Pap smear test during pregnancy
Pap smears are safe – before, during and after pregnancy | Women's Health | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Women's Health; Your Pregnancy Matters
August 3, 2021
Women's Health; Your Pregnancy Matters
Yetunde Awosemusi, M. D. Obstetrics and Gynecology
Pregnancy induces changes in your body and your mind. Many mothers-to-be experience anxiety, which can lead some to second-guess their most routine medical procedures. While this mindset is understandable, one thing you can definitely cross off your “worry list” is the myth that Pap smears are not safe during pregnancy.
It is normal to experience some spotting after a Pap smear, even when you are pregnant. However, this natural response has caused some misconceptions that the Pap smear, a potentially life-saving procedure, isn’t safe during pregnancy.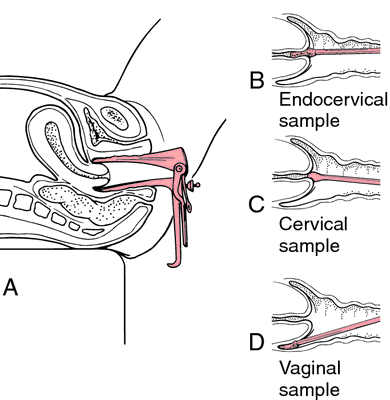
The truth is that getting a Pap smear is safe for you and your baby; it will not cause a miscarriage.
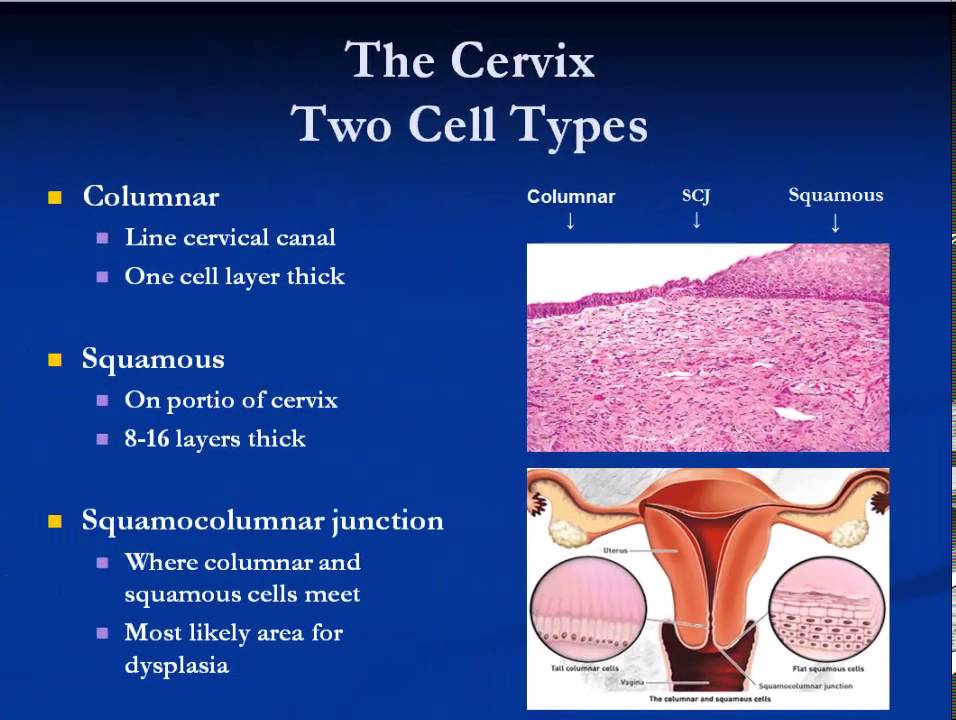
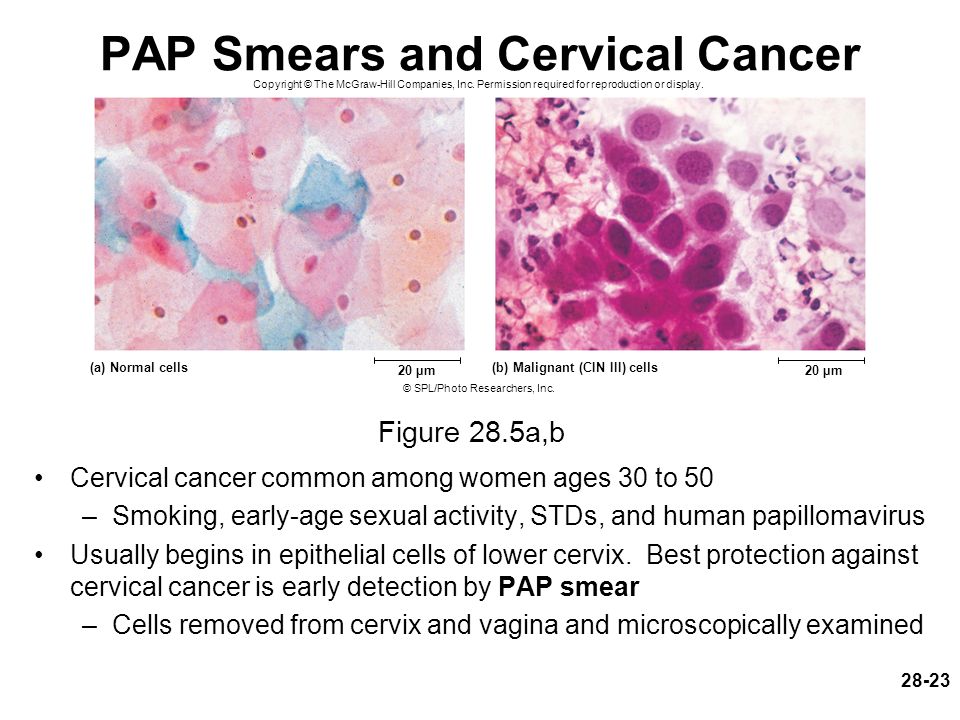
Whether you’re pregnant or not, the Pap smear is the gold standard for screening for cervical cancer. It allows us to collect cells from the surface of the cervix and examine them for abnormalities.
