Internal bleeding from ectopic pregnancy
Ectopic pregnancy | Pregnancy Birth and Baby
Ectopic pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
An ectopic pregnancy is when a fertilised egg implants itself outside the womb, usually in one of the fallopian tubes. This means the embryo will not be able develop into a baby as the fallopian tube is not large enough to support the growing embryo.
In a few cases an ectopic pregnancy causes no noticeable symptoms and is only detected during routine pregnancy testing. However, most women do have symptoms and these usually become apparent between week 4 and week 12 of pregnancy.
Early diagnosis and treatment is important to prevent life-threatening bleeding and also, if possible, so the tube can be saved and it can continue to work.
Symptoms of ectopic pregnancy
If you have an ectopic pregnancy, you might experience:
One-sided abdominal pain — typically on one side of your abdomen (tummy), which can be persistent and severe.
Vaginal bleeding — vaginal bleeding is a different type of bleeding from your regular period. It often starts and stops, and can be bright or dark red in colour. Some women mistake this bleeding for a regular period and do not realise they are pregnant.
Shoulder tip pain — shoulder tip pain is felt where your shoulder ends and your arm begins. It is not known exactly why shoulder tip pain occurs, but it usually occurs when you are lying down and is a sign that the ectopic pregnancy is causing internal bleeding. The bleeding is thought to irritate the phrenic nerve, which is found in your diaphragm (the muscle used during breathing that separates your chest cavity from your abdomen). The irritation to the phrenic nerve causes referred pain (pain that is felt elsewhere) in the shoulder blade.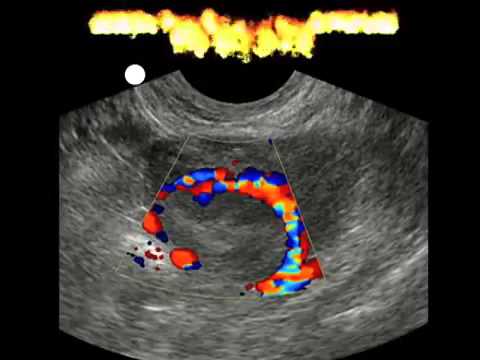
Bowel pain — you may experience pain when passing urine or stools.
Diarrhoea and vomiting — an ectopic pregnancy can cause similar symptoms to a gastrointestinal disease and is often associated with diarrhoea and vomiting.
How is ectopic pregnancy diagnosed?
It can be difficult to diagnose an ectopic pregnancy from the symptoms alone, as they can be similar to other conditions.
Some of the tests used to diagnose an ectopic pregnancy include:
- vaginal ultrasound
- blood tests
- keyhole surgery
How is an ectopic pregnancy treated?
If an ectopic pregnancy is detected at an early stage, a medication called methotrexate is sometimes needed to stop the egg developing. The pregnancy tissue is then absorbed into the woman's body.
Methotrexate is not always needed, as in around half of cases the egg dies before it can grow larger.
Ectopic pregnancies detected at a more advanced stage will require surgery to remove the pregnancy sac.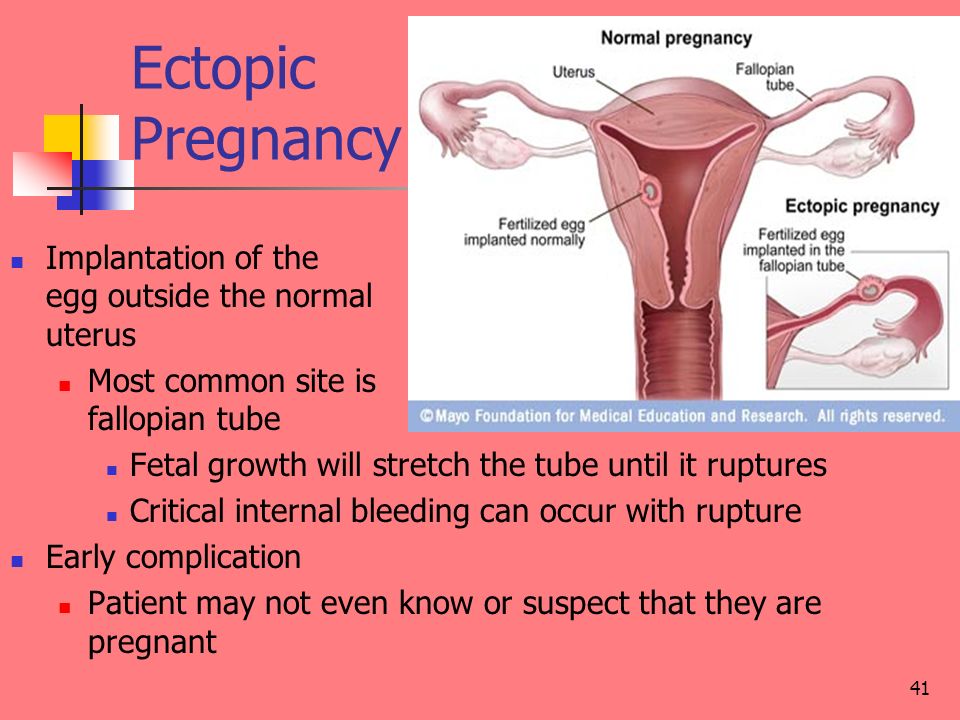
If an ectopic pregnancy is left to develop, there is a risk that the fertilised egg could continue to grow and cause the fallopian tube to split open (rupture), which can cause life-threatening internal bleeding.
Signs of a ruptured fallopian tube are:
- sudden, severe, sharp pain
- feeling faint and dizzy
- feeling nauseous or vomiting
- diarrhoea
- shoulder tip pain
A ruptured fallopian tube is a medical emergency. If you think that you or someone in your care has experienced this complication, call 000 and ask for an ambulance.
Why does an ectopic pregnancy happen?
In a normal pregnancy an egg is fertilised by sperm in one of the fallopian tubes, which connect the ovaries to the womb. The fertilised egg then moves into the womb and implants itself into the womb lining (endometrium), where it grows and develops.
An ectopic pregnancy occurs when a fertilised egg implants itself outside the womb. It most commonly occurs in a fallopian tube (this is known as a tubal pregnancy), often as the result of damage to the fallopian tube or the tube not working properly.
It most commonly occurs in a fallopian tube (this is known as a tubal pregnancy), often as the result of damage to the fallopian tube or the tube not working properly.
Less commonly (in around 2 in 100 cases), an ectopic pregnancy can occur in an ovary, in the abdominal space or in the cervix (neck of the womb).
In many cases, it's not clear why a woman has an ectopic pregnancy. Sometimes it happens when there's a problem with the fallopian tubes, such as them being narrow or blocked.
