How to treat child cough at night
Home Treatments and Seeking Help
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Coughing in toddlers
Colds and coughs are common in young children. Exposure to germs and fighting them helps kids develop their immune systems. Helping your child to feel comfortable and manage their symptoms can help them get the rest they need to help them recover.
A regular cough can last up to two weeks. Many coughs are due to common viruses that have no cure. Unless a cough is extreme or comes with other, serious symptoms (see our list below), the best solution is to offer comfort measures at home.
Cough treatment should aim to keep your child hydrated, relaxed, and sleeping well. It’s not important to try to stop the coughing itself.
Read on to discover toddler cough remedies you can try at home, plus learn how to identify the signs that your child needs to see a doctor.
8 Home remedies
Pay attention to the sound of your child’s cough to help you pick the best home remedy and so that you can properly explain the cough to a doctor. For example:
- Deep cough coming from the chest. It’s likely due to mucus in the airways.
- Tight cough coming from the upper throat. It may be due to an infection and swelling around the larynx (voice box).
- Mild cough with sniffing. It could be due to post-nasal drip from the back of your child’s throat.
1. Use saline nasal drops
You can buy these over-the-counter nasal drops at a pharmacy. Used with a nasal syringe or nose blowing, saline drops can soften mucus to help remove it.
Follow the instructions on the bottle to administer the nasal drops safely.
If it’s impossible to get these little drops in your toddler’s nose, sitting in a warm bath can also clear nasal passages and soften mucus. This helps prevent post-nasal drip.
You may especially want to use saline drops before bed or in the middle of the night if your toddler wakes up coughing.
Saline nasal drops are generally considered safe.
2. Offer fluids
Staying hydrated is especially important when your child is sick. Water helps the body fight illness and keeps airways moist and strong.
One way to make sure your child is getting enough water is to have them to drink one serving of water (8 ounces or 0.23 liters) for each year of their life. For example, a one-year-old needs a minimum of one serving of water per day. A two-year-old needs two servings per day.
If they’re refusing their usual milk or not eating much, younger children may need more water. Offer water freely (at least every hour or two), but don’t push them to drink it.
In addition to enough water, you can offer popsicles to increase fluids and soothe a sore throat.
3. Offer honey
Honey is a natural sweetener that can help soothe a sore throat. Honey also has antibacterial properties and may help fight infection.
Honey also has antibacterial properties and may help fight infection.
Honey isn’t safe for children who are under one year of age because there’s a risk of botulism.
For toddlers over one, you can give a spoonful of honey as often as you like, but be aware of the sugar intake that comes with it.
You can also try mixing the honey in warm water to make it easier for your child to consume the honey. This has the added benefit of helping to hydrate your child, too.
4. Elevate your child’s head when sleeping
Babies under one-and-a-half years old should not sleep with any pillows.
Getting your older toddler to fall asleep with their head on one or more pillows can be difficult, especially if your child is prone to moving around a lot while they’re asleep.
An option other than using pillows in the crib or bed to elevate your toddler’s head, is to try elevating one end of the mattress. You can do this by placing a rolled-up towel under the mattress on the end where your child’s head rests.
However, you should ask your pediatrician before attempting this.
5. Add moisture with a humidifier
Adding moisture to the air helps keep your child’s airways from drying out and loosens mucus. This may ease coughing and congestion.
When purchasing a humidifier, choose a cold air humidifier. Cold air humidifiers are safer for children and as effective as warm air humidifiers. If possible, use purified or distilled water to slow down mineral buildup inside the humidifier.
Run a humidifier all night in the room where your toddler sleeps. During the day, run it in whatever room they’ll be spending the most time in.
If you don’t have a humidifier, you can try running a hot shower and blocking the crack under the bathroom door with a towel. Sit in the steamy bathroom to provide your child with some temporary relief.
6. Talk a walk in cold air
If it’s cold outside, you can try this folk remedy that uses the power of fresh air and exercise to relieve cough symptoms.
Bundle your child up for a walk in cold weather and aim for just a few minutes outside. You don’t want to exhaust your toddler, but there are many anecdotal stories of this helping coughs and shortening the length of a common cold.