Cervical cancer and abnormal Pap smear results are almost always caused by the human papillomavirus (HPV), a sexually transmitted disease currently infecting around 80 million people in the United States. Though the virus is common, the likelihood of it causing cancer is much less common. In fact, most infections go away on their own. Cancer develops when the infection isn’t detected and managed appropriately, which is why Pap smears are so important.
Data from the Centers for Disease Control and Prevention (CDC) show that cervical cancer deaths have decreased over the last several decades as a result of increased Pap smears. If you follow up on your Pap smear results as recommended by your provider, we almost always will catch the cancer.
What’s even more encouraging is that the HPV vaccine, which the CDC recommends for all children ages 11 or 12, can prevent cervical cancer from developing. We still recommend routine Pap smears for people who receive the vaccine, but we are finding very low rates of abnormal Pap smears within this vaccinated population.
As more people recognize the importance of regular Pap smears, questions about the procedure continue to swirl. We’ve answered the most common ones below.
How often should I get a Pap smear?
We recommend a Pap smear every three years for women between the ages of 21 and 30. If your results are normal and you are negative for HPV, you can extend that to every five years from ages 31 to 65. Higher-risk populations, such as people who have an autoimmune disease, should discuss more frequent testing with their provider.
Do I need a Pap smear when I’m pregnant?
Reviewing your Pap smear history is an early, important step during prenatal care.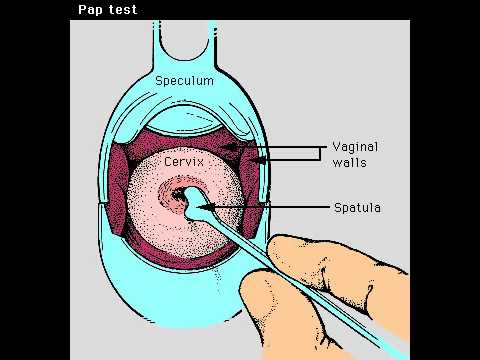 If you received a normal test result within the last three years, you likely don’t need a Pap smear while pregnant.
If you received a normal test result within the last three years, you likely don’t need a Pap smear while pregnant.
We realize, however, that many newly pregnant people are seeing a doctor for the first time in quite a while – maybe their first time ever as an adult – and haven’t had a Pap smear before, or for several years. To support a healthy pregnancy, we want to rule out the possibility of cervical cancer development as soon as possible.
If I do need one, is it safe?
Pap smears while pregnant are safe for you and your baby. Any suggestion that it might cause a miscarriage is false. It is normal to experience minor bleeding after a Pap smear when you are pregnant because blood flow to the uterus increases, which causes the cervix to bleed more easily when touched.
Any type of bleeding is understandably alarming while pregnant, but in this case the blood is coming from the outside of your cervix – not inside the uterus, where the baby is safe and developing.
What happens if I have an abnormal Pap smear?
The next step may be to perform a colposcopy, which allows us to look more closely at the cervix and take a small tissue sample to test the abnormal cells for cancer. The colposcopy is safe during pregnancy – the only cells we touch are on the outside of the cervix, not the inside near your baby.
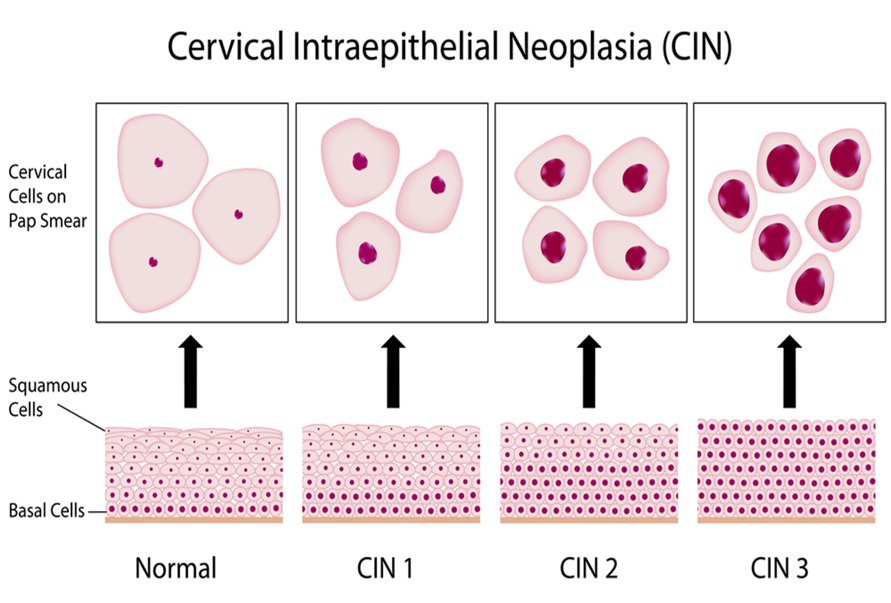
Generally, we divide these test results into what we call low-grade or high-grade “dysplasia” – the existence of abnormal cells:
- Low-grade dysplasia doesn’t usually progress to cancer, so we just watch it and will likely encourage you to come back in a year for another Pap smear.
