Signs of cradle cap in babies
Cradle Cap
Is this your child's symptom?
- A scaly rash on the scalp that starts in newborns
Symptoms of Cradle Cap
- Yellow scales and crusts attached to the scalp
- Occurs in patches
- Scales can be greasy or dry
- Not itchy or painful
- Begins in the first 2 to 6 weeks of life
Cause of Cradle Cap
- Cradle cap is probably caused by hormones from the mother. These hormones cross the placenta before birth. The hormones cause the oil glands in the skin to become overactive. They then release more oil than normal.
- Dead skin cells normally fall off. The extra oil causes these cells to "stick" to the skin. These cells form yellow crusts and scales on the scalp.
When to Call for Cradle Cap
Call Doctor or Seek Care Now
- Baby less than 1 month old with tiny water blisters or pimples in a cluster
- Your child looks or acts very sick
Contact Doctor Within 24 Hours
- Baby less than 1 month old with any water blisters or pimples
- You think your child needs to be seen
Contact Doctor During Office Hours
- Raw rash behind the ears
- Rash spreads beyond the scalp
- Cradle cap gets worse with treatment
- Cradle cap lasts longer than 12 months
- You have other questions or concerns
Self Care at Home
- Mild cradle cap
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Cradle Cap
- What You Should Know About Cradle Cap:
- Cradle cap is a common skin condition of newborns.
- It's caused by overactive oil glands in the scalp.
- It's harmless and will go away on its own. But it takes time.
- Here is some care advice that should help.
- Shampoo Daily:
- Wash the hair with an anti-dandruff shampoo (such as Head and Shoulders).
 Do this twice a week. No prescription is needed. Note: The daily use of anti-dandruff shampoo isn't approved until after 2 years old. But, using it twice a week is fine.
Do this twice a week. No prescription is needed. Note: The daily use of anti-dandruff shampoo isn't approved until after 2 years old. But, using it twice a week is fine. - On the other days, wash the hair with baby shampoo.
- Wash the hair with an anti-dandruff shampoo (such as Head and Shoulders).
- Scalp Massage:
- While the hair is lathered, massage the scalp with a soft brush. You can also use a rough washcloth or your fingers for 5 minutes. Don't worry about hurting the soft spot.
- Baby Oil:
- If the scalp has thick crusts (scales), put some baby oil on the scalp. Do this for 15 minutes before shampooing to soften the crusts.
- Wash all the oil off, however, or it may worsen the cradle cap. (Reason: The oil blocks the oil glands on the baby's scalp.)
- Do not use olive oil. (Reason: may increase the growth of yeast)
- Cradle cap lotions for loosening up the scales are also available without a prescription. Apply the lotion 15 minutes before shampooing.
- Steroid Cream:
- If the rash on the scalp is red and irritated, use 1% hydrocortisone cream.
 An example is Cortaid. No prescription is needed.
An example is Cortaid. No prescription is needed. - Put this on once a day.
- After 1 hour, wash it off with soap and water.
- Do this for 7 days or less.
- If the rash on the scalp is red and irritated, use 1% hydrocortisone cream.
- Expected Course:
- Cradle cap will eventually go away on its own between 6 and 12 months of age. Usually, it doesn't cause any symptoms (such as pain or itching).
- Therefore, treatment is optional. It is mainly done for cosmetic reasons.
- Shampoos, lotions and brushing will reduce the thickness of the scales. They will usually make them go away sooner.
- Return to Child Care:
- Cradle cap cannot be spread to others.
- Your child does not need to miss any child care.
- Call Your Doctor If:
- Gets worse with treatment
- Lasts over 12 months of age
- You think your child needs to be seen
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 10/19/2022
Last Revised: 01/13/2022
Copyright 2000-2022. Schmitt Pediatric Guidelines LLC.
Cradle cap | Pregnancy Birth and Baby
Cradle cap | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is cradle cap?
Cradle cap is the name given to the yellowish, greasy scaly patches that appear on the scalp of young babies. It is a very common, harmless condition that doesn't usually itch or cause discomfort to the baby.
Cradle cap appears most often in babies in the first 2 months and tends to last only a few weeks or months. It is uncommon in babies older than 3 months but may last up to 6 to 12 months in some babies.
It is uncommon in babies older than 3 months but may last up to 6 to 12 months in some babies.
What are the symptoms of cradle cap?
Cradle cap is recognisable by the large, greasy, yellow or brown scales that appear on your baby's scalp. These scales will eventually start to flake and may make the affected skin appear red. Sometimes the hair may also come away with the flakes. Cradle cap is not a serious condition and should not cause your child any problems or irritation. However, it is important not to scratch or pick at the cradle cap, in case an infection develops.