The following are all associated with an increased risk of ectopic pregnancy:
- pelvic inflammatory disease (PID) — an infection of the female reproductive system, typically caused by chlamydia
- smoking
- having a previous history of ectopic pregnancies
- previous surgery on your fallopian tubes — such as an unsuccessful female sterilisation procedure, or other surgery in your pelvis or abdomen
- fertility treatment, such as IVF — taking medication to stimulate ovulation (the release of an egg) can increase the risk of ectopic pregnancy
- becoming pregnant while using an intrauterine device (IUD) or intrauterine system (IUS) for contraception — it's rare to get pregnant while using these, but if you do you're more likely to have an ectopic pregnancy
- becoming pregnant while using the mini (progesterone-only) pill
- having endometriosis
- increasing age — the risk is highest for pregnant women who are aged 35-40
In around half of all cases, there are no obvious risk factors.
Support
The loss of your pregnancy at any stage can have a huge impact on you and your partner. One day you are pregnant and planning your future life with your child, and then within a short time, your pregnancy ends. The ending of an ectopic pregnancy is a form of miscarriage – and the feelings that a woman and her partner may experience can be similarly difficult.
It is not uncommon for feelings of grief and bereavement to last for 6 to 12 months, although these feelings usually improve with time.
Pregnancy, Birth and Baby offers free and confidential support and counselling to women, their partners, friends and relatives. Call on 1800 882 436.
Many women affected by a miscarriage benefit from counselling. SANDS (miscarriage, stillborn and neonatal death support) provide support groups for parents and their family whose baby has died through stillbirth, miscarriage, ectopic pregnancy and medically advised termination.
Information on SANDS groups in Australian states can be obtained from the SANDS Australia website.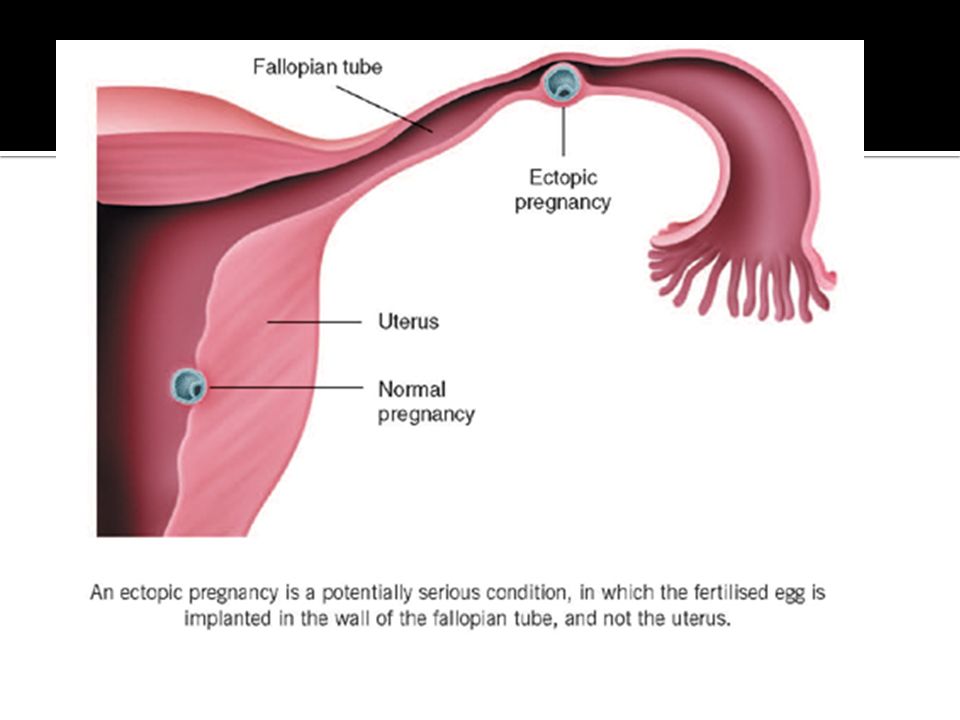
Trying for another pregnancy
It is normally recommended that you wait for at least 2 menstrual cycles before trying for another pregnancy, as this will allow time for your fallopian tubes to recover (if treated with methotrexate, you will need to wait at least 3 to 4 months). However, many women are not emotionally ready to try for another pregnancy so soon.
Your chances of having a successful pregnancy will depend on the underlying health of your fallopian tubes.
If you cannot conceive in the normal way then fertility treatment such as in-vitro fertilisation (IVF) may be an option.
IVF treatment is where an egg is fertilised by a sperm outside the womb (usually in a test tube) and, after fertilisation, the embryo is surgically implanted into the womb.
Sources:
Healthy WA (Ectopic pregnancy), The Royal Women's Hospital (Ectopic pregnancy), National Institute for Health and Clinical Excellence (Ectopic pregnancy and miscarriage)Learn more here about the development and quality assurance of healthdirect content.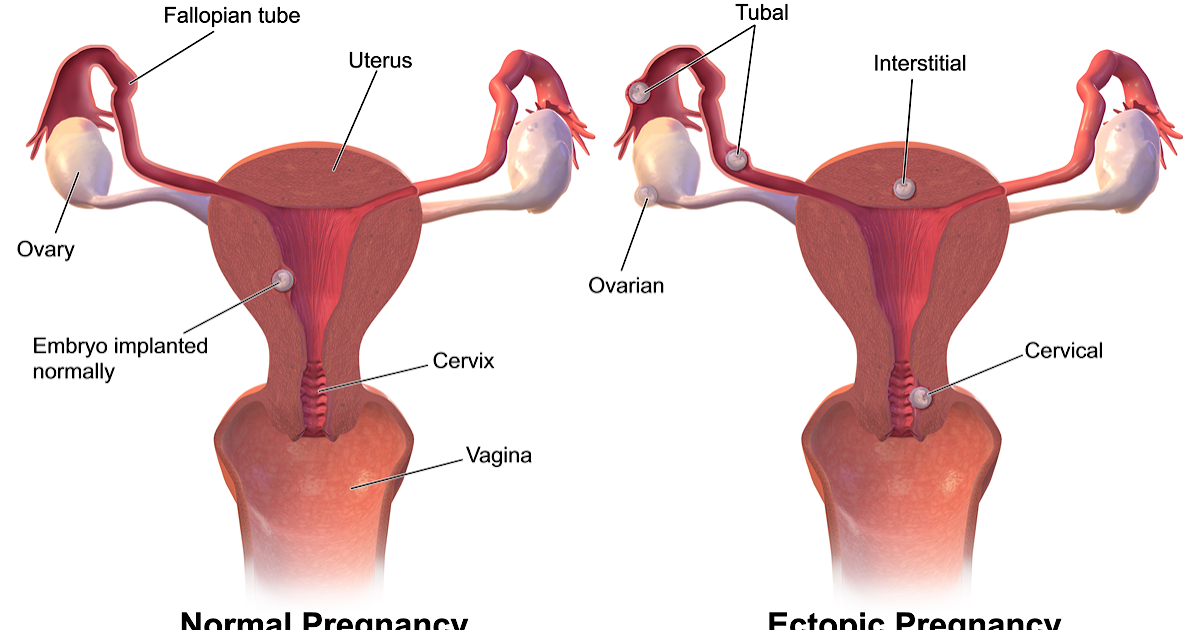
Last reviewed: April 2020
Back To Top
Related pages
- Pregnancy loss
- Experiencing a pregnancy loss
Need more information?