- High-grade dysplasia has an increased chance of progressing to cancer, so we will likely recommend a loop electrosurgical excision procedure (LEEP) after delivery.
LEEP removes the outside portion of the cervix containing the abnormal cells, and it can increase the risk of pregnancy complications like preterm birth or losing the baby in the second trimester. Because cervical cancer is a slow-growing disease, we can usually postpone the procedure until after delivery and watch the area closely, performing a colposcopy every trimester to monitor the dysplasia’s progress.
Because cervical cancer is a slow-growing disease, we can usually postpone the procedure until after delivery and watch the area closely, performing a colposcopy every trimester to monitor the dysplasia’s progress.
Pregnancy weakens the immune system, which can increase the likelihood of abnormal results, so sometimes the high-grade dysplasia resolves itself after pregnancy. If it does progress to cancer, we will work with you to develop a personalized treatment plan that incorporates your specific health conditions and needs. As an academic medical center, we can streamline your access to some of the best oncologists in the U.S., right here at UT Southwestern.
If you need a Pap smear, it is safe to get one during pregnancy. Along with the HPV vaccine, Pap smear is a vital tool that helps make cervical cancer preventable – and it will give you one less thing to worry about as you prepare for the healthy birth of your baby.
To visit with an Ob/Gyn or certified nurse-midwife, call 214-645-8300 or request an appointment online.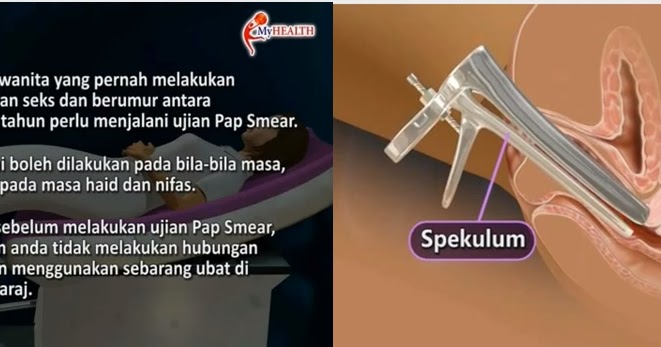
More in: Women's Health, Your Pregnancy Matters
Men's Health; Prevention; Women's Health
- Safia Khan, M.D.
- Zaiba Jetpuri, D.O.
December 28, 2022
Women's Health
- Patrick M.
 Weix, M.D., Ph.D.
Weix, M.D., Ph.D.
December 8, 2022
Plastic Surgery; Women's Health
- Abby Culver, M.D.
- Christine Carman Stiles, M.D.
December 5, 2022
Women's Health
- Maude Carmel, M.
 D.
D.
October 17, 2022
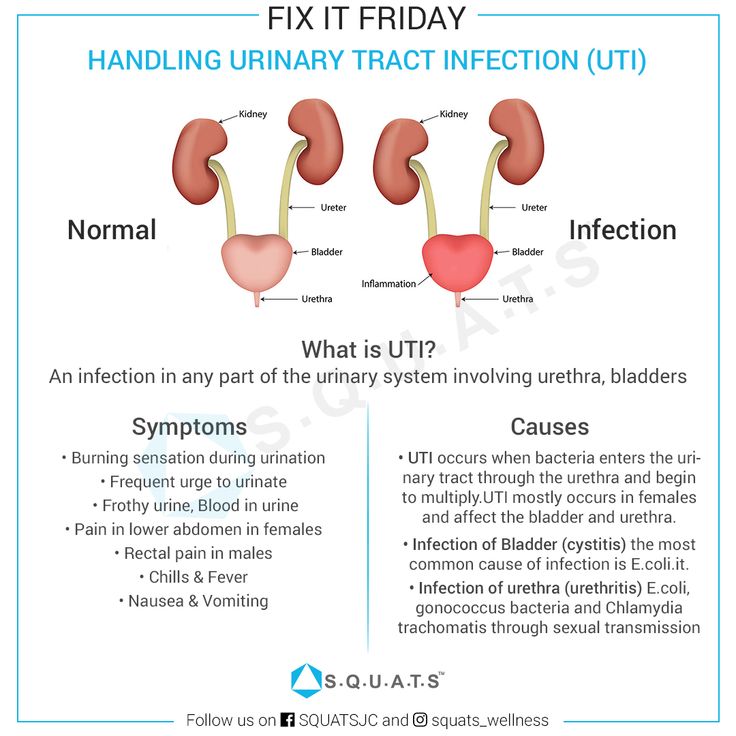
Men's Health; Women's Health; Your Pregnancy Matters
- Yair Lotan, M.D.
September 6, 2022
Pediatrics; Women's Health
- Nirupama DeSilva, M.
 D.
D. - Jason Jarin, M.D.
August 31, 2022
Women's Health
- Abey Eapen, M.D., Ph.D.
August 18, 2022
Men's Health; Women's Health
July 26, 2022
Prevention; Women's Health
- Andrea Jochim, M.
 D., Ph.D.
D., Ph.D.
July 25, 2022
More Articles
Cervical screening during pregnancy | Pregnancy Birth and Baby
Cervical screening during pregnancy | Pregnancy Birth and Baby beginning of content5-minute read
Listen
You may be wondering if it’s safe to have a cervical screening test while you’re pregnant, and whether the benefits outweigh any risks. Routine cervical screening is the best way to protect yourself against cervical cancer. Of the 800 women diagnosed with cervical cancer each year in Australia, 1 in 5 were never screened or were not up to date with screening.
What is cervical screening?