Some parents even try opening the freezer door and standing their toddler in front of it for a few minutes if the child wakes up to a coughing fit in the middle of the night.
7. Apply vapor rub
It’s controversial whether vapor rubs that contain camphor or menthol are beneficial. Caretakers have been rubbing this balm on children’s chest and feet for generations, but one animal study suggested it may actually increase mucus, which can dangerously block tiny toddler airways.
Ask your pediatrician before using any vapor rub. If you do use a vapor rub, applying it to your child’s feet may be safer than on the chest where toddlers might touch it and then get it in their eyes.
Never use vapor rub on babies under two, and never put it on a child’s face or under their nose.
8. Use essential oils
These herbal products are gaining in popularity and some may be effective at easing a cough or muscle aches when applied on the skin or diffused into the air.
But always talk with your doctor before using essential oils. Not all oils are safe for toddlers, and dosage isn’t regulated.
Can you offer cough medicine?
Cough medicine isn’t recommended for toddlers or any child under six. It’s also not safe for young children, and it’s usually not effective at relieving their symptoms.
Any combination medicine for treating more than one symptom is likely to give kids more side effects and increase the risk of overdose.
Only offer cough drops to children four years old and older due to choking risks.
For children over the age of one, you can try a homemade cough recipe of honey dissolved in warm water and lemon juice.
Treatments from the doctor
In some cases, you may need to see a doctor to treat your child’s cough.
If your child has croup, their pediatrician may prescribe a steroid to decrease inflammation. Croup causes a tight, barking cough that tends to occur along with a fever.
The cough is usually worse at night. Steroids work best when given right away and they can be given to even very young toddlers.
If your doctor determines that your toddler has a bacterial infection, they may prescribe antibiotics. It’s important to give your child the full treatment: don’t stop antibiotics just when symptoms go away.
Does my toddler need to see a doctor?
If you’ve been treating your child’s cough at home for a few days and it’s getting worse, call your pediatrician’s office. The on-call nurse can give you more treatment ideas and help you decided whether or not to come in for a visit.
Asthma and allergies can cause chronic coughs and need to be treated by a doctor. Make an appointment if you think your toddler’s cough is due to either asthma or allergies.
Signs that your child should see a doctor include:
- cough that lasts more than 10 days
- fever over 100.
 4˚F (38˚C) for more than 3 days
4˚F (38˚C) for more than 3 days - labored breathing
- chest pain
- muscles pulling in around the neck or rib cage when breathing
- tugging on the ears, which may be a sign of ear infection
The doctor will observe your child’s breathing and, in some cases, may use an X-ray to get a diagnosis.
Go to an emergency room if your child:
- is lethargic or seems very ill
- showing signs of dehydration
- has rapid breathing or can’t catch their breath
- develops a blue tinge on the lips, nails, or skin, which is a sign of a lack of oxygen
The takeaway
Coughing is a common symptom in toddlers and can last for weeks.
Coughs may sound serious and can interrupt sleep, but unless your child is having difficulty breathing, showing signs of croup, or looking seriously sick, you can usually treat coughs at home.
Coughing (for Parents) - Nemours KidsHealth
What Are Coughs?
Coughs are one of the most common symptoms of childhood illness. A cough can sound awful, but usually isn't a sign of a serious condition. In fact, coughing is a healthy and important reflex that helps protect the airways in the throat and chest.
A cough can sound awful, but usually isn't a sign of a serious condition. In fact, coughing is a healthy and important reflex that helps protect the airways in the throat and chest.
What Are the Different Types of Coughs?
Sometimes, though, a cough needs a doctor's care. Understanding the different types of cough can help you know when to handle them at home and when to call your doctor.
The most common types of coughs are:
- "barky" cough
- whooping cough
- cough with wheezing
- nighttime cough
- daytime cough
- cough with a fever
- cough with vomiting
- persistent cough
"Barky" Cough
Barky coughs are usually caused by swelling in the upper airway. Most of the time, a barky cough comes from croup, a swelling of the larynx (voice box) and trachea (windpipe). Younger children have smaller airways that, if swollen, can make it hard to breathe. Kids younger than 3 are most at risk for croup because their airways are so narrow.