Ectopic pregnancy
An ectopic pregnancy occurs when a fertilised egg implants outside the uterus (womb)
Read more on WA Health website
What is Ectopic Pregnancy? | Ectopic Pregnancy Symptoms | How do I know if I have had an Ectopic Pregnancy? | Ectopic Pregnancy Treatment - Sexual Health Victoria
Ectopic pregnancy is a pregnancy that develops outside the uterus, usually in one of the fallopian tubes. In almost all cases, the embryo dies.
Read more on Sexual Health Victoria website
Pregnancy loss
Unfortunately not all pregnancies are successful. Find out more on miscarriage, ectopic pregnancy, molar pregnancy and stillbirth and neonatal birth.
Find out more on miscarriage, ectopic pregnancy, molar pregnancy and stillbirth and neonatal birth.
Read more on Pregnancy, Birth & Baby website
The Pink Elephants Support Network - What is Miscarriage?
The vast majority of miscarriages will happen in the first 12 weeks of pregnancy, with some even happening before you knew you would have known you were pregnant
Read more on Pink Elephants Support Network website
Reasons for Miscarriage | Red Nose Australia
Read more on Red Nose website
Bleeding or pain in early pregnancy
One in 4 women will experience bleeding and/or pain during their first 12 weeks of pregnancy.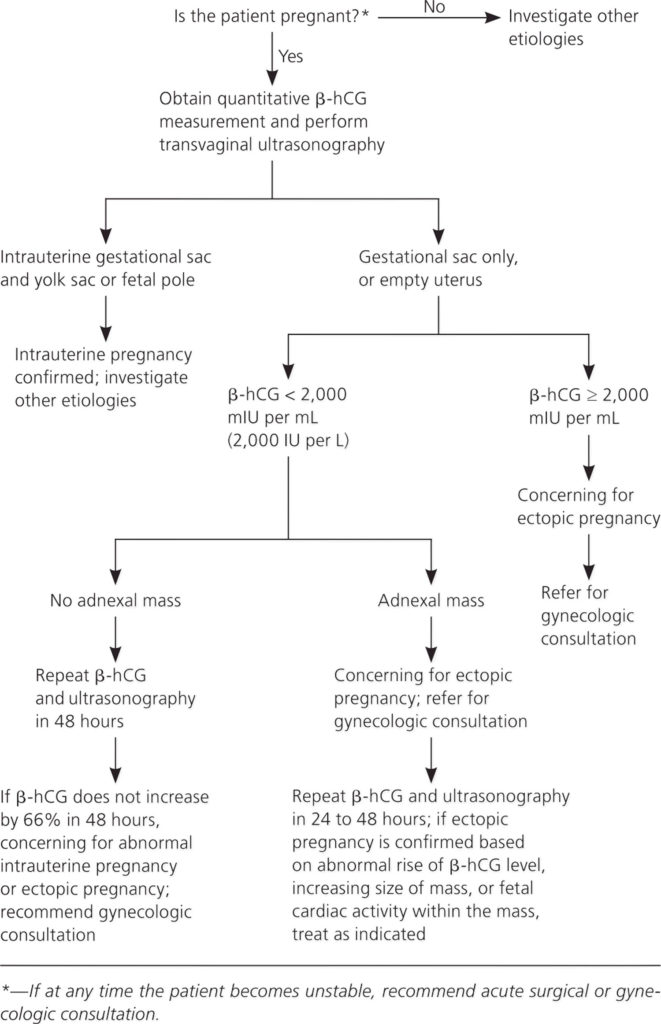 Unfortunately half of these pregnancies may also end in miscarriage, which cannot be prevented.
Unfortunately half of these pregnancies may also end in miscarriage, which cannot be prevented.
Read more on WA Health website
Miscarriage
Miscarriage Despite being common and widespread, miscarriage can be a heartbreaking experience – with up to one in five pregnancies ending before week 20
Read more on Gidget Foundation Australia website
Permanent Contraception: Female Sterilisation | Family Planning NSW
Female sterilisation is a permanent form of contraception. It's a surgical procedure to block the fallopian tubes that carry the egg to the uterus.
Read more on Family Planning NSW website
Pregnancy Options - Sexual Health Victoria
Sexual Health Victoria (formally Family Planning Victoria) focuses on reproductive and sexual health care, education and advocacy. Our vision is to improve ever
Our vision is to improve ever
Read more on Sexual Health Victoria website
Pregnancy Options - Sexual Health Victoria
Sexual Health Victoria (formally Family Planning Victoria) focuses on reproductive and sexual health care, education and advocacy. Our vision is to improve ever
Read more on Sexual Health Victoria website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.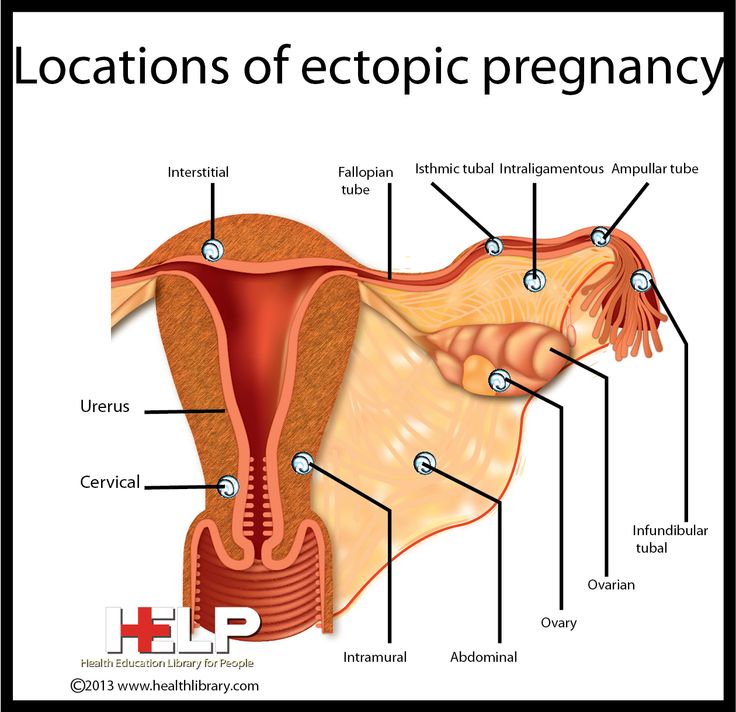
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Case Report: Non-operative treatment of ruptured ectopic pregnancy
- Journal List
- BMJ Case Rep
- PMC4932335
BMJ Case Rep.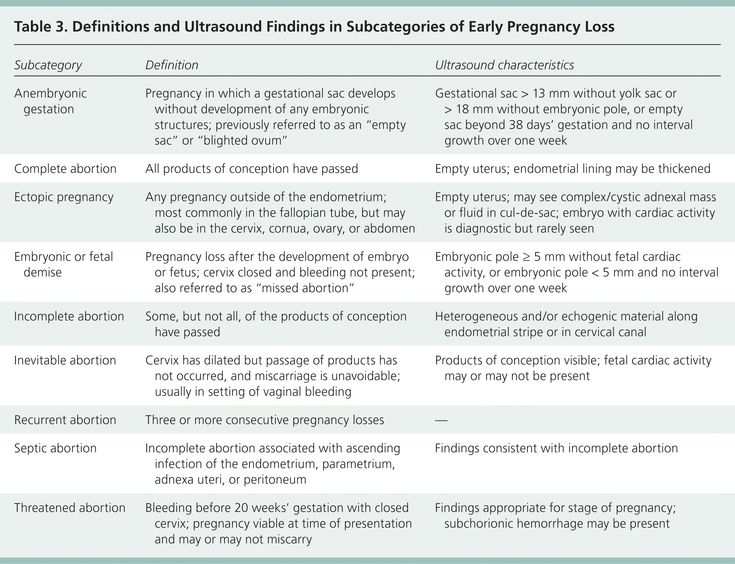 2016; 2016: bcr2016215311.