Cervical screening is a simple way to check the health of your cervix.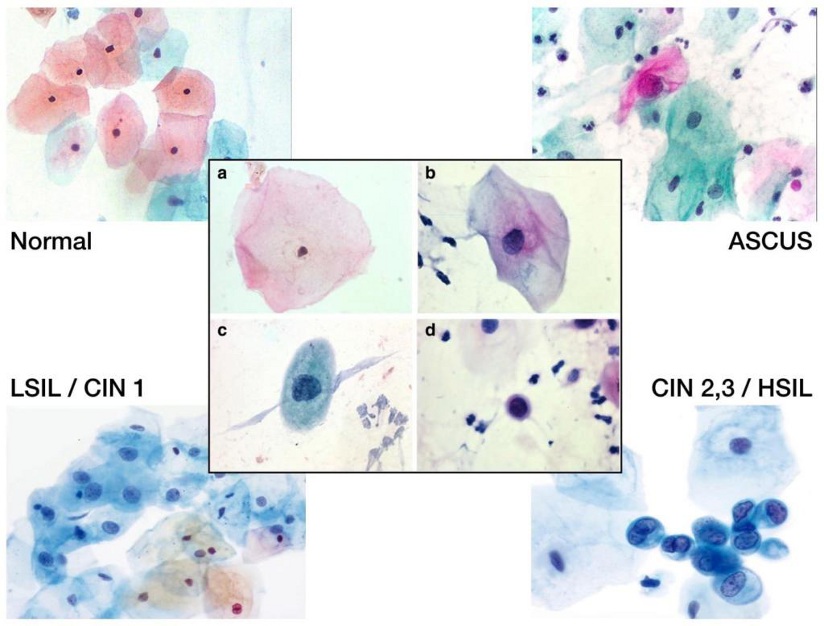 The cervix is the opening of the womb (uterus) at the top of the vagina. The cervical screening test looks for evidence of human papillomavirus (HPV), is a virus that can cause changes to cells in your cervix — which can develop into cervical cancer.
The cervix is the opening of the womb (uterus) at the top of the vagina. The cervical screening test looks for evidence of human papillomavirus (HPV), is a virus that can cause changes to cells in your cervix — which can develop into cervical cancer.
The cervical screening test has replaced the Pap test (or, ‘smear’), which was offered to women every 2 years.
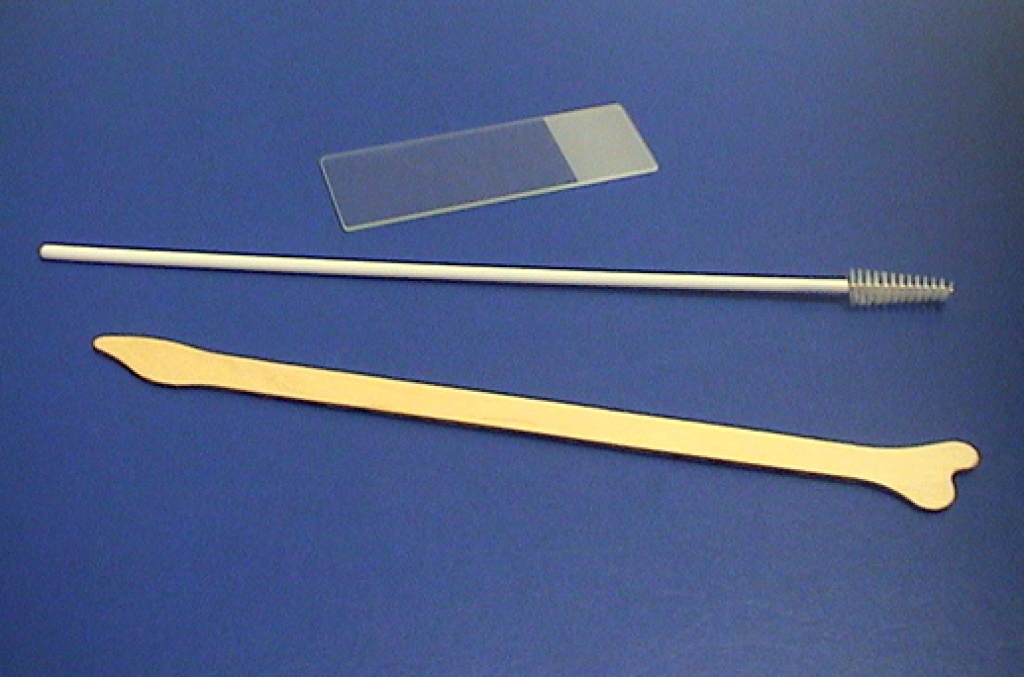
During a cervical screening test, an instrument called a speculum is gently inserted into the vagina, so the health provider performing the screen can see your cervix. A soft spatula or ‘broom’ type brush is then used to collect the sample. The cervical screening test looks and feels the same as the Pap test. The procedure might feel a bit uncomfortable but shouldn’t hurt.
How often should I have a cervical screening test?
Cervical screening can be done every 5 years, if your results are normal. You should have the test if:
- you’re aged between 25 and 74 years
- you have ever been sexually active
- you have a cervix
If you’ve had a Pap test before, your first cervical screening test should be 2 years after your last Pap test.
It’s best to start cervical screening at 25 years of age — studies show there’s no extra benefit to testing women under 25. While women under 25 don’t need routine cervical screening, if you have pain during sex, or unusual bleeding or discharge at any age, see your healthcare provider as soon as you can.
If you are under 25 years and were previously screened, and received an abnormal test result, you should continue to follow your doctor's advice.
