnancies end in miscarriage. There are several classifications of miscarriage:
- Complete – when the embryo and surrounding tissues have emptied out of the uterus. It typically involves cramping and bleeding. These resolve quickly, usually in a few days to a week.
- Incomplete or inevitable – when the cervix opens, and some tissue is expelled (released). The embryo or tissue may not completely leave the uterus. This can cause continued pain and bleeding.
- Missed – when the embryo has died, but it stays in the uterus. You may have no idea that it has happened. It is often discovered when pregnancy symptoms stop, or an ultrasound shows no heartbeat.
- Threatened – when you experience some bleeding and cramping, but the cervix remains closed. A miscarriage may or may not happen.
- Recurrent –when you have 3 or more miscarriages in your first trimester.
Other problems can also result in an early pregnancy loss:
- Chemical pregnancy – This is a very early miscarriage. It usually happens in the first few weeks after conception. Chromosomal abnormalities keep the embryo from developing normally. The tissue is passed from your uterus around the same time that you normally have your period. Many women don’t even know they are pregnant when they have a miscarriage from a chemical pregnancy.
- Blighted ovum –This is also called an embryonic pregnancy. It happens when the fertilized egg implants in the wall of the uterus, but a fetus never develops.
- Ectopic pregnancy –This is when the fertilized egg implants somewhere other than the uterus.
 Often, it implants in the fallopian tube. This can cause serious problems for the mother. Treatment — usually surgery — is needed right away to remove the tissue. This is never a viable pregnancy.
Often, it implants in the fallopian tube. This can cause serious problems for the mother. Treatment — usually surgery — is needed right away to remove the tissue. This is never a viable pregnancy. - Molar pregnancy –This is a rare problem that starts with a genetic error during fertilization. This causes abnormal tissue to grow instead of an embryo. It is not a viable pregnancy. But it still causes regular pregnancy symptoms. These include a missed period, positive pregnancy test, and nausea.
Symptoms of early pregnancy loss
The most common symptoms of miscarriage are bleeding and cramping. But they don’t necessarily mean you’re having a miscarriage. Up to one-third of pregnancies come with some bleeding early on. About half of those result in normal pregnancies. If you have any bleeding or cramping in your first trimester, call your doctor.
There are other common signs that indicate you may be having a miscarriage. If you experience any of these symptoms, call your doctor right away:
- Mild to severe back pain (worse than menstrual cramps)
- Weight loss
- White-pink mucus discharge from the vagina
- Contractions (painful, happening every 5 to 20 minutes)
- Tissue that looks like a clot passing from the vagina
- Sudden decrease in signs of pregnancy
What causes early pregnancy loss?
In some cases, the cause of your pregnancy loss is unknown. Often, it is a random problem with chromosomes that happens at conception. You might be afraid that you did something that caused your miscarriage. But things like working, exercising, having sex, or morning sickness do not cause miscarriage. Any kind of fall or blow is rarely to blame. The research on the effects of alcohol, tobacco, and caffeine is unclear. So, there is nothing you could have done to prevent it. It is not the result of anything you did or didn’t do. You should never blame yourself for a miscarriage.
Often, it is a random problem with chromosomes that happens at conception. You might be afraid that you did something that caused your miscarriage. But things like working, exercising, having sex, or morning sickness do not cause miscarriage. Any kind of fall or blow is rarely to blame. The research on the effects of alcohol, tobacco, and caffeine is unclear. So, there is nothing you could have done to prevent it. It is not the result of anything you did or didn’t do. You should never blame yourself for a miscarriage.
How is early pregnancy loss diagnosed?
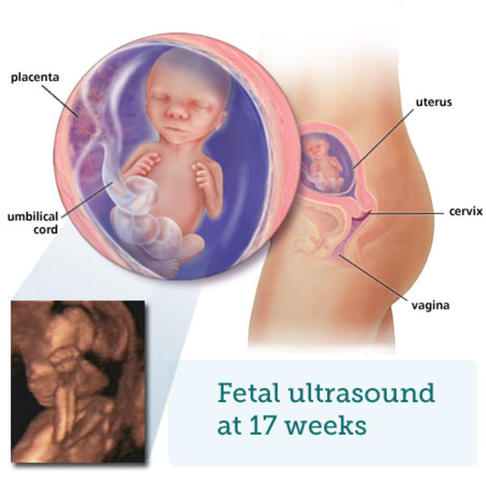
Your doctor will start by asking you questions about your symptoms and when they started. They will do a physical exam. Your doctor might do an ultrasound. This can reveal if the embryo is still growing, and it can check for a heartbeat. They may also order blood tests. These can measure pregnancy hormone levels. This can give your doctor an idea if you are losing the pregnancy.
Can early pregnancy loss be prevented or avoided?
There is no conclusive research that says there is anything you can do to prevent a miscarriage. You didn’t cause it, so you couldn’t have prevented it.
You didn’t cause it, so you couldn’t have prevented it.
Risk factors
Patients who are pregnant and who have had a miscarriage are at greater risk of having another one. Your risk also increases as you get older. You are at highest risk when you are age 35 or older. Some medical conditions also increase your risk. These include:
- Diabetes.
- Thyroid disease.
- Polycystic ovary syndrome.
- Problems with the immune system.
Even if you have one of these conditions, you can’t do anything to avoid having a miscarriage. Many patients who are pregnant and have these health conditions have healthy pregnancies.
Early pregnancy loss treatment
There are two main types of treatment for miscarriage: non-surgical and surgical.
Non-surgical
In many cases, your body passes all of the pregnancy tissue naturally. This could take a few days up to a few weeks. No treatment is needed. If it is taking a long time, your doctor can give you medicine that can help pass the tissue.
The process of passing the tissue can involve heavy bleeding, cramping pain, diarrhea, and nausea. Your doctor may give you pain medicine to help ease your symptoms. If you are in your first trimester, the tissue will be small. It will look like a blood clot. It will not look like a baby.
Your doctor may do an ultrasound or blood tests after you are finished with the miscarriage. This will confirm that the miscarriage is complete, and no tissue remains.
Surgical
Surgical treatment is usually done if there are complications with your miscarriage.
Complications could include:
- An infection
- Heavy bleeding
- Any condition that keeps pregnancy tissue inside your uterus
Common surgical treatments include:
- Vacuum aspiration.In this procedure, a thin tube is inserted into your uterus. It is connected to a suction device. The pregnancy tissue is suctioned out of your body. The procedure is done under local anesthesia.
 Your doctor can perform it in his or her office.
Your doctor can perform it in his or her office. - Dilation and curettage (D&C).This procedure opens the cervix and uses an instrument to remove the pregnancy tissue. It is usually done under regional or general anesthesia. Your doctor will perform it in a hospital or surgery center.
After treatment, your doctor may recommend you not put anything into your vagina for a few weeks. This includes using tampons and having sex. This helps prevent infection. Signs of infection include:
- Heavy bleeding
- Fever
- Chills
- Severe pain
Call your doctor right away if you have any of these symptoms.
Living with early pregnancy loss
Everyone handles loss differently. Some patients who are pregnant may have trouble coping with the feelings that can go along with miscarriage. If you are very upset or feel like you need help, there are resources available. Talk to your doctor. They may be able to refer you to a local support group.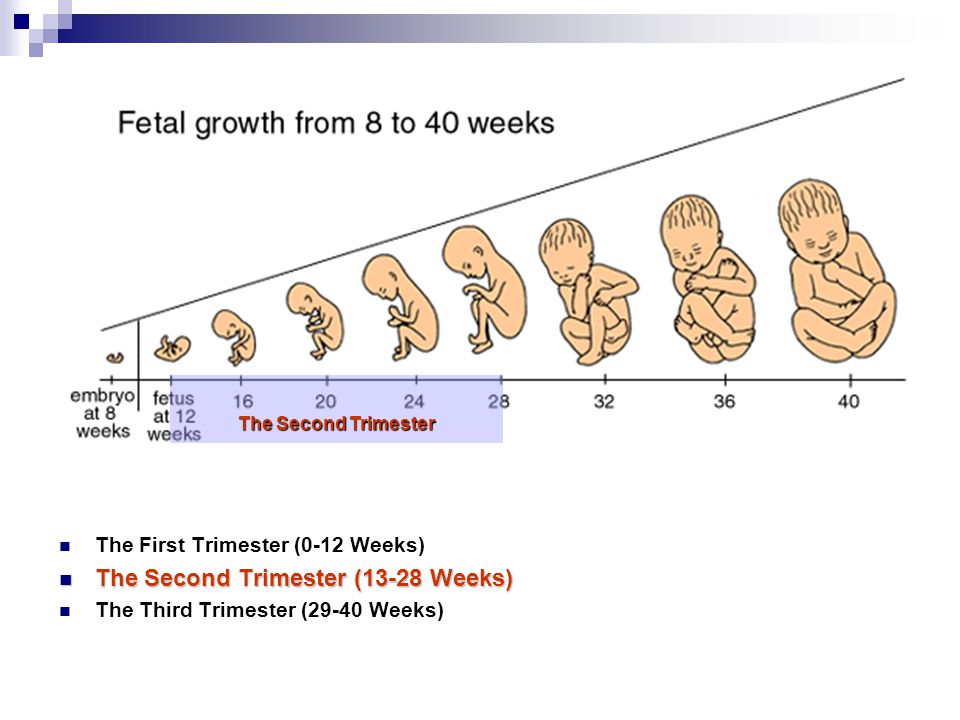 There are also national resources you can access, such as SHARE: Pregnancy and Infant Loss Support. It lists local support groups and offers online resources that could help you.