2016; 2016: bcr2016215311.
Published online 2016 Jun 13. doi: 10.1136/bcr-2016-215311
Case Report
Author information Article notes Copyright and License information Disclaimer
Ruptured ectopic pregnancy often causes abdominal pain, vaginal bleeding and internal haemorrhage; it is a very serious condition and can be life-threatening. Patients with a ruptured ectopic pregnancy are normally treated by surgical intervention. We describe a case of a 20-year-old woman who presented with abdominal pain and vaginal bleeding. Urine human chorionic gonadotropin was positive and on examination she had localised tenderness of the abdomen. Transvaginal ultrasonography revealed a ruptured tubal pregnancy along with blood in the abdomen. The patient was closely monitored and treated conservatively, with a successful outcome. She recovered uneventfully. Our case shows that non-operative treatment of a ruptured ectopic pregnancy may be a possible non-invasive treatment option in highly selected patients.
Ectopic pregnancy occurs in 1.3–2.4% of all pregnancies and is one of the most common causes of first trimester complications.1–4 Ectopic pregnancy is considered to be a gynaecological emergency, and can be life-threatening.1–4 It accounts for up to 6% of all pregnancy-associated deaths.24 The incidence of ectopic pregnancies that rupture is around 18%, and presumably rises with increasing gestational age.14 The majority of patients present at week 4–8 of gestation.14
The typical symptoms of a ruptured ectopic pregnancy are vaginal bleeding and abdominal pain. Hence, ectopic pregnancy should be suspected when a woman presents with vaginal bleeding and abdominal pain, and a positive pregnancy test.
The internal haemorrhage that occurs due to rupture of an ectopic pregnancy may be life-threatening.1 Surgery is considered to be the gold standard of treatment for ruptured ectopic pregnancy. 2 In this case, we present a woman with a ruptured ectopic pregnancy who was treated successfully using non-operative measures.
2 In this case, we present a woman with a ruptured ectopic pregnancy who was treated successfully using non-operative measures.
A 20-year-old woman presented with vaginal bleeding and abdominal pain. She had no history of operative procedures. She had once been treated with antibiotics, for pelvic inflammatory disease. At presentation, there was no fever, no dysuria and no vaginal discharge. Urine human chorionic gonadotropin was positive. She had been taking oral contraceptive pills, however, not consistently. She suffered from nausea and had a 2-day history of vomiting. Otherwise, she had no subjective signs of pregnancy. She had had an episode of vaginal bleeding 2 weeks prior and menstrual bleeding the month before this as well, though her menstrual bleedings had been irregular. Gestational age was uncertain based on history, though, probably between 5 and 8 weeks.
During the day of presentation, the vaginal bleeding decreased and the patient suffered from an increase in abdominal pain.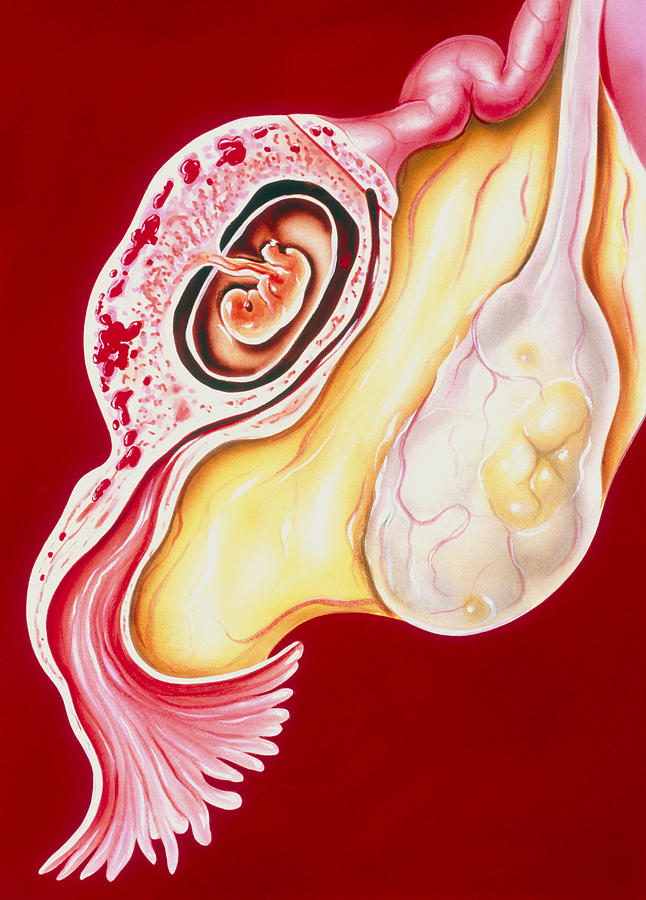 The pain was radiating towards the groin, lower back and right shoulder.
The pain was radiating towards the groin, lower back and right shoulder.