It usually starts on the scalp and can sometimes spread behind the ears. The patches may appear on other parts of your baby’s body, such as the nappy area (groin), the nose, armpits or backs of the knees. When it appears on a part of the body other than the scalp, it is called by its medical term seborrhoeic dermatitis.
What causes cradle cap?
The cause of cradle cap is not clear, although it may be linked to overactive sebaceous glands. These are glands in the skin that produce an oily substance called sebum.
These are glands in the skin that produce an oily substance called sebum.
It is thought that some babies keep some of their mother’s hormones in their bodies for several weeks or months after the birth. These hormones may make their glands more active, so they produce more sebum. The excess sebum causes old skin cells to stick to the scalp, instead of drying up and falling off as they would normally do.
Cradle cap is not contagious and is not caused by a lack of cleanliness. If a baby has cradle cap, it does not mean that the child has an infection or is not being looked after properly. Research has found that babies who get cradle cap often have family members with allergy-type conditions, such as asthma and eczema. A small number of babies who have cradle cap may develop other types of seborrhoeic dermatitis, such as dandruff, when they are older.
How is cradle cap treated?
Cradle cap requires no specific treatment and will clear up on its own with time. But if you’re unsure at any stage, visit a doctor who can help with the diagnosis and reassure you.
If you want to improve cradle cap faster, massage a small amount of baby oil or olive oil into the scalp at night to soften the patchy scales. In the morning, using a soft baby brush or cloth, gently remove any loose particles, and then wash the hair with a baby shampoo.
In time, the crusts will soften and should lift off easily with a cotton bud or soft baby toothbrush.
Shampoos that contain ground nut oil or peanut oil are best avoided in children under 5 years old.
Taking care with shampoos
Shampoos are available over the counter at pharmacies to loosen cradle cap. Check the patient information leaflet before you use these for any ingredients your child is allergic to, and follow the instructions carefully. You should avoid getting any in your baby’s eyes as these shampoos are stronger than baby shampoo. Speak to your pharmacist for advice. If the shampoo or other treatments worsen the condition, stop the treatments and see a doctor as your baby may have eczema.
Shampoos that contain ground nut oil or peanut oil are best avoided in children under 5 years old.
When should I see my doctor?
If the cradle cap becomes inflamed or infected, a course of antibiotics or an antifungal cream or shampoo, such as ketoconazole, may be prescribed by a doctor. A mild steroid cream such as hydrocortisone may be recommended for an inflamed rash.
It’s a good idea to see the doctor if:
- cradle cap continues after your baby is 3 months or is itchy to your baby, as this may be a sign of eczema and will need to be treated differently
- the cradle cap does not improve with treatment or your baby has signs of cradle cap on the face or body (seborrhoeic dermatitis)
- the skin under crusts becomes inflamed – this can be a sign of infection and will need different treatment
- you’re not sure it is cradle cap
Sources:
Royal Children’s Hospital Melbourne (Cradle cap), Raising Children Network (Cradle cap), The Australasian College of Dermatologists (Seborrhoeic Dermatitis and Cradle Cap)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- About the fontanelle
Need more information?
Cradle cap: symptoms, causes and self-care - MyDr.com.au
Cradle cap usually gets better on its own, within a few weeks of appearing.There are several things you can do at home (self-care) to try to improve cradle cap and treatments are available from your doctor.
Read more on myDr website
Cradle cap treatment: babies | Raising Children Network
Cradle cap is the oily, scaly crust that babies get on scalps and torsos and in body folds. It usually doesn’t need treatment and goes away by itself.
Read more on raisingchildren.net.au website
ACD A-Z of Skin - Seborrhoeic Dermatitis and Cradle Cap
A-Z OF SKIN Seborrhoeic Dermatitis and Cradle Cap BACK TO A-Z SEARCH What is it? Seborrhoeic dermatitis is inflammation of the skin that usually occurs on areas of the body such as the head and trunk where there are a greater number of oil glands
Read more on Australasian College of Dermatologists website
Dandruff in children and teenagers | Raising Children Network
Dandruff is common and normal in children and teens. You can usually treat it with anti-dandruff shampoo. Read more about dandruff treatment and causes.
You can usually treat it with anti-dandruff shampoo. Read more about dandruff treatment and causes.