There are also national resources you can access, such as SHARE: Pregnancy and Infant Loss Support. It lists local support groups and offers online resources that could help you.
Questions to ask your doctor
- I’m having symptoms of miscarriage. What are the chances that I will miscarry?
- How will I know what caused my early pregnancy loss?
- Is there an advantage to letting the tissue pass naturally over having a D&C?
- Will a miscarriage affect my ability to get pregnant again?
- How long should I wait after an early pregnancy loss to try to get pregnant again?
Resources
National Institutes of Health, MedlinePlus: Miscarriage
National Institute of Child Health and Human Development: Pregnancy Loss
SHARE: Pregnancy and Infant Loss Support
Signs and Symptoms of Early Pregnancy Loss
1. Wang X, Chen C, Wang L, Chen D, Guang W, French J. Conception, early pregnancy loss, and time to clinical pregnancy: a population-based prospective study. Fertil Steril. 2003;79(3):577–584. [PubMed] [Google Scholar]
Fertil Steril. 2003;79(3):577–584. [PubMed] [Google Scholar]
2. Wilcox AJ, Weinberg CR, O’Connor JF, et al. Incidence of early loss of pregnancy. N Engl J Med. 1988;319(4):189–194. [PubMed] [Google Scholar]
3. Cumming GP, Klein S, Bolsover D, et al. The emotional burden of miscarriage for women and their partners: trajectories of anxiety and depression over 13 months. BJOG. 2007;114(9):1138–1145. [PubMed] [Google Scholar]
4. Frost J, Bradley H, Levitas R, Smith L, Garcia J. The loss of possibility: scientisation of death and the special case of early miscarriage. Sociol Health Illn. 2007;29(7):1003–1022. [PubMed] [Google Scholar]
5. Lok IH, Neugebauer R. Psychological morbidity following miscarriage. Best Pract Res Clin Obstet Gynaecol. 2007;21(2):229–247. [PubMed] [Google Scholar]
6. Peel E. Pregnancy loss in lesbian and bisexual women: an online survey of experiences. Hum Reprod. 2010;25(3):721–727. [PMC free article] [PubMed] [Google Scholar]
7. Swanson KM, Connor S, Jolley SN, Pettinato M, Wang TJ. Contexts and evolution of women’s responses to miscarriage during the first year after loss. Res Nurs Health. 2007;30(1):2–16. [PubMed] [Google Scholar]
Swanson KM, Connor S, Jolley SN, Pettinato M, Wang TJ. Contexts and evolution of women’s responses to miscarriage during the first year after loss. Res Nurs Health. 2007;30(1):2–16. [PubMed] [Google Scholar]
8. Simmons RK, Singh G, Maconochie N, Doyle P, Green J. Experience of miscarriage in the UK: qualitative findings from the National Women’s Health Study. Soc Sci Med. 2006;63(7):1934–1946. [PubMed] [Google Scholar]
9. Ananth CV, Savitz DA. Vaginal bleeding and adverse reproductive outcomes: a meta-analysis. Paediatr Perinat Epidemiol. 1994;8(1):62–78. [PubMed] [Google Scholar]
10. Saraswat L, Bhattacharya S, Maheshwari A. Maternal and perinatal outcome in women with threatened miscarriage in the first trimester: a systematic review. BJOG. 2010;117(3):245–257. [PubMed] [Google Scholar]
11. Koren G, Madjunkova S, Maltepe C. The protective effects of nausea and vomiting of pregnancy against adverse fetal outcome—a systematic review. Reprod Toxicol. 2014;47:77–80. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
12. Weigel RM, Weigel M. Nausea and vomiting of early pregnancy and pregnancy outcome. A meta-analytical review. BJOG. 1989;96(11):1312–1318. [PubMed] [Google Scholar]
13. Centers for Disease Control and Prevention. Facts About Stillbirth. Atlanta, GA: Centers for Disease Control and Prevention; 2015. http://www.cdc.gov/ncbddd/stillbirth/facts.html. Accessed April 29, 2016. [Google Scholar]
14. Makrydimas G, Sebire N, Lolis D, Vlassis N, Nicolaides K. Fetal loss following ultrasound diagnosis of a live fetus at 6–10 weeks of gestation. Ultrasound Obstet Gynecol. 2003;22(4):368–372. [PubMed] [Google Scholar]
15. Everett C. Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice. BMJ. 1997;315(7099):32–34. [PMC free article] [PubMed] [Google Scholar]
16. Peckham CH. Uterine bleeding during pregnancy. I. When not followed by immediate termination of pregnancy. Obstet Gynecol. 1970;35(6):937–941. [PubMed] [Google Scholar]
1970;35(6):937–941. [PubMed] [Google Scholar]
17. Weiss JL, Malone FD, Vidaver J, et al.; FASTER Consortium. Threatened abortion: a risk factor for poor pregnancy outcome, a population-based screening study. Am J Obstet Gynecol. 2004;190(3):745–750. [PubMed] [Google Scholar]
18. Harville EW, Wilcox AJ, Baird DD, Weinberg CR. Vaginal bleeding in very early pregnancy. Hum Reprod. 2003;18(9):1944–1947. [PubMed] [Google Scholar]
19. Hasan R, Baird DD, Herring AH, Olshan AF, Jonsson Funk ML, Hartmann KE. Association between first-trimester vaginal bleeding and miscarriage. Obstet Gynecol. 2009;114(4):860–867. [PMC free article] [PubMed] [Google Scholar]
20. Brandes JM. First-trimester nausea and vomiting as related to outcome of pregnancy. Obstet Gynecol. 1967;30(3):427–431. [PubMed] [Google Scholar]
21. Klebanoff MA, Koslowe PA, Kaslow R, Rhoads GG. Epidemiology of vomiting in early pregnancy. Obstet Gynecol. 1985;66(5):612–616. [PubMed] [Google Scholar]
22. Kullander S, Kallen B. A prospective study of drugs and pregnancy. II. Anti-emetic drugs. Acta Obstet Gynecol Scand. 1976;55(2):105–111. [PubMed] [Google Scholar]
Kullander S, Kallen B. A prospective study of drugs and pregnancy. II. Anti-emetic drugs. Acta Obstet Gynecol Scand. 1976;55(2):105–111. [PubMed] [Google Scholar]
23. Medalie JH. Relationship between nausea and/or vomiting in early pregnancy and abortion. Lancet. 1957;273(6986):117–119. [PubMed] [Google Scholar]
24. Speert H, Guttmacher AF. Frequency and significance of bleeding in early pregnancy. J Am Med Assoc. 1954;155(8):712–715. [PubMed] [Google Scholar]
25. Tierson FD, Olsen CL, Hook EB. Nausea and vomiting of pregnancy and association with pregnancy outcome. Am J Obstet Gynecol. 1986;155(5):1017–1022. [PubMed] [Google Scholar]
26. Weigel MM, Reyes M, Caiza ME, et al. Is the nausea and vomiting of early pregnancy really feto-protective? J Perinat Med. 2006;34(2):115–122. [PubMed] [Google Scholar]
27. Weigel MM, Weigel RM. Nausea and vomiting of early pregnancy and pregnancy outcome. An epidemiological study. Br J Obstet Gynaecol. 1989;96(11):1304–1311. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
28. Weng X, Odouli R, Li DK. Maternal caffeine consumption during pregnancy and the risk of miscarriage: a prospective cohort study. Am J Obstet Gynecol. 2008;198(3):279 e271-278. [PubMed] [Google Scholar]
29. Wen W, Shu XO, Jacobs DR, Jr, Brown JE. The associations of maternal caffeine consumption and nausea with spontaneous abortion. Epidemiology. 2001;12(1):38–42. [PubMed] [Google Scholar]
30. Chan RL, Olshan AF, Savitz DA, et al. Severity and duration of nausea and vomiting symptoms in pregnancy and spontaneous abortion. Hum Reprod. 2010;25(11):2907–2912. [PMC free article] [PubMed] [Google Scholar]
31. Kouk LJ, Neo GH, Malhotra R, et al. A prospective study of risk factors for first trimester miscarriage in Asian women with threatened miscarriage. Singapore Med J. 2013;54(8):425–431. [PubMed] [Google Scholar]
32. Pollack AZ, Buck Louis GM, Sundaram R, Lum KJ. Caffeine consumption and miscarriage: a prospective cohort study. Fertil Steril. 2010;93(1):304–306. [PMC free article] [PubMed] [Google Scholar]
Fertil Steril. 2010;93(1):304–306. [PMC free article] [PubMed] [Google Scholar]
33. Cunningham F, Leveno K, Bloom S, Hauth J, Rouse D, Spong C. Williams Obstetrics. 23rd ed New York City, NY: McGraw-Hill Education; 2009. [Google Scholar]