On physical examination, the patient was haemodynamically stable. The abdomen was found with localised tenderness and peritoneal irritation in the lower abdomen. Laboratory investigation showed haemoglobin of 6.9 mmol/L. Gynaecological investigation showed anteflexion of the uterus and bleeding from the uterine cavity. Transvaginal ultrasonography showed blood and haematoma in the uterine cavity. To the left of the uterus, the salpinx was surrounded by free fluid, which was consistent with blood (). The findings were consistent with a ruptured tubal ectopic pregnancy. Doppler ultrasonography revealed no ongoing bleeding. Abdominal ultrasonography showed blood in the peritoneal cavity, but no free fluid could be detected in Morisson's pouch between the liver and right kidney.
Open in a separate window
Ruptured left tubal ectopic pregnancy with free fluid consistent with blood.
The patient was monitored carefully.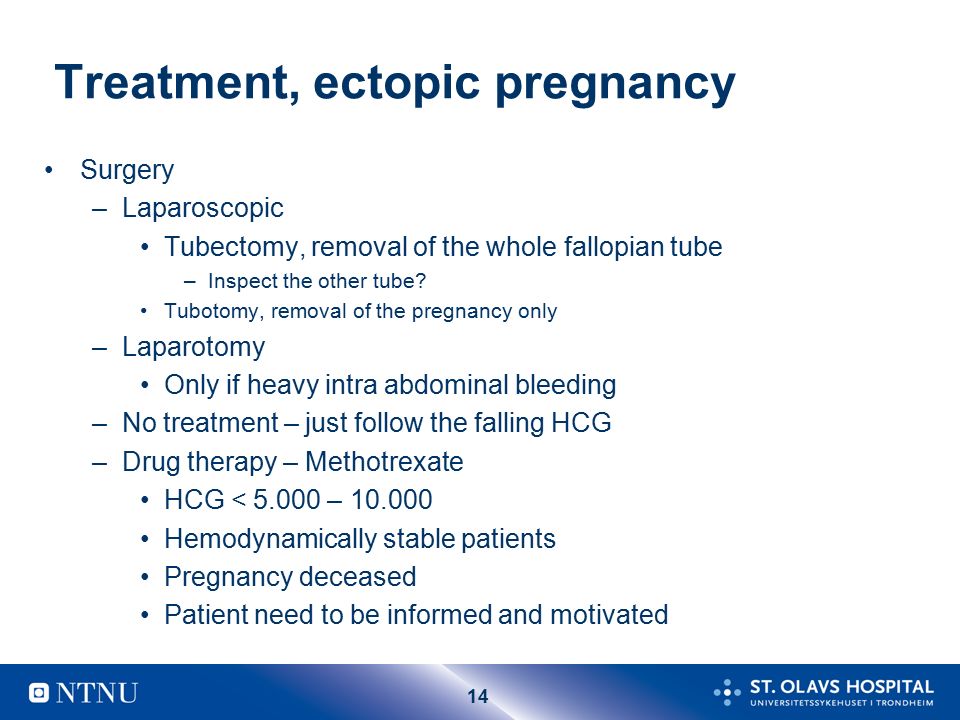 Vital signs including blood pressure, heart rate, respiratory rate and body temperature were recorded regularly. The patient remained haemodynamically stable. Laboratory investigations were repeated, showing stable haemoglobin levels.
Vital signs including blood pressure, heart rate, respiratory rate and body temperature were recorded regularly. The patient remained haemodynamically stable. Laboratory investigations were repeated, showing stable haemoglobin levels.
A miscarriage can also present with vaginal bleeding and lower abdominal pain. Hence miscarriage was considered a differential diagnosis.
Tubal abortion, that is, the embryo being expelled by the fallopian tube before rupture occurs, can be considered in the differential diagnosis. Tubal abortion may cause pain and bleeding.
The patient was treated non-operatively. She received nil per mouth, and was observed closely with monitoring of blood pressure, pulse, respiratory rate, body temperature, haemoglobin levels and symptoms of ongoing bleeding (dizziness, loss of consciousness). Moreover, she was treated with intravenous liquid therapy, to compensate for the hypovolemia that had occurred while she was bleeding, and to administer fluid while she received nil per mouth.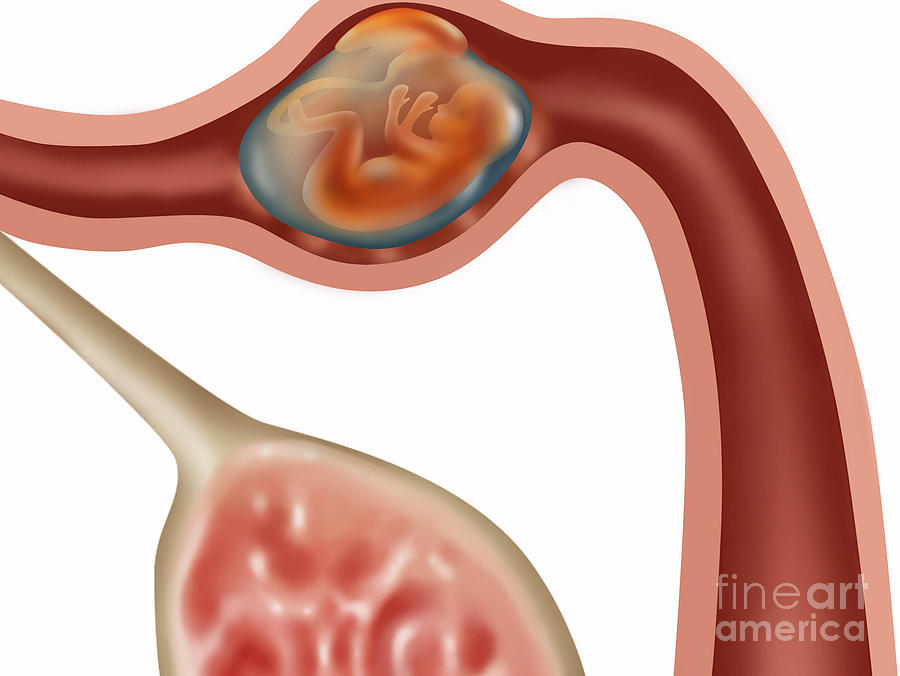 She also received intravenous tranexamic acid at a dose of 1 g four times daily to prevent bleeding.
She also received intravenous tranexamic acid at a dose of 1 g four times daily to prevent bleeding.
Operative treatment was considered, but since the patient was haemodynamically stable, and vaginal ultrasound including Doppler showed no ongoing bleeding, expectant management was chosen.
During admission, the vaginal bleeding and abdominal pain decreased. The patient was discharged from hospital 2 days after admission. At discharge, her haemoglobin level was 6.4 mmol/L. She continued treatment with oral tranexamic acid for a few more days. Three days after discharge, she was seen in the out-patient department. She was doing fine, and transvaginal ultrasonography showed no ongoing ectopic pregnancy; the amount of free intra-abdominal fluid had decreased considerably.