Read more on raisingchildren.net.au website
Nappy rash - MyDr.com.au
Nappy rash can result from contact dermatitis, or from a fungal thrush infection. Find out how to manage this condition and when you should see your doctor.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Death in the cradle. Which children are threatened by sudden death syndrome | Child health | Health
Anna Shatokhina
Estimated reading time: 6 minutes
53573
Shutterstock. com
com
A tragic phenomenon in medicine, a mystery without an answer - this is how the syndrome of sudden infant death is often called. And indeed, such an extremely mysterious and inexplicable phenomenon began to manifest itself more and more often. In essence, this is the death of a child under the age of 1 year without any signs of illness and abnormalities at the autopsy. The baby simply dies for no apparent reason, unexpectedly and quietly. What is such a syndrome, why it can develop and how to deal with it - in the material of AiF.ru.
Risk group
Sudden infant death syndrome is not clearly defined. The death of a child is often described as unexplained. At the same time, both on the body of the crumbs and in the house, there are no direct or indirect factors that could serve as a catalyst - neither infections, nor bacteria, nor genetic abnormalities, nor other pathological problems. Doctors still cannot explain why such a problem develops. However, a number of studies on this topic have led to some conclusions. So, for example, according to statistics, most often SIDS occurs in children under the age of 8 months, with the largest number of cases recorded at the age of 2-4 months. Of the total number of dead children, 60% are boys. As for time, the death of babies is celebrated at night - from midnight to 6 in the morning.
However, a number of studies on this topic have led to some conclusions. So, for example, according to statistics, most often SIDS occurs in children under the age of 8 months, with the largest number of cases recorded at the age of 2-4 months. Of the total number of dead children, 60% are boys. As for time, the death of babies is celebrated at night - from midnight to 6 in the morning.
We study the causes
There are no main and clear reasons for the development of SIDS. However, some doctors suspect that the imperfect work of the brain becomes a catalyst, when literally second failures occur in it, which can quickly unbalance the body of the crumbs. Others are sure that the leading role in the development of such a pathology belongs to heart rhythm failures - children who have a prolonged QT interval on the ECG are susceptible to it. In addition, there is a theory according to which ARDS develops due to the fact that the position of a sleeping child on the stomach with the head turned to the side causes compression of the spinal artery, which causes hypoxia and apnea.
Today, doctors single out only concomitant factors that can provoke a corresponding reaction. Among them:
- Sleeping on the stomach (this factor is often called the main one)
- Overwrapping
- Too soft mattress and pillows
- The presence of causeless respiratory arrest, incl. if such a situation was noted among the brothers and sisters of the child
- The age of the mother is under 20, when she is single and was not registered with a doctor
- Maternal illness during pregnancy
- Small gap between pregnancies (less than a year)
- Difficult delivery
- Prematurity
- Artificial feeding
- Sleeping in different rooms with parents
Sleep apnea was also common in these children. At the same time, it should be understood that in an absolutely healthy baby, short pauses of 12-15 seconds can occur in the first year, and this is a variant of the norm. If such pauses in breathing take 20 seconds or more and are accompanied by pallor of the skin, lethargy, decreased muscle tone, then they speak of a full-fledged and life-threatening sleep apnea.
Why morning?
Sudden infant death most often occurs early in the morning. And this is quite understandable, because. in any person - be it an adult or a baby - a section of the nervous system, which is called parasympathetic, is activated at night - it is responsible for lowering the frequency of breathing and heart rate. Also in the morning, the level of glucocorticoids in the blood decreases, which also causes a decrease in the reserve capacity of the body.
If parents have time to notice the baby's breathing stops during sleep, the situation can be corrected. First of all, the respiratory center should be stimulated. It is necessary to take the child in your arms and stir him up - you should not be afraid to wake him up in such a situation, the main thing here is to save his life. After the breath has appeared, it is worth gently massaging the arms, legs, feet and earlobes. It is also advised to vigorously run your finger along the spine.