34. Johns J, Jauniaux E, Burton G. Factors affecting the early embryonic environment. Rev Gynaecol Perinat Pract. 2006;6(3-4):199–210. [Google Scholar]
35. Dickey R, Olar T, Curole D, Taylor S, Matulich E. Relationship of first-trimester subchorionic bleeding detected by color Doppler ultrasound to subchorionic fluid, clinical bleeding, and pregnancy outcome. Obstet Gynecol. 1992;80(3 pt 1):415–420. [PubMed] [Google Scholar]
36. Hook EB. Dietary cravings and aversions during pregnancy. Am J Clin Nutr. 1978;31(8):1355–1362. [PubMed] [Google Scholar]
37. Profet M. Pregnancy sickness as adaptation: a deterrent to maternal ingestion of teratogens In: Barkow JH, Cosmides L, Tooby J, eds. The Adapted Mind. Oxford, UK: Oxford University Press; 1995: 327–366. [Google Scholar]
38. Sherman PW, Flaxman SM. Nausea and vomiting of pregnancy in an evolutionary perspective. Am J Obstet Gynecol. 2002;186(5):s190–s197. [PubMed] [Google Scholar]
39. Huxley RR. Nausea and vomiting in early pregnancy: its role in placental development. Obstet Gynecol. 2000;95(5):779–782. [PubMed] [Google Scholar]
40. Coad J, Al-Rasasi B, Morgan J. Nutrient insult in early pregnancy. Proc Nutr Soc. 2002;61(01):51–59. [PubMed] [Google Scholar]
41. Forbes S. Pregnancy sickness and embryo quality. Trends Ecol Evol. 2002;17(3):115–120. [Google Scholar]
42. Stein Z, Susser M. Miscarriage, caffeine, and the epiphenomena of pregnancy: the causal model. Epidemiology. 1991;2(3):163–167. [PubMed] [Google Scholar]
43. Furneaux EC, Langley-Evans AJ, Langley-Evans SC. Nausea and vomiting of pregnancy: endocrine basis and contribution to pregnancy outcome. Obstet Gynecol Surv. 2001;56(12):775–782. [PubMed] [Google Scholar]
44. Goodwin TM. Nausea and vomiting of pregnancy: an obstetric syndrome. Am J Obstet Gynecol. 2002;86(suppl 5):s184–s189. [PubMed] [Google Scholar]
45. Goodwin TM, Montoro M, Mestman JH, Pekary AE, Hershman JM. The role of chorionic gonadotropin in transient hyperthyroidism of hyperemesis gravidarum. J Clin Endocrinol Metabol. 1992;75(5):1333–1337. [PubMed] [Google Scholar]
46. Cardwell MS. Pregnancy sickness: a biopsychological perspective. Obstet Gynecol Surv. 2012;67(10):645–652. [PubMed] [Google Scholar]
47. Norwitz ER, Schust DJ, Fisher SJ. Implantation and the survival of early pregnancy. New Engl J Med. 2001;345(19):1400–1408. [PubMed] [Google Scholar]
Miscarriage: causes, symptoms, diagnosis, prevention
Article content
- Symptoms and signs of miscarriage
- Causes of development
- Risk factors
- Complications
- When to see a doctor
- Preparing for a visit to a gynecologist
- Diagnosis of missed pregnancy
- Treatment
- Home remedies
- Prophylaxis
- How to make an appointment with an obstetrician-gynecologist?
A frozen pregnancy at an early stage is the death of the fetus in the womb. It stops its development and dies for up to 28 weeks. Symptoms may be mild, which increases the risk of maternal toxicity. If during pregnancy the fetus froze and stopped its development, an urgent visit to an obstetrician-gynecologist is necessary.
Symptoms and signs of missed pregnancy
A frozen pregnancy at an early stage proceeds absolutely imperceptibly, it can last for 1-2 weeks. This is the danger of the situation.
After 10-12 days, a woman has the first symptoms of a missed pregnancy:
- discharge with blood;
- severe pain in lower abdomen;
- after 18 weeks, you can track the cessation of fetal movement.
There are no symptoms of a missed pregnancy in the first trimester. Sometimes there are spotting spotting, there is a pulling feeling below the navel.
The second frozen pregnancy indicates the presence of a pathology that requires careful study.
Causes of development
Unfortunately, the first missed pregnancy is more common. This is due to the lack of preparation of one's own body. This can happen to any woman.
Main reasons:
- genetic and chromosomal abnormalities cause the development of anomalies that are incompatible with the life of the fetus;
- the fetus was infected with sexually transmitted infections and viruses - even before pregnancy, the risk of the presence or development of such diseases must be excluded;
- hormonal failure increases the risk of miscarriage, progesterone levels should be monitored during gestation;
- a clotting problem causes blood clots to form, preventing them from delivering enough oxygen to the baby;
- Rh conflict causes the production of antibodies that provoke oxygen starvation of the fetus.
Risk factors
Accurately answer the question "Why does pregnancy freeze?" pretty hard.
Consider the most common factors:
- viral diseases can affect the development of the fetus;
- the main reason is hormonal imbalance;
- non-compliance with doctor's recommendations;
- severe stress;
- overheating or severe freezing is prohibited during childbearing;
- smoking and alcohol;
- very tight clothing may harm pregnancy;
- should abandon self-medication and taking drugs not prescribed by a doctor, the body's chemical processes are closely interconnected with each other, the effect can be unpredictable.
Complications
Signs of a missed pregnancy cause the following complications:
- depression. Requires medical treatment, visits to a psychiatrist;
- mummification of the fetus occurs with prolonged missed pregnancy, mummification occurs due to calcium salts, requires surgical intervention;
- infection of the mother's body. Toxins, which are formed due to the decomposition of the fetus, quickly enter the woman's blood. There is sepsis, intoxication, the correct blood clotting is disturbed;
- Lithopedion is a fossilized fetus that has undergone calcification in the body. A woman may not feel any painful symptoms.
When to see a doctor
The gynecologist should observe his patients throughout the entire period of pregnancy. If there is a risk of a missed pregnancy, the terms of which do not exceed 12 weeks, you should immediately consult a doctor. He will determine the condition of the fetus and prescribe further examinations and treatment.
He will determine the condition of the fetus and prescribe further examinations and treatment.
Preparing for a Gynecological Visit
- Shower before visiting a doctor.
- It is better to visit a doctor with an empty bladder, so as not to interfere with palpation.
- Do not take drugs that can affect the microflora or the general condition of the body, this will prevent the doctor from taking an accurate anamnesis.
Symptoms of a missed pregnancy may not appear at all. To avoid intoxication of the body, you should regularly visit a gynecologist.
Diagnosis of missed pregnancy
Diagnosis is carried out in 2 ways: a blood test and ultrasound. If fetal cardiac arrest is detected on ultrasound, the patient is referred to a gynecologist for further procedures.
The patient can make an appointment and get a consultation at a convenient time for him. The pregnancy management program fully complies with clinical guidelines and the latest standards.
JSC "Medicine" (clinic of Academician Roitberg) is located in the Central Administrative District of Moscow, not far from Mayakovskaya, Belorusskaya, Novoslobodskaya, Tverskaya, Chekhovskaya metro stations. Address: 2nd Tverskoy-Yamskoy lane, building 10.
Treatment
Treatment occurs in 3 ways:
- curettage;
- aspiration;
- artificial childbirth.
Curettage - curettage of the uterine cavity. Cleaning after a frozen pregnancy is carried out for a period of 5 weeks.
Aspiration - pumping out the remains of the fetal egg. Carried out in the early stages up to 5 weeks.