A cough from croup can start suddenly, often in the middle of the night. Most kids with croup will also have stridor, which is a noisy, harsh breathing that happens when the child inhales (breathes in).
Whooping Cough
Whooping cough (pertussis) is an infection of the airways caused by the
bacteriaBordetella pertussis. Kids with pertussis will have spells of back-to-back coughs without breathing in between. At the end of the coughing, they'll take a deep breath in that makes a "whooping" sound. Other symptoms are a runny nose, sneezing, mild cough, and a low-grade fever.
Whooping cough can happen at any age, but is most severe in infants under 1 year old who did not get the pertussis vaccine, which is part of the DTaP vaccine (diphtheria, tetanus, acellular pertussis). It's very contagious, so all kids should get the pertussis shot at 2 months, 4 months, 6 months, 15 months, and 4–6 years of age.
Cough With Wheezing
If your child makes a wheezing (whistling) sound when breathing out (exhaling), this could mean that the lower airways in the lungs are swollen. This can happen with asthma or with the viral infection bronchiolitis. Wheezing also can happen if the lower airway is blocked by a foreign object. A child who starts to cough after inhaling something such as food or a small toy should see a doctor.
Nighttime Cough
Lots of coughs get worse at night. When your child has a cold, the mucus from the nose and sinuses can drain down the throat and trigger a cough during sleep. This is only a problem if the cough won't let your child sleep.
Asthma also can trigger nighttime coughs because the airways tend to be more sensitive and irritable at night.
Daytime Cough
Cold air or activity can make coughs worse during the daytime. Try to make sure that nothing in your house — like air freshener, pets, or smoke (especially tobacco smoke) — is making your child cough.
Cough With a Fever
A child who has a cough, mild fever, and runny nose probably has a common cold. But coughs with a fever of 102°F (39°C) or higher can sometimes be due to pneumonia, especially if a child is weak and breathing fast. In this case, call your doctor immediately.
Cough With Vomiting
Kids often cough so much that it triggers their gag reflex, making them throw up. Also, a child who has a cough with a cold or an asthma flare-up might vomit if lots of mucus drains into the stomach and causes nausea. Usually, this is not cause for alarm unless the vomiting doesn't stop.
Persistent Cough
Coughs caused by colds due to viruses can last weeks, especially if a child has one cold right after another. Asthma, allergies, or a chronic infection in the sinuses or airways also might cause lasting coughs. If your child still has a cough after 3 weeks, call your doctor.
How Are Types of Coughs Diagnosed?
If you're concerned about your child's cough, call your doctor. Depending on the type of cough, other symptoms, and how long it's lasting, the doctor might want to see your child.
Depending on the type of cough, other symptoms, and how long it's lasting, the doctor might want to see your child.
Many health care providers now offer telehealth visits, which can save parents a trip to the office (especially for a nighttime cough). "Video chatting" lets doctors see and hear a child cough, and often this is enough to make a diagnosis or rule out a serious problem. Hearing the cough will help the doctor decide whether (and how) to treat it.
How Are Coughs Treated?
Most coughs are caused by viruses and have to just run their course. Sometimes, this can take up to 2 weeks. Doctors usually don't prescribe antibiotics because these only work against bacteria.
Unless a cough won't let your child sleep, cough medicines are not needed. They might help a child stop coughing, but they don't treat the cause of the cough. If you do use an over-the-counter (OTC) cough medicine, call the doctor to be sure of the correct dose and to make sure it's safe for your child.
Do not use OTC combination medicines (like "Tylenol Cold") — they have more than one medicine in them, and kids can have more side effects than adults and are more likely to get an overdose of the medicine.
Cough medicines are not recommended for any children under 6 years old.
How Can I Help My Child Feel Better?
To help your coughing child feel better:
- For a "barky" or "croupy" cough, turn on the hot water in the shower in your bathroom and close the door so the room will steam up. Then, sit in the bathroom with your child for about 20 minutes. The steam should help your child breathe more easily. Try reading a book together to pass the time.