Over 50% of ectopic pregnancies are asymptomatic before tubal rupture.1 Early diagnosis of an ectopic extrauterine pregnancy is of utmost importance to reduce the number of complications, especially death. 2 Surgery is considered the gold standard for treatment of ruptured ectopic pregnancy. Non-operative treatment has become increasingly popular for treatment of traumatic intra-abdominal lesions such as of the liver, spleen and pancreas.5 We have searched the literature extensively, but been unable to find any case reports or other literature on non-operative treatment of ruptured ectopic pregnancy. Rupture in itself is considered a definite surgical indication in ectopic pregnancy.23 One study pointed out that some ectopic pregnancies undergo spontaneous resolution, but not if there was a rupture.1 Tubal rupture is usually associated with profound haemorrhage, though this case shows that expectant management with close monitoring of vital signs and haemodynamic stability may be a valuable treatment option for highly selected patients.1 Consequences of operative versus non-operative treatment on patient morbidity and mortality, as well as long-term outcome for future fertility and patient recovery in general after surgery, are unclear.
2 Surgery is considered the gold standard for treatment of ruptured ectopic pregnancy. Non-operative treatment has become increasingly popular for treatment of traumatic intra-abdominal lesions such as of the liver, spleen and pancreas.5 We have searched the literature extensively, but been unable to find any case reports or other literature on non-operative treatment of ruptured ectopic pregnancy. Rupture in itself is considered a definite surgical indication in ectopic pregnancy.23 One study pointed out that some ectopic pregnancies undergo spontaneous resolution, but not if there was a rupture.1 Tubal rupture is usually associated with profound haemorrhage, though this case shows that expectant management with close monitoring of vital signs and haemodynamic stability may be a valuable treatment option for highly selected patients.1 Consequences of operative versus non-operative treatment on patient morbidity and mortality, as well as long-term outcome for future fertility and patient recovery in general after surgery, are unclear.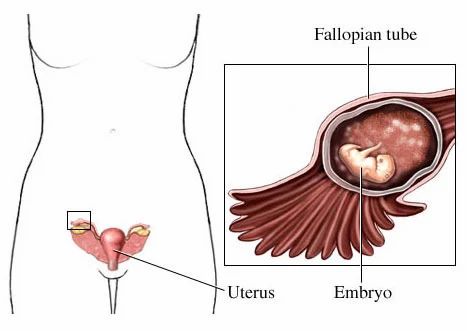 Other case reports and case studies are needed to confirm that non-operative treatment is a safe treatment option for highly selected patients with ruptured ectopic pregnancy.
Other case reports and case studies are needed to confirm that non-operative treatment is a safe treatment option for highly selected patients with ruptured ectopic pregnancy.
Learning points
Patients with established pregnancy presenting with abdominal pain, vaginal bleeding or signs of internal bleeding may have a ruptured ectopic pregnancy.
Surgical intervention is standard treatment for ruptured ectopic pregnancies.
More research is needed to clarify whether non-operative treatment of ruptured ectopic pregnancy in highly selected patients is a valuable treatment option.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
1. Taran FA, Kagan KO, Hübner M et al.. The diagnosis and treatment of ectopic pregnancy. Dtsch Arztebl Int 2015;112:693–703. 10.3238/arztebl. 2015.0693 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2015.0693 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2. Berretta R, Dall'Asta A, Merisio C. Tubal ectopic pregnancy: our experience from 2000 to 2013. Acta Biomed 2015;86:176–80. [PubMed] [Google Scholar]
3. Hajenius PJ, Mol F, Mol BW et al.. Interventions for tubal ectopic pregnancy. Cochr Database Syst Rev 2007;(1):CD000324. [PMC free article] [PubMed] [Google Scholar]
4. Babu AS, Roy J, Das D et al.. Is surgical intervention for ectopic pregnancy in a low resource set-up avoidable? J Clin Diagn Res 2014;8:OC16–19. 10.7860/JCDR/2014/8226.4815 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
5. Haugaard MV, Wettergren A, Hillingsø JG et al.. Non-operative versus operative treatment for blunt pancreatic trauma in children. Cochrane Database Syst Rev 2014;2:CD009746 10.1002/14651858.CD009746.pub2 [PubMed] [CrossRef] [Google Scholar]
Articles from BMJ Case Reports are provided here courtesy of BMJ Publishing Group
Ectopic pregnancy - American Medical Clinic
Ectopic pregnancy is a serious medical condition. This complication is very dangerous for a woman. If an ectopic pregnancy is not removed on time, there is a risk of intra-abdominal bleeding. And this, in turn, threatens the health and life of the patient. Therefore, noticing the early symptoms of an ectopic pregnancy, you should immediately see a doctor. This condition requires urgent medical attention.
This complication is very dangerous for a woman. If an ectopic pregnancy is not removed on time, there is a risk of intra-abdominal bleeding. And this, in turn, threatens the health and life of the patient. Therefore, noticing the early symptoms of an ectopic pregnancy, you should immediately see a doctor. This condition requires urgent medical attention.
The uterus is a muscular organ that exists to bear a child. However, sometimes the egg, having been fertilized, does not enter the uterine cavity, but is fixed in the ovaries, tubes or abdominal cavity. As a result, there are pains during an ectopic pregnancy and a rupture of an organ (for example, a fallopian tube) is possible.
Why does an ectopic pregnancy occur?
Causes of ectopic pregnancy may be as follows:
- pelvic inflammatory disease, especially chronic
- endometriosis
- congenital malformation of the tubes
- IVF complication
The question of why an ectopic pregnancy occurs worries many women.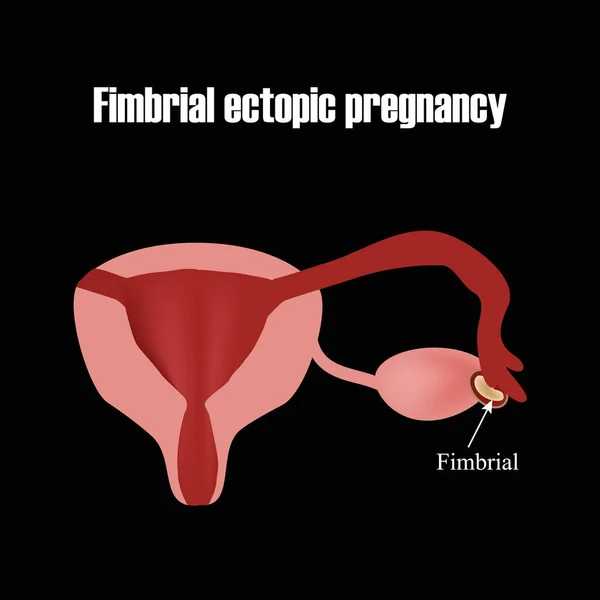 However, it is possible to establish the true causes of an ectopic pregnancy only after a laparoscopic operation to remove it.