Curettage and aspiration are performed under anesthesia. The procedure takes about 30 minutes. After the operation, a course of antibiotics is prescribed. The patient then visits the doctor every week. If complications do not appear, and the causes of a missed pregnancy are eliminated, a woman can continue life in her usual rhythm.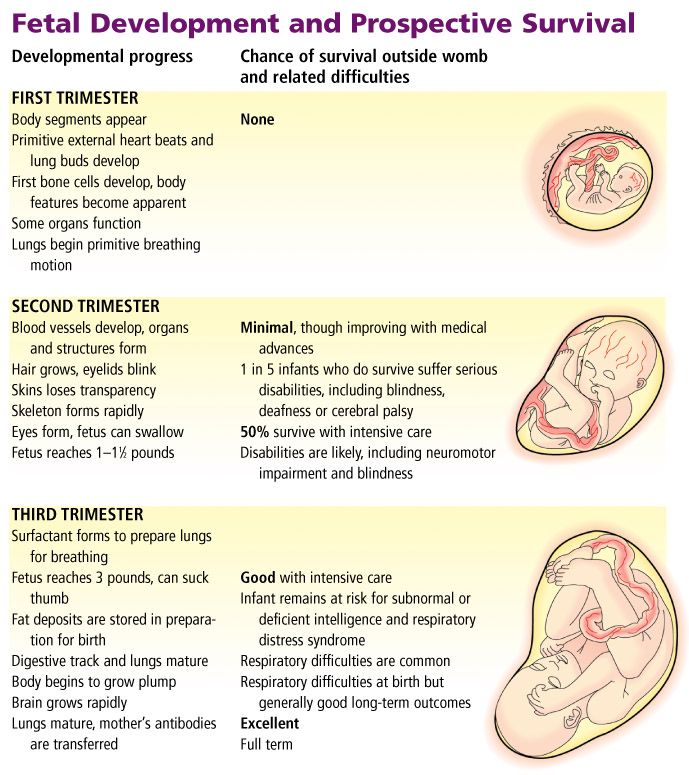
After the loss of an embryo, many women are depressed, they begin to blame themselves for doing something wrong. This is an absolute mistake that can lead to depression. To alleviate your condition, you should contact a psychologist, as well as a gynecologist and other specialists who will help prepare the body for pregnancy.
After treatment, a woman can plan a pregnancy after a missed pregnancy in six months.
Home remedies
Treatment of a missed pregnancy, the terms of which exceeded 12 weeks, involves surgery. At home, the restoration of the body is impossible. Successful recovery requires a large number of tests and a long recovery, associated with the use of antibiotics. At home, it is possible to raise the overall tone of the body.
Important! During gestation, any drugs should be taken as prescribed by a doctor. Many decoctions and herbs have a negative effect on the fetus and can even provoke early labor or miscarriage.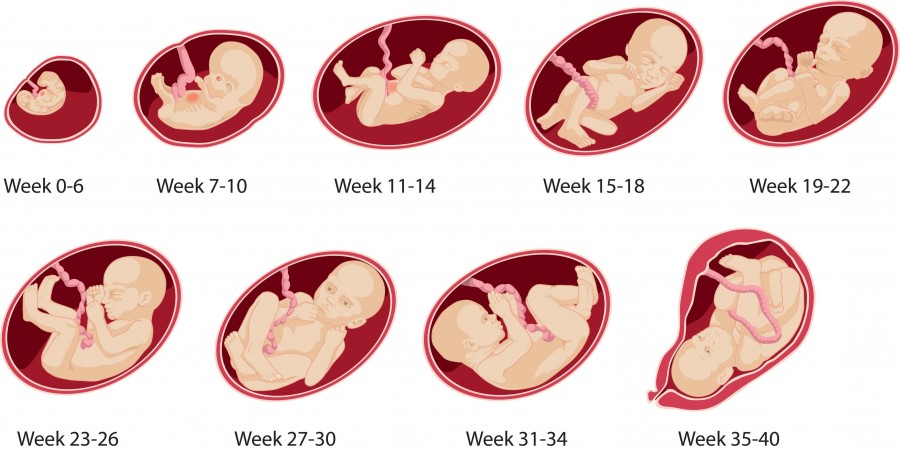
To raise your progesterone levels, you need to:
- include fermented milk products, cheeses, cottage cheese, milk, cream in the diet;
- eat fatty fish;
- do not forget about nuts, berries, fruits and vegetables;
- drink a decoction of plantain seeds, hogweed, raspberry leaves.
It is better to use decoctions in the second half of the cycle. Drink a drink in a volume of 200 ml, no more than 2 times a day.
Important! Decoctions that increase progesterone should not be drunk simultaneously with hormonal drugs.
To prepare for pregnancy, you need:
- replace coffee with tea with chamomile, mint, rosehip and oregano;
- replace sugar and sweeteners with natural honey;
- drink more pure water;
- be treated for sexual infections and maintain health with a decoction of the red brush, hog uterus, coltsfoot.
Prevention
Prevention is a thorough preparation for a new bearing of the fetus. To do this, it is necessary to study the problem of a previous stop in the development of the embryo.
To do this, it is necessary to study the problem of a previous stop in the development of the embryo.
To exclude signs of a frozen pregnancy, you need:
- visit a geneticist who will consult a man and a woman. He will calculate the probability of a missed pregnancy;
- Both partners should be screened for sexually transmitted infections. If they are present, do not start conception until the body is fully restored;
- before conception, you need to find out the Rh factor and blood type. If the Rh is negative, the woman should be observed by a doctor who will control the dynamic observation and will control the antibody titer;
- control of the hormone progesterone will reduce the risk of miscarriage and developmental arrest. If its level is too low, a woman is prescribed special drugs.
It also makes sense to stop smoking and drinking pleasure drinks. It is necessary to do this not only for a woman, but also for a man.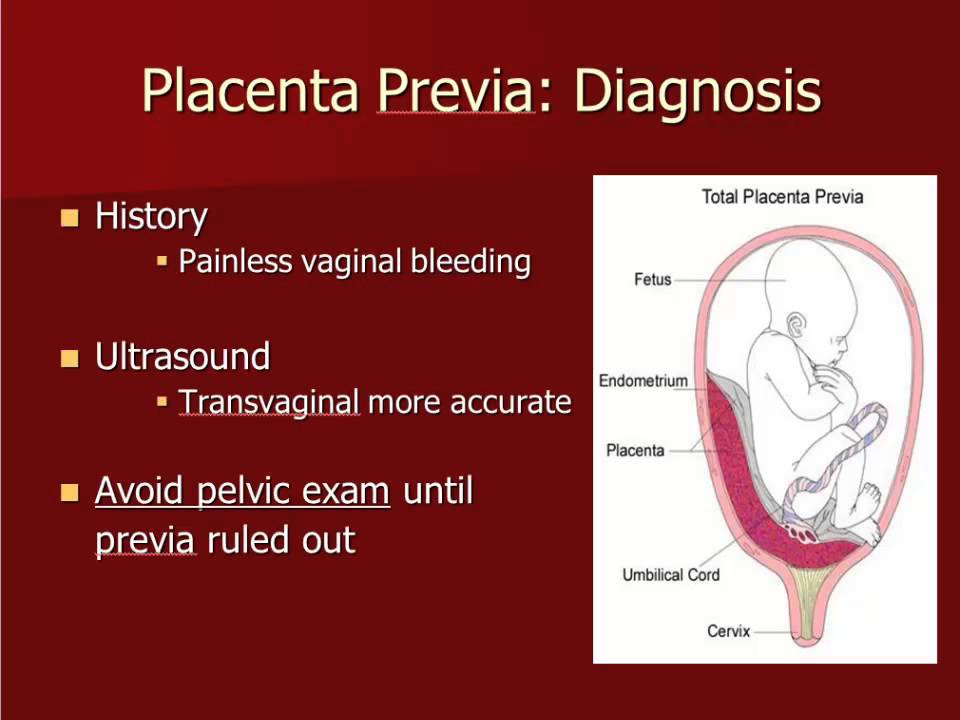
How to make an appointment with an obstetrician-gynecologist?
You can make an appointment with a doctor by filling out a simple form on the website or by calling +7 (495) 775-73-60. You can call around the clock. The causes of a missed pregnancy cannot be detected on their own, consultation of several specialists is required.
We are located near Mayakovskaya metro station and Belorusskaya metro station.
Missed pregnancy - causes, terms, signs of missed pregnancy
According to statistics, it is observed in one of 176 women. At the same time, it is difficult to guess which woman will have a fading pregnancy - age, social status and other factors are of secondary importance.
The concept of a missed pregnancy
A missed pregnancy means intrauterine death of the fetus, which occurs due to the development of irreversible processes. Thus, the development of the embryo stops, and its gradual decomposition occurs.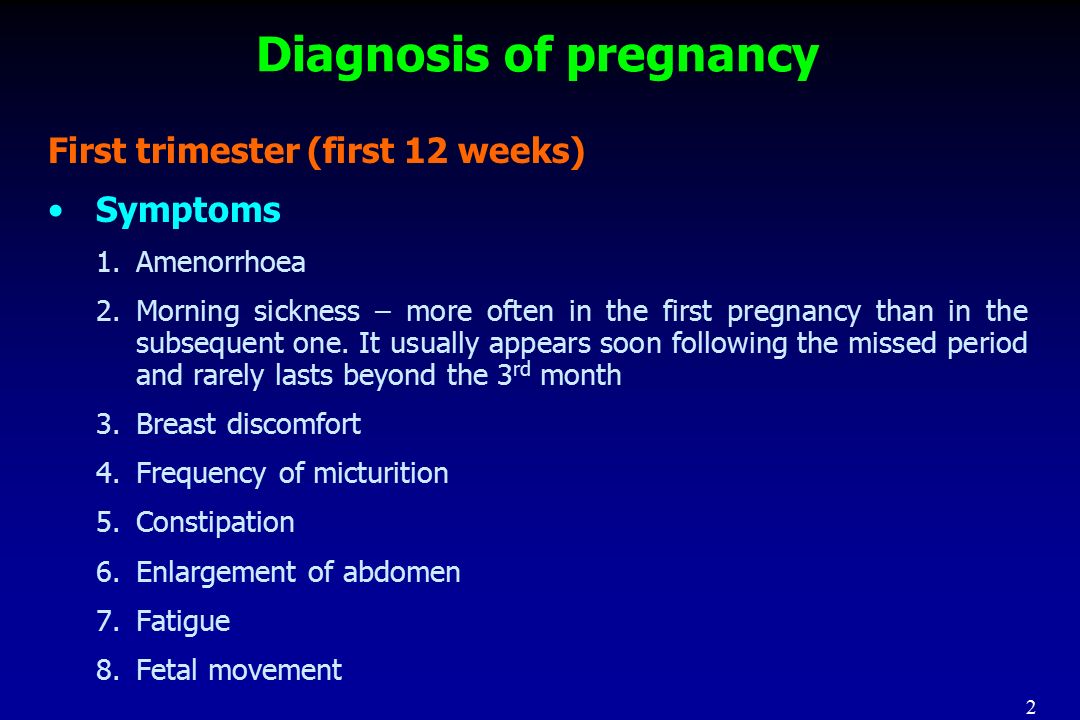
Miscarriage does not have sharp symptoms that are characteristic of a miscarriage, but it is dangerous in its own way and needs to be diagnosed in a timely manner.