- A cool-mist humidifier in your child's bedroom might help with sleep.
- Sometimes, brief exposure to cool air outdoors can relieve the cough. Make sure to dress your child appropriately for the outdoor weather and try this for 10–15 minutes.
- Cool beverages like juice can be soothing and it is important to keep your child hydrated.
 But do not give soda or orange juice, as these can hurt a throat that is sore from coughing.
But do not give soda or orange juice, as these can hurt a throat that is sore from coughing. - You should not give your child (especially a baby or toddler) OTC cough medicine without first checking with your doctor.
- If your child has asthma, make sure you have an asthma action plan from your doctor. The plan should help you choose the right asthma medicines to give.
- Cough drops are OK for older kids, but kids younger than 3 years old can choke on them. It's better to avoid cough drops unless your doctor says that they're safe for your child.
When Should I Call the Doctor?
Always call your doctor if your child is coughing and:
- has trouble breathing or is working hard to breathe
- is breathing faster than usual
- has a blue or dusky color to the lips, face, or tongue
- has a high fever (especially if your child is coughing but does NOT have a runny or stuffy nose)
- has any fever and is younger than 3 months old
- is younger than 3 months old and has been coughing for more than a few hours
- makes a "whooping" sound when breathing in after coughing
- is coughing up blood
- has stridor (a noisy or musical sound) when breathing in
- has wheezing when breathing out (unless your doctor already gave you an asthma action plan)
- is weak, cranky, or irritable
- is dehydrated; signs include dizziness, drowsiness, a dry or sticky mouth, sunken eyes, crying with little or no tears, or peeing less often (or having fewer wet diapers)
Cough syrup and cough solution - is there a difference? What is the best liquid cough remedy?
Published: May 13
Updated: June 17
Reading time: 4 minutes
Liquid cough preparations are popular because of their ease of use in both children and adults. How is a syrup different from a solution and is there a difference in what form of medicine to take? Let's figure it out in this article.
How is a syrup different from a solution and is there a difference in what form of medicine to take? Let's figure it out in this article.
Liquid dosage forms
Liquid dosage forms of preparations are obtained by dissolving the medicinal substance in a solvent - oil, water, alcohol and others. The liquid form is popular for several reasons:
- flexible dosing;
- the possibility of creating a medicine with a pleasant taste and smell, which is especially important in the treatment of children;
- predictable rate of drug action;
- less irritant;
- a wide range of ways to administer the drug to the body, for example, in the form of injections or syrups for oral administration.
There are several types of liquid dosage forms.
- Solutions.
The dosage form is obtained by dissolving the active substance in a solvent. It can be distilled water, glycerin, alcohol or various oils. The solution is always transparent, does not contain sediment and undissolved particles. This dosage form can be used both internally and externally in the form of lotions. In addition, solutions are administered intravenously and intramuscularly.
The solution is always transparent, does not contain sediment and undissolved particles. This dosage form can be used both internally and externally in the form of lotions. In addition, solutions are administered intravenously and intramuscularly. - Syrups.
The drug in the form of a syrup is intended for oral administration. It is a solution of sugars in high concentration, to which the active substance is added. The concentration of sugar in the syrup is not less than 64%. In less concentrated syrups, there is a risk of bacterial growth; in more concentrated syrups, precipitation in the form of sugar is possible. The preparations have a pleasant taste and smell, which are achieved by adding flavoring syrups (their share in the medicinal substance is from 5 to 20%). - Drops.
Such a dosage form may contain several active ingredients added to the solvent. Drops can be used both internally and externally. Liquid medicine in the form of drops is convenient to use due to the high concentration of the active substance in the preparation - they are easy to dose and take orally.
- Emulsions.
Consist of mutually insoluble liquids, such as oil and water. Emulsions are used orally, topically and parenterally (for example, by injection). To create a medicine, peach, castor, olive and other oils are used that do not mix with water. This dosage form helps to mask the unpleasant taste and smell of the drug, as well as reduce the intensity of the irritating effect. In addition, oils accelerate the absorption of the drug, since fat is absorbed faster in the digestive tract.