Checkups, scans and tests during pregnancy
Learn more about what checkups, scans and tests you can have during pregnancy.
I'm pregnant — can I have a cervical screening test?
Cervical screening can be performed at any time, including before becoming pregnant and during your pregnancy. Your pregnancy might be the first chance your healthcare provider has to offer you a cervical screening test. Cervical cancer tends to be diagnosed in women who aren’t routinely screened.
Is it part of standard antenatal care?
You may be asked about your cervical screening history during your first antenatal visit, and offered cervical screening if you haven't had one within the recommended time. This is an important opportunity to take steps to keep yourself healthy and well, throughout your pregnancy and beyond.
This is an important opportunity to take steps to keep yourself healthy and well, throughout your pregnancy and beyond.
What is 'self-collection' cervical screening and can this be done during pregnancy?
Self-collection is where you are shown how to collect your own sample for cervical screening.
You may be offered the option of self-collection of a vaginal swab for HPV testing. Your healthcare provider should outline the process and discuss the small risk of bleeding or spotting that may occur because of this test.
In some instances, if the test returns a positive result, you may be asked to return to your doctor so they can perform another test.
Is there any danger to the baby?
It’s safe to have a cervical screening test during your pregnancy. The benefits to your health outweigh any risks to your baby.
Whatever the outcome of the screening test, it’s generally safe to continue your pregnancy — since HPV infection during pregnancy doesn’t usually affect the baby.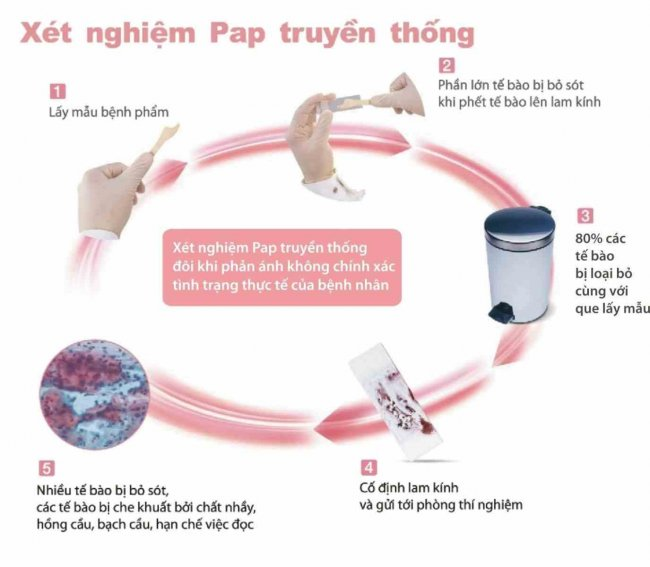 Even if there are abnormal cells on the cervix, it’s very rare for this to progress into cancer during a pregnancy.
Even if there are abnormal cells on the cervix, it’s very rare for this to progress into cancer during a pregnancy.
That’s why, in most cases, your healthcare provider will wait until after your baby is born to do a repeat test and, if necessary, treat cervical cancer.
What happens if the result is not normal?
If your test shows you have HPV, your healthcare provider will monitor the infection and is likely to recommend further tests to better understand the changes to your cervical cells. Even when results show an HPV infection, it normally takes 10 or more years for it to develop into cervical cancer. Only about 1 in 20 pregnant women will have abnormal cervical cells after further investigation.
Sources:
National Cervical Screening Program (Self-collection and the Cervical National Screening Test: Factsheet), National Cervical Screening Program (About the test), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Cervical screening in Australia), National Cervical Screening Program (Guidelines for the management of screen-detected abnormalities, screening in specific populations and investigation of abnormal vaginal bleeding. Screening in Pregnancy Screening in Pregnancy), Australian Government Department of Health (Pregnancy Care Guidelines: Antenatal Visits), Cancer Council Australia (Cervical cancer screening: summary of recommendations)
Screening in Pregnancy Screening in Pregnancy), Australian Government Department of Health (Pregnancy Care Guidelines: Antenatal Visits), Cancer Council Australia (Cervical cancer screening: summary of recommendations) Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Check-ups, tests and scans available during your pregnancy
- Routine antenatal tests
- Your first antenatal visit
- Antenatal care during your pregnancy
Need more information?
Understanding your Pap test or cervical screening test results | Cancer Council
The Pap test (sometimes called the Pap smear) has changed to the cervical screening test. Find out about how the changes impact you here
Find out about how the changes impact you here
Read more on Cancer Council Australia website
Cervical Screening | Pap Smear | Jean Hailes
All you need to know about cervical screening tests and how they differ from pap smears. Learn why and when you should have one and how they work.
Read more on Jean Hailes for Women's Health website
Pap smear tests - MyDr.com.au
Pap smear tests are currently used in Australia as a screening test for cervical cancer. A Pap smear test can detect changes in the cells of the cervix that may develop into cancer.