Missed pregnancy should be distinguished from another pathology - an empty fetal egg. This is a fertilized egg attached to the tissues of the uterus, but there is no embryo in it.
Causes
The most common factor in the fading of pregnancy are gene mutations, when the death of the embryo occurs for up to 8 weeks. In addition to chronic and hereditary diseases of future parents, the pathology can be provoked by the consumption of drugs and alcohol in large quantities, potent drugs. The risk of pathology increases when a woman continues to eat, smoke and drink alcoholic beverages.
Sometimes a factor in the fading of pregnancy is the use of potent medications that is not agreed with the doctor. In this regard, in the first weeks of pregnancy, drug therapy is prescribed with extreme caution and in exceptional situations. After the 10th week, when the placenta is finally formed, the embryo is better protected from destructive external factors. Therefore, in the second trimester, taking the necessary medications can be resumed.
After the 10th week, when the placenta is finally formed, the embryo is better protected from destructive external factors. Therefore, in the second trimester, taking the necessary medications can be resumed.
The risk of pregnancy fading also increases in the following cases :
- Rh-conflict of mother and child: this primarily concerns women with multiple miscarriages and a history of abortions. With each termination of pregnancy, the body is more willing to reject the fetus, which gradually reduces the chances of successfully bearing a child.
- Viral and infectious processes: in complicated forms, there is a high risk of infection of the unborn child and its abnormal development, as well as death. When infected with rubella, measles or chickenpox, pregnant women are advised to have an abortion. Otherwise, it will remain to raise a child with developmental disabilities, which doctors must warn about.
- Hormonal disorders: with a deficiency of prolactin or an excess of testosterone, which is often manifested by irregular menstruation, the risk of miscarriage increases.

Multiple abortions, past cases of ectopic pregnancy and anomalies in the structure of the uterus are a reason for the special control of a pregnant woman. Close attention of a doctor is also required by women over 35 years old.
There is a high probability of pathology in women who neglect the management of pregnancy by a doctor. Therefore, for a successful delivery, registration with a specialist is required no later than 7-8 weeks of pregnancy.
It is also very important to undergo tests prescribed by narrow specialists - this is necessary for the early detection of genetic abnormalities and the prevention of serious complications.
Terms of increased risk
Cases of miscarriage are fixed at different terms, including when only a few days remain before delivery. But, according to statistics, the greatest risks occur at certain times:
- 3-4 weeks after conception;
- 7-11 weeks;
- 16-18 weeks.
The highest percentage of missed pregnancies is determined by doctors before the 14th week, after the 20th week the embryo is already less vulnerable. In the first weeks, the fetus ceases to function due to hormonal surges and due to hereditary causes, after the first trimester, its development is interrupted by infectious and viral diseases.
In the first weeks, the fetus ceases to function due to hormonal surges and due to hereditary causes, after the first trimester, its development is interrupted by infectious and viral diseases.
Symptoms
In the early stages of pregnancy
Miscarriage is not expressed by acute clinical symptoms, so women often notice the pathology too late. However, it is deadly because the decomposition of the fetus causes intoxication of the mother's body. In the future, this has a bad effect on reproductive health and complicates attempts to bear a child in the future.
It is important to pay close attention to your condition in order to notice possible symptoms of a fading pregnancy in time:
- Vaginal discharge: first, about 48 hours, white discharge is noted, then mucus appears with bloody patches, bleeding gradually increases. So the body tries to expel the foreign body.
- Features of toxicosis: attachment of the fetus to the endometrium provokes the production of the hormone hCG, which causes vomiting.
 With a frozen pregnancy, the production of hCG stops, the feeling of nausea goes away. However, early diagnosis is not made. It happens that a decrease in the intensity of toxicosis is simply an adaptation of a woman's body to the presence of a fetus.
With a frozen pregnancy, the production of hCG stops, the feeling of nausea goes away. However, early diagnosis is not made. It happens that a decrease in the intensity of toxicosis is simply an adaptation of a woman's body to the presence of a fetus. - Jumps in basal temperature: in the normal state, this figure does not exceed 37 ° C. After the death of the embryo, it decreases to 36.7 ° C, and when it decomposes, it rises sharply to 37.5 ° C.
- Feeling unwell: observed with a long decomposition of the fetus, when the pathology has not yet been identified - a woman perceives a bad state of health as a cold, a general breakdown. Then there are other serious signs: dizziness, fever, abdominal cramps, anxiety.
In late pregnancy
In the second and third trimesters, the fetus gains weight well and grows to a large size. Therefore, in addition to the symptoms characteristic of pathology in the early stages, other manifestations are also observed:
- The fetus does not move for more than 24 hours.

- Stomach hurts and pulls.
- Leaking amniotic fluid with a characteristic putrid odor.
If the fetus does not move for more than 24 hours, another pathology is possible. Similar symptoms are characteristic of a lack of oxygen, which is caused by the umbilical cord wrapping around the neck and torso of the child. But it is also a reason for emergency medical attention, since a child wrapped around the umbilical cord can still be saved.
Regular breast assessments are recommended. With a frozen pregnancy for up to 25 weeks, after a few days, the mammary glands acquire their normal size. In the later stages, colostrum sometimes begins to stand out from the chest after the death of the fetus.
It is also possible to reduce the abdomen, which is caused by leakage of amniotic fluid. These are attempts by the body to expel the fetus, which has become a foreign body. Symptoms usually start within 2-3 days after the embryo has lost viability.
Diagnosis
Any of the above symptoms is a serious reason to visit a doctor and undergo the following diagnostic measures:
- visual examination in the gynecologist's office;
- hCG blood test;
- ultrasound examination;
- measurement of basal body temperature.
Medical examination and ultrasound are the main research methods, blood sample and basal temperature measurement are auxiliary.
On ultrasound for up to 7 weeks, the fetus may not yet show signs of vital activity read by the device. Also, the reason for the lack of signs of life often becomes an incorrectly established gestational age. Therefore, abortion is sometimes delayed until a second ultrasound.
The fetus is delayed in development up to 4 weeks in case of stress loads or failures of the hormonal system. If, after a second ultrasound performed after 2 weeks, the fetus remains unchanged in size, this is a sign of its death.
Ultrasound is usually enough to make a diagnosis. In the first weeks, this is evidenced by the incorrect location and ruptures of the fetal egg. In the later stages, there is no heartbeat, the dimensions do not correspond to the deadline.
Treatment
If the diagnosis is confirmed, the woman is scheduled for an abortion. Each patient has their own method.
Each patient has their own method.
First trimester
Medical abortion is usually prescribed to terminate a missed pregnancy up to 9 weeks in Russia and up to 12 weeks in the West. The active ingredients are mifepristone and misoprostol. With high efficiency, this method has the following contraindications:
- ectopic pregnancy;
- severe anemia;
- renal and hepatic insufficiency;
- poor blood clotting.
Curettage is a traditional way of terminating a pregnancy, which is prescribed only when the effectiveness of medications is low and to clean the uterus from embryo fragments. Curettage is indicated until the 12th week of pregnancy. Whenever possible, doctors try to avoid this procedure, since irreversible consequences are possible as a result of trauma to the tissues of the reproductive organs.
Before the curettage procedure, a woman must undergo ultrasound, ECG, donate blood, consult an anesthesiologist. The scraping procedure consists of the following steps:
The scraping procedure consists of the following steps:
- Intravenous anesthesia (using a fast-acting agent).
- Treatment of genital organs with antiseptics.
- Fixation of the cervix with forceps and dilation of the cervical canal.
- Curettage of the mucous membranes of the uterus and cervical canal with a curette - a gynecological instrument with a loop at the end.