Solutions and syrups are most often used to treat coughs. Drugs in such dosage forms have a pleasant taste, are absorbed faster than tablet forms and begin to act in the gastrointestinal tract. Let's talk more about these types of drugs.
Cough syrup
Cough syrup is indicated for ARVI and other respiratory diseases. Antitussive syrups can be of two types.
- For dry cough.
Such drugs begin to act quickly, and the effect develops after the first application. They suppress the work of the cough center or reduce the sensitivity of the nerve endings of the respiratory tract. Dry cough syrups do not eliminate the cause of its occurrence, but only help adults and children reduce the manifestations of an unpleasant symptom.
They suppress the work of the cough center or reduce the sensitivity of the nerve endings of the respiratory tract. Dry cough syrups do not eliminate the cause of its occurrence, but only help adults and children reduce the manifestations of an unpleasant symptom. - For wet cough.
Wet cough syrups for children and adults may have an expectorant or mucolytic effect. Expectorants stimulate the excretion of sputum, mucolytics reduce its viscosity, making it easier to leave the respiratory tract.
Cough syrup may have anti-inflammatory and decongestant effects. You can drink cough syrup only after consulting a specialist, as the wrong choice of medicine can aggravate the disease and lead to complications .
Cough solution
Cough solution for adults and children can help relieve symptoms. The composition of the drug "Rengalin" includes affinity purified antibodies to histamine, bradykinin, morphine, so it helps to suppress inflammation in the airways and improve the drainage function of the airways. The drug is intended for children from 3 years of age and adults suffering from dry and wet cough. The active components of the solution inhibit the activity of the cough center, helping to alleviate an unproductive dry cough. In addition, the drug prevents the accumulation of sputum. Before using the drug, you should consult with your doctor.
The drug is intended for children from 3 years of age and adults suffering from dry and wet cough. The active components of the solution inhibit the activity of the cough center, helping to alleviate an unproductive dry cough. In addition, the drug prevents the accumulation of sputum. Before using the drug, you should consult with your doctor.
Similar articles
01 October
Smoker's cough
December 15
Tracheitis in adults
01 October
Cough does not go away for a long time: what to do?
Rengalin is the most prescribed antitussive drug. According to the 2019 RxTest™ Prescribing Audityear. Database "Market research system "Pharmxplorer", conducted by Proxima Research LLC.
"Product of the Year - 2021" in the nomination: "CONSUMER TRUST IN THE CATEGORY "MEDIUMS USED IN THE TREATMENT OF DRY AND WET COUGH"
How to relieve night cough | How to soothe a wet cough at night
Author, editor and medical expert
Petrashevich Anna Aleksandrovna
Number of views: 770 561
Date last updated: 09/23/2022
Title
Contents
Why is night cough dangerous?
How to relieve a night cough and relieve an attack?
Cough is an unpleasant phenomenon in itself, which prevents you from doing your usual activities and significantly worsens your general well-being. But when this condition does not stop day or night, the consequences can be much more serious than just feeling tired due to lack of sleep.
But when this condition does not stop day or night, the consequences can be much more serious than just feeling tired due to lack of sleep.
WHAT IS A NIGHT COUGH DANGEROUS?