If the baby does not wake up and breathing is not restored, it is necessary to start the resuscitation procedure and call for emergency help.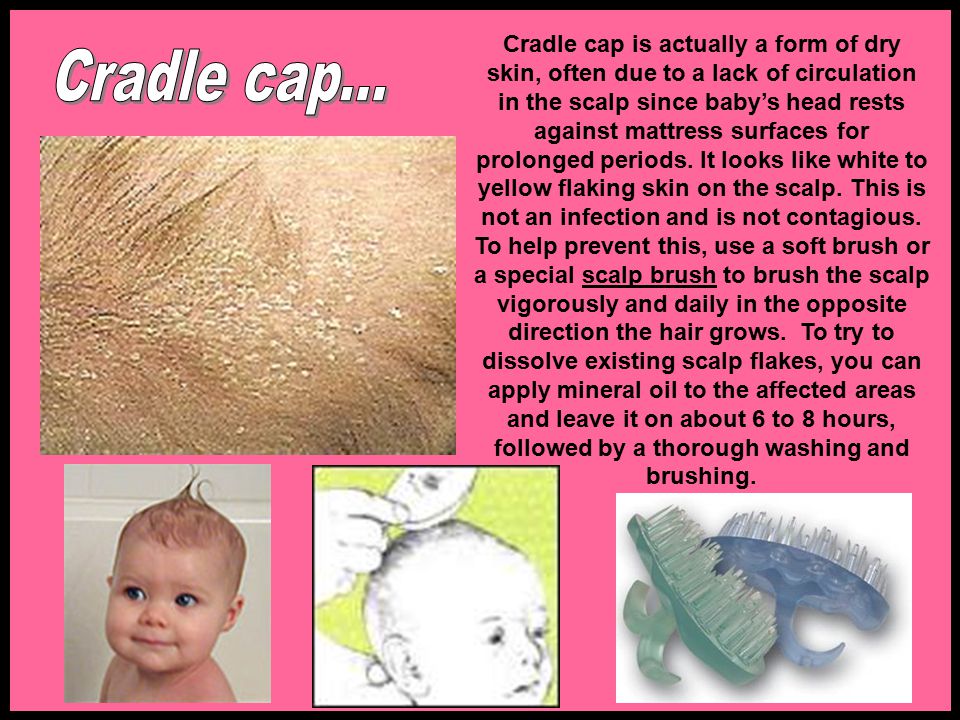
Rules for prevention
The main danger of sudden infant death syndrome lies precisely in its suddenness - it is impossible to predict it. At the same time, doctors have identified those measures that can act as preventive measures. So, for example, you should ensure that the baby sleep on his back - today there are many devices for this that securely fix the baby and prevent it from rolling over. You will also have to exclude soft bedding sets. An excellent solution would be a hard mattress and a sleeping bag - it will perform the function of a blanket, while not covering the child completely. There should not be any soft toys in the bed either. Despite the fact that one of the risk factors is separate sleep with parents, it is still not worth making a choice in favor of joint sleep. Ideally, if the baby will sleep in his own crib or cradle next to the parent's bed.
Dress your baby properly before going to bed – don't choose too warm clothes, and the temperature in the room should not exceed 20 degrees. If there was feeding before going to bed, you must definitely wait for the baby to burp.
If there was feeding before going to bed, you must definitely wait for the baby to burp.
Particular attention should be paid to the child in the following situations:
- High fever, especially during sleep
- Refusal to eat
- Decreased locomotor activity
- Presence of a respiratory infection
- Sleep of a baby after a long tantrum and crying
- Sleep in new conditions (e.g. away)
It is worth being fully prepared and carefully monitor your baby, then there is an opportunity to prevent the development of ADHD and save the baby's life.
sudden death syndrome child health
Next article
The most interesting in social networks
Media news2
Found anomaly leading to Sudden Infant Death Syndrome
Sudden Infant Death Syndrome has become more understandable to scientists. In some cases, anomalies in the development of the brain are to blame, which prevent the baby from rolling over in time and not suffocating in his sleep.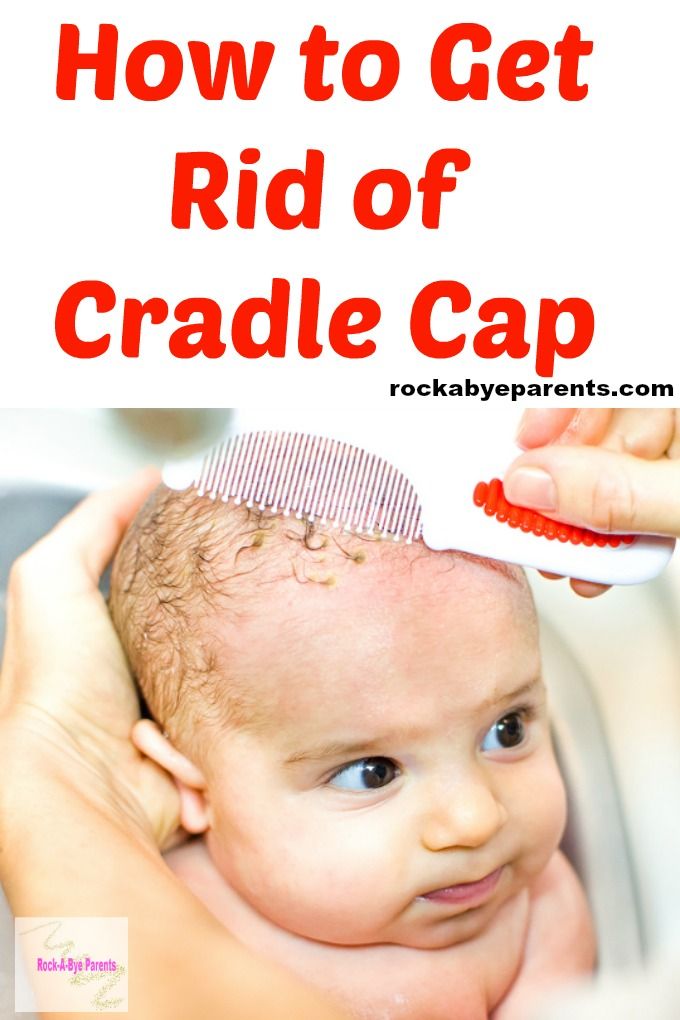
An international team of scientists led by researchers from the University of Adelaide (Australia) has come close to understanding the causes of unexplained infant deaths, one of the most complex mysteries of modern medicine.