- Treatment of the uterus with drugs to stimulate contractions and a disinfectant iodine solution.
After the procedure is completed, the doctor removes the fixation instruments and applies a cold compress to the woman's abdomen. This helps to tone the uterus due to vasoconstriction. After 6-7 weeks, the menstrual cycle is restored.
Second trimester
At 13-22 weeks of pregnancy, other methods are used that cause artificial induction of labor:
- Intramial: 20% sodium chloride solution is injected into the water bladder with a special thin needle.
- Isolated: Mifepristone or misoprostol is injected into the genital tract, and one of these drugs is given by mouth.
In case of contraindications or low effectiveness of the above methods, a load is applied to the pre- posed section of the amniotic sac.
Third trimester
In the third trimester, the only sure way is artificial labor, which is carried out urgently and without anesthesia. Cesarean section is excluded due to the high risk of infection of the woman.
Rehabilitation
In order for the results of treatment to have a positive effect, the woman must strictly follow the doctor's recommendations and continue rehabilitation therapy:
- Hormone therapy for the regeneration of uterine endometrial cells.
- Antibacterial therapy including macrolides or cephalosporins to prevent infection of the endometrium.
- Physiotherapy necessary for the healing of uterine tissues.
- Taking immunostimulating drugs.

Consequences
Termination of pregnancy, even for medical reasons, in any way, is a blow to the reproductive system of a woman. Therefore, a complete rehabilitation of the body is possible no earlier than six months later. All this time, hormone therapy is necessary in accordance with the doctor's recommendations.
If not properly treated, a missed pregnancy has a devastating effect on women's health and causes the following complications:
- Mental disorder: after an abortion, a woman has doubts about her next attempts to become pregnant and bear a child, fear of failure grows. Therefore, treatment must be accompanied by competent psychotherapy.
- Inflammatory processes in the uterus: this common complication occurs after curettage, because during the procedure the mucous membranes are stopped and the tissues of the uterus remain defenseless against bacteria.
- Adhesive processes: adhesion and adhesion of the inner surfaces of the uterus to each other is usually the result of inflammation.
 This provokes deformation of the uterus, which, if not properly treated, most likely leads to infertility.
This provokes deformation of the uterus, which, if not properly treated, most likely leads to infertility.
Infertility, the most serious complication of a miscarriage, is caused by non-compliance with medical recommendations and improper treatment. Therefore, it is not enough to terminate a frozen pregnancy. Throughout the rehabilitation period and until a new pregnancy, a woman should be regularly observed by a gynecologist.
Prevention
In order for the pathology not to recur, competent preparation for pregnancy should not be neglected. Future parents must undergo a comprehensive medical examination, including blood samples, genetic tests, ultrasound screening and other procedures. The doctor may prescribe additional diagnostic procedures. You should not conceive a child if one of the spouses had rubella, chickenpox or severe flu less than six months ago. Pregnancy planning also includes the treatment of chronic diseases even before the first attempts at conception.
Other preventive measures are also recommended:
- healthy lifestyle;
- timely vaccination;
- control over the state of the hormonal system;
- genetic counseling;
- refusal of air travel in the first weeks of pregnancy.
High-quality preparation is a long-proven factor in the successful onset and bearing of pregnancy. Even if a woman has previously experienced unsuccessful pregnancy attempts with miscarriages and missed pregnancy, competent planning gives a chance to endure and give birth to a healthy child at 90% of cases. After a diagnosed fading, it is necessary to plan a pregnancy with the support of multidisciplinary specialists and quality control over the woman's health.
“The fetus froze”, “The heart of the fetus stopped” - these phrases are heard by about 20% of Russian women during a routine routine examination or after an extended ultrasound. And then - the cruel "You will give birth again."
It seems that it is impossible to realize and accept: just yesterday you thought up a name for the baby you carried under your heart and managed to fall in love with, but today you have to come to terms with the loss of an unborn child.
“Twice in my life, doctors said the most important words —“ you are pregnant ”— and the most terrible —“ the pregnancy is frozen, we are preparing for hospitalization, ”writes our reader Elena. - The first time it happened during an ultrasound. I looked at the monitor, on which a little man with miniature arms and legs was already looming, the doctor moved the device over my stomach and noted something in the medical record. Everything happened as usual. And suddenly, for some reason, they began to call another gynecologist by phone. After a long deliberation, the doctors came up with a terrible verdict: “We are very sorry, but your fetus is dead.” It is the fetus, not the child. This happened at 24 weeks. Three years later, I managed to get pregnant again, but I stayed in an interesting position for only 7 weeks. My friends don't understand my grief. Everyone repeats like parrots: you will give birth again. I look at the only ultrasound of my first baby and I don't believe I can carry a baby. I am tormented by guilt in front of the baby, which doctors call the embryo.
I am tormented by guilt in front of the baby, which doctors call the embryo.
Elena Remez
ELENA REMEZ
Obstetrician-gynecologist, candidate of medical sciences, leading specialist of the SM-Clinic holding
The first signs of missed pregnancy
term, - explains Elena Anatolyevna. - From the moment of conception to 8 weeks - the most important and decisive period in the development of the embryo. It is at this time that genetic mutations can occur, leading to severe malformations of the fetus and its death.
A woman may independently suspect a missed pregnancy by indirect signs, for example, a sudden cessation of toxicosis, the appearance of pulling pains in the lower abdomen and spotting from the genital tract, the absence of pain in the chest (women may notice that their mammary glands have ceased to "pour" and abruptly decreased in size).
“If you notice something like this, you should immediately contact a gynecologist to clarify the situation and take timely measures. The doctor will prescribe an ultrasound scan and blood tests to confirm the diagnosis or refute suspicions, ”emphasizes Elena Anatolyevna.
The doctor will prescribe an ultrasound scan and blood tests to confirm the diagnosis or refute suspicions, ”emphasizes Elena Anatolyevna.
Why does miscarriage occur?
In the first trimester, the main cause of miscarriage is genetic mutations, unfortunately we are not able to influence this. Also during this period, the embryo is more susceptible to the influence of negative external factors, so it is important to plan pregnancy and strictly adhere to a healthy lifestyle: exclude alcohol, do not take medications without consulting a doctor, postpone studies using x-rays, do not come into contact with chemicals.
At the beginning of pregnancy, the expectant mother should try to avoid viral diseases. Even SARS can lead to sad consequences. The presence of problems associated with hormonal imbalance and hemostasis can also cause the death of the embryo, so it is important to find out all the risk factors before pregnancy.
Immune, hormonal and hemostatic system failures; acute and chronic processes in the uterus and appendages, pathological processes in the cervical canal, infections of the genital tract, as well as stress, work overload, an overly active lifestyle can cause fetal loss not only in the early stages, but also in the second and third trimesters .
Miscarriages may be due to past abortions, miscarriages or pelvic surgeries. To avoid this, doctors recommend conducting a pre-gravid examination - a medical examination of the state of the female body, during which various pathologies are detected before conception. History taking, blood tests, genetics consultation, screening for hereditary diseases.
When can I try to get pregnant again?
The recovery period depends on how long the pregnancy loss occurred. If this happened in the first trimester (the period from the 3rd to the 8th week is especially dangerous, when the internal organs of the child are being formed), then it will take six months to restore the body.
“During the first month, excessive physical activity, visits to baths, saunas, sexual intercourse are prohibited,” the doctor notes. “It is also recommended to undergo a full examination during this period, consult a psychologist and a geneticist.”
Treatment is individual for every woman. The doctor may prescribe hormone therapy, genetic studies, examinations for sexually transmitted infections, MRI of the pelvic organs, etc. In some cases, laparoscopy or hysteroscopy is necessary.
The doctor may prescribe hormone therapy, genetic studies, examinations for sexually transmitted infections, MRI of the pelvic organs, etc. In some cases, laparoscopy or hysteroscopy is necessary.
A missed pregnancy is not a sentence
“If a woman has already had a missed pregnancy in her anamnesis, what should be done to prevent this from happening again?”. This question often worries patients, says the doctor. - I want to immediately reassure expectant mothers: a missed pregnancy is not a sentence, but a serious reason to undergo a full examination, which will help identify the cause of the loss of a child, if possible, eliminate it or correct it with medications. This will allow you to plan a future pregnancy as safely as possible.
There is a chance to carry and give birth to a healthy child even after two or more missed pregnancies. There are many happy examples in medical practice when women already despaired of becoming mothers, but fate gave them such an opportunity.
Unfortunately, the loss of a child at an early stage of pregnancy is quite common. After the first miscarriage, a woman lives in constant fear and is afraid that the second attempt to become a mother will turn into a tragedy.
“A miscarriage is a spontaneous termination of pregnancy before the fetus reaches a viable term. A fetus weighing up to 500 g is considered viable, which corresponds to a period of less than 22 weeks of pregnancy. Many women face this diagnosis. About 80 percent of miscarriages occur before 12 weeks of pregnancy."