Read more on myDr website
Pap Smear Tests | Cervical Screening Tests - Sexual Health Victoria
Cervical Screening (formerly Pap Smear or Pap Test) is a 5-yearly test for those between the ages of 25 – 74 years, to check cervical health. Book an appointmen
Book an appointmen
Read more on Sexual Health Victoria website
Your questions answered on cervical screening tests | Know Pathology Know Healthcare
A cytologist answers questions about cervical cancer screening and why you should get up to date
Read more on Know Pathology Know Healthcare website
Cervical Cancer - Frequently Asked Questions
Frequently asked questions of the Australian Cervical Cancer Foundation. FAQ
Read more on Australian Cervical Cancer Foundation website
Cervical cancer screening | Cancer Council
Read about the cervical screening program designed to work together with the HPV vaccination program, to help reduce the incidence of cervical cancer
Read more on Cancer Council Australia website
What happens if your cervical screening test is positive? | Know Pathology Know Healthcare
Find out how cervical screening tests are performed and what happens when a cervical screening test is positive for HPV
Read more on Know Pathology Know Healthcare website
Cervical screening: what health professionals wish you knew | Know Pathology Know Healthcare
The people who perform your tests told us their messages to women about cervical screening, cancer and why vaccinated and young women still need the test
Read more on Know Pathology Know Healthcare website
Samantha’s story - Surviving HPV related cancer | Australian Government Department of Health and Aged Care
Samantha survived a rare but aggressive form of cervical cancer that her doctor said was highly likely caused by human papillomavirus (HPV). She urges all parents to sign the consent form so their child can be protected against HPV related disease as part of the school based immunisation program.
She urges all parents to sign the consent form so their child can be protected against HPV related disease as part of the school based immunisation program.
Read more on Department of Health and Aged Care website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.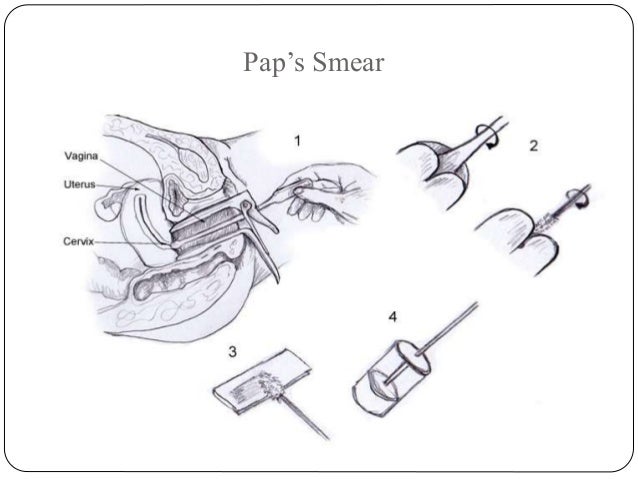
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Cytology smear | KGBUZ "Vladivostok Polyclinic No. 6"
29 Jun 2015
[dt_sc_hr_invisible]
[dt_sc_callout_box type="type2" button_text="On map" target="_blank ]
A smear for cytology can be taken at
st. Borisenko d. 29 examination room (room 3)
[/dt_sc_callout_box]
[dt_sc_clear]
A cytology smear - (presence of atypical cells) is a laboratory diagnostic method that allows you to detect pathological abnormalities in the cells of the cervix.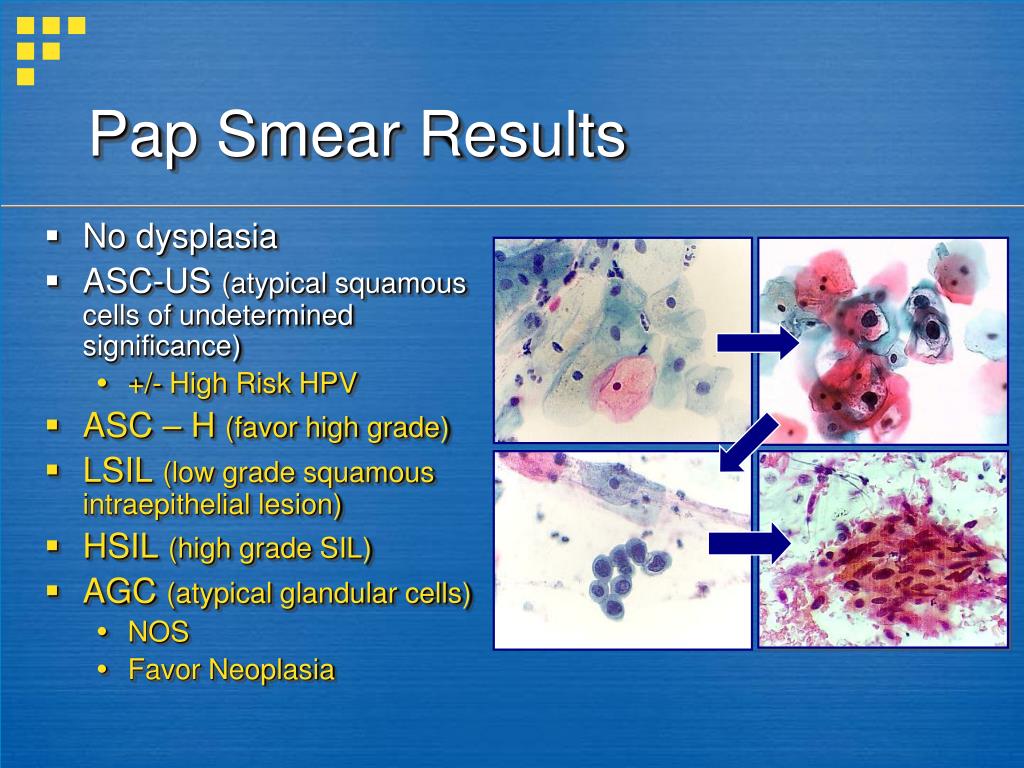 Other names for this analysis are Pap test and Pap smear. This analysis is assigned not only to pregnant women, but also to every woman who has reached the age of 18 with a frequency of once a year. During pregnancy, it is given when registering for the management of a pregnant woman, and if a woman has erosion (ectopia) of the cervix, it is also repeated at the 30th week of pregnancy. nine0003
Other names for this analysis are Pap test and Pap smear. This analysis is assigned not only to pregnant women, but also to every woman who has reached the age of 18 with a frequency of once a year. During pregnancy, it is given when registering for the management of a pregnant woman, and if a woman has erosion (ectopia) of the cervix, it is also repeated at the 30th week of pregnancy. nine0003
- In addition to pregnancy, there are other indications for this test:
- menstrual disorder
- infertility
- genital herpes;
- taking hormonal contraceptives;
- human papillomavirus (HPV)
- obesity
- before placing an intrauterine device in a woman
- in the presence of a large number of sexual partners;
- when planning a pregnancy. nine0020
Before giving a smear for cytology, a woman is recommended to exclude all sexual contacts for two days, do not douche, do not use vaginal preparations (lubricants, creams, suppositories). Immediately before visiting the doctor for the last time, you need to empty your bladder 2-3 hours before the appointment. If a woman has specific discharge or itching in the vagina, then the smear should be postponed until a complete cure.