Every year, thousands of outwardly healthy children die in the world due to the so-called sudden infant death syndrome (SIDS), for example, 3.5 thousand babies die in the USA alone. In another way, this syndrome is also called death in the cradle. SIDS was included in the International Classification of Diseases at 1975, and began to study it 15 years before.
Researchers note factors correlated with the syndrome: sleeping on the stomach, bed that is too soft, poor maternal health and difficult delivery, intrauterine developmental problems. Children under six months of age are most at risk, they account for 90% of all cases.
It is known that death occurs from respiratory arrest, but the exact causes of infant death have not yet been established.
In a study published in the journal PLOS ONE , scientists led by Fiona Bright of the University of Adelaide have isolated brain malformations in infants — especially premature babies and boys — that for the first time have been directly linked to sudden infant deaths.
"One of the reasons why SIDS cases can be so scary for parents is that death often occurs without any early warning," Bright explained.
Scientists used samples of the medulla oblongata of 76 infants who died before the age of one year. 55 babies died from SIDS, the rest from chronic and sudden onset diseases or hypoxia.
Using the method of autoradiography, scientists found that in children who died from SIDS, the mechanism of binding substance P to the NK1R receptor was impaired. Substance P is a neuropeptide found in the brain and spinal cord, part of the nervous system, thyroid gland, skin and muscles. It affects, in particular, the expansion of blood vessels, causes contraction of smooth muscles and is responsible for the transmission of pain impulses to the central nervous system.
For example, the skin cells of a naked mole rat are deprived of substance P, so the animals do not feel cuts and burns (however, after an injection of a neuropeptide, pain sensations appear). At the same time, no such violations were found in the rest of the children.
Scientists believe that these developmental anomalies in areas of the brain that control head and neck movements, breathing, heartbeat, and the body's response to lack of oxygen may be the reason
that sleeping on your stomach is a risk factor for SIDS.
“Despite the fact that the true cause of SIDS has not yet been determined, many studies have indicated that in some cases children were not completely healthy before death. These children seem to have some kind of internal vulnerability that puts them at increased risk, Bright explains. -
We have now found significant abnormalities in key areas of the brainstem in children, especially in those areas that control breathing and head and neck movements. This anomaly is directly related to cases of SIDS. Substance P and NK1R neuroreceptors play a critical role in the brain's control of the respiratory system, the circulatory system, and the body's response to hypoxia - that is, lack of oxygen at the cellular level," Bright explained.
This anomaly is directly related to cases of SIDS. Substance P and NK1R neuroreceptors play a critical role in the brain's control of the respiratory system, the circulatory system, and the body's response to hypoxia - that is, lack of oxygen at the cellular level," Bright explained.
In other words, the brain of an infant with such a deviation is not always able to create a motor response to life-threatening moments,
occurring during sleep, such as when a pillow or blanket covers a child's airway.
“And even though these children may otherwise appear to be completely healthy, their brains and bodies are not capable of responding properly when the child is somehow deprived of oxygen,” Bright says.
According to co-author Roger Byard, this discovery explains why it is dangerous for children to sleep on their stomachs. “It has been known for many years that babies who sleep on their stomachs have a higher risk of sudden death – and now we understand much better why this is so,” says Byard.