Causes of miscarriage
Approximately half of early miscarriages occur due to genetic pathologies in the development of the fetus, that is, defects in the number and composition of chromosomes. It is in the first weeks that the formation of the baby's organs begins, which requires 23 normal chromosomes from each of the future parents. When at least one abnormal changes occur, there is a risk of losing a child.
At 8-11 weeks the rate of such miscarriages is 41-50%, at 16-19weeks of pregnancy, the frequency of miscarriages caused by chromosomal defects drops to 10 to 20 percent.
There are other causes of miscarriage. Among them:
- Congenital and acquired disorders of the anatomy of the genital organs If there are fibroids, polyps in the uterus, this can cause abnormal development of the embryo. The threat of miscarriage may be in women with an abnormal development of the uterus.
- Infectious causes Numerous studies have shown that the risk of miscarriage increases in the presence of sexually transmitted infections. Dangerous for a pregnant woman are measles, rubella, cytomegalovirus, as well as diseases that occur with an increase in body temperature. Intoxication of the body often leads to the loss of a child.
- Endocrine causes Problems with childbearing occur with diabetes, thyroid disease, adrenal gland disorders.
- Unfavorable ecology, exposure
- Blood clotting disorders (thrombosis, antiphospholipid syndrome) APS (antiphospholipid syndrome) is a disease in which a lot of antibodies are produced in the human body to phospholipids - chemical structures from which parts of cells are built. The body mistakenly perceives its own phospholipids as foreign and begins to defend itself against them: it produces antibodies to them that damage blood components. Blood clotting increases, microthrombi appear in small vessels that feed the fetal egg and placenta. Blood circulation in the fetal egg is disturbed. As a result, the pregnancy stops or the growth of the fetus slows down. Both of these lead to miscarriage. All this is due to the hormonal background that has changed during pregnancy.
- Lifestyle and bad habits Nicotine addiction, alcohol use, obesity.
Is it possible not to notice a miscarriage
Sometimes women mistake a miscarriage for normal menstruation. This occurs during the so-called biochemical pregnancy, when there is a violation of the implantation of the embryo at a very early stage and menstruation begins. But before the appearance of spotting, the test will show two strips.
This occurs during the so-called biochemical pregnancy, when there is a violation of the implantation of the embryo at a very early stage and menstruation begins. But before the appearance of spotting, the test will show two strips.
The classic variant is when a miscarriage is manifested by bleeding against the background of a long delay in menstruation, which rarely stops on its own. Therefore, even if a woman does not follow the menstrual cycle, the signs of an interrupted pregnancy will be immediately noticed by the doctor during examination and ultrasound.
Alarm
Symptoms of a miscarriage can be completely different, and depending on them, as a rule, you can predict the likelihood of maintaining and successfully continuing this pregnancy.
For the threat of miscarriage is characterized by pulling pains in the lower abdomen and lumbar region, scanty bloody discharge from the genital tract. Ultrasound signs: the tone of the uterus is increased, the cervix is not shortened and closed, the body of the uterus corresponds to the gestational age, the fetal heartbeat is recorded.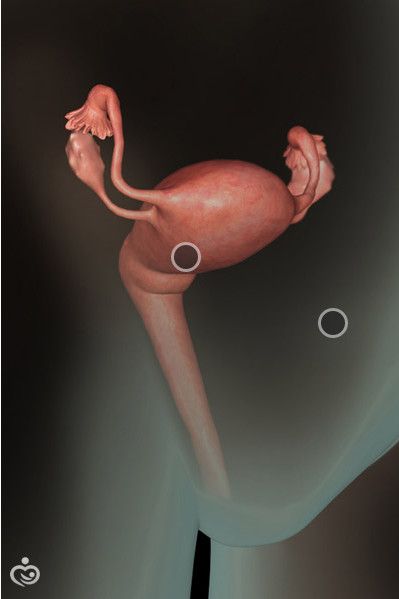
Started miscarriage — pain and discharge from the genital tract are more pronounced, the cervix is ajar.
Miscarriage in progress - cramping pain in the lower abdomen, copious bloody discharge from the genital tract. On examination, as a rule, the uterus does not correspond to the gestational age, the cervix is open, the elements of the fetal egg are in the cervix or in the vagina.
Incomplete miscarriage - the pregnancy was interrupted, but there are delayed elements of the fetal egg in the uterine cavity. This is manifested by ongoing bleeding due to the lack of a full contraction of the uterus.
Non-progressive pregnancy - the death of an embryo (up to 9 weeks) or a fetus up to 22 weeks of gestation in the absence of any signs of termination of pregnancy.
Important!
Severe abdominal pain and bloody discharge at any stage of pregnancy is a reason for an urgent appeal to an obstetrician-gynecologist with a decision on hospitalization in a gynecological hospital.
Is it possible to avoid miscarriage
“Today, there are no methods to prevent miscarriages,” says the doctor. “Therefore, it is very important to comprehensively prepare for pregnancy before it occurs by visiting an obstetrician-gynecologist and following all the necessary recommendations for examination and taking the necessary drugs.”
But if, nevertheless, the pregnancy could not be maintained, then the birth of a child can be planned again no earlier than 3-6 months after the miscarriage. This time is needed to figure out, together with the attending physician, what are the causes of miscarriage and whether it is possible to avoid them in the future.
By the way, a common misconception for both women and men is that only the woman is to blame for the loss of pregnancy, but this is far from being the case.
“A man is also responsible, which is why future dads are required to perform a study - a spermogram and be screened for genital infections, since with a pathology of spermatozoa, the likelihood of miscarriage due to genetic abnormalities increases many times,” emphasizes our expert.
There is always a chance
Most women whose first pregnancy ends in a miscarriage have a high chance of a successful next pregnancy (about 85 percent) if they are examined before pregnancy and the causes are corrected. “A woman who has lost a child needs the support of her family and friends. Sometimes words are unnecessary, just be there. Duty phrases from the series “You will definitely give birth”, “It was just an embryo” hurt very much. The best consolation is to advise you to see a doctor,” says Natalia Kalinina.
In a non-developing pregnancy, which is also called a "missed pregnancy", the death of the embryo/fetus occurs, but there are no clinical signs of spontaneous miscarriage.
Causes of miscarriage
The causes of miscarriage are very diverse, for example, stopping the development of the embryo/fetus may be due to an inflammatory process as a result of the action of various microorganisms. Most often, the causative agents of inflammation are: streptococci, staphylococci, E. coli, Klebsiella, rubella virus, cytomegalovirus, herpes simplex virus, Coxsackie virus, mycoplasmas, chlamydia, treponema, mycobacteria, toxoplasma, plasmodia, fungi (thrush).
coli, Klebsiella, rubella virus, cytomegalovirus, herpes simplex virus, Coxsackie virus, mycoplasmas, chlamydia, treponema, mycobacteria, toxoplasma, plasmodia, fungi (thrush).
Chronic infectious diseases in a woman most often do not directly lead directly to intrauterine death of the fetus, but cause certain disturbances in its development, which contribute to intrauterine death under the influence of other factors. For example, as a result of direct exposure to an infectious factor, a heart defect is formed in the fetus, which prevents its further normal development. However, not always and not every infection leads to the death of the embryo/fetus. In this case, the influence of the infection depends on the route of its penetration, the involvement of the fetus and amniotic membranes in the infection, the type and activity of the pathogen, the number of penetrating microorganisms, the duration of the mother's disease, the activity of the body's defenses, and other factors.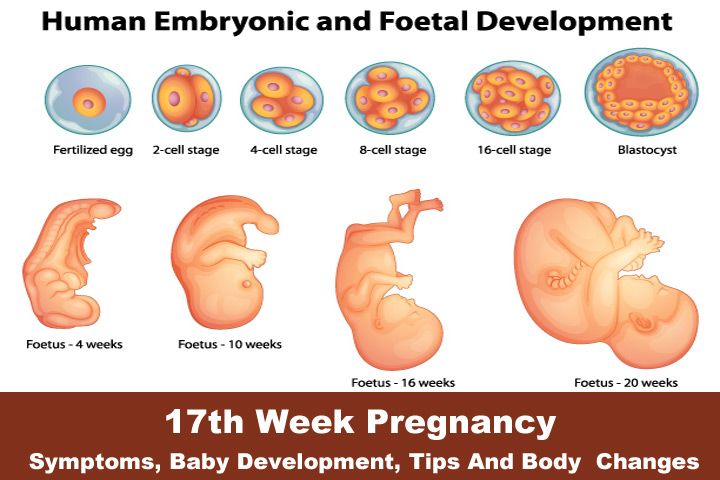
Microorganisms can enter the uterus from the lower parts of the reproductive system, infecting the amniotic fluid, which is then swallowed by the fetus. The infection can spread through the amniotic membranes, and further to the fetus, causing damage to its internal organs, which, in turn, is the cause of its death. The infection can also get to the fetus from chronic foci of inflammation in the fallopian tubes and ovaries.