However, it is possible to establish the true causes of an ectopic pregnancy only after a laparoscopic operation to remove it.
Symptoms of an ectopic pregnancy
Many women wonder how to distinguish an ectopic pregnancy from a normal one. Doctors recommend that you carefully monitor your condition and pay attention to the main symptoms of ectopic pregnancy:
- pain in ectopic pregnancy
- bleeding
Pain during an ectopic pregnancy is aching, cramping in nature. Painful sensations appear from the moment of attachment of the fetal egg. If a rupture occurs, bleeding begins, pain radiates to the anus, and can spread throughout the abdomen, a woman may feel pain during an ectopic pregnancy while urinating or trying to empty the intestines.
Bleeding during an ectopic pregnancy occurs in the abdominal cavity. However, due to a drop in hormone levels, uterine bleeding is often observed. The volume of allocations is usually meager. Bleeding during an ectopic pregnancy lasts a long time.
Bleeding during an ectopic pregnancy lasts a long time.
Both of these symptoms require immediate medical attention. Rarely, bleeding during an ectopic pregnancy is accompanied by fever, which signals the onset of the inflammatory process.
Early ectopic pregnancy: treatment
There is only one possible way to treat pathology - the removal of an ectopic pregnancy by surgery. However, before proceeding with the operation, doctors conduct a diagnosis. External signs of ectopic pregnancy must be confirmed by laboratory and instrumental methods of examination.
There are three ways that help to make a diagnosis:
1) pregnancy can be diagnosed if menstruation is delayed by 2-3 days. To do this, conduct a test for hCG. There are no signs of an ectopic pregnancy yet.
2) After one and a half to two weeks from the start of the delay, an ultrasound examination can be performed. If a fetal egg is not visualized in the area of \u200b\u200bthe uterus, a second appointment will be scheduled in a few days.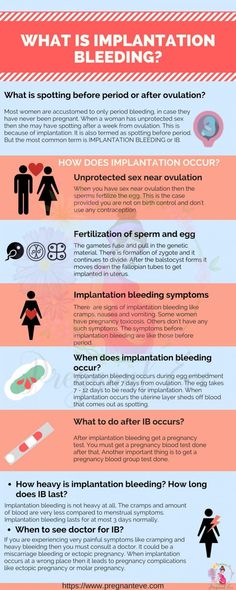 If the same picture is observed at the second appointment, the doctor will suspect an ectopic pregnancy. Early symptoms of an ectopic pregnancy may be absent.
If the same picture is observed at the second appointment, the doctor will suspect an ectopic pregnancy. Early symptoms of an ectopic pregnancy may be absent.
3) fetal heartbeat appears after 2.5-3 weeks. The first early symptoms of an ectopic pregnancy may already appear. On an ultrasound, a growing ovum will be seen in the tubes, ovaries, or abdomen.
Ectopic pregnancy is treated only surgically. At the American Medical Clinic, operations are performed laparoscopically. Often, a woman usually sees a specialist when symptoms of an ectopic pregnancy appear, and the fallopian tube is almost always removed during surgery.
The Department of Operative Gynecology of AMK has everything you need to perform the most complex operations. Our doctors are specialists with extensive experience. They know how to distinguish an ectopic pregnancy and are able to quickly and reliably make a diagnosis. If an operation is necessary, patients are guaranteed an individual approach.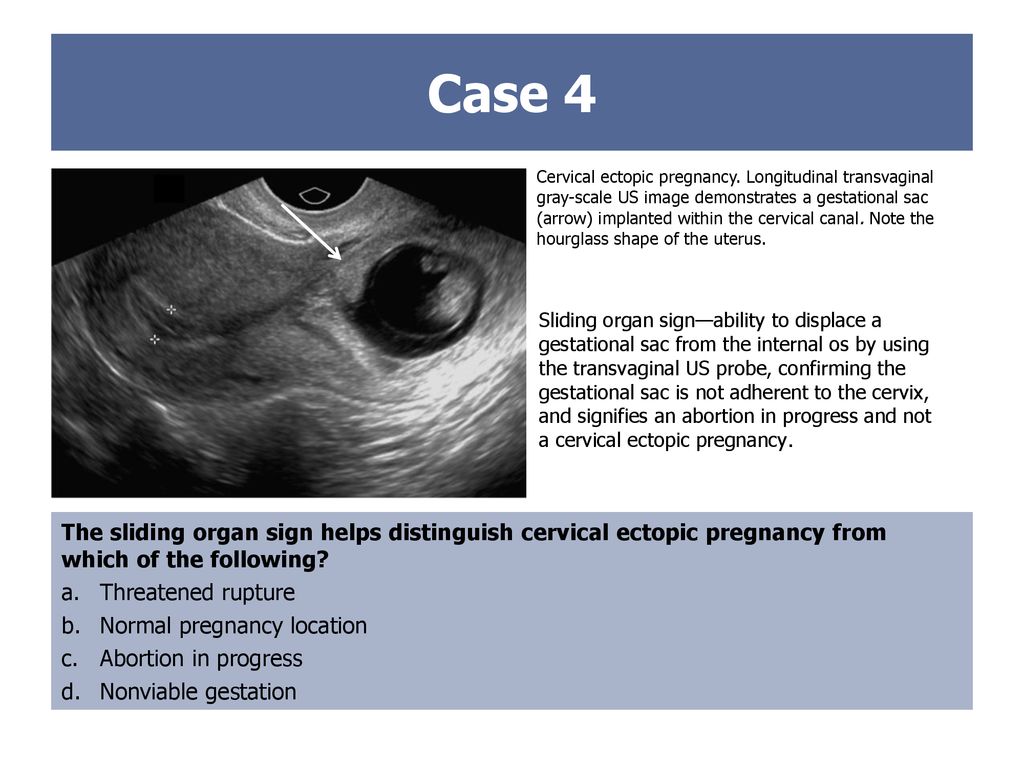 We use only modern techniques and materials that allow us to remove an ectopic pregnancy with a minimal risk of complications.
We use only modern techniques and materials that allow us to remove an ectopic pregnancy with a minimal risk of complications.
Ectopic pregnancy - early signs, first manifestations
home
Articles
Signs of an ectopic pregnancy. How not to miss pathology
According to the latest statistics, ectopic pregnancy accounts for approximately 2% of all pregnancies. At the same time, tubal ectopic pregnancy is most often diagnosed.
Ectopic pregnancy threatens with serious complications - rupture of the fetal egg and peritonitis, recurrence of ectopic pregnancy, infertility. Often it is a threat to a woman's life and, as statistics show, in 3% of all cases it ends in death. Therefore, it is very important to be able to recognize the first signs of an ectopic pregnancy in time.