Coughing attacks that occur at night can cause many temporary and even permanent health problems. To understand how harmful this condition is to the body, only one of the complications can be cited. Will you like memory impairment, decreased visual acuity, and impaired smell? It would seem that what does a night cough have in common with the loss of such important functions as the ability to clearly see the world around, remember information and smell? The relationship is more obvious than it seems at first glance: oxygen starvation and lack of rest in the main organ of the human body - the brain. In the dark, the brain must rest and restore the resources spent during the day. These processes are possible only in the process of deep sleep, into which the body is simply not able to immerse itself - it is constantly awakened by a cough.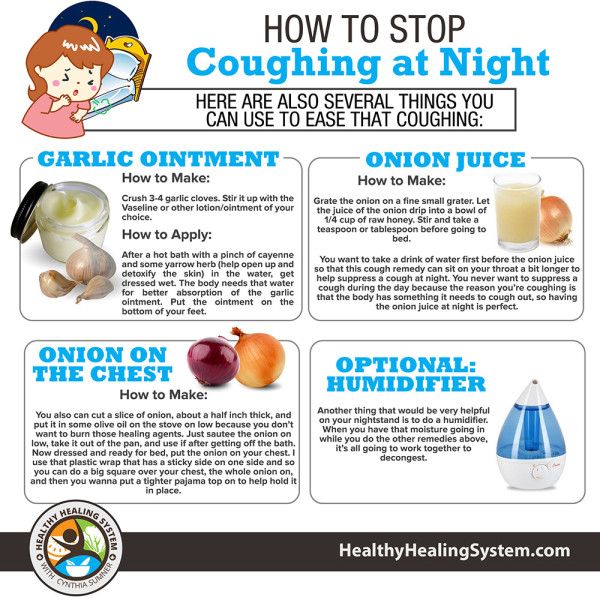 You will survive several of these nights without consequences, but a prolonged dry or wet night cough will sooner or later lead to chronic brain fatigue with subsequent dysfunction of its various areas. What to do if a night cough interferes with normal life?
You will survive several of these nights without consequences, but a prolonged dry or wet night cough will sooner or later lead to chronic brain fatigue with subsequent dysfunction of its various areas. What to do if a night cough interferes with normal life?
HOW TO ELIMINATE A NIGHT COUGH AND RELIEF A ATTRACTION?
Soothing a nocturnal cough in a child or adult is not an easy task, but it is quite doable. By following the recommendations listed below, you will significantly improve not only the quality of sleep, but also recovery from an illness accompanied by a cough.
-
Take care of full nasal breathing. A stuffy nose makes you breathe through your mouth, which leads to drying of the mucous membrane of the throat, itching and ... a coughing fit is repeated again and again, as the body tries to moisten the airways in this way, pushing the mucus out of the bronchi.
-
Lower the room temperature.
 If your comfortable bedroom temperature is 22 degrees, lower it to 20. The lower the temperature, the higher the humidity and the easier it is for you to breathe. But do not get carried away: an excessive decrease in degrees will have the opposite effect, and the cough will begin already due to spasms when inhaling cold air. Do not forget: during colds, bronchitis and other ailments, the mucous membranes are very sensitive - use your own well-being as an indicator, and not just a thermometer.
If your comfortable bedroom temperature is 22 degrees, lower it to 20. The lower the temperature, the higher the humidity and the easier it is for you to breathe. But do not get carried away: an excessive decrease in degrees will have the opposite effect, and the cough will begin already due to spasms when inhaling cold air. Do not forget: during colds, bronchitis and other ailments, the mucous membranes are very sensitive - use your own well-being as an indicator, and not just a thermometer. -
Keep your feet warm. Feet and bronchi are far apart, but still within the same circulatory system. The warmer the legs, the greater the flow of blood to them and, as a result, its outflow from the upper respiratory tract. This will help calm the cough by relieving swelling of the mucous membranes and making it more efficient to clear mucus from the bronchi.
-
Drink plenty of water.
 It is generally accepted that the consumption of large amounts of fluid makes sense only in viral diseases that are accompanied by an increase in body temperature. But with a wet night cough, drinking plenty of water helps no less: compotes and tea that you drink during the day reduce the viscosity of not only blood, but also other fluids, including mucus, which your bronchi try to push out during coughing fits. Make it easy for them: don't forget to drink more.
It is generally accepted that the consumption of large amounts of fluid makes sense only in viral diseases that are accompanied by an increase in body temperature. But with a wet night cough, drinking plenty of water helps no less: compotes and tea that you drink during the day reduce the viscosity of not only blood, but also other fluids, including mucus, which your bronchi try to push out during coughing fits. Make it easy for them: don't forget to drink more. -
Do not eat at night. A full stomach is one of the night cough provocateurs even in a healthy person. Moreover, a late dinner can worsen the condition with bronchitis. Make sure that the last meal is no later than 2 hours before you take a horizontal position and the likelihood that a night cough will interfere with sleep will be much less.
You may also be interested in:
The syrup has a complex action: it removes phlegm, clears the bronchi and relieves inflammation.