The death of the embryo/fetus may be due to a violation of the immune relationship, given that the fetal egg is half foreign to the mother's body. At the same time, rejection reactions are activated, aimed at defeating the fetal egg and removing it from the uterus. Non-developing pregnancy can be caused by various chromosomal disorders in the first 6-7 weeks of pregnancy, chromosomal changes are present in 60-75% of cases of spontaneous abortion, at 12-17 weeks. - in 20-25%, at 17-28 weeks. at 2-7%. With age, the likelihood of chromosomal abnormalities increases. The causes of the development of chromosomal disorders are also unfavorable external factors. The thrombotic complications caused by genetic defects in the blood coagulation system in a pregnant woman can cause an arrest in the growth and development of the embryo/fetus. The most common among them are: factor V Leiden mutation, prothrombin G202110A mutation, methyltetrahydrofolate reductase mutation, plasminogen activator gene polymorphism, platelet receptor polymorphism.
The causes of the development of chromosomal disorders are also unfavorable external factors. The thrombotic complications caused by genetic defects in the blood coagulation system in a pregnant woman can cause an arrest in the growth and development of the embryo/fetus. The most common among them are: factor V Leiden mutation, prothrombin G202110A mutation, methyltetrahydrofolate reductase mutation, plasminogen activator gene polymorphism, platelet receptor polymorphism.
Blood coagulation disorders caused by antiphospholipid syndrome also determine the unfavorable development of the embryo/fetus. In the early stages of pregnancy, the role of the direct damaging effect of antiphospholipid antibodies on the structures of the fetal egg, followed by spontaneous abortion, is not excluded. With this pathology, the process of implantation of the fetal egg is disrupted. In addition, with antiphospholipid syndrome, a decrease in the formation of placental vessels and a decrease in its function, which may be the cause of an undeveloped pregnancy.![]() Another cause of impaired development of the embryo / fetus and placenta in antiphospholipid syndrome is thrombosis and damage to the uteroplacental vessels.
Another cause of impaired development of the embryo / fetus and placenta in antiphospholipid syndrome is thrombosis and damage to the uteroplacental vessels.
Hormonal changes are also distinguished among the causes of miscarriage. Violation of the formation and decrease in the function of the corpus luteum in the ovary leads to a decrease in progesterone and inadequate preparation of the uterus for implantation of the fetal egg. In this regard, the formation of uteroplacental circulation is disrupted, which entails a decrease in the blood supply to the embryo/fetus, and its death. Often, such disorders occur with excessive accumulation in the body of a woman of male sex hormones (Stein-Leventhal syndrome, adrenogenital syndrome), with reduced or increased thyroid function.
The shorter the gestational age, the higher the sensitivity of the embryo/fetus to the action of damaging factors. However, it decreases unevenly throughout fetal development. There are critical periods during pregnancy, in which the ovum, embryo, fetus are especially vulnerable to adverse effects: the implantation period (7-12 days), the embryogenesis period (3-8 weeks), the placenta formation period (up to 12 weeks), the formation period the most important functional systems of the fetus (20-24 weeks).
Clinical signs - symptoms of missed pregnancy
There are a number of consecutive disorders, characteristic of missed pregnancy : decrease and cessation of uteroplacental circulation against the background of damage to the structures of the placenta; cessation of uteroplacental circulation; violation of the structure of the inner layer of the uterus (endometrium), caused by the presence of dead elements of the fetal egg in the uterine cavity.
Clinical signs of miscarriage may be extremely poor against the background of the cessation of the increase in the size of the uterus and their inconsistency with the gestational age. However, the uterus can be of normal size, can be reduced, and can even be enlarged if it is filled with blood during detachment of the fetal egg.
For some time after the death of the embryo/fetus, the patient may feel pregnant. However, over time, the subjective signs of pregnancy gradually disappear. Smearing spotting from the genital tract and spastic pains in the abdomen are periodically noted. Chorionic gonadotropin in the blood of a woman, as a rule, is at an extremely low level or even completely absent.
Chorionic gonadotropin in the blood of a woman, as a rule, is at an extremely low level or even completely absent.
Diagnosis of non-developing pregnancy
0498 ultrasound in the absence of a fetal heartbeat. One of the most common options for non-developing pregnancy is anembryony, i.e. the absence of an embryo in the cavity of the fetal egg after 5-6 weeks of pregnancy. In this case, the fetal egg is smaller than expected, and the embryo is not visualized.
In other cases of non-developing pregnancy, according to ultrasound, the fetal egg matches or lags in size in its development, the embryo can be visualized, but without a heartbeat. Often, a retrochorial hematoma can be detected, which is an accumulation of blood at the site of detachment of the fetal egg from the uterine wall.
With a longer stay of the dead embryo in the uterus, visualization of the embryo is impossible, there are no signs of its vital activity. The size of the uterus lags behind the gestational age, there is a deformation of the fetal egg with fuzzy contours.
Removal of the dead ovum
The death of the embryo/fetus is not always accompanied by its spontaneous expulsion from the uterus. Often there are cases when a dead fetal egg lingers in the uterus for an indefinitely long time. The reason for such a delay may be: primary tight attachment of the fetal egg to the uterine wall during implantation, inferiority of immune rejection reactions of the dead fetal egg, and a decrease in the contractile activity of the uterus.
If a dead embryo is in the uterus for 2-4 weeks or more, the elements of the decay of the dead fetal egg enter the maternal bloodstream, which leads to a violation of the blood coagulation system and can cause massive bleeding when trying to terminate the pregnancy. In this regard, before curettage of the uterus in order to remove the dead fetal egg, it is necessary to perform studies of the state of the blood coagulation system and, if necessary, conduct appropriate treatment.
After a thorough examination and appropriate preparation of the woman (carrying out therapeutic and preventive measures aimed at reducing the risk of possible complications), it is necessary to terminate the miscarriage. For this purpose, instrumental or drug-induced dilation of the cervix and instrumental removal of the contents of the uterus are performed. It is also possible to use special medications for non-operative removal of the ovum from the uterus. An ultrasound scan should be performed immediately during the abortion or immediately after it is completed to ensure that parts of the fetus and placenta have been completely removed. After removal of the fetal egg in non-developing pregnancy, regardless of the method of termination, it is advisable to conduct anti-inflammatory treatment.
For this purpose, instrumental or drug-induced dilation of the cervix and instrumental removal of the contents of the uterus are performed. It is also possible to use special medications for non-operative removal of the ovum from the uterus. An ultrasound scan should be performed immediately during the abortion or immediately after it is completed to ensure that parts of the fetus and placenta have been completely removed. After removal of the fetal egg in non-developing pregnancy, regardless of the method of termination, it is advisable to conduct anti-inflammatory treatment.
In each case of a non-developing pregnancy, an in-depth examination is required to identify possible causes of abortion with their subsequent elimination or weakening of the effect.
How to reduce the risk of embryo death?
To reduce the likelihood of possible damaging factors in the course of pregnancy, it is necessary to conduct a screening examination of 90,501 patients planning a pregnancy, as well as women in the early stages of pregnancy, for urogenital infection. It is also important to conduct medical genetic counseling in order to identify high-risk groups for congenital and hereditary pathologies. In the presence of endocrine causes of miscarriage, appropriate corrective hormonal therapy should be selected.
It is also important to conduct medical genetic counseling in order to identify high-risk groups for congenital and hereditary pathologies. In the presence of endocrine causes of miscarriage, appropriate corrective hormonal therapy should be selected.
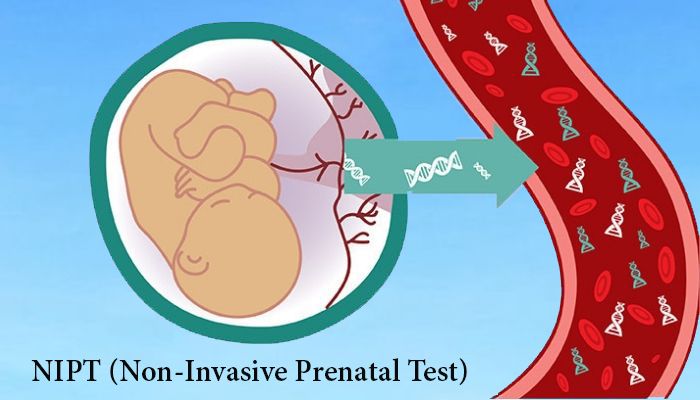
It is also important to identify various autoimmune disorders and their correction. Re-pregnancy is possible when the identified causes of embryo/fetal death are eliminated, and after the necessary treatment has been carried out. In case of a new pregnancy, an ultrasound examination is performed, markers of possible fetal developmental disorders are determined in the blood, including: α - fetoprotein, chorionic gonadotropin, PAPP-A test in the most informative terms. According to indications, invasive prenatal diagnostics is also carried out, including chorion biopsy, amniocentesis or cordocentesis to determine chromosomal and a number of monogenic diseases of the fetus. In addition, they carry out therapeutic and preventive measures aimed at eliminating the infectious process, conduct specific anti-inflammatory therapy in combination with immunocorrectors, correct violations of the blood coagulation system and prevent placental insufficiency from 14-16 weeks of pregnancy.