Immediately before visiting the doctor for the last time, you need to empty your bladder 2-3 hours before the appointment. If a woman has specific discharge or itching in the vagina, then the smear should be postponed until a complete cure.
The procedure for taking a smear for a cytological examination is the same as for taking a smear for the vaginal microflora. When conducting an internal gynecological examination, cells are taken from the inner and outer surfaces of the cervix using a special brush. The procedure itself is short (about 10 seconds) and practically imperceptible. In some women, as a result of scraping, the site of taking a smear may bleed a little for one to two days, which manifests itself as spotting spotting from the genital tract. According to the results of a smear for cytology, an assessment of cervical cells is carried out - their number, shape, size, nature of location. All these parameters together give a complete picture of the general condition of the cervix and allow for an accurate diagnosis of background, cancerous and precancerous diseases of the cervix.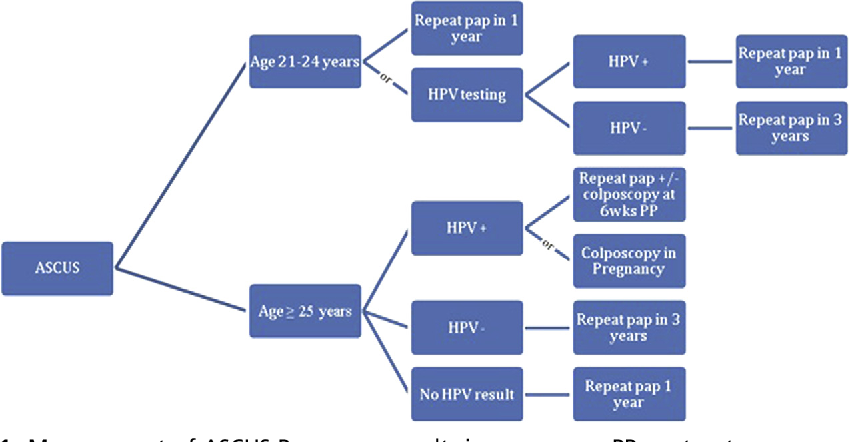 The results of a smear are considered normal (negative) when absolutely all cells are of the correct shape and size, and no abnormal cells are found. If the results of the smear are bad, then the doctors put one of the following conclusions: “atypia”, “dysplasia of the 1st, 2nd or 3rd degree”. If dysplasia of the first degree is detected, a woman will need to retake the test after five to six months. If atypical (pathological, cancerous) cells are found in a smear for cytology, a woman will need an additional examination, which consists in repeating a cytological examination after a while, as well as in conducting a colposcopic examination with taking cervical tissues for a biopsy. Thanks to such methods of examination, the doctor will clarify the diagnosis and decide on the further treatment of the patient. An important point is that during pregnancy, colposcopy with cell biopsy is practically not performed for women, only in exceptional cases. Usually they wait until a woman gives birth to a child, unless there is a direct threat to the life and health of both the mother herself and her baby.
The results of a smear are considered normal (negative) when absolutely all cells are of the correct shape and size, and no abnormal cells are found. If the results of the smear are bad, then the doctors put one of the following conclusions: “atypia”, “dysplasia of the 1st, 2nd or 3rd degree”. If dysplasia of the first degree is detected, a woman will need to retake the test after five to six months. If atypical (pathological, cancerous) cells are found in a smear for cytology, a woman will need an additional examination, which consists in repeating a cytological examination after a while, as well as in conducting a colposcopic examination with taking cervical tissues for a biopsy. Thanks to such methods of examination, the doctor will clarify the diagnosis and decide on the further treatment of the patient. An important point is that during pregnancy, colposcopy with cell biopsy is practically not performed for women, only in exceptional cases. Usually they wait until a woman gives birth to a child, unless there is a direct threat to the life and health of both the mother herself and her baby.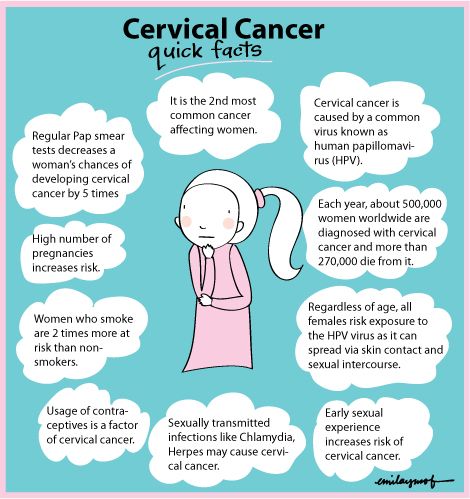 nine0003
nine0003
On the basis of the Territorial Center for Disaster Medicine, a hotline has been set up to discuss the availability and quality of free medical care. Calls from citizens are accepted by phone 8 (423) 260-50-98 around the clock.