Further in the article, we will analyze in detail at what time an ectopic pregnancy can manifest itself, its signs in early and late terms, as well as on ultrasound.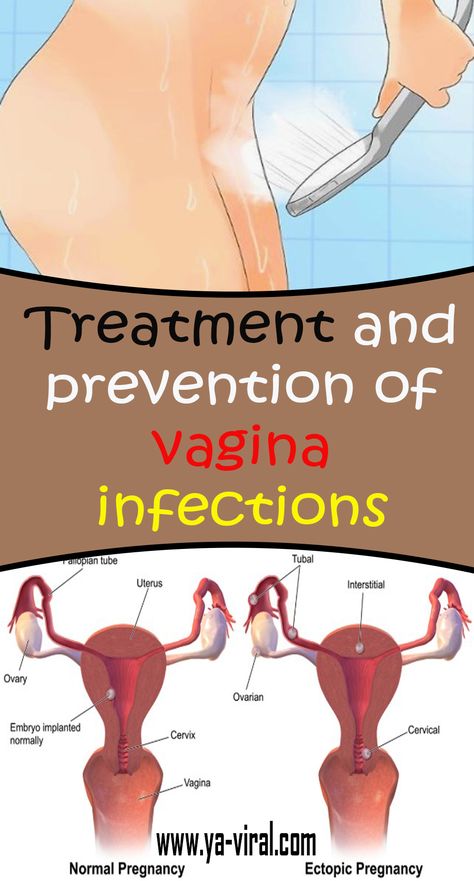
How an ectopic pregnancy manifests itself: the first signs
Given all of the above, it is very important to know how an ectopic pregnancy manifests itself. Timely diagnosis of this pathology will help to avoid complications, and in some cases even save the life of a woman.
In the early stages, women can often ignore unusual symptoms and believe that this is how a normal pregnancy should proceed.
Indeed, as the ovum develops, even with an ectopic pregnancy, a woman may show signs of a normal pregnancy, namely:
- No menses
- Increase in basal body temperature
- Breast engorgement
- Nausea, vomiting
However, along with these symptoms, the first signs of an ectopic pregnancy appear, which should alert. So how does an ectopic pregnancy manifest itself?
The following symptoms may indicate an atypical pregnancy:
- Unpleasant sensations in the lower abdomen, aching, pulling pains in the location of the fetal egg, or in the lower abdomen, mainly on one side - the very first signs of an ectopic pregnancy.
 Pain may increase during urination or defecation.
Pain may increase during urination or defecation. - Scanty bloody, spotting discharge that usually lasts a long time. In rare cases, uterine bleeding, or profuse spotting, resembling menstruation, is observed.
- With severe blood loss in the early stages, signs of shock may occur, namely, pale skin, tachycardia, drop in blood pressure, loss of consciousness.
How long can an ectopic pregnancy appear
The timing when the first signs of an ectopic pregnancy appear is individual in each case. In some women, an ectopic pregnancy can be asymptomatic right up to the development of complications, while in others, adverse symptoms can be noticed already from the first weeks of pregnancy.
Usually, the first signs appear with an increase in the size of the fetal egg. Therefore, at what time an ectopic pregnancy appears can be established using ultrasound. Usually, a fetal egg is visualized at a period of 4.5-5 weeks of pregnancy.
The average time for an ectopic pregnancy to appear is 3 to 8 weeks.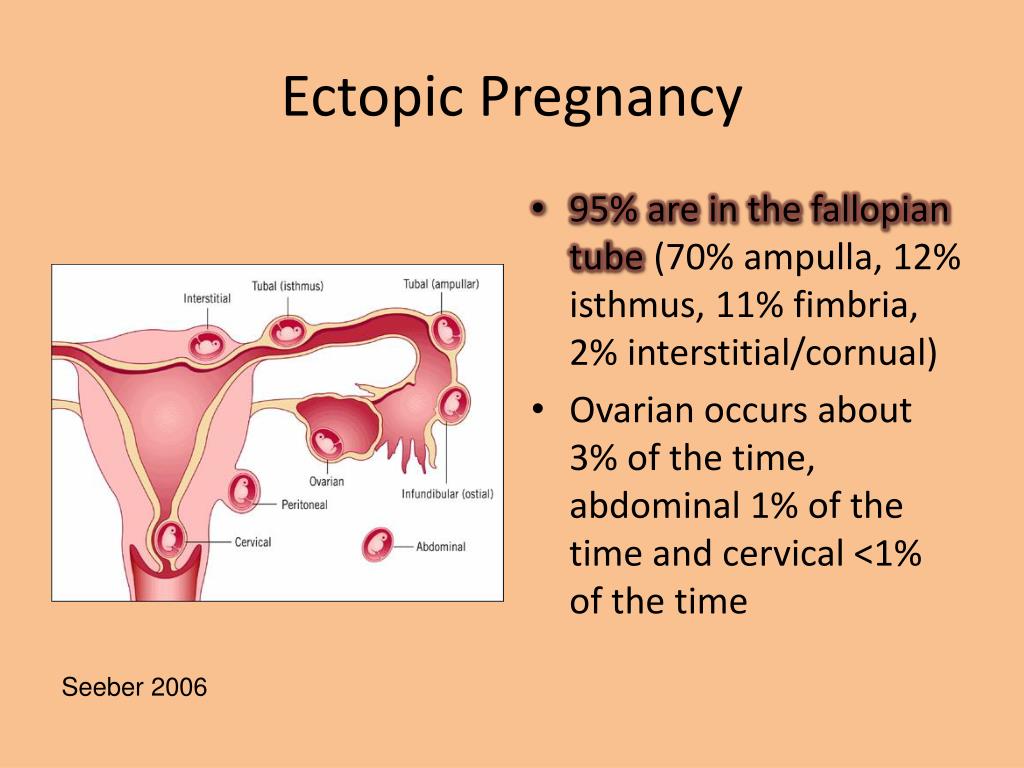 It is during this period that the highest risk of adverse symptoms!
It is during this period that the highest risk of adverse symptoms!
What are the signs of an ectopic pregnancy at a later date
If you ignore the first signs of an ectopic pregnancy, the risk of complications increases significantly. An ectopic pregnancy can have two outcomes - abortion, or rupture of the fallopian tube, or another organ in which the fetal egg has attached.
In the first case, with an ectopic pregnancy, the signs include intense pain, pain in the posterior vaginal fornix, and bleeding. With intense bleeding, symptoms of shock may appear - a decrease in blood pressure, tachycardia, a weak rapid pulse, shallow breathing, weakness, loss of consciousness.
Signs in case of rupture of the fallopian tube resemble those of ovarian apoplexy. Life-threatening internal bleeding develops, acute, dagger pain in the lower abdomen occurs, which can radiate to the perineum and anus, symptoms of shock are expressed. This condition requires immediate hospitalization!
Signs of ectopic pregnancy on ultrasound
With such a pathology as an ectopic pregnancy, ultrasound signs can be determined at about 4.