Official information about the coronavirus in Russia on the portal - stopcoronavirus.rf, a single hotline - 8-800-2000-112.
"Hot line" of Roszdravnadzor on observance of the rights of citizens in the field of health protection - 8 800 550 99 03
Cytological smear (Pap smear, Pap test)
In recent years, oncological diseases have become more common, including endometrial and cervical cancer. For their diagnosis, a method such as a Pap test or a Pap test is used, which allows you to identify cancer cells in the secret of the vagina. The technique is quite simple, painless for the patient and gives results with high accuracy, but in Perm such a study is not carried out in every clinic.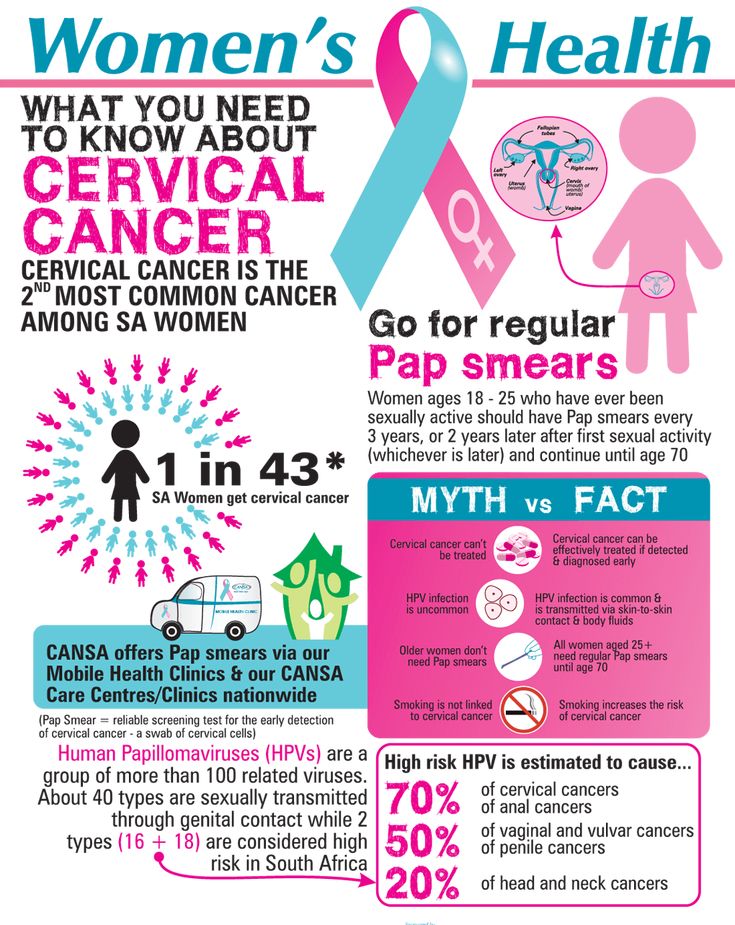 We are ready to offer our patients to make a smear for a Pap test. nine0003
We are ready to offer our patients to make a smear for a Pap test. nine0003
Pap smear at a glance
The analysis refers to a cytological procedure in which the resulting sample is stained with special formulations. The material is taken by scraping from the upper layer of the cervix, and after staining, it is studied under a microscope. In addition to endometrial cancer, the Pap test can also detect oncology in other organs:
- in the lungs;
- in the stomach;
- in the bladder.
Other biological secretions such as urine, feces or sputum are collected from patients for this purpose. A Pap test can also be used to examine tissue samples taken from a biopsy. nine0003
Women are more likely to be diagnosed with cervical cancer using this technique than other types of cancer. To obtain a biomaterial, the patient sits in a gynecological chair, then a scraping is taken from the transition zone of the cervix. The resulting sample is applied to a glass slide, fixed, stained and examined under a microscope.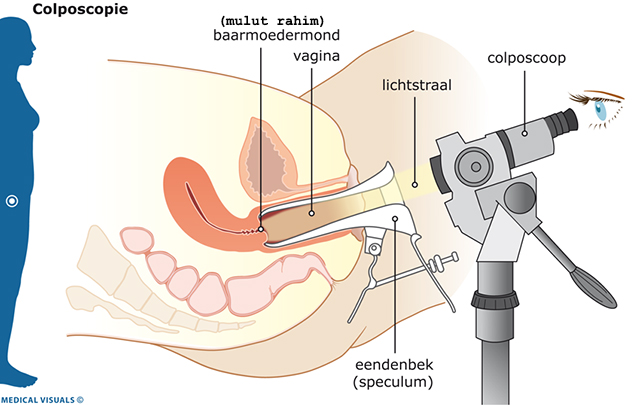 An experienced laboratory assistant will immediately see oncological or abnormal cells if they are present in the material.
An experienced laboratory assistant will immediately see oncological or abnormal cells if they are present in the material.
How to prepare for a Pap smear
The material is taken for examination during a standard gynecological examination in cases where the woman is not taking contraceptives and hormonal drugs. These drugs can change the composition of the mucus and top layer of the cervix, making it more likely to give an erroneous result.
Rules for preparing for the test:
- stop sexual intercourse two days in advance;
- stop injecting drugs into the vagina, and do not douche or put cotton swabs two days before the due date; nine0020
- be tested for cervicitis, if found, treat if possible.
Pap smears for follow-up cytology may be performed on any day except menstruation. Also, the material is not taken if there is bleeding from the uterus. If necessary, a Pap test can be done during menstruation, but the effectiveness will be significantly reduced.